Professional Documents
Culture Documents
Good Physician Communication
Uploaded by
Patrick Darmawan TaslimOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Good Physician Communication
Uploaded by
Patrick Darmawan TaslimCopyright:
Available Formats
PERS PE C T IV E A Good Physician — On Complacency and Communication
A Good Physician — On Complacency and Communication
A Good Physician — On Complacency and Communication
Michelle M. Kittleson, M.D., Ph.D.
I n the fall of 1997, my medical
school roommate lent me her
copy of Anne Fadiman’s The Spirit
for updates and never went back
myself.
After a few months, the pa-
recite the names and dosages of
his medications by heart. His fa-
ther appeared relieved to no lon-
Catches You and You Fall Down.1 I tient received the magic call. He ger be our go-between, and I was
stayed awake for two nights, fas- sailed through transplantation ashamed because I had never
cinated and appalled by the mis- and was home within 10 days. bothered to learn more than the
understanding between the young I should have been proud, but an patient’s medical history.
Hmong patient’s family and He had had a myocardial
her American physicians. Tak- infarction in his early 40s,
ing the cautionary tale to which was complicated by
heart, I dutifully used the tri- ventricular septal rupture. Af-
angular seating arrangement ter surgery, he was left with
recommended for patient, in- an ischemic cardiomyopathy,
terpreter, and physician. Often and 2 years later, consider-
before the interpreter could ation of a transplant was
translate a response, I knew warranted. His condition was
whether the patient was con- stabilized with low-dose ino-
fused, unconvinced, or fright- trope support, and I planned
ened, and I delighted in the to discharge him to wait for a
power of this connection. heart transplant as an outpa-
But much can change in tient. But his insurance com-
two decades. I recently cared pany decided that though they
for a 45-year-old man for over a adage from William Osler nagged would approve transplantation,
month and never spoke to him. at me: “The good physician treats they would not approve a defi-
He was admitted with cardiogen- the disease; the great physician brillator. How could he go home
ic shock, stabilized, and listed treats the patient who has the with inotropic support but no
for heart transplantation. Every disease.” I knew I had missed defibrillator? Alternatively, how
morning, I rounded with my the mark. could he be listed as an outpa-
heart failure team. The patient, At the patient’s first visit to tient with a projected wait time
pulmonary artery catheter se- the heart transplant clinic after of months to years, yet remain in
cured to his neck, usually looked surgery, we had our first conver- the hospital?
up when we entered but then re- sation. I perched on the exam- He spent 2 weeks in limbo,
turned his attention immediate- room stool, one point of a trian- and every day I explained to the
ly to his ever-present phone. gle with the patient and the father his son’s uncertain future.
His father was the other con- American Sign Language (ASL) I described my attempts to corner
stant in the room. Every morn- interpreter, and introduced my- the insurance company’s medical
ing, as I spoke to his father, I self. As the interpreter’s hands director across time zones and
glanced at my patient. He would fluttered like birds, I was equally his seemingly conscious efforts
offer a half-hearted smile, but I charmed and embarrassed. to duck my calls. I offered the
never knew how much he under- My patient had a bright and option of a wearable defibrilla-
stood or what he was thinking. ready smile. He joked about his tor, and when the insurance com-
I sometimes asked the cardiology low pain tolerance but still tried pany also declined to pay for that,
fellow to circle back after rounds to avoid pain medications. He was I described our (also unsuccess-
to see whether the patient had excited because he could climb a ful) attempts to finagle a free
any questions, but I never asked flight of stairs. He was proud to device.
1798 n engl j med 381;19 nejm.org November 7, 2019
PE R S PE C T IV E A Good Physician — On Complacency and Communication
The patient’s body ultimately (for me) inertia. I was relieved to on the radar of his new life. He
made the decision for us. His cre- avoid explaining the same frus- was also resigned, explaining that
atinine level, the canary-in-the- trating medical quandary twice he had stared at his phone be-
coal-mine of organ perfusion, each morning. I fell into a com- cause trying to follow spoken
worsened, and he required high- placency born of pragmatism conversation was too frustrating.
er doses of inotropic support that and confidence in my abilities: After the third visit, I emphati-
justified listing him as an inpa- I knew I was providing the best cally signed “You’re awesome,”
tient. The uncertainty about how medical care, so I ignored the realizing a few months too late
to safely usher him to transplan- importance of direct communi- that nuances of tone and style
tation was resolved. Throughout cation. could be conveyed without a voice.
it all, his father was calm, while In the two decades since I fin- I never returned my roommate’s
my patient’s face, lit only by the ished medical school, medical di- copy of The Spirit Catches You and
glow of his phone, remained in- lemmas have ceased to keep me You Fall Down, and Fadiman’s
scrutable. Whenever I care for a up at night; there is rarely a situ- words now offer an ironic re-
patient in the hospital awaiting a ation I have not encountered al- minder and reproach: “Every ill-
transplant, I always ask, “Is there ready. But after that clinic visit, ness is not a set of pathologies
anything we can do to make your I did lose sleep. How had my pa- but a personal story.”1 My patient
life easier?” But I never asked him. tient felt, being ignored each had a happy ending and he has
Why had I settled for being morning? How frustrated was he, forgiven me, but that is beside
just a good physician? Half the a grown man, made to rely on the point. It is harder to forgive
problem was logistics: scheduling his father to understand his own myself. I suspect I will always
a daily real-life ASL interpreter, care? And what if his condition feel a prickle of guilt and embar-
available in the 2-hour window had worsened, warranting dis- rassment when I see him, and
allotted for teaching rounds, cussions of mechanical circula- that small sting will remind me
seemed impossible. The other half tory support or hospice? I had of something I will not forget
was the absurdity of a video inter- neglected to gain the trust that again: diseases may become rou-
preter: between the fuzzy screen, is essential for guiding patients tine with experience, but patients
the static-filled audio, and the through difficult decisions. When must not.
time delay, any conversation would presented with the unique chal- Disclosure forms provided by the author
have left us more confused and lenge of caring for a deaf patient, are available at NEJM.org.
frustrated than when we started. I took the convenient way out,
In retrospect, I should have every day, for a month. I’d set a From the Department of Cardiology, Smidt
Heart Institute, Cedars-Sinai Medical Cen-
used his father as interpreter in- poor example for my team, I’d ter, Los Angeles.
stead of messenger. But on my failed to comfort a patient in
first day, neither the patient nor need, and I’d missed out on the 1. Fadiman A. The spirit catches you and
his father requested that I speak joy of that relationship. you fall down:a Hmong child, her American
doctors, and the collision of two cultures.
directly with the patient, and af- On his second clinic visit, I New York:Farrar, Straus and Giroux, 1997.
ter the second and third days worked up the courage to apolo-
passed with the same calm ac- gize. He was nonplussed yet gra- DOI: 10.1056/NEJMp1907319
ceptance, we fell into an easy cious, my negligence but a blip Copyright © 2019 Massachusetts Medical Society.
A Good Physician — On Complacency and Communication
n engl j med 381;19 nejm.org November 7, 2019 1799
You might also like
- Hypnosis in The Emergency Department BIERMANDocument5 pagesHypnosis in The Emergency Department BIERMANAyoub LilouNo ratings yet
- The Lost Art of Dying: Reviving Forgotten WisdomFrom EverandThe Lost Art of Dying: Reviving Forgotten WisdomRating: 4 out of 5 stars4/5 (9)
- Wounded HealerDocument2 pagesWounded HealerNuka Vardidze100% (2)
- Neurology: Timothy E. Welty, Pharm.D., FCCP, BCPSDocument68 pagesNeurology: Timothy E. Welty, Pharm.D., FCCP, BCPSAlmaha AlfakhriNo ratings yet
- Sacks, Oliver - 'The Lost Virtues of The Asylum'Document3 pagesSacks, Oliver - 'The Lost Virtues of The Asylum'DylanOSullivan100% (1)
- Care at The Time of DeathDocument11 pagesCare at The Time of DeathmultiusosvariadosNo ratings yet
- Essiac: T (Ature, S: CaivcerDocument7 pagesEssiac: T (Ature, S: CaivcerSerene LakeNo ratings yet
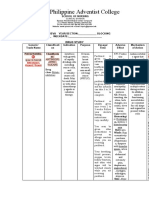
- "A Beautiful Mind": Clinical-in-Charge: Mrs. Aissa R. CarlitDocument51 pages"A Beautiful Mind": Clinical-in-Charge: Mrs. Aissa R. CarlitYejiNo ratings yet
- Nursing Care Plan Endometrial CancerDocument2 pagesNursing Care Plan Endometrial Cancerderic87% (15)
- Ten Traits of Great Physicians - 230228 - 085304Document6 pagesTen Traits of Great Physicians - 230228 - 085304lakshminivas PingaliNo ratings yet
- ARTÍCULOSDocument308 pagesARTÍCULOSDavid OlveraNo ratings yet
- Atbaseline NejmDocument2 pagesAtbaseline NejmSandeep SasidharanNo ratings yet
- Jama Kahn 2020 Po 200029Document2 pagesJama Kahn 2020 Po 200029laax_siuyenNo ratings yet
- Ethical Issues in The Management of Geriatric Cardiac PatientsDocument3 pagesEthical Issues in The Management of Geriatric Cardiac PatientsOana Nicole StoicanNo ratings yet
- Perspective: New England Journal MedicineDocument3 pagesPerspective: New England Journal MedicineLina MariaNo ratings yet
- On The Cover: PTSD and Our VetsDocument1 pageOn The Cover: PTSD and Our VetsRyan Drake RomeroNo ratings yet
- Hughes 1990 Inside MadnessDocument3 pagesHughes 1990 Inside Madnessgiamma87triNo ratings yet
- Preskorn 1980Document2 pagesPreskorn 1980Dhira AmaraNo ratings yet
- Enhancing Case Detection of Selected Inherited Disorders Through Expanded Newborn Screening in The PhilippinesDocument7 pagesEnhancing Case Detection of Selected Inherited Disorders Through Expanded Newborn Screening in The PhilippinesDerekBryanNo ratings yet
- Competencies in Palliative Care For Cardiology FellowsDocument4 pagesCompetencies in Palliative Care For Cardiology Fellowsandrey prawiroNo ratings yet
- Fuera de La Camisa de FuerzaDocument3 pagesFuera de La Camisa de FuerzaSamanta CadenasNo ratings yet
- Medchirrev76788 0206Document2 pagesMedchirrev76788 0206danny b.No ratings yet
- Bedell 04 Words That HarmDocument4 pagesBedell 04 Words That HarmR.L. BandaNo ratings yet
- Perspective: New England Journal MedicineDocument3 pagesPerspective: New England Journal MedicineSuwandi ChangNo ratings yet
- Deficient Knowledge - NCPDocument2 pagesDeficient Knowledge - NCPEmmeline Dycangchon-GarmaNo ratings yet
- Board Desember 2015 Fix Answer - BALIDocument67 pagesBoard Desember 2015 Fix Answer - BALIrahageng wida kusuma100% (1)
- Jama Halloran 2022 Po 220013 1651681368.46199Document2 pagesJama Halloran 2022 Po 220013 1651681368.46199JNo ratings yet
- Taggedh1Ten Traits of Great Physicians: TaggedendreviewDocument5 pagesTaggedh1Ten Traits of Great Physicians: TaggedendreviewJuan Carlos LazoNo ratings yet
- Paradox of HopeDocument2 pagesParadox of HopeRafael TerceiroNo ratings yet
- Case Study - Reversal of Brain Tumours With Nutritional ProtocolDocument3 pagesCase Study - Reversal of Brain Tumours With Nutritional ProtocolThanh NguyNo ratings yet
- Clinical Case Discussion: Electroconvulsive Therapy For The Treatment of Refractory ManiaDocument6 pagesClinical Case Discussion: Electroconvulsive Therapy For The Treatment of Refractory ManiaDewi NofiantiNo ratings yet
- Perspective: New England Journal MedicineDocument3 pagesPerspective: New England Journal MedicinedavideNo ratings yet
- Musings of A Modern Day Witch DoctorDocument4 pagesMusings of A Modern Day Witch DoctorRick Chavez, M.D.No ratings yet
- EstagiosmaniaDocument8 pagesEstagiosmaniaemiliaellenamNo ratings yet
- L. Warneke, M.D.: - Progression of Symptoms: Usually TheDocument5 pagesL. Warneke, M.D.: - Progression of Symptoms: Usually TheShradha PatilNo ratings yet
- Tales From The Temporal Lobes: PerspectiveDocument3 pagesTales From The Temporal Lobes: PerspectiveDini CahyaNo ratings yet
- 57-Year-Old Woman With Covid-19 and DelusionsDocument9 pages57-Year-Old Woman With Covid-19 and DelusionsNazly ÁlvarezNo ratings yet
- CASE Study SampleDocument6 pagesCASE Study SampleMary Shane Aragon MoraldeNo ratings yet
- The Art of Medicine: Trial and ErrorDocument2 pagesThe Art of Medicine: Trial and ErrorMuhNo ratings yet
- Screen Shot 2021-02-27 at 14.52.53Document2 pagesScreen Shot 2021-02-27 at 14.52.53Agnes PoppyNo ratings yet
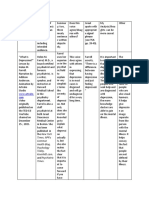
- Care Plan: Assessment DataDocument13 pagesCare Plan: Assessment Dataapi-520930030No ratings yet
- Beastly Beatitudes (1) - The Case of A Patient With Severe BorderlDocument9 pagesBeastly Beatitudes (1) - The Case of A Patient With Severe BorderlAimen MurtazaNo ratings yet
- Perspective: New England Journal MedicineDocument5 pagesPerspective: New England Journal MedicineTha Vila Le ColloNo ratings yet
- Counsellingthe Cancerpatient: Surgeon'Scounsel : George T. Pack, M.DDocument5 pagesCounsellingthe Cancerpatient: Surgeon'Scounsel : George T. Pack, M.DMigori ArtNo ratings yet
- HAITI - Earthquake 2010: A Lesson in ResilienceDocument4 pagesHAITI - Earthquake 2010: A Lesson in ResiliencemrpennantNo ratings yet
- Nejmp 1917203Document2 pagesNejmp 1917203Jorge RoblesNo ratings yet
- Central Philippine Adventist College: Assessment & Drug EffectsDocument3 pagesCentral Philippine Adventist College: Assessment & Drug EffectsAmy Rose AbuevaNo ratings yet
- Research ChartDocument4 pagesResearch Chartapi-419671795No ratings yet
- Burnout: of Centaurs, Poisoned Arrows, and Nautilus Shells: Brent W. Beasley, MD, MBADocument3 pagesBurnout: of Centaurs, Poisoned Arrows, and Nautilus Shells: Brent W. Beasley, MD, MBALeon BosnjakNo ratings yet
- Medical Tales From The Far Side of The World: Spirit Chicken-Or Lunch?Document40 pagesMedical Tales From The Far Side of The World: Spirit Chicken-Or Lunch?أيهم غزالNo ratings yet
- Secondary Mania in Older Adults: John O. Brooks III, PH.D., M.D. Jennifer C. Hoblyn, M.D., M.P.HDocument6 pagesSecondary Mania in Older Adults: John O. Brooks III, PH.D., M.D. Jennifer C. Hoblyn, M.D., M.P.HmaghfiraniNo ratings yet
- By Paul Pearsall, PHD Gary E. Schwartz, PHD Linda G. Russek, PHDDocument8 pagesBy Paul Pearsall, PHD Gary E. Schwartz, PHD Linda G. Russek, PHDJOSH USHERNo ratings yet
- Anxiety R:T Death ThreatDocument8 pagesAnxiety R:T Death ThreatAlfredo BaulaNo ratings yet
- NEJM Case Symptomatic Atrial Fibrillation With Associated AnxietyDocument8 pagesNEJM Case Symptomatic Atrial Fibrillation With Associated AnxietyLucía Flores FaríasNo ratings yet
- Brmedj03749 0035fDocument1 pageBrmedj03749 0035fSiti sarkia FatarubaNo ratings yet
- OP1005 Inside 79Document1 pageOP1005 Inside 79Marsha LecourNo ratings yet
- ANSWRSDocument4 pagesANSWRSkathleen mae corderoNo ratings yet
- Chest InjuryDocument17 pagesChest InjuryAira Dy PinedaNo ratings yet
- No Bad Blood-Surviving Severe Anemia Without Transfusion: A 51-Year-Old FemaleDocument2 pagesNo Bad Blood-Surviving Severe Anemia Without Transfusion: A 51-Year-Old Femaleclark coronaNo ratings yet