Professional Documents
Culture Documents
Oral Health & Dental Science
Uploaded by
imane boujoualOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Oral Health & Dental Science
Uploaded by
imane boujoualCopyright:
Available Formats
Research Article ISSN 2639-9490
Research Article Oral Health & Dental Science
Effectiveness of Analgesics in the Treatment of Temporomandibular
Dysfunction: A Systematic Literature Review
Boujoual I1*, Rhattas S2, Amessegher F2, Gamrani M3 and Andoh A2
1
Department of fixed prosthodontics, Faculty of dentistry, Hassan
II University Casablanca, Morocco. *
Correspondence:
Boujoual I., Department of fixed prosthodontics, Faculty of
Unit of fixed prosthodontics, University Hospital Ibn Rochd,
2
dentistry, Hassan II University Casablanca, Morocco.
Faculty of dentistry, Hassan II University Casablanca, Morocco.
Received: 09 Jun 2022; Accepted: 11 Jul 2022; Published: 16 Jul 2022
3
Private exercise, Morocco.
Citation: Boujoual I*, Rhattas S, Amessegher F, et al. Effectiveness of Analgesics in the Treatment of Temporomandibular Dysfunction:
A Systematic Literature Review. Oral Health Dental Sci. 2022; 6(2); 1-9.
ABSTRACT
Introduction: Temporo-mandibular dysfunctions correspond to a defect adaptation of the manducatory apparatus.
Different therapeutic methods are available for the treatment of these pathologies: Splints, physical therapies,
occlusal therapies, surgery or pharmacological treatments. The objective of our work is to analyze the clinical
effectiveness of analgesics in the treatment of disorders of the masticatory apparatus by applying the Evidence
approach Based Dentistry.
Methods: The collection of data from the literature scientific was carried out among the production that appeared
during the period from 2011 to 2021. The documentary research was carried out using accessible databases via
the Internet namely MEDLINE, ELSEVIER and Cochrane Database of Systematic through their PubMed, Science
Direct and Cochrane library search engines, as well as the website Google Scholar. A bottom-up manual search
covering the same study period was carried out in order to enrich our bibliography. The writing of this systematic
review followed the guidelines of the PRISMA Statement (Preferred Reporting Items for Systematic Reviews and
Meta-Analyses).
Results: 9 relevant randomized clinical trials were selected after critical reading guided by the CASP type reading
grids. The items have been listed in 4 categories according to the route of administration of the analgesics (topical
route, oral, intramuscular route and intra-articular route) and classified in tables according to the PICO criteria
(Participants/Interventions/Comparison/Results “Outcomes”). The results of our study show a significant reduction
in the intensity of the pain and the rates of cytokines as well as a significant increase in maximum mouth opening.
Conclusion: The use of analgesics increases the efficacy of treatment by decreasing pain intensity and cytokine
levels, through both their analgesic and anti-inflammatory actions. This efficacy is similar for both levels II and III.
However, additional long-term clinical studies with a larger sample size are needed to confirm the data collected
and to further explore the effect of analgesics in the treatment of TMDs.
Keywords components; a passive articular component (temporomandibular
Neuromuscular system, Temporomandibular joint Disorders, and occlusal) and an active muscular component, which
Pharmacological therapies. maintain reciprocal relations of influence between them, in
coordination with the neuromuscular system [1]. The health of
Introduction this apparatus is maintained by a coordinated, interdependent, and
The manducatory apparatus is a system formed by several harmonious functioning of its determinants. A lack of adaptation
Oral Health Dental Sci, 2022 Volume 6 | Issue 2 | 1 of 9
of this apparatus can be responsible for several pathologies Materials and Methods
(osteoarthritis, disc dislocation, myofacial pain, musculo-articular Research Strategy
pathologies...). The absence of a systematic taxonomy for all The literature search was based on scientific databases accessible
these disorders means that they are grouped under global terms via the Internet. An electronic search was carried out using the
such as "craniomandibular dysfunctions or disorders (CMD)", or international databases MEDLINE, and ELSEVIER through
"temporomandibular disorders". their search engines; respectively PubMed, Science Direct,
as well as the Google Scholar site. The collection of data from
Temporomandibular joint Disorders (TMD). This term is the scientific literature was carried out among the scientific
defined as the symptomatic expression of a pathology that can be production that appeared during the period from January 2011
originating from muscles, joints, or a combined one. This includes to January 2021. The electronic search strategy was carried
anatomical, histological, and functional abnormalities of the out using the following keywords: Temporomandibular joint
muscular and articular systems [2]. The three characteristic signs disorders, Craniomandibular disorders, Analgesics, Analgesics,
of these disorders are noise (clicking, clenching, clacking), pain opioids, Analgesics, and Non-Narcotic. These terms were then
(aching), and dyskinesias [3]. The multitude of symptoms of these combined through Boolean operators to arrive at the Boolean
disorders results from the great number and the intricacy of the equations below: "Temporomandibular joint disorders" (Mesh)
biological, structural, and psychosocial cofactors implied in the And" Analgesics ˝(Mesh), "Craniomandibular disorders" (Mesh),
triggering and evolution of these dysfunctions [4]. And "Analgesics" (Mesh), "Temporomandibular joint disorders"
(Mesh) And "Analgesics, Opioid" (Mesh), "Temporomandibular
This multifactorial character makes therapy and prognosis more joint disorders" (Mesh) And "Analgesics, Non-Narcotic" (Mesh).
complicated and leads the patient to under diagnosis or therapeutic
wandering. Global treatment aims at reducing pain, improving Eligibility Criteria
function, and acting on psychism. For this purpose, different Inclusion Criteria: Articles included in our literature search were
therapeutic approaches are available, such as maxillofacial randomized controlled trials that met all of the following inclusion
physiotherapy [5], therapeutic education, cognitive-behavioral criteria: studies with a publication date between 2011 and 2021,
therapies, hypnosis [6], relaxation, the use of occlusal orthoses written in French or English, human studies, low dropout rate,
[7], and pharmacological therapies (analgesics, anxiolytics, identical follow-up between groups, adequate statistical analysis.
anti-inflammatories, muscle relaxants, antidepressants, etc.)
Many clinical studies on peripheral opioid analgesia have been Exclusion Criteria
developed in patients with persistent joint pain, a problem of Articles were excluded if they met any of the following criteria:
major relevance and prevalence. Of these, temporomandibular studies with publication dates before 2011, animal studies, anti-
joint (TMJ) pain has long been recognized as one of the most inflammatory studies, case series, retrospective studies, literature
difficult types of joint pain to treat [8]. reviews, letters to the editor, and studies funded by manufacturers.
The most commonly considered analgesics for oral administration Literature Selection Strategy
are codeine and oxycodone, with hydromorphone reserved for Two readers to reduce the risk of excluding relevant studies,
severe intractable pain. If oral administration is not a reasonable minimize the risk of judgment error and subjectivity, and ensure
option, patches may be considered for those trained in its use [9]. the reproducibility of results performed study selection and
Parenteral injection of analgesics (intramuscular, intradermal, quality assessment independently. This approach was also used
intra-articular, etc.) is most commonly used for the treatment for data extraction, which is particularly prone to error. In case
of TMD, especially in combination with arthrocentesis [10]. of discrepancies, the articles concerned were discussed between
Analgesics act by binding to specific cell receptors in the central the two readers to reach a consensus. The initial electronic search
and peripheral nervous systems [11], which play a key role in was carried out on various search engines. The selection was made
modulating pain and inflammation [12]. There is recent evidence initially by two readers (B.I., G.M.) based on titles and abstracts.
for the existence of a peripheral subtype of the μ-opioid receptor The same readers according to the eligibility criteria analyzed
in TMJ tissues [13], thus explaining the possible benefits of this the selected articles. The Critical Appraisal Skills Programme
treatment modality. However, many theories consider the use (CASP) critical reading grids (Appendix 1) guided the full-text
of analgesics to be only a symptomatic and palliative treatment; reading. This second step allowed the final selection of potentially
without treating the cause, relieving pain will eventually reappear. eligible articles. After having explored all the electronic databases
This lack of consensus concerning the place of analgesics in the mentioned above using search engines, the bibliography of
management of disorders of the manducatory apparatus causes the selected articles was finally studied to detect other articles
practitioners to be confused about the use of these molecules. In following the same path as our study.
light of the above, this thesis proposes to conduct a systematic
review by applying the Evidence-Based Dentistry approach, Risk of Bias (Methodological Quality Assessment)
with the main objective of evaluating the clinical effectiveness of The critical reading of the articles was based on 2 tools for
analgesics in the management of manducatory dysfunction. assessing methodological quality. The first tool is the CASP
Oral Health Dental Sci, 2022 Volume 6 | Issue 2 | 2 of 9
checklist (Critical Appraisal Skills Programme): this tool proposes of intra-articular analgesics. This category was subdivided into
11 questions. The first two questions are filter questions, to which two other categories according to the variables studied: Analysis
the answer is quick. If the answer is positive, it is appropriate of cytokine changes and Analysis of pain intensity, maximal
to move on to the next questions. The second one is the risk of mouth opening, clicking sounds, and/or mandibular movements.
bias assessment from the "Cochrane Handbook for Systematic The description of the articles included in our review was carried
Reviews of Interventions" adapted and updated by Higgins and out according to the PICO criteria (Participants/ Intervention/
colleagues in 2011. It includes Selection bias: Which refers to Comparison/ Outcomes).
systematic differences in the baseline characteristics of the groups
being compared. To limit the risk of selection bias, the method for Risk of Bias in Included Studies
generating the randomization sequence must be appropriate and Bias was assessed using the tool recommended by the Cochrane
the principle of secret assignment must be respected. Performance Handbook for Systematic Reviews of Interventions "The
bias: Refers to systematic differences between groups in the care of Handbook" online guide adapted by Higgins et al. in 2011.45
participants. To limit the risk of performance bias, participants and this tool is used to estimate the risk of bias in meta-analyses and
the health care team should be blinded to the interventions received. systematic reviews of clinical randomized trials.
Detection bias: Refers to systematic differences between groups in
the way the outcome is assessed. To limit the risk of detection Discussion
bias, the evaluator should be blinded. Attrition bias: Refers to Treatment's Effect on Pain
systematic differences between groups regarding withdrawals of The visual analog scale was used to identify pain intensity, the
participants from the trial. Publication and selective reporting bias: standard method in assessing pain and responses to analgesic
Refers to systematic differences between reported and unreported treatment because it is simple, reproducible, sensitive, and linear.
outcomes. Other biases: In addition, other sources of bias are All studies concluded that analgesics were clinically effective in
relevant in some circumstances. For each article, the risk of bias managing pain in these patients. However, these results should
estimate was divided into 3 categories "High risk," "Minimal risk," be analyzed with caution since this method may be a source of
and "Uncertain risk." The judgment criteria for estimating the risk biases, since patients may be inclined to indicate a greater or lesser
for each bias were listed in the risk of bias assessment tables. degree of satisfaction with their treatment if it is nominative.
Arthrocentesis is a minimally invasive surgical technique that
Writing Protocol essentially rinses the joint by placing needles into the upper
The writing of this thesis work followed the guidelines of the joint compartment. Introduced by Nitzan et al. in 1991 [23],
PRISMA Statement "Preferred Reporting Items for Systematic this procedure has quickly gained notoriety among practitioners
reviews and Meta-Analyses" considered as a writing guide treating TMJ disorders. The use of intra-articular medications after
according to Moher et al. in 2009, helping authors to write their arthrocentesis has gained popularity over the past decade. Several
systematic literature reviews or meta-analyses by evaluating all clinical trials have attempted to improve the efficacy of TMJ
clinical trials in response to a specific clinical question. arthrocentesis by injecting corticosteroids, sodium hyaluronate,
platelet-rich plasma, etc. into the joint space.
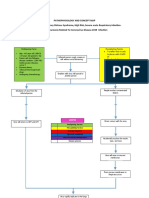
Results Experience with arthroscopic procedures on knee joints has shown
The results of our search are presented in the form of a flow
that intra-articular analgesics can be injected at the end of the
chart (Figure 1) exposing the choice of the selected articles. A procedure to provide early pain relief [24] and has inspired several
general description of the studies will be highlighted in a table, clinicians to evaluate its use after TMJ arthrocentesis.
and then the articles will be categorized according to the route
of administration, and classified in tables according to the PICO The systematic reviews by Siyan Liu and colleagues [25],
criteria (Participants/Interventions/Comparison/Outcomes). Venkatesan Gopalakrishnan and colleagues [10] plus the meta-
analysis by Yan Liu and colleagues [26]. Also confirmed that
Selection of Articles intra-articular injection of analgesics had a positive effect on pain
Flow Chart reduction after arthrocentesis, considering that the presence of
The selection of the articles followed several steps presented in the intra-articular opioid receptors located in the synovium makes it
form of a flow chart suggested by "The PRISMA Statement. possible to obtain a powerful, direct, and lasting analgesic action
of the opioids at the affected site, bypassing their central effect.
Figure 1: Flow chart illustrating the different stages of publication
selection in the systematic literature review. Ganti S. et al. [15] state that the use of tramadol in pain control
began long ago, and over the past four decades, it has been the drug
Descriptive Results of choice for controlling severe pain disorders [27]. However, the
Description of results according to PICO criteria: results of their study show that its efficacy is still lower than the
The studies were classified into four main categories: Administration combination of glucosamine and chondroitin sulfate. These results
of topical analgesics, Administration of oral analgesics, seem to agree with those of Damlar I. et al. [28].
Administration of intramuscular analgesics, and Administration
Oral Health Dental Sci, 2022 Volume 6 | Issue 2 | 3 of 9
Table 1: Description of studies according to PICO criteria.
Route of
Author/Year Population Intervention Comparison Outcomes
administration
-Experimental and Global Pain:
Significant increase in VAS scores for
capsaicin-treated subjects compared
to vehicle-treated subjects, the VAS
measures during 1 to 7 days were
significantly greater in the control
-Size:
vehicle group than in the capsaicin
70 Subjects Capsaicin powder was Between two groups:
treatment group (P = 0.001). The VAS
-Sexe: compounded into an 8% (w/v) 1- Healthy control subjects:
ratings were significantly lower for the
Effect of topical Campbell B.K. topical emollient cream base; - 30: capsaicin cream
capsaicin-treated subjects over the 1-wk
analgesic et al. 2017 [14] Female only - 24: vehicle cream
post-application period (P = 0.033).
administration The vehicle cream was the same 2- Sick subjects :
-Thermal Pain Threshold: Significant
-Age: topical solution but contained no - 8: Capsaicin cream
decrease in thermal pain threshold at
capsaicin. - 8: Vehicle cream
2 h after application of the cream in
18 to 65 years old
the 2 groups treated with capsaicin, no
significant difference in the 2 groups
treated with the vehicle cream. -Pressure
Pain Threshold: No significant change
in pressure pain threshold values for all
groups.
-Pain VAS score: Significant decrease
The patients were divided in pain in all 3 groups (P<0.05) -MMO:
Conscious sedation was
into three groups of 20 Significant increase in MMO in all 3
performed, and Normal saline
each. Group I received groups. -IL-6: Significant decrease in
lavage was performed in the upper
a combination of 1.5 g of IL-6 levels in-group I, no significant
-Size: 60 subjects joint space. This sample was used
glucosamine and 1.2 g of difference from baseline in groups II
Effect of oral -Sexe: to assess the level of IL–6, IL–1ß,
Ganti Srivinas chondroitin sulfate per day and III. - IL-1β: - Significant decrease
analgesic 30 males, TNF–α, and PGE2. Thereafter,
et al. 2018 [15] and group II received 50 for group I, Significant increase for
administration 30 females each group of patients received the
mg tramadol HCL peroral. group II, No significant difference for
-Age: undetermined designated test molecule
Group III received Sodium group III. -TNF-α: The difference was
- The same procedure was
hyaluronate 10 mg/ml, 2 ml not statistically significant in the three
repeated after 8 weeks to obtain
injection syringe on each groups. -PGE2: The difference was
synovial fluid.
joint. not statistically significant in the three
groups.
• Masseter level:
- VAS scores: Statistically significant
difference between patients treated
with morphine 5mg and those treated
with saline. No statistically significant
difference between the morphine 5mg
The dose of morphine used for
group and the lidocaine group. Morphine
TMJ treatments ranges from 0.1
5 groups were randomly 1.5mg did not significantly reduce mean
mg to 10 mg.
divided: scores until after 48 hours, whereas
A single injection of the test
-GI: Masseter saline morphine 5mg resulted in an immediate
-Siez: 51 Subjects molecule was made over 10
Effect of Soo-Kyung -GII: Morphine 1,5mg reduction in scores that persisted
-Sexe: 27 Males, seconds.
intramuscular Kang et al. 2018 masseter throughout the observation period.
24 Females -Age: - At the most painful site of the
administration of [16] -GIII: Morphine 5mg -PPT: Aucune différence statistiquement
between 20–59 superficial masseter muscle,
analgesics masseter significative entre tous les groupes.
years old. - At the level of the trapezius
-GIV: Lidocaine masseter -PPtol: Overall significant increase in
muscle contralateral to the painful
-GV: Morphine 5mg PPtol measures for groups 1, 2, and 3 but
masseter,
trapezium not in group 4. No statistically significant
Follow-up: 24 and 48 hours after
difference between the different groups.
the injection.
• Trapezius level:
Intramuscular injection of 5 mg
morphine into the contralateral trapezius
did not result in significant changes in
VAS, PPT, and PPtol scores measured at
the painful masseter muscle.
Oral Health Dental Sci, 2022 Volume 6 | Issue 2 | 4 of 9
After Preparation of the operative
40 patients were divided
site and collection of synovial - After one month, there was a significant
randomly into two equal
fluid aspirate. Hydraulic pressure decrease in IL-6 levels in both groups.
groups with chief complaints
-Size: 40 Subjects was created by injecting 2 ml of there was a statistically significant
El-Gerby Y.M. of limited mouth opening,
saline solution, The joint was then difference between the two groups: the
et al. 2015 [17] TMJ pain, and clicking sounds
-Age: undetermined washed with 300 to 500 ml of maximum decrease in IL-6 was observed
in the TMJ
saline solution. In the end, 1 ml of in patients in group I who received a
-GI: Tramadol
the test molecule was injected. tramadol injection
-GII: sodium hyaluronate
Follow-up: after one month
-VAS scores: After 3 days, there was
no statistically significant difference
between the two groups, however, after
1 month and 6 months Group II showed
The tested joints were a statistically significantly higher mean
After the Preparation of randomly divided into two percentage decrease in VAS than Group
the operative site, the groups: -Group I: injection I. -MMO: Pre-operatively, after 3 days
auriculotemporal nerve block was of 1 ml. of commercially and after 6 months, Group II showed
performed with 0.5 ml of the local available COX – 2 inhibitors: statistically significantly higher mean
-Size 24 subjects anesthetic solution. Hydraulic Groupe I-A: disc displacement MMO than Group I, however, there was
-Sexe:6 Males,18 pressure was created by injecting with reduction, Group I-B: no statistically significant difference
Tamer Hamed
Females 2 ml of saline solution, The joint disc displacement without between the two groups after 1 month.
A. 2012 [18]
-Age: between was then washed with 300 to 500 reduction -Group II: - Lateral excursion: Pre-operatively,
20–59 years old ml of saline solution. In the end, Injection of 1 ml. of tramadol there was no statistically significant
1 ml of the test molecule was hydrochloride: Groupe II- difference between the two groups,
injected. A: disc displacement with however, after 3 days, after 1 month
Follow-up: 3 days, 1 month, 6 reduction, Groupe II-B: and after 6 months, Group II showed
months disc displacement without statistically significantly higher mean
reduction lateral excursion than Group I.
Effect of intra- Comparing groups 1-A and 1-B as well as
articular groups 2-A and 2-B, the results showed no
analgesic statistically significant differences for any
administration of the variables studied
-After preparation of the operative
- Evaluation of Pain: There was a highly
site, the auriculotemporal nerve
significant reduction in pain score level
block 0.3 to 0.5 ml of an anesthetic
in both groups as in group I was and in
solution was injected and then
group II
the needle was introduced into The selected patients were
-MMO: At six months postoperatively:
the upper joint compartment and divided randomly into two
Mouth opening increased significantly
-Size: 40 Subjects approximately 3.5 ml of anesthetic equal groups :
El-Gerby M et in-group I from (17.30 ± 2.85) to (49.80
-Age: solution was injected. Hydraulic Group I: 20 patients (1ml of
al. 2015 [19] ± 2.19) and group II from (16.70 ± 3.29)
undetermined pressure was created by injecting 2 tramadol)
to (38.15 ± 3.54). The difference between
ml of saline solution; The joint was Group II: 20 patients (1ml
the two groups is statistically significant.
then washed with 300 to 500 ml of sodium hyaluronate)
-Clicking Sound: After six months,
saline solution. In the end, 1 ml of
in the group I clicking was reported at
the test molecule was injected.
25 % while in-group II clicking where
Follow-up: 3 days, 1 month, 6
continuous elevation to 50 %.
months
After the preparation of the
-VAS Scores: Significant decrease in
operative site, local anesthesia
VAS scores during follow-up periods in
was obtained with 2%articaine
Patients were randomly all groups.
hydrochloride, 0.5-1 ml. A needle
divided into 3 groups of 10 Mean VAS scores for pain in mouth
was placed in the upper joint
each: opening in the morphine group decreased
-Size : 30 patients space. After distension of the upper
-GI de control: 1ml of 5% from (7.3±1.6) to (1.2±0.8) and were
-Sexe : 25 Females compartment with 2 ml of Ringer's
Sipahi A. et al. Ringer's lactate. significantly lower than those observed
et 5Males lactate, another needle of the same
2015 [20] -GII: 0.01 g Morphine made in the placebo group during all follow-
-Age : between diameter was placed to provide
up to 10 ml with Ringer's up periods. In the tramadol group:
16–50 years old drainage. The joint was irrigated
lactate change from (7.1±1.7) to (.5±1.8); no
with 60-100 ml of Ringer's lactate,
-G III: 50mg of was mixed statistically significant difference from
one of the needles was removed,
with 1 ml of 5% Ringer's the morphine group.
and the study drug was administered
lactate. -MMO: No significant difference in
through the remaining needle.
maximum mouth opening between the
Follow-up: 15min, 1 month, 3
different groups.
months, 6 months
Oral Health Dental Sci, 2022 Volume 6 | Issue 2 | 5 of 9
- Pain score: Preoperatively and
immediately, post-operative there was
no significant difference between Group
I and II. In the following post-operative
observation times1week, 1 month, and 6
months; there was a significant difference
After preparation of the operative
between both groups (p < 0.0001), with
site, the auriculotemporal nerve
higher values, recorded in group II.
block 0.3 to 0.5 ml of an anesthetic Between two groups of 20
-MMO: Preoperatively and immediately
solution, Hydraulic pressure patients, each randomly
-Size: 40 patients post-operative there was no significant
was created by injecting 2 ml of divided:
Fayed M. et al. -Sexe: 20 F and difference between Group I and II. In
saline solution; The joint was then Group I: Intra-articular
2016 [21] 20 H the following post-operative observation
washed with 300 to 500 ml of injection of 1ml fentanyl
-Age: between times 1 week, 1 month, and 6 months;
saline solution. In the end, 1 ml of Group II: Intra-articular
2°–34 years old there was a significant difference
the test molecule was injected. injection of 1ml of Sodium
between both groups, with higher values
Follow-up: Immediately after the hyaluronate
recorded in group I (p < 0.0001).
procedure, at1 week, 3 months,
-Mandibular functions: Preoperatively
and 6 months.
and immediately post-operative there
was no significant difference between
Group I and II. In the following post-
operative observation times1week, 1
month, and 6 months; there was a greater
mean value in group I.
-After the Preparation
-Pain score: After 6 months: Statistically
of the operative site, the
significant difference between the two
auriculotemporal nerve block
groups; greater reduction in pain score in
was performed with 0,3-0,5 ml
the group I
of the local anesthetic solution. Between two randomly
-Size: 40 patients -MMO: Statistically significant
Al-Kisbi A.M. Hydraulic pressure was created by divided groups:
-Sexe: Females and difference between the two groups;
et al. 2017 [22] injecting 2 ml of saline solution; -Group I: Butorphanol tartrate,
males greater mouth opening was recorded in
The joint was then washed with -Group II: Sodium
the group I
200 ml of saline solution. In Hyaluronate
-Clicking sound: After 6 months:
the end, the test molecule was
Statistically significant difference; more
injected.
patients reported clicking In-group II.
Follow-up: 1 week, then 1, 3, and
6 months after the procedure.
VAS: Visual analog scale, MMO: Maximum mouth opening, TMJ: Temporomandibular joint.
Table 2: Risk of Bias of the Included Studies.
Secret
Study Randomization Blind Procedures Follow-up Risk of bias
assignment
Ganti Srivinas et al. [15] Yes (Not clear) Not clear Not clear Yes Uncertain
Yes (Computer program for generating
Soo-Kyung Kang et al. [16] Yes Oui Yes Low
numbers)
El-Gerby M. et al. [17] Yes (Not clear) Not clear Not clear Yes Uncertain
Tamer Hamed A. [18] Yes (Not clear) Not clear Not clear Yes Uncertain
El-Gerby M. Et al. [19] Yes (Not clear) Not clear Not clear Yes Uncertain
Sipahi A. et Coll. [20] Yes (Not clear) Yes Yes Yes Low
Fayed H.T.A. M. et al. [21] Yes (Not clear) Not clear Not clear Yes Uncertain
Al- Kibsi Taghreed A.M. et al. [22] Yes (Not clear) Not clear Not clear Yes Uncertain
Campbell B.K. et al. [14] Yes (Random number generation program) Yes Yes 2 appropriate exclusions Low
On another hand, we have Sipahi A. et al. trial [20], whose into the trapezius muscle contralateral to the painful masseter to
results showed that the pain scores were lower in the morphine determine whether intramuscular morphine produces analgesic
group. This could be explained by the greater analgesic efficiency responses via the systemic effect. Furthermore, the high dose
of morphine compared to tramadol. However, there was no of morphine (5 mg) used in this study produced no change in
statistically significant difference between these values, which masseter pain and tenderness responses when administered into
supports the results of Christoph T. et al. [29] who inferred that the remote muscle, ruling out the possibility of systemic effects.
morphine and tramadol had a similar effect on nociceptive pain This was confirmed by Kapral S. et al. [30] who proved through
although morphine was more potent. a clinical trial carried out on 60 patients that the analgesic effect
of parenterally administered analgesics is not due to systemic
In the study by Kyang SK. et al. [16], morphine was also injected effects.
Oral Health Dental Sci, 2022 Volume 6 | Issue 2 | 6 of 9
Through the clinical trial conducted by Campbell and Coll [14], it were detected together, there was a high probability of such bone
is possible to stipulate that the use of a co-antalgic has proven its changes.
effectiveness in pain management. However, given the leniency of
the literature on this topic, it is necessary to explore the effects of In our systematic review, two studies [15,17] had as their objective
a higher dose of topical capsaicin before any conclusions can be the analysis of the modification of these inflammatory mediators
drawn about TRPV1 (Transient Receptor Potential Vanilloid type after administration of analgesics:
1) being an effective method of controlling temporomandibular - In fact, the study conducted by El Garby M. et al. [17]
pain and ultimately chronic pain. demonstrated a statistically significant decrease in IL-6 levels
after injection of analgesics, greater than that recorded in subjects
Effect of Treatment on Maximal Mouth Opening who received sodium hyaluronate, thus proving its effectiveness in
Study participants showed a significant increase in this parameter modulating inflammation. The present results are consistent with
at different follow-up periods compared to the other control those of Walker [37] who showed that opioids are fully therapeutic
groups. These results are in agreement with the fact that pain-free drugs and that they exert their anti-inflammatory effects through
jaw movement showed a notable impact on mouth opening and changes in cellular activation and cytokine expression. This
lateral movements [31]. confirms our original hypothesis and proves the curative and not
only the palliative effect of opioids.
The results of the meta-analyses by Liu, Siyan, and colleagues [25]
and Liu Y. and colleagues [26] were also significantly in favor of In the trial conducted by Ganti S. et al. [15], it was shown that
opioids for improvement in maximal mouth opening after three the efficacy of tramadol was lower than that of the combination
and six months of follow-up. of glucosamine and chondroitin sulfate, two protein components
of cartilage. As such, Damlar I. et al. [28] conclude that the
However, despite the significantly greater results in the analgesic glucosamine-chondroitin combination decreases synovial fluid
group compared with the reference treatment group in the Al Kisbi IL1β and IL6 levels in internal TMJ derangements compared
et al. study, the authors relate this improvement primarily to the with tramadol, whereas changes in synovial fluid TNF-α and PGE
fact that the upper joint space lavage reduced inflammatory cells in levels do not reach statistical significance between the two groups.
the joint, widened the joint spaces, and improved mouth opening,
and not to the injection of the analgesic. Indeed, the presence No systematic review has addressed this point, which proves to us
of inflammatory cells and inflammatory mediators, including the lack of sufficient studies that investigate the effect of analgesics
arachidonic acid metabolites and cytokines, has been demonstrated on different mediators of inflammation.
in symptomatic TMJ [32].
Effect of Treatment on Clicking Sound
Therefore, further clinical trials investigating this variable should In studies conducted by El Gerby M. et al. [19] and Al-Kibsi et al.
be conducted to have a clear conclusion. [22], the authors demonstrated a decrease in the number of patients
with clicking sounds after injection of analgesics.
Effect of Treatment on Cytokine Levels
Inflammatory cytokines such as prostaglandins, interleukins, According to El Gerby and Coll [19], the disappearance of the
and TNF-α are potential regulators of osteoclastogenesis [33]. postoperative popping sound was possibly due to the effect of the
Increased levels of IL-1ß (Interleukin 1 beta), IL-6 (Interleukin arthrocentesis procedure, as it dilutes inflammatory mediators and
6), and TNF-α (Tumor Necrosis Factor-Alpha) in synovial releases adhesion and locking of the disc within the joint, which
fluid, which are important outcomes of inflammation, have been facilitates the sliding of the disc into the upper compartment, which
frequently discussed in the literature: is evidenced by the increase in mouth opening and jaw movements
- Kaneyama K. et al. [(34] compared the levels of IL- 1ß, IL-6, in the normal range.
and TNF-α measured in TMJ synovial fluid in 55 patients with
OA and 5 healthy volunteers. The authors found that the levels This explanation is in agreement with Nitzan et al. [23] who stated
of inflammatory mediators were higher in patients with internal that lavage of the upper joint space reduces pain by removing
derangement compared with healthy individuals. inflammatory mediators from the joint, increasing mandibular
- In another study by the same authors [35], synovial fluids mobility by removing intra-articular adhesions, eliminating
obtained from 57 patients with the degenerative joint disease were negative pressure in the joint, reclaiming disc and fossa space
compared with those obtained from 7 healthy individuals. The and improving disc mobility, which reduces mechanical obstruction
authors concluded that inflammatory mediators were associated caused by the anterior position of the disc and thus the clicking sound.
with TMJ abnormalities.
- In a trial of 61 patients with manducatory disorders and 7 healthy Moreover, the efficacy of analgesics in the management of
patients, Kaneyama K. et al. [36] showed that IL-6 and IL-11 manducatory system snapping requires further clinical trials to
concentrations in synovial fluid were increased when there were judge the actual action of these molecules.
bone changes in the condyle. In particular, when IL-6 and IL-11
Oral Health Dental Sci, 2022 Volume 6 | Issue 2 | 7 of 9
Conclusion Hyaluronic Acid on Expression of Cytokine Levels in Internal
The use of analgesics increases the efficacy of treatment by Derangement of Temporomandibular Joint. J Contemp Dent
decreasing pain intensity and cytokine levels, through both their Pract. 2018; 19: 1501-1505.
analgesic and anti-inflammatory actions. This efficacy is similar 16. Kang SK, Lee YH, Park H, et al. Effects of intramuscular
for both levels II and III. However, additional long-term clinical morphine in men and women with temporomandibular
studies with a larger sample size are needed to confirm the data disorder with myofascial pain. Oral Dis. 2018; 24: 1591-1598.
collected and to further explore the effect of analgesics in the 17. El-Gerby Y, El-Sholkamy M, Abdelhai A, et al. The Effect
treatment of TMDs. of Tramadol Hydrochloride In-traarticular Injection on IL-6
Level in Patients with Tempromandibular Joint Internal
References Derangement. Pain Studies and Treatment. 2015; 3: 31-37.
1. Gola R, Chossegros C. Syndrome algodysfonctionnel de 18. Tamer A. Hamed Arthrocentesis with Injection of Tramadol
l'appareil manducateur. Stomatologie et Odontologie. 1993; 15.
and Cox-2 Inhibitor for the Management of Internal
2. Cadden Samuel. Orofacial pain. Guidelines for assessment, Derangements of the Tempromandibular Joint (A Comparative
diagnosis, and management, 4th edition. Euro J of Orthod. Study). J. of Am. Sci. 2012; 8: 277-283.
2008; 31: 216-217.
19. El-Gerby Y, El-Sholkamy M, El- Sharrawy E. Comparative Study
3. Orthlieb J.D, Giraudeau A, Marion Jeany, et al. Prise en charge Between Tramadol Hydrochloride and Sodium Hyaloronate for
des dysfonctions temporomandibulaires. Orale et maxillo-fac. Management of Tempromandibular Joint Internal Derangement.
2016; 11: 1-11. Advances in Surgical Sciences. 2015; 3; 19.
4. Orthlieb J.D, Giraudeau A, Marion Jeany, et al. Articulation 20. Sipahi A, Satilmis T, Basa S. Comparative study in patients with
temporo-mandibulaire, occlusion et bruxisme. Rev. De symptomatic internal derangements of the temporomandibular
Stomatol. 2016; 117: 207-211. joint: analgesic outcomes of arthrocentesis with or without
5. Slade GD, Ohrbach R, Greenspan JD, et al. Painful intra-articular morphine and tramadol. Br J Oral Maxillofac
Temporomandibular Disorder: Decade of Discovery from Surg. 2015; 53: 316-320.
OPERA Studies. J Dent Res. 2016; 95: 1084-1092. 21. Fayed H.-T.-AM, Elsharrawy EA, Hamed TA, et al. Clinical
6. Aguila Maxine, Benichou Mathieu, Hennequin Antonin, et assessment of intra-articular fentanyl injection following
al. Temporomandibular disorders and benefits of a cervical arthrocentesis for management of temporomandibular joint
therapeutic approach in facial myalgia treatment: A review of internal derangement. Future Dental J. 2016; 2: 86-90.
the literature. Oral Health and Care. 2019; 4: 1-6.
22. Al-Kibsi Taghreed, El-Sharrawy Eman, Ghanem Walid, et al.
7. Hennequin A, Tenenbaum B, Caire JM, et al. Hypnothérapie Clinical assessment of intra-articular injection of butorphanol in
et gestion des douleurs oro-faciales dans le cadre des désordres management of temporomandibular joint internal derangement.
temporo- mandibulaires. Cah. De proth. 2020; 189: 330-338. Egyptian J. of Oral & Maxillofac. Surg. 2017; 8: 83-87.
8. Chicre-Alcantara TC, Torres-Chavez KE, Fischer L, 23. Nitzan Dorrit, Dolwick Franklin, Martinez Garza.
et al. Local kappa opioid receptor activation decreases Temporomandibular joint arthrocentesis: A simplified
temporomandibular joint inflammation. 2012; 35: 371-376. treatment for severe, limited mouth opening. J. of oral and
9. Ouanounou A, Goldberg M, Haas DA. Pharmacotherapy in maxillofac. Surg. 1991; 49: 1163-1167
Temporomandibular Disorders: A Review. J Can Dent Assoc. 24. Ryan T, Hodge A, Holyoak R, et al. Tramadol as an adjunct to
2017; 83: 7. intra-articular local anaesthetic infiltration in knee arthroscopy:
10. Gopalakrishnan V, Nagori SA, Roy Chowdhury SK, et al. a systematic review and meta-analysis. ANZ J Surg. 2019; 89:
The use of intra-articular analgesics to improve outcomes 827-832.
after temporomandibular joint arthrocentesis: a review. Oral
25. Liu Siyan, Hu Yingshun, Zhang Xiao. Do intra-
Maxillofac Surg. 2018; 22: 357-364.
articular injections of analgesics improve outcomes after
11. Stein C. The control of pain in peripheral tissue by opioids. N temporomandibular joint arthrocentesis? A systematic review
Engl J Med. 1995; 332: 1685-1690. and meta-analysis. J. of Oral Rehab. 2020; 48: 95-105.
12. Trivedi M, Shaikh S, Gwinnutt C. Pharmacology of Opioids - 26. Liu Y, Wu J.S, Tang Y.L, et al. The multiple-treatments meta-
Part 1. Anaesthesia Tutorial of the Week 64. 2007; 33: 66-73. analysis of inter-articular injection for temporomandibular
13. Hayashi K, Sugisaiki M, Ota S, et al. mu-Opioid receptor osteoarthritis. J. of Oral and Maxillofac. Surg. 2019.
mRNA expression and immunohistochemical localization in 27. Mazieres Bernar, Hucher Michel, Zaïm Mohammed, Garnero
the rat temporomandibular joint. Peptides. 2002; 23: 889-893. Patrick Effect of chondroitin sulphate in symptomatic knee
14. Campbell BK, Fillingim RB, Lee S, et al. Effects of High- osteoarthritis: A multicentre, randomised, double-blind,
Dose Capsaicin on TMD Subjects: A Randomized Clinical placebo-controlled study. Annals of the rheumatic diseases.
Study. JDR Clin Trans Res. 2017; 2: 58-65. 2007; 66: 639-645.
15. Ganti S, Shriram P, Ansari AS, et al. Evaluation of Effect of 28. Damlar Ibrahim, Esen Esen, Tatli Ufuk. Effects of
Glucosamine-Chondroitin Sulfate, Tramadol, and Sodium glucosamine-chondroitin combination on synovial fluid IL-
Oral Health Dental Sci, 2022 Volume 6 | Issue 2 | 8 of 9
1β, IL-6, TNF-α and PGE2 levels in internal derangements Induction of osteoclast-like cells derived from the synovial
of temporomandibular joint. Medicina oral, patologia oral y lavage fluids of patients with temporomandibular joint
cirugia bucal. 2015; 20: e278-283. disorders. OARS, Osteoarthritis Research Society. 2007; 15:
29. Christoph T, Kogel B, Strassburger W. Tramadol has a better 291-299.
potency ratio relative to morphine in neuropathic than in 34. Kaneyama K, Segami N, Sun W, et al. Analysis of tumor
nociceptive pain models. Drugs R D. 2007; 8: 51-57. necrosis factor-alpha, interleukin-6, interleukin-1beta, soluble
tumor necrosis factor receptors I and II, interleukin-6 soluble
30. Kapral Stephan, Gollmann Gabriele, Waltl Barbara, et al.
receptor, interleukin-1 soluble receptor type II, interleukin-1
Tramadol Added to Mepivacaine Prolongs the Duration of an
receptor antagonist, and protein in the synovial fluid of patients
Axillary Brachial Plexus Blockade. Anesthesia and analgesia.
with tempo- romandibular joint disorders. Oral Surg Oral Med
1999; 88: 853-856. Oral Pathol Oral Radiol Endod. 2005; 99: 276-284.
31. Kunjur J, Anand R, Brennan PA, et al. An audit of 405 35. Kaneyama K, Segami N, Nishimura M, et al. Importance of
temporomandibular joint arthrocentesis with intra-articular proinflammatory cytokines in synovial fluid from 121 joints
morphine infusion. Br J Oral Maxillofac Surg. 2003; 41: 29- with temporomandibular disorders. Br J Oral Maxillofac Surg.
31. 2002; 40: 418-423.
32. Nishimura Masaaki, Segami Natsuki, Kaneyama Keiseki, et 36. Kaneyama K, Segami N, Sato J, et al. Interleukin-6 family
al. Comparison of cytokine level in synovial fluid between of cytokines as biochemical markers of osseous changes in
successful and unsuccessful cases in arthrocentesis of the the temporomandibular joint disorders. Br J Oral Maxillofac
temporomandibular joint. J. of oral and maxillofac. Surg. Surg. 2004; 42: 246-250.
2004; 62: 284-287. 37. Walker Sylvia. Anti-inflammatory effects of opioids. Adv Exp
33. Takano Hiroshi, Ariyoshi Wataru, Kanno Takahiro, et al. Med Biol. 2003; 521: 148-160.
© 2022 Boujoual I, et al. This article is distributed under the terms of the Creative Commons Attribution 4.0 International License
Oral Health Dental Sci, 2022 Volume 6 | Issue 2 | 9 of 9
You might also like
- Temporomandibular Joint Dysfunctions: A Systematic Review of Treatment ApproachesDocument13 pagesTemporomandibular Joint Dysfunctions: A Systematic Review of Treatment Approachesnabila puspitaNo ratings yet
- Efficacy of Musculoeskeletal Manual Approach in The Treatment of Temporomandibulaar Joint DisorderDocument8 pagesEfficacy of Musculoeskeletal Manual Approach in The Treatment of Temporomandibulaar Joint DisorderLaura Espejo SalamancaNo ratings yet
- Ijerph 20 02777Document14 pagesIjerph 20 02777Paola ClaudetNo ratings yet
- Medi 96 E6408Document8 pagesMedi 96 E6408Ana Carolina SouzaNo ratings yet
- Manual Therapy: Systematic ReviewDocument8 pagesManual Therapy: Systematic ReviewArlen EvelyNo ratings yet
- JR 2 Prosthodontic Treatment in Patients With Temporomandibular Disorders and Orofacial Pain And:or BruxismDocument10 pagesJR 2 Prosthodontic Treatment in Patients With Temporomandibular Disorders and Orofacial Pain And:or Bruxismaulia zahroNo ratings yet
- Oral Myofunctional Therapy For The Treatment DTMDocument8 pagesOral Myofunctional Therapy For The Treatment DTMmartaNo ratings yet
- Sleep Bruxism: Therapeutic Possibilities Based in EvidencesDocument8 pagesSleep Bruxism: Therapeutic Possibilities Based in EvidencesmutiaNo ratings yet
- 13-Dentistry and Psychology in The Care and Treatment of Odontophobic Patients The Concise Systematic ReviewDocument5 pages13-Dentistry and Psychology in The Care and Treatment of Odontophobic Patients The Concise Systematic ReviewAbi LobatoNo ratings yet
- International Journal of Health Sciences and ResearchDocument11 pagesInternational Journal of Health Sciences and ResearchAbiNo ratings yet
- Is There An Association Between The Use of Antidepressants and Complications Involving Dental Implantes - A Systematic Review and Meta-AnalysisDocument8 pagesIs There An Association Between The Use of Antidepressants and Complications Involving Dental Implantes - A Systematic Review and Meta-AnalysisCaio GonçalvesNo ratings yet
- Interdisciplinary Diagnostic Research For Identification of BrushismDocument6 pagesInterdisciplinary Diagnostic Research For Identification of BrushismViviane MarquesNo ratings yet
- Medoralv16 I3 p425Document5 pagesMedoralv16 I3 p425Diana OliveiraNo ratings yet
- Content ServerDocument6 pagesContent ServerFernando Lopez EncisoNo ratings yet
- Healthcare 10 01566 v2Document16 pagesHealthcare 10 01566 v2crusNo ratings yet
- Calixtre 2015Document15 pagesCalixtre 2015Anderson RodriguesNo ratings yet
- Medoral 21 E579Document8 pagesMedoral 21 E579AngiPaolaPuiconRuizNo ratings yet
- Effectiveness of Prefabricated MyofunctionalDocument10 pagesEffectiveness of Prefabricated MyofunctionalAdina SerbanNo ratings yet
- Dallel 2019impact of Orthodontic Forces On Pulp Reaction A Systematic ReviewDocument6 pagesDallel 2019impact of Orthodontic Forces On Pulp Reaction A Systematic ReviewMICHAEL ERNESTO QUINCHE RODRIGUEZNo ratings yet
- Mandibular Changes Produced by Functional Appliances in Class II Malocclusion: A Systematic ReviewDocument13 pagesMandibular Changes Produced by Functional Appliances in Class II Malocclusion: A Systematic ReviewSai KrupaNo ratings yet
- Orthobiologic Injections For Treating DegenerativeDocument7 pagesOrthobiologic Injections For Treating DegenerativeNacho TorreroNo ratings yet
- Managment in Awake BruxismDocument2 pagesManagment in Awake BruxismIlinca LupuNo ratings yet
- Effectiveness of Myofunctional Therapy in Ankyloglossia: A Systematic ReviewDocument18 pagesEffectiveness of Myofunctional Therapy in Ankyloglossia: A Systematic Reviewmistic0No ratings yet
- Therapies For Bruxism: A Systematic Review and Network Meta-Analysis (Protocol)Document6 pagesTherapies For Bruxism: A Systematic Review and Network Meta-Analysis (Protocol)Wallisson SoaresNo ratings yet
- 2020 Manual Therapy and Excercice in Temporomandibular Joint Disc Displacement Without Reduction. A Systematic ReviewDocument12 pages2020 Manual Therapy and Excercice in Temporomandibular Joint Disc Displacement Without Reduction. A Systematic Reviewjuan pabloNo ratings yet
- Association Between Posterior Crossbite, Skeletal, and Muscle Asymmetry: A Systematic ReviewDocument14 pagesAssociation Between Posterior Crossbite, Skeletal, and Muscle Asymmetry: A Systematic ReviewFANOR ALFONSO MARTINEZ ARCÓNNo ratings yet
- Management of Temporomandibular Disorders: A Rapid Review of Systematic Reviews and GuidelinesDocument15 pagesManagement of Temporomandibular Disorders: A Rapid Review of Systematic Reviews and Guidelinesricardo riquelmeNo ratings yet
- The Efficacy of Instrumental Physical Therapy ThroughDocument15 pagesThe Efficacy of Instrumental Physical Therapy ThroughSanaNo ratings yet
- Occlusal Disharmony and Chronic Oro-Facial PainDocument9 pagesOcclusal Disharmony and Chronic Oro-Facial PaindepttofprosthodonticsNo ratings yet
- Review of New Trends in Myofunctional Therapy OcclDocument4 pagesReview of New Trends in Myofunctional Therapy Occl이창엽No ratings yet
- Art 2Document21 pagesArt 2xdxdxdxdNo ratings yet
- Kees Tra 2014Document21 pagesKees Tra 2014Marco Antonio García LunaNo ratings yet
- 7070 m14xxlDocument11 pages7070 m14xxlLjupce GorgievskiNo ratings yet
- Early Orthodontic Treatment of Skeletal Open-Bite MalocclusionDocument7 pagesEarly Orthodontic Treatment of Skeletal Open-Bite MalocclusionMaria SilvaNo ratings yet
- Prevalence of Musculoskeletal Disorders Among Dentists in Iran: A Systematic ReviewDocument6 pagesPrevalence of Musculoskeletal Disorders Among Dentists in Iran: A Systematic ReviewAbiNo ratings yet
- Soft Occlusal Splint Therapy in The Management of Myofascial Pain Dysfunction Syndrome: A Follow-Up Study in Kashmiri PopulationDocument7 pagesSoft Occlusal Splint Therapy in The Management of Myofascial Pain Dysfunction Syndrome: A Follow-Up Study in Kashmiri PopulationfilzahNo ratings yet
- Badel Michigan Splint and Treatment PDFDocument9 pagesBadel Michigan Splint and Treatment PDF謎超人No ratings yet
- Fleckenstein2010 Article DiscrepancyBetweenPrevalenceAnDocument9 pagesFleckenstein2010 Article DiscrepancyBetweenPrevalenceAnqwerty hrNo ratings yet
- OrtodonciaDocument14 pagesOrtodoncialibroscasitaNo ratings yet
- TENS therapy relieves pain and improves jaw mobility in TMJ disordersDocument10 pagesTENS therapy relieves pain and improves jaw mobility in TMJ disordersirfanadil2006No ratings yet
- Clinical Characterization of Gingival Type of Burning Mouth Syndrome: A Cross-Sectional StudyDocument6 pagesClinical Characterization of Gingival Type of Burning Mouth Syndrome: A Cross-Sectional StudydaruNo ratings yet
- Advantages of Ultrasound Guidance For TMJ Arthrocentesis and Intra-Articular Injection: A Narrative ReviewDocument10 pagesAdvantages of Ultrasound Guidance For TMJ Arthrocentesis and Intra-Articular Injection: A Narrative Reviewnajimohammed020113No ratings yet
- Fphar 11 596099Document17 pagesFphar 11 596099germanNo ratings yet
- Articulo DentalDocument7 pagesArticulo DentalV DreamerNo ratings yet
- Adverse Effects Following Dental Local ADocument19 pagesAdverse Effects Following Dental Local AMaura HokamaNo ratings yet
- J Lebanese Dent Assoc 2017 52 2 53 58 EngDocument6 pagesJ Lebanese Dent Assoc 2017 52 2 53 58 EngMarcel PavoniNo ratings yet
- JMedLife 14 148Document17 pagesJMedLife 14 148Mariana CordeiroNo ratings yet
- 162 Ozonioterapia Intraarticular Atenua EficieDocument8 pages162 Ozonioterapia Intraarticular Atenua EficievigouveiaNo ratings yet
- Treat CMD Gnat NMD Chan 2003Document32 pagesTreat CMD Gnat NMD Chan 2003Constantin IonutNo ratings yet
- Ughreja Myofascial ReleaseDocument9 pagesUghreja Myofascial Releasecris.endo.ceNo ratings yet
- Dentistry Oraldisorders Therapy35Document7 pagesDentistry Oraldisorders Therapy35AnnoasdasdNo ratings yet
- Botulinum Toxin Therapy For Temporomandibular Joint Disorders: A Systematic Review of Randomized Controlled TrialsDocument9 pagesBotulinum Toxin Therapy For Temporomandibular Joint Disorders: A Systematic Review of Randomized Controlled TrialsCaioSelaimenNo ratings yet
- Novel Approach Towards Musculoskeletal PhenotypesDocument12 pagesNovel Approach Towards Musculoskeletal Phenotypescelia Diz CastilloNo ratings yet
- Ocular Complications Following Dental Local Anaesthesia (2011)Document7 pagesOcular Complications Following Dental Local Anaesthesia (2011)JohnNo ratings yet
- Osteoartritis TerapeuticaDocument10 pagesOsteoartritis TerapeuticaYasmin AbassNo ratings yet
- Jensen Et Al-2014-Journal of Oral Pathology & Medicine PDFDocument10 pagesJensen Et Al-2014-Journal of Oral Pathology & Medicine PDFMega MalyndaNo ratings yet
- Work-Related Musculoskeletal Disorders in Iranian Dentists - A Systematic Review and Meta-AnalysisDocument9 pagesWork-Related Musculoskeletal Disorders in Iranian Dentists - A Systematic Review and Meta-AnalysisAbelNo ratings yet
- Prolotherapy For Osteoarthritis and Tendinopathy: A Descriptive ReviewDocument8 pagesProlotherapy For Osteoarthritis and Tendinopathy: A Descriptive ReviewFisiatria UNNo ratings yet
- Healthcare 09 01497Document13 pagesHealthcare 09 01497Ray SirvelNo ratings yet
- 30.plDocument54 pages30.plRobert GarciaNo ratings yet
- Pre AnestesiDocument64 pagesPre AnestesiKevin YonathanNo ratings yet
- EC8073-Medical Electronics PDFDocument12 pagesEC8073-Medical Electronics PDFSwetha Ramesh50% (2)
- SusmpDocument669 pagesSusmpSarmad FarhanNo ratings yet
- Final Rating Remarks Core Values Behavior Statements Quarter 1 2 3 4Document1 pageFinal Rating Remarks Core Values Behavior Statements Quarter 1 2 3 4Jnl RgndnNo ratings yet
- Drink H2O2 Drinking Hydrogen Peroxide Hydrogen Peroxide TherapyDocument28 pagesDrink H2O2 Drinking Hydrogen Peroxide Hydrogen Peroxide TherapyVincent Nickisch100% (1)
- Gima CatalogDocument84 pagesGima Catalogsara şovreNo ratings yet
- Nutritional Problem in ChildrenDocument4 pagesNutritional Problem in Childrennaufal umerNo ratings yet
- Pathophysiology of Hypertension in Chronic Kidney DiseaseDocument7 pagesPathophysiology of Hypertension in Chronic Kidney DiseaseRifka WidianingrumNo ratings yet
- Weebly Professional Development Plan FeedbackDocument3 pagesWeebly Professional Development Plan Feedbackapi-241839714No ratings yet
- Jurnal MFSDocument11 pagesJurnal MFSAfni YusnitaNo ratings yet
- IEEE 1540 - Software Engineering Risk Management: Measurement-Based Life CycleDocument28 pagesIEEE 1540 - Software Engineering Risk Management: Measurement-Based Life Cycleminhlongyb89No ratings yet
- AP LacrimalDocument38 pagesAP LacrimalIoana MovileanuNo ratings yet
- The Inside Story of The Papal Birth ControlDocument5 pagesThe Inside Story of The Papal Birth ControlKenneth DavisNo ratings yet
- 2019 ITENA Catalogue enDocument68 pages2019 ITENA Catalogue enDicktusNo ratings yet
- Treatment and Symptoms of ThalassemiaDocument20 pagesTreatment and Symptoms of Thalassemiamohammed maazNo ratings yet
- General Introduction and Review LiteratureDocument10 pagesGeneral Introduction and Review LiteratureLekshmi NarayananNo ratings yet
- The Osteological Paradox 20 Years Later - Past Perspectives, Future Directions - DeWitte and Stojanowski 2015Document55 pagesThe Osteological Paradox 20 Years Later - Past Perspectives, Future Directions - DeWitte and Stojanowski 2015camilaNo ratings yet
- Green Tea Polyphenols Nutraceuticals of Modern Life (PDFDrive) - 2Document353 pagesGreen Tea Polyphenols Nutraceuticals of Modern Life (PDFDrive) - 2Paulo Aguiar100% (1)
- S1509Document16 pagesS1509rabeaboulahiabzNo ratings yet
- Gaps Australia Into EbookDocument15 pagesGaps Australia Into EbookMadeli Viljoen100% (2)
- Stacey Brockhaus Resume UpdatesDocument4 pagesStacey Brockhaus Resume Updatesapi-481359160No ratings yet
- Concept Map CovidDocument7 pagesConcept Map CovidMaieca Demecillo100% (3)
- Case History EndodonticsDocument1 pageCase History EndodonticsDurva JainNo ratings yet
- Bulliying 1Document34 pagesBulliying 1ahmed abybakarNo ratings yet
- Guardian Angel - Cara MaloneDocument177 pagesGuardian Angel - Cara MalonenoNo ratings yet
- Presentation Datin PH WongDocument38 pagesPresentation Datin PH WongFakhriyahNur IbrahimNo ratings yet
- JCM 11 00011Document11 pagesJCM 11 00011Lal NandaniNo ratings yet
- Region III Pampanga Arayat Candating Youth Development Budget 2022-2024Document4 pagesRegion III Pampanga Arayat Candating Youth Development Budget 2022-2024CHUCKZ CAPARASNo ratings yet
- Student Medical Risk Undertaking FormDocument2 pagesStudent Medical Risk Undertaking Formdr_biltNo ratings yet