Professional Documents
Culture Documents
Transient Response: 54 Shock
Uploaded by
SABRINA DA SILVAOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Transient Response: 54 Shock
Uploaded by
SABRINA DA SILVACopyright:
Available Formats
54
CHAPTER 3 n Shock
replacement during resuscitation should produce clinicians can slow the fluids to maintenance rates.
a urinary output of approximately 0.5 mL/kg/hr These patients typically have lost less than 15% of their
in adults, whereas 1 mL/kg/hr is adequate urinary blood volume (class I hemorrhage), and no further fluid
output for pediatric patients. For children under 1 bolus or immediate blood administration is indicated.
year of age, 2 mL/kg/hr should be maintained. The However, typed and crossmatched blood should be
inability to obtain urinary output at these levels kept available. Surgical consultation and evaluation
or a decreasing urinary output with an increasing are necessary during initial assessment and treatment
specific gravity suggests inadequate resuscitation. of rapid responders, as operative intervention could
This situation should stimulate further volume still be necessary.
replacement and continued diagnostic investigation for
the cause.
Patients in early hypovolemic shock have respiratory Transient Response
alkalosis from tachypnea, which is frequently followed
by mild metabolic acidosis and does not require Patients in the second group, “transient responders,”
treatment. However, severe metabolic acidosis can respond to the initial fluid bolus. However, they
develop from long-standing or severe shock. Metabolic begin to show deterioration of perfusion indices as
acidosis is caused by anaerobic metabolism, as a result the initial fluids are slowed to maintenance levels,
of inadequate tissue perfusion and the production indicating either an ongoing blood loss or inadequate
of lactic acid. Persistent acidosis is usually caused resuscitation. Most of these patients initially have
by inadequate resuscitation or ongoing blood loss. lost an estimated 15% to 40% of their blood volume
In patients in shock, treat metabolic acidosis with (class II and III hemorrhage). Transfusion of blood and
fluids, blood, and interventions to control hemorrhage. blood products is indicated, but even more important
Base deficit and/or lactate values can be useful in is recognizing that such patients require operative
determining the presence and severity of shock, and or angiographic control of hemorrhage. A transient
then serial measurement of these parameters can be response to blood administration identifies patients
used to monitor the response to therapy. Do not use who are still bleeding and require rapid surgical
sodium bicarbonate to treat metabolic acidosis from intervention. Also consider initiating a massive
hypovolemic shock. transfusion protocol (MTP).
Patterns of Patient Response Minimal or No Response
The patient’s response to initial fluid resuscitation is Failure to respond to crystalloid and blood admin-
the key to determining subsequent therapy. Having istration in the ED dictates the need for immediate,
established a preliminary diagnosis and treatment plan definitive intervention (i.e., operation or angio-
based on the initial assessment, the clinician modifies embolization) to control exsanguinating hemorrhage.
the plan based on the patient’s response. Observing On very rare occasions, failure to respond to fluid
the response to the initial resuscitation can identify resuscitation is due to pump failure as a result of
patients whose blood loss was greater than estimated blunt cardiac injury, cardiac tamponade, or tension
and those with ongoing bleeding who require operative pneumothorax. Non-hemorrhagic shock always
control of internal hemorrhage. should be considered as a diagnosis in this group of
The potential patterns of response to initial fluid patients (class IV hemorrhage). Advanced monitoring
administration can be divided into three groups: techniques such as cardiac ultrasonography are useful
rapid response, transient response, and minimal or to identify the cause of shock. MTP should be initiated
no response. Vital signs and management guidelines in these patients (n FIGURE 3-4).
for patients in each of these categories were outlined
earlier (see Table 3-2).
Blood R epl ac ement
Rapid Response
The decision to initiate blood transfusion is based on
Patients in this group, referred to as “rapid responders,” the patient’s response, as described in the previous
quickly respond to the initial fluid bolus and become section. Patients who are transient responders or
hemodynamically normal, without signs of inadequate nonresponders require pRBCs, plasma and platelets
tissue perfusion and oxygenation. Once this occurs, as an early part of their resuscitation.
n BACK TO TABLE OF CONTENTS
You might also like
- Septic Shock TreatmentDocument22 pagesSeptic Shock TreatmentAdreiTheTripleA100% (1)
- 4 Phases of IV Fluid Therapy FinalDocument29 pages4 Phases of IV Fluid Therapy FinalLuqmanul Hakim Junaidden100% (1)
- 160 78-m1Document70 pages160 78-m1George100% (7)
- Heat Cured ElastomersDocument40 pagesHeat Cured ElastomerslberrierNo ratings yet
- GundamDocument25 pagesGundamBattlecruiser ScharnhorstNo ratings yet
- Monitoring and Intervention for the Critically Ill Small Animal: The Rule of 20From EverandMonitoring and Intervention for the Critically Ill Small Animal: The Rule of 20No ratings yet
- Arithmetic Mean PDFDocument29 pagesArithmetic Mean PDFDivya Gothi100% (1)
- Sepsis - 3Document36 pagesSepsis - 3Mohd Ekhwan DarusNo ratings yet
- Uf & Sodium ProfilingDocument32 pagesUf & Sodium Profilinggramaseva Parishath100% (1)
- Educational Strategic Plans in Nigeria: Challenges of Implementation and Ways ForwardsDocument7 pagesEducational Strategic Plans in Nigeria: Challenges of Implementation and Ways ForwardsresearchparksNo ratings yet
- Assessment of bleeding Shock in a Politraumatized PatientFrom EverandAssessment of bleeding Shock in a Politraumatized PatientNo ratings yet
- CongressWatch #197: RA 1337-Innovative Startup ActDocument1 pageCongressWatch #197: RA 1337-Innovative Startup ActMakati Business ClubNo ratings yet
- Digestive System Lesson PlanDocument5 pagesDigestive System Lesson PlanSachi Summers100% (2)
- Refractory Septic ShockDocument5 pagesRefractory Septic ShockBrian Antonio Veramatos LopezNo ratings yet
- Assessing Volume StatusDocument12 pagesAssessing Volume StatusMoises Torres AlvarezNo ratings yet
- Transfusion Medicine and Hemostasis: Clinical and Laboratory AspectsFrom EverandTransfusion Medicine and Hemostasis: Clinical and Laboratory AspectsRating: 4 out of 5 stars4/5 (9)
- S. 14.0 Fluid Therapy - Trauma CasesDocument7 pagesS. 14.0 Fluid Therapy - Trauma CasesroropujiNo ratings yet
- Seminars 2019 PDFDocument200 pagesSeminars 2019 PDFpaingmyintNo ratings yet
- Gtcicyrcp Como Valorar La Respuesta A Volumen en La UciDocument18 pagesGtcicyrcp Como Valorar La Respuesta A Volumen en La UciConny SaldiviaNo ratings yet
- Clinical Evaluation Test Result Trends: DiagnosisDocument3 pagesClinical Evaluation Test Result Trends: DiagnosisStephen CrossNo ratings yet
- Fluid and Electrolyte Management For The Surgical PatientDocument17 pagesFluid and Electrolyte Management For The Surgical PatientFery López NavedaNo ratings yet
- Fluid Management & Blood Component Therapy: Key ConceptsDocument31 pagesFluid Management & Blood Component Therapy: Key ConceptsMohammad Pino HakimNo ratings yet
- SOSD Phases of Fluid ResuscitationDocument8 pagesSOSD Phases of Fluid ResuscitationAvinash KumbharNo ratings yet
- Assessment of Hypovolaemia in The Critically IllDocument10 pagesAssessment of Hypovolaemia in The Critically IllrjerezrNo ratings yet
- Avoiding Common Problems Associated With Intravenous Fluid TherapyDocument13 pagesAvoiding Common Problems Associated With Intravenous Fluid TherapyDeepak AnNo ratings yet
- Shock: Ivan Mucharry Dalitan - PPDS Orthopaedi & Traumatologi Semester IVDocument5 pagesShock: Ivan Mucharry Dalitan - PPDS Orthopaedi & Traumatologi Semester IVusnulNo ratings yet
- 6-Pharm Care Pada Terapi CairanDocument34 pages6-Pharm Care Pada Terapi CairanApt RatnaningrumNo ratings yet
- Perioperativefluid Therapy: Denise Fantoni,, Andre C. ShihDocument12 pagesPerioperativefluid Therapy: Denise Fantoni,, Andre C. ShihDaniela BenavidesNo ratings yet
- Bundle 3 Hour Step4 FluidsDocument4 pagesBundle 3 Hour Step4 FluidsgythrieNo ratings yet
- 2013 IF Fluids in AdultsDocument19 pages2013 IF Fluids in AdultsltgcanlasNo ratings yet
- Introduction To Critical Care Nursing 6th Edition Sole Test BankDocument38 pagesIntroduction To Critical Care Nursing 6th Edition Sole Test Bankgabrielnt3me100% (15)
- Treatment: Loss of Plasma VolumeDocument0 pagesTreatment: Loss of Plasma VolumeIsra AjahNo ratings yet
- 6 PDFDocument2 pages6 PDFellya theresiaNo ratings yet
- Desescalada de FluidosDocument3 pagesDesescalada de FluidosWendy JuampoNo ratings yet
- MalariaDocument5 pagesMalariaMo MonuNo ratings yet
- Pi Is 0039610912000163Document17 pagesPi Is 0039610912000163Hend Al-DreesNo ratings yet
- Functional Hemodinamik MonitoringDocument4 pagesFunctional Hemodinamik MonitoringYudhi AuliaNo ratings yet
- Malbrain Et Al-2022-Intensive Care MedicineDocument6 pagesMalbrain Et Al-2022-Intensive Care Medicinewaldemar russellNo ratings yet
- Burns - Fluid Volume, Risk For DeficientDocument3 pagesBurns - Fluid Volume, Risk For Deficientmakyofrancis20No ratings yet
- 272 Liver Disease Part 2Document7 pages272 Liver Disease Part 2Aliyu Bashir AdamuNo ratings yet
- Ventilatory SupportDocument21 pagesVentilatory SupportAllahbesertkitaNo ratings yet
- Sepsis Parte 1Document16 pagesSepsis Parte 1Maria AlejandraNo ratings yet
- Upper GI BleedDocument8 pagesUpper GI BleedbbyesNo ratings yet
- GiftasupDocument50 pagesGiftasupFizza SiddiquiNo ratings yet
- Santoso2005Document11 pagesSantoso2005ayubahriNo ratings yet
- Plex 2012Document6 pagesPlex 2012Sundar RamanathanNo ratings yet
- Beyond Mean Arterial Pressure and Lactate Perfusion End Points For Managing The Shocked PatientDocument14 pagesBeyond Mean Arterial Pressure and Lactate Perfusion End Points For Managing The Shocked PatientLuis Miguel VillanuevaNo ratings yet
- Sepsis y ShockDocument10 pagesSepsis y ShockJose Alonso Alcoser ArcilaNo ratings yet
- Hemorrhagic or Hypovolemic ShockDocument17 pagesHemorrhagic or Hypovolemic ShockSri AsmawatiNo ratings yet
- Ascorbic Acid NCPDocument8 pagesAscorbic Acid NCPJohann OrtizNo ratings yet
- Fluidoterapia DesrrescutiDocument6 pagesFluidoterapia DesrrescutiWilson Lukeny G. JoséNo ratings yet
- Inotrópicos y Vasopresores PDFDocument22 pagesInotrópicos y Vasopresores PDFJosé Luis Méndez ChagoyaNo ratings yet
- Journal of Critical Care: MD, PHD, FCCM, MDDocument11 pagesJournal of Critical Care: MD, PHD, FCCM, MDIrma Gladys Romero JondécNo ratings yet
- Lactate MonitoringDocument6 pagesLactate Monitoringaliv8s3624No ratings yet
- ABC ResuscitationDocument5 pagesABC ResuscitationIamTineshNo ratings yet
- Sepsis, Sirs and ModsDocument4 pagesSepsis, Sirs and ModsMayra Alejandra Prada SerranoNo ratings yet
- Severe Dengue in ICUDocument35 pagesSevere Dengue in ICUanaeshklNo ratings yet
- Sepsis Parte 2Document12 pagesSepsis Parte 2Maria AlejandraNo ratings yet
- Consider Abdominal Compartment Syndrome in Patients With Refractory HypotensionDocument26 pagesConsider Abdominal Compartment Syndrome in Patients With Refractory HypotensionHari AdityonugrohoNo ratings yet
- Test Bank For Introduction To Critical Care Nursing 7th Edition by Sole Full DownloadDocument16 pagesTest Bank For Introduction To Critical Care Nursing 7th Edition by Sole Full Downloadkristinajohnsoniryjaqcfsk100% (21)
- Approach ConsiderationsDocument5 pagesApproach ConsiderationsGunawan SetiawanNo ratings yet
- I.V. Fluid Therapy IDocument4 pagesI.V. Fluid Therapy IPrabath ChinthakaNo ratings yet
- Expert Statement For Management Hypovolemia in Sepsis PDFDocument8 pagesExpert Statement For Management Hypovolemia in Sepsis PDFRobi HeryantoNo ratings yet
- BMJ g7620 FullDocument10 pagesBMJ g7620 FullRui PenedaNo ratings yet
- Critical Care 123Document66 pagesCritical Care 123Mr.ShazNo ratings yet
- Chemistry Module 3Document14 pagesChemistry Module 3MASHNo ratings yet
- Concept MapDocument1 pageConcept Mapapi-402935758No ratings yet
- Report Text The Duck Billed Platypus: (Ornithorhynchus Anatinus)Document2 pagesReport Text The Duck Billed Platypus: (Ornithorhynchus Anatinus)Lilis IndriyaniNo ratings yet
- Chem 152 Lab ReportDocument21 pagesChem 152 Lab Reportapi-643022375No ratings yet
- 5 Waves AnswersDocument2 pages5 Waves AnswersNoor Ulain NabeelaNo ratings yet
- Gunnar Fischer's Work On Ingmar Bergman's The Seventh Seal and Wild StrawberriesDocument6 pagesGunnar Fischer's Work On Ingmar Bergman's The Seventh Seal and Wild StrawberriesSaso Dimoski100% (1)
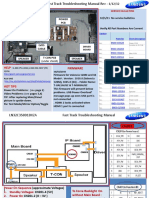
- Samsung LN55C610N1FXZA Fast Track Guide (SM)Document4 pagesSamsung LN55C610N1FXZA Fast Track Guide (SM)Carlos OdilonNo ratings yet
- Republic of The Philippines Department of Education Deped Complex, Pasig City Science Iii K To 12 Curriculum Guide Planner / Budget of WorkDocument3 pagesRepublic of The Philippines Department of Education Deped Complex, Pasig City Science Iii K To 12 Curriculum Guide Planner / Budget of WorkLedie Lou Cetoy SuperalesNo ratings yet
- Grade 7 - R & C - Where Tigers Swim - JanDocument15 pagesGrade 7 - R & C - Where Tigers Swim - JanKritti Vivek100% (3)
- UntitledDocument45 pagesUntitledjemNo ratings yet
- Symantec Endpoint Protection 14.3 RU3 Release NotesDocument28 pagesSymantec Endpoint Protection 14.3 RU3 Release NotesMilind KuleNo ratings yet
- Course: Consumer Behaviour: Relaunching of Mecca Cola in PakistanDocument10 pagesCourse: Consumer Behaviour: Relaunching of Mecca Cola in PakistanAnasAhmedNo ratings yet
- Exploded View: 22031050000281 RF-S218XAR1 Product Model Customer ModelDocument9 pagesExploded View: 22031050000281 RF-S218XAR1 Product Model Customer ModelPablo GuerraNo ratings yet
- E650E650M-17 Guía Estándar para El Montaje de Sensores Piezoeléctricos de Emisión Acústica1Document4 pagesE650E650M-17 Guía Estándar para El Montaje de Sensores Piezoeléctricos de Emisión Acústica1fredy lopezNo ratings yet
- Body LanguageDocument17 pagesBody LanguageAR PiZaNo ratings yet
- Graphs in ChemDocument10 pagesGraphs in Chemzhaney0625No ratings yet
- Theater InstallationDocument7 pagesTheater InstallationtemamNo ratings yet
- Rapid History Taking: 1. Patient ProfileDocument3 pagesRapid History Taking: 1. Patient ProfileTunio UsamaNo ratings yet
- A Review of The Mental Workload LiteratureDocument36 pagesA Review of The Mental Workload LiteratureArlene LaguaNo ratings yet
- VisualizationDocument2 pagesVisualizationKIRAN H SNo ratings yet
- Combustion FundamentalsDocument30 pagesCombustion FundamentalsPrem SagarNo ratings yet
- Annex 1: Homeroom Guidance Monitoring Tool (School Level) Homeroom Guidance Monitoring ToolDocument2 pagesAnnex 1: Homeroom Guidance Monitoring Tool (School Level) Homeroom Guidance Monitoring ToolMariel Gregore0% (1)
- Pengaruh Pemberian Dosis Pupuk Urea Terhadap Pertumbuhan Tanaman Bayam Cabut Putih (AmaranthusDocument10 pagesPengaruh Pemberian Dosis Pupuk Urea Terhadap Pertumbuhan Tanaman Bayam Cabut Putih (AmaranthusMartha YhunickeNo ratings yet