Professional Documents
Culture Documents
Microscopy Session - (B) : SGD - (D)
Uploaded by
Cherry RahimaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Microscopy Session - (B) : SGD - (D)
Uploaded by
Cherry RahimaCopyright:
Available Formats
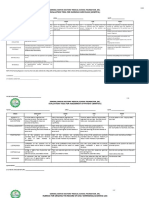
FEB.
8, 2022 (TUESDAY)
7:30am – 9:30am
● Microscopy Session - (B)
● SGD – (D)
9:30am – 11:30am
● Microscopy Session – (D)
● SGD – (B)
GENERAL PATHOLOGY WORKSHEETS 177-182
Guide Questions to Amoebic Liver Abscess:
1. What is the etiologic agent of this case?
- Entamoeba histolytica
2. Discuss briefly its pathogenesis.
- The organism has 2 stages of life, the cystic stage which is the infective stage
and the trophozoite stage which ends up causing invasive disease.]Upon
ingestion of contaminated food and water; the infection starts with ingestion of
the quadrinucleate cyst of E. histolytica. Excystation in the small intestinal lumen
is followed by production of motile, potentially invasive trophozoites. Once the
trophozoites invade the colonic epithelium, subsequent spread to extraintestinal
sites such as the liver (by hematogenous spread through the portal circulation)
and peritoneum can occur. The organism causes hepatic inflammation followed
by necrosis which results in an abscess formation.
3. What is the usual clinical manifestations and work-up in patient’s presenting with
alternating diarrhea and constipation?
- IBS-M(mixed) when a person suffers from alternating diarrhea and constipation.
Guide Questions to Pyogenic Liver Abscess:
1. What is the most common etiologic agent of this case?
- Escherichia coli and Klebsiella pneumoniae
2. Discuss briefly its etiopathogenesis
- Since liver receives its blood circulation from the systemic and portal circulations,
it is more susceptible to getting infections and abscesses from the bloodstream.
The usual pathophysiology for pyogenic liver abscesses is Bowel content
leakage and peritonitis. Bacteria travel to the liver via the portal vein and reside
there. Infection can also originate in the biliary system. Hematogenous spread is
also a potential etiology.
3. Describe the features to distinguish amoebic form pyogenic liver abscess
- Amoebic liver abscess: Caused by parasite, from poor sanitation and
contaminated drinking water. Inflammation with abundant neutrophils.
Macroscopic Fine needle aspirate findings: Thick, chocolate brown odorless
“anchovy paste”
- Pyogenic Liver abscess: Caused by bacteria, from biliary/impacted gall stone,
systemic infection. Necrosis with absence of neutrophils. Macroscopic Fine
needle aspirate findings: Purulent, foul smelling.
4. How will you manage this case to prevent early demise of the patient
- Percutaneous drainage of the abscess along with antibiotics is the mainstay
therapy. Antibiotic treatment in small responsive abscesses.
Guide Questions to Typhoid Liver Nodules:
1. Discuss briefly how do patients acquire typhoid fever?
- If one consumes food or drink contaminated with Samonella typhi or Samonella
paratyphi, the bacteria can multiply and spread into the bloodstream, causing
typhoid fever or paratyphoid fever.
2. Discuss briefly its etiopathogenesis. How do the bacteria cause disease, infects the
intestine and liver?
- The pathogenesis of enteric fever depends on a number of factors including the
infecting species and infectious dose. Ingested organisms survive exposure to
gastric acid before gaining access to the small bowel, where they penetrate the
epithelium, enter the lymphoid tissue, and disseminate via the lymphatic or
hematogenous route. When Salmonella bacteria are ingested, they pass through
a person's stomach and colonize the small & large intestine. There, the bacteria
invade the intestinal mucosa and proliferate, which affect almost all major organs
including the liver.. The bacteria can invade the lymphoid tissues of the
gastrointestinal tract and spread to the bloodstream.
3. What are the signs and symptoms of typhoid fever and how is it diagnosed?
- Most people with Salmonella infection have diarrhea, fever, and stomach cramps.
Symptoms usually begin six hours to six days after infection and last four to
seven days. However, some people do not develop symptoms for several weeks
after infection and others experience symptoms for several weeks. Diagnosing
Salmonella infection requires testing a specimen (sample), such as stool (poop)
or blood. Testing can help guide treatment decisions. Infection is diagnosed when
a laboratory test detects Salmonella bacteria in stool, body tissue, or fluids.
Guide Questions to Schistosomiasis of the Liver:
1. Discuss the etiopathogenesis of schistosomiasis of the liver
- Hepatic schistosomiasis results from the host’s granulomatous cell-mediated
immune response to the soluble egg antigen of S.mansoni, which progesses to
irreversible fibrosis and consequently, several portal hypertension.
2. The parasite incite what type of inflammatory reaction
- Schistosoma japonicum eggs cause granulomatous inflammation in the host liver
during the acute phase and lead to chronic liver damage
3. In what regions of the Philippines Schistosomiasis in endemic?
- The known endemic areas in the Philippines are the provinces of Mindoro
Oriental and Sorsogon in Southern Luzon; the provinces of North, East and
Western Samar; Leyte; and Bohol in Eastern Visayas, and all the provinces of
Mindanao with the exception of Misamis Oriental, Davao Oriental and
Maguindanao.
4. What schistosome specie is prevalent in the Philippines?
- The species of schistosome endemic in the Philippines is S. japonicum
Guide Questions ot the CPC of the Liver:
1. Discuss the pathogenesis of CPC of the liver.
- Congestion predisposes to hepatic injury through three major pathogenetic
mechanism:
1. Decreased hepatic blood flow
2. Decreased arterial congestion
3. Increased Hepatic venous pressure
- Elevated central venous pressure transmits to the hepatic veins and sinusoids,
and thereby decreases portal venous inflow.
- Increased hepatic venous pressure also causes sinusoidal congestion, dilation
of sinusoidal fenestrae, and exudation of protein and fluid into the space of Disse.
- Accumulation of exudate into the space of Disse then impairs diffusion of oxygen
and nutrients to hepatocytes.
- Decreased hepatic blood flow further increases susceptibility to injury in settings
that compromise arterial flow, such as hypotension, arrhythmias, or left‐sided
heart failure, which can precipitate ischemic hepatopathy.
2. What are the complications of the CPC of the liver? Explain.
- Due to elevated hepatic venous pressure and decrease in hepatic veouse flow
caused by hypoxia in hepatic parenchyma will eventually diffuse hepatocyte
death causing complications of;
-Hepatic fibrosis
-development of beign and malignant liver masses
Guide Questions to Fatty Change:
1. What substances have accumulated to produce fatty steatosis?
- Triglycerides and other fats in the liver cells
2. What are possible causes of fatty steatosis and which of these may have produced the
fatty liver seen in this case?
- Alcohol abuse, rapid weight loss and malnutrition may lead to fatty steatosis.
- In this case, malnutrition or undernutrition caused the production of fatty liver to
the patient.
3. What causes fatty steatosis in alcoholism?
- Alcohol consumption causes shunting of normal substrates away from catabolism
and toward lipid biosynthesis due to decreased NAD due to ethanol metabolism
4. Is the accumulation of fat in this liver reversible or irreversible change?
- Reversible
5. Discuss the pathogenesis of fatty steatosis.
- Fatty acids derived by hydrolysis from dietary or adipocyte triglycerides are
transported to the liver, where they may be oxidized for energy, converted to
other substances such as phospholipids, or esterified back into triglycerides. The
triglycerides, in turn, may be cached within the hepatocyte or packaged into very
low-density lipoproteins and exported into the blood, in this way transferring
triglycerides back to adipose tissue reserves. There is thus a net circulation of
fatty acids between the liver and adipose tissue, maintaining a balance between
the triglyceride reservoirs of each. A disturbance in the commerce or processing
of fatty acids can lead to an accumulation of hepatic triglycerides; when this
exceeds 5% of liver weight, steatosis can be appreciated histologically.
Guide Questions to Liver Cirrhosis:
1. What is the most common cause of liver disease in the Philippines? In the United
States?
- Hepatitis B
- Obesity and Excessive alcohol consumption
2. What are the different stages of alcoholic liver disease?
a. Hepatocellular steatosis or fatty change
b. Alcoholic hepatitis
c. Steatofibrosis up to and including cirrhosis in the late stages of disease
3. What is cirrhosis and what are the key histologic features of cirrhosis?
- Cirrhosis is a condition marked by the diffuse transformation of the entire liver
into regenerative parenchymal nodules surrounded by fibrous bands and variable
degrees of vascular shunting.
4. What are the two common causes of cirrhosis?
- Hepatitis
- Alcohol abuse
5. Discuss the causal relationship of Hepatitis B and Hepatitis C with cirrhosis.
- Both HBV and HCV are known to cause HCC via promoting inflammatory
reactions and oxidative stress in the liver, though HCV is thought to contribute to
greater oxidative DNA damage than HBV. Under these conditions, liver damage
occurs, and sequentially followed by fibrosis, cirrhosis, and HCC.
6. What are the complications of cirrhosis?
- Portal hypertension
- Ascites
- Portosystemic Shunts
- Splenomegaly
7. What is portal hypertension?
- Portal hypertension is an increase in portal venous blood flow resulting from a
hyperdynamic circulation.
8. What is cardiac cirrhosis and how does it differ from hepatic cirrhosis?
- Cardiac cirrhosis is a term used to include the spectrum of hepatic disorders that
occur secondary to hepatic congestion due to cardiac dysfunction, especially the
right heart chambers. This condition may present with symptoms such as
shortness of breath, paroxysmal nocturnal dyspnea, orthopnea, and leg swelling.
9. What kind of liver damage is associated with chronic right-sided heart failure?
- Congestive hepatopathy
Guide Questions to Hepatocellular Carcinoma:
1. Discuss the etiopathogeneis of this particular case that leads to Hepatocellular
Carcinoma (HCCA).
- HCC is the most common primary hepatic malignant neoplasm, often occurring in
the setting of cirrhosis related to chronic liver disease such as chronic hepatitis B
and C, autoimmune hepatitis, alcoholic/nonalcoholic fatty liver disease, and
hemochromatosis.
It is believed that the chronic injury, inflammation, and hepatocyte regeneration
that are seen in these disorders contribute to the acquisition of driver mutations
that lead to HCC development. As with other cancers, HCC is associated with
complementary sets of driver mutations that lead to the acquisition of cancer
hallmarks. Among the most common are activating mutations in the β-catenin
gene, mutations in the TERT (telomerase transcriptase), and inactivating
mutations in TP53 (up to 60% of tumors).
2. What conditions are commonly associated with HCCA?
- Cirrhosis
- Viral hepatitis (Hepatitis B & C)
- Autoimmune hepatitis
- Alcoholic/nonalcoholic fatty liver disease
- Hemochromatosis
-
3. What is the key laboratory findings in HCCA?
- Microscopically, well and moderately differentiated HCC are composed of cells
that resemble normal hepatocytes, while poorly differentiated tumors show
marked cytologic atypia. The tumor cells grow in thick plates or trabeculae,
pseudo-glandular structures with bile plugs, or sheets.
-
4. How does HCCA spread to the other sites of the body?
- Extrahepatic HCC can occur in 1 of 3 ways: direct extension, hematogenous
spread, or lymphatic invasion. Rupture of a HCC focus may result in
intraperitoneal implantation of tumour cells onto peritoneal or omental surfaces.
Reported frequencies of HCC metastatic sites include lungs (55%), lymph nodes
(53%), bone (28%), adrenal glands (11%), peritoneum and/or omentum (11%),
and brain (2%). Rare sites of metastasis include the rectum, spleen, diaphragm,
duodenum, esophagus, pancreas, seminal vesicle, and bladder
5. The majority of hepatic malignancies are what type of cancers?
- Malignant tumors in the liver can be primary or metastatic. Among primary
epithelial tumors, the most common are hepatocellular carcinoma and
intrahepatic cholangiocarcinoma
-
6. What are the common causes of death of patients with HCCA?
- Most HCC patients have two liver diseases, cirrhosis and HCC, each of which is
an independent cause of death.
- 57% of patients with unresectable HCC died as a direct result of cancer
progression, but 43% did not. The latter died from complications of their cirrhosis,
including sepsis, GI bleeds, and renal failure.
Guide Questions to Chronic Cholecystitis:
1. What is cholecystitis?
- Inflammation of the gallbladder may be acute, chronic, or acute superimposed on
chronic, and almost always occurs in association with gallstones.
2. Discuss the etiopathogenesis of gallstone formation.
- When bile is concentrated in the gallbladder, it can become supersaturated with
these substances, which then precipitate from the solution as microscopic
crystals. The crystals are trapped in the gallbladder mucus, producing gallbladder
sludge. Over time, the crystals grow, aggregate, and fuse to form macroscopic
stones. Occlusion of the ducts by sludge and/or stones produces the
complications of gallstone disease.
3. Give the types of gallbladder stones and list its components.
a. Cholesterol stones – cholesterol monohydrate, pale yellow, radioluscent,
Western, Formed through:
i. Bile saturation
ii. Gallbladder hypomotility – nucleation
iii. Mucus hypersecretion – crystal-trapping
b. Pigment stones – bilirubin calcium salts, black or brown, radiopaque, Asian,
Formed through:
i. Bile saturation
ii. Hemolytic anemia – unconjugated
iii. Biliary tract infection
c. Mixed stones
4. Define cholestasis, cholecystolithiasis, choledocholithiasis.
- Cholestasis is a condition caused by extrahepatic or intrahepatic obstruction of
bile channels or by defects in hepatocyte bile secretion.
- Cholecystolithiasis refers to the presence of stones in the gallbladder.
- Choledocholithiasis occurs when a gallstone blocks the common bile duct and
bile cannot flow past it, instead backing up into the liver.
5. What is Murphy's sign?
- Murphy's sign is elicited in patients with acute cholecystitis by asking the patient
to take in and hold a deep breath while palpating the right subcostal area. If pain
occurs when the inflamed gallbladder comes into contact with the examiner's
hand, Murphy's sign is positive.
6. What are the clinical features of cholecystitis?
- Severe pain in your upper right or center abdomen.
- Pain that spreads to your right shoulder or back.
- Tenderness over your abdomen when it's touched.
Guide Questions to Biliary Cirrhosis:
1. What is primary biliary cirrhosis?
- Primary biliary cholangitis (PBC), this disease was known as primary biliary
cirrhosis, it is an autoimmune disease whose primary feature is nonsuppurative,
inflammatory destruction of small- and medium-sized intrahepatic bile ducts.
2. What is the difference between primary and secondary biliary cirrhosis? Explain.
- Primary biliary cirrhosis - inflammation and destruction of bile ducts in the liver.
- Secondary biliary cirrhosis - results from prolonged bile duct obstruction or
narrowing or closure of the bile duct.
3. What causes primary biliary cirrhosis?
- The bile ducts become damaged and injured, causing bile to build up in the liver.
This further damages the liver and may lead to scarring (cirrhosis).
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Clin Path PagesDocument6 pagesClin Path PagesCherry RahimaNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Neoplasia Benign Tumors LaboratoryDocument2 pagesNeoplasia Benign Tumors LaboratoryCherry RahimaNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- General Pathology Bimonthly Exam Compilation Updated 2Document197 pagesGeneral Pathology Bimonthly Exam Compilation Updated 2Cherry Rahima100% (1)
- 1.05 - General Pathology - Diseases of The Immune System (Part 3) - Dr. AleraDocument15 pages1.05 - General Pathology - Diseases of The Immune System (Part 3) - Dr. AleraCherry RahimaNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- 1.02 General Pathology - Cellular Pathology Part 1 - Dr. Abelardo AleraDocument9 pages1.02 General Pathology - Cellular Pathology Part 1 - Dr. Abelardo AleraCherry RahimaNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- 1.05 General Pathology - Diseases of The Immune System (Part 2) - Dr. AleraDocument13 pages1.05 General Pathology - Diseases of The Immune System (Part 2) - Dr. AleraCherry RahimaNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- 1.05 General Pathology - Diseases of The Immune System (Part 1) - Dr. AleraDocument12 pages1.05 General Pathology - Diseases of The Immune System (Part 1) - Dr. AleraCherry RahimaNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Neoplasia Benign Malignant TumorsDocument6 pagesNeoplasia Benign Malignant TumorsCherry RahimaNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- 1.06 General Pathology - Neoplasia (Part 1) - Dr. Annette SallilasDocument17 pages1.06 General Pathology - Neoplasia (Part 1) - Dr. Annette SallilasCherry RahimaNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- 1.02 General Pathology - Cellular Pathology (Part 2) - Dr. Abelardo AleraDocument7 pages1.02 General Pathology - Cellular Pathology (Part 2) - Dr. Abelardo AleraCherry RahimaNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- A. B. C. D.: General PathologyDocument13 pagesA. B. C. D.: General PathologyCherry RahimaNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- GP Exam Compiled 1st BiDocument136 pagesGP Exam Compiled 1st BiCherry RahimaNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Unit Exam #1: Blood Vessels: B.) Advanced Glycation End ProductsDocument85 pagesUnit Exam #1: Blood Vessels: B.) Advanced Glycation End ProductsCherry RahimaNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Renal Pathology Unit ExamDocument50 pagesRenal Pathology Unit ExamCherry RahimaNo ratings yet
- General Pathology Practical Exam Renal PathologyDocument16 pagesGeneral Pathology Practical Exam Renal PathologyCherry RahimaNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- 3 Bimonthly: Lymphoid Tissue Disorders Unit Exam: Answer: ADocument36 pages3 Bimonthly: Lymphoid Tissue Disorders Unit Exam: Answer: ACherry RahimaNo ratings yet
- General Pathology 2nd BM Neoplasia Blood Vessel Cardiovascular Pathology Pulmonary PathologyDocument64 pagesGeneral Pathology 2nd BM Neoplasia Blood Vessel Cardiovascular Pathology Pulmonary PathologyCherry RahimaNo ratings yet
- Adrenal Cortical TumorsDocument8 pagesAdrenal Cortical TumorsSabrina whtNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Does Social Media Influence Consumer Buying Behavior An Investigation of Recommendations and PurchasesDocument7 pagesDoes Social Media Influence Consumer Buying Behavior An Investigation of Recommendations and Purchasesyash_28No ratings yet
- Apush Leq Rubric (Long Essay Question) Contextualization (1 Point)Document1 pageApush Leq Rubric (Long Essay Question) Contextualization (1 Point)Priscilla RayonNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Agrarian ReformDocument40 pagesAgrarian ReformYannel Villaber100% (2)
- Use Reuse and Salvage Guidelines For Measurements of Crankshafts (1202)Document7 pagesUse Reuse and Salvage Guidelines For Measurements of Crankshafts (1202)TASHKEELNo ratings yet
- Chap6 Part1Document15 pagesChap6 Part1Francis Renjade Oafallas VinuyaNo ratings yet
- Channels of CommunicationDocument3 pagesChannels of CommunicationIrin ChhinchaniNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Dry Wall, Ceiling, and Painting WorksDocument29 pagesDry Wall, Ceiling, and Painting WorksFrance Ivan Ais100% (1)
- HelloDocument31 pagesHelloShayne Dela DañosNo ratings yet
- Review of Related LiteratureDocument9 pagesReview of Related LiteratureMarion Joy GanayoNo ratings yet
- Baybay - Quiz 1 Code of EthicsDocument2 pagesBaybay - Quiz 1 Code of EthicsBAYBAY, Avin Dave D.No ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Facilities Strategic Asset Management Plan TemplateDocument85 pagesFacilities Strategic Asset Management Plan Templateoli mohamedNo ratings yet
- 1 3 Quest-Answer 2014Document8 pages1 3 Quest-Answer 2014api-246595728No ratings yet
- IsaiahDocument7 pagesIsaiahJett Rovee Navarro100% (1)
- 5 Point Scale PowerpointDocument40 pages5 Point Scale PowerpointMíchílín Ní Threasaigh100% (1)
- E F Eng l1 l2 Si 011Document2 pagesE F Eng l1 l2 Si 011Simona ButeNo ratings yet
- PEDIA OPD RubricsDocument11 pagesPEDIA OPD RubricsKylle AlimosaNo ratings yet
- IAB Digital Ad Operations Certification Study Guide August 2017Document48 pagesIAB Digital Ad Operations Certification Study Guide August 2017vinayakrishnaNo ratings yet
- Steps For Copyright ApplicationDocument7 pagesSteps For Copyright ApplicationLeah MedenillaNo ratings yet
- Directory of Schools For The Deaf in The PhilippinesDocument6 pagesDirectory of Schools For The Deaf in The PhilippinesVERA Files100% (1)
- Problem Based LearningDocument23 pagesProblem Based Learningapi-645777752No ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Evolution of Designed Industrial Symbiosis Networks in The Ulsan Eco-Industrial Park - Research and Development Into Business ADocument10 pagesEvolution of Designed Industrial Symbiosis Networks in The Ulsan Eco-Industrial Park - Research and Development Into Business Asanyukta sinhaNo ratings yet
- E-Governance Horizon Report 2007 PDFDocument240 pagesE-Governance Horizon Report 2007 PDFtouhedurNo ratings yet
- DODGER: Book Club GuideDocument2 pagesDODGER: Book Club GuideEpicReadsNo ratings yet
- PH Water On Stability PesticidesDocument6 pagesPH Water On Stability PesticidesMontoya AlidNo ratings yet
- Contoh Rancangan Pengajaran Harian (RPH)Document7 pagesContoh Rancangan Pengajaran Harian (RPH)Farees Ashraf Bin ZahriNo ratings yet
- Ancient Egyptian TimelineDocument5 pagesAncient Egyptian TimelineMariz Miho100% (2)
- A Brief History of LinuxDocument4 pagesA Brief History of LinuxAhmedNo ratings yet
- Why Nations Fail - SummaryDocument3 pagesWhy Nations Fail - SummarysaraNo ratings yet
- Governance Whitepaper 3Document29 pagesGovernance Whitepaper 3Geraldo Geraldo Jr.No ratings yet
- Instant Loss On a Budget: Super-Affordable Recipes for the Health-Conscious CookFrom EverandInstant Loss On a Budget: Super-Affordable Recipes for the Health-Conscious CookRating: 3.5 out of 5 stars3.5/5 (2)
- Forever Strong: A New, Science-Based Strategy for Aging WellFrom EverandForever Strong: A New, Science-Based Strategy for Aging WellNo ratings yet