Professional Documents
Culture Documents
IVF in The US: Multiple Gestation, Economic Competition, and The Necessity of Excess
Uploaded by
durgesh yadavOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
IVF in The US: Multiple Gestation, Economic Competition, and The Necessity of Excess
Uploaded by
durgesh yadavCopyright:
Available Formats
K.
Faber
predictive value of transvaginal Doppler ultrasonography in an in-vitro unfertilized and presumed parthenogenetically activated human oocytes
fertilization programme: a preliminary study. Hum. Reprod., 12, 191–196. demonstrates a high frequency of sperm penetration. Hum. Reprod., 9,
Dokras, A., Sargent, L., Ross, C. et al. (1991) The human blastocyst: 2381–2388.
morphology and human chorionic gonadotropin secretion in vitro. Hum. Van Blerkom, J., Davis, P. and Lee, J. (1995) ATP content of human oocytes
Reprod., 6, 1143–1151. and developmental potential and outcome after in-vitro fertilization and
Dokras, A., Sargent, L., and Barlow, D. (1993) Human blastocyst grading: an embryo transfer. Hum. Reprod., 10, 415–454.
indicator of developmental potential? Hum. Reprod., 8, 2119–2127. Van Blerkom, J., Antczak, M. and Schrader, R. (1997) The developmental
Faber, K. (1997) IVF in America: Multiple gestations, economic competition, potential of the human oocyte is related to the dissolved oxygen content of
the necessity of excess. Hum. Reprod., 12, 1614–1616. follicular fluid: association with vascular endothelial growth factor levels
Feng, H., Wen., X., Amet, T. and Presser, S. (1996) Effect of different co and perifollicular blood flow characteristics Hum. Reprod., 12, 1610–1614.
culture systems in early human embryo development. Hum. Reprod., 11, Vlad, M., Walker, D., and Kennedy, R. (1996) Nuclei number in human
1525–1528. embryos co-cultured with human ampullary cells. Hum. Reprod., 11,
Fujino, Y., Ozaki, K., Yamamusi, S., Ito, F. et al. (1996) DNA fragmentation 1678–1686.
of oocytes in aged mice. Hum. Reprod., 11, 1480–1483. Wall, M., Marks, K., Smith, T. et al. (1996) Cytogenetic and fluorescent in-
Gardner, D., Lane, M., Calderone, I. and Leeton, J. (1996) Environment of situ hybridization chromosomal studies on in-vitro fertilized and
intracytoplasmic sperm injected ‘failed–fertilized’ human oocytes. Hum.
Downloaded from https://academic.oup.com/humrep/article/12/8/1614/700082 by guest on 26 February 2022
the preimplantation human embryo in vivo: metabolite analysis of oviduct
and uterine fluids and metabolism of cumulus cells. Fertil. Steril., 65, Reprod., 11, 2230–2238.
349–353. Winston, N., Braude, P., Pickering, S. et al. (1991) The incidence of abnormal
Gregory, L., Booth, A., Wells, C. and Walker, S. (1994) A study of the morphology and nucleocytoplasmic ratios in 2-, 3- and 5-day human pre-
cumulus–corona cell complex in in-vitro fertilization and embryo transfer, embryos. Hum. Reprod., 6, 17–24.
a prognostic indicator of the failure of implantation. Hum. Reprod., 9, Zenzes, T., Wang, P. and Casper, R. (1992) Evidence for a maternal
1308–1317. predisposition to chromosomal aneuploidy in multiple oocytes of some
Hardy, K., Handyside, A. and Winston, R. (1989) The human blastocyst: cell in vitro fertilization patients. Fertil. Steril., 57, 1396–1401.
number, death and allocation during late preimplantation development
in vitro. Development, 107, 597–604.
Kligman, l., Benadiva, C., Alikani, M. and Munné, S. (1996) The presence
of multinucleated blastomeres in human embryos is correlated with
IVF in the US: multiple gestation,
chromosomal abnormalities. Hum. Reprod., 11, 1492–1498. economic competition, and the
Kumat, B., Brown, L., Manseau, E. et al. (1995) Expression of vascular
permeability factor/vascular endothelial growth factor by human granulosa
necessity of excess
and theca lutein cells. Role in corpus luteum development. Am. J. Pathol.,
146, 157–165 Kenneth Faber
Magli, M., Gianaroli, L., Fiorentino, A. et al. (1996) Improved cleavage rate
of human embryos cultured in antibiotic-free medium. Hum. Reprod., 11, University of Colorado Health Sciences, Colorado
1520–1524. Reproductive Endocrinology, 3600 E Alameda Suite 220,
Magnusson, C., Hillensjo, T., Hamberger, L. and Nilsson. L. (1986) Oxygen Denver, Colorado 80209, USA
consumption by human oocytes and blastocysts grown in vitro. Hum.
Reprod., 3, 183–184.
Munné, S., Lee, A., Rosenwaks, Z. et al. (1993) Diagnosis of major
chromosomal aneuploidies in human preimplantation embryos. Hum.
In the practice of advanced reproductive medicine we have
Reprod., 8, 2185–2191. progressed from the miracle baby to the day of the litter. In a
Nargund, G., Bourne, T., Doyle, P. et al. (1996) Association between ultrasound few short years we have radically changed the incidence of
indices of follicular blood flow, oocyte recovery, and preimplantation multiple gestation, yet we have virtually no idea of the long-
embryo quality Hum. Reprod., 11, 109–113.
Quinn, P., Moinipanah, R., Steinberg, J. and Weathersbee, P. (1995) Successful
term impact these changes will have on our patients, their
human in vitro fertilization using a modified human tubal fluid medium children or society. There is ample evidence of the immediate
lacking glucose and phosphate ions. Fertil. Steril., 63, 922–924. costs of treating these complicated pregnancies and an entire
Turner, K. and Lenton, E. (1996) The influence of Vero cell culture on human practice, almost a growth industry itself, of multifetal reduction
embryo development and chorionic gonadotrophin production in vitro. Hum.
Reprod., 11, 1966–1974. has been born as a result of the practice patterns of infertility
Urner, F., Bianchi, P., Campana, A. and Sakkas, D. (1993) Evidence for sperm specialists in the US. Clearly, the progressive increase in
entry into assumed unfertilized human oocytes after subzonal sperm pregnancy rates that has occurred in most programmes reflects
microinjection. Hum. Reprod., 8, 2167–2173.
the additive effects of improvements in the clinical management
Van Blerkom, J. (1993) Development of human embryos to the hatched
blastocyst stage in the presence or absence of a monolayer of Vero cells. of patients and in laboratory methods. With increased success
Hum. Reprod., 8, 1525–1539. has come the now commonplace occurrence of higher order
Van Blerkom, J. (1994a) Intrinsic factors affecting the outcome of laboratory gestations and the ‘epidemic’ of multifetal reductions. I believe
assisted conception in the human. In Van Blerkom, J. (ed.), The Biological
Basis of Early Reproductive Failure in the Human: Applications to that the roots of this phenomenon lie not in the inability
Medically-Assisted Conception. Oxford University Press, Oxford, UK, pp. among in-vitro fertilization (IVF) practitioners to recognize
3–27. this dramatic change in outcome, but rather in the nature
Van Blerkom, J. (1994b) Developmental failure in human reproduction of competition among IVF clinics with similar levels of
associated with chromosomal abnormalities and cytoplasmic pathologies in
meiotically mature human oocytes. In Van Blerkom, J. (ed.), The Biological competence, and the intentions of those providing these services
Basis of Early Reproductive Failure in the Human: Applications to to attract new infertility patients or maintain those already in
Medically-Assisted Conception. Oxford University Press, Oxford, UK, pp. their programme. It is my belief that such pregnancies represent
283–325.
Van Blerkom, J. (1996) The influence of intrinsic and extrinsic factors on the a failure rather than a success of the IVF enterprise.
developmental potential and chromosomal normality of the human oocyte. Selective intrauterine abortion is only the most obvious
J. Soc. Gynecol. Invest., 3, 3–11. symptom of the larger issue of multiple gestation. I believe
Van Blerkom, J. and Henry, G. (1992) Oocyte dysmorphism and aneuploidy
in meiotically-mature human oocytes after ovarian stimulation. Hum.
the rightness or wrongness of this practice has nothing to do
Reprod., 7, 379–390. with the abortion issue. Regardless of the pro-life feelings of
Van Blerkom, J., Davis, P. and Merriam, J. (1994) A retrospective analysis of a patient, she cannot ignore the poor outcome of higher order
1614
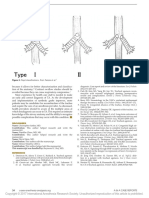
Embryo transfer and multiple gestation
multiple gestations. She must face the real possibility of having deliveries, one of the children has a significant developmental
no healthy children if she were to continue such a pregnancy. delay (Evans et al., 1990).
Likewise, very few infertility patients start care with the idea Prospective patients may not appreciate the incidence of
of one day having to make a decision regarding abortion. multiple gestation or the need for eventual reduction. While
Thus, in the individual case the morality of multifetal reduction pregnancy rates are published and disseminated among infertil-
has little relevance, it is a matter of making the best of a ity support group members, the risks of treatment may not be
bad situation as the patient’s conscience allows. The ethical as well appreciated. As long as this continues, physicians will
dilemma of multifetal reduction relates to its role in only be encouraged to place higher numbers of embryos to
encouraging clinicians to increase the risk of its necessity by increase their pregnancy rates, with the obvious result of
exonerating their irresponsible practices. The ethical conflict increasing multiple gestation.
is magnified by the fact that the clinic reports these pregnancies A recent survey of infertility patients clearly demonstrated
as a success while it is ultimately left to the patients to deal that they overwhelmingly desire multiple gestation (Gleicher
Downloaded from https://academic.oup.com/humrep/article/12/8/1614/700082 by guest on 26 February 2022
with the psychological consequences of fetal reduction and et al., 1995). Only half of these couples objected to triplets
financial and emotional consequences attendant with three, and 20% found quadruplets acceptable. To the patients, failure
four or even five babies if reduction is not elected. is defined as a negative pregnancy test. The physicians must
The incidence of multiple gestation has continued to increase decide their role in this conflict. Do they act as the patients’
[Society for Assisted Reproductive Technology (SART) and agent in providing the outcome they desire, or do they attempt
The American Society for Reproductive Medicine (ASRM), to educate and even deny the service that the patient desires?
1996]. One might have predicted that clinicians would change As providers we must look beyond a laboratory test and to
their practice in order to maintain acceptable pregnancy rates the health of the mother during the pregnancy and to the health
while limiting the multiple pregnancy rate. In fact, every of the children that result. Despite the fact that multiple
ASRM/SART report shows only higher multiple rates (SART/ gestation accounts for the majority of neonatal morbidity in
ASRM, 1996). The easy access and improving success of IVF patients (Tan et al., 1992), some fertility care providers
multifetal reduction allows clinicians to place embryos without see their role as accommodating the patients’ desire for this
enough concern about multiple pregnancies. Thus, the relation- outcome. Rather than educate their patients about the risk of
ship between the infertility specialist and the one who cleans permanent disability to children of higher order gestation,
these providers apparently believe that this is an issue of
up the mistakes is a symbiotic one. By making the complicated
patient choice. The physician–patient relationship implies that
pregnancy someone else’s problem, the incidence of the
the physician will act in the patient’s best interest; that
problem only increases.
responsibility cannot be abdicated, regardless of the patient’s
We cannot know the precise extent of multiple gestations that
desires or the possible impact on the economic health of the
result from assisted reproductive technology (ART) procedures.
physician’s practice. It is simply wrong to practice medicine
The last summary from the ASRM/SART reports results from
in any way that does not minimize the risk of complications.
clinics in 1994 and demonstrated a 36.3% multiple pregnancy
If no one else has the perspective, we must be able to see that
rate, with 6.7% triplets or higher (SART/ASRM, 1996). Fur-
there are worse outcomes than not being pregnant.
thermore, 55% of the children born from in-vitro fertilization
The reporting system for infertility clinics and the way it is
(IVF) and gamete intra-Fallopian transfer (GIFT) in 1994 were
used in this country bears part of the responsibility for the
from multiple gestation, with 15% part of a triplet or higher continued increase in multiple pregnancy. The SART database
pregnancy. Of course, we have no data regarding how many was originally developed to protect patients from clinics where
pregnancies and fetuses were reduced to arrive at that number. pregnancy rates were very poor. Today, however it is used as
It would be unfair to charge that this is a problem that only advertising and a way of comparing successful clinics. Many
occurs in programmes where there is a blatant disregard for clinics send out annual reports of their statistics. Infertility
patient safety. In our own programme we have seen a progress- support groups encourage its use for this purpose and the
ive rise in the percentage of higher order multiple gestation. media is happy to report that Dr X has the best pregnancy
We have transferred fewer embryos than ever, but our twinning rates in the city, state, country etc. It is possible, therefore,
rate hovers around 50% and triplets account for ~10% of the that the system devised to protect patients may increase their
pregnancies in 1996. We have tried to use ultrasound Doppler risk of this complication by encouraging physicians to seek
flow patterns and observations of very early embryonic devel- and report the highest pregnancy rates.
opment to pick the best, and thereby limit the number of Insurance coverage patterns in the US also contribute to the
embryos placed. Nevertheless, along with increasing pregnancy high incidence of multiple gestation among IVF patients.
rates we have increased the multiple pregnancy rate. Typically, patients do not have insurance coverage for ART
The cost of these higher order pregnancies has been docu- procedures, but have full benefits for pregnancy care. Thus,
mented in many studies. One study from Boston reported that to the patient, the financial risk is in having an unsuccessful
just the hospital maternal and neonatal care was .US$109 IVF cycle, not in the often exorbitant costs of the resultant
000 for the average triplet gestation in 1994, or 11 times multiple gestation. If third-party payers want to reduce the
higher than a singleton pregnancy (Callahan et al., 1994). This cost of IVF pregnancies, they need to become involved in the
cost pales in comparison with the cost of raising three payment of IVF. This would reduce the pressure on patients
children simultaneously, especially if, as in 40% of quadruplet and their fertility specialists to have a pregnancy at any cost.
1615
M.Bustillo
In addition, if they are paying the bill they could reasonably The obvious considerations include the possible maternal and
ask to limit the number of embryos placed. perinatal morbidity and mortality of such pregnancy and
I believe that the incidence of multiple gestation and the premature delivery with its associated increased psychosocial
need for multifetal reduction will continue to increase until and financial costs.
infertility specialists, patients, and those paying for the results Practitioners have known for many years that the pregnancy
of these pregnancies agree that this is a serious concern. I also rate per completed ART procedure increases when a greater
believe that we can best address these concerns in the privacy number of oocytes or embryos are transferred. For instance,
of the physician–patient relationship rather than governmental the pregnancy rates reported by French National IVF Registry
regulation, although if this does not happen, some sort of (FIVNAT) for the years 1986–1990 ranged from 9.1–12.1%
control would be an improvement over the current system. In for one embryo transfers and incrementally increased for
order for this to happen, however, all parties involved need to transfers of two, three and four embryos with rates of 29.5–
modify their behaviour. Clinics need to stop gauging their 34.9% for transfers with four embryos (Walters, 1996). How-
Downloaded from https://academic.oup.com/humrep/article/12/8/1614/700082 by guest on 26 February 2022
worth by a pregnancy rate, and patients must support clinical ever, replacing a higher number of oocytes in gamete intra-
decisions that increase the probability of having healthy Fallopian transfer (GIFT) or embryos following in-vitro fertil-
children, even if the result may be a marginal decrease in ization (IVF) also proportionally increases the probability of
pregnancy rate. a multiple gestation of not only twins, triplets but also of
We who provide these services are entitled to celebrate our higher order (more than triplets) (Walters, 1996). Therefore,
patients’ successes. There are many thousands of families with the transfer of multiple oocytes or embryos is advantageous
children who were born as a result of the advances in in achieving pregnancy but has concomitant increased risks
reproductive medicine and the dedication of clinicians and (Franco, 1994). These risks can seriously affect the desired
scientists devoted to the field. I fear that we may not be as overall outcome of yielding a reasonable number of healthy
proud of the changes we have brought about in our society babies without total financial as well as emotional bankruptcy of
and the premature and subsequently damaged children that the treated families and/or the medical reimbursement system.
have been a result of preventable multiple gestations. The advent of embryo cryopreservation, in the programmes
where it is successful, has relieved practitioners of the necessity
to inseminate only a limited number of oocytes, to transfer all
References the oocytes or embryos generated in one cycle, or to discard
Society for Assisted Reproductive Technology/The American Society for normal supernumerary embryos. Despite the availability of
Reproductive Medicine (1996) Assisted reproductive technology in the cryopreservation, it is not unusual for ART programmes to
United States and Canada: 1994 results generated from the American
Society for Reproductive Medicine/Society for Assisted Reproductive transfer three or more embryos in IVF (World Collaborative
Technology Registry. Fertil. Steril., 66, 697–705. Report, 1993) and four or more oocytes in GIFT (Redgment
Callahan, T.L., Hall, J.E., Ettner, S.L. et al. (1994) The economic impact of et al., 1994). This generally results in a better pregnancy rate
multiple-gestation pregnancies and the contribution of assisted-reproduction
techniques to their incidence. N. Engl. J. Med., 331, 244–249. than the transfer of two or more embryos or fewer than four
Evans, M.I., May, M., Drugan, A. et al. (1990) Selective termination: clinical oocytes respectively. The probability of obtaining a multiple
experience and residual risks. Am. J. Obstet. Gynecol., 162, 1568–1575. pregnancy is related to the cumulative prospect of survival
Gleicher, N., Campbell, D.P., Chan C.L. et al. (1995) The desire for multiple and implantation of each individual embryo transferred or
births in couples with infertility problems contradicts present practice
patterns. Hum. Reprod., 10, 1079–1084. generated in vivo in GIFT. Undoubtedly, there are many factors,
Tan, S.L., Doyle, P., Campbell, S. et al. (1992) Obstetric outcome of in vitro both known and unknown, that may affect implantation rates.
fertilization pregnancies compared to normally conceived pregnancies. Am. The most widely observed and important is the age of the
J. Obstet. Gynecol., 167, 778–784.
woman providing the oocytes for IVF or GIFT (Tan et al.,
1990; van Kooij et al., 1996). Assessment of oocyte maturity
Imposing limits on the number of and of embryo quality by morphological appearance and rate
of cleavage, although not entirely reliable, gives the clinician
oocytes and embryos transferred: is it an approximation of a particular oocyte’s prognosis for fertiliza-
necessary/wise or naughty/nice? tion (for both GIFT and IVF) and of an embryo’s chance of
implantation in IVF (Steer et al., 1992; Shulman et al., 1993).
Marı́a Bustillo Mature oocytes are required for normal fertilization and the
Center for Human Reproduction, Box 1175, 635 Madison faster cleaving and better looking embryo has generally a
Av., New York, NY 10022, USA higher implantation rate. Likewise, embryos from younger
women in general have a higher likelihood of implanting. This
To whom correspondence should be addressed at: 245
E93 #28D, New York, NY 10128, USA. is nowhere more apparent than when glancing at the overall
results for ovum donation programmes.
In general, the reported success rates for GIFT are slightly
Twins, triplets, and more! They are everywhere; in the play- better than for IVF (Meirow and Schenker, 1995). Unquestion-
grounds, schools, shopping malls and often featured in the ably, the populations subjected to these two techniques are not
media. As assisted reproductive technologies (ART) become the same. More importantly, it appears that GIFT may be better
more widely applied, there is a justifiably growing concern in the older age patient especially when a high-order oocyte
about the resulting greater percentage of multiple pregnancies. transfer is performed (Qasim et al., 1995). It remains to be
1616
You might also like
- Life-Saving Esophageal Intubation in Neonate With Undiagnosed Tracheal Agenesis (A & A Case Reports, Vol. 9, Issue 1) (2017) DGDFGDocument1 pageLife-Saving Esophageal Intubation in Neonate With Undiagnosed Tracheal Agenesis (A & A Case Reports, Vol. 9, Issue 1) (2017) DGDFGMahdi WashahaNo ratings yet
- Vancouver References StyleDocument10 pagesVancouver References StylePitambar PoudelNo ratings yet
- Kelahiran Prematur Spontan Memajuan Menuju Penemuan Predisposisi GenetikDocument63 pagesKelahiran Prematur Spontan Memajuan Menuju Penemuan Predisposisi GenetikRismawati ArifNo ratings yet
- Achondroplasia and PregnancyDocument4 pagesAchondroplasia and PregnancyCristina GalloNo ratings yet
- Daftar Pustaka: Liver Physiol 290:G505-G510, 2006Document2 pagesDaftar Pustaka: Liver Physiol 290:G505-G510, 2006Shaoran AuliaNo ratings yet
- Malefactor Human Infertility Diagnosis Treatment: Fertility SterilityDocument270 pagesMalefactor Human Infertility Diagnosis Treatment: Fertility SterilityMd ShotonNo ratings yet
- Whitelaw 2015Document2 pagesWhitelaw 2015Juan Guillermo BuenaventuraNo ratings yet
- V15n2a04 15Document1 pageV15n2a04 15Lalo Hernández cruzNo ratings yet
- Sex and Congenital Diaphragmatic Hernia: OriginalarticleDocument5 pagesSex and Congenital Diaphragmatic Hernia: OriginalarticleBlank SpaceNo ratings yet
- PIIS0002937823001564Document2 pagesPIIS0002937823001564Kalaivathanan VathananNo ratings yet
- 02.materno - Cap10-18 CompressedDocument42 pages02.materno - Cap10-18 Compressedthaisagoraer1No ratings yet
- NIH Public Access: Author ManuscriptDocument26 pagesNIH Public Access: Author ManuscriptDr.ManageNo ratings yet
- Tubal Factor Infertility Tubal Factor Infertility: The Possible Effect of Hydrosalpinx Fluid Human EmbryosDocument15 pagesTubal Factor Infertility Tubal Factor Infertility: The Possible Effect of Hydrosalpinx Fluid Human EmbryosWaode RadmilaNo ratings yet
- The Nature of Aneuploidy - Scott1571Document9 pagesThe Nature of Aneuploidy - Scott1571CaroKandelNo ratings yet
- This Content Downloaded From 120.126.70.24 On Wed, 29 Mar 2023 11:59:10 UTCDocument8 pagesThis Content Downloaded From 120.126.70.24 On Wed, 29 Mar 2023 11:59:10 UTCmarcia suNo ratings yet
- Ross2007 Abs AjogDocument2 pagesRoss2007 Abs AjogAbdillah FauziNo ratings yet
- Williams ObstetriciaDocument70 pagesWilliams ObstetriciaKarolLeylaNo ratings yet
- Pericentric Inversion of Chromosome 1 and 9 in A Case With Recurrent Miscarriage in EgyptDocument3 pagesPericentric Inversion of Chromosome 1 and 9 in A Case With Recurrent Miscarriage in EgypthandikaNo ratings yet
- Eucaryotic Gene RegulationFrom EverandEucaryotic Gene RegulationRichard AxelNo ratings yet
- Kertenkele Canlılığının EvrimiDocument2 pagesKertenkele Canlılığının EvrimiAlara AğalarNo ratings yet
- The Developmental Biology of ReproductionFrom EverandThe Developmental Biology of ReproductionClement MarkertNo ratings yet
- Son Hombres y Mujeres Realmente Tan DistintosDocument4 pagesSon Hombres y Mujeres Realmente Tan DistintosfitoscribdNo ratings yet
- BibliographyDocument17 pagesBibliographyChristian D BlessingNo ratings yet
- Editing The Human Genome Where ART and Science IntersectDocument4 pagesEditing The Human Genome Where ART and Science IntersectBadtz MaruNo ratings yet
- The Placenta Goes Viral Retroviruses ControlDocument7 pagesThe Placenta Goes Viral Retroviruses ControlCarla Zueck DartizNo ratings yet
- Daftar Pustaka: (Medline)Document14 pagesDaftar Pustaka: (Medline)nurfitriaNo ratings yet
- Paternally Induced Transgenerational Environmental Reprogramming of Metabolic Gene Expression in MammalsDocument13 pagesPaternally Induced Transgenerational Environmental Reprogramming of Metabolic Gene Expression in MammalsAshok KumarNo ratings yet
- Han 1999Document2 pagesHan 1999Araceli Enríquez OvandoNo ratings yet
- Impact of Androgen Supplementation On The FolliculjjDocument2 pagesImpact of Androgen Supplementation On The Folliculjjdivya maniNo ratings yet
- Daftar Pustaka FixDocument4 pagesDaftar Pustaka FixhexiNo ratings yet
- Nonfamilial Hypokalemic Periodic Paralysis and Thyrotoxicosis in A 16-Year-Old MaleDocument5 pagesNonfamilial Hypokalemic Periodic Paralysis and Thyrotoxicosis in A 16-Year-Old MaleHeinz EnchieNo ratings yet
- Fendo 13 1107903Document3 pagesFendo 13 1107903puspitaNo ratings yet
- Association Between Male Genital Anomalies and Adult Male Reproductive Disorders A Population-Based Data Linkage Study Spanning More Than 40 YearsDocument8 pagesAssociation Between Male Genital Anomalies and Adult Male Reproductive Disorders A Population-Based Data Linkage Study Spanning More Than 40 YearsMade Moniaga PrawiraNo ratings yet
- Parthenogenesis: Birth of A New Lineage or Reproductive Accident?Document4 pagesParthenogenesis: Birth of A New Lineage or Reproductive Accident?Afifah ShehreyaNo ratings yet
- Khilyatul Mufida 22010111120040 Lap - Kti Bab 8Document27 pagesKhilyatul Mufida 22010111120040 Lap - Kti Bab 8Hafid JuniorNo ratings yet
- Nejmoa 061760Document16 pagesNejmoa 061760nqchi180418No ratings yet
- NEJMcibr 1100692Document2 pagesNEJMcibr 1100692JulitaMelisaNo ratings yet
- Novel Genes and Mutations in Patients Affected by Recurrent Pregnancy LossDocument14 pagesNovel Genes and Mutations in Patients Affected by Recurrent Pregnancy LossarusezNo ratings yet
- Historical and Clinical Perspectives On CHR TranslocationsDocument14 pagesHistorical and Clinical Perspectives On CHR TranslocationsAsma HMILANo ratings yet
- Autism and The Gastrointestinal Tract: ReferencesDocument3 pagesAutism and The Gastrointestinal Tract: References__aguNo ratings yet
- Artigo SODocument6 pagesArtigo SORoberto BuenoNo ratings yet
- Ibuprofen Is Deleterious For The Development of First Trimester Human Fetal Ovary Ex VivoDocument12 pagesIbuprofen Is Deleterious For The Development of First Trimester Human Fetal Ovary Ex VivoLuisFernandoMarcaMolfinoNo ratings yet
- Gynecology, Vol 96, No 2, University of North Carolina at Chapel HillDocument4 pagesGynecology, Vol 96, No 2, University of North Carolina at Chapel HillWidiana KosasihNo ratings yet
- Artigo 1Document3 pagesArtigo 1Lucas DutraNo ratings yet
- Atypical Brucella Marine Toads: Inopinata-Like Species in 2Document3 pagesAtypical Brucella Marine Toads: Inopinata-Like Species in 2eduardoNo ratings yet
- Duplication, Selection and Gene Conversion in A Drosophila Mojavensis Female Reproductive Protein FamilyDocument15 pagesDuplication, Selection and Gene Conversion in A Drosophila Mojavensis Female Reproductive Protein FamilyJulian PadroNo ratings yet
- Accepted Manuscript: 10.1016/j.ajog.2015.05.009Document31 pagesAccepted Manuscript: 10.1016/j.ajog.2015.05.009Oswaldo De LeónNo ratings yet
- Vitamin D in IVFDocument7 pagesVitamin D in IVFMohamed AliNo ratings yet
- J Ajog 2005 03 009Document2 pagesJ Ajog 2005 03 009Denni PrasetyoNo ratings yet
- A Study of Two Sequential Culture Media - Impact On Embryo Quality and Pregnancy RatesDocument8 pagesA Study of Two Sequential Culture Media - Impact On Embryo Quality and Pregnancy RatesTuan PhanNo ratings yet
- Virro 2004Document7 pagesVirro 2004Tiffany LamNo ratings yet
- 2015 Embryos, DOHaD and David BarkerDocument7 pages2015 Embryos, DOHaD and David BarkerNguyễn Tiến HồngNo ratings yet
- Cell-Free Fetal DNA - A Trigger For Parturition: Clinical Implications of Basic ResearchDocument3 pagesCell-Free Fetal DNA - A Trigger For Parturition: Clinical Implications of Basic ResearchCarmePonsNo ratings yet
- Jurnal Imunologi AbortusDocument45 pagesJurnal Imunologi AbortusFajar Al-HabibiNo ratings yet
- Immunological Influence on Human Fertility: Proceedings of the Workshop on Fertility in Human Reproduction, University of Newcastle, Australia, July 11-13, 1977From EverandImmunological Influence on Human Fertility: Proceedings of the Workshop on Fertility in Human Reproduction, University of Newcastle, Australia, July 11-13, 1977Barry BoettcherNo ratings yet
- Adult Somatic Cells To The Rescue Nuclear Reprogramming A 2014 Fertility AnDocument6 pagesAdult Somatic Cells To The Rescue Nuclear Reprogramming A 2014 Fertility Ancuongduong172839No ratings yet
- Is Momincharge Implications of Resource Provisioning On The Evolution of The PlacentaDocument11 pagesIs Momincharge Implications of Resource Provisioning On The Evolution of The PlacentaAlan David Ruiz GarcíaNo ratings yet
- Dor 2Document10 pagesDor 2Alce Alce EverdienNo ratings yet
- Irst Aid Andaging: Ashutosh Sharma Demonstrator/ Tutor Nursing College, UPUMS, Saifai, Etawah UPDocument14 pagesIrst Aid Andaging: Ashutosh Sharma Demonstrator/ Tutor Nursing College, UPUMS, Saifai, Etawah UPdurgesh yadavNo ratings yet
- Faradism Under Pressure For EdemaDocument4 pagesFaradism Under Pressure For EdemaDr GowrishankarPotturi PT71% (7)
- Basic Nursing & First Aid (Theory)Document1 pageBasic Nursing & First Aid (Theory)durgesh yadavNo ratings yet
- Massage For Therapists A Guide To Soft Tissue Therapies: October 2010Document3 pagesMassage For Therapists A Guide To Soft Tissue Therapies: October 2010reza ghazizadeNo ratings yet
- Management of Childhood and Adolescent DisordersDocument26 pagesManagement of Childhood and Adolescent Disordersdurgesh yadav100% (1)
- Syllabus For Bachelor of Physiotherapy (BPT) Academic ProgrammeDocument36 pagesSyllabus For Bachelor of Physiotherapy (BPT) Academic ProgrammevikasmaeNo ratings yet
- Muscle Physiology: Dr. EbneshahidiDocument37 pagesMuscle Physiology: Dr. EbneshahidiAnonymous dwPTJOhsNo ratings yet
- Questions For Mark About India IVF 2021-7-30Document4 pagesQuestions For Mark About India IVF 2021-7-30durgesh yadavNo ratings yet
- BACHELOR OF PHYSIOTHERAPY Ist YEARDocument34 pagesBACHELOR OF PHYSIOTHERAPY Ist YEARdurgesh yadavNo ratings yet
- Empower 2e B1 Word List GermanDocument102 pagesEmpower 2e B1 Word List GermanOmid SofeNo ratings yet
- 11 - Reciprocal InnervationDocument20 pages11 - Reciprocal Innervationbreinfout fotosNo ratings yet
- NAMS 2022 Hormone-Therapy-Position-StatementDocument28 pagesNAMS 2022 Hormone-Therapy-Position-StatementPaul PIETTENo ratings yet
- Jihan Rahma Fadillah 46-50Document14 pagesJihan Rahma Fadillah 46-50Hendry RahmanantoNo ratings yet
- MRCP BCC 2Document5 pagesMRCP BCC 2zhichee91No ratings yet
- Abdominal Aortic Aneurysm: AetiologyDocument7 pagesAbdominal Aortic Aneurysm: AetiologyKelvin MaikanaNo ratings yet
- H-046-003758-00 Wash Solution FDADocument4 pagesH-046-003758-00 Wash Solution FDABagus KrisdianNo ratings yet
- How To Get The Perfect Tattoo PDFDocument11 pagesHow To Get The Perfect Tattoo PDFSebastian GuevaraNo ratings yet
- Construction Management Term PaperDocument5 pagesConstruction Management Term Paperbctfnerif100% (1)
- GEN 013 Day 02 SASDocument5 pagesGEN 013 Day 02 SASAlbert King CambaNo ratings yet
- Nurse Anesthetist ThesisDocument8 pagesNurse Anesthetist Thesissamanthajonessavannah100% (2)
- Urinary Retention NCP GARCIA J.Document2 pagesUrinary Retention NCP GARCIA J.Jimlord GarciaNo ratings yet
- Does This Dyspneic Patient in The Emergency Department Have Congestive Heart Failure?Document13 pagesDoes This Dyspneic Patient in The Emergency Department Have Congestive Heart Failure?Jorge MéndezNo ratings yet
- PreviewpdfDocument88 pagesPreviewpdfHeidy Montes Galarza100% (1)
- Portfolio of Products For ExportDocument8 pagesPortfolio of Products For ExportYeni Paola Ibarra RodríguezNo ratings yet
- Updated BMI Monitoring of Pat Dexter L Ginon 1Document3 pagesUpdated BMI Monitoring of Pat Dexter L Ginon 1Fredimar PatarayNo ratings yet
- Chest PainDocument5 pagesChest PainAndrei MurariuNo ratings yet
- David A. Crenshaw PHD - Therapeutic Engagement of Children and Adolescents - Play, Symbol, Drawing, and Storytelling Strategies (2008, Jason Aronson, Inc.)Document176 pagesDavid A. Crenshaw PHD - Therapeutic Engagement of Children and Adolescents - Play, Symbol, Drawing, and Storytelling Strategies (2008, Jason Aronson, Inc.)mamta100% (1)
- OSSSC Diploma in Pharmacy..Document8 pagesOSSSC Diploma in Pharmacy..RAJANI SathuaNo ratings yet
- Common Medical AbbreviationsDocument1 pageCommon Medical Abbreviationskedwards108No ratings yet
- UntitledDocument54 pagesUntitledJody AdewaleNo ratings yet
- Barlow - Unified Protocol - WorkbookDocument224 pagesBarlow - Unified Protocol - WorkbookAshly Arias100% (1)
- Disruptive Mood Dysregulation DisorderDocument13 pagesDisruptive Mood Dysregulation DisorderNyoman SuryaNo ratings yet
- Final SBFR Training PPT 19th April 2022 MoHDocument113 pagesFinal SBFR Training PPT 19th April 2022 MoHDaniel Firomsa100% (6)
- 2021 Obesity AlgorithmDocument143 pages2021 Obesity AlgorithmKhishignemekhMunkhbatNo ratings yet
- Fear of Public SpeakingDocument11 pagesFear of Public SpeakingMustanser GhiasNo ratings yet
- Kapolei High School Track and Field Rules and RegualtionsDocument4 pagesKapolei High School Track and Field Rules and Regualtionsapi-494337591No ratings yet
- Personality and Learning Style: Evidence For Big Five TraitsDocument6 pagesPersonality and Learning Style: Evidence For Big Five TraitsAnonymous CwJeBCAXpNo ratings yet
- Argument EssayDocument6 pagesArgument Essayapi-509629455No ratings yet
- 9RESPIRATORY THERAPY EQUIPMENT PPTDocument6 pages9RESPIRATORY THERAPY EQUIPMENT PPTJack OneNo ratings yet