Professional Documents
Culture Documents
Anaphy - Cardiovascular System - Blood
Uploaded by
Aileen Demaguila0 ratings0% found this document useful (0 votes)
9 views3 pagesOriginal Title
ANAPHY - CARDIOVASCULAR SYSTEM - BLOOD
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
9 views3 pagesAnaphy - Cardiovascular System - Blood
Uploaded by
Aileen DemaguilaCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 3
ANATOMY & PHYSIOLOGY
CHAPTER 19: CARDIOVASCULAR SYSTEM
• Antibodies – plasma proteins that are produced
ANATOMY OF THE BLOOD
during certain immune responses
BLOOD AND HOMEOSTASIS • Antigens (foreign substances) stimulate production of
• Blood contributes to homeostasis by transporting millions of different antibodies
oxygen, carbon dioxide, nutrients, and hormones to and • Antibody binds specifically to the antigen that stimulated
from your body’s cells. It also helps regulate body pH and its production and thus disables the invading antigen
temperature, and provides protection against disease
through Phagocytosis and the production of Antibodies FORMED ELEMENTS
FUNCTIONS AND PROPERTIES OF BLOOD • Includes three principal components: red blood cells,
CARDIOVASCULAR SYSTEM white blood cells, and platelets
• Cardio = Heart & Vascular = Blood or blood vessels • Red Blood Cell (RBC) – erythrocytes transports oxygen
• Consists of three interrelated components: Blood, heart, from the lungs to body cells and delivers carbon dioxide
and blood vessels from body cells to the lungs
• White Blood Cell (WBC) – leukocytes protect the body
HEMATOLOGY from invading pathogens and other foreign substances
• Branch of science concerned with the study of blood, • Types of WBCs: neutrophils, basophils, eosinophils,
blood-forming tissues, and the disorders associated with monocytes, and lymphocytes
them • Lymphocyte’s subdivisions: B cells, T cells, and neutral
killer (NK) cells
BLOOD • Platelets – fragments of cells that do not have a nucleus;
• Liquid connective tissue that consists of cells surrounded they release chemicals that promote blood clotting when
by a liquid extracellular matrix blood vessels are damaged
• Blood Plasma – suspends various cells and cell fragments • The percentage of total blood volume occupied by RBCs
• Blood transports oxygen from the lungs and nutrients is called Hematocrit
from the gastrointestinal tract, which diffuse from the • A significant drop in hematocrit indicates anemia; a
blood into the interstitial fluid and then into body cells lower-than-normal number pf RBCs
• Polycethemia when the percentage of RBCs is
INTERSTITIAL FLUID abnormally high, and hematocrit may be 65% or higher
• Fluid that bathes body cells and is constantly FORMATION OF BLOOD CELLS
renewed by the blood • Lymphocytes can live for years while most other blood
FUNCTIONS OF BLOOD cells live for hours, days, or weeks
1. TRANSPORTATION • The number of red blood cells and platelets remains
Blood transports oxygen, carbon dioxide, nutrients, rather steady while that of white blood cells varies
hormones, heat, and waste products depending on invading pathogens and other foreign
antigens
2. REGULATION
• The process of producing/developing blood cells is called
Blood regulates homeostasis of all body fluids, pH,
Hemopoiesis (hematopoiesis)
body temperature, and water content of cells
• Red Bone Marrow is a highly vascularized connective
3. PROTECTION tissue located in the microscopic spaces between
Blood protects against excessive loss by clotting and trabeculae of spongy bone tissue
uses white blood cells to protect against infection • About 0.05-0.1% of red bone marrow cells are called
pluripotent stem cells or hemocytoblasts and are
derived from mesenchyme
• In order to form blood cells, pluripotent stem cells in red
bone marrow produce stem cells: myeloid stem cells
and lymphoid stem cells
• During hemopoiesis, some of myeloid stem cells
differentiate into progenitor cells
RED BLOOD CELLS
• Red blood cells or erythrocytes contains the protein
COMPONENTS OF BLOOD hemoglobin that is used to carry oxygen to all cells and
BLOOD PLASMA to carry some carbon dioxide to the lungs
• When the formed elements are removed from blood, a • Each hemoglobin, molecule contains an iron ion which
straw-colored liquid is left allows each molecule to bind four oxygen molecule
1|CHAPTER 19: CARDIOVASCULAR SYST EM: THE BLOOD
ANATOMY & PHYSIOLOGY
CHAPTER 19: CARDIOVASCULAR SYSTEM
• Red blood cells have no nucleus or other organelles and • Platelets only survive in 5 to 9 days
are biconcave discs – this allows them to carry oxygen
STEM CELL TRANSPLANTS FROM BONE MARROW AND
more efficiently
CORD BLOOD
• Hemoglobin is involved in regulating blood flow and
blood pressure via release of nitric oxide (NO) – no • Bone marrow transplants are performed to replace
causes of vasodilation, which improves blood flow and cancerous red bone marrow with normal red bone
enhances oxygen delivery marrow – the donor’s marrow is usually collected from
• Red blood cells also contain carbonic anhydrase, which the iliac crest of the hip bone
catalyzes the conversion of carbon dioxide and water to • Stem cells collected and frozen from an umbilical cord
carbonic acid – Carbonic acid transports about 70% of after birth may also be used, and have advantages over
carbon dioxide in the plasma bone marrow transplants
• Red blood cells live for only about 120 days – dead cells HOMEOSTASIS
are removed from the circulation by the spleen and liver • Homeostasis is a sequence of responses that stops
• Breakdown products from the red blood cells are bleeding.
recycles and reused • When blood vessels are damaged or ruptured, the
• ERYTHROPIOESIS, the production of red blood cells, homeostatic response must be quick, localized to the
starts in the red bone marrow with a precursor cell called region of damage, and carefully controlled in order to be
proerythroblast effective
Erythropoietin, a hormone released by the kidneys in • Once the clot forms, it retracts (tightens) to pull the
response to hypoxia (lowered oxygen concentration) edges of the damaged vessel together – Vitamin K is
stimulates differentiation of hematopoietic stem cells needed for normal clot formation because it is used in
into erythrocytes the synthesis of 4 clotting factors
• Reticulocytes (immature red blood cells) enter the • Small, unwanted clots are usually dissolved by plasmin,
circulation and mature in 1 to 2 days an enzyme that is part of the fibrinolytic system
WHITE BLOOD CELLS Vascular Spasm
• White blood cells or leukocytes • When arteries or arterioles are damaged, the circularly
• In general, an elevation in the white blood count arranged smooth muscle in their walls contracts
indicates an infection or inflammation immediately
Platelet Plug Formation
• A low white blood cell count may develop due to several
Blood Clotting
causes
• Involves several clotting (coagulation) factors
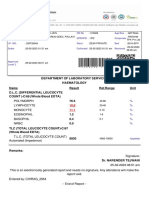
• A differential white blood cell count will help to
determine if a problem exists • Blood clotting can be activated in one of two ways:
Extrinsic Pathway and Intrinsic Pathway
• White blood cell’s proteins are called major
histocompatibility (MHC) antigens • Both of these pathways lead to the formation of
prothrombinase and, from there, the common
GRANULAR LEUKOCYTES pathway continues
• Neutrophil – as the cells age, the number of nuclear BLOOD GROUP AND BLOOD TYPES
lobes increases b/cause older neutrophils thus have Blood is characterized into different blood groups based on
several differently shaped are often called the presence or absence of glycoprotein and glycolipid
polymorphonuclear leukocytes (PMNs) antigens (agglutinogens) on the surface of red blood cells
• Eosinophil – the large, uniform sized granules are
eosinophilic – they stain red orange with acidic dyes. • There are 24 blood groups and more that 100 antigens
• Basophil – the round, variable sized granules are • Because these antigens are genetically controlled, blood
basophilic – they stain blue purple with basic dyes types vary among different populations
• Classification is based on antigens labeled A, B or AB,
AGRANULAR LEUKOCYTES with O being the absence of the antigens
• An additional antigen, Rh, is present in 85% of humans
• Lymphocyte
• Blood plasma usually contains antibodies (agglutinins)
• Monocyte
that react with A or B antigens
PLATELETS • An individual will not have agglutinins against his or her
• Megakaryocytes in red bone marrow splinter into 2000- own blood type
3000 fragments to create the platelets that contain many • Typing and cross-matching are performed to determine
vesicles but no nucleus a person’s blood type
• Platelets are use to clot the blood – under the influence • A drop of blood is mixed with an antiserum that will
of the hormone thrombopoietin, hemopoietic stem cells agglutinate blood cells that possess agglutinogens that
differentiate into platelets react with it
2|CHAPTER 19: CARDIOVASCULAR SYST EM: THE BLOOD
ANATOMY & PHYSIOLOGY
CHAPTER 19: CARDIOVASCULAR SYSTEM
HEMOLYTIC DISEASE OF THE NEWBORN
At birth, small amounts of fetal blood leak into the maternal
circulation
• If the baby is Rh+ and the mother is Rh-, she will develop
antibodies to the Rh factor
• During her next pregnancy with an Rh+ baby, when she
transfers antibodies to the fetus (a normal occurrence),
transferred anti Rh antibodies will attack some fetus’ red
blood cells causing agglutination and hemolysis
DISORDERS: HOMEOSTATIC IMBALANCES
• Sickle cell disease is a genetic anemia (oxygen-carrying
capacity of the blood is reduced)
• The red blood cells of individuals with this disease
contain hemoglobin-S (Hb-S), which causes red blood
cells to bend into a sickle shape when it gives up oxygen
to the interstitial fluid
3|CHAPTER 19: CARDIOVASCULAR SYST EM: THE BLOOD
You might also like
- PSG 712 Blood-1Document54 pagesPSG 712 Blood-1preciousNo ratings yet
- BloodDocument76 pagesBloodKerby Dela Fuente Alison100% (1)
- Fast Facts: Leukemia: From initial gene mutation to survivorship supportFrom EverandFast Facts: Leukemia: From initial gene mutation to survivorship supportNo ratings yet
- ANATOMY AND PHYSIOLOGY OF BLOODDocument11 pagesANATOMY AND PHYSIOLOGY OF BLOODArah Lyn ApiagNo ratings yet
- BLOODDocument12 pagesBLOODRinalyn BalderramaNo ratings yet
- Blood PPT NotesDocument7 pagesBlood PPT NotesArce JohnsonNo ratings yet
- Blood (Anaphy)Document8 pagesBlood (Anaphy)CORONEL, SOPHIANo ratings yet
- Blood: A Vital Transport SystemDocument33 pagesBlood: A Vital Transport SystemCORONEL, SOPHIANo ratings yet
- CVS BloodDocument39 pagesCVS BloodMohan GuptaNo ratings yet
- Blood Circulation OverviewDocument24 pagesBlood Circulation OverviewWenzy Razzie cruzNo ratings yet
- Hematologi 1Document57 pagesHematologi 1Till JannahNo ratings yet
- Blood: Raeesa Sattar Faculty of Allied Health SciencesDocument25 pagesBlood: Raeesa Sattar Faculty of Allied Health SciencesNAMRA RASHEEDNo ratings yet
- 1 BloodDocument77 pages1 BloodVisaNathan100% (1)
- Hematologic DisorderDocument7 pagesHematologic Disordermawel100% (2)
- The Circulatory System: Components of Blood and Lymph (Detail Study)Document11 pagesThe Circulatory System: Components of Blood and Lymph (Detail Study)Parardha DharNo ratings yet
- 1-Blood Composition and FunctionDocument43 pages1-Blood Composition and FunctionKaleem Mohammad100% (2)
- BLOOD Update-1Document56 pagesBLOOD Update-1ahmadfadi343No ratings yet
- The University of Zambia School of Medicine Department of Physiological SciencesDocument64 pagesThe University of Zambia School of Medicine Department of Physiological Sciencesblaze zimbaNo ratings yet
- University of Guyana Health Sciences FacultyDocument44 pagesUniversity of Guyana Health Sciences FacultySatrohan SurjnarineNo ratings yet
- Cardiovascular SystemDocument14 pagesCardiovascular SystemDionne EllaNo ratings yet
- Hematology Lecture 1 - Blood and Its Components - BackupDocument51 pagesHematology Lecture 1 - Blood and Its Components - BackupHaizickNo ratings yet
- Blood and Its ComponentsDocument22 pagesBlood and Its ComponentsSudhir Singh100% (1)
- Hema Mod 4Document17 pagesHema Mod 4Moon KillerNo ratings yet
- Blood Cells: By, Shobhana PandianDocument60 pagesBlood Cells: By, Shobhana PandianhrishikeshanandNo ratings yet
- Hematology Lab Rotation-1Document31 pagesHematology Lab Rotation-1shanzayenzay9No ratings yet
- Chapter 4 Blood Coagulation and Coagulation Disorders _32f6d4d0c67589df3863ad91f445f357Document27 pagesChapter 4 Blood Coagulation and Coagulation Disorders _32f6d4d0c67589df3863ad91f445f357daisysintszwaiNo ratings yet
- Understanding the Composition and Functions of BloodDocument30 pagesUnderstanding the Composition and Functions of BloodPriyanka RameshNo ratings yet
- Human Anatomy and Physiology II: Topic: Anatomy of The Blood Sub Topic: Introduction To Blood and Its CompositionsDocument28 pagesHuman Anatomy and Physiology II: Topic: Anatomy of The Blood Sub Topic: Introduction To Blood and Its Compositionsngong ngong ametNo ratings yet
- Blood and Its FunctionsDocument47 pagesBlood and Its FunctionsMatende husseinNo ratings yet
- 9 Anatomy 2021 BloodDocument32 pages9 Anatomy 2021 BloodDanica DaniotNo ratings yet
- Cardiovascular Physiology 4Document75 pagesCardiovascular Physiology 4maxmus4No ratings yet
- NATSCI Pre Final Lec Notes BLOODDocument5 pagesNATSCI Pre Final Lec Notes BLOODNIKKANo ratings yet
- Blood ReviewDocument13 pagesBlood ReviewDeleted AccountNo ratings yet
- Blood Lecture SlidesDocument144 pagesBlood Lecture Slidesgrace ncubeNo ratings yet
- Heamatology Chapter 1Document38 pagesHeamatology Chapter 1Taima'a AlamaratNo ratings yet
- Histology of Blood CellsDocument80 pagesHistology of Blood CellsKamal AhmedNo ratings yet
- Blood: Group 1Document25 pagesBlood: Group 1Arian May MarcosNo ratings yet
- Hematology: - The Science Dealing With The FormationDocument104 pagesHematology: - The Science Dealing With The FormationYamSomandarNo ratings yet
- Darah Dan HematopoisisDocument81 pagesDarah Dan HematopoisisSheldy PrawibowoNo ratings yet
- BloodDocument49 pagesBloodDale TelgenhoffNo ratings yet
- BIOL 221 - Blood Functions and CompositionDocument32 pagesBIOL 221 - Blood Functions and CompositionAleandra LettNo ratings yet
- Blood, Coagulation of Blood & Bleeding Disorders 12 - 7 - 19Document62 pagesBlood, Coagulation of Blood & Bleeding Disorders 12 - 7 - 19AntarleenaNo ratings yet
- Blood Part 1Document35 pagesBlood Part 1Keziah TampusNo ratings yet
- Blood Anatomy and Physiology: Functions, Components, FormationDocument28 pagesBlood Anatomy and Physiology: Functions, Components, FormationPORTRAIT OF A NURSENo ratings yet
- Cardiovascular System - BloodDocument67 pagesCardiovascular System - BloodCla NuvalNo ratings yet
- Introduction to Blood Composition and HaemopoiesisDocument119 pagesIntroduction to Blood Composition and HaemopoiesisShamsuddeen UsmanNo ratings yet
- Characteristics and Functions of Blood ComponentsDocument51 pagesCharacteristics and Functions of Blood ComponentssamayaNo ratings yet
- Blood and Lymph Nodes: P. Manyau School of Pharmacy University of ZimbabweDocument18 pagesBlood and Lymph Nodes: P. Manyau School of Pharmacy University of Zimbabwebrian mgabiNo ratings yet
- Cardiovascular System - BloodDocument8 pagesCardiovascular System - BloodVernice LopezNo ratings yet
- 112lec HematologyDocument11 pages112lec HematologyChelsea Faith SarandiNo ratings yet
- Blood Physiology 2022Document116 pagesBlood Physiology 2022Gurmessa FekaduNo ratings yet
- Circulatory SystemDocument74 pagesCirculatory SystemMICHAEL AFIADENYONo ratings yet
- CLS 224 Lecture 4: Understanding Blood CompositionDocument54 pagesCLS 224 Lecture 4: Understanding Blood CompositionalfaristurkiNo ratings yet
- Hematology 2020Document63 pagesHematology 2020odiodi57No ratings yet
- Introduction To HematologyDocument61 pagesIntroduction To HematologyThis is PonyNo ratings yet
- Blood Vascular SystemDocument29 pagesBlood Vascular Systemgarimaupadhyay20002No ratings yet
- Anatomy and Physiology of BLOOD: Preet KaurDocument37 pagesAnatomy and Physiology of BLOOD: Preet KaurPreet KaurNo ratings yet
- Lecture Blood CellsDocument15 pagesLecture Blood Cellsdp6cv2m5wnNo ratings yet
- Anaphy - Tissue Level of Organization P1Document3 pagesAnaphy - Tissue Level of Organization P1Aileen DemaguilaNo ratings yet
- Anaphy - Introduction To The Human BodyDocument7 pagesAnaphy - Introduction To The Human BodyAileen DemaguilaNo ratings yet
- Anaphy - Tissue - Part 1Document5 pagesAnaphy - Tissue - Part 1Aileen DemaguilaNo ratings yet
- Anaphy - Chapter 23 - Respiratory SystemDocument9 pagesAnaphy - Chapter 23 - Respiratory SystemAileen DemaguilaNo ratings yet
- Shaka Patka Grade 11 ShortnotesDocument5 pagesShaka Patka Grade 11 ShortnotesDilshan DhanushaNo ratings yet
- Induce Pluripotent Stem Cell Methods, Development and Advancesn 02 FebDocument11 pagesInduce Pluripotent Stem Cell Methods, Development and Advancesn 02 FebGJESRNo ratings yet
- Stem Cells Notes - BIO SUmmDocument3 pagesStem Cells Notes - BIO SUmmMuffaddal MustafaNo ratings yet
- Unit 1-Lecture 3 Intro To Immuno-Acquired ImmunityDocument65 pagesUnit 1-Lecture 3 Intro To Immuno-Acquired ImmunityBecky GoodwinNo ratings yet
- BIO 202 Blood Lab 22S PDFDocument2 pagesBIO 202 Blood Lab 22S PDFTraci GardnerNo ratings yet
- Cells and Cellular Activities of The Immune System: Lymphocytes and Plasma CellsDocument5 pagesCells and Cellular Activities of The Immune System: Lymphocytes and Plasma Cellsrenato renatoNo ratings yet
- Test Bank For Clinical Hematology and Fundamentals of Hemostasis 5th Edition HarmeningDocument6 pagesTest Bank For Clinical Hematology and Fundamentals of Hemostasis 5th Edition HarmeningWilbur Penny100% (29)
- Ijhoscr: ABO Blood Grouping Mismatch in Hematopoietic Stem Cell Transplantation and Clinical GuidesDocument7 pagesIjhoscr: ABO Blood Grouping Mismatch in Hematopoietic Stem Cell Transplantation and Clinical GuidesMohana ReddyNo ratings yet
- Acute Leukemias: Atu Level 300 Practical SectionDocument35 pagesAcute Leukemias: Atu Level 300 Practical SectionAbdul Raouf KhalidNo ratings yet
- Module 3 Lesson 11 Gene TherapyDocument10 pagesModule 3 Lesson 11 Gene TherapyJannie Rose MarquezNo ratings yet
- Hematopoiesis: Pluri - Several) or Hemocytoblasts. These Cells Have The Capacity To Develop Into Many Different Types ofDocument12 pagesHematopoiesis: Pluri - Several) or Hemocytoblasts. These Cells Have The Capacity To Develop Into Many Different Types ofRajender ArutlaNo ratings yet
- Activation and Maturation of T and B LymphocytesDocument21 pagesActivation and Maturation of T and B LymphocytesIka BakarNo ratings yet
- Stem Cells in Regenerative MedicineDocument28 pagesStem Cells in Regenerative MedicineSumanta Kar100% (1)
- Blood Examination ReportDocument6 pagesBlood Examination Reportapi-3745021No ratings yet
- C19 2 Hemopoiesis Eythropoiesis LeukopoiesisDocument11 pagesC19 2 Hemopoiesis Eythropoiesis Leukopoiesisnurul azisyah auraNo ratings yet
- Embryonic Stem Cells: Review ArticleDocument6 pagesEmbryonic Stem Cells: Review ArticleFabLab EIUNo ratings yet
- Position Paper On Stem Cell Therapy 131008Document2 pagesPosition Paper On Stem Cell Therapy 131008Autism Society PhilippinesNo ratings yet
- Neuroglia: Cells That Support NeuronsDocument15 pagesNeuroglia: Cells That Support NeuronsnadimNo ratings yet
- Hematopoiesis Part 1Document11 pagesHematopoiesis Part 1Gab PeaceNo ratings yet
- Hemotology ReviewDocument61 pagesHemotology ReviewSukma EffendyNo ratings yet
- ErythropoiesisDocument3 pagesErythropoiesisSubhasish BarikNo ratings yet
- 2 HaemopoiesisDocument50 pages2 HaemopoiesisWasana Mendis100% (2)
- Childrens FBC Reference Ranges PDFDocument1 pageChildrens FBC Reference Ranges PDFmfaddhilNo ratings yet
- EDEXCEL- BIOLOGY- IAL Stem Cells: Natural Reservoir and Unique AbilitiesDocument12 pagesEDEXCEL- BIOLOGY- IAL Stem Cells: Natural Reservoir and Unique AbilitiesSwarnapaliliyanageNo ratings yet
- Significance of Blood Cell ProductionDocument3 pagesSignificance of Blood Cell ProductionKervy Jay AgraviadorNo ratings yet
- Stem Cell Research ControversyDocument3 pagesStem Cell Research ControversyCarlosNo ratings yet
- Rgci Care Reports1677339022895Document1 pageRgci Care Reports1677339022895Akshay ChaudhryNo ratings yet
- Macrophages: Development and Tissue Specialization: Chen Varol, Alexander Mildner, and Steffen JungDocument35 pagesMacrophages: Development and Tissue Specialization: Chen Varol, Alexander Mildner, and Steffen JungGustavo VilcapazaNo ratings yet
- CBC ReportDocument1 pageCBC ReportKamal DeepNo ratings yet
- Haemopoiesis: Written By: Fayzah Alshammari Date: 20/02/2021Document5 pagesHaemopoiesis: Written By: Fayzah Alshammari Date: 20/02/2021fayzah alshammariNo ratings yet
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 3.5 out of 5 stars3.5/5 (2)
- The Ancestor's Tale: A Pilgrimage to the Dawn of EvolutionFrom EverandThe Ancestor's Tale: A Pilgrimage to the Dawn of EvolutionRating: 4 out of 5 stars4/5 (811)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- Tales from Both Sides of the Brain: A Life in NeuroscienceFrom EverandTales from Both Sides of the Brain: A Life in NeuroscienceRating: 3 out of 5 stars3/5 (18)
- All That Remains: A Renowned Forensic Scientist on Death, Mortality, and Solving CrimesFrom EverandAll That Remains: A Renowned Forensic Scientist on Death, Mortality, and Solving CrimesRating: 4.5 out of 5 stars4.5/5 (397)
- Crypt: Life, Death and Disease in the Middle Ages and BeyondFrom EverandCrypt: Life, Death and Disease in the Middle Ages and BeyondRating: 4 out of 5 stars4/5 (3)
- The Consciousness Instinct: Unraveling the Mystery of How the Brain Makes the MindFrom EverandThe Consciousness Instinct: Unraveling the Mystery of How the Brain Makes the MindRating: 4.5 out of 5 stars4.5/5 (93)
- Good Without God: What a Billion Nonreligious People Do BelieveFrom EverandGood Without God: What a Billion Nonreligious People Do BelieveRating: 4 out of 5 stars4/5 (66)
- This Is Your Brain On Parasites: How Tiny Creatures Manipulate Our Behavior and Shape SocietyFrom EverandThis Is Your Brain On Parasites: How Tiny Creatures Manipulate Our Behavior and Shape SocietyRating: 3.5 out of 5 stars3.5/5 (31)
- 10% Human: How Your Body's Microbes Hold the Key to Health and HappinessFrom Everand10% Human: How Your Body's Microbes Hold the Key to Health and HappinessRating: 4 out of 5 stars4/5 (33)
- A Brief History of Intelligence: Evolution, AI, and the Five Breakthroughs That Made Our BrainsFrom EverandA Brief History of Intelligence: Evolution, AI, and the Five Breakthroughs That Made Our BrainsRating: 4.5 out of 5 stars4.5/5 (4)
- Who's in Charge?: Free Will and the Science of the BrainFrom EverandWho's in Charge?: Free Will and the Science of the BrainRating: 4 out of 5 stars4/5 (65)
- The Other Side of Normal: How Biology Is Providing the Clues to Unlock the Secrets of Normal and Abnormal BehaviorFrom EverandThe Other Side of Normal: How Biology Is Providing the Clues to Unlock the Secrets of Normal and Abnormal BehaviorNo ratings yet
- The Lives of Bees: The Untold Story of the Honey Bee in the WildFrom EverandThe Lives of Bees: The Untold Story of the Honey Bee in the WildRating: 4.5 out of 5 stars4.5/5 (44)
- Undeniable: How Biology Confirms Our Intuition That Life Is DesignedFrom EverandUndeniable: How Biology Confirms Our Intuition That Life Is DesignedRating: 4 out of 5 stars4/5 (11)
- Human: The Science Behind What Makes Your Brain UniqueFrom EverandHuman: The Science Behind What Makes Your Brain UniqueRating: 3.5 out of 5 stars3.5/5 (38)
- Wayfinding: The Science and Mystery of How Humans Navigate the WorldFrom EverandWayfinding: The Science and Mystery of How Humans Navigate the WorldRating: 4.5 out of 5 stars4.5/5 (18)
- The Second Brain: A Groundbreaking New Understanding of Nervous Disorders of the Stomach and IntestineFrom EverandThe Second Brain: A Groundbreaking New Understanding of Nervous Disorders of the Stomach and IntestineRating: 4 out of 5 stars4/5 (17)
- Superlative: The Biology of ExtremesFrom EverandSuperlative: The Biology of ExtremesRating: 4.5 out of 5 stars4.5/5 (51)
- Buddha's Brain: The Practical Neuroscience of Happiness, Love & WisdomFrom EverandBuddha's Brain: The Practical Neuroscience of Happiness, Love & WisdomRating: 4 out of 5 stars4/5 (215)
- Eels: An Exploration, from New Zealand to the Sargasso, of the World's Most Mysterious FishFrom EverandEels: An Exploration, from New Zealand to the Sargasso, of the World's Most Mysterious FishRating: 4 out of 5 stars4/5 (30)
- The Molecule of More: How a Single Chemical in Your Brain Drives Love, Sex, and Creativity--and Will Determine the Fate of the Human RaceFrom EverandThe Molecule of More: How a Single Chemical in Your Brain Drives Love, Sex, and Creativity--and Will Determine the Fate of the Human RaceRating: 4.5 out of 5 stars4.5/5 (515)
- Human Errors: A Panorama of Our Glitches, from Pointless Bones to Broken GenesFrom EverandHuman Errors: A Panorama of Our Glitches, from Pointless Bones to Broken GenesRating: 3.5 out of 5 stars3.5/5 (56)
- Darwin's Dangerous Idea: Evolution and the Meaning of LifeFrom EverandDarwin's Dangerous Idea: Evolution and the Meaning of LifeRating: 4 out of 5 stars4/5 (523)
- The Mind & The Brain: Neuroplasticity and the Power of Mental ForceFrom EverandThe Mind & The Brain: Neuroplasticity and the Power of Mental ForceNo ratings yet
- The Dragons of Eden: Speculations on the Evolution of Human IntelligenceFrom EverandThe Dragons of Eden: Speculations on the Evolution of Human IntelligenceRating: 4 out of 5 stars4/5 (632)