Professional Documents
Culture Documents
Empyema in Children: A 25-Year Study
Uploaded by
Diego AndradeOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Empyema in Children: A 25-Year Study
Uploaded by
Diego AndradeCopyright:
Available Formats
16. Konstan MW, Schluchter MD, Xue W, Davis PB. Clinical use of ibuprofen is al.
al. Infant care patterns at epidemiologic study of cystic fibrosis sites that achieve superior
associated with slower FEV1decline in children with cystic fibrosis. Am J Respir Crit childhood lung function. Pediatrics 2007;119:e531-7.
Care Med 2007;176:1084-9. 21. Zemel BS, Jawad AF, FitzSimmons S, Stallings VA. Longitudinal relationship
17. Merkus PJFM, Tiddens HAWM, de Jonste JC. Annual lung function changes in among growth, nutritional status, and pulmonary function in children with cystic
young patients with chronic lung disease. Eur Respir J 2002;19:886-91. fibrosis: analysis of the Cystic Fibrosis Foundation National CF Patient Registry.
18. Fuchs HJ, Borowitz DS, Christiansen DH, Morris E, Nash M, Ramsey B, et al. J Pediatr 2000;137:374-80.
Effect of aerosolized recombinant human DNase on exacerbations of respiratory symp- 22. Konstan MW, Butler SM, Wohl ME, Stoddard M, Matousek R, Wagener J, et
toms and on pulmonary function in patients with cystic fibrosis. N Engl J Med al. Growth and nutritional indexes in early life predict pulmonary function in cystic
1994;331:637-42. fibrosis. J Pediatr 2003;142:624-30.
19. Quan JM, Tiddens HAWM, Sy JP, McKenzie S, Montgomery M, Robinson P, 23. Ratjen F, Paul K, van Koningsbruggen S, Breitenstein S, Rietschel E, Niko-
et al. A two-year randomized, placebo-controlled trial of dornase alpha in young patients laizik W. DNA concentrations in BAL fluid of cystic fibrosis patients with early
with cystic fibrosis with mild lung function abnormalities. J Pediatr 2001;139:813-20. lung disease: influence of treatment with dornase alpha. Pediatr Pulmonol 2005;
20. Padman R, McColley SA, Miller DP, Konstan M, Morgan W, Schechter M, et 39:1-4.
50 Years Ago in The Journal of Pediatrics
EMPYEMA IN CHILDREN: A 25-YEAR STUDY
Lionakis BL, Gray SW, Skandalakis JE, and Hopkins WA. J Pediatr 1958;53:719-25
“. . .this study covers the period of practical extinction of empyema” and “1947 should mark the essential closing of
this chapter of the history of thoracic surgery” are 2 ill-fated prophesies made by these authors based on their observation
that the incidence of childhood empyema had fallen dramatically after the introduction of antibiotics in the late 1940s.
Contrary to their predictions, however, the worldwide incidence of childhood empyema continues to increase, the reason
for which remains unknown. The most common causative organisms remain pneumococcus and staphylococcus;
however, there is evidence that pneumococcal serotype 1 is becoming more dominant. This shift in serotype has been
speculated to be due to the introduction of a 7-valent pneumococcal vaccine that does not cover serotype 1; however, to
date an association, but not a causation, has been shown.
Despite the increase in cases, the outcomes for children with empyema have improved greatly since the time of this
report. In the authors’ observation period from 1932 to 1957, the average length of hospital stay was 7 weeks, and death
occurred in approximately 50% of children under age 2 years. Today, death rarely occurs, and the average hospital stay
is less than 1 week after intervention.
Although it has been recognized since Hippocrates’ time that drainage of empyema is essential, the best method to
do so remains controversial. Rib section, the treatment of choice 50 years ago, has been replaced by primary video-assisted
thoracoscopic surgery (VATS), and chest drainage has been refined by the use of small percutaneous drains with
instillation of fibrinolytics, which is cheaper than and as effective as VATS. The past 5 decades also have seen the
development of imaging techniques to aid diagnosis. Although ultrasound is a useful tool, some children may be receiving
unnecessary exposure to radiation from routine computed tomography scans, which may not affect management.1 We
need to be mindful not to do unnecessary harm as we strive to perfect the prevention and treatment of empyema in
children over the next 50 years.
Adam Jaffé, MD, FRCP, FRCPCH, FRACP
Respiratory Department
Sydney Children’s Hospital, Randwick
School of Women’s and Children’s Health
University of New South Wales
Sydney, Australia
10.1016/j.jpeds.2008.05.019
REFERENCE
1. Jaffé A, Calder AD, Owens CM, Stanojevic S, Sonnappa S. The role of routine computed tomography in paediatric pleural empyema. Thorax 2008;63:897-902.
Improvements in Lung Function Outcomes in Children with Cystic Fibrosis are Associated with Better
Nutrition, Fewer Chronic Pseudomonas aeruginosa Infections, and Dornase Alfa Use 757
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (589)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (842)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5806)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Pulmonary Function Test (PFT)Document24 pagesPulmonary Function Test (PFT)hm3398No ratings yet
- Quill Love LettersDocument8 pagesQuill Love LettersDiego AndradeNo ratings yet
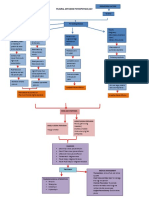
- Pleurl Effusion Pathophysiology DiagramDocument2 pagesPleurl Effusion Pathophysiology DiagramAkiraMamo67% (3)
- FU - The - Freeform - Universal - RPG - (Classic - Rules) 2Document24 pagesFU - The - Freeform - Universal - RPG - (Classic - Rules) 2Diego AndradeNo ratings yet
- Micro Chapbook RPG: Room Chart (D6)Document2 pagesMicro Chapbook RPG: Room Chart (D6)Diego Andrade0% (1)
- Pulmonary DisordersDocument53 pagesPulmonary DisordersAhmad Makhlouf100% (1)
- RESPI QuestionDocument14 pagesRESPI QuestionCarmela Marie Eriguel CuetoNo ratings yet
- Scientific Book Jicccim 2018Document171 pagesScientific Book Jicccim 2018ngwinda90No ratings yet
- Pocket Fantasy RPG Ver. 3.6Document4 pagesPocket Fantasy RPG Ver. 3.6Diego AndradeNo ratings yet
- Mechanical VentilatorDocument9 pagesMechanical VentilatorAnusha Verghese100% (2)
- Modes of Mechanical VentilationDocument34 pagesModes of Mechanical Ventilationsbraj86100% (1)
- NCP Bronchila Ashma Dra.Document3 pagesNCP Bronchila Ashma Dra.ЯicaЯdo BautistaNo ratings yet
- LAMU Term 1B IMED Written ExamDocument12 pagesLAMU Term 1B IMED Written ExamSecret AgentNo ratings yet
- A Lonely Knave Solo Roleplay (Knave)Document2 pagesA Lonely Knave Solo Roleplay (Knave)Diego Andrade0% (1)
- Modes of Mechanical VentilationDocument4 pagesModes of Mechanical Ventilationsgod34100% (1)
- Non Invasive Ventilation and Weaning PDFDocument748 pagesNon Invasive Ventilation and Weaning PDFAny Córdova100% (2)
- Tecme Neumovent Technical Manual 94Document94 pagesTecme Neumovent Technical Manual 94Marina Garza GaliciaNo ratings yet
- BTS Guidelines For The Management of Pleural Infection in ChildrenDocument21 pagesBTS Guidelines For The Management of Pleural Infection in ChildrenDiego AndradeNo ratings yet
- Randomised Trial of Intrapleural Urokinase in The Treatment of Childhood EmpyemaDocument5 pagesRandomised Trial of Intrapleural Urokinase in The Treatment of Childhood EmpyemaDiego AndradeNo ratings yet
- 839 1 FullDocument3 pages839 1 FullDiego AndradeNo ratings yet
- Thoracic EmpyemaDocument3 pagesThoracic EmpyemaDiego AndradeNo ratings yet
- RCCM 200601-027ocDocument7 pagesRCCM 200601-027ocDiego AndradeNo ratings yet
- Camargos 2015Document6 pagesCamargos 2015Diego AndradeNo ratings yet
- CRGE Conjectural Roleplaying GM EmulatorDocument32 pagesCRGE Conjectural Roleplaying GM EmulatorDiego AndradeNo ratings yet
- Dodi Daftar PustakaDocument3 pagesDodi Daftar PustakaToni PinemNo ratings yet
- Persistent Cough in ChildrenDocument6 pagesPersistent Cough in Childrenyujin KimNo ratings yet
- HemothoraxDocument27 pagesHemothoraxShreyasi AnkushNo ratings yet
- BiPAP A40 - BrochureDocument2 pagesBiPAP A40 - BrochureDonny AndiNo ratings yet
- # Davidson - Review # Respiratory - MedicineDocument18 pages# Davidson - Review # Respiratory - Medicineemtiaz zamanNo ratings yet
- Pocket Guide For Asthma Management and PreventionDocument33 pagesPocket Guide For Asthma Management and PreventionRiaNo ratings yet
- Catalog - Intra Catheters - SemnatDocument4 pagesCatalog - Intra Catheters - SemnatFatima VessaliusNo ratings yet
- Reflection Respiratory SystemDocument4 pagesReflection Respiratory SystemAin Sufiza0% (1)
- Thoracic Emergency Trauma QuestionnairesDocument7 pagesThoracic Emergency Trauma QuestionnairesMeliza BancolitaNo ratings yet
- Assessment of Patients With Respiratory Disorders Basic Respiratory Care ModalitiesDocument15 pagesAssessment of Patients With Respiratory Disorders Basic Respiratory Care ModalitiesJhosita Flora LarocoNo ratings yet
- History and Physical Exam For COPDDocument10 pagesHistory and Physical Exam For COPDCathy GuerreroNo ratings yet
- JSS MoUDocument88 pagesJSS MoUchetanhiremathNo ratings yet
- Normal and Abnormal Findings of Thorax and LungsDocument3 pagesNormal and Abnormal Findings of Thorax and LungsOtherin Ojibwa TejanoNo ratings yet
- E60a4042 ME2512 Medicine 1 Respiratory 2023-2024Document39 pagesE60a4042 ME2512 Medicine 1 Respiratory 2023-2024Iona PatrickNo ratings yet
- Jarvis Chapter 18 Study GuideDocument5 pagesJarvis Chapter 18 Study GuideEmily Cheng100% (2)
- No. TGL Materi: Rehabilitation of Cardiovascular and Respiratory DisorderDocument6 pagesNo. TGL Materi: Rehabilitation of Cardiovascular and Respiratory DisorderFatimah AzzahraNo ratings yet
- Weaning ProtocolDocument6 pagesWeaning ProtocolerwanNo ratings yet
- 2006 129 1344-1348 Christopher E. Brightling: Clinical Applications of Induced SputumDocument7 pages2006 129 1344-1348 Christopher E. Brightling: Clinical Applications of Induced Sputumjoal510No ratings yet