Professional Documents
Culture Documents
14TB Hivdm
Uploaded by
melese fishaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
14TB Hivdm
Uploaded by
melese fishaCopyright:
Available Formats
AIDS & Clinical Esmael et al.
, J AIDS Clin Res 2013, 4:12
http://dx.doi.org/10.4172/2155-6113.1000263
Research
Research Article Open Access
Tuberculosis and Human Immune Deficiency Virus Co-infection in
Debre Markos Referral Hospital in Northwest Ethiopia: A Five Years
Retrospective Study
Ahmed Esmael1*, Girma Tsegaye2, Moges Wubie1 and Mengistu Endris3
1Department of Microbiology, Immunology & Parasitology, Debre Markos University, Ethiopia
2
Department of public health, Debre Markos University, Ethiopia
3
Department of Medical Microbiology, University of Gondar, Ethiopia
Abstract
Background: Tuberculosis (TB) and Human Immunodeficiency Virus (HIV) are major public health problems,
especially in Sub-Saharan Africa including Ethiopia. So, updated information on TB-HIV co-infection might be important
for the planning, resource allocation, prevention and control activities.
Objective: To determine the TB-HIV co-infection and possible associated factors among patients attended TB
clinic in five years (2008-2013) at a referral Hospital in Northwest Ethiopia.
Methods: A retrospective study was conducted among 717 TB patients who are registered at DOTs clinic of Debre
Markos referral hospital. Socio-demographic and clinical data of the study participants were collected from the TB log
from the DOTS clinic. Data were entered and analyzed using SPSS version 16 software.
Results: The prevalence of TB-HIV co-infection was 44% (321/717). The trend of co-infection was decreased
from 2008/9 179 (49.2%) to 2012/13 29 (44.6%). Types of TB and age group were significantly associated with TB-HIV
co-infection.
Conclusion: The prevalence of TB-HIV co-infection was high. Therefore, actions targeting (health education and
early case detection) on those predictors are necessary to effectively reduce TB-HIV co-infection and strengthen the
collaborative activities.
Keywords: Tuberculosis; TB-HIV co-infection; Western ethiopia extra-pulmonary and smear negative tuberculosis than smear positive
cases [19,22].
Introduction
East Gojam is one of the 11 zones in Amhara region with a total
According to World Health Organization (WHO), there were population of 2,153,937. Only 8% of the inhabitants of have access to
an estimated 8.7 million incident cases of TB (range, 8.3 million-9.0 electricity. Majority of the inhabitants were farmer (85%). The case
million) globally [1]. Africa, more specifically Sub-Saharan Africa, faces detection and treatment success rate of TB in the zone was 26% and
the worst TB epidemic, where TB associated morbidity and mortality 86%, respectively [24,25].
occurs mainly in the economically productive age group (15-60 years) Despite this needs, there is no adequate and recent data in Ethiopia
[2]. especially in this study area. Assessment of TB and HIV co-infection
Available data indicated, Ethiopia has been one of the 22 high TB might be important for the planning, resource allocation, prevention
burden countries [3] with an incidence and prevalence rate of 300 and and control activities. Therefore this study aimed to assess TB-HIV co-
470 cases per 100,000 populations respectively. Among all new TB cases infection and the possible associated factors among patients attended
notified to federal ministry of health, 30% were smear positive [4,5]. TB clinic in Debre Markos Referral Hospital, Northwest Ethiopia.
Moreover, the national adult human immunodeficiency virus Methods
(HIV) prevalence infection in Ethiopia was 1.5% [6]. In 2009, the HIV/ Study setting
AIDS Prevention and Control Office (HAPCO) estimated that there
were around 1,116,216 people living with HIV. There were also a total The study was conducted at Debre Markos Referral Hospital in
855,720 AIDS orphans in the country [7,8].
TB is the leading cause of death among people living with HIV.
*Corresponding author: Ahmed Esmael, Department of Microbiology, Immunology
Almost one in four deaths among people with HIV is due to TB. In & Parasitology, Debre Markos University, Ethiopia, Tel: +251-058-771-6768; E-mail:
2010, 350,000 people died of HIV-associated TB [9]. esmaelahmed8@gmail.com
TB and HIV co-infection has been well documented in Sub-Saharan Received October 18, 2013; Accepted November 18, 2013; Published November
23, 2013
African set up [10]. Studies showed that the prevalence of co-infection
was 31.25%, even the rate was as high as 80% [11,12]. Studies in Ethiopia Citation: Esmael A, Tsegaye G, Wubie M, Endris M (2013) Tuberculosis and
Human Immune Deficiency Virus Co-infection in Debre Markos Referral Hospital
also depicted that the co-infection condition has being on increasing in Northwest Ethiopia: A Five Years Retrospective Study. J AIDS Clin Res 4: 263.
rate 6.6%, to 75% in the previous decade (1990-2000) [13-18]. doi: 10.4172/2155-6113.1000263
TB-HIV co-infection has been associated with different age group Copyright: © 2013 Esmael A, et al. This is an open-access article distributed under
the terms of the Creative Commons Attribution License, which permits unrestricted
[17], geographical location [19] and clinical presentation of TB [20-23]. use, distribution, and reproduction in any medium, provided the original author and
For instance, the high prevalence of HIV was observed in patients with source are credited.
J AIDS Clin Res
ISSN:2155-6113 JAR an open access journal Volume 4 • Issue 12 • 1000263
Citation: Esmael A, Tsegaye G, Wubie M, Endris M (2013) Tuberculosis and Human Immune Deficiency Virus Co-infection in Debre Markos Referral
Hospital in Northwest Ethiopia: A Five Years Retrospective Study. J AIDS Clin Res 4: 263. doi: 10.4172/2155-6113.1000263
Page 2 of 4
Debre Markos, which is 300 km away from Addis Ababa. The hospital meninges, etc. Diagnosis of EPTB was based on fine needle aspiration
provides health service to more than 3.5 million populations in its cytology or biochemical analyses of cerebrospinal/pleural/ascitic fluid
catchments. or histopathological examination or strong clinical evidence consistent
with active extrapulmonary tuberculosis, followed by a decision of a
In the hospital, DOTS clinic is operating under the National
Tuberculosis and Leprosy Program (NTLCP) of Ethiopia, under which clinician to treat with a full course of anti-tuberculosis chemotherapy.
patients are diagnosed with tuberculosis by examination of morning- In all the cases of EPTB, sputum examinations and chest radiographs
spot sputum smears by Zeihel-Nieelsen staining, for the presence of were used to investigate the involvement of lung parenchyma. This
Acid fast bacilli (AFB), chest radiographs, and for EPTB, pathological hospital lacks the facilities for culture and drug susceptibility testing.
investigations were used. A patient with at least two sputum specimens Statistical analysis: After data collection, the data were entered
who were positive for acid-fast bacilli is smear positive pulmonary TB. A and coded in to Epi data version 3.1 and exported to SPSS version
patient with symptoms suggestive of TB and radiographic abnormalities 16.0 statistical software. Data were cleaned for inconsistencies and
consistent with pulmonary TB is smear negative pulmonary TB. EPTB missing values. Data cleaning was made by doing descriptive statistics
is confirmed by taking needle aspiration from organ other than TB, run like frequency by removing missing/conflicting ideas and responses to
AFB and radiographic abnormalities. questions about relevant information. Recoding and re-categorizing
Patients are referred to the DOTS clinic where they are registered were made for relevant variables. Frequencies and summary statistics
and treated according to the National Tuberculosis and Leprosy Control (mean, standard deviation, and percentage) were used to describe
Program (NTLCP) [8]. the study population in relation to socio-demographic and other
relevant variables. The degree of association between dependent and
Study design and data collection independent variables was assessed using adjusted odds ratio with 95%
We analyzed a five year retrospective records of 717 tuberculosis confidence interval. A bivariate and multivariate logistic regression
patients registered at Debre Markos referral Hospital`s DOTS clinic was performed to assess statistical association between dependent and
from June 2008 to August 2013. Weight of patient was measured by independent variable. It was done by entering each independent variable
weight balance. The reviewed documents contained basic information separately into bivariate analysis. Then, all variables were entered for
such as patient's age, sex, weight address, TB type, and HIV status. the multivariate logistic regression model. In the multivariate logestic
regression models significant association was declared at p-value less
Inclusion and exclusion criteria than 0.05. Finally data was interpreted with the existed data by referring
Inclusion criteria: All data from 2008-2013 in DOTS clinic of to literature reviews.
Debre Markos referral hospital.
Ethical considerations: Ethical clearance was obtained from
Exclusion criteria: Incomplete data on log book of DOTS clinic. Research and Publication Directorate Office of Debre Markos
University, Ethiopia.
Definitions
According to the standard definitions of the National Tuberculosis
Results
and Leprosy Control Program guideline (NLCP) adopted from WHO Characteristics of study participants
[8], the following clinical case definitions were used:
A total of 717 TB patients were enrolled in this study. Of whom,
Incomplete data: If any one of the information which was reviewed 371 (51.7%) were males with mean age of 30.6 years. The mean initial
on log book (patient's age, sex, address, TB type, weight and HIV status) weight during intensive anti-tuberculosis treatment was 45.2 KGs (SD
was missed. ± 22.9). Most of the study participants were urban resident 457 (63.7%),
new cases 705 (98.3%) and had smear negative pulmonary TB 433
Smear-positive pulmonary TB
(60.4%) (Table 1).
A patient with at least two sputum specimens which were positive
for acid-fast bacilli (AFB) by microscopy, or a patient with only one Characteristics Frequency Percent
sputum specimen which was positive for AFB by microscopy, and chest
Male 371 51.7
radiographic abnormalities consistent with active pulmonary TB. Sex
Female 346 48.3
Smear-negative pulmonary TB <18 124 17.3
Age 18-30 287 40
A patient with symptoms suggestive of TB, with at least two
>31 306 42.7
sputum specimens which were negative for AFB by microscopy,
Urban 457 63.7
and with chest radiographic abnormalities consistent with active Residenc
Rural 259 36.3
pulmonary TB (including interstitial or miliary abnormal images), or
a patient with two sets of at least two sputum specimens taken at least New 705 98.3
two weeks apart, and which were negative for AFB by microscopy, Category Relapse 11 1.5
and radiographic abnormalities consistent with pulmonary TB and Default 1 0.1
lack of clinical response to one week of broad spectrum antibiotic Smear positive Pulmonary TB 103 14.4
therapy. TB Type Smear negative Pulmonary TB 433 60.4
Extra-pulmonary TB 181 25.2
Extrapulmonary TB
Over all 717 100
This included tuberculosis of organs other than the lungs, such as Table 1: Characteristics of the study participants registered at DOTS clinic at
lymph nodes, abdomen, genitourinary tract, skin, joints and bones, Debre Markos referral hospital from June 2013 to August 2013.
J AIDS Clin Res
ISSN:2155-6113 JAR an open access journal Volume 4 • Issue 12 • 1000263
Citation: Esmael A, Tsegaye G, Wubie M, Endris M (2013) Tuberculosis and Human Immune Deficiency Virus Co-infection in Debre Markos Referral
Hospital in Northwest Ethiopia: A Five Years Retrospective Study. J AIDS Clin Res 4: 263. doi: 10.4172/2155-6113.1000263
Page 3 of 4
TB and HIV co-infection In the present, study, the prevalence of TB and HIV co-infection
was 44.8%. In line with these studies in African countries showed
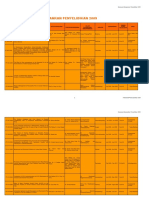
The prevalence of TB and HIV co-infection was 44.8% (321/717)
that the co-occurrence of both infections is well established fact. The
(Table 3). The highest rate of co-infection was observed among smear
prevalence of co-infection also depends on the prevalence of HIV
negative pulmonary TB 32.4 % (206/717), urban residents 28.8%
in a given country [11-18]. For instance, study in Cameron [26], in
(206/717) and 18-30 age groups 17% (122/717) (Table 2). The trend of
Ghana [27] and in Zimbabwe [28] depicted that the prevalence of co-
TB-HIV co-infection was decreased from 2008 to 2012 while raise in
occurrence was 51.6%, 46.2%, and 44%, respectively.
2013 (Figure 1 and Table 2).
In the present study, majority of study participants who showed
Associated factors of TB-HIV co-infection TB/HIV co-infection was pulmonary negative 232(72.3%) and extra
In multivariate analysis extra pulmonary TB and age group (18-30, pulmonary type 51(15.9%). The occurrence of TB/HIV co-infection was
31-40 and 41-50) independently associated with TB -HIV co-infection 2.4 times higher in extra pulmonary tuberculosis cases than pulmonary
(P<0.05) (Table 2). positive cases. This finding was consistent with Daniel et al. in Ethiopia
and Sharma et al. in India which showed that high prevalence of co-
Discussions infection was observed in patients with extra-pulmonary and smear
Currently, the number of TB cases has been increased by several negative tuberculosis than smear positive cases [19,21].
folds especially in sub-Saharan African set up. The presence of high
Studies, especially in sub-Saharan African countries showed that
HIV infection is claimed as the main risk factor for the increment of
the number of HIV infected TB cases were higher in urban than rural
TB patients [3,9].
areas [19,26-28]. Possibly this might be due to a presence of high
prevalence of HIV infection [8,9]. However in our findings, there was
no significance difference in the rate of TB/HIV co-infection.
TB-HIV
60 In the present study age group (18-30 and ≥31) had statistical
49.2%(179/364)
50 significance association with the occurrence of TB/HIV co-infection.
39.3%(33/84)
44.6%(29/65) This finding was in agreement with studies conducted by in Ethiopia
40
42.7% (56/131) [17], in Cameron [26], and in Ghana [27].
30 32.9% (23/70)
TB-HIV
Currently there has been a conflicting report of occurrence of TB/
20
HIV co-infection with regards to sex. For instance Adji et al. in Cameron
10 showed that women had significantly more TB/HIV co-infected than
0
men (42%) [26]. However Demissie et al. in Ethiopia indicated that TB/
2008/9 2009/10 2010/11 2011/12 2012/13 HIV co-infection did not have any significance difference with sex [17].
Our study also depicted similar findings.
year
Figure 1: Trend of TB and TB-HIV co-infection at Debre Markos referral Moreover, studies in Ethiopia indicated that the prevalence of TB/
hospital from June 2013 to August 2013. HIV co-infection was 6.6% in 1990, 20-25% in 1995, 44.4% in 1996,
TB-HIV co-infection
Variables COR (95%CI) P-value AOR (95% CI) P-value
Yes No
Sex
Male 161 210 1 ---- 1 ----
Female 160 186 0.89 (0.6-1.20) 0.46 0.78 (0.54-1.06) 0.12
Age (years)
<18 35 89 1 ---- 1 ----
18-30 122 165 2.93 (1.8-4.61) 0.007 2.52 (1.25-3.14) 0.005
≥31 164 142 1.56 (1.1-2.16) 0.000 1.34 (1.1-2.05) 0.001
Residence
Urban 206 251 0.96 (0.7-1.31) 0.81 0.71 (0.63-1.28) 0.46
Rural 115 145 1 ---- 1 ----
Type of TB
Smear positive PTB 38 65 1 ---- 1 ----
Smear negative PTB 232 201 0.50 (0.3-0.79) 0.02 0.74 (0.35-1.77) 0.59
Extra PTB 51 130 1.49 (0.8-2.49) 0.13 2.44 (1.01-6.14) 0.03
Table 2: Bi and Multivariate analysis of TB/HIV co-infection (n=717) with different variables at Debre Markos referral hospital from June 2013 to August 2013.
Year
TB Cases Total
2008/9 2009/10 2010/11 2011/12 2012/13
TB-HIV co-infection 179 (49.2) 56 (42.7) 33 (39.3) 23 (32.9) 29 (44.6) 323 (44.8)
HIV negative TB cases 185 (50.8) 75 (57.3) 51 (60.7) 47 (67.1) 36 (55.4) 394 (55.2)
Total 364 (51.0) 131 (18.3) 84 (11.8) 70 (9.8) 65 (9.1) 717 (100)
Table 3: Trend of TB and TB-HIV co-infection at Debre Markos referral hospital from June 2008 to August 2013.
J AIDS Clin Res
ISSN:2155-6113 JAR an open access journal Volume 4 • Issue 12 • 1000263
Citation: Esmael A, Tsegaye G, Wubie M, Endris M (2013) Tuberculosis and Human Immune Deficiency Virus Co-infection in Debre Markos Referral
Hospital in Northwest Ethiopia: A Five Years Retrospective Study. J AIDS Clin Res 4: 263. doi: 10.4172/2155-6113.1000263
Page 4 of 4
45.3 in 1997 and 52.1% in 2007 [13-18]. However in our study, the 13. Gellete A, Kebede D, Berhane Y (1997) Tuberculosis and HIV infection in
Southern Ethiopia. Ethiop J Health Dev 11: 51-59.
co-infection rate was continuously decreased from 2009 to 2012 while
somewhat rise during 2013. The possible explanation for this might be 14. Kefene H, Zewdie D, Desta B, Kebede T (1990) The prevalence of HIV-I
due to the current strategic plan of the federal minister of health of Antibodies in 106 TB patients. Ethiop J Health Dev 4: 197-200.
Ethiopia, which expands health facilities across the country. As a result 15. Mitike G, Kebede D, Yeneneh H (1997) HIV infection and anti-tuberculosis
the number of cases who notified in the hospital might be reduced. drug resistance among pulmonary tuberculosis patients in Harrar Tuberculosis
Centre, Ethiopia. East Afr Med J 74: 154-157.
Conclusion and Recommendation 16. Madebo T, Nysaeter G, Lindtjørn B (1997) HIV infection and malnutrition
change the clinical and radiological features of pulmonary tuberculosis. Scand
The prevalence of TB and HIV co-infection was higher than most J Infect Dis 29: 355-359.
previous studies in Ethiopia. The rate of TB-HIV co-infection was
17. Demissie M, Lindtjørn B, Tegbaru B (2000) Human immunodeficiency virus
significantly associated with type of TB and age groups (18-30, ≥31) (HIV) infection in tuberculosis patients in Addis Ababa. Ethiop. J. Health Dev
in our study. Therefore, actions targeting (health education and early 14: 277-282.
case detection) on those predictors are necessary to effectively reduce 18. Kassu A, Mengistu G, Ayele B, Diro E, Mekonnen F, et al. (2007) Coinfection
TB-HIV co-infection. and clinical manifestations of tuberculosis in human immunodeficiency virus-
infected and uninfected adults at a teaching hospital, northwest Ethiopia. J
Competing Interests Microbiol Immunol Infect 40: 116-122.
This work was ethically cleared by RPO of Debre Markos University. 19. Datiko DG, Yassin MA, Chekol LT, Kabeto LE, Lindtjørn B (2008) The rate of
TB-HIV co-infection depends on the prevalence of HIV infection in a community.
There is no any competing of interest. No future financial aid was BMC Public Health 8: 266.
received from any organization for publication or other interest.
20. Sume GE, Etogo D, Kabore S, Gnigninanjouena O, Epome SS, et al. (2008)
Sero prevalence of human immunodeficiency virus infection among tuberculosis
Author’s Contributions patients in the Nylon district hospital tuberculosis treatment centre. East Afr
Med J 85: 529-536.
AE and ME: conception and initiation of the study, design,
implementation, analysis and writing. GT and MW: implementation, 21. Sharma SK, Mohan A (2004) Extrapulmonary tuberculosis. Indian J Med Res
and analysis. All authors read and approved the final manuscript. 120: 316-353.
22. Golden MP, Vikram HR (2005) Extrapulmonary tuberculosis: an overview. Am
Acknowledgements Fam Physician 72: 1761-1768.
Our acknowledgements go to A to Tariku Belachew, director of Debre 23. Gebremariam MK, Bjune GA, Frich JC (2011) Lay beliefs of TB and TB/HIV co-
Markos hospital and all members of RPO of Debre Markos University infection in Addis Ababa, Ethiopia: a qualitative study. BMC Res Notes 4: 277.
that facilitating all the bureaucratic procedures smoothly and swiftly. The
24. Central Statistical Agency of Ethiopia (CSA).
authors also thank data collectors, Debre Markos hospital laboratory and
DOTs clinic staffs for their unreserved support during the study period. 25. Amhara National Regional State Health Bureau Fifth National TB Research
Conference.
References
26. Pefura Yone EW, Kuaban C, Kengne AP (2012) HIV testing, HIV status and
1. WHO (2012) Gains in TB control at risk due to 3 million missed patients and outcomes of treatment for tuberculosis in a major diagnosis and treatment
drug resistance. Global tuberculosis report. centre in Yaounde, Cameroon: a retrospective cohort study. BMC Infect Dis
2. WHO (2000) Regional Office for South-East Asia, New Delhi. TB in South-East. 12: 190.
3. Prasad R (2010) Multidrug and extensively drug-resistant TB (M/XDR-TB): 27. Adjei AA, Adiku TK, Ayeh-Kumi PF, Hesse IF (2006) Prevalence of human
problems and solutions. Indian J Tuberc 57: 180-191. immunodeficiency virus infection among tuberculosis suspect patients in Accra,
Ghana. West Afr J Med 25: 38-41.
4. WHO (2010) Tuberculosis country profiles.
28. Houston S, Ray S, Mahari M, Neill P, Legg W, et al. (1994) The association
5. Ministry of Health (2008) National tuberculosis control program in Ethiopia. of tuberculosis and HIV infection in Harare, Zimbabwe. Tuber Lung Dis 75:
220-226.
6. Demissie BS, Solomon AW (2011) Magnitude and causes of childhood
blindness and severe visual impairment in Sekoru District, Southwest Ethiopia:
a survey using the key informant method. Trans R Soc Trop Med Hyg 105:
507-511.
7. Federal Ministry of Health (FMoH): National Consensus Meeting on Single
Point HIV Prevalence Estimate. Palace Hotel, Adama, Ethiopia.
8. Ministry of Health (2010/11-2014/15) Federal Democratic Republic of Ethiopia.
Submit your next manuscript and get advantages of OMICS
9. WHO (2011/2012) Tuberculosis Global Facts.
Group submissions
10. World Health organization (2004) The world health report 2004 - changing
Unique features:
history.
• User friendly/feasible website-translation of your paper to 50 world’s leading languages
11. WHO report (2010) Global tuberculosis control. • Audio Version of published paper
• Digital articles to share and explore
12. Gao J, Zheng P, Fu H (2013) Prevalence of TB/HIV co-infection in countries
Special features:
except China: a systematic review and meta-analysis. PLoS One 8: e64915.
• 300 Open Access Journals
• 25,000 editorial team
• 21 days rapid review process
• Quality and quick editorial, review and publication processing
• Indexing at PubMed (partial), Scopus, EBSCO, Index Copernicus and Google Scholar etc
Citation: Esmael A, Tsegaye G, Wubie M, Endris M (2013) Tuberculosis and • Sharing Option: Social Networking Enabled
Human Immune Deficiency Virus Co-infection in Debre Markos Referral • Authors, Reviewers and Editors rewarded with online Scientific Credits
Hospital in Northwest Ethiopia: A Five Years Retrospective Study. J AIDS Clin • Better discount for your subsequent articles
Res 4: 263. doi: 10.4172/2155-6113.1000263 Submit your manuscript at: http://www.omicsonline.org/submission
J AIDS Clin Res
ISSN:2155-6113 JAR an open access journal Volume 4 • Issue 12 • 1000263
You might also like
- 215067-Article Text-530618-1-10-20210927Document7 pages215067-Article Text-530618-1-10-20210927Yayew MaruNo ratings yet
- Nihpp rs3758745v1Document20 pagesNihpp rs3758745v1Yulia Niswatul FauziyahNo ratings yet
- Tuberculosis Vih EthiopiaDocument9 pagesTuberculosis Vih Ethiopiajulma1306No ratings yet
- The Burden of Bacteriologically Negative TB DiagnosisDocument9 pagesThe Burden of Bacteriologically Negative TB DiagnosisMeiyanti MeiyantiNo ratings yet
- EthiopiaDocument15 pagesEthiopiaVincentius Michael WilliantoNo ratings yet
- 19 Ninan EtalDocument6 pages19 Ninan EtaleditorijmrhsNo ratings yet
- Los Gemelos TerriblesDocument24 pagesLos Gemelos TerriblesNatalia Nohemy SorianoNo ratings yet
- Directly Observed Treatment Short-Course (DOTS) For Tuberculosis Control Program in Gambella Regional State, Ethiopia: Ten Years ExperienceDocument8 pagesDirectly Observed Treatment Short-Course (DOTS) For Tuberculosis Control Program in Gambella Regional State, Ethiopia: Ten Years ExperienceTammy Utami DewiNo ratings yet
- Prevalence and Determinants of Human Immunodeficiency Virus and Tuberculosis Co-Infection at Kampala International University Teaching HospitalDocument6 pagesPrevalence and Determinants of Human Immunodeficiency Virus and Tuberculosis Co-Infection at Kampala International University Teaching HospitalKIU PUBLICATION AND EXTENSIONNo ratings yet
- Jurnal 10 HariantoDocument7 pagesJurnal 10 Hariantoaryzamelindah channelNo ratings yet
- Cohorte 10 PDFDocument7 pagesCohorte 10 PDFLaura MottaNo ratings yet
- Drug-Resistance Patterns of Mycobacterium Among Multi Drug-Resistant Tuberculosis Suspected Patients From EthiopiaDocument16 pagesDrug-Resistance Patterns of Mycobacterium Among Multi Drug-Resistant Tuberculosis Suspected Patients From EthiopiaaulianmediansyahNo ratings yet
- Epidemiological and Clinical Correlates of Malaria-Helminth Co-Infections in Southern EthiopiaDocument7 pagesEpidemiological and Clinical Correlates of Malaria-Helminth Co-Infections in Southern EthiopiaAdrian KhomanNo ratings yet
- Ali2016 Article OutcomesOfTBTreatmentInHIVCo-iDocument9 pagesAli2016 Article OutcomesOfTBTreatmentInHIVCo-itishaNo ratings yet
- Influential Factors in TBHIV Co-Infection Among HIV-Positive Patients at Jinja Regional Referral Hospital, UgandaDocument12 pagesInfluential Factors in TBHIV Co-Infection Among HIV-Positive Patients at Jinja Regional Referral Hospital, UgandaKIU PUBLICATION AND EXTENSIONNo ratings yet
- 1 - Incidence of Tuberculosis Meningitis in A High HIV Prevalence Serie de Caso 2018 (Modelo para o Trabalho)Document9 pages1 - Incidence of Tuberculosis Meningitis in A High HIV Prevalence Serie de Caso 2018 (Modelo para o Trabalho)SERGIO LOBATO FRANÇANo ratings yet
- s12879-019-4651-6Document13 pagess12879-019-4651-6n.m.l.h.189No ratings yet
- Five Years Malaria Trend Analysis in Woreta Health Center, Northwest EthiopiaDocument8 pagesFive Years Malaria Trend Analysis in Woreta Health Center, Northwest EthiopiaMegbaruNo ratings yet
- MDR Somalia EID March 2013Document3 pagesMDR Somalia EID March 2013hirsi200518No ratings yet
- Irini Sereti, Gregory P. Bisson, Graeme Meintjes - HIV and Tuberculosis - A Formidable Alliance-Springer International Publishing (2019)Document347 pagesIrini Sereti, Gregory P. Bisson, Graeme Meintjes - HIV and Tuberculosis - A Formidable Alliance-Springer International Publishing (2019)alicia albujarNo ratings yet
- Intestinal Parasitic Infections and Associated Factors Among People Living With HIV/AIDS in Ethiopia: A Systematic Review and Meta AnalysiDocument17 pagesIntestinal Parasitic Infections and Associated Factors Among People Living With HIV/AIDS in Ethiopia: A Systematic Review and Meta AnalysiminiwhiteyNo ratings yet
- Document PDFDocument7 pagesDocument PDFnur fadlilahNo ratings yet
- Directly Observed TreatmentDocument9 pagesDirectly Observed TreatmentNovelia CarolinNo ratings yet
- Epidemiology of Tuberculosis and HIV Coinfections in Singapore, 2000 2014Document6 pagesEpidemiology of Tuberculosis and HIV Coinfections in Singapore, 2000 2014jessicaNo ratings yet
- Research On Prevalence of TB FinalDocument9 pagesResearch On Prevalence of TB FinalBontuNo ratings yet
- Costs and Cost-Effectiveness of Gene Xpert Compared To Smear Microscopy For The Diagnosis of Pulmonary Tuberculosis Using Real-World Data From Arsi Zone, EthiopiaDocument10 pagesCosts and Cost-Effectiveness of Gene Xpert Compared To Smear Microscopy For The Diagnosis of Pulmonary Tuberculosis Using Real-World Data From Arsi Zone, Ethiopiadiana.alyNo ratings yet
- Kaforou 2013Document18 pagesKaforou 2013Ellyana PerwitasariNo ratings yet
- Global Evidence Directing Regional Preventive Strategies in Southeast Asia For Fighting TBorHIVDocument12 pagesGlobal Evidence Directing Regional Preventive Strategies in Southeast Asia For Fighting TBorHIVAura NirwanaNo ratings yet
- Diagnosis & Treatment of Tuberculosis in HIV Co-Infected PatientsDocument16 pagesDiagnosis & Treatment of Tuberculosis in HIV Co-Infected PatientsdevisilalahiNo ratings yet
- Original Article: Magnitude of Cryptococcal Antigenemia 369Document6 pagesOriginal Article: Magnitude of Cryptococcal Antigenemia 369MegbaruNo ratings yet
- Falla InmunologicaDocument10 pagesFalla InmunologicaAlejandra OrtizNo ratings yet
- A Retrospective Study of Pulmonary Tuberculosis (PTB) Prevalence Amongst Patients Attending Infectious Diseases Hospital (Idh) in Kano, NigeriaDocument6 pagesA Retrospective Study of Pulmonary Tuberculosis (PTB) Prevalence Amongst Patients Attending Infectious Diseases Hospital (Idh) in Kano, NigeriaJenness VillanuevaNo ratings yet
- Fungi: The Burden of Fungal Infections in EthiopiaDocument14 pagesFungi: The Burden of Fungal Infections in EthiopiaclaraNo ratings yet
- Undiagnosed Tuberculosis in Patients With HIV Infection Who Present With Severe Anaemia at A District HospitalDocument6 pagesUndiagnosed Tuberculosis in Patients With HIV Infection Who Present With Severe Anaemia at A District HospitalDian EsthyNo ratings yet
- Researcharticle Open AccessDocument12 pagesResearcharticle Open Accesswosen wondNo ratings yet
- BMC Public Health: Risk Factors For Pulmonary Tuberculosis: A Clinic-Based Case Control Study in The GambiaDocument7 pagesBMC Public Health: Risk Factors For Pulmonary Tuberculosis: A Clinic-Based Case Control Study in The Gambiapuskesmas beloNo ratings yet
- Typhoid Fever in Children in Africa : ViewpointDocument9 pagesTyphoid Fever in Children in Africa : ViewpointFaiz Yunanto MangoendiprodjoNo ratings yet
- Knowledge, Health Seeking Behavior and Perceived Stigma Towards Tuberculosis Among Tuberculosis Suspects in A Rural Community in Southwest EthiopiaDocument7 pagesKnowledge, Health Seeking Behavior and Perceived Stigma Towards Tuberculosis Among Tuberculosis Suspects in A Rural Community in Southwest EthiopiaAqsha RamadhanisaNo ratings yet
- Epidemiological Risk Factors For Adult Dengue in Singapore: An 8-Year Nested Test Negative Case Control StudyDocument9 pagesEpidemiological Risk Factors For Adult Dengue in Singapore: An 8-Year Nested Test Negative Case Control StudydouwesdNo ratings yet
- Tuberculosis Recurrence After Completion Treatment in A European City - Reinfection or Relapse?Document8 pagesTuberculosis Recurrence After Completion Treatment in A European City - Reinfection or Relapse?tishaNo ratings yet
- 1201 Sanchez Padilla High Prevalence of Multidrug Resistant Tuberculosis Swaziland 2009 2010 Emerging Infectious Diseases 18 1Document9 pages1201 Sanchez Padilla High Prevalence of Multidrug Resistant Tuberculosis Swaziland 2009 2010 Emerging Infectious Diseases 18 1dewi ayu wulandariNo ratings yet
- Articles: BackgroundDocument10 pagesArticles: BackgroundEgi NabilaNo ratings yet
- Burden and Consequences of Tuberculosis Among HIV-Infected Individuals Insights From The Itojo Hospital HIV Clinic in Ntungamo DistrictDocument8 pagesBurden and Consequences of Tuberculosis Among HIV-Infected Individuals Insights From The Itojo Hospital HIV Clinic in Ntungamo DistrictKIU PUBLICATION AND EXTENSIONNo ratings yet
- Viral Hepatitis: Acute HepatitisFrom EverandViral Hepatitis: Acute HepatitisResat OzarasNo ratings yet
- Factors Impacting Tuberculosis Treatment Adherence in Rural TurkeyDocument7 pagesFactors Impacting Tuberculosis Treatment Adherence in Rural TurkeyAnonymous QPXAgjBwNo ratings yet
- Jurnal 9Document9 pagesJurnal 9Fida NadhirNo ratings yet
- Tmi 12919Document10 pagesTmi 12919Andi Nur AiynunNo ratings yet
- Pro (Ing3Document17 pagesPro (Ing3ilhamNo ratings yet
- Malaria Vs DBDDocument9 pagesMalaria Vs DBDade hajizah br ritongaNo ratings yet
- Introduction PartDocument4 pagesIntroduction PartZemetu Gimjaw AlemuNo ratings yet
- Adiutarini 3Document7 pagesAdiutarini 3Eva Tirtabayu HasriNo ratings yet
- Tuberculosis: A Global Health Problem: EditorialDocument3 pagesTuberculosis: A Global Health Problem: EditorialzihanNo ratings yet
- Paired Matched Case Control Study ChinaDocument12 pagesPaired Matched Case Control Study ChinaBadal BhandarkarNo ratings yet
- Bacteriological Prevalence Tuberculosis Among Children Seen Health Facilities Nasarawa State Nigeria 2576 8484 EAST 18 121Document5 pagesBacteriological Prevalence Tuberculosis Among Children Seen Health Facilities Nasarawa State Nigeria 2576 8484 EAST 18 121fatimakh462No ratings yet
- Hypoglycemia and Anemia Associated With Malaria Among Pregnant Mothers Living With HIV Attending Aminu Kano Teaching Hospital, Kano State-NigeriaDocument6 pagesHypoglycemia and Anemia Associated With Malaria Among Pregnant Mothers Living With HIV Attending Aminu Kano Teaching Hospital, Kano State-NigeriaUMYU Journal of Microbiology Research (UJMR)No ratings yet
- Malaria TselemtiDocument18 pagesMalaria TselemtiMegbaruNo ratings yet
- The Aetiology and Antibiotic Management of Community-Acquired Pneumonia in Adults in Europe: A Literature ReviewDocument15 pagesThe Aetiology and Antibiotic Management of Community-Acquired Pneumonia in Adults in Europe: A Literature ReviewPutu Sukma RadhanaNo ratings yet
- Jia2 25392Document10 pagesJia2 25392Herpriiy BatukhNo ratings yet
- ArticleDocument9 pagesArticleNaresh Babu.TNo ratings yet
- Sepsis Proposal1Document34 pagesSepsis Proposal1Appiah Peter OforiNo ratings yet
- UKN Obstetri Maret 2021Document18 pagesUKN Obstetri Maret 2021anton suponoNo ratings yet
- Pyloric Stenosis CaseDocument54 pagesPyloric Stenosis CaseMaria0% (1)
- What Causes CancerDocument2 pagesWhat Causes CancerSilla, KyshiaNo ratings yet
- Risk AssesmentDocument2 pagesRisk AssesmentChristopher Stewart0% (1)
- Instruction: Read The Questions Comprehensively and Choose The Letter That Best Correspond To TheDocument5 pagesInstruction: Read The Questions Comprehensively and Choose The Letter That Best Correspond To TheMaren Pendon100% (2)
- New Nursing Diagnoses 2012-2014Document11 pagesNew Nursing Diagnoses 2012-2014CarmenNoemiSantos100% (1)
- Sub - Medical Surgical Nursing: Assignment On CVP MonitoringDocument11 pagesSub - Medical Surgical Nursing: Assignment On CVP Monitoringkamini ChoudharyNo ratings yet
- Pir June 2015, Volume 36, Issue 6Document55 pagesPir June 2015, Volume 36, Issue 6Angie LuperdiNo ratings yet
- Bakery Workers' Exposure to Flour Dust and Respiratory HealthDocument178 pagesBakery Workers' Exposure to Flour Dust and Respiratory HealthShiji Sadiq LukmanNo ratings yet
- Biology Notes CHPTR 12Document14 pagesBiology Notes CHPTR 12Wan HasliraNo ratings yet
- Thesis Parkinson DiseaseDocument8 pagesThesis Parkinson Diseaseaouetoiig100% (1)
- Critical Values List: Arterial Blood GasesDocument3 pagesCritical Values List: Arterial Blood Gasesiq_dianaNo ratings yet
- Prostate CancerDocument5 pagesProstate CancerBrilliant Osai-OyeteNo ratings yet
- Real World' Evidence: A Dangerous DelusionDocument32 pagesReal World' Evidence: A Dangerous DelusionNational Press FoundationNo ratings yet
- Efficacy of Levetiracetam in The Treatment Of.21Document3 pagesEfficacy of Levetiracetam in The Treatment Of.21andiNo ratings yet
- DR Arpit Agarwal Pharma Capsule 3 Drugs For GITDocument33 pagesDR Arpit Agarwal Pharma Capsule 3 Drugs For GITarpitsnmcNo ratings yet
- Periprosthetic Fractures of The Proximal Femur Beyond The Vancouver ClassificationDocument8 pagesPeriprosthetic Fractures of The Proximal Femur Beyond The Vancouver ClassificationDavidBeatonComuladaNo ratings yet
- Bovine Ephemeral Fever: ImportanceDocument4 pagesBovine Ephemeral Fever: ImportanceAamir AliNo ratings yet
- Leukemia in Children: 1 Rahul Dhaker, Asst. Professor, RCNDocument41 pagesLeukemia in Children: 1 Rahul Dhaker, Asst. Professor, RCNRahul DhakerNo ratings yet
- Drug StudyDocument13 pagesDrug StudyGi Ey ElNo ratings yet
- Allied Health ProfessionalsDocument19 pagesAllied Health ProfessionalsReihnard RosariioNo ratings yet
- Case No. 4: GLOCOSE 6 Phosphate DeficiencyDocument5 pagesCase No. 4: GLOCOSE 6 Phosphate DeficiencyReham QueNo ratings yet
- Paeds One Word-1-3Document18 pagesPaeds One Word-1-3Killian SibzNo ratings yet
- Data Penyelidikan 2009Document86 pagesData Penyelidikan 2009Alex Phang Kean ChangNo ratings yet
- High quality blood agar production with MEDIAJET and DOSE ITDocument2 pagesHigh quality blood agar production with MEDIAJET and DOSE ITBenjamin TantiansuNo ratings yet
- 2023 Complications and Treatment Errors in Peri-Implant Hard Tissue ManagementDocument22 pages2023 Complications and Treatment Errors in Peri-Implant Hard Tissue Managementmatias cofreNo ratings yet
- Yoga Mudras For Balancing Dosha (Vata, Pitta, & Kapha) : Home Articles Mudras Poses PranayamaDocument26 pagesYoga Mudras For Balancing Dosha (Vata, Pitta, & Kapha) : Home Articles Mudras Poses PranayamaDanaNo ratings yet
- HRSL ScriptsDocument3 pagesHRSL ScriptsFolajimi AdebowaleNo ratings yet
- Palm Grass Blood Clot StudyDocument20 pagesPalm Grass Blood Clot StudyRichele QuilantangNo ratings yet
- CASE STUDY (Gastro)Document3 pagesCASE STUDY (Gastro)Jake Yvan DizonNo ratings yet