Professional Documents
Culture Documents
Dichgans M. (2007)
Uploaded by
Rusda AnandaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Dichgans M. (2007)
Uploaded by
Rusda AnandaCopyright:
Available Formats
Review
Genetics of ischaemic stroke
Martin Dichgans
Ischaemic stroke is a heterogeneous multifactorial disorder. Epidemiological data provide substantial evidence for a Lancet Neurol 2007; 6: 149–61
genetic component to the disease, but the extent of predisposition is unknown. Large progress has been made in Department of Neurology,
single-gene disorders associated with ischaemic stroke. The identification of NOTCH3 mutations in patients with Neurologische Klinik, Klinikum
Grosshadern, Ludwig-
cerebral autosomal dominant arteriopathy with subcortical infarcts and leucoencephalopathy (CADASIL) has led to
Maximilians-University,
new insights on lacunar stroke and small-vessel disease. Studies of sickle-cell disease have drawn attention to the D-81377 München, Germany
importance of modifier genes and of gene–gene interactions in determining stroke risk. They have further highlighted (M Dichgans MD)
a potential role of genetics in predicting stroke risk. Little is known about the genes associated with complex Correspondence to:
multifactorial stroke. There are probably many alleles with small effect sizes. Genetic-association studies on a wide Prof Martin Dichgans
martin.dichgans@med.uni-
range of candidate pathways, such as the haemostatic and inflammatory system, homocysteine metabolism, and the
muenchen.de
renin-angiotensin aldosterone system, suggest a weak but significant effect for several at-risk alleles. Genome-wide
linkage studies in extended pedigrees from Iceland led to the identification of PDE4D and ALOX5AP. Specific
haplotypes in these genes have been shown to confer risk for ischaemic stroke in the Icelandic population, but their
role in other populations is unclear. Advances in high-throughput genotyping and biostatistics have enabled new
study designs, including genome-wide association studies. Their application to ischaemic stroke requires the
collaborative efforts of multiple centres. This approach will contribute to the identification of additional genes, novel
pathways, and eventually novel therapeutic approaches to ischaemic stroke.
Introduction emphasises the importance of stroke subtypes and lends
Stroke is the third most common cause of death and the support to the view that large-vessel stroke and myocardial
most common cause of disability in developed countries. infarction share similar pathological mechanisms and
About 80% of strokes are ischaemic. Atherosclerosis genetic susceptibility.
(large-artery disease), cardioembolism, and small-vessel Further insight has come from studies on intermediate
disease (lacunar stroke) are by far the most common phenotypes. There is strong evidence, for example, for a
causes, but various other mechanisms exist (figure 1).1 genetic component to atherosclerosis as an independent
Non-modifiable risk factors (age, African and Asian race, trait. Carotid intima-medial wall thickness (IMT)—a
male sex) and acquired risk factors (hypertension, cigarette
smoking, diabetes, atrial fibrillation, and obesity) account Genes
for much of the risk of ischaemic stroke.2 Yet, stroke risk
remains insufficiently explained by these factors.
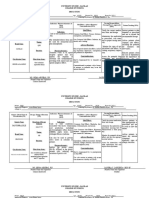
1 2 3 4 5
Genetic factors and intermediate phenotypes Vascular risk factors Stroke mechanism Infarct size
Ischaemic stroke
Studies in twins, families, and animal models provide and stroke outcome
substantial evidence for a genetic contribution to • Hypertension Artherosclerosis
ischaemic stroke.3,4 However, the extent of genetic • Smoking
(large-artery disease)
predisposition is uncertain. In twins, concordance rates
for the disease were reported to be about 65% greater in • Diabetes Cardioembolism
monozygotic than in dizygotic twins, but most twin (cardiac disease)
• Obesity
studies have been relatively small. In case–control
studies, a family history of stroke was shown to increase •Dyslipidaemia Small-vessel disease
the risk of ischaemic stroke by about 75%,3 which is in
• Homocysteine
line with the data from studies in twins, but a precise Other specific
estimate is difficult to ascertain. Genetic predisposition • Others mechanisms
differs depending on age and stroke subtype. Both twin
and family-history studies suggest a stronger genetic 2
component in stroke patients aged younger than 70 years
than in those who are older.3,5,6 Also, genetic factors seem
Environment
to be more important in large-vessel stroke and small-
vessel stroke than in cryptogenic stroke, and there is no Figure 1: Genetic factors and ischaemic stroke
epidemiological evidence for a genetic component in Genetic factors might affect stroke risk at various levels. They could act through conventional risk factors (1),
cardioembolic stroke.5–7 A common observation in interact with conventional and environmental risk factors (2), or contribute directly to an established stroke
mechanism such as atherosclerosis or small-vessel disease (3). Genetic factors could further affect the latency to
epidemiological studies has been that a family history of stroke (4) or infarct size and stroke outcome (5). Genetic factors might affect stroke risk at various levels. Similarly,
myocardial infarction is more common in large-vessel environmental factors and interactions between genes and the environment could occur at various levels. MR
stroke than in other stroke subtypes.5–7 This finding images were provided by the Department of Neuroradiology, Klinikum Grosshadern.
http://neurology.thelancet.com Vol 6 February 2007 149
Review
surrogate measure for subclinical atherosclerosis—is most robust findings have been on single-gene disorders,
largely controlled by genetics.8 Heritability estimates for which will therefore be discussed first.
IMT range from about 30% to 60%,9,10 which means that
much of the variability is due to genetic factors. Single-gene disorders
Importantly, this genetic effect seems largely independent Mendelian conditions are an important cause of stroke,
from known risk factors as most estimates were obtained especially in young stroke patients without known risk
while adjusting for demographic and vascular risk factors.24,25 In some disorders stroke is the prevailing
factors. On average, studies enrolling largely participants manifestation, whereas in others it is part of a wider
with cardiovascular disease reported higher heritabilities phenotypic spectrum (table 1). Most single-gene disorders
than studies in population-based samples,10 which are associated with specific stroke subtypes, which
emphasises the importance of genetic factors in together with the accompanying systemic features can
cardiovascular disease. Additionally, there is evidence for lead to diagnosis. The following disorders are especially
a genetic contribution to ischaemic white-matter relevant in clinical practice and are therefore discussed
lesions—a surrogate measure for cerebral small-vessel in more detail.
disease. Heritability estimates for cerebral white-matter
lesions have been in the range of 55–70%, again CADASIL
depending on the population under investigation.11,12 Cerebral autosomal dominant arteriopathy with
Because of the strong genetic contribution, investigators subcortical infarcts and leucoencephalopathy (CADASIL)
have started to use IMT and white-matter-lesion volumes is a heritable small-vessel disease caused by mutations in
as targets for genetic studies.13 NOTCH3.20 The clinical phenotype comprises recurrent
Genetic factors can act at several levels (figure 1). They strokes and transient ischaemic attacks, progressive
can contribute to conventional risk factors such as hyper- cognitive impairment, and psychiatric disturbance with
tension, diabetes, or homocysteine concentrations,14,15 onset usually in the third to sixth decade. About a third of
which have a known genetic component. They might patients develop migraine with aura.26,27 Neuroimaging
further interact with environmental factors16,17 or findings are similar to those for sporadic small-vessel
contribute directly to an intermediate phenotype such as disease. A relatively unique and diagnostically important
atherosclerosis.18–20 For example, sequence variants in feature of CADASIL, however, is bilateral involvement of
inflammatory cytokine genes seem to interact with the anterior temporal white matter and external capsule
smoking status to affect atherosclerosis risk. Finally, (figure 2).28,29 Strokes involving the territory of a large
genetic factors could affect latency to stroke, infarct size artery have occasionally been reported but are probably
after vessel occlusion, or stroke outcome.4,21–23 coincidental.
There are many studies investigating potential risk NOTCH3 encodes a cell-surface receptor, which has a
genes for common multifactorial stroke. However, the role in arterial development and is expressed on vascular
Mode of Gene Stroke mechanism Associated clinical features Diagnostic test
inheritance
CADASIL AD NOTCH3 Small-vessel disease Migraine with aura Mutational screening,
skin biopsy
Fabry’s disease X-linked GAL Large-artery disease and Angiokeratoma, neuropathic pain, acroparaesthesia, hypohydrosis, α-galactosidase activity,
small-vessel disease corneal opacities, cataract, renal failure, cardiac failure mutational screening
Sickle-cell disease AR HBB Large-artery disease, small- Pain crisis, bacterial infection, vaso-occlusive crises, pulmonary and Peripheral blood smear,
vessel disease, haemodynamic abdominal crises, anaemia, myelopathy, seizure electrophoresis, mutational
insufficiency analysis
Homocystinuria AR CBS and others Large-artery disease, Mental retardation, atraumatic dislocation of lenses, skeletal Urine analysis, plasma levels of
cardioembolism, small-vessel abnormalities (Marfan-like), premature atherosclerosis, homocysteine and methionine,
disease, arterial dissection thromboembolic events (mutational screening)
MELAS Maternal Mitochondrial Complex (microvascular and Developmental delay, sensorineural hearing loss, short stature, seizures, Muscle biopsy, mutational
DNA neuronal factors) episodic vomiting, diabetes, migraine-like headache, cognitive decline analysis of mtDNA
Marfan syndrome AD FBN1 Cardioembolism and arterial Pectus carinatum or excavatum, upper- to-lower-segment ratio <0·86 or Clinical diagnosis (mutational
dissection arm-span-to-height ratio >1·5, scoliosis >20%, ectopia lentis, dilation or screening)
dissection of the ascending aorta, lumbosacral dural ectasia
Ehlers-Danlos AD COL3A1 Arterial dissection Easy bruising, thin skin with visible veins, characteristic facial features, Biochemical studies, mutational
syndrome type IV rupture of arteries, uterus, or intestines screening
Pseudoxanthoma AR ABCC6 Large-artery disease and Skin changes (increased elasticity and yellow-orange papular lesions), Skin biopsy, mutational
elasticum small-vessel disease ocular changes (angioid streaks), hypertension screening
AD=autosomal dominant. AR=autosomal recessive. HBB=haemoglobin beta. CADASIL=cerebral autosomal dominant arteriopathy with subcortical infarcts and leucoencephalopathy. MELAS=mitochondrial
myopathy, encephalopathy, lactacidosis, and stroke. mtDNA=mitochondrial DNA.
Table 1: Single-gene disorders associated with ischaemic stroke
150 http://neurology.thelancet.com Vol 6 February 2007
Review
smooth-muscle cells. The Notch3 receptor is a heterodimer
composed of a large extracellular fragment and a smaller
transmembrane intracellular fragment. Mutations are
greatly stereotyped in that most, if not all, mutations
change the number of cysteine residues within one of
the extracellular epidermal-growth-factor-like repeat
domains.30,31 There have been single reports of mutations
not affecting cysteine residues,32 but the role of these
sequence variants is controversial. The mutational
spectrum is broad. About 95% of patients have missense
mutations that cluster in exons 3–6.31 Preliminary evidence
suggests that some mutations are associated with a slightly
more aggressive phenotype.27,33–35 In general, however, the
genotype seems to have no major effect on the phenotype.
The mechanisms by which NOTCH3 mutations become Figure 2: Characteristic brain MRI changes in CADASIL
pathogenic are still poorly understood. Most mutations do Involvement of the anterior temporal white matter (arrow) and external capsule (arrowheads) in a 67 year old
female patient with CADASIL (FLAIR image).
not seem to interfere with Notch3 receptor signalling.36
However, studies in patients and transgenic mice have
shown that the mutant Notch3 receptor accumulates in measuring α-galactosidase A activity or by screening for
arteries and precapillaries.37,38 Electron microscopy shows mutations. In women, measurements of enzyme activity
granular osmiophilic deposits within the vascular basal are less reliable because of skewed inactivation of the
lamina, which are specific for CADASIL, are present X chromosome in female mutation carriers. The
throughout the arterial system, and can therefore be used mutational spectrum is broad. Most patients carry
for diagnostic purposes.39 An important observation has missense or non-sense mutations in the coding region of
been that the clinical course and MRI findings can vary GLA. Enzyme-replacement therapy with recombinant
from relatively benign to very severe.26,27 Evidence suggests α-galactosidase A is effective in reducing globotriao-
that variations in disease severity are due to a modifying sylceramide deposition and improving some of the
effect of genetic factors distinct from the causative symptoms.45,46 A benefit on stroke has not been shown, but
NOTCH3 mutation.40 neither randomised trial was sufficiently powered to study
this outcome.
Fabry’s disease
Fabry’s disease is an X-linked systemic disorder caused Sickle-cell disease
by deficiency of the lysosomal enzyme α-galactosidase A Sickle-cell disease is the most common cause of stroke in
(table 1). Deficiency in this enzyme results in progressive children.25 The disease can be caused by the homozygous
accumulation of glycosphingolipids, particularly state for haemoglobin S (HbS) or by the compound
globotriaosylceramide in the myocardium, renal heterozygous state with other haemoglobinopathies such
epithelium, skin, eye, and vasculature. Onset is typically as haemoglobin C (HbC) or α-thalassaemia.47 HbS results
in childhood or adolescence with acroparaesthesia, from an aminoacid substitution in the β chain. About 25%
angiokeratoma, or hypohidrosis being common signs. of patients with HbS/HbS and 10% of those with HbS/
Systemic complications involving the kidneys, heart, and HbC will have a stroke by the age of 45 years.48 In patients
brain usually follow in mid-adulthood. with HbS/HbS the incidence of ischaemic stroke is highest
Fabry’s disease is surprisingly common in young stroke between 2 years and 5 years (0·70 per 100 patient-years)
patients. In a large series of young (18–55 years) patients and lowest between 20 years and 30 years (0·04 per 100
with cryptogenic stroke 4·9% of men and 2·4% of women patient-years). Conversely, the risk of haemorrhagic stroke
were shown to carry a functionally relevant mutation in is highest in the third decade (0·44 per 100 patient-years).48
the α-galactosidase gene (GLA).24 Cerebrovascular Stroke recurrence is common. Clinically overt strokes are
symptoms occur from both large-artery disease and typically due to large-artery disease, characterised by
small-vessel disease, with a preference for the posterior intimal thickening, proliferation of fibroblasts and smooth-
circulation.24,41–43 Small-vessel disease in Fabry’s disease is muscle cells, and eventually thrombus formation. This
associated with white-matter changes and evidence process is usually confined to the supraclinoid internal
suggests that the extent of such lesions is affected by carotid artery and the proximal portions of the middle and
polymorphisms in the genes for interleukin 6, endothelial anterior cerebral arteries.49 Ischaemic infarcts are
nitric oxide synthase, factor V, and protein Z.44 These commonly located in borderzone regions, in particular the
findings on potential modifier genes are promising but anterior and deep borderzone region.25,50 Apart from overt
await confirmation. stroke, many patients develop silent infarcts.25,51 These
Fabry’s disease may be suspected on the basis of the infarcts are small, located in subcortical regions, and
associated systemic signs (table 1) and confirmed by attributed to small-vessel disease.
http://neurology.thelancet.com Vol 6 February 2007 151
Review
A critical component in the pathogenesis of both large- be distinguished from milder (15–100μmol/L) hyper-
artery disease and small-vessel disease is an abnormal homocysteinaemia, which is a risk factor for stroke in the
interaction between sickled red blood cells and the general population and is associated with deficient dietary
vascular endothelium.25,52 Sickled red blood cells tend to B6, B12, or folate. The most common cause of
adhere to the endothelium, thus favouring thrombus homocystinuria is a deficiency of cystathionine beta-
formation and vascular occlusion. Endothelial activation synthase (CBS), a key enzyme in the degradation of
further promotes remodelling of the arterial wall and homocysteine.60 More rarely, homocystinuria results from
vasculopathy. disturbances in the conversion of homocysteine to
The risk of stroke in sickle-cell disease seems to be methionine by a pathway that requires the formation of
strongly affected by modifier genes.53–55 In fact, the stroke methylated derivatives of folate and B12.
phenotype in sickle-cell disease has become a prominent About 50% of untreated patients with CBS deficiency
example of modifying genetic effects in mendelian have a thromboembolic event by the age of 30 years and
traits. An inhibitory effect of fetal haemoglobin (HbF) about a third of these events involve the cerebrovascular
on the polymerisation of HbS has been known for many system.61 Homocystinuria can cause stroke not only
years. Concentrations of HbF are under genetic control through atherosclerosis and thromboembolism but also
and have a major effect on sickle-cell disease in general. through small-vessel disease and arterial dissection.62,63
A more specific effect on stroke has been identified for Homocysteine has been shown to injure endothelial cells
polymorphisms in various genes associated with and increase smooth-muscle-cell proliferation in vitro.63
inflammation and cell adhesion. Thus, polymorphisms Putative factors by which homocysteine might induce
in the cell-adhesion molecules VCAM and P-selectin, vascular injury further include extracellular matrix
for example, were shown to be associated with stroke modification, lipoprotein oxidation, and effects on
risk in sickle-cell disease.54,56,57 Also, there is evidence for platelets and coagulation.64 Patients with concurrent
a role of the interleukin 4 receptor gene in determining homocystinuria and factor V Leiden have an increased
stroke risk.57 risk of thrombosis.65
A major methodological step has been the use of Bayesian Around a half of the patients with CBS deficiency
networks. By applying such networks to a large number of respond to B6. Those who respond tend to have a later
single-nucleotide polymorphisms, Sebastiani and onset, a milder phenotype, and a better prognosis than
colleagues54 identified 31 single-nucleotide polymorphisms non-responders.66 The mutational spectrum of CBS
in 12 genes that were shown to interact with HbF in deficiency is broad.67 There are many private mutations
modulating stroke risk. The network included P-selectin (ie, unique to one family) but some mutations, in
and several genes in the transforming growth factor β particular Ile278Thr and Gly307Ser, are relatively
(TGF β) pathway, which has been associated with stroke in common.67,68 An important observation regarding
other studies. Remarkably, this network accurately predicted genotype–phenotype correlations has been that some
the occurrence of stroke in an independent sample on the mutations, including Ala114Val and Ile278Thr, are
basis of genotyping of just a few single-nucleotide associated with B6 responsiveness whereas others, in
polymorphisms. These observations draw attention to the particular Gly307Ser, are associated with B6 resistance.
importance of modifier genes in monogenic disorders. Early diagnosis of homocystinuria is essential as
They further emphasise a potential role of genetics in the complications can be reduced by early treatment.
prediction of stroke risk. The risk of stroke in sickle-cell
disease can be substantially reduced by transfusion MELAS
therapy.25,58 Transcranial ultrasound has been recommended The syndrome of mitochondrial myopathy, enceph-
for use as a screening tool to identify children at high risk alopathy, lactic acidosis, and stroke-like episodes (MELAS)
for stroke and criteria have been developed for the initiation is associated with several mutations in mitochondrial
and duration of transfusion therapy.2,58,59 Yet, chronic DNA.69,70 About 80% of patients carry an A to G transition
transfusion can cause adverse effects and identification of at position 3243 in the tRNALeu (UUR) gene. The second most
patients at risk of stroke remains a challenge. In this regard, common mutation (T3271C) is found in about 10% of
screening methods based on genotyping are a potentially cases. The relative distribution of mutant and wild-type
important approach.54 mtDNA might vary in different tissues explaining in part
the immense phenotypic diversity of mitochondrial
Homocystinuria disorders. MELAS is associated with various symptoms
Homocystinuria encompasses a group of mostly (table 1). However, monosymptomatic cases with stroke
autosomal recessive enzyme deficiencies, which cause as the sole manifestation do exist.70
high (>100μmol/L) plasma concentrations of homocysteine The cerebral lesions underlying stroke-like episodes in
and homocystinuria. The disease should be considered in MELAS differ from typical ischaemic infarcts; the cortex
any child with stroke, mental retardation, atraumatic is almost invariably involved. In many cases, lesions are
(mostly downward) dislocation of the ocular lenses, or not limited to vascular territories and there are no
Marfan-like skeletal abnormalities. Homocystinuria must embolic or stenotic lesions on angiography. Also,
152 http://neurology.thelancet.com Vol 6 February 2007
Review
diffusion-weighted MRI may show an increase in the pseudoxanthoma elasticum,80 which is associated with
apparent diffusion coefficient within acute lesions, stenotic lesions of the distal carotid artery and with small-
suggesting vasogenic rather than cytotoxic oedema.71 vessel disease (table 1).80,84
These observations point towards mechanisms other
than pure ischaemic infarction. Current hypotheses Moyamoya disease
include: 1) a disturbance of the blood–brain barrier; Moyamoya disease is a chronic progressive syndrome
2) impaired autoregulation of cerebral blood flow;72 and that is characterised by bilateral occlusion of the terminal
3) primary defects in neuronal oxidative metabolism. carotid artery in association with telangiectatic vessels at
Lesions can spread over time or substantially regress on the base of the brain.85 The disease is uncommon in non-
subsequent scans.73 Asian populations whereas its prevalence in Japan is
estimated to be three or more in 100 000. The most
Connective tissue disorders frequent manifestations in childhood are transient
Ischaemic stroke is a well-known complication of several ischaemic attack, ischaemic stroke, and epileptic seizures.
heritable connective tissue disorders. Marfan’s syndrome Rupture of telangiectatic vessels causes intracranial
is an autosomal dominant systemic disorder affecting haemorrhage—the main manifestation in patients older
the musculoskeletal system, cardiovascular system, and than 30 years.85,86 About 10% of moyamoya cases occur as
the eye.74 The diagnosis is usually established on clinical familial cases, but the pattern of inheritance is not
grounds (table 1),75 whereas the role of genetic testing is clear.87,88 Both polygenic inheritance and an autosomal
limited. Marfan’s syndrome is caused by mutations in a dominant mode of transmission with incomplete
very large gene (FBN1; 65 exons) and more than 90% of penetrance have been suggested. Moyamoya disease has
families have a private mutation, which renders been linked to genetic loci on chromosomes 3p, 8q, and
mutational screening very laborious.76 FBN1 encodes 17q89–91 and moyamoya-like changes have been described
fibrillin 1, an extracellular matrix protein. Fibrillin 1 is in association with a variety of single-gene disorders,
expressed in many tissues, including the heart and elastic including sickle-cell disease, pseudoxanthoma elasticum,
arteries. It shares homology with TGFβ binding proteins and neurofibromatosis type 1.
and there is increasing evidence for a key role of TGFβ
signalling in Marfan’s syndrome.74,77 Cerebrovascular Miscellaneous
complications of the disease include transient ischaemic Ischaemic stroke can occur as a complication of several
attacks, ischaemic infarcts, and subdural haematoma. In heritable cardiomyopathies,92,93 dysrhythmias,94 haem-
a retrospective series on 513 patients, neurovascular oglobinopathies,95 coagulopathies,96,97 dyslipidaemias,98
manifestations were associated with cardiac sources of and vasculopathies.99–101 In some cases an association with
embolism, in particular prosthetic heart valves, mitral stroke has been firmly established.93 In many others an
valve prolapse, and atrial fibrillation, whereas there was association is less well documented or a matter of
no association with aortic disease or cerebral artery controversy. A detailed discussion of these disorders is
dissection.78 However, other studies have observed an beyond the scope of this article. Most of them are covered
association with aortic and cerebral artery dissection.79,80 by specific reviews.92,94,97,98
Further causes of ischaemic stroke include chronic
anticoagulant therapy and perioperative embolic events Common multifactorial stroke and genetic risk
in patients undergoing aortic root replacement.81 factors for ischaemic stroke
Ehlers-Danlos syndrome type IV, the vascular type, is The genetic contribution to common multifactorial
an autosomal dominant disorder resulting from stroke seems to be polygenic. Most likely, there are many
mutations in COL3A1, the gene for collagen type III.82 alleles with small effect sizes (relative risk <1·5). However,
The disorder may be suspected on the basis of the because of their wide distribution, on a population basis
associated clinical features (table 1) and can be confirmed the impact on stroke is large. It is increasingly recognised
by mutational screening or biochemical studies on that the effects of some alleles are limited to one or few
cultured fibroblasts (synthesis of an abnormal type III stroke subtypes (figure 1) and that effect sizes may vary
procollagen). The mutational spectrum is broad and depending on sex and ethnic origin.19,102
neomutations are common.82 About 50% of the index Most previous studies investigating genetic risk factors
cases have no apparent family history. Cerebrovascular for human stroke have taken a candidate gene approach
complications are common and include intracranial using case–control methodologies. To be reliably
aneurysms, arterial dissection, and spontaneous rupture detected, small relative risks require large sample sizes,
of large and medium-sized arteries.80,83 In a series of probably in the order of 1000 patients or more.103,104
419 patients, 11% had neurovascular complications.82 However, few studies have achieved such numbers. This
Carotid artery dissection and fistulae involving the carotid difficulty, together with differences in sample
artery were the most frequent findings. characteristics and study design, could explain much of
Ischaemic stroke has also been recognised as a the inconsistency between studies. Table 2 and the
complication of osteogenesis imperfecta and webtable summarise the results from case–control See Online for webtable
http://neurology.thelancet.com Vol 6 February 2007 153
Review
Polymorphism Genetic model Study Patients’ characteristics Cases (carriers/ Controls (carriers/ OR (95% CI) (unadjusted)
individuals) individuals)
MTHFR C677T Recessive 106 Meta-analysis (22 studies) 463/3387 630/4597 1·24 (1·08–1·42)
108 IS (women, 18–49 years) 26/193 69/764 1·5 (0·9–2·6)
63 SVD (lacunar S) 33/170 16/170 2·72 (1·32–5·60)
109 IS 14/146 2/55 2·81 (0·61–12·99)
110 Cryptogenic IS/TIA (<50 years) 9/93 26/186 0·66 (0·33–1·47)
ACE Ins/Del Recessive 106 Meta-analysis (11 studies) 903/2990 2993/11 305 1·21 (1·08–1·35)
114 IS (18–85 years) 153/456 149/459 1·05 (0·80–1·38)
115 IS (without CES, 50–97 years) 116/215 111/236 1·3 (0·9–1·9)
116 IS (without CES) 48/108 37/79 0·95 (0·69–1·30)
Factor V Leiden Arg506Gln Dominant 106 Meta-analysis (26 studies) 287/4588 901/13 798 1·33 (1·12–1·58)
119 IS/TIA (<60 years) 29/468 30/468 0·96 (0·57–1·63)
120 Cryptogenic IS/TIA with PFO 13/220 21/362 1·02 (0·50–2·10)
120 IS or TIA 11/196 21/362 0·97 (0·46–2·05)
108 IS (women, 18–49 years) 14/179 42/763 1·8 (0·9–3·6)
121 IS (15–45 years) 4/115 10/180 1·62 (0·46–4·06)
122 IS (>80 years) 1/114 6/150 0·22 (0·03–1·85)
110 Cryptogenic IS/TIA (<50 years) 15/93 13/186 3·19 (1·38–7·39)
123 Cryptogenic IS with PFO 4/57 1/104 7·8 (0·85–71·31)
124 Cryptogenic IS (<50 years) 2/49 5/294 2·62 (0·49–13·95)
Prothrombin G20210A Dominant 106 Meta-analysis (19 studies) 105/3028 210/7131 1·44 (1·11–1·86)
108 IS (women, 18–49 years) 5/188 18/763 1·0 (0·3–3·0)
121 IS (15–45 years) 8/115 10/180 1·27 (0·48–3·35)
122 IS (>80 years) 6/114 5/150 1·61 (0·48–5·42)
110 Cryptogenic IS/TIA (<50 years) 1/93 6/186 0·33 (0·04–2·75)
123 Cryptogenic IS with PFO 2/57 0*/104 1·0 (1·0–1·1)
124 Cryptogenic IS <50 years 4/49 7/294 3·75 (1·05–13·34)
PAI1 4G/5G Recessive 106 Meta-analysis (4 studies) nr/842 nr/1189 1·47 (1·13–1·92)
125 IS (18–69 years) 131/600 134/600 0·97 (0·74–1·28)
126 IS (25–74 years) 43/222 107/542 0·98 (0·66–1·45)
127 IS (18–75 years) 29/123 29/123 1·0 (0·6–1·8)
126 IS (25–74 years) 14/89 42/218 0·78 (0·40–1·52)
Candidate genes and polymorphisms were selected if there was at least one positive study reporting a significant association with ischaemic stroke and if the total number of studies was two or more. Studies
were selected if they fulfilled the following criteria (adopted from reference 106): 1) population consists of predominantly white patients; 2) population consists mainly of adults (age >18 years); 3) use of
neuroimaging (CT or MRI); 4) genotype frequencies for ischaemic stroke reported. Studies on populations already included in reference 106 are not included. MTHFR=methylenete-tetrahydrofolate reductase.
IS=ischaemic stroke. SVD=small-vessel disease. S=stroke. TIA=transient ischaemic attack. CES=cardioembolic stroke. LVD=large-vessel disease. PFO=patent foramen ovale. nr=not reported. *p set at 0·5 to
calculate unadjusted odds ratio.
Table 2: Selected candidate gene case–control association studies in ischaemic stroke
association studies on ischaemic stroke in predominantly In a meta-analysis15 involving more than 15 000 people
white populations. Here we focus on selected pathways without cardiovascular risk, the weighted mean difference
and candidate genes. in plasma homocysteine between individuals with the TT
and CC genotype was 1·93 μmol/L.15 This difference
Homocysteine metabolism corresponds to an expected odds ratio for overall stroke of
Mild to moderate increases in plasma homocysteine are about 1·20.105 In a meta-analysis on the relation between
associated with a heightened risk of stroke.105 A common the C677T polymorphism and stroke the observed odds
polymorphism (C677T) in the gene encoding 5.10-methyl ratio for overall stroke was 1·26 for TT vs CC.15 The effect
enetetrahydrofolate reductase (MTHFR), a critical enzyme seems to be largely independent of ethnic background
in homocysteine catabolism, has been shown to be and a similar odds ratio was found for ischaemic stroke
associated with both raised homocysteine concentrations only (table 2),106 with a possible gene-dose effect for the
and increased stroke risk. C677T results in an amino-acid T allele.107 Few authors have looked at ischaemic stroke
substitution and renders the enzyme thermolabile. The subtypes or intermediate phenotypes.8,63,108–110 In one study,
TT genotype, which is present in about 10% of the both homocysteine concentrations and the MTHFR
population, increases total homocysteine by about 20%. C677T allele were shown to be significant risk factors for
154 http://neurology.thelancet.com Vol 6 February 2007
Review
small-vessel disease,63 adding to the notion that the G20210A polymorphism, and the plasminogen activator
association with stroke is not limited to large-artery inhibitor 1 (PAI1) 4G/5G polymorphism all confer a small
disease. Overall, the TT genotype of the C677T but significant risk for ischaemic stroke (table 2).
polymorphism has been established as a moderate risk However, most large studies have not found an association
factor for ischaemic stroke and the increase in risk seems between prothrombotic states and overall incidence of
to be largely mediated through raised homocysteine ischaemic stroke. Also, in the meantime several negative
concentrations (figure 1). Whether homocysteine- studies have been published including studies on
lowering treatment can reduce the risk of stroke is still cryptogenic stroke (table 2, webtable).108,110,119–127 On balance,
unclear.111,112 prothrombotic states might be responsible for stroke in
some younger patients128 and in those with additional risk
Renin-angiotensin-aldosterone system factors (table 2).108,119 However, there is less evidence for a
Evidence suggests that genetic variation in the renin- role of prothrombotic states in unselected patients with
angiotensin-aldosterone system (RAAS) contributes to common multifactorial stroke.
the risk of ischaemic stroke. Among the various sequence
variations in RAAS, the insertion/deletion (I/D) Phosphodiesterase 4D
polymorphism in angiotensin converting enzyme (ACE) A major discovery has been that variation in the
is the most extensively studied. ACE produces angiotensin phosphodiesterase 4D (PDE4D) gene is associated with
II and catabolises bradykinin thereby affecting vascular ischaemic stroke in the Icelandic population.129 PDE4D
tone, endothelial function, and smooth-muscle-cell resides within a 20cM region on chromosome 5q12
proliferation. RAAS has a well-documented effect on (STRK1), which had previously been identified through
systemic blood pressure. Mean ACE activity concentration genome-wide linkage analysis. In association analyses
in DD carriers are around twice those found in II carriers. several single-nucleotide polymorphisms in PDE4D
Thus, the I/D polymorphism has become a strong were associated with the combined phenotype of
candidate for cardiovascular risk.113 cardiogenic and carotid stroke. Furthermore, an at-risk
In a meta-analysis106 including 2990 predominantly haplotype, comprising microsatellite AC008818-1 and
white patients and 11 305 controls, the DD genotype was SNP45 was shown to confer a relative risk of 1·5 for the
shown to confer a small but significant risk of ischaemic combined phenotype.129 PDE4D degrades second
stroke (odds ratio 1·21; 95% CI 1·08–1·35). Since then, messenger cAMP, which is a key signal transduction
there have been several studies with non-significant molecule in multiple cell types, including vascular
results (table 2).114–116 However, none of them was powered endothelial, smooth muscle, and inflammatory cells.
to detect a 20% risk increase. On balance, the available Since associations were limited to cardiogenic and
data suggest that any effect of the D allele on ischaemic carotid stroke it was suggested that PDE4D acts through
stroke is small. The effect of the I/D polymorphism on atherosclerosis. Yet, a subsequent study found no
ischaemic stroke subtypes,95 intermediate phenotypes,8 association between various single-nucleotide
and blood pressure113 has been explored in several small polymorphisms and IMT.130 Replication studies in other
studies, but with variable results. populations including Asians and blacks have yielded
Recent findings suggest that the A1166C polymorphism variable results.17,130–140 Several studies reported nominally
of the angiotensin II type-1-receptor gene is associated significant associations between single-nucleotide
with ischaemic stroke (webtable). However, the number polymorphisms or haplotypes and stroke. However,
of available studies is small and in one study the there is much heterogeneity with regard to the associated
association with ischaemic stroke disappeared when genetic variants and stroke subtypes (table 3).141 This
adjusting for risk factors.114 A1166C has been associated heterogeneity could be due in part to different study
with several vascular phenotypes and it seems possible designs. Also, it seems possible that the effect of PDE4D
that this polymorphism acts by affecting blood pressure. on stroke varies between populations depending on
The angiotensinogen (AGT) gene was investigated in different genetic backgrounds and environmental
several studies with conflicting results (webtable).117 A influences.17 Despite extensive genotyping of the PDE4D
potentially interesting observation, however, is the gene region, the disease-causing genetic variant has not
reported association between an AGT promoter haplotype been identified so far. Yet, there is increasing evidence
and cerebral small-vessel disease.118 that the STRK1 locus contributes to the risk of ischaemic
stroke.132
Haemostatic system
Prothrombotic states, such as activated protein C ALOX5AP and the leukotriene pathway
resistance and the underlying Factor V Leiden ALOX5AP is another gene that has been discovered
polymorphism, are an established risk factor for venous through genome-wide linkage analysis. A common
thrombosis but their role in ischaemic stroke is still haplotype (HapA) in ALOX5AP is associated with a
debated. According to a recent meta-analysis,106 the factor 1·8-fold increased risk of myocardial infarction and a
V Leiden Arg506Gly polymorphism, the prothrombin 1·7-fold increased risk of stroke in the Icelandic
http://neurology.thelancet.com Vol 6 February 2007 155
Review
Reference Study design Study population (number of individuals) Findings*
129 CC Iceland: stroke+TIA (864) / CBC (908) Large-artery stroke and cardioembolic stroke combined: 45,41,87,89,56, AC008818-1, haplotype
Large-artery stroke: 83, DG5S397
Cardioembolic stroke: AC008818-1
131 CC Germany: IS (601) / CBC (736) No significant associations
130 CC UK: IS (737) / CBC (933) Large artery stroke: 19,87
Cardioembolic stroke: 2,13,14,15,20,26
130 CC Germany: CBS (1000) for IMT No significant association with IMT and Carotid plaque
132 Linkage Sweden: 56 families with stroke Linkage to PDE4D region (two linkage peaks)
132 CC Sweden: stroke (275) / CBC (550) No significant associations
133 Linkage USA: 104 families with IS No Linkage to PDE4D region
133 CC USA: IS (377) / C (263) Ischaemic stroke: 56,83, haplotype
Large-artery stroke : 45,83
Cardioembolic stroke: 45
134 CC Netherlands: IS (88) / CBC (190) Small vessel stroke: 39,45 (only in inbred individuals)
135 CC Pakistan: IS (200) / CBC (250) Ischaemic stroke: 83
136 CC Japan: non-CE IS (208) / Outpatients (270) Non-cardioembolic ischaemic stroke: haplotype
137 CC USA: (357) / CBC (303) Ischaemic stroke: 41 (only in whites), haplotype (in whites and blacks)
Cardioembolic stroke: 87 and haplotype (whites and blacks); 41 (only in whites), 83 and 89 (only in blacks)
Small-vessel stroke: haplotype (only in whites)
Cryptogenic stroke: haplotype (in whites and blacks)
138 CC Germany: IS (1181) / CBC (1569) No significant associations
No significant associations
139 CC USA: woman with IS (248) / CBC (560) Ischaemic stroke: 9,42,219,220, AC008818-1 (in non-hypertensives), 175 (in hypertensives), haplotypes
140 CC USA: male incident IS (259) / C (259) Ischaemic stroke: 56 (all ischaemic stroke); 42,45,56 (subjects without baseline hypertension)
17 CC USA: women with IS (224) / CBC (221) Ischaemic stroke: rs918592,83,89,42, rs1498606 (all ischemic stroke), rs918592 (current smoking, dose effect)
Large-artery stroke: rs918592
Small-vessel stroke: rs918592
Cryptogenic stroke: rs918592
CC=case–contol study. TIA=transient ischaemic attack. CBC=community based controls. CBS=community based sample. IS=ischaemic stroke. IMT=intima-media thickness. C=controls. *Numbers refer to single
nucleotide polymorphisms (SNPs) and microsatellite markers that were significantly associated with the respective phenotype. SNPs are labelled according to reference 129.
Table 3: The PDE4D gene and ischaemic stroke
population.19 The association was stronger in men than Other candidate pathways and genes
women and was significant for both ischaemic and There is a long list of candidate gene pathways and genes
haemorrhagic stroke. The association between HapA and that have been studied for a possible association with
ischaemic stroke was subsequently replicated in the ischaemic stroke. Among the most widely investigated
Scottish population, which shares a common ancestry genes are those involved in inflammation (eg,
with the Icelandic population.142 Studies in other interleukin 1, interleukin 6, TNFα, toll-like receptor 4, P-
populations reported no association between HapA or selectin and E-selectin, C-reactive protein), lipid
other haplotypes and ischaemic stroke.131,133,143 However, in metabolism (eg, apolipoprotein E, paraoxonase, epoxide
a German sample several single-nucleotide hydrolase), nitric oxide release, and extracellular matrix
polymorphisms including one out of four single- (matrix metalloproteinases). Many of them are listed in
nucleotide polymorphisms constituting HapA were the webtable or discussed in reviews.106,145 In most cases,
associated with ischaemic stroke. ALOX5AP encodes 5- however, findings were either negative or could not be
lipoxygenase activating protein (FLAP), an important replicated in subsequent studies.
component of the leukotriene pathway. Leukotrienes are
proinflammatory mediators that are implicated in the Animal data
pathogenesis and progression of atherosclerosis.144 Only Experimental crossbreeding in an inbred strain of
recently, genetic variation in another gene involved in hypertensive rats, which are spontaneously hypertensive
leukotriene biosynthesis, the LTA4 hydrolase gene, was and prone to stroke, has led to the identification of three
shown to confer risk for myocardial infarction, especially major genetic loci that affect stroke risk in these animals.4,21
in patients with previous stroke or peripheral artery Str1, Str2, and Str3 were identified through a genome-
disease.102 These findings emphasise the importance of wide screening process with quantitative locus mapping
the leukotriene pathway in stroke. The importance of in F2 crosses. All three loci were shown to affect the time
ALOX5AP for specific stroke subtypes remains to be to stroke onset in stroke-prone spontaneously hypertensive
determined. rats fed a stroke-permissive diet.21 The Str2 locus was later
156 http://neurology.thelancet.com Vol 6 February 2007
Review
identified in an independent study as a risk locus for Because of the modest success of candidate gene
infarct volume after occlusion of the middle cerebral studies there is a growing interest in systematic
artery.4 Str2 colocalises with the gene for atrial natriuretic hypothesis-free approaches. Genome-wide studies using
peptide (ANP) on rat chromosome 5. Yet, the role of the 100 000 to 500 000 single-nucleotide polymorphisms
ANP gene in ischaemic stroke is still unclear both in rats have become technically possible but are a major
and in human beings (webtable). Also, the genetic challenge in terms of resources and study design. Such
variants underlying STR1, STR2, and STR3 remain to be studies require the collaborative effort of multiple centres
identified. and the construction of large databases containing
Another genetic approach, besides experimental clinical and epidemiological data.
crossbreeding, has been the targeted disruption of genes. Linkage-based methods are the strategy of choice when
For example, mice deficient in neuronal nitric oxide analysing monogenic disorders and there are several
synthase have been shown to develop smaller infarcts disorders that await gene identification.99–101 Linkage-
and less severe functional deficits than control animals based methods can also be applied to common
following occlusion of the middle cerebral artery.146 These multifactorial stroke129,147 and studies like the siblings with
studies have helped in understanding the mechanism of ischaemic stroke study (SWISS) have taken this
ischaemic stroke and in defining candidate genes for approach.132,148 The principles of linkage and association
genetic association studies in human beings. However, may further be combined in a single test. This is done in
they are less well suited to identify naturally occurring the transmission disequilibrium test and the sibling
risk alleles for stroke. transmission disequilibrium test, which use internal
controls (parents or siblings). However, there are a
Future directions number of challenges to the application of linkage-based
The technologies for high-throughput genotyping are methods to complex disorders.149
rapidly developing as are the statistical methods to Analysis of intermediate phenotypes such as IMT has
analyse increasingly complex data. The technical some advantages over the analysis of complex endpoints
developments are likely to outpace the collection of large such as stroke.8 For example, IMT is associated with a
carefully phenotyped samples. The future of stroke single pathology (atherosclerosis) rather than multiple
genetics will therefore depend on the samples available causes, which increases homogeneity and power. Also,
and on close collaborations between clinicians and IMT is a quantitative trait, which allows more powerful
geneticists. statistical methods to be applied. Yet, any findings for
Association-based methods are a powerful instrument IMT will need to be separately assessed for their effect on
to identify small relative risks. In this respect they are stroke. Because of a stronger genetic component in
particularly suited to address common multifactorial young patients, focusing on juvenile stroke seems
stroke. The candidate gene approach remains a valid especially promising, but recruiting large numbers is
strategy and there are several means by which the power difficult in such a selected population. In conclusion,
of such studies can be improved.103,104 Critical issues there are various strategies that should be regarded as
include the selection of candidate genes and appropriate complementary.
phenotypes, the phenotyping protocols, sample-size Recently, pharmacogenetics, which investigates
issues, and replication in independent cohorts. These genetically determined variations in response to drugs,
aspects have been the subject of recent reviews.103,104 has emerged as a promising research area. Thus, for
Comprehensive analyses of whole genes with genotyping example, polymorphisms in the genes for the hepatic
of multiple single-nucleotide polymorphisms and microsomal enzyme P450 2C9 (CYP2C9) and for vitamin
haplotype-based analyses have started to replace small K epoxide reductase complex 1 (VKORC1) have been
studies on single polymorphisms.19,129 The identification shown to strongly affect individual sensitivity to
of PDE4D as a risk gene for stroke provides a good warfarin.150,151 Also, recent trialists have started to stratify
example of the shift in paradigms and has drawn patients according to their genotypes.152 The idea behind
attention to the complex associations between at-risk these studies is to beneficially affect patient safety and
alleles, associated markers, and associated haplotypes individual treatment strategies, but the transition into
within and across populations. Because of the clinical practice has not yet been made. Genetic testing
heterogeneity of stroke, analyses according to stroke has become a valuable tool in diagnosing single-gene
subtypes are essential. Interactions with environmental disorders associated with ischaemic stroke, whereas it is
risk factors will need to be considered as there is evidence currently not recommended in patients with common
for such interplay in stroke. Also, some genes are likely multifactorial stroke.
to interact in determining stroke risk and researchers
have started to look at epistatic (gene–gene) interactions. Conclusion
However, such studies make great demands on sample Much progress has been made in the identification of
size. At any rate, replication of novel findings in different genes for mendelian conditions associated with stroke.
cohorts and settings remains the key. However, comparatively little is known about the genes
http://neurology.thelancet.com Vol 6 February 2007 157
Review
13 DeStefano AL, Atwood LD, Massaro JM, et al. Genome-wide scan
Search strategy and selection criteria for white matter hyperintensity: the Framingham Heart Study.
Stroke 2006; 37: 77–81.
References for this review were identified by searches of 14 Marteau JB, Zaiou M, Siest G, Visvikis-Siest S. Genetic determinants
PubMed from 1966 to September, 2006, by combinations of of blood pressure regulation. J Hypertens 2005; 23: 2127–43.
the terms “stroke”, “ischaemic”, “gene”, “mutation”, 15 Casas JP, Bautista LE, Smeeth L, Sharma P, Hingorani AD.
Homocysteine and stroke: evidence on a causal link from
“polymorphism”, and “association”. Articles were also mendelian randomisation. Lancet 2005; 365: 224–32.
identified through searches of the author’s own files. Selection 16 Jerrard-Dunne P, Sitzer M, Risley P, Buehler A, von Kegler S,
of material for inclusion was based on quality and relevance. Markus HS. Inflammatory gene load is associated with enhanced
inflammation and early carotid atherosclerosis in smokers. Stroke
2004; 35: 2438–43.
17 Song Q, Cole JW, O’Connell JR, et al. Phosphodiesterase 4D
involved in multifactorial stroke. The identification of polymorphisms and the risk of cerebral infarction in a biracial
PDE4D and ALOX5AP as risk genes for ischaemic stroke population: the Stroke Prevention in Young Women study.
Hum Mol Genet 2006; 15: 2468–78.
in the Icelandic population represents a breakthrough, 18 Lusis AJ, Fogelman AM, Fonarow GC. Genetic basis of
but the role of these genes in other populations is less atherosclerosis: part I: new genes and pathways. Circulation 2004;
clear. There are various methodological approaches, yet 110: 1868–73.
19 Helgadottir A, Manolescu A, Thorleifsson G, et al. The gene
careful phenotyping and large sample sizes remain the encoding 5-lipoxygenase activating protein confers risk of
key. Collaborative efforts from multiple centres are myocardial infarction and stroke. Nat Genet 2004; 36: 233–39.
needed to elucidate the genetic basis of common 20 Joutel A, Corpechot C, Ducros A, et al. Notch3 mutations in
CADASIL, a hereditary adult-onset condition causing stroke and
multifactorial ischaemic stroke. dementia. Nature 1996; 383: 707–10.
Conflicts of interest 21 Rubattu S, Volpe M, Kreutz R, Ganten U, Ganten D,
I have no conflicts of interest. Lindpaintner K. Chromosomal mapping of quantitative trait loci
contributing to stroke in a rat model of complex human disease.
Acknowledgments Nat Genet 1996; 13: 429–34.
I thank Michael O’Sullivan for critically reading the manuscript and for 22 Meschia JF. Clinically translated ischemic stroke genomics. Stroke
helpful comments. I am supported by the Deutsche 2004; 35 (11 suppl 1): 2735–39.
Forschungsgemeinschaft (SFB 596/TPA4). No funding body had a role 23 Mallolas J, Hurtado O, Castellanos M, et al. A polymorphism in the
in the preparation of the review or in the decision to submit it for EAAT2 promoter is associated with higher glutamate
publication. concentrations and higher frequency of progressing stroke.
References J Exp Med 2006; 203: 711–17.
1 Adams HP, Bendixen BH, Kappelle LJ, et al. Classification of 24 Rolfs A, Bottcher T, Zschiesche M, et al. Prevalence of Fabry disease
subtype of acute ischaemic stroke: definitions for use in a in patients with cryptogenic stroke: a prospective study. Lancet 2005;
multicenter clinical trial. TOAST (Trial of Org 10172 in Acute Stroke 366: 1794–96.
Treatment). Stroke 1993; 24: 35–41. 25 Switzer JA, Hess DC, Nichols FT, Adams RJ. Pathophysiology and
2 Goldstein LB, Adams R, Alberts MJ, et al. Primary prevention of treatment of stroke in sickle-cell disease: present and future.
ischemic stroke: a guideline from the American Heart Association/ Lancet Neurol 2006; 5: 501–12.
American Stroke Association Stroke Council. Stroke 2006; 26 Dichgans M, Mayer M, Uttner I, et al. The phenotypic spectrum of
37: 1583–633. CADASIL: clinical findings in 102 cases. Ann Neurol 1998; 44: 731–39.
3 Flossmann E, Schulz UG, Rothwell PM. Systematic review of 27 Opherk C, Peters N, Herzog J, Luedtke R, Dichgans M. Long-term
methods and results of studies of the genetic epidemiology of prognosis and causes of death in CADASIL: a retrospective study in
ischemic stroke. Stroke 2004; 35: 212–27. 411 CADASIL patients. Brain 2004; 127: 2533–39.
4 Jeffs B, Clark JS, Anderson NH, et al. Sensitivity to cerebral 28 Auer DP, Putz B, Gossl C, Elbel GK, Gasser T, Dichgans M.
ischaemic insult in a rat model of stroke is determined by a single Differential lesion patterns in CADASIL and sporadic subcortical
genetic locus. Nat Genet 1997; 16: 364–67. arteriosclerotic encephalopathy: MR imaging study with statistical
5 Schulz UG, Flossmann E, Rothwell PM. Heritability of ischemic parametric group comparison. Radiology 2001; 218: 443–51.
stroke in relation to age, vascular risk factors, and subtypes of 29 O’Sullivan M, Jarosz JM, Martin RJ, Deasy N, Powell JF,
incident stroke in population-based studies. Stroke 2004; 35: 819–24. Markus HS. MRI hyperintensities of the temporal lobe and external
6 Jerrard-Dunne P, Cloud G, Hassan A, Markus HS. Evaluating the capsule in patients with CADASIL. Neurology 2001; 56: 628–34.
genetic component of ischemic stroke subtypes: a family history 30 Joutel A, Vahedi K, Corpechot C, et al. Strong clustering and
study. Stroke 2003; 34: 1364–69. stereotyped nature of Notch3 mutations in CADASIL patients.
7 Jood K, Ladenvall C, Rosengren A, Blomstrand C, Jern C. Family Lancet 1997; 350: 1511–15.
history in ischemic stroke before 70 years of age: the Sahlgrenska 31 Peters N, Opherk C, Bergmann T, Castro M, Herzog J, Dichgans M.
Academy Study on Ischemic Stroke. Stroke 2005; 36: 1383–87. Spectrum of mutations in biopsy-proven CADASIL: implications
8 Humphries SE, Morgan L. Genetic risk factors for stroke and for diagnostic strategies. Arch Neurol 2005; 62: 1091–94.
carotid atherosclerosis: insights into pathophysiology from 32 Mazzei R, Conforti FL, Lanza PL, et al. A novel Notch3 gene
candidate gene approaches. Lancet Neurol 2004; 3: 227–35. mutation not involving a cysteine residue in an Italian family with
9 Fox CS, Polak JF, Chazaro I, et al. Genetic and environmental CADASIL. Neurology 2004; 63: 561–64.
contributions to atherosclerosis phenotypes in men and women: 33 Lesnik Oberstein SA, van den Boom R, Van Buchem MA, et al.
heritability of carotid intima-media thickness in the Framingham Cerebral microbleeds in CADASIL. Neurology 2001; 57: 1066–70.
Heart Study. Stroke 2003; 34: 397–401. 34 Dichgans M, Filippi M, Bruning R, et al. Quantitative MRI in
10 Moskau S, Golla A, Grothe C, Boes M, Pohl C, Klockgether T. CADASIL: correlation with disability and cognitive performance.
Heritability of carotid artery atherosclerotic lesions: an ultrasound Neurology 1999; 52: 1361–67.
study in 154 families. Stroke 2005; 36: 5–8. 35 Singhal S, Bevan S, Barrick T, Rich P, Markus HS. The influence of
11 Atwood LD, Wolf PA, Heard-Costa NL, et al. Genetic variation in genetic and cardiovascular risk factors on the CADASIL phenotype.
white matter hyperintensity volume in the Framingham Study. Brain 2004; 127: 2031–38.
Stroke 2004; 35: 1609–13. 36 Peters N, Opherk C, Zacherle S, Capell A, Gempel P, Dichgans M.
12 Turner ST, Jack CR, Fornage M, Mosley TH, Boerwinkle E, CADASIL associated Notch3 mutations have differential effects
de Andrade M. Heritability of leukoaraiosis in hypertensive both on ligand binding and ligand-induced Notch3 receptor
sibships. Hypertension 2004; 43: 483–87. signaling through RBP-Jk. Exp Cell Res 2004; 299: 454–64.
158 http://neurology.thelancet.com Vol 6 February 2007
Review
37 Joutel A, Andreux F, Gaulis S, et al. The ectodomain of Notch3 63 Hassan A, Hunt BJ, O’Sullivan M, et al. Homocysteine is a risk
receptor accumulates within the cerebrovasculature of CADASIL factor for cerebral small vessel disease, acting via endothelial
patients. J Clin Invest 2000; 105: 597–605. dysfunction. Brain 2004; 127: 212–19.
38 Ruchoux MM, Domenga V, Brulin P, et al. Transgenic mice 64 Bellamy MF, McDowell IF. Putative mechanisms for vascular
expressing mutant notch3 develop vascular alterations characteristic damage by homocysteine. J Inherit Metab Dis 1997; 20: 307–15.
of cerebral autosomal dominant arteriopathy with subcortical infarcts 65 Mandel H, Brenner B, Berant M, et al. Coexistence of hereditary
and leukoencephalopathy. Am J Pathol 2003; 162: 329–42. homocystinuria and factor V Leiden: effect on thrombosis. N Engl J
39 Ruchoux MM, Chabriat H, Bousser MG, Baudrimont M, Med 1996; 334: 763–68.
Tournier-Lasserve E. Presence of ultrastructural arterial lesions in 66 Yap S, Boers GH, Wilcken B, et al. Vascular outcome in patients
muscle and skin vessels of patients with CADASIL. Stroke 1994; with homocystinuria due to cystathionine beta-synthase deficiency
25: 2291–92. treated chronically: a multicenter observational study.
40 Opherk C, Peters N, Holtmannspoetter M, Gschwendtner A, Arterioscler Thromb Vasc Biol 2001; 21: 2080–85.
Muller-Myhsok B, Dichgans M. Heritability of MRI lesion volume in 67 Kraus JP, Janosik M, Kozich V, et al. Cystathionine beta-synthase
CADASIL: evidence for genetic modifiers. Stroke 2006; 37: 2684–89. mutations in homocystinuria. Hum Mutat 1999; 13: 362–75.
41 Crutchfield KE, Patronas NJ, Dambrosia JM, et al. Quantitative 68 Sebastio G, Sperandeo MP, Panico M, de Franchis R, Kraus JP,
analysis of cerebral vasculopathy in patients with Fabry disease. Andria G. The molecular basis of homocystinuria due to
Neurology 1998; 50: 1746–49. cystathionine beta-synthase deficiency in Italian families, and report
42 Grewal RP. Stroke in Fabry’s disease. J Neurol 1994; 241: 153–56. of four novel mutations. Am J Hum Genet 1995; 56: 1324–33.
43 Mitsias P, Levine SR. Cerebrovascular complications of Fabry’s 69 Pavlakis SG, Phillips PC, DiMauro S, De Vivo DC, Rowland LP.
disease. Ann Neurol 1996; 40: 8–17. Mitochondrial myopathy, encephalopathy, lactic acidosis, and
44 Altarescu G, Moore DF, Schiffmann R. Effect of genetic modifiers strokelike episodes: a distinctive clinical syndrome. Ann Neurol
on cerebral lesions in Fabry disease. Neurology 2005; 64: 2148–50. 1984; 16: 481–88.
45 Schiffmann R, Kopp JB, Austin HA, et al. Enzyme replacement 70 Martinez-Fernandez E, Gil-Peralta A, Garcia-Lozano R, et al.
therapy in Fabry disease: a randomized controlled trial. JAMA 2001; Mitochondrial disease and stroke. Stroke 2001; 32: 2507–10.
285: 2743–49. 71 Yoneda M, Maeda M, Kimura H, Fujii A, Katayama K, Kuriyama M.
46 Eng CM, Guffon N, Wilcox WR, et al. Safety and efficacy of Vasogenic edema on MELAS: a serial study with diffusion-weighted
recombinant human alpha-galactosidase A: replacement therapy in MR imaging. Neurology 1999; 53: 2182–84.
Fabry’s disease. N Engl J Med 2001; 345: 9–16. 72 Clark JM, Marks MP, Adalsteinsson E, et al. MELAS: Clinical and
47 Old J. Hemoglobinopathies and thalassemias. In: Rimoin DI, pathologic correlations with MRI, xenon/CT, and MR spectroscopy.
Connor JM, Pyeritz RE, Korf B, eds. Emery’s and Rimoin’s Neurology 1996; 46: 223–27.
principles and practice of medical genetics. 4th edn. London: 73 Iizuka T, Sakai F, Kan S, Suzuki N. Slowly progressive spread of the
Churchill Livingstone, 2002: 1861–98. stroke-like lesions in MELAS. Neurology 2003; 61: 1238–44.
48 Ohene-Frempong K, Weiner SJ, Sleeper LA, et al. Cerebrovascular 74 Judge DP, Dietz HC. Marfan’s syndrome. Lancet 2005; 366: 1965–76.
accidents in sickle cell disease: rates and risk factors. Blood 1998; 75 De Paepe A, Devereux RB, Dietz HC, Hennekam RC, Pyeritz RE.
91: 288–94. Revised diagnostic criteria for the Marfan syndrome.
49 Stockman JA, Nigro MA, Mishkin MM, Oski FA. Occlusion of large Am J Med Genet 1996; 62: 417–26.
cerebral vessels in sickle-cell anemia. N Engl J Med 1972; 287: 846–49. 76 Nollen GJ, Mulder BJ. What is new in the Marfan syndrome?
50 Pavlakis SG, Bello J, Prohovnik I, et al. Brain infarction in sickle cell Int J Cardiol 2004; 97 (suppl 1): 103–08.
anemia: magnetic resonance imaging correlates. Ann Neurol 1988; 77 Neptune ER, Frischmeyer PA, Arking DE, et al. Dysregulation of
23: 125–30. TGF-beta activation contributes to pathogenesis in Marfan
51 Schatz J, White DA, Moinuddin A, Armstrong M, DeBaun MR. syndrome. Nat Genet 2003; 33: 407–11.
Lesion burden and cognitive morbidity in children with sickle cell 78 Wityk RJ, Zanferrari C, Oppenheimer S. Neurovascular
disease. J Child Neurol 2002; 17: 891–95. complications of marfan syndrome: a retrospective, hospital-based
52 Hebbel RP, Osarogiagbon R, Kaul D. The endothelial biology of study. Stroke 2002; 33: 680–84.
sickle cell disease: inflammation and a chronic vasculopathy. 79 Spittell PC, Spittell JA, Joyce JW, et al. Clinical features and
Microcirculation 2004; 11: 129–51. differential diagnosis of aortic dissection: experience with 236 cases
53 Driscoll MC, Hurlet A, Styles L, et al. Stroke risk in siblings with (1980 through 1990). Mayo Clin Proc 1993; 68: 642–51.
sickle cell anemia. Blood 2003; 101: 2401–04. 80 Schievink WI, Michels VV, Piepgras DG. Neurovascular
54 Sebastiani P, Ramoni MF, Nolan V, Baldwin CT, Steinberg MH. manifestations of heritable connective tissue disorders: a review.
Genetic dissection and prognostic modeling of overt stroke in sickle Stroke 1994; 25: 889–903.
cell anemia. Nat Genet 2005; 37: 435–40. 81 Gott VL, Greene PS, Alejo DE, et al. Replacement of the aortic root in
55 Steinberg MH, Adewoye AH. Modifier genes and sickle cell patients with Marfan’s syndrome. N Engl J Med 1999; 340: 1307–13.
anemia. Curr Opin Hematol 2006; 13: 131–36. 82 Pepin M, Schwarze U, Superti-Furga A, Byers PH. Clinical and
56 Taylor JG, Tang DC, Savage SA, et al. Variants in the VCAM1 gene genetic features of Ehlers-Danlos syndrome type IV, the vascular
and risk for symptomatic stroke in sickle cell disease. Blood 2002; type. N Engl J Med 2000; 342: 673–80.
100: 4303–09. 83 North KN, Whiteman DA, Pepin MG, Byers PH. Cerebrovascular
57 Hoppe C, Klitz W, Cheng S, et al. Gene interactions and stroke risk complications in Ehlers-Danlos syndrome type IV. Ann Neurol 1995;
in children with sickle cell anemia. Blood 2004; 103: 2391–96. 38: 960–64.
58 Adams RJ, McKie VC, Hsu L, et al. Prevention of a first stroke by 84 van den Berg JS, Hennekam RC, Cruysberg JR, et al. Prevalence of
transfusions in children with sickle cell anemia and abnormal symptomatic intracranial aneurysm and ischaemic stroke in
results on transcranial Doppler ultrasonography. N Engl J Med 1998; pseudoxanthoma elasticum. Cerebrovasc Dis 2000; 10: 315–19.
339: 5–11. 85 Ikezaki K, Han DH, Kawano T, Kinukawa N, Fukui M. A clinical
59 Adams RJ, Brambilla D. Discontinuing prophylactic transfusions comparison of definite moyamoya disease between South Korea
used to prevent stroke in sickle cell disease. N Engl J Med 2005; and Japan. Stroke 1997; 28: 2513–17.
353: 2769–78. 86 Hallemeier CL, Rich KM, Grubb RL, et al. Clinical features and
60 Mudd SH, Levy HL, Skovby F. Disorders of transsulfuration. In: outcome in North American adults with moyamoya phenomenon.
Scriver CR, Beaudet AL, Sly WS, Valle D, eds. The metabolic basis Stroke 2006; 37: 1490–96.
of inherited disease. New York: McGraw Hill, 1995: 1279–327. 87 Fukuyama S, Kanai M, Osawa M. Clinical genetic analysis on the
61 Mudd SH, Skovby F, Levy HL, et al. The natural history of moyamoya disease. In: Fukui M, ed. Annual report 1990: the
homocystinuria due to cystathionine beta-synthase deficiency. research committee on sponataneous occlusion of the circle of
Am J Hum Genet 1985; 37: 1–31. willis (moyamoya disease) of the ministry of health and welfare.
62 Kelly PJ, Furie KL, Kistler JP, et al. Stroke in young patients with Fukuoka, Japan: Ministry of Health and Welfare, 1991: 53–59.
hyperhomocysteinemia due to cystathionine beta-synthase 88 Fukui M. Current state of study on moyamoya disease in Japan.
deficiency. Neurology 2003; 60: 275–79. Surg Neurol 1997; 47: 138–43.
http://neurology.thelancet.com Vol 6 February 2007 159
Review
89 Ikeda H, Sasaki T, Yoshimoto T, Fukui M, Arinami T. Mapping of a 116 Tuncer N, Tuglular S, Kilic G, Sazci A, Us O, Kara I. Evaluation of
familial moyamoya disease gene to chromosome 3p24.2-p26. the angiotensin-converting enzyme insertion/deletion
Am J Hum Genet 1999; 64: 533–37. polymorphism and the risk of ischaemic stroke. J Clin Neurosci
90 Yamauchi T, Tada M, Houkin K, et al. Linkage of familial moyamoya 2006; 13: 224–27.
disease (spontaneous occlusion of the circle of Willis) to 117 Sethi AA, Tybjaerg-Hansen A, Gronholdt ML, Steffensen R,
chromosome 17q25. Stroke 2000; 31: 930–35. Schnohr P, Nordestgaard BG. Angiotensinogen mutations and risk
91 Sakurai K, Horiuchi Y, Ikeda H, et al. A novel susceptibility locus for ischemic heart disease, myocardial infarction, and ischemic
for moyamoya disease on chromosome 8q23. J Hum Genet 2004; 49: cerebrovascular disease: six case-control studies from the
278–81. Copenhagen City Heart Study. Ann Intern Med 2001; 134: 941–54.
92 Franz WM, Muller OJ, Katus HA. Cardiomyopathies: from genetics 118 Schmidt H, Fazekas F, Kostner GM, van Duijn CM, Schmidt R.
to the prospect of treatment. Lancet 2001; 358: 1627–37. Angiotensinogen gene promoter haplotype and microangiopathy-
93 Maron BJ, Olivotto I, Bellone P, et al. Clinical profile of stroke in related cerebral damage: results of the Austrian Stroke Prevention
900 patients with hypertrophic cardiomyopathy. J Am Coll Cardiol Study. Stroke 2001; 32: 405–12.
2002; 39: 301–07. 119 Lalouschek W, Schillinger M, Hsieh K, et al. Matched case-control
94 Roberts R, Brugada R. Genetic aspects of arrhythmias. study on factor V Leiden and the prothrombin G20210A mutation
Am J Med Genet 2000; 97: 310–18. in patients with ischemic stroke/transient ischemic attack up to the
age of 60 years. Stroke 2005; 36: 1405–09.
95 Hassan A, Markus HS. Genetics and ischaemic stroke. Brain 2000;
123: 1784–812. 120 Lichy C, Reuner KH, Buggle F, et al. Prothrombin G20210A
mutation, but not factor V Leiden, is a risk factor in patients with
96 Strater R, Becker S, von Eckardstein A, et al. Prospective
persistent foramen ovale and otherwise unexplained cerebral
assessment of risk factors for recurrent stroke during childhood: a
ischemia. Cerebrovasc Dis 2003; 16: 83–87.
5-year follow-up study. Lancet 2002; 360: 1540–45.
121 Rubattu S, Speranza R, Ferrari M, et al. A role of TNF-alpha gene
97 Haywood S, Liesner R, Pindora S, Ganesan V. Thrombophilia and
variant on juvenile ischemic stroke: a case-control study.
first arterial ischaemic stroke: a systematic review. Arch Dis Child
Eur J Neurol 2005; 12: 989–93.
2005; 90: 402–05.
122 Santamaria A, Oliver A, Borrell M, et al. Risk of ischemic stroke
98 Naukkarinen J, Ehnholm C, Peltonen L. Genetics of familial
associated with functional thrombin-activatable fibrinolysis
combined hyperlipidemia. Curr Opin Lipidol 2006; 17: 285–90.
inhibitor plasma levels. Stroke 2003; 34: 2387–91.
99 Yanagawa S, Ito N, Arima K, Ikeda S. Cerebral autosomal recessive
123 Karttunen V, Hiltunen L, Rasi V, Vahtera E, Hillbom M. Factor V
arteriopathy with subcortical infarcts and leukoencephalopathy.
Leiden and prothrombin gene mutation may predispose to
Neurology 2002; 58: 817–20.
paradoxical embolism in subjects with patent foramen ovale.
100 Jen J, Cohen AH, Yue Q, et al. Hereditary endotheliopathy with Blood Coagul Fibrinolysis 2003; 14: 261–68.
retinopathy, nephropathy, and stroke (HERNS). Neurology 1997;
124 Aznar J, Mira Y, Vaya A, et al. Factor V Leiden and prothrombin
49: 1322–30.
G20210A mutations in young adults with cryptogenic ischemic
101 Verreault S, Joutel A, Riant F, et al. A novel hereditary small vessel stroke. Thromb Haemost 2004; 91: 1031–34.
disease of the brain. Ann Neurol 2006; 59: 353–57.
125 Jood K, Ladenvall P, Tjarnlund-Wolf A, et al. Fibrinolytic gene
102 Helgadottir A, Manolescu A, Helgason A, et al. A variant of the polymorphism and ischemic stroke. Stroke 2005; 36: 2077–81.
gene encoding leukotriene A4 hydrolase confers ethnicity-specific
126 Wiklund PG, Nilsson L, Ardnor SN, et al. Plasminogen activator
risk of myocardial infarction. Nat Genet 2006; 38: 68–74.
inhibitor-1 4G/5G polymorphism and risk of stroke: replicated
103 Dichgans M, Markus HS. Genetic association studies in stroke: findings in two nested case-control studies based on independent
methodological issues and proposed standard criteria. Stroke 2005; cohorts. Stroke 2005; 36: 1661–65.
36: 2027–31.
127 van Goor ML, Garcia EG, Leebeek F, Brouwers GJ, Koudstaal P,
104 Healy DG. Case-control studies in the genomic era: a clinician’s Dippel D. The plasminogen activator inhibitor (PAI-1) 4G/5G
guide. Lancet Neurol 2006; 5: 701–07. promoter polymorphism and PAI-1 levels in ischemic stroke: a case-
105 Wald DS, Law M, Morris JK. Homocysteine and cardiovascular disease: control study. Thromb Haemost 2005; 93: 92–96.
evidence on causality from a meta-analysis. BMJ 2002; 325: 1202. 128 Juul K, Tybjaerg-Hansen A, Steffensen R, Kofoed S, Jensen G,
106 Casas JP, Hingorani AD, Bautista LE, Sharma P. Meta-analysis of Nordestgaard BG. Factor V Leiden: the Copenhagen City Heart
genetic studies in ischemic stroke: thirty-two genes involving Study and 2 meta-analyses. Blood 2002; 100: 3–10.
approximately 18 000 cases and 58 000 controls. Arch Neurol 2004; 129 Gretarsdottir S, Thorleifsson G, Reynisdottir ST, et al. The gene
61: 1652–61. encoding phosphodiesterase 4D confers risk of ischemic stroke.
107 Cronin S, Furie KL, Kelly PJ. Dose-related association of MTHFR Nat Genet 2003; 35: 131–38.
677T allele with risk of ischemic stroke: evidence from a cumulative 130 Bevan S, Porteous L, Sitzer M, Markus HS. Phosphodiesterase 4D
meta-analysis. Stroke 2005; 36: 1581–87. gene, ischemic stroke, and asymptomatic carotid atherosclerosis.
108 Slooter AJ, Rosendaal FR, Tanis BC, Kemmeren JM, van der Graaf Y, Stroke 2005; 36: 949–53.
Algra A. Prothrombotic conditions, oral contraceptives, and the risk 131 Lohmussaar E, Gschwendtner A, Mueller JC, et al. ALOX5AP gene
of ischemic stroke. J Thromb Haemost 2005; 3: 1213–17. and the PDE4D gene in a central European population of stroke
109 Dikmen M, Ozbabalik D, Gunes HV, et al. Acute stroke in relation patients. Stroke 2005; 36: 731–36.
to homocysteine and methylenetetrahydrofolate reductase gene 132 Nilsson-Ardnor S, Wiklund PG, Lindgren P, et al. Linkage of
polymorphisms. Acta Neurol Scand 2006; 113: 307–14. ischemic stroke to the PDE4D region on 5q in a Swedish
110 Grossmann R, Geisen U, Merati G, et al. Genetic risk factors in population. Stroke 2005; 36: 1666–71.
young adults with ‘cryptogenic’ ischemic cerebrovascular disease. 133 Meschia JF, Brott TG, Brown RD, et al. Phosphodiesterase 4D and
Blood Coagul Fibrinolysis 2002; 13: 583–90. 5-lipoxygenase activating protein in ischemic stroke. Ann Neurol
111 Lonn E, Yusuf S, Arnold MJ, et al. Homocysteine lowering with 2005; 58: 351–61.
folic acid and B vitamins in vascular disease. N Engl J Med 2006; 134 van Rijn MJ, Slooter AJ, Schut AF, et al. Familial aggregation, the
354: 1567–77. PDE4D gene, and ischemic stroke in a genetically isolated
112 Hankey GJ. Is plasma homocysteine a modifiable risk factor for population. Neurology 2005; 65: 1203–09.
stroke? Nat Clin Pract Neurol 2006; 2: 26–33. 135 Saleheen D, Bukhari S, Haider SR, et al. Association of
113 Sayed-Tabatabaei FA, Oostra BA, Isaacs A, van Duijn CM, phosphodiesterase 4D gene with ischemic stroke in a Pakistani
Witteman JC. ACE polymorphisms. Circ Res 2006; 98: 1123–33. population. Stroke 2005; 36: 2275–77.
114 Brenner D, Labreuche J, Poirier O, Cambien F, Amarenco P. Renin- 136 Nakayama T, Asai S, Sato N, Soma M. Genotype and haplotype
angiotensin-aldosterone system in brain infarction and vascular association study of the STRK1 region on 5q12 among Japanese: a
death. Ann Neurol 2005; 58: 131–38. case-control study. Stroke 2006; 37: 69–76.
115 Rubattu S, Di Angelantonio E, Stanzione R, et al. Gene 137 Woo D, Kaushal R, Kissela B, et al. Association of
polymorphisms of the renin-angiotensin-aldosterone system and the Phosphodiesterase 4D with ischemic stroke: a population-based
risk of ischemic stroke: a role of the A1166C/AT1 gene variant. case-control study. Stroke 2006; 37: 371–76.
J Hypertens 2004; 22: 2129–34.
160 http://neurology.thelancet.com Vol 6 February 2007
Review
138 Kuhlenbaumer G, Berger K, Huge A, et al. Evaluation of single 145 Sudlow C, Martinez Gonzalez NA, Kim J, Clark C. Does
nucleotide polymorphisms in the phosphodiesterase 4D gene apolipoprotein E genotype influence the risk of ischemic stroke,
(PDE4D) and their association with ischaemic stroke in a large intracerebral hemorrhage, or subarachnoid hemorrhage?
German cohort. J Neurol Neurosurg Psychiatry 2006; 77: 521–24. Systematic review and meta-analyses of 31 studies among 5961
139 Brophy VH, Ro SK, Rhees BK, et al. Association of cases and 17 965 controls. Stroke 2006; 37: 364–70.
phosphodiesterase 4D polymorphisms with ischemic stroke in a US 146 Huang Z, Huang PL, Panahian N, Dalkara T, Fishman MC,
population stratified by hypertension status. Stroke 2006; 37: Moskowitz MA. Effects of cerebral ischemia in mice deficient in
1385–90. neuronal nitric oxide synthase. Science 1994; 265: 1883–85.
140 Zee RY, Brophy VH, Cheng S, Hegener HH, Erlich HA, Ridker PM. 147 Gretarsdottir S, Sveinbjornsdottir S, Jonsson HH, et al. Localization
Polymorphisms of the phosphodiesterase 4D, cAMP-specific of a susceptibility gene for common forms of stroke to 5q12.
(PDE4D) gene and risk of ischemic stroke: a prospective, nested Am J Hum Genet 2002; 70: 593–603.
case–control evaluation. Stroke 2006; 37: 1955–57. 148 Meschia JF, Brown RD, Brott TG, Chukwudelunzu FE, Hardy J,
141 Rosand J, Bayley N, Rost N, de Bakker PI. Many hypotheses but no Rich SS. The Siblings With Ischemic Stroke Study (SWischaemic
replication for the association between PDE4D and stroke. strokeS) protocol. BMC Med Genet 2002; 3: 1.
Nat Genet 2006; 38: 1091–92. 149 Risch N, Merikangas K. The future of genetic studies of complex
142 Helgadottir A, Gretarsdottir S, St Clair D, et al. Association between human diseases. Science 1996; 273: 1516–17.
the gene encoding 5-lipoxygenase-activating protein and stroke 150 Taube J, Halsall D, Baglin T. Influence of cytochrome P-450
replicated in a Scottish population. Am J Hum Genet 2005; CYP2C9 polymorphisms on warfarin sensitivity and risk of over-
76: 505–09. anticoagulation in patients on long-term treatment. Blood 2000;
143 Zee RY, Cheng S, Hegener HH, Erlich HA, Ridker PM. Genetic 96: 1816–19.
variants of arachidonate 5-lipoxygenase-activating protein, and risk 151 Rieder MJ, Reiner AP, Gage BF, et al. Effect of VKORC1 haplotypes
of incident myocardial infarction and ischemic stroke: a nested on transcriptional regulation and warfarin dose. N Engl J Med 2005;
case-control approach. Stroke 2006; 37: 2007–11. 352: 2285–93.
144 Qiu H, Gabrielsen A, Agardh HE, et al. Expression of 152 Hakonarson H, Thorvaldsson S, Helgadottir A, et al. Effects of a
5-lipoxygenase and leukotriene A4 hydrolase in human 5-lipoxygenase-activating protein inhibitor on biomarkers associated
atherosclerotic lesions correlates with symptoms of plaque with risk of myocardial infarction: a randomized trial. JAMA 2005;
instability. Proc Natl Acad Sci USA 2006; 103: 8161–66. 293: 2245–56.
http://neurology.thelancet.com Vol 6 February 2007 161
You might also like
- Relative Familial ClusterDocument8 pagesRelative Familial ClusterIgn_SkyfangNo ratings yet
- Stroke GeneticsDocument13 pagesStroke GeneticsRenato RamonNo ratings yet
- Genetica de La DemenciaDocument20 pagesGenetica de La Demenciajhoel cruzNo ratings yet
- Genetic Risk Factors For Ischemic and Hemorrhagic Stroke: Stroke (JF Meschia, Section Editor)Document11 pagesGenetic Risk Factors For Ischemic and Hemorrhagic Stroke: Stroke (JF Meschia, Section Editor)natasyahNo ratings yet
- Childhood Cognitive Ability and Risk ofDocument7 pagesChildhood Cognitive Ability and Risk ofChouaib OujhainNo ratings yet
- Congenital Heart Diseases Genetics, Noninherited Risk Factors, and SignalingDocument12 pagesCongenital Heart Diseases Genetics, Noninherited Risk Factors, and SignalingMilena CelyNo ratings yet
- Alzheimer's Disease: Genes, Pathogenesis and Risk PredictionDocument7 pagesAlzheimer's Disease: Genes, Pathogenesis and Risk PredictionWindaNo ratings yet
- Clonal Hematopoiesis and Risk For Atherosclerotic CardiovascularDocument15 pagesClonal Hematopoiesis and Risk For Atherosclerotic CardiovasculargiulioNo ratings yet
- Referensi Tesis 1Document6 pagesReferensi Tesis 1Endy SusenoNo ratings yet
- Childhood Arterial Ischemic StrokeDocument12 pagesChildhood Arterial Ischemic StrokeKota AnuroopNo ratings yet
- Basic Kes Zavoreo Demarin 355 359 PDFDocument5 pagesBasic Kes Zavoreo Demarin 355 359 PDFgeraldi radityaNo ratings yet
- J Ejrad 2012 12 026Document8 pagesJ Ejrad 2012 12 026AnnetNo ratings yet
- Physical Factors Effecting Cerebral Aneurysm PathophysiologyDocument20 pagesPhysical Factors Effecting Cerebral Aneurysm Pathophysiologymira ariantiNo ratings yet
- NIH Public Access: Author ManuscriptDocument11 pagesNIH Public Access: Author ManuscriptGabriela PopescuNo ratings yet
- ioi60144_2388_2394Document7 pagesioi60144_2388_2394orangeshibuya99No ratings yet
- Age-Related Clonal HematopoiesisDocument11 pagesAge-Related Clonal HematopoiesisgiulioNo ratings yet
- A Prospective Evaluation of An Angiotensin-Converting-Enzyme Gene Polymorphism and The Risk of Ischemic Heart DiseaseDocument6 pagesA Prospective Evaluation of An Angiotensin-Converting-Enzyme Gene Polymorphism and The Risk of Ischemic Heart DiseaseMuthu KumarNo ratings yet
- Circgen 121 003635Document8 pagesCircgen 121 003635szumutku fanniNo ratings yet
- Family History of Alzheimer's Disease and Cortical Thickness in Patients With DementiaDocument7 pagesFamily History of Alzheimer's Disease and Cortical Thickness in Patients With DementiaMarcos Josue Costa DiasNo ratings yet
- Enfermedad CardiovascularDocument20 pagesEnfermedad CardiovascularMerari Lugo OcañaNo ratings yet
- Psoriasis With Vascular DiseaseDocument4 pagesPsoriasis With Vascular Diseasemegh dutNo ratings yet
- Stroke IskemikDocument49 pagesStroke IskemikyasserNo ratings yet
- The Role of Genetic Variation in Haemorrhagic Stroke: An UpdateDocument4 pagesThe Role of Genetic Variation in Haemorrhagic Stroke: An UpdateLulu LuwiiNo ratings yet
- Periodontitis y Enfermedad CardiovascularDocument8 pagesPeriodontitis y Enfermedad CardiovascularDafne MendozaNo ratings yet
- Genética Da EMDocument12 pagesGenética Da EMilc67123No ratings yet
- Coronary Heart Disease Risk Factors and Atherosclerosis in Young PeopleDocument9 pagesCoronary Heart Disease Risk Factors and Atherosclerosis in Young PeopleHadi KuriryNo ratings yet
- Gim 2014144Document7 pagesGim 2014144AvneelNo ratings yet
- Cold Spring Harb Perspect Biol-2018-Erkkinen-A033118Document46 pagesCold Spring Harb Perspect Biol-2018-Erkkinen-A033118Brenda GutiérrezNo ratings yet
- Ictus en Joven Ferro2010Document12 pagesIctus en Joven Ferro2010Mez RealNo ratings yet
- Stroke in Systemic Lupus Erythematosus and Antiphospholipid Syndrome: Risk Factors, Clinical Manifestations, Neuroimaging, and TreatmentDocument9 pagesStroke in Systemic Lupus Erythematosus and Antiphospholipid Syndrome: Risk Factors, Clinical Manifestations, Neuroimaging, and TreatmentKarl Martin PinedaNo ratings yet
- Alzheimer Dementia JAMADocument4 pagesAlzheimer Dementia JAMAAna RendónNo ratings yet
- Faktor Risiko THD Stroke Iskemik EnglishDocument6 pagesFaktor Risiko THD Stroke Iskemik EnglishZiafadeNo ratings yet
- Update Managemant Unrupture Aneurysm 2018Document8 pagesUpdate Managemant Unrupture Aneurysm 2018Mikha ManurungNo ratings yet
- Circresaha 116 308398Document25 pagesCircresaha 116 308398ekaNo ratings yet
- The Current Landscape of Genetic Testing in Cardiovascular Malformations: Opportunities and ChallengesDocument11 pagesThe Current Landscape of Genetic Testing in Cardiovascular Malformations: Opportunities and ChallengesGlauce L TrevisanNo ratings yet
- Epidemiology and PreventionDocument9 pagesEpidemiology and PreventiondrelvNo ratings yet
- Klein 2014Document10 pagesKlein 2014Diana TricoracheNo ratings yet
- Emerging Molecular Mechanisms of Vascular Dementia: ReviewDocument8 pagesEmerging Molecular Mechanisms of Vascular Dementia: ReviewJuan Jose Eraso OsorioNo ratings yet
- Genetics of Endocrinology: Amit R. Majithia - David Altshuler - Joel N. HirschhornDocument20 pagesGenetics of Endocrinology: Amit R. Majithia - David Altshuler - Joel N. HirschhornDr Mehul Kumar ChourasiaNo ratings yet
- Biomolecules 09 00879Document23 pagesBiomolecules 09 00879Laura Daniela MurilloNo ratings yet
- Circgenetics 112 963439Document7 pagesCircgenetics 112 96343932. Nguyễn Tiến Thái SơnNo ratings yet
- Neuropathologic Features of Central Nervous System HemangioblastomaDocument11 pagesNeuropathologic Features of Central Nervous System HemangioblastomaDavid Camilo GomezNo ratings yet
- Stroke Prevention and Treatment in Sickle Cell Disease: Robert J. Adams, MS, MDDocument4 pagesStroke Prevention and Treatment in Sickle Cell Disease: Robert J. Adams, MS, MDMeshaki MbarukaNo ratings yet
- Premature Atherosclerotic Cardiovascular Disease Trends in INcidence, Related Risk FactorDocument14 pagesPremature Atherosclerotic Cardiovascular Disease Trends in INcidence, Related Risk FactorAda DaiNo ratings yet
- Association Between Multiple Cardiovascular Risk FactorsDocument7 pagesAssociation Between Multiple Cardiovascular Risk FactorsRicardo CarminatoNo ratings yet
- Ajiboye 2015Document11 pagesAjiboye 2015editingjuryNo ratings yet
- BMJ k96 FullDocument9 pagesBMJ k96 FullDheaNo ratings yet
- Dilated Cardiomyopathy Causes, Mechanisms, and Current and Future Treatment ApproachesDocument14 pagesDilated Cardiomyopathy Causes, Mechanisms, and Current and Future Treatment ApproachesBatoulNo ratings yet
- Circulationaha 107 703389 PDFDocument7 pagesCirculationaha 107 703389 PDFlidia_694187376No ratings yet
- Hemostatic and Thrombotic Considerations in The Diagnosis and ManagementDocument12 pagesHemostatic and Thrombotic Considerations in The Diagnosis and Managementender izaguirreNo ratings yet
- Screening para Biomarcadores Asociado A EVC Isquemico en Fibrilacion AuricularDocument41 pagesScreening para Biomarcadores Asociado A EVC Isquemico en Fibrilacion AuricularAdán TreminioNo ratings yet
- Genetic Cardiomyopathies: ReviewDocument9 pagesGenetic Cardiomyopathies: ReviewThaís ValençaNo ratings yet
- Heart FailureDocument4 pagesHeart FailureHany ElbarougyNo ratings yet
- 1 s2.0 S0735109716332739 MainDocument11 pages1 s2.0 S0735109716332739 MainBhagya Narayan PanditNo ratings yet
- New Coronary Heart Disease Risk Factors - 2022 - AjmDocument2 pagesNew Coronary Heart Disease Risk Factors - 2022 - AjmBladimir CentenoNo ratings yet
- Genetics of Dilated CardiomyopathyDocument12 pagesGenetics of Dilated CardiomyopathyPhạm Quang LongNo ratings yet
- Hemorrhagic and Ischemic Strokes Compared: Stroke Severity, Mortality, and Risk FactorsDocument5 pagesHemorrhagic and Ischemic Strokes Compared: Stroke Severity, Mortality, and Risk FactorssavitageraNo ratings yet
- Pathophysiology and Genetic Factors in Moyamoya DiseaseDocument6 pagesPathophysiology and Genetic Factors in Moyamoya Diseasethomsoon01No ratings yet
- Content ServerDocument8 pagesContent ServerNourma Kusuma WinawanNo ratings yet
- Fast Facts: Myelodysplastic Syndromes: Determining risk, tailoring therapy, supporting patientsFrom EverandFast Facts: Myelodysplastic Syndromes: Determining risk, tailoring therapy, supporting patientsNo ratings yet
- Ladecola C, Anrather J. (2012)Document13 pagesLadecola C, Anrather J. (2012)Rusda AnandaNo ratings yet
- Dhandapani, M. Krishnan., and Brann, W. Darrell. (2003)Document10 pagesDhandapani, M. Krishnan., and Brann, W. Darrell. (2003)Rusda AnandaNo ratings yet
- b-Adducin Required for Memory EnrichmentDocument15 pagesb-Adducin Required for Memory EnrichmentRusda AnandaNo ratings yet
- Ernfors P, Kucera J, Lee KF, Et Al. (1995)Document9 pagesErnfors P, Kucera J, Lee KF, Et Al. (1995)Rusda AnandaNo ratings yet
- Administrative Reform in Developing Nations - Ali Farazmand - 2002Document280 pagesAdministrative Reform in Developing Nations - Ali Farazmand - 2002Rusda AnandaNo ratings yet
- Models of Local GovernanceDocument277 pagesModels of Local GovernanceRusda AnandaNo ratings yet
- Assessment of Medical Waste Management in Seven Hospitals in Lagos, NigeriaDocument11 pagesAssessment of Medical Waste Management in Seven Hospitals in Lagos, NigeriaRusda AnandaNo ratings yet
- 1 s2.0 S2212567116302805 MainDocument4 pages1 s2.0 S2212567116302805 MainRusda AnandaNo ratings yet
- 21025Document11 pages21025Rusda AnandaNo ratings yet
- Tugas KLP 1 Safe Management of Wastes From Health Care ActivitiesDocument21 pagesTugas KLP 1 Safe Management of Wastes From Health Care ActivitiesRusda AnandaNo ratings yet
- Admission FormDocument1 pageAdmission FormYasin AhmedNo ratings yet
- Labor Induced AugmentedDocument9 pagesLabor Induced Augmentednursereview83% (6)
- MASTITE GANGRENOSA BOVINA POR Clostridium Perfring - Amandio Steffen NetoDocument5 pagesMASTITE GANGRENOSA BOVINA POR Clostridium Perfring - Amandio Steffen NetoAmandio Steffen NetoNo ratings yet
- Randomized Controlled TrialsDocument22 pagesRandomized Controlled TrialsJerome G ThampiNo ratings yet
- PNLE Nursing Licensure Exam OutlineDocument11 pagesPNLE Nursing Licensure Exam OutlineJehanie LukmanNo ratings yet
- Eating Disorders and The Internet: The Therapeutic PossibilitiesDocument7 pagesEating Disorders and The Internet: The Therapeutic PossibilitiesPaula SalidoNo ratings yet
- Brintellix: What Is in This LeafletDocument5 pagesBrintellix: What Is in This LeafletFsNo ratings yet
- Amlodipine Captopril MetronidazoleDocument5 pagesAmlodipine Captopril Metronidazolekhrysty1506No ratings yet
- Acute Appendicitis PaperDocument6 pagesAcute Appendicitis Paperapi-279084200No ratings yet
- Certificate For COVID-19 Vaccination: Beneficiary DetailsDocument1 pageCertificate For COVID-19 Vaccination: Beneficiary DetailsGlobal printNo ratings yet
- People v. Filomeno G.R. No. L-33211Document11 pagesPeople v. Filomeno G.R. No. L-33211fgNo ratings yet
- High Blood Pressure Thesis StatementDocument8 pagesHigh Blood Pressure Thesis StatementCheapestPaperWritingServiceCanada100% (1)
- Healthcare System in MalaysiaDocument11 pagesHealthcare System in MalaysiaHui Pin100% (1)
- EMRA Antibiotic Guide EMRADocument2 pagesEMRA Antibiotic Guide EMRAPaoNu0% (3)
- Texas Has The Highest Maternal Mortality Rate in The Developed WorldDocument5 pagesTexas Has The Highest Maternal Mortality Rate in The Developed WorldDixanetNo ratings yet
- Nur330 Final PaperDocument8 pagesNur330 Final Paperapi-541746043No ratings yet
- Drug Study - MirceraDocument2 pagesDrug Study - MirceraRene John FranciscoNo ratings yet
- Otiflox New Ear DropsDocument9 pagesOtiflox New Ear DropsShreyas ModiNo ratings yet
- Pharmacology: Dr. Rakesh A Malpure Dr. Chandresh B DumatarDocument3 pagesPharmacology: Dr. Rakesh A Malpure Dr. Chandresh B DumatarChandresh DumatarNo ratings yet
- 298Document200 pages298Ching Chi TatNo ratings yet
- 3D Versus Standard Miniplate Fixation in The Management of Mandibular FracturesDocument9 pages3D Versus Standard Miniplate Fixation in The Management of Mandibular FracturesGATOT WIDYATMO PRINGGODIGDONo ratings yet
- Frozen Shoulder (Buku Komplit Etiologi DLL)Document7 pagesFrozen Shoulder (Buku Komplit Etiologi DLL)Ricky Diah Ayu AnggrainiNo ratings yet
- Drug StudyDocument5 pagesDrug StudyTracy Malingin QuimqueNo ratings yet
- Radiological Diagnostics of Respiratory SystemDocument70 pagesRadiological Diagnostics of Respiratory SystemVAISHALI CHOUDHARYNo ratings yet
- Nurse's Notes on Patient Admitted for Abnormal Uterine BleedingDocument6 pagesNurse's Notes on Patient Admitted for Abnormal Uterine BleedingAina De LeonNo ratings yet
- Drug Dose Determination Using Pharmacokinetic PrinciplesDocument36 pagesDrug Dose Determination Using Pharmacokinetic PrinciplesSreya Sanil100% (1)
- Igims DirectoryDocument28 pagesIgims DirectoryRavi ManiyarNo ratings yet
- Ro-Ils PaperDocument4 pagesRo-Ils Paperapi-502011468No ratings yet
- Gary Earle ResumeDocument2 pagesGary Earle Resumeapi-310096159No ratings yet
- Urquhart 2019Document9 pagesUrquhart 2019Vanessa DuzNo ratings yet