Professional Documents
Culture Documents
Failure of Endodontic Treatment: The Usual Suspects: Review
Uploaded by
Carlos San MartinOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Failure of Endodontic Treatment: The Usual Suspects: Review
Uploaded by
Carlos San MartinCopyright:
Available Formats
Published online: 2019-09-23
Review Article
Failure of endodontic treatment: The usual suspects
Sadia Tabassum1, Farhan Raza Khan1
Correspondence: Dr Sadia Tabassum 1
Operative Dentistry, Aga Khan University Hospital,
Email: sadyatabassum@gmail.com Karachi, Pakistan
ABSTRACT
Inappropriate mechanical debridement, persistence of bacteria in the canals and apex, poor obturation quality, over
and under extension of the root canal filling, and coronal leakage are some of the commonly attributable causes of
failure. Despite the high success rate of endodontic treatment, failures do occur in a large number of cases and most
of the times can be attributed to the already stated causes. With an ever increasing number of endodontic treatments
being done each day, it has become imperative to avoid or minimize the most fundamental of reasons leading to
endodontic failure. This paper reviews the most common causes of endodontic failure along with radiographic examples.
Key words: Endodontics, periapical periodontitis, root canal therapy
INTRODUCTION of any infected pulp tissue so the canal space can
be shaped and prepared to be filled with an inert
Endodontic treatment is fairly predictable in nature material thus preventing or minimizing any chances
with reported success rates up to 86–98%.[1] However, of reinfection. However, failure ensues when the
there has not been a consensus in the literature endodontic treatment falls short of the standard
upon a consistent definition of “success” criteria clinical principles.[3]
of endodontic treatment. Likewise “failure” has
variable definitions. It has been defined in some PERSISTENCE OF BACTERIA
studies as a recurrence of clinical symptoms along
with the presence of a periapical radiolucency.[2] An One of the foremost causes of endodontic failure
endodontically treated tooth should be evaluated is persistent microbiological infection. [4] The role
clinically as well as radiographically for its root canal of bacteria in periradicular infection has been well
treatment to be deemed successful. Patient should established in literature and endodontic treatment
be scheduled for follow ups to ascertain that the will be afflicted with a higher chance of failure if
treatment is a success and the tooth in question is microorganisms persist in the canals at the time of
functional. Myriad of factors have been implicated in root canal obturation.[5] Bacteria harbored in root
the failure of endodontic treatment. The usual factors canal areas such as isthmuses, dentinal tubules and
which can be attributed to endodontic failure are: ramifications may evade disinfectants.[6] A study
• Persistence of bacteria (intra-canal and extra-canal) performed by Lin et al. on 236 cases of endodontic
• Inadequate filling of the canal (canals that are treatment failures found a correlation between the
poorly cleaned and obturated) presence of bacterial infection in the canals and
• Overextensions of root filling materials
• Improper coronal seal (leakage) This is an open access article distributed under the terms of the Creative
• Untreated canals (both major and accessory) Commons Attribution‑NonCommercial‑ShareAlike 3.0 License, which allows
• Iatrogenic procedural errors such as poor access others to remix, tweak, and build upon the work non‑commercially, as long as the
author is credited and the new creations are licensed under the identical terms.
cavity design
• Complications of instrumentation (ledges, For reprints contact: reprints@medknow.com
perforations, or separated instruments).
How to cite this article: Tabassum S, Khan FR. Failure of endodontic
treatment: The usual suspects. Eur J Dent 2016;10:144-7.
The aim of endodontic treatment is thorough
debridement and cleaning of the root canal system DOI: 10.4103/1305-7456.175682
144 © 2016 European Journal of Dentistry | Published by Wolters Kluwer - Medknow
Tabassum and Khan: Endodontic failure
periradicular rarefaction in endodontic failures.[7] obturation is 4 times more likely to fail than under
Bacteria present in the periradicular area will be obturated canals. In the presence of an existing
inaccessible to disinfection procedures. Canals with periradicular lesion, an overextended root canal filling
negative cultures for bacteria are said to have higher will have a worse prognosis than a tooth without excess
success rates as opposed to those canals which test filling material.[9] Moreover in a study,[14] an association
positive.[8] Treatment is more likely to fail in these was found between increased incidence of periapical
teeth with pretreatment periradicular rarefactions periodontitis and inadequate or overextended root
than those without these radiographic changes.[9] fillings. However paradoxical results were reported
Other than improper debridement of the canal, a leaky in a study by Lin et al., in which the apical extent of
apical seal is also a contributory factor in endodontic the root fillings did not seem to have any significant
failure due to microbiological persistence.[4] Seepage correlation with treatment failures[7] [Figure 2a and b].
of fluids is likely to occur if apical seal is not properly
established. This can perpetuate periradicular IMPROPER CORONAL SEAL
inflammation anytime. The chances of a favorable
outcome are invariably higher when an affective A well-sealing coronal restoration is essential after
cleaning of the canal has been undertaken. Thus the completion of obturation as it would prevent the
the importance of thorough debridement cannot be ingress of any microorganisms, which are present in
over emphasized [Figure 1a and b]. the ambient environment.[15] Swanson and Madison[16]
emphasized in their study that coronal leakage
INADEQUATE OR OVEREXTENDED should be considered as a potential factor resulting in
ROOT FILLING endodontic failure. The importance of a good quality
coronal restoration was also emphasized by Ray
Apart from proper disinfection and debridement of and Trope in their study[17] and later, their work was
canals, another factor which is of colossal importance replicated by another retrospective study performed
is the quality of obturation. The quality of root canal on 1001 endodontically treated teeth.[10] The results
obturation was the most important factor in the success of this latter study showed that success rates of the
of the endodontic treatment in a study carried out teeth with poor quality coronal restorations fell in
on 1001 endodontically treated teeth.[10] In another contrast to teeth with good quality obturation and
study which assessed teeth with endodontic failures, coronal restorations. However the main determining
65% of the cases exhibited poor quality obturation factor in the success of the root canal was proved to
whereas 42% of the teeth had some canals which were be the quality of the root canal filling in this study
left untreated.[11] Success rates are naturally lower for rather than the quality of the coronal restoration.
obturations which are under or overextended and Nevertheless, an impervious seal at the coronal area
are highest for those which end flush or within 2 mm is vital for a successful prognosis of an endodontically
of the apex.[12] According to a study,[13] overextended treated tooth [Figure 3]. Ng et al., in their meta-analysis
stated that pooled success rate for teeth which have
satisfactory restorations is higher than those teeth
which have poor quality restorations.[8]
COMPLICATIONS OF INSTRUMENTATION
Rotary instruments tend to fracture in the canals
when either laws of access cavity preparation are not
a b
Figure 1: (a) Endodontic treatment in this patient failed due to a leaky
a b
apical seal which resulted in a persistent periapical radiolucency.
(b) Retrograde endodontic treatment was done to seal the apices so a Figure 2: (a) The success rate is reduced: With overextended obturation.
favorable environment can occur for the healing of the infection (b) And under extended obturation
European Journal of Dentistry, Vol 10 / Issue 1 / Jan-Mar 2016 145
Tabassum and Khan: Endodontic failure
adhered to or guidelines regarding the use of rotary
instruments are not followed. As a consequence
of fracture, the access to the apical portion of
the root canal is decreased and this could have a
deleterious effect on canal disinfection and later
on, on obturation. Most of the studies done on the
effect of fractured instruments have demonstrated
the minimal influence on the success rate of the
treatment. [9,18,19] The stage of instrumentation at
which the instrument breaks can have an effect on
the prognosis. The disinfection and obturation of
the part of canal distal to the fractured instrument
becomes difficult possibly leading to the presence
of persistent infection in that area. [19] However,
the fractured instrument itself has less to do with Figure 3: Improper coronal seal along with under extended obturation
failure because most of the times, the success is has played havoc resulting in periapical periodontitis
only affected when a concomitant infection is
present.[3] A clinical investigation on relationship
of broken rotary instruments to endodontic case
prognosis confirmed that in the absence of any
preoperative infection and periradicular changes,
a separated instrument is most likely not to affect
the prognosis.[20] Hence it would be very rare that
the fractured instrument is directly involved in
endodontic failure [Figure 4a and b].
UNTREATED CANALS a b
Figure 4: (a) File separated in apical third of the mesial canal of a
It is not an uncommon practice to miss a canal while mandibular molar. (b) The tooth is asymptomatic after a follow-up
after 2 years
carrying out endodontic treatment especially in molar
teeth where one root, one canal formula is frequently
over ruled by the fact that number of canals are more
than the number of roots. Moreover, a less than
adequate access opening makes it difficult for the
primary dentist to locate the supplemental canals.
The inability to treat all the canals is one of the causes
leading to endodontic failure. Bacteria residing in
these canals lead to the persistence of symptoms.
a b
The results of one study carried out on 5616 molars
Figure 5: (a) Patient remained symptomatic after the treatment of
which were retreated showed that failure to locate the maxillary first molar. (b) On follow-up visit, mesiobuccal 2 was located
MB2 canal had resulted in a significant decrease in and obturated
the long-term prognosis of those teeth.[21] In another
prospective study carried out by Hoen and Pink,[11] the success. Regular follow ups aid in assessing the
the incidence of missed canals were reported to outcome and should be done at least on a yearly basis to
be 42% of all the 1100 endodontically failing teeth monitor any changes. However clinical thoroughness
[Figure 5a and b]. during the treatment phase can potentially benefit the
clinician and the patient in the long run.
CONCLUSIONS
Financial support and sponsorship
To sum it up, these “usual suspects” should be kept Nil.
in mind while carrying out the endodontic treatment.
Giving attention to details not only improves the Conflicts of interest
finesse of the endodontic quality but also maximizes There are no conflicts of interest.
146 European Journal of Dentistry, Vol 10 / Issue 1 / Jan-Mar 2016
Tabassum and Khan: Endodontic failure
REFERENCES 13. Swartz DB, Skidmore AE, Griffin JA Jr. Twenty years of endodontic
success and failure. J Endod 1983;9:198-202.
14. Segura-Egea JJ, Jiménez-Pinzón A, Poyato-Ferrera M, Velasco-Ortega
1. Song M, Kim HC, Lee W, Kim E. Analysis of the cause of failure in E, Ríos-Santos JV. Periapical status and quality of root fillings and
nonsurgical endodontic treatment by microscopic inspection during coronal restorations in an adult Spanish population. Int Endod J
endodontic microsurgery. J Endod 2011;37:1516-9. 2004;37:525-30.
2. Ashley M, Harris I. The assessment of the endodontically treated 15. Bayram HM, Celikten B, Bayram E, Bozkurt A. Fluid flow evaluation
tooth. Dent Update 2001;28:247-52. of coronal microleakage intraorifice barrier materials in endodontically
3. Siqueira JF Jr. Aetiology of root canal treatment failure: Why treated teeth. Eur J Dent 2013;7:359-62.
well-treated teeth can fail. Int Endod J 2001;34:1-10. 16. Swanson K, Madison S. An evaluation of coronal microleakage
4. Endo MS, Ferraz CC, Zaia AA, Almeida JF, Gomes BP. Quantitative in endodontically treated teeth. Part I. Time periods. J Endod
and qualitative analysis of microorganisms in root-filled teeth with 1987;13:56-9.
persistent infection: Monitoring of the endodontic retreatment. Eur J 17. Ray HA, Trope M. Periapical status of endodontically treated teeth
Dent 2013;7:302-9. in relation to the technical quality of the root filling and the coronal
5. Sjögren U, Figdor D, Persson S, Sundqvist G. Influence of infection restoration. Int Endod J 1995;28:12-8.
at the time of root filling on the outcome of endodontic treatment of 18. Simon S, Machtou P, Tomson P, Adams N, Lumley P. Influence of
teeth with apical periodontitis. Int Endod J 1997;30:297-306. fractured instruments on the success rate of endodontic treatment.
6. Lin LM, Pascon EA, Skribner J, Gängler P, Langeland K. Clinical, Dent Update 2008;35:172-4, 176, 178-9.
radiographic, and histologic study of endodontic treatment failures. 19. Kerekes K, Tronstad L. Long-term results of endodontic treatment
Oral Surg Oral Med Oral Pathol 1991;71:603-11. performed with a standardized technique. J Endod 1979;5:83-90.
7. Lin LM, Skribner JE, Gaengler P. Factors associated with endodontic 20. Crump MC, Natkin E. Relationship of broken root canal instruments
treatment failures. J Endod 1992;18:625-7. to endodontic case prognosis: A clinical investigation. J Am Dent
8. Ng YL, Mann V, Rahbaran S, Lewsey J, Gulabivala K. Outcome Assoc 1970;80:1341-7.
of primary root canal treatment: Systematic review of the 21. Wolcott J, Ishley D, Kennedy W, Johnson S, Minnich S, Meyers J. A 5 yr
literature - Part 2. Influence of clinical factors. Int Endod J 2008;41:6-31. clinical investigation of second mesiobuccal canals in endodontically
9. Engström B, Lundberg M. The correlation between positive culture treated and retreated maxillary molars. J Endod 2005;31:262-4.
and the prognosis of root canal therapy after pulpectomy. Odontol
Revy 1965;16:193-203.
Access this article online
10. Tronstad L, Asbjørnsen K, Døving L, Pedersen I, Eriksen HM. Influence
of coronal restorations on the periapical health of endodontically Quick Response Code:
treated teeth. Endod Dent Traumatol 2000;16:218-21.
11. Hoen MM, Pink FE. Contemporary endodontic retreatments: An
analysis based on clinical treatment findings. J Endod 2002;28:834-6. Website:
12. Kojima K, Inamoto K, Nagamatsu K, Hara A, Nakata K, Morita I, et al. www.eurjdent.com
Success rate of endodontic treatment of teeth with vital and nonvital
pulps. A meta-analysis. Oral Surg Oral Med Oral Pathol Oral Radiol
Endod 2004;97:95-9.
European Journal of Dentistry, Vol 10 / Issue 1 / Jan-Mar 2016 147
You might also like
- Failure of Endodontic Treatment: The Usual Suspects: ReviewDocument4 pagesFailure of Endodontic Treatment: The Usual Suspects: ReviewTasyafikiNo ratings yet
- Eu Dent JDocument5 pagesEu Dent JfionaNo ratings yet
- Joor 12423Document6 pagesJoor 12423AKSNo ratings yet
- Applied Sciences: Regenerative Endodontics As The Future Treatment of Immature Permanent TeethDocument17 pagesApplied Sciences: Regenerative Endodontics As The Future Treatment of Immature Permanent TeethFoysal SirazeeNo ratings yet
- Outcome of Revascularization Procedure A Retrospective Case Series PDFDocument8 pagesOutcome of Revascularization Procedure A Retrospective Case Series PDF吳國豪No ratings yet
- Traditional and Contemporary Techniques For Optimizing Root Canal IrrigationDocument9 pagesTraditional and Contemporary Techniques For Optimizing Root Canal IrrigationrintanfsNo ratings yet
- Endodontic Retreatment in Case of Failure: Case ReportDocument3 pagesEndodontic Retreatment in Case of Failure: Case ReportputriraudatulNo ratings yet
- Endodontic Treatment FailureDocument8 pagesEndodontic Treatment FailureHawzheen SaeedNo ratings yet
- Tissue Response To Dental CariesDocument24 pagesTissue Response To Dental CariesGabriel Miloiu100% (1)
- Copia de Tissue Response To Dental CariesDocument7 pagesCopia de Tissue Response To Dental Cariesjorefe12No ratings yet
- Review Article: Restoration of Endodontically Treated Teeth Review and Treatment RecommendationsDocument10 pagesReview Article: Restoration of Endodontically Treated Teeth Review and Treatment RecommendationsKrupali JainNo ratings yet
- Abstract and Key WordsDocument10 pagesAbstract and Key WordsAliyah SaraswatiNo ratings yet
- Case Report Treatment of A Periodontic-Endodontic Lesion in A Patient With Aggressive PeriodontitisDocument10 pagesCase Report Treatment of A Periodontic-Endodontic Lesion in A Patient With Aggressive PeriodontitissulistiyaNo ratings yet
- Is Endodontic Re-Treatment Mandatory For Every Relatively Old Temporary Restoration?: A Narrative ReviewDocument7 pagesIs Endodontic Re-Treatment Mandatory For Every Relatively Old Temporary Restoration?: A Narrative ReviewARTNo ratings yet
- Pulp Revascularization of A Necrotic Infected Immature Permanent Tooth: Case Report and Review of The LiteratureDocument4 pagesPulp Revascularization of A Necrotic Infected Immature Permanent Tooth: Case Report and Review of The LiteratureRiad BachoNo ratings yet
- Criteria For The Ideal Treatment Option For Failed Tics Surgical or NonsurgicalDocument8 pagesCriteria For The Ideal Treatment Option For Failed Tics Surgical or NonsurgicalPaRpArOsSaNo ratings yet
- Restoring Proximal Caries Lesions Conservatively With Tunnel RestorationsDocument8 pagesRestoring Proximal Caries Lesions Conservatively With Tunnel RestorationsyesikaichaaNo ratings yet
- Ex Vivo Microbial Leakage Analysis of Polytetrafluoroethylene Tape and Cotton Pellet As Endodontic Access Cavity SpacersDocument7 pagesEx Vivo Microbial Leakage Analysis of Polytetrafluoroethylene Tape and Cotton Pellet As Endodontic Access Cavity SpacersAbhishek Isaac MathewNo ratings yet
- Traditional and Contemporary Techniques For Optimizing Root Canal IrrigationDocument8 pagesTraditional and Contemporary Techniques For Optimizing Root Canal IrrigationfebrinaNo ratings yet
- Regenerative Endodontics Barriers and Strategies For Clinical Translation 2012 Dental Clinics of North AmericaDocument11 pagesRegenerative Endodontics Barriers and Strategies For Clinical Translation 2012 Dental Clinics of North AmericaCaioSelaimenNo ratings yet
- Failure of Root Canal Treatment PDFDocument2 pagesFailure of Root Canal Treatment PDFMelissaNo ratings yet
- ADJALEXU - Volume 43 - Issue 2 - Pages 7-12Document6 pagesADJALEXU - Volume 43 - Issue 2 - Pages 7-12Belinda SalmaNo ratings yet
- 697-Article Text-2692-1-10-20191204Document7 pages697-Article Text-2692-1-10-20191204silviana yusufNo ratings yet
- Selective Caries ExcavationDocument10 pagesSelective Caries Excavationjorefe12No ratings yet
- Retrograde PreparationDocument16 pagesRetrograde Preparationwhussien7376100% (1)
- Horizontal Posts PDFDocument6 pagesHorizontal Posts PDFaishwarya singhNo ratings yet
- Is Coronal Restoration More Important Than Root Filling For Ultimate Endodontic Success?Document7 pagesIs Coronal Restoration More Important Than Root Filling For Ultimate Endodontic Success?GowriNo ratings yet
- OOOO Ricucci 2000Document6 pagesOOOO Ricucci 2000karlaNo ratings yet
- Internal Root Resorption Sixty Four ThouDocument8 pagesInternal Root Resorption Sixty Four ThouMihaela TuculinaNo ratings yet
- Endodontology: Editor: Larz S. W. Spa NgbergDocument6 pagesEndodontology: Editor: Larz S. W. Spa NgbergHenrique Silva PessoaNo ratings yet
- Potential Mesenchymal and Dental Pulp Stem Cell Usage For Regeneration of Dentine and Its ComplicationsDocument10 pagesPotential Mesenchymal and Dental Pulp Stem Cell Usage For Regeneration of Dentine and Its ComplicationsAthenaeum Scientific PublishersNo ratings yet
- Influence of Age and Apical Diameter on TheDocument6 pagesInfluence of Age and Apical Diameter on ThethaynamodtkowskiNo ratings yet
- J Pharm Bioallied SciDocument10 pagesJ Pharm Bioallied SciSuaeni Kurnia WirdaNo ratings yet
- Regenerative Endodontics: A Way ForwardDocument9 pagesRegenerative Endodontics: A Way ForwardCynthia LlangaNo ratings yet
- Failed Root Canals The Case For Extraction and Immediate Implant PlacementDocument3 pagesFailed Root Canals The Case For Extraction and Immediate Implant PlacementKarin Noga VerhagenNo ratings yet
- Which Endodontic Access Cavity Is Best? A Literature Review: GeneralDocument5 pagesWhich Endodontic Access Cavity Is Best? A Literature Review: GeneralEdinam Gaveh100% (1)
- Bergenholtz Spangberg 2004 Controversies in EndodonticsDocument16 pagesBergenholtz Spangberg 2004 Controversies in Endodontics筒井絢子No ratings yet
- Expert Consensus On Regenerative Endodontic ProceduresDocument13 pagesExpert Consensus On Regenerative Endodontic Procedures朱嘉琪No ratings yet
- 2016 Dental Pulp Revascularization of Necrotic Permanent Teeth WithDocument6 pages2016 Dental Pulp Revascularization of Necrotic Permanent Teeth Withbenlaifaoui.amira.2511No ratings yet
- Causes and Manifestations of Non-Surgical Endodontic Treatment FailureDocument5 pagesCauses and Manifestations of Non-Surgical Endodontic Treatment FailureMatt246No ratings yet
- 1 s2.0 S0300571220301767 Main PDFDocument10 pages1 s2.0 S0300571220301767 Main PDFCesar AmaroNo ratings yet
- Clinical Case Reports - 2023 - Vyver - Apexification of Dens Evaginatus in A Mandibular Premolar A Case ReportDocument6 pagesClinical Case Reports - 2023 - Vyver - Apexification of Dens Evaginatus in A Mandibular Premolar A Case ReportIqra KhanNo ratings yet
- Carranza's Clinical Periodontology 2002Document6 pagesCarranza's Clinical Periodontology 2002Lia Optimeze Alwayz100% (1)
- Margenes RestaurativosDocument18 pagesMargenes RestaurativosCdjuan GnNo ratings yet
- Do Not Miss It"radix Entamolaris in Pediatric Patients An Endodontic Challenge: A Case Series and Review of Literature."Document5 pagesDo Not Miss It"radix Entamolaris in Pediatric Patients An Endodontic Challenge: A Case Series and Review of Literature."arshad khandayNo ratings yet
- Lambrianidis Ledging EndodontictopicsDocument20 pagesLambrianidis Ledging EndodontictopicsAyu Diah LestariNo ratings yet
- Aej 12087Document6 pagesAej 12087drvivek reddyNo ratings yet
- Article 1603861587Document7 pagesArticle 1603861587Nathania AstriaNo ratings yet
- Apexogenesis and ApexificationDocument4 pagesApexogenesis and ApexificationAlandNovrianDwiSaputraNo ratings yet
- Lesion Sterilization and Tissue Repair Therapy (LSTR) of Necrotic Primary Molars: Case ReportDocument4 pagesLesion Sterilization and Tissue Repair Therapy (LSTR) of Necrotic Primary Molars: Case ReportOmar CoronelNo ratings yet
- Restoration of Endodontically Treated Teeth Review and Treatment RecommendationsDocument31 pagesRestoration of Endodontically Treated Teeth Review and Treatment RecommendationsDr.O.R.GANESAMURTHINo ratings yet
- Periapical GranulomaDocument6 pagesPeriapical GranulomaEzza RiezaNo ratings yet
- Int Endodontic J - 2020 - Silva - Current Status On Minimal Access Cavity Preparations A Critical Analysis and A ProposalDocument18 pagesInt Endodontic J - 2020 - Silva - Current Status On Minimal Access Cavity Preparations A Critical Analysis and A ProposalPhương Thanh HoàngNo ratings yet
- Acceso Min Analisis CriticoDocument19 pagesAcceso Min Analisis CriticoDarianNo ratings yet
- Case Report: Overhanging Fillings in Restorative Dental Treatments and EndodonticsDocument5 pagesCase Report: Overhanging Fillings in Restorative Dental Treatments and EndodonticsKarissa NavitaNo ratings yet
- Lu Et Al. - 2020 - Regenerative Endodontic Procedures For Traumatized IMMATUREDocument6 pagesLu Et Al. - 2020 - Regenerative Endodontic Procedures For Traumatized IMMATUREghaithmechriinfoNo ratings yet
- Revascularization-Associated Intracanal Calcification: A Case Report With An 8-Year ReviewDocument4 pagesRevascularization-Associated Intracanal Calcification: A Case Report With An 8-Year ReviewIvan PolancoNo ratings yet
- Factors Influencing Repair of Dental Restorations With Resin CompositeDocument7 pagesFactors Influencing Repair of Dental Restorations With Resin CompositehbusyNo ratings yet
- Methods of Filling Root CanalsDocument23 pagesMethods of Filling Root CanalsBîrsanu ElenaNo ratings yet
- The Effects of Antimicrobials On Endodontic Biofilm BacteriaDocument8 pagesThe Effects of Antimicrobials On Endodontic Biofilm BacteriaCarlos San MartinNo ratings yet
- Mandibular Canine With Two Canals A Case Report in Saudi ArabiaDocument5 pagesMandibular Canine With Two Canals A Case Report in Saudi ArabiaCarlos San MartinNo ratings yet
- ContentServer Asp-8Document4 pagesContentServer Asp-8Lorena YépezNo ratings yet
- Universitat International de Catalunya Master Online in Endodontics Asymptomatic Apical PeriodontitisDocument14 pagesUniversitat International de Catalunya Master Online in Endodontics Asymptomatic Apical PeriodontitisCarlos San MartinNo ratings yet
- Mlohw7Document5 pagesMlohw7Carlos San MartinNo ratings yet
- Clinical Efficacy of Activated Irrigation in Endodontics: A Focused ReviewDocument16 pagesClinical Efficacy of Activated Irrigation in Endodontics: A Focused ReviewCarlos San MartinNo ratings yet
- 2185RDE - Rde 45 E23Document12 pages2185RDE - Rde 45 E23Carlos San MartinNo ratings yet
- AAE Position StatementDocument5 pagesAAE Position StatementCarlos San MartinNo ratings yet
- Root Canal MicrofloraDocument9 pagesRoot Canal MicrofloraCarlos San MartinNo ratings yet
- 3 DObturationDocument10 pages3 DObturationsonygabrielNo ratings yet
- Srep 17823Document6 pagesSrep 17823Carlos San MartinNo ratings yet
- Materials 14 02427Document12 pagesMaterials 14 02427Carlos San MartinNo ratings yet
- 1974 Seidberg, B. H., & Schilder, H. (1974) - An Evaluation of EDTA in Endodontics.Document12 pages1974 Seidberg, B. H., & Schilder, H. (1974) - An Evaluation of EDTA in Endodontics.Carlos San MartinNo ratings yet
- 2020 Article 91Document6 pages2020 Article 91Carlos San MartinNo ratings yet
- Aetiology of Root Canal Treatment Failure - Why Well-Treated Teeth Can FailDocument10 pagesAetiology of Root Canal Treatment Failure - Why Well-Treated Teeth Can FailFlorin IonescuNo ratings yet
- K Uttler 1955Document9 pagesK Uttler 1955Carlos San MartinNo ratings yet
- Hipocloritstoma 1Document7 pagesHipocloritstoma 1Crina AnutaNo ratings yet
- 20 Repair of Lateral Root Perforation of Mandibular Centtral Incisors With Biodentine - A Case Report Libre PDFDocument4 pages20 Repair of Lateral Root Perforation of Mandibular Centtral Incisors With Biodentine - A Case Report Libre PDFCarlos San MartinNo ratings yet
- Ca OH2Document7 pagesCa OH2Carlos San MartinNo ratings yet
- Endodontology 4: RootsDocument44 pagesEndodontology 4: RootsCarlos San Martin100% (1)
- Endodontology 1: RootsDocument44 pagesEndodontology 1: RootsCarlos San Martin100% (1)
- 2014 01 Jan-Feb Endodontic Practice USDocument60 pages2014 01 Jan-Feb Endodontic Practice USCarlos San MartinNo ratings yet
- Endodontology 1: International Magazine ofDocument44 pagesEndodontology 1: International Magazine ofCarlos San MartinNo ratings yet
- Endodontology 3: RootsDocument44 pagesEndodontology 3: RootsCarlos San MartinNo ratings yet
- Biodentine Clinical Study For EndoDocument7 pagesBiodentine Clinical Study For EndoEric ThielkNo ratings yet
- Endodontology 2: RootsDocument44 pagesEndodontology 2: RootsCarlos San MartinNo ratings yet
- 2013 Metzger - The Role of Mechanical Instrumentation in The Cleaning of Root CanalsDocument23 pages2013 Metzger - The Role of Mechanical Instrumentation in The Cleaning of Root CanalsCarlos San MartinNo ratings yet
- 2013 Metzger - The Self-Adjusting File SystemDocument22 pages2013 Metzger - The Self-Adjusting File SystemCarlos San MartinNo ratings yet
- Bio DentineDocument2 pagesBio DentineCarlos San MartinNo ratings yet
- Cash Flow Statement and Balance Sheet of A Solar Power Plant in APDocument35 pagesCash Flow Statement and Balance Sheet of A Solar Power Plant in APSriharsha Vavilala100% (1)
- DRW Questions 2Document16 pagesDRW Questions 2Natasha Elena TarunadjajaNo ratings yet
- Arpit Y2Document7 pagesArpit Y2swapnil jainNo ratings yet
- CasesDocument8 pagesCasesLinh TrịnhNo ratings yet
- 6wa Retrofit GuideDocument13 pages6wa Retrofit GuideAnonymous X5q33TQ100% (1)
- Order From U.S. Disctrict Judge Jesus G. Bernal To Chino Valley UnifiedDocument9 pagesOrder From U.S. Disctrict Judge Jesus G. Bernal To Chino Valley UnifiedBeau YarbroughNo ratings yet
- Pilkington Profilit Techn Info enDocument12 pagesPilkington Profilit Techn Info enSalmonelo Abdul RamosNo ratings yet
- Key Benefits of Cloud-Based Internet of Vehicle (IoV) - Enabled Fleet Weight Management SystemDocument5 pagesKey Benefits of Cloud-Based Internet of Vehicle (IoV) - Enabled Fleet Weight Management SystemVelumani sNo ratings yet
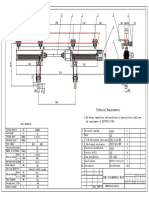
- 2X16-24 Monorail Hoist-04 - 2Document1 page2X16-24 Monorail Hoist-04 - 2RafifNo ratings yet
- MP Process Flow - MBA - MM - MHRMDocument2 pagesMP Process Flow - MBA - MM - MHRMKAVITHA A/P PARIMAL MoeNo ratings yet
- Filiation and Support ClaimsDocument3 pagesFiliation and Support ClaimsEugene BalagotNo ratings yet
- Engg Maths Sem 3 Curve FittingDocument13 pagesEngg Maths Sem 3 Curve FittingRonak Raju ParmarNo ratings yet
- Autoencoder Asset Pricing ModelsDocument22 pagesAutoencoder Asset Pricing ModelsEdson KitaniNo ratings yet
- Internship ReportDocument171 pagesInternship ReportShahrukh MunirNo ratings yet
- Analysis Report PDFDocument4 pagesAnalysis Report PDFJever BorjaNo ratings yet
- BUSINESS TALE - A Story of Ethics, Choices, Success - and A Very Large Rabbit - Theme of Ethics Code or Code of Business Con - EditedDocument16 pagesBUSINESS TALE - A Story of Ethics, Choices, Success - and A Very Large Rabbit - Theme of Ethics Code or Code of Business Con - EditedBRIAN WAMBUINo ratings yet
- C Programming JNTU PDFDocument171 pagesC Programming JNTU PDFfakeNo ratings yet
- Java Programming: Lab Assignment 2Document17 pagesJava Programming: Lab Assignment 2Sanjana chowdary50% (4)
- Challenging Cognitive Distortions HealthyPsych - ComDocument1 pageChallenging Cognitive Distortions HealthyPsych - ComLeila MargaridaNo ratings yet
- Lucsuhin National High School Daily Lesson Plan on Accounting ConceptsDocument6 pagesLucsuhin National High School Daily Lesson Plan on Accounting ConceptsALMA ACUNANo ratings yet
- Inspection & Testing of Elastic Rail Clips PDFDocument5 pagesInspection & Testing of Elastic Rail Clips PDFfiemsabyasachi0% (1)
- Republic of The Philippines, Petitioner, vs. Sandiganbayan, Major General Josephus Q. Ramas and Elizabeth Dimaano, RespondentsDocument23 pagesRepublic of The Philippines, Petitioner, vs. Sandiganbayan, Major General Josephus Q. Ramas and Elizabeth Dimaano, RespondentsKenzo RodisNo ratings yet
- Kneehab XP Instructions and UsageDocument16 pagesKneehab XP Instructions and UsageMVP Marketing and DesignNo ratings yet
- Order 824218 470773 PDFDocument4 pagesOrder 824218 470773 PDFMadalina JariiNo ratings yet
- AMD DEL: Popat / Hitul MR AI0817Document1 pageAMD DEL: Popat / Hitul MR AI0817Mahan YadavNo ratings yet
- Best Frequency Strategies - How Often To Post On Social Media PDFDocument24 pagesBest Frequency Strategies - How Often To Post On Social Media PDFLiet CanasNo ratings yet
- Lab Manual 2 PrintDocument17 pagesLab Manual 2 Printmonikandakumar ramachandranNo ratings yet
- Reviewer in EntrepreneurshipDocument3 pagesReviewer in EntrepreneurshipJazz Add100% (1)
- FINAL Exam - Answer SheetDocument1 pageFINAL Exam - Answer SheetViggo VillanuevaNo ratings yet
- Simple Problem On ABC: RequiredDocument3 pagesSimple Problem On ABC: RequiredShreshtha VermaNo ratings yet