Professional Documents
Culture Documents
Micronutrient Supplementation and Monitoring
Uploaded by
Gabriel LorcaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Micronutrient Supplementation and Monitoring
Uploaded by
Gabriel LorcaCopyright:
Available Formats
Digestive diseases
Division A
Guideline
Micronutrient supplementation and monitoring after
total and subtotal gastrectomy
Key messages
Vitamins and minerals are likely to be poorly absorbed after gastrectomy.
All patients should take a daily multivitamin and mineral tablet.
After total gastrectomy, all patients should receive 12 weekly vitamin B12 injections.
It is possible that micronutrient deficiency could develop even with supplementation.
All patients should be regularly screened for micronutrient deficiencies as outlined
below.
Summary
All patients who have undergone total or partial gastrectomy (excluding sleeve
gastrectomy) should receive daily oral multivitamin and mineral supplementation
and intramuscular vitamin B12 supplementation every 12 weeks. Micronutrient
status should be monitored as per the schedule below:
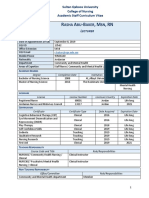
Test Frequency
U&Es (including magnesium) Six monthly for two years, then annually
Creatinine Six monthly for two years, then annually
Liver function tests Six monthly for two years, then annually
Full blood count Six monthly for two years, then annually
Ferritin Six monthly for two years, then annually
B12 (pre-injection) Annually
Folate Six monthly for two years, then annually
Calcium Six monthly for two years, then annually
Vitamin D Six monthly for two years, then annually
INR Six monthly for two years, then annually
Vitamin A Annually
Vitamin E Annually
Zinc Annually
Copper Annually
Selenium Annually
Cambridge University Hospitals NHS Foundation Trust Page 1 of 8
Micronutrient supplementation and monitoring after total and subtotal gastrectomy
Version 1; Approved July 2018
Digestive diseases
Division A
1 Scope
Departmental – pertinent to oesophago-gastric surgery and gastroenterology.
2 Purpose
To provide guidelines for micronutrient supplementation and monitoring in the
gastrectomy population to facilitate prevention and early detection of
micronutrient deficiency.
These guidelines are not intended to be used in the bariatric surgery population.
3 Definitions
Gastrectomy – total or subtotal gastrectomy with Roux-en-Y reconstruction or
equivalent, not sleeve gastrectomy.
4 Introduction
The long-term metabolic and nutritional consequences of gastrectomy are
unclear, as there have been no good quality long-term studies. This document is
based on guidelines published for the bariatric surgical population, which have
been amended to reflect the different nutritional challenges experienced by the
gastrectomy population1-4. The few long-term studies of micronutrient deficiency
after upper gastrointestinal surgery support this approach5,6.
The clinical presentation of micronutrient deficiency can be subtle, and may
include non-specific visual and neurological symptoms. The presence of
unexplained non-specific symptoms in the post-gastrectomy patient should
instigate prompt biochemical assessment and consideration of referral to a
specialist in nutrition or clinical biochemistry.
A comprehensive set of guidance on the management of long-term symptoms in
this patient group can be accessed at:
http://fg.bmj.com/content/early/2016/10/14/flgastro-2016-100714 7
Within this document, key recommendations are highlighted in bold, above
rationale for the guidance in normal script.
Cambridge University Hospitals NHS Foundation Trust Page 2 of 8
Micronutrient supplementation and monitoring after total and subtotal gastrectomy
Version 1; Approved July 2018
Digestive diseases
Division A
This document is intended to guide the hospital team and general practitioner
caring for a patient who has undergone total or partial gastrectomy. Within the
prophylactic total gastrectomy group, this includes patients undergoing surgery
in their 20s, who may manifest micronutrient deficiencies years or decades later.
All patients should have testing as below every six months for the first two years
post-surgery, then annually thereafter. Micronutrient deficiencies can still occur
many years after the index surgery, although the interval of testing may be
extended if the patient has experienced many years of stable results (albeit with
a low threshold for a full micronutrient assessment in the presence of any
symptoms). Replacement of micronutrient deficiencies in this population can be
challenging, and carry its own risks, and consideration should be given to
seeking specialist support from local nutrition services and/or the specialist
dietitians within the Cambridge Oesophago-Gastric Centre.
It is worth noting that some drug formulations, particularly enteric coated tablets,
are poorly absorbed in this population, as there is no reservoir in which the
tablets can be dissolved, and intestinal transit is rapid.
All supplements can be purchased over the counter from a pharmacy or
supermarket.
5 Responsibilities
This document has been produced with input from the departments of surgery
(Mr Geoffrey Roberts, Mr Richard Hardwick), Gastroenterology (Dr Dunecan
Massey, Professor Rebecca Fitzgerald), Clinical Biochemistry (Dr Claire Meek,
Professor Fiona Gribble) and Dietetics (Miss Nicola Sunderland, Mrs Sam
Grimes).
It has been externally peer reviewed by Dr J Andreyev, Consultant
Gastroenterologist, The Royal Marsden Hospital.
It has been reviewed by the oesophago-gastric cancer specialist MDT.
6 Guidance
6.1 Routine supplements in the post-gastrectomy patient
All patients after gastrectomy are recommended to receive a daily multivitamin
and mineral tablet (including Vitamin B complex), and at least three monthly
vitamin B12 intramuscular injection regardless of nutritional state. Simple
multivitamin tablets without minerals are insufficient. Over the counter A-Z
multivitamin and mineral supplements are normally adequate.
Cambridge University Hospitals NHS Foundation Trust Page 3 of 8
Micronutrient supplementation and monitoring after total and subtotal gastrectomy
Version 1; Approved July 2018
Digestive diseases
Division A
6.2 Persistent malabsorption and diarrhoea
Patients with persisting malabsorption may have another underlying cause and
we recommend a low threshold for screening for pancreatic exocrine
insufficiency, coeliac disease, bile acid malabsorption and small intestinal
bacterial overgrowth in refractory cases of micro or macro-nutrient deficiency.
Steatorrhoea may be underdiagnosed in the post-gastrectomy group, and result
in multiple, refractory, vitamin and mineral deficiencies. The primary causes are
pancreatic exocrine insufficiency, bile acid malabsorption and small intestinal
bacterial overgrowth. We recommend that patients with steatorrhoea be
investigated with faecal elastase and hydrogen/ methane breath tests and, if
these are negative, a SeHCAT scan.
6.3 General biochemistry
Annual creatinine, urea, electrolytes (including magnesium) and liver
function tests should be performed.
Patients are at risk of dehydration and protein energy malnutrition. Unfortunately
there is no single biochemical test which can give an indication of global
nutritional status. All biochemical measurements need to be interpreted in the
light of clinical factors, including the patient’s weight, any recent weight change
and the presence of any inflammatory or infective processes, which will increase
nutritional requirements.
Albumin can be regarded as a (poor) surrogate marker of chronic malnutrition in
the absence of acute illness (ie when the C-reactive protein and white cell count
are both normal).
6.4 Anaemia
To identify and prevent anaemia, annual testing for Full Blood Count,
ferritin, transferrin saturation, B12 (pre-injection) and folate should be
performed. All pregnancies in this patient group should be regarded as at
higher risk for neural tube defect and the mother should be treated with
high dose folate commencing prior to pregnancy.
Absorption of iron, folate and B12 is significantly impaired after gastrectomy8.
Many patients may have anaemia due to a deficiency of more than one nutrient.
Regardless of the mean corpuscular volume, all patients presenting with
anaemia should have a full assessment of haematinics, vitamin B12 and folate,
with supplementation as indicated. Oral iron replacement should be with
chewable or soluble tablets (patient must purchase from outside pharmacy), or
syrup, as non-dissolvable forms can pass intact through the entire intestinal
tract9.
Cambridge University Hospitals NHS Foundation Trust Page 4 of 8
Micronutrient supplementation and monitoring after total and subtotal gastrectomy
Version 1; Approved July 2018
Digestive diseases
Division A
The high risk of folate malabsorption after gastrectomy means that all women
considering pregnancy should be treated as at risk of a neural tube defect, and
treated accordingly with high dose folate10.
Women should be encouraged to have planned pregnancies with a pre-
pregnancy nutritional assessment. It should also be noted that some multivitamin
preparations contain high levels of vitamin A and may be inappropriate in the
pre-conception and pregnant period.
6.5 Bone density
All patients should have annual testing for calcium and vitamin D.
It is possible that patients are at risk of osteoporosis due to impaired absorption
of calcium and vitamin D after gastrectomy. Limited studies indicated the risk
may be as high as 71% in the post-menopausal female population11-16. This is
an area of clinical uncertainty and will benefit from further research.
There is at present insufficient evidence to support routine DXA screening for
osteoporosis in this patient group, however this may change in the future. We
recommend a low threshold for DXA scanning in this population, and
opportunistic screening should be considered in all post-gastrectomy patients
over the age of 50 or post-menopause (whichever comes earlier).
6.6 Fat soluble vitamins
All patients should have annual testing for vitamins A, E and D, and an INR
check which provides an assessment of the adequacy of vitamin K stores.
The degree and severity of fat malabsorption in patients after a gastrectomy is
unclear, although recent literature suggests it is a notable risk and carries the
added complication of fat soluble vitamin malabsorption 17.
Patients with deficiencies should be given supplementation and appropriate
dietary advice. A low threshold for interval testing should be applied if the patient
has steatorrhea or non-specific visual or neurological symptoms.
6.7 Vitamin C
Testing for possible vitamin C deficiency should be performed after
consultation with a clinical biochemist.
The incidence of vitamin C deficiency in bariatric surgery patients is up to 34%18
and vitamin C malabsorption is possible in the post-gastrectomy group. Early
diagnosis and treatment of deficiency may prevent clinical manifestations,
however accurate measurement is challenging and requires specialist input.
Routine testing is not recommended.
Cambridge University Hospitals NHS Foundation Trust Page 5 of 8
Micronutrient supplementation and monitoring after total and subtotal gastrectomy
Version 1; Approved July 2018
Digestive diseases
Division A
6.8 Zinc and copper
All patients should have annual testing for zinc and copper levels and
supplementation, if necessary, should be at a ratio of 8-15mg of zinc to
1mg of copper. Supplementation of zinc or copper without the other must
be avoided.
Zinc and copper are primarily absorbed in the proximal small intestine, which is
partly bypassed after a gastrectomy19. Deficiency of either should be considered
in the post gastrectomy population. Zinc and copper compete for the same
transporter for absorption from the intestine into the blood, and excessive zinc
consumption, for example during supplementation, can precipitate copper
deficiency. Copper deficiency presents insidiously but can cause neurological
abnormalities, gait disturbance and anaemia. Absorption of supplemented zinc
and copper may be poor.
6.9 Selenium
All patients should have selenium levels checked annually.
There is no evidence to support routine testing for selenium levels in the
absence of chronic diarrhoea or other evidence of malabsorption 20. However, the
absence of long-term data in the gastrectomy cohort limits our
recommendations, and unpublished data suggest a not inconsiderable incidence
of selenium deficiency in the post-gastrectomy population.
6.10 Thiamine
There is no evidence for routine testing for thiamine levels, however if a patient
suffers significant weight loss or has symptoms suggestive of Wernicke/
Korsakoff syndrome they should be promptly admitted to hospital for IV thiamine
replacement.
7 Monitoring compliance with and the effectiveness of this
document
These are guidelines, representing best available evidence, and are intended to
guide both local practice and support GPs following up patients who have
undergone gastrectomy. It is envisaged that these guidelines will be circulated to
GPs at the point of discharge of patients from routine outpatient follow up, and it
will therefore not be possible to formally assess compliance in all patients, given
our national catchment area for prophylactic gastrectomy.
For local patients, compliance will be assessed by internal audit on a two-yearly
basis, responsibility resting with the oesophago-gastric MDT.
Cambridge University Hospitals NHS Foundation Trust Page 6 of 8
Micronutrient supplementation and monitoring after total and subtotal gastrectomy
Version 1; Approved July 2018
Digestive diseases
Division A
8 References
1. Tack J, Deloose E. Complications of bariatric surgery: dumping syndrome, reflux
and vitamin deficiencies. Best practice & research Clinical gastroenterology.
2014;28(4):741-749.
2. Mechanick JI, Youdim A, Jones DB, et al. Clinical practice guidelines for the
perioperative nutritional, metabolic, and nonsurgical support of the bariatric
surgery patient--2013 update: cosponsored by American Association of Clinical
Endocrinologists, the Obesity Society, and American Society for Metabolic &
Bariatric Surgery. Surg Obes Relat Dis. 2013;9(2):159-191.
3. O’Kane M PJ, Aasheim E, Barth J, Batterham R, Welbourn R. Guidelines on
perioperative and postoperative biochemical monitoring and micronutrient
replacement for patients undergoing bariatric surgery. 2014;
http://www.bomss.org.uk/bomss-nutritional-guidance/, 2016.
4. van der Post RS, Vogelaar IP, Carneiro F, et al. Hereditary diffuse gastric cancer:
updated clinical guidelines with an emphasis on germline CDH1 mutation
carriers. J Med Genet. 2015;52(6):361-374.
5. Stael von Holstein C, Ibrahimbegovic E, Walther B, Akesson B. Nutrient intake
and biochemical markers of nutritional status during long-term follow-up after
total and partial gastrectomy. European journal of clinical nutrition.
1992;46(4):265-272.
6. Walther B, Clementsson C, Vallgren S, Ihse I, Akesson B. Fat malabsorption in
patients before and after total gastrectomy, studied by the triolein breath test.
Scandinavian Journal of Gastroenterology. 1989;24(3):309-314.
7. Andreyev HJ, Davidson SE, Gillespie C, Allum WH, Swarbrick E. Practice
guidance on the management of acute and chronic gastrointestinal problems
arising as a result of treatment for cancer. Gut. 2012;61(2):179-192.
8. Jun JH, Yoo JE, Lee JA, et al. Anemia after gastrectomy in long-term survivors of
gastric cancer: A retrospective cohort study. International journal of surgery.
2016;28:162-168.
9. Langdon DE. Liquid and chewable iron in post-gastrectomy anaemia. Alimentary
pharmacology & therapeutics. 1999;13(4):567.
10. Kaurah P, Fitzgerald R, Dwerryhouse S, Huntsman DG. Pregnancy after
prophylactic total gastrectomy. Familial cancer. 2010;9(3):331-334.
11. Krupski W, Tatara MR, Bury P, et al. Negative Effects of Total Gastrectomy on
Bone Tissue Metabolism and Volumetric Bone Mineral Density (vBMD) of
Lumbar Spine in 1-Year Study in Men. Medicine. 2016;95(7):e2817.
12. Lim JS, Kim SB, Bang HY, Cheon GJ, Lee JI. High prevalence of osteoporosis in
patients with gastric adenocarcinoma following gastrectomy. World journal of
gastroenterology : WJG. 2007;13(48):6492-6497.
13. Adachi Y, Shiota E, Matsumata T, Iso Y, Yoh R, Kitano S. Osteoporosis after
gastrectomy: bone mineral density of lumbar spine assessed by dual-energy X-
ray absorptiometry. Calcif Tissue Int. 2000;66(2):119-122.
Cambridge University Hospitals NHS Foundation Trust Page 7 of 8
Micronutrient supplementation and monitoring after total and subtotal gastrectomy
Version 1; Approved July 2018
Digestive diseases
Division A
14. Liedman B, Bosaeus I, Mellstrom D, Lundell L. Osteoporosis after total
gastrectomy. Results of a prospective, clinical study. Scand J Gastroenterol.
1997;32(11):1090-1095.
15. Mellstrom D, Johansson C, Johnell O, et al. Osteoporosis, metabolic aberrations,
and increased risk for vertebral fractures after partial gastrectomy. Calcified
tissue international. 1993;53(6):370-377.
16. Tovey FI, Godfrey JE, Lewin MR. A gastrectomy population: 25-30 years on.
Postgraduate Medical Journal. 1990;66(776):450-456.
17. Heneghan HM, Zaborowski A, Fanning M, et al. Prospective Study of
Malabsorption and Malnutrition After Esophageal and Gastric Cancer Surgery.
Ann Surg. 2015;262(5):803-807; discussion 807-808.
18. Clements RH, Katasani VG, Palepu R, et al. Incidence of vitamin deficiency after
laparoscopic Roux-en-Y gastric bypass in a university hospital setting. The
American surgeon. 2006;72(12):1196-1202; discussion 1203-1194.
19. Lee HH, Prasad AS, Brewer GJ, Owyang C. Zinc absorption in human small
intestine. The American journal of physiology. 1989;256(1 Pt 1):G87-91.
20. Papamargaritis D, Aasheim ET, Sampson B, le Roux CW. Copper, selenium and
zinc levels after bariatric surgery in patients recommended to take multivitamin-
mineral supplementation. Journal of trace elements in medicine and biology :
organ of the Society for Minerals and Trace Elements (GMS). 2015;31:167-172.
Equality and diversity statement
This document complies with the Cambridge University Hospitals NHS
Foundation Trust service equality and diversity statement.
Disclaimer
It is your responsibility to check against the electronic library that this printed out
copy is the most recent issue of this document.
Document management
Approval: James Wheeler (CD Gen Surgery)- 25 May 2018
JDTC approval: 17 July 2018
Owning department: Digestive diseases
Author(s): Geoffrey Roberts
Pharmacist: Emma Williams
File name: Gastrectomy micronutrients Version1 July 2018.doc
Supersedes: n/a (new document)
Version number: 1 Review date: July 2021
Local reference: Document ID: 100825
Cambridge University Hospitals NHS Foundation Trust Page 8 of 8
Micronutrient supplementation and monitoring after total and subtotal gastrectomy
Version 1; Approved July 2018
You might also like
- Use of Peptide Growth Factors For Adult Patients With Intestinal Failure2018Document12 pagesUse of Peptide Growth Factors For Adult Patients With Intestinal Failure2018Ramez AntakiaNo ratings yet
- Nutritional Support in Gastrointestinal DiseaseDocument8 pagesNutritional Support in Gastrointestinal DiseaseDoinitsa RogacNo ratings yet
- Rare but Devastating Micronutrient Deficiencies in RYGB PatientsDocument10 pagesRare but Devastating Micronutrient Deficiencies in RYGB PatientsYazen JoudehNo ratings yet
- Referat NutrisiDocument24 pagesReferat NutrisiYulisa Prahasti Dewa AyuNo ratings yet
- Bariatric Surgery: Postoperative Nutritional Management - UpToDateDocument32 pagesBariatric Surgery: Postoperative Nutritional Management - UpToDateKaren Jbo100% (1)
- Nutrition in ICU: DR Rahul VarshenyDocument50 pagesNutrition in ICU: DR Rahul VarshenyAntar InenigogNo ratings yet
- Office: of The SecretaryDocument10 pagesOffice: of The SecretaryJoseph TrinidadNo ratings yet
- 6.nutrition in The Surgical PatientDocument56 pages6.nutrition in The Surgical Patientoliyad alemayehuNo ratings yet
- Medical Nutrition Therapy For The Critically IllDocument11 pagesMedical Nutrition Therapy For The Critically IllPutri DeskantariNo ratings yet
- Nutricion GastrectomiaDocument12 pagesNutricion GastrectomiaMaría Isabel Escobar EscalonaNo ratings yet
- Moore Et Al-2018-Clinical Liver DiseaseDocument4 pagesMoore Et Al-2018-Clinical Liver DiseaseCarlos Francisco Enciso MartinezNo ratings yet
- For The Surgical Patient: Kelly Sparks LDN, RDDocument47 pagesFor The Surgical Patient: Kelly Sparks LDN, RDManikandaprabhu sivaNo ratings yet
- Guidelines Pre-Op and Pos-OpDocument23 pagesGuidelines Pre-Op and Pos-OpDavid EsmanhottoNo ratings yet
- Colleen Major Case Study - WebsiteDocument23 pagesColleen Major Case Study - Websiteapi-249707182No ratings yet
- Micronutrieint Loss ObeseDocument10 pagesMicronutrieint Loss ObeseYazen JoudehNo ratings yet
- PN-Guidelines Nassaur UniversityDocument17 pagesPN-Guidelines Nassaur Universitygshdhdjsjjd hdhdhdhdjdNo ratings yet
- Review: Berkeley N Limketkai, Wendi Lebrett, Lisa Lin, Neha D ShahDocument10 pagesReview: Berkeley N Limketkai, Wendi Lebrett, Lisa Lin, Neha D ShahAdiel OjedaNo ratings yet
- Obesity Medicine: Irina A. Lapik, Alexey V. Galchenko, Kamilat M. Gapparova TDocument9 pagesObesity Medicine: Irina A. Lapik, Alexey V. Galchenko, Kamilat M. Gapparova TMakbule ERÇAKIRNo ratings yet
- Parenteralnutrition: Indications, Access, and ComplicationsDocument21 pagesParenteralnutrition: Indications, Access, and ComplicationsJair Alexander Quintero PanucoNo ratings yet
- Miscelaneas: Nutritional Considerations During Critical IllnessDocument4 pagesMiscelaneas: Nutritional Considerations During Critical IllnessandreigustvNo ratings yet
- Dietary Interventions in Gastrointestinal Diseases: Foods, Nutrients, and Dietary SupplementsFrom EverandDietary Interventions in Gastrointestinal Diseases: Foods, Nutrients, and Dietary SupplementsNo ratings yet
- Nutritional Pyramid For Post-Gastric Bypass Patients: Current StatusDocument9 pagesNutritional Pyramid For Post-Gastric Bypass Patients: Current StatusvcaguiarNo ratings yet
- Nutritional Intervention in Chronic Kidney Disease: EditorialDocument2 pagesNutritional Intervention in Chronic Kidney Disease: EditorialDaniel DarmawanNo ratings yet
- Overview of Perioperative Nutrition Support - UpToDateDocument20 pagesOverview of Perioperative Nutrition Support - UpToDateduong tien truongNo ratings yet
- IDPN BENEFITS FOR HD PATIENTSDocument7 pagesIDPN BENEFITS FOR HD PATIENTSCarlos Miguel Mendoza LlamocaNo ratings yet
- 1-What Is Nutritional Assessment A Quick Guide For Critical CareDocument5 pages1-What Is Nutritional Assessment A Quick Guide For Critical CaredemetceritNo ratings yet
- 2021 Diabetes Clinical Practice GuidelineDocument15 pages2021 Diabetes Clinical Practice GuidelineAbdulfetah AhmedNo ratings yet
- Gastrectomy NutritionDocument10 pagesGastrectomy NutritionBalasubramanian NatarajanNo ratings yet
- Sbs Damini MamDocument12 pagesSbs Damini MamDhamu ShanthiNo ratings yet
- MadsenArticle July 06Document16 pagesMadsenArticle July 06Kouba MarciminiNo ratings yet
- Nutrition Support in Critically Ill Patients - Parenteral NutritionDocument7 pagesNutrition Support in Critically Ill Patients - Parenteral Nutritionrazieh.shekariNo ratings yet
- B 12Document11 pagesB 12Vijay MgNo ratings yet
- JMedNutrNutraceut2277-5417572 150255Document7 pagesJMedNutrNutraceut2277-5417572 150255jufranNo ratings yet
- Michael Kaminski-Case 5Document7 pagesMichael Kaminski-Case 5api-302058832No ratings yet
- Nutritional Status in Peritoneal Dialysis Nutritional Guidelines, Adequacy and the Management of MalnutritionDocument14 pagesNutritional Status in Peritoneal Dialysis Nutritional Guidelines, Adequacy and the Management of MalnutritionrocastelviNo ratings yet
- Nutrition in The Critically Ill PatientDocument13 pagesNutrition in The Critically Ill PatientnainazahraNo ratings yet
- Nutrition in Gastrointestinal Cancer Patient: Intensive Care Unit RSPAD Gatot Soebroto 2021Document16 pagesNutrition in Gastrointestinal Cancer Patient: Intensive Care Unit RSPAD Gatot Soebroto 2021Muhammad Baihaqi SiddiqNo ratings yet
- Nutritional Support in Intensive Care Unit (ICU) Patients: More Than Choosing The Route: Enteral and Parenteral NutritionDocument3 pagesNutritional Support in Intensive Care Unit (ICU) Patients: More Than Choosing The Route: Enteral and Parenteral NutritionZoraide OrtegamNo ratings yet
- Vegan Patients Eating Disorders Mar19Document5 pagesVegan Patients Eating Disorders Mar19gipanef547No ratings yet
- New Microsoft Office PowerPoint PresentationDocument27 pagesNew Microsoft Office PowerPoint PresentationDr-Iyad AljuaidiNo ratings yet
- Nutricion PerioperatoriaDocument11 pagesNutricion PerioperatoriaAndres Neira QuezadaNo ratings yet
- MFN-005 Unit-4 PDFDocument17 pagesMFN-005 Unit-4 PDFShubhendu ChattopadhyayNo ratings yet
- ESPEN Guidelines On Enteral Nutrition: PancreasDocument10 pagesESPEN Guidelines On Enteral Nutrition: PancreasAdiel OjedaNo ratings yet
- 10 Diet and Nutrition For Liver Disease and HepatitisDocument71 pages10 Diet and Nutrition For Liver Disease and HepatitisMubark Al AwlaqyNo ratings yet
- Liver JournalDocument29 pagesLiver Journalrenitha ratuNo ratings yet
- PIIS2405457716301917Document2 pagesPIIS2405457716301917Abbas AmirNo ratings yet
- Bab IDocument24 pagesBab Iyoga zunandy pratamaNo ratings yet
- Nutrition and Bariatric SurgeryFrom EverandNutrition and Bariatric SurgeryJaime Ruiz-TovarNo ratings yet
- Clinical Study: Nutritional Status Assessment in Cirrhotic Patients After Protein SupplementationDocument5 pagesClinical Study: Nutritional Status Assessment in Cirrhotic Patients After Protein SupplementationNimas Mita EtikaNo ratings yet
- Alternative E-Reserves Renal Disease SIM Case StudyDocument11 pagesAlternative E-Reserves Renal Disease SIM Case Studyapi-490571442No ratings yet
- 2024_tracto_digestivo_bajoDocument36 pages2024_tracto_digestivo_bajosulbey878No ratings yet
- Renal Nutrition Management Protocol 2015 PDFDocument27 pagesRenal Nutrition Management Protocol 2015 PDFShefali RawatNo ratings yet
- Nutritional Pathophysiology of Obesity and its Comorbidities: A Case-Study ApproachFrom EverandNutritional Pathophysiology of Obesity and its Comorbidities: A Case-Study ApproachNo ratings yet
- Guide enteral feeding hospital patientsDocument12 pagesGuide enteral feeding hospital patientsKoushik Sharma AmancharlaNo ratings yet
- Nutritional Management of Acute Kidney InjuryDocument7 pagesNutritional Management of Acute Kidney Injuryrahmanrais91No ratings yet
- Int Failure in Children 11.16Document8 pagesInt Failure in Children 11.16Sandya PallapotuNo ratings yet
- Parenteral NutritionDocument10 pagesParenteral NutritionCandice LavigneNo ratings yet
- MNT Cancer - 12 NovDocument63 pagesMNT Cancer - 12 Novs59865No ratings yet
- Vitamina B12Document5 pagesVitamina B12luisNo ratings yet
- LLL ESPEN Nutrisi Perioperatif Modul 2 PDFDocument12 pagesLLL ESPEN Nutrisi Perioperatif Modul 2 PDFKevin AdrianNo ratings yet
- Professional CV Rasha Abu BakerDocument4 pagesProfessional CV Rasha Abu BakerHamed NazariNo ratings yet
- Krok M Nursing: Test Items For Licensing ExaminationDocument20 pagesKrok M Nursing: Test Items For Licensing Examinationhasan ahmdNo ratings yet
- Hepatitis C and D: A Guide to Transmission, Pathogenesis, Diagnosis and TreatmentDocument78 pagesHepatitis C and D: A Guide to Transmission, Pathogenesis, Diagnosis and TreatmentWara RizkyNo ratings yet
- MEASLES PresentationDocument29 pagesMEASLES PresentationMobin Ur Rehman Khan100% (3)
- Think Right Now! - I Am Healed NowDocument3 pagesThink Right Now! - I Am Healed NowvaltroduoNo ratings yet
- Activity IntoleranceDocument2 pagesActivity Intolerancejunex123No ratings yet
- EPISTAXIS: CAUSES AND MANAGEMENTDocument21 pagesEPISTAXIS: CAUSES AND MANAGEMENTasssadulllahNo ratings yet
- Poor Diet, Lack of Sunshine Linked to Rising DepressionDocument7 pagesPoor Diet, Lack of Sunshine Linked to Rising DepressionAndri Ferdian100% (1)
- Estimation of Sterols in Edible Fats and Oils (Sabir Et Al., 2003)Document4 pagesEstimation of Sterols in Edible Fats and Oils (Sabir Et Al., 2003)Pankaj ParmarNo ratings yet
- Peads HistoryDocument2 pagesPeads Historyapi-349464568No ratings yet
- Plasma ProteinDocument57 pagesPlasma ProteinadulNo ratings yet
- Gestational DiabetesDocument3 pagesGestational DiabetesCortex Pluss0% (1)
- Neomune PelniDocument57 pagesNeomune PelniSutiyono TyoNo ratings yet
- Health Declaration (Triage) Form: (A) Covid-19 (B) Mers Cov and (C) Ebola Virus Disease (Evd)Document1 pageHealth Declaration (Triage) Form: (A) Covid-19 (B) Mers Cov and (C) Ebola Virus Disease (Evd)Nakul Singh ParkwayIndiaNo ratings yet
- TB Screening FormDocument1 pageTB Screening FormBrianKoNo ratings yet
- VancoDocument2 pagesVancoDr. Usman HashmiNo ratings yet
- Genograms: Practical Tools PhysiciansDocument6 pagesGenograms: Practical Tools PhysiciansThariq Mubaraq DrcNo ratings yet
- Exam Question Bi Form2Document11 pagesExam Question Bi Form2Princess DyanaNo ratings yet
- Langerhans Cell Histiocytosis (LCH) : Guidelines For Diagnosis, Clinical Work-Up, and Treatment For Patients Till The Age of 18 YearsDocument10 pagesLangerhans Cell Histiocytosis (LCH) : Guidelines For Diagnosis, Clinical Work-Up, and Treatment For Patients Till The Age of 18 Yearsadrian Morales PeraltaNo ratings yet
- Elderly Care Services & Options in 40 CharactersDocument37 pagesElderly Care Services & Options in 40 CharactersSilvestri Purba100% (2)
- OtoscopeDocument3 pagesOtoscopeVpjunaib JunaibNo ratings yet
- Non-Motor Symptoms in Atypical Parkinsonian SyndromesDocument21 pagesNon-Motor Symptoms in Atypical Parkinsonian Syndromesנועה פרץNo ratings yet
- Protocol Final 2014 Last PDFDocument222 pagesProtocol Final 2014 Last PDFAbdelrahman MamdouhNo ratings yet
- Me So TheraphyDocument92 pagesMe So TheraphyRembulan RamadhantyNo ratings yet
- Philhealth Lost P154B To Overpayments, Fraud: Jovic Yee @jovicyeeinqDocument4 pagesPhilhealth Lost P154B To Overpayments, Fraud: Jovic Yee @jovicyeeinqSheila Mae AramanNo ratings yet
- 2021ITE Answers-2Document80 pages2021ITE Answers-2إكرام النايبNo ratings yet
- CRP 17Document5 pagesCRP 17Eka Satria AnanditaNo ratings yet
- Moll FlandersDocument5 pagesMoll FlandersMónika FülöpNo ratings yet
- Assessment of NewbornDocument26 pagesAssessment of Newbornaybee_14No ratings yet
- Can Meditation Be A Remedy For Psychosomatic Disorder?Document5 pagesCan Meditation Be A Remedy For Psychosomatic Disorder?IJELS Research JournalNo ratings yet