Professional Documents
Culture Documents
2019 - YEARS Algorithm For Tep
Uploaded by
FranciscoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
2019 - YEARS Algorithm For Tep
Uploaded by
FranciscoCopyright:
Available Formats
Articles
Simplified diagnostic management of suspected pulmonary
embolism (the YEARS study): a prospective, multicentre,
cohort study
Tom van der Hulle, Whitney Y Cheung, Stephanie Kooij, Ludo F M Beenen, Thomas van Bemmel, Josien van Es, Laura M Faber,
Germa M Hazelaar, Christian Heringhaus, Herman Hofstee, Marcel M C Hovens, Karin A H Kaasjager, Rick C J van Klink, Marieke J H A Kruip,
Rinske F Loeffen, Albert T A Mairuhu, Saskia Middeldorp, Mathilde Nijkeuter, Liselotte M van der Pol, Suzanne Schol-Gelok, Marije ten Wolde,
Frederikus A Klok, Menno V Huisman, for the YEARS study group*
Summary
Background Validated diagnostic algorithms in patients with suspected pulmonary embolism are often not used Lancet 2017; 390: 289–97
correctly or only benefit subgroups of patients, leading to overuse of computed tomography pulmonary angiography Published Online
(CTPA). The YEARS clinical decision rule that incorporates differential D-dimer cutoff values at presentation, has May 23, 2017
http://dx.doi.org/10.1016/
been developed to be fast, to be compatible with clinical practice, and to reduce the number of CTPA investigations in
S0140-6736(17)30885-1
all age groups. We aimed to prospectively evaluate this novel and simplified diagnostic algorithm for suspected acute
This online publication has
pulmonary embolism. been corrected. The corrected
version first appeared at
Methods We did a prospective, multicentre, cohort study in 12 hospitals in the Netherlands, including consecutive thelancet.com on June 27, 2017
patients with suspected pulmonary embolism between Oct 5, 2013, to July 9, 2015. Patients were managed by See Comment page 210
simultaneous assessment of the YEARS clinical decision rule, consisting of three items (clinical signs of deep vein *YEARS study group is listed at
thrombosis, haemoptysis, and whether pulmonary embolism is the most likely diagnosis), and D-dimer the end of this paper
concentrations. In patients without YEARS items and D-dimer less than 1000 ng/mL, or in patients with one or more Department of Thrombosis and
Hemostasis (T van der Hulle MD,
YEARS items and D-dimer less than 500 ng/mL, pulmonary embolism was considered excluded. All other patients F A Klok MD,
had CTPA. The primary outcome was the number of independently adjudicated events of venous thromboembolism Prof M V Huisman MD) and
during 3 months of follow-up after pulmonary embolism was excluded, and the secondary outcome was the number Department of Emergency
of required CTPA compared with the Wells’ diagnostic algorithm. For the primary outcome regarding the safety of Medicine (C Heringhaus MD),
Leiden University Medical
the diagnostic strategy, we used a per-protocol approach. For the secondary outcome regarding the efficiency of the Center, Leiden, Netherlands;
diagnostic strategy, we used an intention-to-diagnose approach. This trial is registered with the Netherlands Trial Department of Vascular
Registry, number NTR4193. Medicine (W Y Cheung MD,
Prof S Middeldorp MD) and
Department of Radiology
Findings 3616 consecutive patients with clinically suspected pulmonary embolism were screened, of whom 151 (4%) (L F M Beenen MD), Academic
were excluded. The remaining 3465 patients were assessed of whom 456 (13%) were diagnosed with pulmonary Medical Center, Amsterdam,
embolism at baseline. Of the 2946 patients (85%) in whom pulmonary embolism was ruled out at baseline and Netherlands; Department of
remained untreated, 18 patients were diagnosed with symptomatic venous thromboembolism during 3-month follow- Internal Medicine, Haga
Hospital, The Hague,
up (0·61%, 95% CI 0·36–0·96) of whom six had fatal pulmonary embolism (0·20%, 0·07–0·44). CTPA was not Netherlands (S Kooij MD,
indicated in 1651 (48%) patients with the YEARS algorithm compared with 1174 (34%) patients, if Wells’ rule and A T A Mairuhu MD,
fixed D-dimer threshold of less than 500 ng/mL would have been applied, a difference of 14% (95% CI 12–16). L M van der Pol MD);
Department of Medicine,
Gelre Hospital, Apeldoorn,
Interpretation In our study pulmonary embolism was safely excluded by the YEARS diagnostic algorithm in patients Netherlands
with suspected pulmonary embolism. The main advantage of the YEARS algorithm in our patients is the absolute (T van Bemmel MD);
14% decrease of CTPA examinations in all ages and across several relevant subgroups. Department of Pulmonology,
Onze Lieve Vrouwe Gasthuis
Hospital, Amsterdam,
Funding This study was supported by unrestricted grants from the participating hospitals. Netherlands (J van Es MD);
Department of Medicine, Red
Introduction exposure and contrast medium induced nephropathy.2–6 To Cross Hospital, Beverwijk,
Netherlands (L M Faber MD);
The clinical diagnosis of pulmonary embolism is non- avoid these problems, validated diagnostic algorithms for
Department of Pulmonology
specific and should therefore be followed by objective suspected acute pulmonary embolism, using sequential (G M Hazelaar MD) and
testing. Because of its diagnostic accuracy and wide testing, have been introduced.7 In these algorithms, a Department of Medicine
availability, multidetector row computed tomography normal D-dimer test result in patients with low probability (M M C Hovens MD), Rijnstate
Hospital, Arnhem,
pulmonary angiography (CTPA) is the imaging test of safely excludes pulmonary embolism.8 Correct application
Netherlands; Department of
choice to confirm acute pulmonary embolism in most of these algorithms obviates the need for CTPA in 20–30% Medicine, Medisch Centrum
patients. Increasing use of CTPA with diminishing of patients, with an overall 3-month diagnostic failure Haaglanden, The Hague,
prevalence of pulmonary embolism—to even less than rate of less than 1·5% after initial negative ruling Netherlands (H Hofstee MD);
Department of Medicine,
10%1—has led to overdiagnosis of mostly subsegmental of the algorithm.7–9 An age-adjusted D-dimer threshold
University Medical Center
pulmonary embolism and unnecessary risks of radiation (age × 10 ng/mL for patients aged >50 years) has been
www.thelancet.com Vol 390 July 15, 2017 289
Articles
Utrecht, Utrecht, Netherlands
(Prof K A H Kaasjager MD, Research in context
M Nijkeuter MD); Department
of Hematology, Erasmus Evidence before this study Added value of this study
Medical Center, Rotterdam, We did not do a systematic search on this topic. However, on In this study, a novel and simplified diagnostic algorithm for
Netherlands (M J H A Kruip MD, the basis of several prospective management studies, suspected acute pulmonary embolism (the YEARS algorithm) has
S Schol-Gelok MD); Department
of Medicine (R F Loeffen MD)
patients with clinically suspected pulmonary embolism been prospectively investigated. The YEARS algorithm consists
and Department of should be managed according to a validated diagnostic of only three items of the original Wells’ clinical decision rule—
Pulmonology algorithm consisting of clinical decision rule such as the Wells’ ie, clinical signs of deep vein thrombosis, haemoptysis, and
(R C J van Klink MD), Alrijne rule, which predicts the pretest probability of pulmonary whether pulmonary embolism is the most likely diagnosis—were
Hospital, Leiderdorp,
Netherlands; and Department
embolism, a D-dimer test, and eventually a multirow detector found to be the most predictive for pulmonary embolism. This
of Medicine, Flevo Hospital, computed tomography pulmonary angiography (CTPA). By simplified clinical decision rule was combined with variable
Almere, Netherlands using such a diagnostic algorithm, pulmonary embolism can D-dimer threshold depending on the presence of one of these
(M ten Wolde MD) be excluded without CTPA in 20–30% of patients, thereby items. In patients in whom none of the items were present,
Correspondence to: omitting radiation exposure. In a meta-analysis, the 3-month a D-dimer test threshold of 1000 ng/mL was used whereas a
Prof Menno V Huisman,
Department of Thrombosis and
risk of venous thromboembolism in patients managed D-dimer threshold of 500 ng/mL was used when one or more
Hemostasis, Leiden University without CTPA is 0·65% (95% CI 0·38–1·11). Importantly, most items were present.
Medical Center, 2300 RC Leiden, CTPA results are still negative for pulmonary embolism, Our study showed that the YEARS algorithm is safe during
Netherlands indicating that many patients are exposed to unnecessary
m.v.huisman@lumc.nl 3 months of follow-up in all patients who had pulmonary
radiation. An age-adjusted D-dimer threshold embolism excluded. In patients managed without CTPA, the
(age × 10 ng/mL for patients >50 years) has been validated 3-month risk of venous thromboembolism was well comparable
prospectively, reporting an absolute reduction of 11·6% to the risk reported by a meta-analysis after the current standard
(95% CI 10·5–12·9) in the need for CTPA. Only patients aged algorithm was used. The advantage of the YEARS algorithm is an
50 years or older, and foremost those older than 75 years absolute reduction of 14% of CTPA compared with the current
benefit from this strategy whereas the exposure to standard algorithm and, importantly, an 8·7% reduction
unnecessary radiation might be more relevant to younger compared with the age-adjusted D-dimer threshold. In this
individuals, particularly women. Therefore, one of the context, patients younger than 50 years also benefit from the
remaining challenges is to further reduce the number of CTPA YEARS algorithm.
without reducing the safety of diagnostic management.
Implications of all the available evidence
Additionally, despite firm evidence of its safety and efficiency,
There are two main advantages of the YEARS algorithm. First,
several studies reported that adherence to recommended
the YEARS algorithm leads to an absolute 14% decrease in the
diagnostic algorithms outside clinical studies is poor. This
number of CTPA examinations that is applicable to all ages.
finding might be partly due to its complexity, and insufficient
This decrease is a major step forward in reducing unnecessary
time at busy emergency departments, which hampers the use
radiation exposure in patients with suspected pulmonary
of sequential tests. Improved adherence to the algorithm has
embolism. Second, the YEARS algorithm leads to a simpler
been shown to significantly decrease the mean number of
and more efficient diagnostic management of patients with
diagnostic tests used along with—and more importantly—the
suspected pulmonary embolism than standard diagnostic
number of diagnostic failures. For instance, one study
algorithms such as the Christopher Study algorithm, which is
reported a failure rate of 7·7% in patients who were managed
likely to improve the adherence to correct diagnostic
inappropriately compared with only 1·2% in patients
management of suspected pulmonary embolism and thereby
managed appropriately.
lead to better safety and efficiency in daily clinical practice.
validated prospectively, reporting an absolute reduction of D-dimer testing is frequently ordered and known at
11·6% (95% CI 10·5–12·9) in the need for CTPA.10 a low clinical threshold or even before the clinical
Importantly, only patients aged 50 years or older, and assessment.15,16 Improved adherence to the algorithm, for
foremost those older than 75 years benefit from instance by implementation of a clinical decision
this strategy whereas when considering the life-time support system, has been shown to significantly decrease
attributable cancer risk, the exposure to unnecessary the mean number of diagnostic tests used along with—
radiation is considered more relevant to younger and more importantly—the number of diagnostic
individuals, particularly women.3 failures.17,18
Despite firm evidence of its safety and efficiency, On the basis of a post-hoc derivation and validation
adherence to recommended diagnostic strategies in study,19 three items of the original Wells’ clinical decision
clinical practice is variable. This variation might be rule—ie, clinical signs of deep vein thrombosis,
partly due to complexity of these strategies, and haemoptysis, and whether pulmonary embolism is the
insufficient time at busy emergency departments, which most likely diagnosis—were the most predictive for
hampers the use of sequential tests.11–14 In daily practice, pulmonary embolism. They allowed the use of a
290 www.thelancet.com Vol 390 July 15, 2017
Articles
differential D-dimer threshold based on the presence of Physicians were not blinded for the D-dimer test result
one of these items, without losing sensitivity. Hence, when they assigned the YEARS items.
this algorithm—which we call YEARS—involves the In patients with no YEARS items and a D-dimer
simultaneous assessment of only the three above concentration less than 1000 ng/mL, pulmonary
mentioned items and a D-dimer test threshold of embolism was considered excluded and further testing
500 ng/mL in presence, and 1000 ng/mL in absence of was withheld. In patients with one or more YEARS
one of the YEARS items. The YEARS algorithm was items and a D-dimer concentration less than
designed to be more easily applied in a busy clinical 500 ng/mL, pulmonary embolism was also considered
practice than currently used diagnostic strategies, and excluded and further testing was withheld. All other
to further decrease the number of necessary CTPA patients—ie, either with no YEARS item and a D-dimer
examinations in patients of all ages. In this study, we concentration of 1000 ng/mL or more, or with one or
aimed to prospectively evaluate this novel and simplified more items and a concentration of 500 ng/mL or
diagnostic algorithm for suspected acute pulmonary more—were referred for CTPA to show or exclude the
embolism. diagnosis of pulmonary embolism. The appendix
shows the full CTPA scan protocol. Patients in whom
Methods pulmonary embolism was ruled out were left untreated
Study design and patients and followed up for 3 months. They were instructed to
We did a prospective, multicentre, cohort outcome study return to the hospital in the event of symptoms of
evaluating the safety and efficiency of the YEARS venous thromboembolism, after which objective
algorithm in patients with suspected acute pulmonary diagnostic tests were done to confirm or refute the
embolism between Oct 5, 2013, and July 9, 2015 (figure 1).19 disease. Follow-up consisted of a scheduled outpatient
The algorithm was implemented as standard diagnostic visit or telephone interview after 3 months. At this
strategy in 12 participating hospitals in the Netherlands. visit, information about complaints suggestive of
The full study protocol is available in the appendix. venous thromboembolism was obtained. Patients in See Online for appendix
Consecutive outpatients and inpatients with clinically whom acute pulmonary embolism was confirmed at
suspected acute (first or recurrent) pulmonary embolism baseline were treated with anticoagulants according to
were eligible for inclusion if they were aged 18 years or international guidelines.
older. Exclusion criteria were treatment with therapeutic
doses of anticoagulants initiated 24 hours or more before Outcomes
eligibility assessment, life expectancy less than 3 months The primary outcome was the 3-month incidence of
or geographic inaccessibility precluding follow-up, symptomatic venous thromboembolism in the overall
pregnancy, or allergy to intravenous contrast agent. The population and in patients managed with and without
protocol was centrally approved by the institutional CTPA separately. The diagnosis of pulmonary
review board of the Leiden University Medical Center, embolism or deep vein thrombosis was based on
Leiden, Netherlands, which waived the need for predefined criteria (appendix). In case of clinically
informed consent; this decision was endorsed by the suspected pulmonary embolism or deep vein
local institutional review board of each participating thrombosis, objective diagnostic tests were required,
centre including CTPA for suspected pulmonary embolism
and compression ultrasonography for suspected
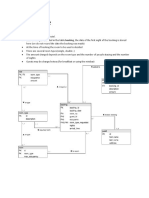
Procedures
An attending physician who suspected acute pulmonary
embolism assessed the patients, and then evaluated the Suspected acute pulmonary embolism
YEARS score by assessing the presence or absence of
each of the YEARS items—ie, symptomatic deep vein
Order D-dimer test and score presence of the three YEARS items:
thrombosis, haemoptysis, and whether pulmonary Clinical signs of deep vein thrombosis
embolism is the most likely diagnosis—(scored as yes or Haemoptysis
Pulmonary embolism the most likely diagnosis
no) with the pretest probability dependent threshold of
the D-dimer test (figure 1). D-dimer concentrations were
measured upon presentation of the patient, according
to local practice, with automated well validated high- 0 YEARS items 0 YEARS items ≥1 YEARS items ≥1 YEARS items
sensitive quantitative D-dimer assays (Vidas D-dimer D-dimer <1000 ng/mL D-dimer ≥1000 ng/mL D-dimer <500 ng/mL D-dimer ≥500 ng/mL
Exclusion, Biomerieux, Marcy-L’Étoile, France; Tinaquant,
Roche Diagnostica, Mannheim, Germany; STA-LIA, Pulmonary embolism Order CTPA Pulmonary embolism Order CTPA
DiagnosticaStago, Asnieres, France; and Innovance, excluded excluded
Siemens, Marburg, Germany). Our study reflected daily
clinical practice in which D-dimer concentrations are Figure 1: YEARS algorithm
often determined at presentation to the emergency ward. CTPA=computed tomography pulmonary angiography.
www.thelancet.com Vol 390 July 15, 2017 291
Articles
3616 patients with clinically suspected acute pulmonary embolism
151 excluded
37 life expectancy <3 months or inability of follow-up
15 anticoagulant treatment for >24 h
95 pregnancy
4 contraindication to CTPA
3465 study patients managed according to the YEARS algorithm
1743 no YEARS items 1722 ≥1 YEARS items
1320 D-dimer <1000 ng/mL 423 D-dimer ≥1000 ng/mL 331 D-dimer <500 ng/mL 1391 D-dimer ≥500 ng/mL
16 CTPA done because of protocol 1 no D-dimer test done 24 CTPA done because of protocol violation, 2 no D-dimer test done
violation, none showing acute pulmonary of which 3 were indicative of pulmonary
embolism embolism and received anticoagulants
368 pulmonary embolism 55 pulmonary embolism 990 pulmonary embolism 401 pulmonary embolism
excluded after CTPA confirmed by CTPA and excluded after CTPA confirmed by CTPA
received treatment and received treatment
1306 did not receive 352 did not receive 327 did not receive 966 did not receive
anticoagulant anticoagulant anticoagulant anticoagulant
treatment treatment treatment treatment
14 started anticoagulant 16 started anticoagulant 4 started anticoagulant 24 started anticoagulant
treatment for reasons treatment for reasons treatment for reasons treatment for reasons
other than venous other than venous other than venous other than venous
thromboembolism thromboembolism thromboembolism thromboembolism
Follow-up at 3 months Follow-up at 3 months Follow-up at 3 months Follow-up at 3 months
2 non-fatal events 3 non-fatal events 3 non-fatal events 4 non-fatal events
1 pulmonary embolism 2 pulmonary embolism 3 pulmonary embolism 4 deep vein thrombosis
1 deep vein thrombosis 1 deep vein thrombosis (diagnosed at baseline) 1 pulmonary embolism
2 pulmonary embolism 3 pulmonary embolism not excluded as cause of
not excluded as cause of not excluded as cause of death
death death 1 lost to follow-up
4 lost to follow-up
Figure 2: Flowchart of study patients
CTPA=computed tomography pulmonary angiography.
deep vein thromboembolism. In case of death, theoretical proportion of CTPA examinations that
information was obtained from the hospital records. would have been required if the algorithm, using the
Deaths were classified as caused by pulmonary two-level Wells’ rule outcome and fixed D-dimer
embolism if it was confirmed by autopsy, was shown threshold of less than 500 ng/mL, would have been
by objective testing before death, or could not be applied in the study population and to historical data.20
confidently excluded as a cause of death. An Finally, we compared the efficiency to the scenario in
independent adjudication committee assessed and which the age-adjusted D-dimer concentration would
adjudicated all suspected venous thromboembolism have been applied (calculated by age × 10 µg/L in
and deaths during follow-up. patients >50 years). This comparison was done post hoc
The secondary outcome was the proportion of because the final evidence supporting this approach
required CTPA examinations to complete the YEARS was not available at the moment of drafting of the
algorithm at baseline, as compared post hoc with the protocol.10 The Wells’ rule was calculated by an
292 www.thelancet.com Vol 390 July 15, 2017
Articles
independent researcher (TvdH) based on the YEARS
Patients (n=3465)
criteria entered in the case record form and information
from the medical charts. Mean age (years) 53 (18)
Women 2154 (62%)
Statistical analysis Median duration of complaints (days) 3 (1–8)
On the basis of derivation cohort of the YEARS COPD with treatment 423 (12%)
algorithm, we expected a failure rate of 1·2% in patients Heart failure with treatment 137 (4%)
managed without CTPA.19 The sample size was based Oestrogen use (% of women) 337 (16%)
on this assumption, with the aim to keep the upper Immobilisation or surgery in the past 4 weeks 407 (12%)
limit of the 95% CI of this point estimate below 2·7%.21 Outpatient 2996 (86%)
This number reflects the 3-month incidence of venous Heart rate greater than 100 beats per min 683 (20%)
thromboembolism after normal conventional pul History of pulmonary embolism or deep vein 359 (10%)
monary angiography. Any venous thromboembolism thrombosis
incidence with a complete confidence interval below Malignancy 336 (9·7%)
this safety threshold was considered to be safe. We Data are mean (SD), n (%), or median (IQR). COPD=chronic obstructive pulmonary
calculated that we needed to include 1333 patients disease.
managed without CTPA, with a two-sided α of 5% and a
Table 1: Baseline characteristics of patients with suspected pulmonary
β of 80%. Because 44% of patients in the combined embolism
YEARS derivation and validation cohort could have
been managed without CTPA and accounting for up to
7·5% loss to follow-up, a total of 3260 patients with Patients (n) Total venous Fatal pulmonary
suspected pulmonary embolism would be required.19 thromboembolism embolism* (n [%, 95% CI])
(n [%, 95% CI])
For the primary outcome regarding the safety of the
diagnostic strategy, we used a per-protocol approach. Completed algorithm 2946 18 (0·61%, 0·36–0·96) 6 (0·20%, 0·07–0·44)
For the secondary outcome regarding the efficiency of Patients managed without CTPA 1629 7 (0·43%, 0·17–0·88) 2 (0·12%, 0·01–0·44)
the diagnostic strategy, we used an intention-to-diagnose Patients managed with CTPA 1317 11 (0·84%, 0·47–1·5) 4 (0·30%, 0·12–0·78)
approach. The difference between approaches was how Patients in whom pulmonary embolism was excluded by either a low YEARS score or CT scanning were left untreated.
to report the number of CTPA that were done but not CTPA=computed tomography pulmonary angiography. *Patients who remained untreated and were not lost to
indicated by the strategy. By using this approach, follow-up.
pulmonary embolism diagnosed at presentation on a Table 2: Primary outcomes of venous thromboembolism events during 3-month follow-up
CTPA that was not indicated was considered as failures
of the diagnostic strategy.
For the secondary outcome analysis, we determined Results
the absolute difference in the number of required CTPA From Oct 5, 2013, to July 9, 2015, 3616 consecutive
examinations between the different clinical scenarios. patients with clinically suspected pulmonary embolism
Finally, we reported outcomes of not predefined post- were screened in the 12 participating hospitals, of
hoc analyses for relevant subgroups: patients with whom 151 (4·2%) were excluded (figure 2). Table 1
malignancy, patients 50 years or older, patients with a summarises the baseline characteristics. Overall,
history of venous thromboembolism, and inpatients pulmonary embolism was detected in 456 (13%) of
and patients with complaints for more than 7 days. All 3465 patients: in 55 (3·2%) of 1743 patients with none
descriptive parameters and exact 95% CIs around the of the YEARS items and 401 (23%) of 1722 patients with
observed incidences were calculated. All analyses were one or more YEARS items.
done with SPSS (version 23). According to the intention-to-diagnose approach, of the
This study is registered with the Netherlands Trial 2946 (85%) patients in whom pulmonary embolism was
Register, number NTR4193. ruled out at baseline, who remained untreated, and
completed the follow-up period, 18 patients were
Role of the funding source diagnosed with symptomatic venous thromboembolism
This study was an academically sponsored trial. The during 3-month follow-up, with an incidence of 0·61%
steering committee, consisting of the authors, had final (95% CI 0·36–0·96). The incidence of fatal pulmonary
responsibility for the study design, oversight, and data embolism was 0·20% (six patients, 95% CI 0·07–0·44;
verification and analyses. The sponsor was not involved in table 2). In a worst case scenario, accounting the
the study. All members of the steering committee five patients who were lost to follow-up (four patients had
contributed to the interpretation of the results, approved pulmonary embolism excluded without CTPA and one
the final version of the manuscript, and vouch for the patient had a negative CTPA) as recurrent venous
accuracy and completeness of the data reported. The final thromboembolism, the 3-month incidence would have
decision to submit the manuscript was made by the been 0·78% (23 of 2951 patients, 95% CI 0·49–1·2). For
corresponding author on behalf of all coauthors. the per-protocol approach, the failure rate of the
www.thelancet.com Vol 390 July 15, 2017 293
Articles
diagnostic algorithm was 0·51% (15 of 2943 patients,
Difference with YEARS algorithm
95% CI 0·31–0·84) with a 0·20% 3-month risk of fatal
combination with a D-dimer threshold of
7·4 (5·0–11)
pulmonary embolism (six of 2943, 0·08–0·46).
Efficiency compared with Wells’ rule in
19 (15–24)
15 (13–16)
14 (13–16)
13 (12–14)
14 (12–15)
14 (13–15)
14 (13–15)
13 (11–15)
14 (11–17)
% (95%CI) In the intention-to-diagnose approach, CTPA was not
done in 1611 (46%) patients and it was not indicated in
1651 (48%) patients following the per-protocol approach.
413/2996
If the standard diagnostic algorithm using Wells’
196/1448
365/2599
409/3106
453/3129
282/2017
113/866
65/469
25/336
69/359
rule and D-dimer with fixed threshold of <500 ng/mL
n/N
would have been applied, 1174 (34%) patients could
<500 ng/mL
have been managed without CTPA at baseline, for an
Managed
CTPA (n)
without
absolute difference of 13% (difference in intention-to-
37
1137
1039
704
901
470
273
54
1120
135
diagnose approach 437 CTPA examinations, 95% CI
10–15%) and 14% (difference in per-protocol approach
embolism was excluded at baseline
Overall incidence after pulmonary
477 CTPA examinations, 12–16%) in favour of the
0·59 (0·36–0·96)
0·26 (0·07–0·96)
0·15 (0·04–0·56)
0·55 (0·33–0·92)
0·41 (0·23–0·73)
0·83 (0·23–3·0)
YEARS algorithm.
0·73 (0·45–1·2)
0·98 (0·6–1·6)
1·0 (0·40–2·6)
2·6 (1·3–5·2)
If Wells’ rule and the age-adjusted D-dimer threshold
% (95% CI)
would have been applied, 1348 (39%) patients could have
been managed without CTPA at baseline, an absolute
difference of 8·7% (difference in per-protocol approach
11/2679
16/1642
2/1309
14/2558
16/2195
16/2710
CTPA examinations 303, 95% CI 6·4–11%) and of 7·6%
patients
4/393
2/756
2/241
7/272
Events/
Data are n or n (%), unless otherwise specified. PE=pulmonary embolism. CTPA=computed tomography pulmonary angiography. VTE=venous thromboembolism.
(difference in intention-to-diagnose approach CTPA
examinations 263, 95% CI 5·3–9·9%).
In the subgroups of patients younger than 50 years and
Incidence in patients managed
0·84 (0·46–1·5)
0·96 (0·50–1·8)
0·81 (0·14–4·6)
0·24 (0·04–1·4)
50 years and older, a 14% absolute reduction in the
0·54 (0·25–1·2)
0·71 (0·36–1·4)
0·53 (0·15–1·9)
1·5 (0·52–4·4)
2·4 (1·0–5·4)
1·1 (0·6–2·0)
number of required CTPA examinations was observed
% (95% CI)
when the YEARS algorithm was applied compared with
the standard diagnostic algorithm, with failure rates of
0·11% (one of 894, 95% CI 0·02–0·63) and 0·81%
with CTPA
6/1106
10/1193
8/1119
(six of 740, 0·37–1·8), respectively. Table 3 summarises
9/942
10/902
3/198
patients
1/415
1/124
2/375
5/211
Events/
the results for the other subgroups.
Risk of VTE during 3-month follow-up
Figure 2 shows the management of all 3465 included
patients. Of the 1651 patients who should have been
0·40 (0·18–0·86)
Incidence in patients managed
0·42 (0·19–0·91)
0·11 (0·02–0·63)
0·32 (0·14–0·74)
managed without CTPA, the protocol was violated in
0·51 (0·09–2·9)
0·85 (0·15–4·7)
0·81 (0·37–1·8)
0·56 (0·27–1·2)
3·2 (0·90–11)
40 patients. CTPA showed pulmonary embolism in
% (95% CI)
0 (0–1·0)
three patients who were treated with anticoagulants. These
observations were considered diagnostic failures and are
Table 3: Primary outcome and efficiency in subgroups of the total study population
without CTPA
included in the primary outcome. Furthermore, 18 (1·1%)
of 1651 patients were treated with oral anticoagulants for
patients
6/1439
7/1253
5/1573
6/1517
Events/
1/894
0/381
1/195
6/740
1/117
2/61
other reasons (ie, eight atrial fibrillation, one superficial
thrombophlebitis, and nine other reasons including
idiopathic pulmonary hypertension and peripheral arterial
PE at baseline Managed
without
disease) and four (0·24%) of 1651 patients were lost to
62
1590
900
1266
752
386
123
1529
200
1452
CTPA
follow-up. Four of the remaining 1589 patients returned
with symptomatic events of venous thromboembolism
126 (8·7%)
330 (16%)
107 (30%)
362 (14%)
66 (14%)
399 (13%)
390 (13%)
57 (17%)
94 (11%)
349 (11%)
(table 4). The 3-month incidence of venous thrombo
embolism in patients who did not have CTPA according to
the YEARS algorithm was 0·43% (seven of 1629, 95% CI
0·17–0·88) and of fatal pulmonary embolism was 0·12%
Patients
(two of 1629, 0·01–0·44; table 2). Seven other patients
336
3129
1448
2599
2017
866
359
3106
469
2996
(0·43%) died of non-venous-thrombo embolism-related
causes.
Of the 1358 patients in whom CTPA ruled out
Complaints ≤7 days
Complaints >7 days
No history of VTE
pulmonary embolism, 40 patients (2·95%) were treated
Aged <50 years
Aged ≥50 years
No malignancy
History of VTE
with anticoagulants for other reasons (ie, 20 atrial
Malignancy
Outpatient
Inpatient
fibrillation, three superficial thrombophlebitis, one
splanchnic vein thrombosis, one thrombus in the left
ventricle, one high-dose thrombosis prophylaxis, one
294 www.thelancet.com Vol 390 July 15, 2017
Articles
Sex Age YEARS Wells’ D-dimer Interval Outcome Circumstances of outcome event Adjudicated as
(years) score score* concentration (days)
(ng/mL)
Patient 1 Female 59 0 0 609 54 Death Patient developed cardiac arrest during admission for Pulmonary embolism not
acute severe pancreatitis, and was known to have excluded as cause of death
myotonic dystrophy type 1 with severe cardiomyopathy
and arrhythmias; implantable cardioverter-defibrillator
was deactivated after regular unjustified defibrillations;
resuscitation was unsuccessful
Patient 2 Male 78 0 1 898 11 Death Patient was diagnosed with end-stage metastasised Pulmonary embolism not
oropharyngeal carcinoma; found deceased in nursing home excluded as cause of death
Patient 3 Female 89 0 1·5 610 18 Pulmonary embolism Patient diagnosed on CTPA with subsegmental pulmonary Non-fatal pulmonary
embolism during admission for pneumonia and acute embolism
heart failure related to severe aortic valve stenosis and
mitral valve insufficiency. Patient died 7 days after
treatment, which was voluntarily withheld
Patient 4 Male 52 0 1 560 49 Deep vein thrombosis Patient had deep vein thrombosis 14 days after surgery for Deep vein thrombosis
glioblastoma multiforme
Patient 5 Female 21 2 5·5 380 0 Pulmonary embolism CTPA done because of protocol violation at baseline Non-fatal pulmonary
embolism
Patient 6 Male 58 1 3 420 0 Pulmonary embolism CTPA done because of protocol violation at baseline Non-fatal pulmonary
embolism
Patient 7 Female 71 1 6 410 0 Pulmonary embolism CTPA done because of protocol violation at baseline Non-fatal pulmonary
embolism
CTPA=computed tomography pulmonary angiography. *Calculated post hoc.
Table 4: Diagnostic failures in patients who were managed without CTPA at baseline
suspected but later ruled out pulmonary vein 0·12–0·78) of patients in our study compared with 0·6%
thrombosis, one vena cava superior syndrome due to (0·4–1·1) in another study using standard algorithms.22
mediastinal mass, and 12 other reasons including The advantage of the YEARS algorithm over existing
idiopathic pulmonary hypertension and peripheral algorithms is the large reduction in the need for CTPA,
arterial disease) and one patient (0·07%) was lost to which reduces radiation exposure and overdiagnosis,1–4,23
follow-up. Of the 1317 remaining patients, 11 patients and is achieved by using variable D-dimer thresholds
returned with symptomatic events of venous thrombo depending on the clinical probability. This study is the
embolism (table 5). The 3-month incidence of venous first prospective outcome study that validated a D-dimer
thromboembolism was 0·84% (11 of 1317, 95% CI threshold of 1000 ng/mL in patients with a low clinical
0·47–1·5) and incidence of fatal pulmonary embolism probability.
was 0·30% (four of 1317, 0·12–0·78; table 2). 85 other While our study was ongoing, another strategy to
patients (6·5%) died of non-venous-thromboembolism- reduce the number of CTPA has been validated in a
related causes. prospective outcome study: the age-adjusted D-dimer
threshold.10 If this strategy would have been applied to
Discussion our study population, the YEARS algorithm would have
Our study showed that the YEARS algorithm safely led to an absolute reduction of 8·7% (95% CI 6·4–11) of
excluded acute pulmonary embolism. An absolute 14% CTPA. The main reason for this difference is the
decrease in the need for CTPA was achieved, compared applicability of the YEARS algorithm to patients with
with the standard algorithm. The 3-month incidence of suspected acute pulmonary embolism in all ages, and
venous thromboembolism in patients who did not not only in patients older than 50 years. In patients
undergo CTPA was in line with that observed in studies younger than 50 years, the YEARS algorithm leads to
using algorithms with sequential diagnostic testing and a 14% absolute reduction of CTPA. Of note, reducing the
traditional two-level Wells’ score, and a fixed cutoff number of CTPA is very relevant for young patients,
concentration of D-dimer of 500 ng/mL: 0·43% (95% CI particularly women, in whom concerns have been raised
0·17–0·88) in our study versus 0·34% (0·036–0·96) about long-term effects of radiation on the risk of breast
reported by a meta-analysis.20 Moreover, the risk of cancer.
recurrent venous thromboembolism in patients with a Methodological strengths of the study include the large
normal CTPA was comparable to the risk observed in number of consecutive patients, the near complete
previous studies using standard algorithms: 0·84% follow-up, and the independent adjudication of endpoints.
(95% CI 0·47–1·5) versus 1·2% (0·8–1·8).22 Additionally, Furthermore, by studying a real-world cohort of patients
fatal pulmonary embolism occurred in 0·30% (95% CI in daily practice, we expect that the YEARS algorithm can
www.thelancet.com Vol 390 July 15, 2017 295
Articles
Sex Age YEARS Wells’ D-dimer Interval Outcome Circumstances of outcome event Adjudicated as
(years) score score* concentration (days)
(ng/mL)
Patient 1 Male 50 0 1·5 1070 34 Deep vein thrombosis Patient had vena cava superior syndrome caused by Thrombosis of the vena
thrombosis at the site of the pacemaker leads cava superior
Patient 2 Female 73 0 3 1480 69 Death Patient died in hospital under the clinical diagnosis of a Pulmonary embolism not
pneumonia and acute heart failure excluded as cause of death
Patient 3 Female 79 0 3 2400 26 Pulmonary embolism Initiation of anticoagulation because of suspected pulmonary Non-fatal pulmonary
embolism without CTPA confirmation after hospital embolism
admission because of heart failure and COPD exacerbation
Patient 4 Female 82 0 0 2550 Unknown Death Patient died in nursing home after hospital admission Pulmonary embolism not
because of acute heart failure and exacerbation of COPD excluded as cause of death
Patient 5 Female 57 0 1 4170 12 Pulmonary embolism Patient was known to have recurrent sarcoma of the uterus; Non-fatal pulmonary
subsegmental pulmonary embolism diagnosed embolism
postoperatively; patient died 33 days after diagnosis of
pulmonary embolism during palliative care in a hospice
Patient 6 Female 70 0 1 2400 17 Death Patient died after sudden collapse followed by unsuccessful Pulmonary embolism not
resuscitation 1 day after surgery for gastric carcinoma excluded as cause of death
Patient 7 Female 73 1 5·5 2500 6 Deep vein thrombosis Patient was known to have leukaemia; developed Deep vein thrombosis
thrombosis of the brachial vein after superficial
thrombophlebitis related to an intravenous catheter
Patient 8 Male 84 1 4 5000 32 Deep vein thrombosis Patient was known to have metastasised prostate cancer; Deep vein thrombosis
developed deep vein thrombosis after immobilisation
during admission at the hospital
Patient 9 Female 66 1 7 1325 43 Death Patient had curative treatment for lung cancer and a stent Pulmonary embolism not
placed for post-radiation stenosis of the trachea; patient died excluded as cause of death
at home after sudden haemoptysis
Patient 10 Male 70 1 3 5000 68 Deep vein thrombosis Patient had subclavian vein thrombus associated with Deep vein thrombosis
intravenous catheter
Patient 11 Female 48 1 3 747 78 Deep vein thrombosis Patient developed deep vein thrombosis and was diagnosed Deep vein thrombosis
with antiphospholipid syndrome
CTPA=computed tomography pulmonary angiography. COPD=chronic obstructive pulmonary disease. *Calculated post hoc.
Table 5: Diagnostic failures in patients who were managed with CTPA at baseline
be easily implemented outside the participating study dying in an outpatient setting. Even so, although
sites, and that our data for safety and efficiency are pulmonary embolism was conservatively adjudicated as
representative for non-trial conditions. Additionally, our the cause of death in these patients, the recurrence rate
results are in line with the numbers reported in the initial observed in our study remained well below the safety
derivation and retrospective validation study of our threshold, reinforcing the validity of our findings.
algorithm.19 Of note, although haemodynamic instability Furthermore, the prevalence of pulmonary embolism
was not a formal exclusion criterion of this study, we have was higher than observed in large cohorts in North
described a cohort of only haemodynamically stable America, but lower than observed in previous studies in
patients. Europe. The study patients were relatively young, but
Limitations of our the study are the absence of a control identical to those in an earlier large diagnostic
group because we did not do a randomised study and management study by our group.7 The results of the
could therefore not directly compare the risk of venous subgroup analyses, however, confirm the validity of
thromboembolism with a control group that would have applying the YEARS algorithm in a patient cohort with
been managed with traditional algorithms. However, the higher pulmonary embolism prevalence of up to 30%
low observed 3-month risk of venous thromboembolism and provide evidence of the generalisability of our
and near complete follow-up strongly support the chosen findings. Lastly, there were 43 violations of the study
study design. Moreover, although an independent protocol, with a D-dimer test not done in three patients
committee evaluated and adjudicated all endpoints, and a non-indicated CTPA done in 40 patients, of which
autopsy was hardly scarcely done. As a consequence, it three confirmed the presence of acute pulmonary
was difficult to exclude pulmonary embolism as a embolism. This number is comparable to that in the
possible cause of death in six patients during follow-up. Christopher study, in which two of 25 unjustified CTPA
These patients already had or developed extensive examinations revealed pulmonary embolism.7 Finally,
comorbidity, or went into the final stage of a terminal because of the small number of patients with cancer
illness during the follow-up period, with most of them included in our study, the safety of this algorithm for
296 www.thelancet.com Vol 390 July 15, 2017
Articles
patients with suspected pulmonary embolism in the 6 Schuur JD, Carney DP, Lyn ET, et al. A top-five list for emergency
presence of cancer remains to be determined. medicine: a pilot project to improve the value of emergency care.
JAMA Intern Med 2014; 174: 509–15.
In conclusion, the YEARS diagnostic algorithm safely 7 Christopher Study Investigators. Effectiveness of managing
ruled out acute pulmonary embolism in patients suspected pulmonary embolism using an algorithm combining
presenting with clinically suspected pulmonary embolism, clinical probability, D-dimer testing, and computed tomography.
JAMA 2006; 295: 172–79.
with a low risk for venous thromboembolism during a 8 van Es N, van der Hulle T, van Es J, et al. Wells rule and D-dimer
3-month follow-up. The main advantage of the YEARS testing to rule out pulmonary embolism: a systematic review and
algorithm is the absolute 14% decrease in the number of individual-patient data meta-analysis. Ann Intern Med 2016;
165: 253–61.
CTPA examinations that is applicable to all ages and was 9 Douma RA, Mos IC, Erkens PM, et al. Performance of 4 clinical
shown consistently across subgroups. decision rules in the diagnostic management of acute pulmonary
embolism: a prospective cohort study. Ann Intern Med 2011;
Contributors
154: 709–18.
TvdH, FAK, JvE, SM, and MVH designed the study. TvdH, FAK, and MVH
10 Righini M, van Es J, den Exter PL, et al. Age-adjusted D-dimer
managed the study with support and input from all other authors. TvdH,
cutoff levels to rule out pulmonary embolism: the ADJUST-PE
FAK, and MVH analysed the data, which were interpreted by all other study. JAMA 2014; 311: 1117–24.
authors. TvdH, FAK, and MVH wrote the first draft of the manuscript,
11 Roy PM, Meyer G, Vielle B, et al. Appropriateness of diagnostic
which was reviewed, modified, and approved by all other authors. All management and outcomes of suspected pulmonary embolism.
authors vouch for the accuracy and completeness of the data reported and Ann Intern Med 2006; 144: 157–64.
for keeping the study to the protocol. 12 Newnham M, Stone H, Summerfield R, et al. Performance of
Declaration of interests algorithms and pre-test probability scores is often overlooked in
We declare no competing interests. the diagnosis of pulmonary embolism. BMJ 2013; 346: f1557.
13 Teismann NA, Cheung PT, Frazee B. Is the ordering of imaging
YEARS study group for suspected venous thromboembolism consistent with D-dimer
Writing group: Netherlands T van der Hulle, F A Klok, C Heringhaus, result? Ann Emerg Med 2009; 54: 442–46.
M V Huisman (Leiden University Medical Center, Leiden); W Y Cheung, 14 Adams DM, Stevens SM, Woller SC, et al. Adherence to
S Middeldorp, L F M Beenen (Academic Medical Center, Amsterdam); PIOPED II investigators’ recommendations for computed
S Kooij, A T A Mairuhu, L M van der Pol (Haga Hospital, The Hague); tomography pulmonary angiography. Am J Med 2013; 126: 36–42.
H Hofstee (Medisch Centrum Haaglanden, The Hague); M J H A Kruip, 15 Jones P, Elangbam B, Williams NR. Inappropriate use and
S Schol-Gelok (Erasmus Medical Center, Rotterdam); M ten Wolde interpretation of D-dimer testing in the emergency department:
(Flevo Hospital, Almere); G M Hazelaar, MMC Hovens; T van Bemmel; an unexpected adverse effect of meeting the “4-h target”.
J van Es (Onze Lieve Vrouwe Gasthuis Hospital, Amsterdam); L M Faber Emerg Med J 2010; 27: 43–47.
(Red Cross Hospital, Beverwijk); K A H Kaasjager, M Nijkeuter (University 16 Gibson NS, Sohne M, Gerdes VE, Nijkeuter M, Buller HR.
Medical Center Utrecht, Utrecht); R F Loeffen, R C J van Klink (Alrijne The importance of clinical probability assessment in interpreting
Hospital, Leiderdorp). a normal D-dimer in patients with suspected pulmonary
Contributing authors: Netherlands A J Fogteloo, L J M Kroft (Leiden embolism. Chest 2008; 134: 789–93.
University Medical Center, Leiden); M P Brekelmans (Academic Medical 17 Roy PM, Durieux P, Gillaizeau F, et al. A computerized
Center, Amsterdam); R M J Vermaire, H Bastiaansen-Bergsma (Haga handheld decision-support system to improve pulmonary
embolism diagnosis: a randomized trial. Ann Intern Med 2009;
Hospital, The Hague); J S Biedermann (Erasmus Medisch Centrum,
151: 677–86.
Rotterdam); A Klijn, S van der Voort, A W E Lieveld (Flevo Hospital,
18 Jiménez D, Resano S, Otero R, et al. Computerised clinical
Almere); P Y de Jong (Rijnstate Hospital, Arnhem); C G Schaar (Gelre
decision support for suspected PE. Thorax 2015; 70: 909–11.
Hospital, Apeldoorn); A Iglesias del Sol (Alrijne Hospital, Leiderdorp).
19 van Es J, Beenen LFM, Douma RA, et al. A simple decision rule
Adjudication committee: Netherlands H ten Cate, K Hamulyak (Maastricht
including D-dimer to reduce the need for computed tomography
University Medical Center, Maastricht). scanning in patients with suspected pulmonary embolism.
Acknowledgments J Thromb Haemost 2015; 138: 1428–35.
This study was supported by unrestricted grants from the participating 20 Pasha SM, Klok FA, Snoep JD, et al. Safety of excluding acute
hospitals. pulmonary embolism based on an unlikely clinical probability by
the Wells rule and normal D-dimer concentration:
References a meta-analysis. Thromb Res 2010; 125: e123–27.
1 Wiener RS, Schwartz LM, Woloshin S. Time trends in pulmonary 21 van Beek EJ, Brouwerst EM, Song B, et al. Clinical validity of a
embolism in the United States: evidence of overdiagnosis. normal pulmonary angiogram in patients with suspected
Arch Intern Med. 2011; 171: 831–37. pulmonary embolism—a critical review. Clin Radiol 2001;
2 Sarma A, Heilbrun ME, Conner KE, et al. Radiation and chest CT 56: 838–42.
scan examinations: what do we know? Chest 2012; 142: 750–60. 22 Mos IC, Klok FA, Kroft LJ, et al. Safety of ruling out acute
3 Brenner DJ, Hall EJ. Computed tomography—an increasing source pulmonary embolism by normal computed tomography
of radiation exposure. N Engl J Med 2007; 357: 2277–84. pulmonary angiography in patients with an indication for
4 O’Neill J, Murchison JT, Wright L, et al. Effect of the introduction of computed tomography: systematic review and meta-analysis.
helical CT on radiation dose in the investigation of pulmonary J Thromb Haemost 2009; 7: 1491–98.
embolism. Br J Radiol 2005; 78: 46–50. 23 Wiener RS, Schwartz LM, Woloshin S. When a test is too good:
5 Kooiman J, Klok FA, Mos IC, et al. Incidence and predictors of how CT pulmonary angiograms find pulmonary emboli that do
contrast-induced nephropathy following CT-angiography for clinically not need to be found. BMJ 2013; 347: f3368.
suspected acute pulmonary embolism. J Thromb Haemost 2010;
8: 409–11.
www.thelancet.com Vol 390 July 15, 2017 297
You might also like
- Clinical Cases in Chronic Thromboembolic Pulmonary HypertensionFrom EverandClinical Cases in Chronic Thromboembolic Pulmonary HypertensionWilliam R. AugerNo ratings yet
- Years Tep en EmbarazoDocument11 pagesYears Tep en EmbarazoAngela Maria Giraldo MillanNo ratings yet
- Nej Mo A 1507807Document11 pagesNej Mo A 1507807Leiniker NavarroNo ratings yet
- Blue ProtocolDocument11 pagesBlue Protocoloana florianaNo ratings yet
- Diagnosis of Pulmonary Embolism With D-Dimer Adjusted To Clinical ProbabilityDocument10 pagesDiagnosis of Pulmonary Embolism With D-Dimer Adjusted To Clinical Probabilityon miniNo ratings yet
- Age-Adjusted D-Dimer Cutoff Levels To Rule Out Pulmonary Embolism The ADJUST-PE StudyDocument8 pagesAge-Adjusted D-Dimer Cutoff Levels To Rule Out Pulmonary Embolism The ADJUST-PE StudyRoxana Maria MunteanuNo ratings yet
- 10 1001@jamaneurol 2019 0525Document5 pages10 1001@jamaneurol 2019 0525Axel DuncanNo ratings yet
- Pulmonary EmbolismDocument14 pagesPulmonary EmbolismChrysi TsiouriNo ratings yet
- Comparison of International Guideline Recommendations For Rhe Diagnosis Pulmonary EmbolismDocument14 pagesComparison of International Guideline Recommendations For Rhe Diagnosis Pulmonary EmbolismdrjavierbuenfilNo ratings yet
- 2018 - Chronic Thromboembolic Pulmonary HypertensionDocument10 pages2018 - Chronic Thromboembolic Pulmonary HypertensionSebastian PuertoNo ratings yet
- JTD 09 03 768Document11 pagesJTD 09 03 768nanaNo ratings yet
- Journal Pulmonary HypertensionDocument8 pagesJournal Pulmonary HypertensionFirman SyahNo ratings yet
- Thoracoscopic Drainage of EmpyemaDocument5 pagesThoracoscopic Drainage of EmpyemaDr Nilesh NagdeveNo ratings yet
- Management of Patients Admitted With Pneumothorax: A Multi-Centre Study of The Practice and Outcomes in Hong KongDocument7 pagesManagement of Patients Admitted With Pneumothorax: A Multi-Centre Study of The Practice and Outcomes in Hong Kongハルァン ファ烏山No ratings yet
- Fa y StrokeDocument11 pagesFa y StrokeCatherine Galdames HinojosaNo ratings yet
- Thrombolysis With Alteplase 3 To 4.5 Hours After Acute Ischemic StrokeDocument13 pagesThrombolysis With Alteplase 3 To 4.5 Hours After Acute Ischemic StrokeParvathy R NairNo ratings yet
- JurnalDocument8 pagesJurnalwiliaNo ratings yet
- Eficacia de La Telemedicina en El Manejo de La Insuficiencia CardíacaDocument11 pagesEficacia de La Telemedicina en El Manejo de La Insuficiencia CardíacaSMIBA MedicinaNo ratings yet
- Long-Term Outcome After Thrombolysis For Acute Lower Limb IschaemiaDocument9 pagesLong-Term Outcome After Thrombolysis For Acute Lower Limb IschaemiaIdham Adyasa Manggala PutraNo ratings yet
- Nejmoa2107727-Alteplase in StrokeDocument12 pagesNejmoa2107727-Alteplase in Stroketommy taylor084No ratings yet
- MEDENOX Trial - Enoxa Vs Placebo em Pacientes Críticos Clínicos - NEJM 1999Document8 pagesMEDENOX Trial - Enoxa Vs Placebo em Pacientes Críticos Clínicos - NEJM 1999Larissa BianchiniNo ratings yet
- Comparison of 3 Clinical Models For Predicting The Probability of Pulmonary EmbolismDocument8 pagesComparison of 3 Clinical Models For Predicting The Probability of Pulmonary EmbolismAlirio Rodrigo Bastidas GoyesNo ratings yet
- Reynolds 2010Document6 pagesReynolds 2010Putra PratamaNo ratings yet
- RCCM 202212-2300ocDocument14 pagesRCCM 202212-2300ocLucas PereiraNo ratings yet
- Evaluation of The "Hemoptysis" Item in Clinical Decision Rules For The Diagnosis of Pulmonary Embolism in The Emergency DepartmentDocument8 pagesEvaluation of The "Hemoptysis" Item in Clinical Decision Rules For The Diagnosis of Pulmonary Embolism in The Emergency DepartmentNiatazya Mumtaz SagitaNo ratings yet
- Journal of Cardiothoracic and Vascular Anesthesia: Original ArticleDocument11 pagesJournal of Cardiothoracic and Vascular Anesthesia: Original ArticleRicardoNo ratings yet
- Clopidogrel Versus Ticagrelor o Prasugrel en Pacientes de 70 Años o Más Con Síndrome Coronario Agudo Sin Elevación Del Segmento ST (POPular AGE)Document8 pagesClopidogrel Versus Ticagrelor o Prasugrel en Pacientes de 70 Años o Más Con Síndrome Coronario Agudo Sin Elevación Del Segmento ST (POPular AGE)Frank Antony Arizabal GaldosNo ratings yet
- Race Ii 2010 NejmDocument11 pagesRace Ii 2010 NejmAxel Hiram Hernandez PinedaNo ratings yet
- Compresor Intermitente TVPDocument9 pagesCompresor Intermitente TVPgiseladelarosa2006No ratings yet
- Analysis of Post Operative Systemic To Pulmonary Artery Shunt FailureDocument5 pagesAnalysis of Post Operative Systemic To Pulmonary Artery Shunt FailurePaul HartingNo ratings yet
- Analysis of Patients With Hemoptysis in A Tertiary Referral HospitalDocument8 pagesAnalysis of Patients With Hemoptysis in A Tertiary Referral HospitalNadia Mrz Mattew MuseNo ratings yet
- Annsurg00186 0127Document14 pagesAnnsurg00186 0127Muhammad NomanNo ratings yet
- Reseccion Pulmonar en Hemoptisis SeveraDocument10 pagesReseccion Pulmonar en Hemoptisis SeverarafodocNo ratings yet
- Diagnosis of Pulmonary Embolism During PregnancyDocument9 pagesDiagnosis of Pulmonary Embolism During PregnancyFátima AlmeidaNo ratings yet
- Membrane Versus Centrifuge-Based Therapeutic Plasma Exchange, A Randomized Prospective Crossover StudyDocument6 pagesMembrane Versus Centrifuge-Based Therapeutic Plasma Exchange, A Randomized Prospective Crossover Studyalida romeroNo ratings yet
- Roberts2015 PDFDocument11 pagesRoberts2015 PDFJeff LapianNo ratings yet
- Articles: BackgroundDocument11 pagesArticles: BackgroundricardojosesotofontalvoNo ratings yet
- Managementul Acut Al TVC La Cei in Tratament Cu AntiagregantDocument21 pagesManagementul Acut Al TVC La Cei in Tratament Cu AntiagregantDrHellenNo ratings yet
- Catheter Ablation For Atrial Fibrillation: Original ArticleDocument7 pagesCatheter Ablation For Atrial Fibrillation: Original ArticleGavin WinkelNo ratings yet
- Hemoptysis - Etiology, Evaluation and Treatment in A University HospitalDocument8 pagesHemoptysis - Etiology, Evaluation and Treatment in A University HospitalAngga Maulana IbrahimNo ratings yet
- Ahmad 2018Document14 pagesAhmad 2018Cristopher OchoaNo ratings yet
- Neto2016 2 PDFDocument9 pagesNeto2016 2 PDFAnderson LondoñoNo ratings yet
- Glycemic Control and Radiographic Manifestations of Tuberculosis in Diabetic PatientsDocument17 pagesGlycemic Control and Radiographic Manifestations of Tuberculosis in Diabetic PatientsGlenda B AjilaNo ratings yet
- PNEUNODocument7 pagesPNEUNOAnselmo SantosNo ratings yet
- Management of Pneumothorax in Emergency Medicine Departments: Multicenter TrialDocument6 pagesManagement of Pneumothorax in Emergency Medicine Departments: Multicenter TrialYuliana WiralestariNo ratings yet
- Comprehensive Analysis of The Results of The Pioped Study: Ã %//Q) Lungscaninterpretation. MethodsdatafromthepiopedDocument8 pagesComprehensive Analysis of The Results of The Pioped Study: Ã %//Q) Lungscaninterpretation. MethodsdatafromthepiopedPedro BurgosNo ratings yet
- HemoptisisDocument7 pagesHemoptisiswiliaNo ratings yet
- New England Journal Medicine: The ofDocument10 pagesNew England Journal Medicine: The ofNatalia ArizaNo ratings yet
- Acceso Vascular para RPTDocument10 pagesAcceso Vascular para RPTSergey ProskurinNo ratings yet
- Percutaneous Transluminal Angioplasty and Stenting As First-Choice Treatment in Patients With Chronic Mesenteric IschemiaDocument6 pagesPercutaneous Transluminal Angioplasty and Stenting As First-Choice Treatment in Patients With Chronic Mesenteric IschemiaCotaga IgorNo ratings yet
- CTEPH and Klippel Trenaunay SyndromeDocument6 pagesCTEPH and Klippel Trenaunay SyndromeAndreiSefNo ratings yet
- Endocarditis in The Elderly: Clinical, Echocardiographic, and Prognostic FeaturesDocument8 pagesEndocarditis in The Elderly: Clinical, Echocardiographic, and Prognostic FeaturesMehdi285858No ratings yet
- Olesen2018 PDFDocument9 pagesOlesen2018 PDFS3V4_9154No ratings yet
- CTEPH - JACC 2020 - FocusDocument15 pagesCTEPH - JACC 2020 - FocusDaniela PekeNo ratings yet
- Mertens2021 Article TransthoracicVersusTranshiatalDocument9 pagesMertens2021 Article TransthoracicVersusTranshiatalDr Shiv ChopraNo ratings yet
- Icvts Ivv355 FullDocument7 pagesIcvts Ivv355 FullAldo AtjehNo ratings yet
- 1 s2.0 S1743919121003848 MainDocument7 pages1 s2.0 S1743919121003848 MainYaum AamrunaNo ratings yet
- 1 s2.0 S0007091217542075 MainDocument11 pages1 s2.0 S0007091217542075 Maineny_sumaini65No ratings yet
- Estenosis Traqueal ComplejaDocument8 pagesEstenosis Traqueal ComplejaFabiolaNo ratings yet
- JTD 10 06 3216Document9 pagesJTD 10 06 3216madeNo ratings yet
- TL-WR1043ND V2 DatasheetDocument3 pagesTL-WR1043ND V2 DatasheetFlávio OliveiraNo ratings yet
- PostProcessing BruyereDocument45 pagesPostProcessing BruyereThirugnanam DhandayuthapaniNo ratings yet
- DISC 322-Optimization Methods For Management Science - Sec 2 - Dr. Muhammad Tayyab - Spring 2020 PDFDocument6 pagesDISC 322-Optimization Methods For Management Science - Sec 2 - Dr. Muhammad Tayyab - Spring 2020 PDFMuhammad UsmanNo ratings yet
- Sem 3Document1 pageSem 3aes eventNo ratings yet
- Getinge Solsus SpecificationDocument16 pagesGetinge Solsus SpecificationNada SolomunNo ratings yet
- Components of Valve Assembly Shown 27 and 28. Ofthe Are Figures 37. Use Bottom-Up Approach AssemblyDocument2 pagesComponents of Valve Assembly Shown 27 and 28. Ofthe Are Figures 37. Use Bottom-Up Approach AssemblyLuis Perez MarquezNo ratings yet
- Natural and Artificial Rockslide DamsDocument649 pagesNatural and Artificial Rockslide DamsCarlos Augusto Sánchez RondónNo ratings yet
- OMS413 Review Questions (Chapters 1,2,3,4 and 5) Part I. ConceptDocument2 pagesOMS413 Review Questions (Chapters 1,2,3,4 and 5) Part I. Conceptdev4c-1No ratings yet
- European Toolkit For Policy Making and Usage IFMSA EYFDocument19 pagesEuropean Toolkit For Policy Making and Usage IFMSA EYFSKNo ratings yet
- Globalization: Chapter 2, Sec 4 Social StudiesDocument143 pagesGlobalization: Chapter 2, Sec 4 Social StudiesJoel CerezoNo ratings yet
- Maintenance Request Procedure 2Document2 pagesMaintenance Request Procedure 2azhan114No ratings yet
- Cornetto Pop Award - Brief v3Document14 pagesCornetto Pop Award - Brief v3Adji Ard100% (1)
- Tara Sanitary Wares & Tiles: QuotationDocument2 pagesTara Sanitary Wares & Tiles: Quotationsharath mathewNo ratings yet
- BrochureDocument3 pagesBrochurealhumdulilahNo ratings yet
- Tir Lens Guide-Web PDFDocument8 pagesTir Lens Guide-Web PDFFilozófus ÖnjelöltNo ratings yet
- Grade Point Average: What's Wrong and What's The Alternative?Document12 pagesGrade Point Average: What's Wrong and What's The Alternative?annisa AnnisaNo ratings yet
- 14-Fire Alarm Controller JB-QB-4508 - Operation Manual - REV - 05Document33 pages14-Fire Alarm Controller JB-QB-4508 - Operation Manual - REV - 05Cristal Gumalang100% (2)
- 3.4 Cold Bending: Yct Technical Guide 3-Section 3 - Installation GuideDocument1 page3.4 Cold Bending: Yct Technical Guide 3-Section 3 - Installation GuidemohansafNo ratings yet
- Design Fabrication of A Solar Powered Stirling EngineDocument65 pagesDesign Fabrication of A Solar Powered Stirling EngineSirajus Salekin [Id:37]No ratings yet
- Analytics AssignmentDocument4 pagesAnalytics AssignmentShishir MaxNo ratings yet
- Goodman, Nelson - On StarmakingDocument3 pagesGoodman, Nelson - On StarmakingAilin DurrutyNo ratings yet
- Statistical Signal Processing: ECE 5615 Lecture Notes Spring 201 9Document32 pagesStatistical Signal Processing: ECE 5615 Lecture Notes Spring 201 9rizwanNo ratings yet
- Ana Criselda B. Magnabihon - ResumeDocument2 pagesAna Criselda B. Magnabihon - ResumearrenzmagnabihonNo ratings yet
- MISUMI - Mold Plastic Injection Standard ComponentDocument1 pageMISUMI - Mold Plastic Injection Standard Componentgemilang metalindoNo ratings yet
- Shivaji University, Kolhapur Programme For Practical /oral Examination To Be Held in April 2018 CENTRE:PVPIT Budhgaon Exam: M.E. - I /Ii/IiiDocument1 pageShivaji University, Kolhapur Programme For Practical /oral Examination To Be Held in April 2018 CENTRE:PVPIT Budhgaon Exam: M.E. - I /Ii/IiisatishNo ratings yet
- Mavic 2 Enterprise: User ManualDocument58 pagesMavic 2 Enterprise: User ManualLeoTNo ratings yet
- Sistemas A320Document115 pagesSistemas A320Juan Pablo Montoya MNo ratings yet
- SubqueryDocument4 pagesSubqueryDGreatWannieNo ratings yet
- Application of Six Sigma With Respect To Abbott Laboratories.Document17 pagesApplication of Six Sigma With Respect To Abbott Laboratories.NITIN SINGHNo ratings yet
- GED102 Module 3 Project: Group Members: Raynard Yu John Luis Arce Miguel Agustin Galang Paul Cauman Renz Eugene GurionDocument6 pagesGED102 Module 3 Project: Group Members: Raynard Yu John Luis Arce Miguel Agustin Galang Paul Cauman Renz Eugene GurionqwertasdfgNo ratings yet