Professional Documents
Culture Documents
Alsrouji y Memon - 2020 - Seronegative Autoimmune Encephalitis
Alsrouji y Memon - 2020 - Seronegative Autoimmune Encephalitis
Uploaded by
Thais LudenaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Alsrouji y Memon - 2020 - Seronegative Autoimmune Encephalitis
Alsrouji y Memon - 2020 - Seronegative Autoimmune Encephalitis
Uploaded by
Thais LudenaCopyright:
Available Formats
PRACTICE | CLINICAL IMAGES
Seronegative autoimmune encephalitis
Owais Alsrouji MD, Anza B. Memon MD
n Cite as: CMAJ 2020 November 30;192:E1638. doi: 10.1503/cmaj.200424
A
68-year-old woman with
a history of rheumatoid A B C
arthritis presented to the
emergency department with
3 months of rapidly progressing
cognitive decline. Examination
revealed new short-term memory
loss, poor attention, difficulty
conceptualizing tasks and inabil-
ity to complete multistep actions.
Three days after admission, the
patient developed limb rigidity,
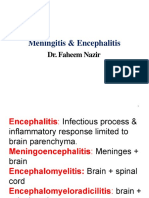
hyperreflexia, exaggerated startle Figure 1: Magnetic resonance imaging (MRI) of the brain of a 68-year-old woman with autoimmune encephal
response, and autonomic dys- itis. (A) Initial brain MRI revealed bilateral confluent hyperintense signal changes in thalami, caudate and
putamen nuclei on axial fluid-attenuated inversion recovery (FLAIR) sequence (arrow). (B) Repeat brain MRI
function with fluctuations in after 2 weeks showed an increase in the degree of bilateral symmetric FLAIR hyperintensity within the basal
blood pressure and heart rate. ganglia (arrow). (C) Repeat brain MRI 8 days postplasmapheresis showed nearly complete resolution of the
Magnetic resonance imaging confluent basal ganglia hyperintensity (arrow).
(MRI) of the patient’s brain showed
bilateral confluent hyperintense signal changes in the basal ganglia increased risk of morbidity and death in untreated patients.2
(Figure 1A). Autoimmune serology revealed positive antinuclear Timely diagnosis and intervention, including immunomodula-
antibody at 1:640 (homogenous pattern; reference range < 1:80) and tory therapies such as intravenous immunoglobulin, high-dose
elevated cyclic citrullinated peptide antibody (> 340 IU/mL [refer- corticosteroids and plasmapheresis, are associated with good
ence range < 7 IU/mL]). Consistent with a diagnosis of seronegative outcomes. Patients with an aggressive or relapsing course
autoimmune encephalitis, serology was negative for glutamic acid require maintenance therapy with immunosuppressants.
decarboxylase, N-methyl-D-aspartate receptor and glycine receptor
antibodies. Cerebrospinal fluid analysis revealed only an elevated References
protein level of 203 mg/dL (normal range 15–55 mg/dL). Further 1. Graus F, Titulaer MJ, Balu R, et al. A clinical approach to the diagnosis of auto-
long-chain fatty acid, toxic, infectious and neoplastic test results immune encephalitis. Lancet Neurol 2016;15:391-404.
were negative (Appendix 1, available at www.cmaj.ca/lookup/ 2. Dutra LA, Abrantes F, Toso FF, et al. Autoimmune encephalitis: a review of
diagnosis and treatment. Arq Neuropsiquiatr 2018;76:41-9.
doi/10.1503/cmaj.200424/tab-related-content), and we diagnosed
the patient with autoimmune encephalitis.
The patient received a 1 g dose of methylprednisolone, after
which gastrointestinal bleeding developed. Two weeks later, a Competing interests: None declared.
repeat brain MRI showed interval worsening of findings (Figure 1B). This article has been peer reviewed.
She was treated with 5 rounds of plasmapheresis, after which a
The authors have obtained patient consent.
repeat brain MRI showed nearly complete resolution of basal
ganglia hyperintensity (Figure 1C). She received rituximab, and Affiliations: Department of Neurology (Alsrouji, Memon), Henry Ford
Hospital; Wayne State University (Memon), School of Medicine,
6 weeks later she had made a full neurologic recovery.
Detroit, Mich.
Autoimmune encephalitis has an incidence of 5–10 per
Acknowledgement: The authors thank Stephanie Stebens for her
100 000 person-years.1 Diagnosis is based on the clinical presen-
assistance with this manuscript.
tation of progressive encephalomyelitis and neuroimaging find-
ings suggestive of encephalitis.1,2 Negative antibody test results Correspondence to: Anza Memon, amemon2@hfhs.org
do not exclude autoimmune encephalitis, and there is an
E1638 CMAJ | NOVEMBER 30, 2020 | VOLUME 192 | ISSUE 48 © 2020 Joule Inc. or its licensors
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5819)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (845)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- DasdasDocument4 pagesDasdasAbdurauf SawadjaanNo ratings yet
- 102551Document27 pages102551محمد البناءNo ratings yet
- Infectious Diseases of Central Nervous SystemDocument1,684 pagesInfectious Diseases of Central Nervous SystemLuciano Arraes100% (1)
- CNS Infection - NelsonDocument13 pagesCNS Infection - Nelsonsai saiNo ratings yet
- Acute ComaDocument16 pagesAcute ComaDean AccountNo ratings yet
- Red and Orange Flags For Secondary Headache (SNOOP 10)Document11 pagesRed and Orange Flags For Secondary Headache (SNOOP 10)rizkiNo ratings yet
- Chapter 22. Infections of The Nervous SystemDocument22 pagesChapter 22. Infections of The Nervous SystemZin LimNo ratings yet
- 6M Case Report Postinfectious CerebellitisDocument14 pages6M Case Report Postinfectious CerebellitisGa B B OrlonganNo ratings yet
- Syndromic NotificationDocument44 pagesSyndromic NotificationAlexandra DukeNo ratings yet
- Meningitis & EncephalitisDocument7 pagesMeningitis & EncephalitisABAKADANo ratings yet
- Ao2010 0017 A PDFDocument13 pagesAo2010 0017 A PDFJeriel de SilosNo ratings yet
- Icd 10 Excell NewDocument491 pagesIcd 10 Excell Newlilik fitriatulNo ratings yet
- ReseachDocument16 pagesReseachexcaliburfay96No ratings yet
- Meningitis & EncephalitisDocument95 pagesMeningitis & Encephalitisfahim nazir QanoongoNo ratings yet
- Aseptic Meningitis: Diagnosis and ManagementDocument13 pagesAseptic Meningitis: Diagnosis and ManagementSandrio UtomoNo ratings yet
- Aseptic MeningitisDocument24 pagesAseptic Meningitisidno1008100% (1)
- IcdDocument1,590 pagesIcdZainalAbidinNo ratings yet
- PhilHealth Circular No. 0035, s.2013 Annex 8 List of Medical Conditions Allowed For Referral PackageDocument7 pagesPhilHealth Circular No. 0035, s.2013 Annex 8 List of Medical Conditions Allowed For Referral PackageChrysanthus HerreraNo ratings yet
- Product BookletDocument46 pagesProduct BookletNARESH JANDIALNo ratings yet
- Fitri PunyaDocument351 pagesFitri PunyaFajar LestariNo ratings yet
- Encephalitis and Mental DisorderDocument15 pagesEncephalitis and Mental DisorderElfany Nur hajjahNo ratings yet
- Menigitis EncephalitisDocument63 pagesMenigitis EncephalitisHussain Azhar100% (1)
- Full Chapter Case Based Approach To Common Neurological Disorders 2024Th Edition Krishna Kumar Oli PDFDocument46 pagesFull Chapter Case Based Approach To Common Neurological Disorders 2024Th Edition Krishna Kumar Oli PDFjosephine.chandler412100% (2)
- (10920684 - Neurosurgical Focus) Hitler's ParkinsonismDocument5 pages(10920684 - Neurosurgical Focus) Hitler's ParkinsonismStuti MardiaNo ratings yet
- Japanese EncephalitisDocument50 pagesJapanese EncephalitisPhilip SebastianNo ratings yet
- IcdDocument180 pagesIcdFitri MoraNo ratings yet
- Central Nervous System Pathology: Presented byDocument70 pagesCentral Nervous System Pathology: Presented byNicholasNo ratings yet
- CHAPTER 17 - Overview of Human Infectious DiseasesDocument3 pagesCHAPTER 17 - Overview of Human Infectious DiseasesJacob PallorinaNo ratings yet
- Assessment of PsychosisDocument73 pagesAssessment of Psychosismanuel ricardo barojas alvarezNo ratings yet
- Acute Encephalitis SyndromeDocument116 pagesAcute Encephalitis SyndromePrateek Kumar PandaNo ratings yet