Professional Documents
Culture Documents
Prevalence of Urinary Incontinence in Women With Osteoporosis
Prevalence of Urinary Incontinence in Women With Osteoporosis
Uploaded by
HamzaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Prevalence of Urinary Incontinence in Women With Osteoporosis
Prevalence of Urinary Incontinence in Women With Osteoporosis
Uploaded by
HamzaCopyright:
Available Formats
WOMEN'S HEALTH
WOMEN'S HEALTH
Prevalence of Urinary Incontinence in Women
With Osteoporosis
Meena M. Sran, PT, PhD
BC Women’s Hospital and Health Centre, Osteoporosis Program, Vancouver BC
Simon Fraser University, Injury Prevention and Mobility Laboratory, Burnaby BC
Abstract Résultats : Soixante-sept pour cent des patientes (277/412) ont
signalé certains symptômes d’incontinence urinaire, 23 % n’ont
Objective: To investigate the prevalence and frequency of urinary signalé aucun symptôme et 10 % ont signalé une impériosité sans
incontinence in women presenting to a specialist osteoporosis fuites. Parmi les patientes qui ont signalé une certaine
clinic. incontinence urinaire, 51 % ont signalé des symptômes
Methods: Participants included 412 female patients aged 22 to d’incontinence à l’effort, d’impériosité et d’incontinence par
94 years (mean 62 years) presenting to a hospital-based specialist impériosité. Près de 40 % de toutes les patientes (163/412) et de
multidisciplinary osteoporosis clinic over one year. The presence 59 % de celles qui présentaient une quelconque incontinence
or absence of urinary incontinence, urgency without leakage, type urinaire (163/277) ont signalé au moins une fuite par semaine.
of symptoms (stress, urge, mixed) and frequency of urinary Conclusion : La prévalence de l’incontinence urinaire au moins
incontinence were recorded. hebdomadaire au sein de cette population est beaucoup plus
Results: Sixty-seven percent of patients (277/412) reported some élevée que ce qui a été signalé par les études menées auprès
symptoms of urinary incontinence, 23% reported no symptoms d’autres populations de femmes âgées. Nous constatons
and 10% reported urgency without any leakage. Of those who également une forte prévalence d’incontinence accompagnée
reported some urinary incontinence, 51% reported symptoms of d’impériosité chez les femmes qui présentent une ostéoporose.
stress incontinence, urgency, and urge incontinence. Almost 40% En fonction de ces résultats et puisque l’incontinence urinaire peut
of all patients (163/412) and 59% of those with any urinary limiter la capacité d’une femme à être physiquement active et
incontinence (163/277) reported leakage at least once per week. accroître le risque de chute et de fracture, le dépistage de
l’incontinence devrait systématiquement faire partie de la prise en
Conclusion: The prevalence of at least weekly urinary incontinence
charge de l’ostéoporose. Les cliniciens qui offrent leurs services à
in this population is much higher than that reported in studies of
des patientes présentant une ostéoporose devraient envisager la
other older adult female populations. There is also a high
présence d’une incontinence au moment de prescrire un
prevalence of incontinence accompanied by urgency in women
programme d’exercice visant la santé osseuse et la prévention
with osteoporosis. Based on these results and because urinary
des chutes.
incontinence can limit a woman’s ability to be physically active and
increase the risk of falls and fractures, screening for incontinence J Obstet Gynaecol Can 2009;31(5):434–439
should be a routine part of osteoporosis management. Clinicians
seeing patients for osteoporosis should consider the presence of INTRODUCTION
incontinence when prescribing exercise for bone health and fall
rinary incontinence (UI) is the second leading reason
prevention.
Résumé U for admission to long-term care1 and a top health pri-
ority for older women.2 The prevalence of UI increases with
Objectif : Explorer la prévalence et la fréquence de l’incontinence
urinaire chez les femmes qui se présentent à une clinique age.3–5 Reported prevalence for weekly UI in older adult
spécialisée en ostéoporose. women ranges from 21% to 28%3,5–7 and the economic cost
Méthodes : Les participantes consistaient en 412 patientes dont of UI in the United States is 16 billion dollars per year.8 Yet
l’âge se situait entre 22 et 94 ans (âge moyen : 62 ans) qui se
sont présentées à une clinique multidisciplinaire (en milieu only 25% of all women with UI seek help.9,10
hospitalier) spécialisée en ostéoporose sur une période d’un an.
La présence ou l’absence d’incontinence urinaire, l’impériosité Osteoporosis is also common in older adult women11 and
sans fuites, le type de symptômes (à l’effort, par impériosité, incurs high costs.12–14 Physical activity is an important part
mixte) et la fréquence de l’incontinence urinaire ont été consignés. of osteoporosis treatment aimed at maintaining bone
mass15 and reducing falls16–20 and should be prescribed for
all patients with osteopenia or osteoporosis. However, UI
Key Words: Osteoporosis, urinary incontinence, prevalence, can significantly limit a woman’s ability to be physically
female, epidemiology
active21 and is an independent risk factor for falls and low
Competing Interests: None declared. trauma fractures in older women.22,23 The presence of UI
Received on October 3, 2008 may dramatically influence exercise prescription and com-
Accepted on February 2, 2009 pliance with exercise in women with osteoporosis, yet it is
434 l MAY JOGC MAI 2009
Prevalence of Urinary Incontinence in Women With Osteoporosis
not routine for physicians24 or other health care profession-
Table 1. Prevalence of UI
als to ask about incontinence, and it is typically only after
symptoms have been present for 6–10 years that women Presence/absence of UI n % of all patients
mention UI to a health care professional.25 The prevalence Any urinary incontinence 277/412 67.2
of UI in women with osteoporosis or osteopenia is not No urinary incontinence 91/412 22.8
known, nor is the prevalence in women presenting to an Urgency only, no leakage 41/412 9.9
osteoporosis clinic. Knowing whether UI is prevalent in
this population may help health care professionals “treat the
whole person,” and result in more woman-centred care. If
UI is prevalent in this population, then clinicians treating Table 2. Frequency of UI
individuals with osteoporosis may need to change their
% of all % of patients
practice to include routine screening for UI and referral for Frequency of UI n patients with UI
treatment, and to consider UI when prescribing exercise for
Once per day or more 69 16.5 24.5
bone health.
Twice in 3 days 41 9.9 14.8
For these reasons, this study was undertaken to investigate Once per week 54 13.1 19.5
the prevalence and frequency of urinary incontinence in Once per month 40 9.7 14.4
women presenting to a specialist osteoporosis clinic. Specif- < Once per month 73 17.7 26.3
ically, a self-administered questionnaire followed by
interview was used to assess (1) the presence or absence of
urinary incontinence, (2) the type of symptoms (stress, urge, by a physiotherapist at the end of the study period. The
mixed) and (3) the frequency of incontinence episodes, in most appropriate answer (once per week, twice in three
all new female patients presenting to the clinic over one days, once per day, once per month, or less than once per
year. month) was recorded on a standardized form. These ques-
METHODS tions are similar to those used in previous epidemiologic
studies3,4,6,26 and have been found to have good specificity,27
Data were collected in a multidisciplinary osteoporosis and accuracy similar to other, longer questionnaires.28
clinic over a one-year period (June 2007 to May 2008). To
be seen in this clinic, patients must be referred by their fam- Descriptive data were calculated. Data were expressed as
ily physician. In the clinic each new patient routinely the percentage of female patients who reported
receives a consultation with a physiotherapist, dietitian, 1. any UI (responded sometimes or yes, always to
physician and a nurse. questions 1 and/or 3)
Over the one-year period, 447 new patients were seen in the 2. no UI (responded never to questions 1 and/or 3)
clinic, of whom 414 (92.6%) were female. All except two
3. urgency only, without leakage (responded sometimes
female patients were included in this study, and all male
or yes, always to question 2 only)
patients were excluded. One female was excluded because
she was paraplegic and used an indwelling catheter; the Data were also expressed as a percentage of all female
other was excluded because she used a urostomy bag. Thus patients with any UI who reported
data for 412 female patients were included. 4. symptoms of stress UI only (responded sometimes or
Prior to attending the clinic, each patient received a stan- yes, always to question 1 only)
dardized questionnaire that included three questions about 5. symptoms of urge UI only (responded sometimes or
urinary incontinence, and each female patient was asked to yes, always to question 3 only)
complete this. The three questions were: (1) Do you leak
urine when you cough, sneeze, laugh, lift, jump, or run? (2) 6. urgency and symptoms of stress UI (responded
Do you rush to the toilet when you feel an urge? (3) Do you sometimes or yes, always to both questions 1 and 2)
lose urine when you rush to the toilet? Each question 7. urgency and symptoms of urge UI (responded
required one of three answers: (i) yes, always; (ii) sometimes; sometimes or yes, always to both questions 2 and 3)
or (iii) never. If the patient answered sometimes, or yes,
Finally, frequency of UI data were expressed as a percentage
always for question (1) or question (3), then the physiother-
of all female patients and of all those with any UI.
apist asked the patient to report how often they have even a
small amount of leakage. The data from the completed This study was approved by the clinical ethics review board
questionnaires were reviewed and entered on a spreadsheet of BC Women’s Hospital and Health Centre.
MAY JOGC MAI 2009 l 435
WOMEN'S HEALTH
Figure 1. Percentage of patients in each age group: 75 years and over (n = 71), 65–74 years
(n = 89), 55–64 years (n = 152), 45–54 years (n = 80), 35–44 years (n = 14), 22–34 years (n = 6)
Percentage of all patients
Age (years)
RESULTS continued to leak urine involuntarily; four had daily leakage,
The 412 female patients ranged in age from 22 to 94 years one leaked twice in three days, three leaked once per week,
(mean 62 ± 12 years [SD]). More than 75% of patients were one leaked once per month, and one leaked less than once
over 55 years of age (Figure 1). Sixty-seven percent of per month. Six patients reported use of medication (five for
patients (277/412) reported some symptoms of UI, 23% UI and one for overactive bladder), two patients had seen a
reported no symptoms of UI and 10% reported urgency physiotherapist specializing in UI, one was waiting to see a
without any leakage (Table 1). Of the patients who reported physiotherapist, and two reported routinely performing
any UI or urgency without leakage, 75% had osteoporosis pelvic floor muscle exercises.
based on bone mineral densitometry (BMD) or a history of DISCUSSION
a low trauma fracture, while the remaining 25% had
osteopenia based on BMD. In a population of women with osteoporosis or osteopenia
who presented to a specialist osteoporosis clinic, 67%
Of those who reported any UI, 51% (143/277) reported reported one symptom or more of UI, and almost 40%
symptoms of stress UI, urgency, and urge UI (answered reported experiencing UI once per week or more. The prev-
sometimes or yes, always to all three questions). Sixteen per- alence of at least weekly UI in this population of women
cent (45/277) reported symptoms of urgency and urge UI, with osteoporosis or osteopenia is much higher than in pre-
and 14% (39/277) reported symptoms of stress UI only or vious studies of older adult women.3,5–7,29 Wetle et al.7
stress UI and urgency. One patient reported symptoms of reported a 21% prevalence of weekly UI in women aged 65
urge UI alone and 10/277 reported symptoms of both or older; Hannestad et al. reported a 25% prevalence across
stress and urge UI (Figure 2). their whole population, and the prevalence reached 40%
Almost 40% of all patients (163/412) and 59% of those only in individuals over 90 years of age. Jackson et al.29
with any UI (163/277) reported leakage one time per week reported a 21% prevalence of weekly UI in women aged
or more (Table 2). 70–79. Brown et al. assessed women of a mean age very
similar to the current study but with coronary artery disease,
Of these 412 female patients, one frequently had renal cal- and reported a 28% prevalence of weekly UI.
culi, one had multiple sclerosis, one had a history of bladder
cancer, and one had had an ovarian cystectomy 12 years These results therefore suggest that the prevalence of UI in
beforehand. In addition, 11 patients had a history of women presenting to an osteoporosis clinic is much higher
anti-incontinence surgery or surgical procedures for pro- than the previously reported prevalence of UI in older adult
lapse. Of these 11 patients, one had undergone two proce- female populations. How the presence of osteoporosis
dures and another had undergone three. Ten of the 11 might increase the risk of UI is not known, but a previous
436 l MAY JOGC MAI 2009
Prevalence of Urinary Incontinence in Women With Osteoporosis
Figure 2. Type of urinary incontinence (UI) symptom(s) reported by all patients reporting any
UI (n = 277)
Percentage of all patients with any UI
Type of UI symptom(s)
study found self-reported osteoporosis to be associated important for the prevention of both UI and osteoporotic
with disposable pad use (OR 2.01).30 Spinal curvature fractures.
(kyphosis/lordosis) associated with spinal osteoporosis
may also play a role. A previous study found spinal curva- A previous study found physicians who spent 15 minutes
ture was related to pelvic organ prolapse,31 and sitting spinal with each patient and saw fewer patients per week were
posture (slump or upright, with or without support) has more likely to screen for UI.38 In the specialist
been shown to influence resting activity of the pelvic floor multidisciplinary clinic in which this study was conducted,
muscles.32 Further, individuals with osteoporotic spinal each patient spends 45 minutes with a physician and is also
compression fractures may present with impaired pulmo- seen by a physiotherapist and a nurse, all of whom have the
nary function,33 which may in turn influence strength, ability to screen for and recommend appropriate treatment
endurance and/or timing of the pelvic floor muscles. for UI. Although this setting is favourable, practical time
constraints should not obviate screening for UI, and clinics
and practitioners must ensure that UI is addressed, because
The majority of patients with UI also reported rushing to
patients are unlikely to describe UI spontaneously.25 A
the toilet when they felt an urge (81.9%; Figure 2), while a
method of routine screening, such as that used in this study,
further 10% who did not report any UI reported rushing
is recommended. While UI screening is relevant for fall pre-
(Table 1). Brown et al.23 reported that weekly or more fre-
vention and exercise prescription in individuals with osteo-
quent urge incontinence increased the risk of falls and low
porosis, it is also part of providing comprehensive care of
trauma fractures in older women. In addition, falls and UI
women’s health issues. In a large population survey, women
were in the top six disability-related priorities identified in a
identified “being seen as a whole person” as their highest
survey of women’s health priorities, and fall-related injuries
psychosocial health priority. Importantly, women with UI
incur enormous cost to the individual and the health sys-
are more likely to suffer from depression and
tem.34 Further, the ability to maintain balance has been
low-self-esteem than women without UI.39 UI can result in
found to be decreased in women with stress UI, compared
isolation from family and friends,40 and marital relation-
with continent women.35
ships and sexual function are negatively affected in women
with UI.41
The results of this study, specifically the high prevalence of
UI and UI accompanied by urgency in this osteoporosis There is strong evidence for the use of supervised individ-
clinic population, indicate that screening for UI should be a ual pelvic floor muscle training as a primary treatment for
routine part of osteoporosis management. Higher levels of UI in women.9,42–44 Clinical practice guidelines recommend
physical activity are also associated with a reduced risk of conservative management for UI in older women; a ran-
UI.36,37 Thus, enabling women to be more active is domized controlled trial of physiotherapy for UI in women
MAY JOGC MAI 2009 l 437
WOMEN'S HEALTH
with osteoporosis and UI in our centre is currently near surgical treatment options for UI in older adult women,
completion. especially women with osteoporosis. Clinicians who are
Poor recognition of patients who could benefit is prevent- seeing patients for osteoporosis should consider the pres-
ing treatment of this prevalent condition.9,45 Whether or not ence of UI when prescribing exercise for bone health and
an individual will seek treatment for UI appears to be more fall prevention.
strongly linked to whether or not they perceive UI as a ACKNOWLEDGEMENTS
problem46 than to the frequency of UI or the amount of The author is a Canadian Institutes of Health Research and
leakage.47 Patients may believe that UI is a normal part of Michael Smith Foundation for Health Research Postdoc-
aging, and may be unaware of the consequences or recom- toral Fellow.
mended treatment. This places greater importance on the
REFERENCES
need for health care professionals to screen for UI and
advise patients of the evidence and recommendations. Edu- 1. Thom DH, Haan MN, Van Den Eeden SK. Medically recognized urinary
incontinence and risks of hospitalization, nursing home admission and
cation by health care professionals, who may primarily be mortality. Age Ageing 1997;26:367–74.
seeing patients for conditions other than UI, may help 2. Tannenbaum C, Mayo N. Women’s health priorities and perceptions of
patients understand the importance of seeking treatment care: a survey to identify opportunities for improving preventative health
for UI, which has been shown to have a significant negative care delivery for older women. Age Ageing 2003;32:626–35.
effect on overall health.48–52 3. Hannestad YS, Rortveit G, Sandvik H, Hunskaar S. A community-based
epidemiological survey of female urinary incontinence: the Norwegian
The questions asked in this study regarding UI symptoms EPINCONT study. Epidemiology of incontinence in the county of
Nord-Trondelag. J Clin Epidemiol 2000;53:1150–7.
are similar to those used in other epidemiologic stud-
4. Minassian VA, Stewart WF, Wood GC. Urinary incontinence in women:
ies,3,4,6,26 and have been shown to have fair accuracy and variation in prevalence estimates and risk factors. Obstet Gynecol
good specificity,27 but further questions regarding which 2008;111:324–31.
activities were more or less of a problem may yield more 5. Temml C, Haidinger G, Schmidbauer J, Schatzl G, Madersbacher S. Urinary
accurate results regarding the type of incontinence.28 The incontinence in both sexes: prevalence rates and impact on quality of life
and sexual life. Neurourol Urodyn 2000;19:259–71.
questions used were found, in a previous study, to
6. Brown JS, Grady D, Ouslander JG, Herzog AR, Varner RE, Posner SF.
over-report mixed UI that should have been diagnosed as Prevalence of urinary incontinence and associated risk factors in
pure stress UI.27 From the perspective of clinical utility, if postmenopausal women. Heart & Estrogen/Progestin Replacement Study
(HERS) Research Group. Obstet Gynecol 1999;94:66–70.
knowledge of the type of UI (stress, urge, or mixed) will
alter the physician or other health care professional’s refer- 7. Wetle T, Scherr P, Branch LG, Resnick NM, Harris T, Evans D, et al.
Difficulty with holding urine among older persons in a geographically
ral or treatment of the patient’s condition, then it would be defined community: prevalence and correlates. J Am Geriatr Soc
advisable to include more detailed questions regarding the 1995;43:349–55.
type of UI, as classifying the type of UI based on responses 8. Wilson L, Brown JS, Shin GP, Luc KO, Subak LL. Annual direct cost of
urinary incontinence. Obstet Gynecol 2001;98:398–406.
to a questionnaire has shown acceptable accuracy.28 Of
9. Fantl J, Newman D, Colling J, DeLancy JOL, Keeys C, Loughery R, et al.
note, the self-administered questionnaire and follow-up Urinary incontinence in adults: acute and chronic management. Rockville,
interview used in this study were also chosen for their feasi- Maryland: Department of Health and Human Services, Public Health
bility, since the clinic’s protocol includes completion of a Service, Agency for Health Care Policy and Research (Clinical Practice
Guideline, 96–0682);1996.
self-administered questionnaire prior to the patient’s first
10. Samuelsson E, Victor A, Tibblin G. A population study of urinary
visit to the clinic. A validated interviewer-administered tool incontinence and nocturia among women aged 20–59 years. Prevalence,
is recommended for future studies. This study did not well-being and wish for treatment. Acta Obstet Gynecol Scand
investigate the prevalence of known risk factors for UI in a 1997;76:74–80.
population with osteoporosis, and a follow-up study may 11. Hanley DA, Josse RG. Prevention and management of osteoporosis:
provide additional insights. Finally, the frequency of consensus statements from the Scientific Advisory Board of the
urgency alone was not assessed. Future studies might Osteoporosis Society of Canada. 1. Introduction. CMAJ 1996;155:921–3.
include this variable given the potential relevance to the risk 12. Brown JP, Josse RG. 2002 clinical practice guidelines for the diagnosis and
management of osteoporosis in Canada. CMAJ 2002;167:S1–34.
for falls.
13. Goeree ROB, Pettitt DB, Cuddy L, Ferraz M, Adachi J. An assessment of
CONCLUSION the burden of illness due to osteoporosis in Canada. J Soc Obstet Gynaecol
Can 1996;18:15–24.
The prevalence of UI in this osteoporosis clinic population
was much higher than that reported in previous studies of 14. Papadimitropoulos EA, Coyte PC, Josse RG, Greenwood c.e. . Current and
projected rates of hip fracture in Canada. CMAJ 1997;157:1357–63.
older adult women. This suggests a need for important
15. Engelke K, Kemmler W, Lauber D, Beeskow C, Pintag R, Kalender WA.
changes in clinical practice, particularly regarding screening,
Exercise maintains bone density at spine and hip EFOPS: a 3-year
referral, and education regarding the negative effect of UI longitudinal study in early postmenopausal women. Osteoporos Int
on health and evidence-based, effective, non-surgical, and 2006;17:133–42.
438 l MAY JOGC MAI 2009
Prevalence of Urinary Incontinence in Women With Osteoporosis
16. Campbell AJ, Robertson MC, Gardner MM, Norton RN, Buchner DM. Falls 34. Stokes J, Lindsay J. Major causes of death and hospitalization in Canadian
prevention over 2 years: a randomized controlled trial in women 80 years and seniors. Chronic Dis Can 1996;17:63–73.
older. Age Ageing 1999;28:513–8.
35. Smith MD, Coppieters MW, Hodges PW. Is balance different in women with
17. Campbell AJ, Robertson MC, Gardner MM, Norton RN, Tilyard MW, and without stress urinary incontinence? Neurourol Urodyn 2008;27:71–8.
Buchner DM. Randomised controlled trial of a general practice programme of
36. Danforth KN, Shah a.d., Townsend MK, Lifford KL, Curhan GC, Resnick
home based exercise to prevent falls in elderly women. BMJ 1997;315:1065–9.
NM, et al. Physical activity and urinary incontinence among healthy, older
18. Gardner MM, Robertson MC, Campbell AJ. Exercise in preventing falls and women. Obstet Gynecol 2007;109:721–7.
fall related injuries in older people: a review of randomised controlled trials.
Br J Sports Med 2000;34:7–17. 37. Kikuchi A, Niu K, Ikeda Y, Hozawa A, Nakagawa H, Guo H, et al.
Association between physical activity and urinary incontinence in a
19. Robertson MC, Campbell AJ, Gardner MM, Devlin N. Preventing injuries in community-based elderly population aged 70 years and over. Eur Urol
older people by preventing falls: a meta-analysis of individual-level data. J Am 2007;52:868–74.
Geriatr Soc 2002;50:905–11.
38. Bland DR, Dugan E, Cohen SJ, Preisser J, Davis CC, McGann PE, et al. The
20. Robertson MC, Gardner MM, Devlin N, McGee R, Campbell AJ. effects of implementation of the Agency for Health Care Policy and Research
Effectiveness and economic evaluation of a nurse delivered home exercise urinary incontinence guidelines in primary care practices. J Am Geriatr Soc
programme to prevent falls. 2: controlled trial in multiple centres. BMJ 2003;51:979–84.
2001;322:701–4.
39. Heidrich SM, Wells TJ. Effects of urinary incontinence: psychological
21. Nygaard I, Girts T, Fultz NH, Kinchen K, Pohl G, Sternfeld B. Is urinary
well-being and distress in older community-dwelling women. J Gerontol Nurs
incontinence a barrier to exercise in women? Obstet Gynecol
2004;30:47–54.
2005;106:307–14.
40. Miner PB Jr. Economic and personal impact of fecal and urinary
22. Boele van Hensbroek P, van Dijk N, van Breda GF, Scheffer AC, van der
incontinence. Gastroenterology 2004;126:S8–13.
Cammen TJ, Lips P, et al. The CAREFALL Triage instrument identifying risk
factors for recurrent falls in elderly patients. Am J Emerg Med 2009;27:23–36. 41. Yip SK, Chan A, Pang S, Leung P, Tang C, Shek D, et al. The impact of
23. Brown JS, Vittinghoff E, Wyman JF, Stone KL, Nevitt MC, Ensrud KE, et al. urodynamic stress incontinence and detrusor overactivity on marital
Urinary incontinence: does it increase risk for falls and fractures? Study of relationship and sexual function. Am J Obstet Gynecol 2003;188:1244–8.
Osteoporotic Fractures Research Group. J Am Geriatr Soc 2000;48:721–5. 42. Belisle S, Blake J, Basson R, Desindes S, Graves G, Grigoriadis S, et al.
24. Swanson JG, Skelly J, Hutchison B, Kaczorowski J. Urinary incontinence in Canadian consensus conference on menopause, 2006 update. J Obstet
Canada. National survey of family physicians’ knowledge, attitudes, and Gynaecol Can 2006;28:S7-S94.
practices. Can Fam Physician 2002;48:86–92. 43. Hay-Smith EJ, Dumoulin C. Pelvic floor muscle training versus no treatment,
25. Hagglund D, Walker-Engstrom ML, Larsson G, Leppert J. Reasons why or inactive control treatments, for urinary incontinence in women. Cochrane
women with long-term urinary incontinence do not seek professional help: Database Syst Rev 2006:CD005654.
a cross-sectional population-based cohort study. Int Urogynecol J Pelvic 44. Wilson PD, Hay-Smith J, Nygaard I, Wyman J, Yamanishi T, Berghmans B, et
Floor Dysfunct 2003;14:296–304. al. Adult conservative management. In: Abrams P, Cardozo L, Khoury S, eds.
26. Fultz NH, Fisher GG, Jenkins KR. Does urinary incontinence affect Incontinence. 3rd ed. France: Health Public Publication Ltd.;2005:856–1059.
middle-aged and older women’s time use and activity patterns? Obstet 45. Wyman JF, Harkins SW, Fantl JA. Psychosocial impact of urinary
Gynecol 2004;104:1327–34. incontinence in the community-dwelling population. J Am Geriatr Soc
27. Sandvik H, Hunskaar S, Vanvik A, Bratt H, Seim A, Hermstad R. Diagnostic 1990;38:282–8.
classification of female urinary incontinence: an epidemiological survey
46. Dugan E, Roberts CP, Cohen SJ, Preisser JS, Davis CC, Bland DR, et al. Why
corrected for validity. J Clin Epidemiol 1995;48:339–43.
older community-dwelling adults do not discuss urinary incontinence with
28. Brown JS, Bradley CS, Subak LL, Richter HE, Kraus SR, Brubaker L, et al. their primary care physicians. J Am Geriatr Soc 2001;49:462–5.
The sensitivity and specificity of a simple test to distinguish between urge and
47. Burgio KL, Ives DG, Locher JL, Arena VC, Kuller LH. Treatment seeking for
stress urinary incontinence. Ann Intern Med 2006;144:715–23.
urinary incontinence in older adults. J Am Geriatr Soc 1994;42:208–12.
29. Jackson RA, Vittinghoff E, Kanaya AM, Miles TP, Resnick HE, Kritchevsky
SB, et al. Urinary incontinence in elderly women: findings from the Health, 48. Dubeau c.e., Simon SE, Morris JN. The effect of urinary incontinence on
Aging, and Body Composition Study. Obstet Gynecol 2004;104:301–7. quality of life in older nursing home residents. J Am Geriatr Soc
2006;54:1325–33.
30. Johnson TM 2nd, Kincade JE, Bernard SL, Busby-Whitehead J, DeFriese GH.
Self-care practices used by older men and women to manage urinary 49. Hunskaar S, Vinsnes A. The quality of life in women with urinary
incontinence: results from the national follow-up survey on self-care and incontinence as measured by the sickness impact profile. J Am Geriatr Soc
aging. J Am Geriatr Soc 2000;48:894–902. 1991;39:378–82.
31. Mattox TF, Lucente V, McIntyre P, Miklos JR, Tomezsko J. Abnormal spinal 50. Johnson TM 2nd, Kincade JE, Bernard SL, Busby-Whitehead J,
curvature and its relationship to pelvic organ prolapse. Am J Obstet Gynecol Hertz-Picciotto I, DeFriese GH. The association of urinary incontinence with
2000;183:1381–4. poor self-rated health. J Am Geriatr Soc 1998;46:693–9.
32. Sapsford RR, Richardson CA, Maher CF, Hodges PW. Pelvic floor muscle 51. Resnick NM, Yalla SV, Laurino E. The pathophysiology of urinary
activity in different sitting postures in continent and incontinent women. incontinence among institutionalized elderly persons. N Engl J Med
Arch Phys Med Rehabil 2008;89:1741–7. 1989;320:1–7.
33. Schlaich C, Minne HW, Bruckner T, Wagner G, Gebest HJ, Grunze M, et al. 52. Subak LL, Brown JS, Kraus SR, Brubaker L, Lin F, Richter HE, et al.
Reduced pulmonary function in patients with spinal osteoporotic fractures. The “costs” of urinary incontinence for women. Obstet Gynecol
Osteoporos Int 1998;8:261–7. 2006;107:908–16.
MAY JOGC MAI 2009 l 439
You might also like
- Medical Medium Thyroid Healing The TruthDocument8 pagesMedical Medium Thyroid Healing The TruthVatsala Saith0% (19)
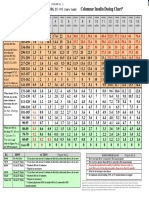
- Columnar Insulin Dosing Chart : (1 ML 1 Unit)Document1 pageColumnar Insulin Dosing Chart : (1 ML 1 Unit)Philippe KinnaerNo ratings yet
- Infections Urinaires Spilf PDFDocument43 pagesInfections Urinaires Spilf PDFsouad sadiNo ratings yet
- Forum Cas CliniquesDocument6 pagesForum Cas CliniquesManal El farhmatNo ratings yet
- Incontinance UrinaireDocument14 pagesIncontinance Urinairemaryam.gynoNo ratings yet
- 2003 Go 261 JacquetinDocument46 pages2003 Go 261 Jacquetinsth39000No ratings yet
- AaaaDocument7 pagesAaaaJean JeanNo ratings yet
- Gériatrie - Incontinence Urinaire Chez La Femme AgéeDocument5 pagesGériatrie - Incontinence Urinaire Chez La Femme Agéehajer chebbiNo ratings yet
- Chirurgie Mini-Invasive de L'incontinenceDocument13 pagesChirurgie Mini-Invasive de L'incontinenceElbordjiNo ratings yet
- Agboranderson2000, 016 Ao Odzebe Pyoneph Brazza 2548-6814-1-SMDocument6 pagesAgboranderson2000, 016 Ao Odzebe Pyoneph Brazza 2548-6814-1-SMtinosan3No ratings yet
- Soust 2019Document7 pagesSoust 2019Putri Rizky AmaliaNo ratings yet
- Problématique de La Prise en Charge de L'insuffisance Rénale Obstétricale Dans Le Service de Néphrologie Du Chu Du Point GDocument3 pagesProblématique de La Prise en Charge de L'insuffisance Rénale Obstétricale Dans Le Service de Néphrologie Du Chu Du Point Gnawalaya518No ratings yet
- Approche Chirurgicale de L'incontinence Anale de L'adulte PDFDocument12 pagesApproche Chirurgicale de L'incontinence Anale de L'adulte PDFMohamed Amine MansouriNo ratings yet
- Recommandations - Bonne Pratique Pour La Prise en Charge Et La Prevention Des Infections Urinaires Associees Aux Soins de L Adulte 2015Document45 pagesRecommandations - Bonne Pratique Pour La Prise en Charge Et La Prevention Des Infections Urinaires Associees Aux Soins de L Adulte 2015xavier.paulmierNo ratings yet
- Les Ovaires Polykystiques: Prise en Charge de L Infertilite en Dehors Des Indications de FivDocument8 pagesLes Ovaires Polykystiques: Prise en Charge de L Infertilite en Dehors Des Indications de FivIJAR JOURNALNo ratings yet
- ArticleDocument10 pagesArticleMaxel JosephNo ratings yet
- 7581french v3Document17 pages7581french v3Hassami SawadogoNo ratings yet
- Effets Gastro Intestinaux Majeurs Des Anti Inflammatoires Non Steroidiens Ains Etude Prospective Marocaine-U9Mk2n8AAQEAAA6pPtYAAAABDocument5 pagesEffets Gastro Intestinaux Majeurs Des Anti Inflammatoires Non Steroidiens Ains Etude Prospective Marocaine-U9Mk2n8AAQEAAA6pPtYAAAABAziz ZakariaNo ratings yet
- Prise en Charge Et Évolution Des Méga-Uretères Primitifs de Découverte AnténataleDocument6 pagesPrise en Charge Et Évolution Des Méga-Uretères Primitifs de Découverte Anténataleracrc3No ratings yet
- Anti Bio TiqueDocument7 pagesAnti Bio Tiquegnepa htgNo ratings yet
- Maladie de Willis-EkbomDocument150 pagesMaladie de Willis-EkbomMihaela-Alexandra PopNo ratings yet
- Travail de Memoire - Avant Projet-1-ReviseDocument17 pagesTravail de Memoire - Avant Projet-1-ReviseJasmin ToussaintNo ratings yet
- Conj 28 2 139Document7 pagesConj 28 2 139AugustinNo ratings yet
- Fertiloscopy Tunisian ExperimentDocument7 pagesFertiloscopy Tunisian ExperimentFatehMoussaNo ratings yet
- Metabolisme Des Glucides EtDocument7 pagesMetabolisme Des Glucides EtRania BouabdallahNo ratings yet
- Introduction OiaDocument1 pageIntroduction Oiagodwe ernestNo ratings yet
- E Volution Clinique de La de Pression Post-Accident Vasculaire Ce Re Bral A' KinshasaDocument7 pagesE Volution Clinique de La de Pression Post-Accident Vasculaire Ce Re Bral A' KinshasaAdèle YoukéNo ratings yet
- SclérodermieDocument4 pagesSclérodermieHenry TraoréNo ratings yet
- 21PSF AB-Eposter PDFDocument146 pages21PSF AB-Eposter PDFZied LouatiNo ratings yet
- AUJ (V03N2) P48a-E 72 ONLINEDocument5 pagesAUJ (V03N2) P48a-E 72 ONLINEOum BanatNo ratings yet
- 03 - Systematique Des Formes D IncontinenceDocument6 pages03 - Systematique Des Formes D IncontinenceIván ATNo ratings yet
- Inf UrinDocument21 pagesInf UrinAissa SadouneNo ratings yet
- Diagnostic Et Prise en Charge Du SOPK en 2021: Diagnosis and Management of PCOS in 2021Document4 pagesDiagnostic Et Prise en Charge Du SOPK en 2021: Diagnosis and Management of PCOS in 2021Ahmed ElNo ratings yet
- NL 31057Document3 pagesNL 31057Sarab AlwardNo ratings yet
- Endoscopic Biliary Drainage As Palliative Treatment For Malignant Biliary Obstruction: Findings and Factors Associated With The Successor FailureDocument6 pagesEndoscopic Biliary Drainage As Palliative Treatment For Malignant Biliary Obstruction: Findings and Factors Associated With The Successor FailureIJAR JOURNALNo ratings yet
- 81982-Article Text-196300-1-10-20121005Document4 pages81982-Article Text-196300-1-10-20121005Youssouf Ibrahim MadiNo ratings yet
- Candiduries Diagnostics Traitement Et Suivi AFU 2011Document8 pagesCandiduries Diagnostics Traitement Et Suivi AFU 2011Mouhcin BelmekiNo ratings yet
- 1 s2.0 S000799602200089X AmDocument15 pages1 s2.0 S000799602200089X Amabdoulazizboutefika14No ratings yet
- Ajol-File-Journals 708 Articles 256960 6526715da19d9Document6 pagesAjol-File-Journals 708 Articles 256960 6526715da19d9youssrabtl7No ratings yet
- Prolapsus Traitement Non ChirurgicaleDocument45 pagesProlapsus Traitement Non Chirurgicalesaffkhal ottNo ratings yet
- La Revue Du Praticien-Néphrologie UrologieDocument140 pagesLa Revue Du Praticien-Néphrologie Urologiedrbadis100% (2)
- Affections Buccodentaires Et Grossesse DR KanéDocument10 pagesAffections Buccodentaires Et Grossesse DR KanéDrissa KonatéNo ratings yet
- TOXINE en MultisitesDocument3 pagesTOXINE en MultisitesAicha BenzagoutaNo ratings yet
- RésuméDocument3 pagesRésumélolaNo ratings yet
- Thèse de Doctorat de L'université Paris-SaclayDocument197 pagesThèse de Doctorat de L'université Paris-SaclayAquarelle Prothesiste OngulaireNo ratings yet
- Évaluation Des Symptômes Dans L'endométrioseDocument4 pagesÉvaluation Des Symptômes Dans L'endométriosebenben31No ratings yet
- Infections Urinaires MasculinesDocument7 pagesInfections Urinaires MasculinesMahefa Serge RakotozafyNo ratings yet
- MainDocument3 pagesMainmalek marouaniNo ratings yet
- Malformations Congénitales Digestives DOUALA 2021Document5 pagesMalformations Congénitales Digestives DOUALA 2021JAMILA SajidNo ratings yet
- Tub Uro GenitaleDocument7 pagesTub Uro GenitaleRoddy RragNo ratings yet
- Benamor 2014Document1 pageBenamor 2014HakimoNo ratings yet
- M LaffaurieDocument71 pagesM Laffaurieifelfli27No ratings yet
- AciclovirDocument18 pagesAciclovirHouzéfa SabiralyNo ratings yet
- PEC Abcès Tubo OvariensDocument11 pagesPEC Abcès Tubo OvariensMaina OumaraNo ratings yet
- 76 241 1 PBDocument5 pages76 241 1 PBabdou koulbouNo ratings yet
- KidneyHealth KidneyCysts FS 2022 FrenchDocument2 pagesKidneyHealth KidneyCysts FS 2022 FrenchBouchra Dou.No ratings yet
- L'échographie Abdominopelvienne en Cas de Suspicion D'appendicite Aiguë: Évaluation Prospective Chez L'adulteDocument5 pagesL'échographie Abdominopelvienne en Cas de Suspicion D'appendicite Aiguë: Évaluation Prospective Chez L'adulteElbordjiNo ratings yet
- CorrectionsDocument21 pagesCorrectionsfaress belloiniNo ratings yet
- 5-Présentation DPC IUASDocument47 pages5-Présentation DPC IUASHoumaleu Romaric AlexNo ratings yet
- Spilf Groupe Recos Iu Sep 18 11 20Document7 pagesSpilf Groupe Recos Iu Sep 18 11 20ifelfli27No ratings yet
- Blood ReportDocument2 pagesBlood ReportDeepak VasudevNo ratings yet
- Study of Coagulation Profile in Type 2 Diabetes Mellitus Patients in Correlation With Long Term Glycemic Control (Hba1c)Document2 pagesStudy of Coagulation Profile in Type 2 Diabetes Mellitus Patients in Correlation With Long Term Glycemic Control (Hba1c)IJAR JOURNALNo ratings yet
- The Entire Endocrinology Lectures Set PDFDocument385 pagesThe Entire Endocrinology Lectures Set PDFoakley bartNo ratings yet
- Hypo BrochureDocument2 pagesHypo Brochurea604No ratings yet
- Primary HyperparathyroidismDocument5 pagesPrimary HyperparathyroidismAbdul QuyyumNo ratings yet
- Interpretation: S12 - FPSC Lankeshwar Lankeswar Survey School Dist. Kamrup P S Jalukbari Guwahati Assam - 781014Document2 pagesInterpretation: S12 - FPSC Lankeshwar Lankeswar Survey School Dist. Kamrup P S Jalukbari Guwahati Assam - 781014Chandan Kumar DasNo ratings yet
- Sata EndocrineDocument10 pagesSata EndocrineMaurice Bryan Roslinda50% (2)
- "Regulation of Blood Glucose": Submitted By: Bemisal Ayaz Roll #. 1 1 DPT 2 Proff EveningDocument5 pages"Regulation of Blood Glucose": Submitted By: Bemisal Ayaz Roll #. 1 1 DPT 2 Proff Eveningaza bellaNo ratings yet
- Nutra Puding Buah NagaDocument2 pagesNutra Puding Buah NagaUun RochmawatiNo ratings yet
- Lecture 14-Thyroid DrugsDocument23 pagesLecture 14-Thyroid DrugsLê Thị Hồng NgọcNo ratings yet
- Guide To Hba1C: Blood Glucose Diagnosing DiabetesDocument3 pagesGuide To Hba1C: Blood Glucose Diagnosing DiabetesTayyab Tahir MinhasNo ratings yet
- Invention of Insulin: Andreea 2016130148Document1 pageInvention of Insulin: Andreea 2016130148Eny KimNo ratings yet
- Study Guide Blood Glucose MonitoringDocument4 pagesStudy Guide Blood Glucose MonitoringDan Dan ManaoisNo ratings yet
- HbA1c and Estimated Average GlucoseDocument2 pagesHbA1c and Estimated Average Glucoseibrahim_barakatNo ratings yet
- FnE MCQsDocument11 pagesFnE MCQsGladys YaresNo ratings yet
- 12 BibliographyDocument10 pages12 BibliographyPraveena.RNo ratings yet
- Diabetes MelitusDocument27 pagesDiabetes Melitusana chasanahNo ratings yet
- Daftar PustakaDocument8 pagesDaftar PustakaErmaffNo ratings yet
- DM RSMD (Dr. Andi Sulistyo H, SP - PD)Document54 pagesDM RSMD (Dr. Andi Sulistyo H, SP - PD)desyNo ratings yet
- Acute Complication of Diabetic MellitusDocument10 pagesAcute Complication of Diabetic MellitusNdzalama Freedom MakhuveleNo ratings yet
- Dr. Ali's Uworld Notes For Step 2 CKDocument29 pagesDr. Ali's Uworld Notes For Step 2 CKmarina shawkyNo ratings yet
- English Espanol: GoiterDocument3 pagesEnglish Espanol: Goiterflex gyNo ratings yet
- PDF Lantus XR Label Information - CompressDocument17 pagesPDF Lantus XR Label Information - CompressDea PermataNo ratings yet
- Blood Glucose Test Worksheet: Activity 4Document3 pagesBlood Glucose Test Worksheet: Activity 4Marcelle Ann C. VillanuevaNo ratings yet
- Yo2pesbjsuqblw4hme2y5jvhDocument2 pagesYo2pesbjsuqblw4hme2y5jvhArghya Roy ChaudhuriNo ratings yet
- Hypoglycemia (DR Fatimah) PDFDocument23 pagesHypoglycemia (DR Fatimah) PDFriopratamasNo ratings yet
- COMMON MCQ Endo 2017 PDFDocument27 pagesCOMMON MCQ Endo 2017 PDFعلي. احمدNo ratings yet
- Pearson, Josie Unit 4 ProjectDocument2 pagesPearson, Josie Unit 4 Projectjosephine pearsonNo ratings yet