Professional Documents
Culture Documents
A Primer On Clinical Pathways: Hospital Pharmacy May 2016
Uploaded by
agung kurniaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
A Primer On Clinical Pathways: Hospital Pharmacy May 2016
Uploaded by
agung kurniaCopyright:
Available Formats
See discussions, stats, and author profiles for this publication at: https://www.researchgate.
net/publication/303394897
A Primer on Clinical Pathways
Article in Hospital pharmacy · May 2016
DOI: 10.1310/hpj5105-416
CITATIONS READS
5 347
3 authors, including:
Erik Abel
Highmark Health
45 PUBLICATIONS 222 CITATIONS
SEE PROFILE
Some of the authors of this publication are also working on these related projects:
Extracorporeal Membrane Oxygenation (ECMO) View project
All content following this page was uploaded by Erik Abel on 15 May 2018.
The user has requested enhancement of the downloaded file.
Hosp Pharm 2016;51(5):416–421
2016 © Thomas Land Publishers, Inc.
www.hospital-pharmacy.com
doi: 10.1310/hpj5105-416
Director’s Forum
A Primer on Clinical Pathways
Rachel Hipp, PharmD, BCPS•; Erik Abel, PharmD, BCPS†; and
Robert J. Weber, PharmD, MS, BCPS, FASHP‡
Leaders in health-system pharmacy are challenged to maintain the highest quality pharmacy ser-
vice at the lowest cost. Clinical pathways are evidence-based road maps that assist in reducing
variations in clinical practice. Integration of clinical pathways within the electronic health record
further helps to facilitate evidence-based practice. This article reviews the evolution of the clinical
pathways, describes their clinical and economic impact, and identifies ways pharmacy directors
can successfully implement these pathways into their institutions. Pharmacy directors can utilize
their skills in this area or task clinical pharmacists to serve as members of the clinical pathway
development team to further enhance patient-centered pharmacy services.
INTRODUCTION Clinical pathways are used to reduce variations
Despite a historic slowing since 2010, health in practice and align decisions with evidence-based
care spending in the United States still ranks among medicine, operational efficiency, and quality. A clini-
the highest per capita while quality outcomes and cal pathway provides clinical oversight and standard
access to care are lagging.1 There have been some expectations for a patient’s clinical course in disease
improvements, including a $316 B Medicare spend- state management or recovery to achieve 4 common
ing decrease between 2009 and 2013.2 goals – decreased care fragmentation, optimized
However, significant changes in payment reform cost effectiveness, improved patient throughput, and
bring a heightened awareness of the need to focus enhanced patient and family education regarding an
on improving delivery of care. The US Department of anticipated treatment course.4
Health and Human Services (HHS) has set a goal for Multiple providers interact with patients dur-
30% of Medicare payments to be based on alterna- ing their stay, which can result in fragmentation
tive payment models by the end of 2016, increasing within the system and create poor outcomes for the
to 50% by the end of 2018. Additionally HHS aims patients. With their unique skill-set for the manage-
to associate 90% of the remaining fee for service ment of medication therapy across the continuum
(FFS) payments with quality or value in some fashion of care, pharmacists play a key role in the devel-
by the end of 2018.3 opment of clinical pathways. These pathways allow
Changes in health care reimbursement demon- proactive engagement and positioning of the core
strate how financial incentives are being realigned to clinical services that pharmacists provide including
facilitate medical practice and behavioral modification. drug use evaluation, drug information, adverse drug
This modification is imperative in transforming health reaction management, drug therapy and pharma-
care delivery in the United States around the funda- cokinetic monitoring, drug counseling, emergency
mental aspects of economic viability, global health, and response participation, medication histories, and
social revitalization and accountability for the better- reconciliation.
ment of public health. Inappropriate variations in care The American College of Clinical Pharmacy
contribute to inefficiency in health care. When varia- (ACCP) has published several position statements on
tions are based on preference rather than evidence- the pharmacists’ role in clinical pathways. They pro-
based decision making, they result in inappropriate mote the pharmacist as a pharmacology and phar-
expenditures in labor costs, increased supply chain macotherapy expert who is specifically involved in
waste or redundancy, and inefficient communication. guideline development and implementation and
*
Specialty Pharmacy Resident, Health-System Pharmacy Administration; †Transformation & Operations Improvement Officer, Clin-
ical Pharmacy Specialist; ‡Administrator, Pharmacy Services, The Ohio State University Wexner Medical Center, Columbus, Ohio
416 Volume 51, May 2016
Director’s Forum
policy development and creation.4 Clinical pathways, field experts to establish expectations for best prac-
supported by evidence-based medicine, can serve as a tices.6 Clinical pathways are operational tools for
roadmap to guide practitioners in providing patient- executing best practices based upon local practice
centered care; clinical pathways can also serve as a and clinical guidelines that are shaped by interdis-
way to control escalating health care costs, particu- ciplinary teams. These pathways create a consistent
larly in the area of pharmaceuticals.5 workflow for care delivery. For example, a total hip
Pharmacy directors must continue to investigate replacement clinical pathway depicts the workflow
ways to enable pharmacist engagement in patient- expected of health care practitioners, establishing the
centered care while facilitating enhancements in time frame for an evidence-based practice to occur.
upstream efficiency, safety, and improved outcomes. This pathway provides a standard framework of
The goal of this article is to highlight the importance expectations in the pre-, intra-, and postoperative
of the pharmacy department’s proactive engagement phases for integrating the practical deliverables from
in clinical pathway development and the integra- the clinical practice guidelines for antibiotic prophy-
tion of optimal pharmacy care within the standard- laxis, glucose management, thrombosis prophylaxis,
ized progression of the pathway. This article will (a) and much more.
summarize the evolution of clinical pathways, (b)
describe the clinical and economic impact of clinical Paper Pathway Use and Process
pathways for health systems, and (c) identify ways Prior to the development of the electronic medi-
that pharmacy leaders can successfully integrate and cal record (EMR), clinical pathways were part of a
implement clinical pathways to grow and leverage paper documentation system.5,6 Caregivers docu-
patient-centered pharmacy services. mented the completion of activities in one location
within the paper chart. These pathways required
HISTORY AND EVOLUTION OF CLINICAL PATHWAYS multiple documents, including order sets, educa-
Clinical pathways emerged in the early 1980s in tional materials, and variance reporting documents.6
response to changes in health care reimbursement.4 The patient chart and clinical pathway were usu-
Reimbursement had been tied to the volume of care ally located at the patient bedside, allowing limited
delivered, with little focus on quality. Restructur- staff to gain access to relevant documents at the
ing realigned the incentives for care, basing them on same time. After integration of EMRs, all staff can
population health management principles that were access patient records and the clinical pathway for
focused on positive health care outcomes. Initially, their treatment. Furthermore, paper documentation
these pathways concentrated on high-yield oppor- of pathway progression that is not integrated into the
tunities for specific patient populations: high risk, natural workflow and management of the patient is
high dollar, or high volume.4 These medical or surgi- redundant. Limited technological capabilities require
cal populations have conditions that are consistent the use of paper documentation; however, technolog-
and predictable, and their care is standardized based ical advancements within health systems will increase
upon medical evidence shown to improve outcomes the ability for implementation of clinical pathways
and efficiency while reducing costs and variability. into the electronic EMR.
Identification of the correct patient populations for
whom to create a clinical pathway is a crucial step Electronic Integration
in the development phase. Such populations will Health care information technology (HIT) has
have high volume conditions that are addressed with evolved over the past decade with the implementa-
consistent evidence-based management and estab- tion of the EMR and standards, such as the Center
lished landmarks in care progression and length of for Medicare & Medicaid’s (CMS) Electronic Health
stay. Opportune areas for clinical pathway develop- Record Incentive Program or “meaningful use crite-
ment and integration are those that exhibit the above ria.” These criteria are used to incentivize and guide
characteristics but that still demonstrate considerable facilities in upgrading paper documentation to a safe
care variation or are beyond benchmark targets for and efficient electronic process. Hospitals need to com-
performance. Table 1 lists a sample clinical pathway ply by these standards for reimbursement from CMS.7
for coronary artery bypass postoperative care. Clinical pathways may serve as an integration tool,
Clinical pathways are different from clinical assisting providers to document achievement of spec-
guidelines. Clinical guidelines are based upon primary ified outcomes or variances in patient-related activi-
evidence, extensive analysis, and discussion amongst ties. Wakamiya and colleagues proposed standard
Hospital Pharmacy 417
Director’s Forum
Table 1. Coronary artery bypass surgery postoperative clinical pathwaya
Steps Predominant outcome goals Outcome Pertinent RN care plan Patient
variances orders documented education
documented released
Clinical pathway entered at end of OR before transfer to ICU
0-24 h • Extubation in <6 h ✔ ✔ ✔ ✔
• Hemodynamic stability
• Central lines removed if criteria met
POD 1 • ICU-PCU transition (order reconciliation and patient ✔ ✔ ✔ ✔
transfer)
• Antibiotics completed, beta-blocker started, analgesia
optimization, VTE prophylaxis, advance diet, convert
medications to PO if able
■ Evaluate for core measure qualifications
■ Initiate discharge planning
■ Ambulate
■ Foley removal if criteria met
■ Ambulate at least x1
POD 2 • Rehab and diabetes assessments completed ✔ ✔ ✔ ✔
• Ambulate x3
• Pacing wires and chest tubes removed if criteria met
POD 3 • Disposition and DC anticoagulation plan established ✔ ✔ ✔ ✔
• Escalate bowel regimen if needed
• Ambulate x3
POD 4 • All meds converted to PO (including diuretics) ✔ ✔ ✔ ✔
• DC readiness order set placed and initiate DC
teaching
• Ambulate x3
POD 5 • Assessment of DC preparedness (discharge if able) ✔ ✔ ✔ ✔
• Chest tube sutures removed
• Ambulate x3
POD 6 • Assessment of DC preparedness (discharge if able) If still an inpatient
• Ambulate x3
POD 7 • Assessment of DC preparedness (discharge if able) If still an inpatient
• Ambulate x3
Note: DC = discharge; ICU = intensive care unit; OR = operating room; PCU = progressive care unit; PO = oral; POD = postoperative day; RN = nurse; VTE =
venous thromboembolism.
a
Adapted from the clinical pathway used at The Ohio State University Wexner Medical Center.
functions that are necessary to maintain a user- integration of order sets, educational materials, nurs-
friendly electronic clinical pathway.8 These include ing documentation sections, and medication, lab, and
displaying, recording, ordering, editing, variance, procedure ordering or discontinuation.7
and statistics. Clinical pathways can be set up in a Clinical pathway integration into HIT also has
variety of modes, whether they are within the physi- limitations; health care providers will need to adapt
cal EMR itself or viewed as paper documentation8; to a new workflow and come to a unified decision
paper documentation is commonly less successful about large variances in their practice. Equipment,
and may serve as a distractor or introduce variance including computers and scanners, must be more
in electronic documentation. Clinical pathways can readily available for nurses and rounding teams.
have multiple layers of functionality based upon the Compliance with the new system can be increased
program used and developer, allowing analysis of when clinical pathways are embedded into rou-
patient outcomes in terms of the individual patient tine work practices and rounding discussions and
and/or target population as a whole. Options include staff have been fully educated on the application.9
418 Volume 51, May 2016
Director’s Forum
Pharmacy directors should work with senior leader- ischarge for Medicare beneficiaries undergoing hip
d
ship and the informatics department and their clini- or knee replacement. Leaders should remain vigilant
cians to identify opportunities for clinical pathways when this standard expands. The CJR stresses the
to assist with frontline supply chain control, opera- need for quality and efficiency improvement through
tional workflow, and improved patient outcomes. multimodal efforts: preoperative risk mitigation
strategy, assessment of standard complication rates,
CLINICAL AND ECONOMIC IMPACT FOR HEALTH acute care throughput, supply chain management,
SYSTEMS causal analysis and mitigation of readmission rates,
Measuring the outcomes of the use of clinical post-acute care care planning and coordination, as
pathways is an important yet challenging process. well as patient engagement and satisfaction.13 Some
During the early years, most research was associated of these indicators have established performance
with the studying the most efficient ways to imple- requirements, and quality indicators will continue to
ment a clinical pathway process.10 With the imple- evolve over time. Electronic clinical pathways with
mentation of electronic clinical pathways, clinical multireporting functionality will allow hospital lead-
outcomes data are more readily accessible. Husini ers to more efficiently assess patient outcomes and
and colleagues surveyed hospitals in 4 states and identify areas for improvement within the pathway.
found that patients who received total knee replace-
ments in institutions with clinical pathways had a PHARMACY LEADERS AND CLINICAL PATHWAY
0.5-day shorter length of stay (LOS) than patients in DEVELOPMENT PROCESS
institutions who did not.11 They also determined that The clinical pathway team determines the goals of
there were 32% fewer adverse events for patients on management for each clinical pathway. The team must
clinical pathways. Norton and colleagues demon- be diverse and inclusive. Members should include phy-
strated a decrease in pediatric asthma patient hospi- sicians, pharmacists, nurses, nurse practitioners, phys-
tal admissions (13.5% vs 27.5%) when patients were ical and occupational therapists, speech therapists,
on a clinical pathway.12 By utilizing a paper clinical case managers, social workers, laboratory members,
pathway, life-saving medications were adminis- and others depending on the type of pathway.4 Phar-
tered more often to patients who required it and in macy directors place themselves within these teams
a shorter amount of time. A recent study completed or identify competent clinical pharmacists to review
by Katzan and colleagues compared the inpatient guidelines and ensure efficacy and safety of therapies
mortality and LOS for patients with ischemic stroke and procedures. It is important that individuals from
before and after implementation of a clinical path- the informatics department be included to ensure the
way.10 A decrease in hospital mortality rate (7.2% clinical pathway is successful alignment of clinical and
pre vs 6.6% post; p = .003) and LOS (6.3 pre vs 6.2 operational consideration upon implementation.
post days; p = .047) was observed for ischemic stroke For pharmacy leaders, evaluation of outcomes is
patients on the clinical pathway.10 Physicians also critically important. They must determine the vari-
noted easier documentation and EMR review post ance, the intervention, or outcome that did not occur
implementation. as predicted. Variances may include LOS, complica-
The reimbursement landscape continues to tion rates, mortality rates, or financial outcomes. The
change to alternative payment models. Demands for selection of an outcome depends on what is best for
higher quality of care place increased financial risk the assessment of the institution’s clinical pathway.
on the provider and the institution. With this change Analyzing variances can be a time intensive process;
in financial accountability, providers need to provide thus when a new clinical pathway is created, results
integrated care models across the continuum of care should be reviewed in standard intervals to ensure
to enhance safer and more efficient care. Starting continued control of process variance and to identify
in January 2016, a new initiative under CMS titled new process improvement opportunities. Identifica-
Comprehensive Care for Joint Replacement Model tion of key variances and successful countermeasures
(CJR) offers an opportunity for electronic clini- may not only improve the outcomes of the patients,
cal pathways to ensure patient success and positive but may also improve staff satisfaction.4
financial return for hospitals.13 The model mandated Pharmacists play a specific role in the develop-
movement of hospitals in 67 selected geographic ment, implementation, and assessment of the clinical
areas into an bundled payment model spanning from pathway. Table 2 describes the roles and activities
3 days prior to admission through 90 days after pharmacists can contribute.
Hospital Pharmacy 419
Director’s Forum
Table 2. Pharmacy role in clinical pathways
Role Activities
Medication therapy management Medication selection; review of high-risk medications
Medication assistance Identify need; assist in obtaining medication during transitions of care
Patient and family educator Educate family and patient on medication changes, side effects,
expected outcomes
Medical staff educator Educate staff on medication place in therapy, duplications, optimal
timing, drug interactions; assist in creation of educational materials
Revise and establish policies and protocols Review current policies in place and recommend amendment based
upon changes in evidence-based medicine or to reflect clinical pathway
management
Research and evaluate outcomes Complete medication use evaluations; create reports and present to
leadership
Resistance to Adopting Clinical Pathways REFERENCES
Understanding the potential of a clinical 1. Davis K, Stremikis K, Squires D, Schoen C. Mirror, mirror
pathway also comes with recognizing the limita- on the wall: How the performance of the U.S. healthcare system
tions and resistance to the growth of clinical path- compares internationally. 2014 Update. The Commonwealth Fund.
ways. The pathway strives for standardization to June 2014. http://www.commonwealthfund.org/~/media/files/
publications/fund-report/2014/jun/1755_davis_mirror_mir-
improve patient outcomes and create institution
ror_2014.pdf. Accessed March 23, 2016.
efficiency. Opponents fear that this standardiza-
tion is in conflict with the goal of personalized or 2. Better care, smarter spending, healthier people: Improving
our health care delivery system. September 29, 2015. https://
precision medicine and creates “cookbook” medi-
www.cms.gov/Newsroom/MediaReleaseDatabase/Fact-
cine, threatening the autonomy of physicians.4 sheets/2015-Fact-sheets-items/2015-09-29-2.html.
Conversely, clinical pathways allow abandonment
3. Cutler DM. Payment reform is about to become a reality.
or discontinuation of the pathway if patients no
JAMA. 2015;313(16):1606-1607.
longer meet requirements. Institutions can build
flexibility into their clinical pathways to ensure 4. Dobesh PP, Bosso J, Wortman S, et al; ACCP Task Force
on Critical Pathways. Critical pathways: The role of phar-
that enough patients within a specific population macy today and tomorrow. Pharmacotherapy. 2006;26(9):
will fit within the pathway framework. Clinical 1358-1368.
pathways are evidence-based road maps that assist
5. Schuld J, Schäfer T, Nickel S, Jacob P, Schilling MK, Rich-
institutions in reducing variation in care and in ter S. Impact of IT-supported clinical pathways on medical
promoting best practice and providing better out- staff satisfaction. A prospective longitudinal cohort study. Int
comes for patients. J Med Inform. 2011;80(3):151-156.
6. Petitta A. Assessing the value of pharmacists’ health-
CONCLUSION system wide services: Clinical pathways and treatment guide-
Pharmacy directors can serve as integral role in lines. Pharmacotherapy. 2000;20(10 Pt 2):327S-332S.
promoting a clinical pathway development team. 7. Department of Health and Human Services, Center for
These pathways, along with HIT, have evolved to Medicare & Medicaid Services. Medicare and Medicaid Pro-
ensure successful care management within insti- grams; Electronic Health Record Incentive Program; Final
tutions. Hospitals can achieve better clinical and Rule. Federal Register. July 2010. Accessed March 21, 2016.
financial outcomes by utilizing an effective clinical 8. Wakamiya S, Yamauchi K. What are the standard func-
pathway that impacts a high risk, high dollar, or tions of the electronic clinical pathways? Int J Med Inform.
high volume medical or surgical condition. Phar- 2009;78(8):543-550.
macy directors can utilize their skills in this endeavor 9. Lenz R, Blaser R, Beyer M, et al. IT support for clinical path-
and engage clinical pharmacists as members of ways–lessons learned. Int J Med Inform. 2007;76(3):397-402.
the clinical pathway development team to ensure 10. Katzan IL, Fan Y, Speck M, et al. Electronic stroke care
medications are utilized appropriately to provide
path: Integrated approach to stroke care. Circ Cardiovasc
patient-centered care. Qual Outcomes. 2015;8(6 suppl 3):S179-189.
420 Volume 51, May 2016
Director’s Forum
11. Husini M, Losina E, Fossel A, Solomon D, Mahomed children with asthma: A prospective study. Arch Dis Child.
N, Katz J. Decreasing medical complications for total knee 2007;92(1):60-66.
arthroplasty: Effect of critical pathways on outcomes. BMC
13. Centers for Medicare & Medicaid Services. Comprehen-
Musculoskelet Disord. 2010;11:160.
sive care for joint replacement mode. https://innovation.cms.
12. Norton SP, Pusic MV, Taha F, Heathcote S, Carleton BC. gov/initiatives/cjr. Accessed February 12, 2016.
Effect of a clinical pathway on the hospitalization rates of
Hospital Pharmacy 421
View publication stats
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5795)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- PCW Applicant's Information SheetDocument2 pagesPCW Applicant's Information SheetCielo Belen SandroNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- AIT - PPO List As at September 2022 2Document9 pagesAIT - PPO List As at September 2022 2Guilherme Ventura100% (1)
- Case Scenario 1: Making Decision Based Upon The Situation (Paternalism and Utilitarianism)Document2 pagesCase Scenario 1: Making Decision Based Upon The Situation (Paternalism and Utilitarianism)Heart BeatingNo ratings yet
- Sushrut Dental Clinic: Dr. Bhagyashree Ramesh Khedkar BDS (Reg No. A-45644)Document1 pageSushrut Dental Clinic: Dr. Bhagyashree Ramesh Khedkar BDS (Reg No. A-45644)Ganesh ganiNo ratings yet
- Is Oet Accepted in Usa - Google SearchDocument1 pageIs Oet Accepted in Usa - Google SearchJune Mark Reyes AlferezNo ratings yet
- Informatics and Nursing Sensitive Quality Indicators: Name Institution Date CourseDocument5 pagesInformatics and Nursing Sensitive Quality Indicators: Name Institution Date CourseKevin SangNo ratings yet
- Curriculum Vitae For Mrs Alita Gloria MpingaDocument9 pagesCurriculum Vitae For Mrs Alita Gloria Mpingaalita ngomaneNo ratings yet
- Payslip For March 2023 - TORM ARAWA (Closed Payroll) : Torm A/S Torm A/SDocument1 pagePayslip For March 2023 - TORM ARAWA (Closed Payroll) : Torm A/S Torm A/SRodelio TomasNo ratings yet
- DHA ExamDocument7 pagesDHA ExamMaraj Raees khan Mohd MarajNo ratings yet
- Cost Effectiveness in Medical EducationDocument43 pagesCost Effectiveness in Medical EducationMarco OliveiraNo ratings yet
- University of The Philippines Manila College of MedicineDocument3 pagesUniversity of The Philippines Manila College of MedicineDhian MorishitaNo ratings yet
- List of Approved Schools With Admission QuotaDocument21 pagesList of Approved Schools With Admission QuotaAdegboye AdedayoNo ratings yet
- Bill Cum Receipt - Ms Humki Devi .Document1 pageBill Cum Receipt - Ms Humki Devi .Rahul SsdotraNo ratings yet
- Phc-Ii Final Exams-2021Document5 pagesPhc-Ii Final Exams-2021Galakpai KolubahNo ratings yet
- The 'S of CSW BillingDocument2 pagesThe 'S of CSW Billingmamatha mamtaNo ratings yet
- UntitledDocument133 pagesUntitledMalou Bautista-EscanerNo ratings yet
- Date Performed Patient's Name Procedure Performed OR Nurse On Duty Supervised byDocument2 pagesDate Performed Patient's Name Procedure Performed OR Nurse On Duty Supervised byjames pasionNo ratings yet
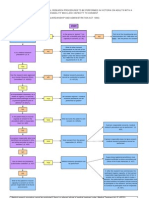
- Approval Process For Medical Research FlowchartDocument1 pageApproval Process For Medical Research FlowchartabcdcattigerNo ratings yet
- Chn-Health-Related Activities in The CommunityDocument3 pagesChn-Health-Related Activities in The CommunityBSN 1-N CASTRO, RicciNo ratings yet
- MedicaidDocument2 pagesMedicaidgeorge josephNo ratings yet
- The Role of Primary Health Care in NigeriaDocument6 pagesThe Role of Primary Health Care in NigeriaGreat OdineNo ratings yet
- OPD Action PlanDocument6 pagesOPD Action PlanTAHIR NURINo ratings yet
- Delegate List: Amanda-Jane ErneDocument20 pagesDelegate List: Amanda-Jane ErneDebjani DuttaNo ratings yet
- Minimum Wage Board 2013 Publishes GazetteDocument3 pagesMinimum Wage Board 2013 Publishes GazetteMahiulhabibNo ratings yet
- NHS FPX 6008 Assessment 2 Needs Analysis For ChangeDocument7 pagesNHS FPX 6008 Assessment 2 Needs Analysis For Changefarwaamjad771No ratings yet
- Saudi Family NetworkDocument232 pagesSaudi Family NetworkIbrahim Ansari 2218073No ratings yet
- Questionnaire - 7853582Document1 pageQuestionnaire - 7853582SMLD Nursing SchoolNo ratings yet
- IELTS Listening Practice Test 5: Section 1Document9 pagesIELTS Listening Practice Test 5: Section 1HoaiNhiNguyenNo ratings yet
- Pharmacy Exam OdishaDocument1 pagePharmacy Exam Odishasimpurock001No ratings yet
- Role Play Helping With Rehabilitation - Group 4 - 2aDocument12 pagesRole Play Helping With Rehabilitation - Group 4 - 2aAbang GotenNo ratings yet