Professional Documents
Culture Documents
Water 1
Water 1
Uploaded by
bidan22Original Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Water 1
Water 1
Uploaded by
bidan22Copyright:
Available Formats
Journal of Nursing Research Vol. 11, No.
4, 2003
The Decision-Making Experience of Mothers Selecting Waterbirth
Chia-Jung Wu Ue-Lin Chung*
ABSTRACT: Waterbirth has been a way of birth for 20 to 30 years abroad, while in Taiwan, only in the past three years
have some women chosen water birth. This study aims to explore the decision-making experience of mothers selecting waterbirth. A phenomenological approach was employed in this study. Nine mothers who had given birth in water successfully in the midwife clinic in the past year were chosen and one-by-one, face-to-face interviews were conducted. The research tools included a basic information questionnaire, a semi-structured and open-ended interview guide, and an audio recorder to record the entire interviews. The content of the interviews was faithfully transcribed and analyzed with Giorgis phenomenological method and Lincoln and Gubas qualitative credibility. Four main concepts concluded from the experience context of the studied women were: (1) Dissatisfaction with existing obstetric practices; (2) Demonstration of autonomy; (3) Consideration of relatives attitude; and (4) Employing strategies to achieve goals. The result of this study can help nursing staff and the public to understand the decision-making experience of mothers selecting waterbirth, and help the contemplation of health care providers with respect to furnishing a more humanized birth environment in hospitals. Key Words: waterbirth, decision-making process.
Introduction
Human waterbirth was first invented by the Russian physiologist Igor Charkovsky in the 1960s. Observing water animals delivering in the water, she found that water could alleviate the impact of gravity on brain cells during the birth of the fetus. She thus thought that waterbirth could be a good childbirth method. In the 1970s, Dr. Michel Odent in France started to introduce waterbirth to hospitals, and Dr. Michael Rosenthal introduced it to the USA in the 1980s. As of 1996, 25,000 babies had been delivered by waterbirth in the USA, while 20,000 babies were delivered by waterbirth in the UK in 1993 alone. The estimated number of babies delivered by waterbirth worldwide is 150,000 from 1985 to 1999 (Harper, 2000; Lin, 2000). There has been a 20- to 30-year history of waterbirth abroad, but waterbirth is still in the rudimentary phase in Taiwan. There have been 30 mothers to date choosing to deliver by waterbirth since September of 1999 in Taiwan; all of these deliveries were carried out in the midwife
clinic. The researchers wanted to study why these women chose waterbirth, and what their decision-making experiences were. So far there has been a lack of studies on waterbirth in Taiwan. Most studies abroad on waterbirth are quantitative, while fewer studies are qualitative. Hence, our study used the phenomenological research method with interviews to collect the data. The results could offer an understanding of the decision-making experience of mothers selecting waterbirth, as a reference for the public and medical staff in Taiwan.
Literature Review
Definition of waterbirth Waterbirth is one way of delivery whereby low risk women immerse themselves in specially designed pools or tubs, and deliver in the posture in which they feel most comfortable. Because they are bathing in warm water during delivery, their muscles are relaxed, and this helps to reduce pain (Milner, 1988).
RN, MSN, Instructor, Ching Kuo Institute of Management and Health; *RN, MN, EdD, Professor & President, National Taipei College of Nursing. Received: June 27, 2003 Revised: September 4, 2003 Accepted: September 12, 2003 Address correspondence to: Ue-Lin Chung, No. 365, Ming-Te Rd., Taipei 112, Taiwan, ROC. Tel: 886(2)2822-7101 ext. 2000; Fax: 886(2)2822-2432; E-mail: uelin@mail1.ntcn.edu.tw
261
J. Nursing Research Vol. 11, No. 4, 2003
Chia-Jung Wu et al.
Reports about waterbirth abroad (1) Aspects of perineal injuries, labor progress, analgesic treatment, and satisfaction with delivery There are inconsistent study results about the impact of waterbirth on the degree of perineal injuries. Some studies (Burns & Greenish, 1993; Geissbuhler & Eberhard, 2000) showed that the probabilities of first- and second-degree tears in the waterbirth group were higher than those in the non-waterbirth group. However, Garland and Jones (1997) stated that the waterbirth and non-waterbirth mothers had the same degree of perineal tears. Conversely, the study of Rush et al. (1996) supported the view that waterbirth is more likely to maintain the perineum intact. As for labor, Halek (2000) pointed out that the survey of 602 lying-in women conducted by the Royal Society of Medicine during 1989-1994 found waterbirth labor to be faster than traditional labor. As for analgesia, most studies concluded that analgesia (e.g., analgesic, epidural analgesia) is less required in waterbirth deliveries (Burke & Kifoyle, 1995; Burns & Greenish, 1993; Geissbuhler & Eberhard, 2000; Rush et al., 1996). Most studies pointed out that mothers who choose waterbirth have greater satisfaction, and are more likely to be willing to choose this childbirth method next time (Burke & Kifoyle, 1995; Church, 1989; Garland & Jones 1997; Geissbuhler & Eberhard, 2000). Additionally, Geissbuhler and Eberhard (2000) found that mothers choosing waterbirth have less blood loss and lower episiotomy rates than mothers choosing traditional childbirth methods. In general, most studies support the following conclusions: mothers choosing waterbirth have faster labor, lower need for analgesia, and lower episiotomy rates, less blood loss, and a higher degree of satisfaction at their delivery experience; waterbirth newborns have higher Apgar scores. However, whether waterbirth decreases the probability of perineal tears remains inconclusive. (2) Infection rate Most studies show that infection rate of waterbirth is minimal, but there are some studies reports of waterbirthrelated infection. For example, Rawal, Shah, Stirk, & Mehtar (1994) stated that the contaminated birth tub will cause newborn bacterial infection (e.g. Pseudomonas aeruginse, Klebsiella pneumoniae, etc.) These bacteria usually grow in the water pump, heating systems, pipes and water. There is a report on a newborn baby developing Pseudomonas sepsis after waterbirth. Hence, Rawal et al.
(1994) emphasized the importance of cleaning the birth tub with water for waterbirth deliveries. (3) Newborn mortality rate Gilbert and Tookey (1999) sampled 4032 low risk women who chose waterbirth in England and Wales in U.K. They found that waterbirth did not have higher mortality rate than that the traditional childbirth method did. Waterbirth in Taiwan Waterbirth has been implemented to date at a midwifery clinic in Hsinchuang in Taiwan. Three years ago, a woman who had studied in France wanted to experience the wonderful waterbirth she had read about on the Internet. She was then referred to a midwife with 26-year midwifery experience. Eventually Taiwan had its first waterbirth. According to the midwife at the clinic, waterbirth is covered by the National Health Insurance program. Waterbirth at home is not easy because the bathtub at home is usually too small, so that the mother has difficulty changing her position. Hence, most mothers choosing waterbirth deliver their babies in the large-size bathtubs at the midwifery clinic. In addition, the water used in the bathtub is sterilized. The procedures of waterbirth are approximately the same in Taiwan as in other countries. Details are described as follows (Harper, 2000; Michelle, 2000; Tsai, 2001, Aug.): (1) First, add filtered sterile water to the pool or bathtub. The water temperature is kept at about 37 C. When the mothers cervical opening is 5 cm wide with strong and regular contractions, she will wash her body and then enter the pool or bathtub with the water level chest high and covering her abdomen. (2) When the newborns head is about to come out, the midwife will tell the mother to open her mouth. Meanwhile, the mother or midwife can support the perineum with her hands so that the newborns head can come out slowly. When the newborns head comes out, the midwife will touch its neck and check whether the umbilical cord is wrapped around the babys neck. (3) If the examination confirms that the umbilical cord is not wrapped around the babys neck, the midwife will encourage the mother to draw a breath and keep exerting herself, and thereby the baby can be delivered successfully. (4) When the newborn is completely delivered, the midwife usually will not remove the baby from the water immediately if its condition is fine. (5) One to five minutes later, the newborn is slowly removed from the water and held close to the mothers chest.
262
Decision-Making Experience of Waterbirth Mothers
J. Nursing Research Vol. 11, No. 4, 2003
(6) When the newborns umbilical artery stops beating, the father cuts the umbilical cord. (7) When the umbilical cord is cut, prepare for the third stage of labor (helping the mother to leave the bathtub and lie on the temporary delivery table. (8) When the mother leaves the water, wrap her body with a blanket to keep her warm. (9) Check if there are perineal tears after the placenta is delivered. Suture the wounds if there are tears. (10) After the waterbirth is complete, the mother should perform breast-feeding as soon as possible. Pay close attention to the postpartum uterine contractions. (11) Sterilize the bathtub and other facilities and keep them dry.
(1997): reading of interviews, division into meaning units, transformation, synthesis and general structure. These are also central concepts of the mothers decision-making process and experience.
Rigor
We used the four indicators of trustworthiness proposed by Lincol and Guba (1985): credibility, transferability, dependability, and confirmability. With regard to credibility, we have started to contact waterbirth mothers at least 10 months before the study was conducted. As we researchers involved ourselves deeply in the study, we could more easily understand and observe the characteristics of phenomena. During the interviews, the participants emotions and body language were thoroughly documented. In the process of data analysis, the investigator and a graduate student with the same training background separately analyzed the data in terms of meaning units, and then compared their results. When the results were different, the two analysts sought a consensus through discussion. Transferability relies on thick description. Each interview of these nine participants took 1 to 1.5 hours, so we had thick description for analysis. The concepts derived from the analysis can give guidance for clinical practice. With regard to dependability, our study documented the interview scenarios using audio recording and non-language information. The data were analyzed and consistency was assured. With regard to confirmability, the audio tapes, documents, interview records, post-interview logs, and data analysis results were all encoded, classified and well preserved. Thus future confirmation or tracing is possible.
Methods
Study Design
We used a qualitative research method. The study is aimed at examining the subjective experience of the decision-making process of mothers choosing waterbirth. We employed phenomenological interviews to collect the experiences of the participants.
Participants
All participants came from the single midwifery clinic where waterbirth is performed. The participants were eligible to enter our study if they met the following criteria: citizens of Taiwan, speaking Mandarin or Taiwanese, having had a successful waterbirth experience within the past year, and being willing to participate in our study. Nine participants were interviewed from December 2001 to April 2002. In fact, no new data were derived from the seventh participant. But to confirm that no new data would be obtained from new participants, two more participants were interviewed.
Results
Data Collection
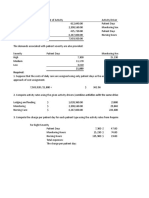
In order to keep the data collection consistent, the investigator was also the interviewer. The interviews were semi-structured. The interview started with questions like Would you please tell us what your expectation for delivery is? Why did you choose waterbirth? How did you make that decision? . The interviewer never tried to influence the responses of the interviewee. The interview lasted from 60 to 90 minutes. The locations of the interviews were mostly homes (eight participants) or quiet coffee shops. Nine mothers, aged 28-41, were interviewed in our study. They included four primiparas and five multiparas. In terms of educational status, one had a high school diploma, five had college degrees, and three had postgraduate degrees. Five were housewives, three were teachers, and one was in the service industry. Eight resided in Taipei and one in Taichung. All of the mothers chose to breastfeed, and their newborns were healthy. Four key concepts extracted from the Giorgi phenomenological data analysis of this study were feeling dissatisfied with existing obstetric practices, demonstrating autonomy, considering relatives attitudes, and employing strategies to achieve goals.
Data Analysis
The analytical procedure was phenomenological in nature and was comprised of five steps, inspired by Giorgi
263
J. Nursing Research Vol. 11, No. 4, 2003
Chia-Jung Wu et al.
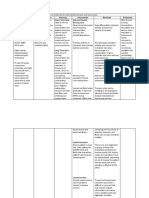
Dissatisfaction With Existing Obstetric Practices
Dissatisfaction with the current medical care system The participants thought that lying-in women are usually encouraged to have a cesarean section (CS). They regarded intravenous (IV) medication and fasting as preparatory procedures for CS, and were afraid of CS. As participant 1 put it, CS is hinted at for mothers in many hospitals in Taiwan, unless the doctors are decent. Why is it necessary to have IV medication, fasting, and intravenous uterine contractor? One will become weak after receiving such treatment, which thereby leads to CS. The other participant described her impression of visiting a hospital as, The delivery room in the obstetric hospital is terrifying. Everything is white and there is a lot of cold metal material. The delivery room looks like an operating room. basically, I suppose that one only goes to the hospital because of sickness. However, doctors usually choose to do CS or use forceps to facilitate the labor, which is fast and brutal. They do not offer a means of relaxation (Participant No. 5). One participant felt that she was being treated as an object on the production line. She though there was no respect, support, warmth, or autonomy in hospitals. The design of the delivery table and the environmental temperature did not meet the needs of mothers. As participant No. 6 put it, I felt like a case or object being packed. Mothers and babies are not treated as independent individuals. The delivery room is not a warm place, and humanity is not considered. A lying-in woman is manipulated and controlled in the hospital! The delivery table is not ergonomically designed. The room temperature is lower than 20 EC. Under such circumstances, the delivery may be more torturous in the wintertime. Negative previous delivery experience The participants feared the non-humanistic medical procedures that they had encountered during their previous deliveries. They found it hard to bear the negligence of medical staff, feelings of being threatened, painful experience of CS, and postpartum complications. As participant No. 2 said, My first delivery was carried out at a clinic. The nurses were not competent in handling my problems, and the doctor arrived when the babys head had come out. That was so terrible! I was in darkness and terror. The placenta was not delivered naturally, so I received a uterine contractor injection. I was so terrified! Another participant (No. 9) also mentioned a similar experience of the doctor being late for her delivery. She was told to hold it when her baby was about to come out.
Such pain was worse than her labor pains. She thought the hospital did not do a good job at all. Experience that falls short of expectations The participants wished to be accompanied by family members during their deliveries. They wanted to perform breast-feeding right after the baby was born. They also wished to try VBAC (Vaginal Birth After Cesarean) and not to need episiotomy. However, these demands cannot be met in the current medical care system. As participant No. 1 put it, When I attended the Mothers Course, I asked if the hospital encouraged the father-to-be to accompany the delivery. The Chief Executive of that hospital said the delivery might be disturbed by the father-to-be. I dont think that the hospital takes our concerns seriously and the hospital does not implement up-to-date care procedures. I was so disappointed.
Demonstration of Autonomy
Due to dissatisfaction with the current medical care system, the participants insisted on their autonomy in their deliveries, and hence they tried to understand and scrutinize childbirth methods outside the system. Autonomy in delivery The participants conceived that they should be able to decide their own childbirth methods. They thought deliveries in hospitals would be dominated by doctors, and doctors would perform CS whenever possible. As participant No. 5 said, My husband supposes that every mother should be able to have a normal spontaneous delivery. When one goes to the hospital, the doctor cannot wait too long, so they will perform CS after a certain point of time (pause). My labor pains were so hard to bear then, that I might have changed my mind at any time. But I told myself and my husband, when I was shivering in pain, that I had to insist [on waterbirth], otherwise all my efforts would have been in vain. Why I insisted was because doctors dominate everything at hospitals. Understanding and scrutinizing alternative childbirth methods The search for alternative childbirth methods was driven by dissatisfaction with the current environment. These mothers assessed the current mainstream childbirth methods and informed themselves about the environment and waterbirth provided at midwifery clinics. Participant No. 6 said, I carefully examined the information about both deliveries at hospitals and childbirth methods outside hospi-
264
Decision-Making Experience of Waterbirth Mothers
J. Nursing Research Vol. 11, No. 4, 2003
tals. I decided to choose waterbirth in the last month of my pregnancy. I received antenatal examinations at both hospitals and midwifery clinics. So, it was not the way other people saidthat I did it simply as an idea! Participant No. 1 said I told my family not to worry. I had assessed waterbirth for a long time, and I had great confidence in it. All the information was saved and documented. Trusting the midwife Although the participants thought midwifery has become gradually obsolete, and facilities at midwifery clinics are less advanced than those at hospitals, they still appreciated the enthusiasm and rich midwifery experience. As the participant No. 7 said, Ms. Tsai [the waterbirth midwife] was so eager to help me, and I took her advice. It is said that childbirth is dangerous, so I have to rely on a skillful, experienced, and attentive doctor. I know midwifery has become less and less popular, but I still have confidence in the techniques of Ms. Tsai. Fulfilling individual dignity of life at the price of taking risks and pressure The participants thought that delivery is an adventure, so they were under great stress and suffered consequences in order to achieve their dignity of life. As participant No. 4 said, Delivery is like an adventure. I decided not to have any operation! I trust Ms. Tsai [the midwife], and will never undergo CS again. Anyway, I am willing to face all the stress and misunderstandings of my family and friends, and accept the consequences. Participant No. 6 said, The pressure came not only from my husbands parents but also my friends. They had no reason to object to my plan since they certainly had less knowledge about waterbirth than I did. I appreciated their concern, but I was so tired of such stress! I could not guarantee that waterbirth would work, and I didnt want to spend efforts explaining anything. All I wanted to do was achieve my goal. So, I kept a low profile during the whole process, I was willing to put up with any stress in order to achieve my dignity of my life.
ipant No. 2 said, Many people in the breast-feeding club had their deliveries at the midwifery clinics, and they were all very satisfied. My parents also agreed with me, because my mother gave birth to her three children at the midwifery clinic. Worries Some relatives had worries about waterbirth although they did not object to it. For example, the family members of participant No. 3 were concerned about the operation scar from a previous CS; participant No. 4 was worried about safety at the midwifery clinic. Participant No. 4 said, My sisters could not believe I decided to deliver at the midwifery clinic, let alone choosing waterbirth. My husband, who has studied traditional Chinese medicine, was worried, too. I have a friend who passed away on the delivery table, and I feel very sad every time I think of this. Luckily my delivery was successful, and everyone was so relieved. Objection Most relatives of the participants did not trust the competency of midwives, and believed that deliveries at hospitals were much safer. Participant No. 1 said, My parents tried to persuade me to deliver at a hospital after they learned I planned to choose waterbirth. My mother-in-law, who works in a hospital, had no trust in the midwife at all. Participant No. 5 said, My father and cousin, who have studied medicine, suggested I should give up the idea of waterbirth at the midwifery clinic. Other relatives who have midwifery licenses also suggested that I should deliver in hospital.
Employing Strategies to Achieve Goals
When relatives held different opinions on waterbirth, the participants might choose some strategies to either reach a consensus among their relatives, or conceal their decisions from their relatives. Attempts at persuasion to reach a consensus The participants used all opportunities to let their husbands read documents about waterbirth, and further explained the benefits of waterbirth to their family members. Participant No. 3 said, I passed some reports about waterbirth to him, and asked him to accompany me when I had my antenatal exams at the midwifery clinic, where he could watch videos and read relevant information. Hence he became less worried after he had more knowledge about waterbirth. Participant No. 8 said, My family could not accept waterbirth and I had to tell them some concepts to help them understand this. They
Consideration of Relatives Attitude
The participants consulted their relatives for their opinions and support, but they encountered various degrees of support and objection. Support Family support, particularly from the husband, is very important for enhancing the confidence of mothers. Partic-
265
J. Nursing Research Vol. 11, No. 4, 2003
Chia-Jung Wu et al.
asked if the water was clean, if the facilities were good enough. They were worried about the scenario if CS was needed. I had to assure them that hospitals were very close just in case of an emergency. I also reminded my parents-in-law of the fact that my mother-in-law delivered at home, not at a hospital. We saw news on TV about women delivering in cars, etc. We were born with the ability to deliver naturally, not necessarily by CS. Mock situations and concealing their decisions intentionally The participants might conceal their decisions from their relatives, and only tell their family members about their deliveries after they delivered their babies. Participant No. 1 said, I had had episodic labor pain every 5 to 10 minutes until midnight. I let my husband know right away while I concealed it from other family members. My mother saw me walk awkwardly, but I still said I was fine. After my delivery was successfully done, I called my family and told them that I just gave birth to my baby. I knew my parents could never accept the idea of waterbirth at the midwifery clinic. Participant No. 4 said, I did not mention my decision to have a waterbirth to my parents or my husbands parents. They just knew when my baby would be due, and that I probably would deliver at the clinic I did not want them to know that I had had a waterbirth. Participant No. 6 had prepared some solutions to several scenarios beforehand: If my labor pains occurred at my parents house, they might stop me from going to the midwifery clinic I used to live with my parents in Taipei, so I moved to Taoyuan after my estimated date of delivery. My husband and I pretended to go out once in a while when we stayed in Taoyuan, so that I could go to the midwifery clinic on a day my mother did not expect at all.
ers will start to consider alternative childbirth methods. The midwife Sha-Ning Tsai (2002) surveyed 22 mothers choosing waterbirth between January 1999 and December 2001, and found that many of these mothers chose waterbirth because they did not want to undergo CS again. The interviews with the nine participants showed that each of them complained about the over-medicalization of deliveries at hospitals nowadays. As Malterud (1993) mentioned, there are two sources of suppression from the medical care system for women: medicalization and negligence of womens grievances and feelings. These two sources of suppression also exist in Taiwan.
Demonstration of Autonomy
When the participants became dissatisfied with the current medical care system, they understood that they should decide their own childbirth methods. Wagner (2001) stated that women at hospitals could not have complete autonomy. They had to sign a self-discharge paper if they failed to negotiate with the hospital regarding their requests. The hospital would refuse to deliver the child. The same phenomenon happened to mothers in our study. Additionally, Hall and Holloway (1998) found that mothers choosing waterbirth had autonomy in waterbirth. They could move their own bodies and change postures as they wanted, in order to release their anxiety and control their labor pains. Also, these mothers could be accompanied by their family members, and thereby share their joy and pains with their family members. These requests, similar to the requests of our participants, could not be met at hospitals. In the decision-making process, the professional attitude of the midwife was very important. The participants appreciated the knowledge and skills of midwives, as well as the enthusiasm and rich midwifery experience of the midwife. Hall and Hollway (1998) reported that mothers were grateful that they were treated as equals and offered chances of negotiation. Therefore, the professional attitudes of the midwife played an important role in the decision-making process of mothers selecting waterbirth.
Discussion
We will discuss the four primary concepts one by one: 1. Dissatisfaction with existing obstetric practices; 2. Demonstration of autonomy; 3. Consideration of relatives attitude; and 4. Employing strategies to achieve goals.
Dissatisfaction With Existing Obstetric Practices
The participants rejected mainstream medical care and sought alternative childbirth methods mainly because of their dissatisfaction with the current medical environment for deliveries, and negative experience of previous deliveries. When doctors fall short of mothers expectations (e.g., doctors cannot accept VBAC), moth-
Consideration of Relatives Attitude
In our family-centered society, the participants still took into account the opinions of their relatives. In the decision-making process, the husbands usually supported their wives, while the husbands parents usually objected to waterbirth. Li and Lee (1998) examined the decision mak-
266
Decision-Making Experience of Waterbirth Mothers
J. Nursing Research Vol. 11, No. 4, 2003
ing experiences on amniocentesis of pregnant women with positive results on maternal serum screening for Downs syndrome, and found that husband was the most important supporter, while the husbands parents were usually objectors. Our study shows similar results.
Employing Strategies to Achieve Goals
The participants chose some strategies when facing the disagreement of their relatives. Li and Lee (1998) pointed out that women who had positive test results for Downs syndrome chose not to tell their husbands parents about their decisions to receive amniocentesis since their husbands parents objected to amniocentesis. These pregnant women tended to use indirect methods in order to understand what opinions their husbands parents held. Sometimes the women just chose to conceal their decisions to undergo amniocentesis from their husbands parents. Our study had similar findings.
Applications to Nursing
Our study found that mothers chose waterbirth because they were dissatisfied with the current medicalized environment of deliveries. Women will have less fear of delivery if they are provided with a delivery environment with more humanity, where fewer medical procedures are introduced. In addition, hospitals should consider setting up waterbirth units as an alternative mode of delivery.
Research Limitations and Suggestions
The participants all came from a single midwifery clinic. These mothers were relatively homogeneous, which could be a limitation. We suggest that future research may use qualitative research methods to further study waterbirth experience, when waterbirth is implemented in multiple institutions. Also, when the sample size is large, we may use quantitative research methods to examine and compare the degrees of satisfaction with delivery experience, labor length, and infection rate, etc., of waterbirth and traditional deliveries. We will then be able to assess waterbirth more thoroughly.
References
Burke, E., & Kifoyle, A. (1995). Waterbirth and bedbirth. Midwives, 108(1), 3-7. Burns, E., & Greenish, K. (1993). Pooling information. Nursing Times, 89(8), 47-49. Church, L. (1989). Waterbirth: One birthing centres observations. Journal of Nurse Midwifery, 34(4), 165-170.
Garland, D., & Jones, K. (1997). Waterbirth: Updating the evidence. British Journal of Midwifery, 5(6), 368-373. Geissbuhler, V., & Eberhard, J. (2000). Waterbirth: A comparative study. Fetal Diagnosis Therapy, 15, 291-300. Gilbert, R.E., & Tookey, R. A. (1999). Perinatal mortality and morbidity among babies delivered in water: Surveillance study and postal survey. British Medical Journal, 319(7208), 483-487. Giorgi, A. (1997). The theory, practice, and evaluation of the phenomenological method as a qualitative reaearch procedure. Journal of Phenomenology Psychology, 28(2), 235-260. Halek, J. L. (2000). Aquadurals and douladurals replace the epidurals. Midwifery Today, 54, 22-25. Hall, S. M., & Holloway, I. M. (1998) Staying in control: Womens experiences of labour in water. Midwifery, 14, 30-36. Harper, B. (2000). Waterbirth basics: From newborn breathing to hospital protocols. Midwifery Today, 54, 9-15. Li, H. J., & Lee, T. Y. (1998). The decision making experiences on amniocentesis of pregnant women with positive results on maternal serum screening for Downs Syndrome. The Journal of Nursing (Taiwan), 3(45),51-64. Lin, Y. H. (2000). Waterbirth. Baby-Mother, 260, 229232. Lincoln, Y. S., & Guba, E. G. (1985). Naturalistic inquiry. Newbury Park, CA: Sage. Malterud, K. (1993). Strategies for empowering womens voices in the medical culture. Health Care for Women Internationa, l14(4),365-73. Michelle, E. (2000). Hydrotherapy during labor. The American Journal of Maternal Child Nursing , 52(4), 198-203. Milner, I. (1988). Water baths for pain relief in labor. Nursing Times, 84(1), 39-40. Rawal, J., Shah, A., Stirk, F., & Mehtar, S. (1994). Water birth and infection in babies. British Medical Journal, 309, 511. Rush, J., Burlock, S., Lambert, K., Loosley-Millman, M., Hutchison, B., & Emkin, M. (1996). The effects of whirlpool baths in labour: A randomised, controlled trial. Birth, 23(3), 136-143. Tsai, S.N. (2001, Aug.). Experience sharing: Waterbirth accouching. In the 2001 Annual Meeting of the Association of Midwives, Republic of China, 2001 Annual Meeting of The Association of Midwives Handouts. Taipei: Municipal Chungshin Hospital. Tsai, S.N. (2002). An alternative labor and delivery method-waterbirth. Baby-Mother, 305, 40-46. Wagner, W. (2001). Fish cant see water: The need to humanize birth. International Journal of Gynecology & Obsterics, 75, 25-37.
267
Copyright of Journal of Nursing Research (Taiwan Nurses Association) is the property of Taiwan Nurses Association and its content may not be copied or emailed to multiple sites or posted to a listserv without the copyright holder's express written permission. However, users may print, download, or email articles for individual use.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5810)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (844)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (346)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Service Blueprint HospitalDocument1 pageService Blueprint HospitalRaghav R Chawla40% (5)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- ABC, Resource Drivers, Service Industry Glencoe Medical Clinic Operates A Cardiology Care Unit and A Maternity Care UnitDocument3 pagesABC, Resource Drivers, Service Industry Glencoe Medical Clinic Operates A Cardiology Care Unit and A Maternity Care UnitKailash KumarNo ratings yet
- Historical Evolution of Nursing ResearchDocument9 pagesHistorical Evolution of Nursing ResearchGayathri R100% (2)
- Assessment Scientific Analysis Planning Intervention Rationale Evaluation Short Term GoalDocument4 pagesAssessment Scientific Analysis Planning Intervention Rationale Evaluation Short Term GoalJayson OlileNo ratings yet
- 1,000 Questions To Help You Pass The Emergency Medicine BoardsDocument338 pages1,000 Questions To Help You Pass The Emergency Medicine Boardseric91% (11)
- Fetal Cerebro-Placental Ratio and Adverse Perinatal Outcome: Systematic Review and Meta-Analysis of The Association and Diagnostic PerformanceDocument8 pagesFetal Cerebro-Placental Ratio and Adverse Perinatal Outcome: Systematic Review and Meta-Analysis of The Association and Diagnostic Performancebidan22No ratings yet
- European Journal of Obstetrics & Gynecology and Reproductive BiologyDocument15 pagesEuropean Journal of Obstetrics & Gynecology and Reproductive Biologybidan22No ratings yet
- Diagnostics 07 00012Document10 pagesDiagnostics 07 00012bidan22No ratings yet
- AmniotomiDocument8 pagesAmniotomibidan22No ratings yet
- Menopause Hormone Replacement TherapyDocument4 pagesMenopause Hormone Replacement Therapybidan22No ratings yet
- Abnormal Vaginal Bleeding Policar 051611Document69 pagesAbnormal Vaginal Bleeding Policar 051611bidan22No ratings yet
- Early Amniotomy After Vaginal Misoprostol For Induction of Labor: A Randomized Clinical TrialDocument5 pagesEarly Amniotomy After Vaginal Misoprostol For Induction of Labor: A Randomized Clinical Trialbidan22No ratings yet
- Antiphospholipid Antibody Syndrome and PregnancyDocument17 pagesAntiphospholipid Antibody Syndrome and Pregnancybidan22No ratings yet
- Contingency Plan For Covid - 19Document12 pagesContingency Plan For Covid - 19anneNo ratings yet
- ACE PALAWAN MGAS-SIXTH FLOOR-ModelDocument1 pageACE PALAWAN MGAS-SIXTH FLOOR-ModelBerlin Andrew SionNo ratings yet
- Diploma Entrants Admissions List 2018 2019 PDFDocument15 pagesDiploma Entrants Admissions List 2018 2019 PDFAyesigwa Gerald96No ratings yet
- Resume Kelsi WeakleyDocument2 pagesResume Kelsi Weakleyapi-276879599No ratings yet
- Maintaining Fluid Balance: Barbara WorkmanDocument8 pagesMaintaining Fluid Balance: Barbara WorkmanNurul HendrianiNo ratings yet
- MKT-PK3-01-01 Identifikasi, Penilaian & Pengendalian RisikoDocument3 pagesMKT-PK3-01-01 Identifikasi, Penilaian & Pengendalian RisikoDania RachmawatiNo ratings yet
- Nejmoa1611593 AppendixDocument43 pagesNejmoa1611593 AppendixFasihaNo ratings yet
- Radiographs in Prosthodontics / Orthodontic Courses by Indian Dental AcademyDocument38 pagesRadiographs in Prosthodontics / Orthodontic Courses by Indian Dental Academyindian dental academy100% (4)
- Certificate For COVID-19 Vaccination: Beneficiary DetailsDocument1 pageCertificate For COVID-19 Vaccination: Beneficiary DetailsAshok KumarNo ratings yet
- Nurse To Nurse Bedside Shift Report LB 5th WeekDocument12 pagesNurse To Nurse Bedside Shift Report LB 5th Weekapi-527286440No ratings yet
- RSMPD Abstract E-BookDocument185 pagesRSMPD Abstract E-BookjesslinaNo ratings yet
- Questions For NursingDocument26 pagesQuestions For Nursingjoan olanteNo ratings yet
- Adverse Drug Reaction Monitoring Reporting PDFDocument3 pagesAdverse Drug Reaction Monitoring Reporting PDFRossana Rizqita PutriNo ratings yet
- Condylomata AcuminataDocument10 pagesCondylomata Acuminataalejandro fernandezNo ratings yet
- Guidelines Made Simple Chest PainDocument18 pagesGuidelines Made Simple Chest PainPaul JohnNo ratings yet
- Post ExamDocument7 pagesPost ExamJean Cuenta0% (1)
- The Safe Use of Syringe Driver in Palliative CareDocument3 pagesThe Safe Use of Syringe Driver in Palliative CarecohenserbanNo ratings yet
- Practical Application of Statistics in NursingDocument3 pagesPractical Application of Statistics in NursingApong JuanNo ratings yet
- Theories of AgingDocument2 pagesTheories of AgingJeremiah JustoNo ratings yet
- Listening - Sample 1Document15 pagesListening - Sample 1Mamdouh GallowNo ratings yet
- Restorative Dentistry: " The Sandwich Technique "Document11 pagesRestorative Dentistry: " The Sandwich Technique "Asya Mubarak100% (1)
- Public Health Informatics and GISDocument52 pagesPublic Health Informatics and GISNise Mon KuriakoseNo ratings yet
- Detailed Lesson Plan in Health 9Document6 pagesDetailed Lesson Plan in Health 9marvierose0% (1)
- Concept Communicable DiseasesDocument477 pagesConcept Communicable DiseasesrimeoznekNo ratings yet
- An Overview of Asthma Management - UpToDateDocument83 pagesAn Overview of Asthma Management - UpToDatedocjime9004No ratings yet