0% found this document useful (0 votes)
226 views18 pagesOsteopathic Assessment Guide
This document provides guidance on performing a physical therapy examination, including:
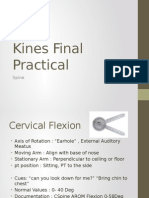
1. Evaluating range of motion, end feels, and palpating tissues for asymmetries or restrictions.
2. Performing a standing postural assessment examining anterior and posterior body landmarks.
3. Testing range of motion for various joints like the cervical spine, shoulder, elbow, and assessing gait, balance, and proprioception.
4. Identifying somatic dysfunctions through static and dynamic evaluation and incorporating tests of asymmetry, restriction, tissue texture changes and tenderness.
Uploaded by
joe doweCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as DOCX, PDF, TXT or read online on Scribd
0% found this document useful (0 votes)
226 views18 pagesOsteopathic Assessment Guide
This document provides guidance on performing a physical therapy examination, including:
1. Evaluating range of motion, end feels, and palpating tissues for asymmetries or restrictions.
2. Performing a standing postural assessment examining anterior and posterior body landmarks.
3. Testing range of motion for various joints like the cervical spine, shoulder, elbow, and assessing gait, balance, and proprioception.
4. Identifying somatic dysfunctions through static and dynamic evaluation and incorporating tests of asymmetry, restriction, tissue texture changes and tenderness.
Uploaded by
joe doweCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as DOCX, PDF, TXT or read online on Scribd