Professional Documents
Culture Documents
Reative Arthiritis
Uploaded by
Theepan ThuraiOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Reative Arthiritis
Uploaded by
Theepan ThuraiCopyright:
Available Formats
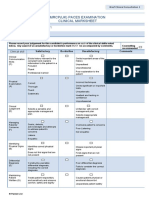
Integrated clinical assessment
Reactive arthritis:
Follow-up Questions/Answers
What do you think the most likely diagnosis is here, and can you offer me a
differential diagnosis as well?
o This gentleman has presented with an acute history of oligoarthritis that has been
predated by a diarrhoeal illness about 3–4 weeks ago.
o My top differential would be reactive arthritis.
o My differential would include a first presentation of rheumatoid arthritis.
o Given the family history of psoriatic disease, I would consider psoriatic arthritis.
o I feel that, given the examination, a septic knee or an episode of gout is less likely.
You mentioned diarrhoeal illness as a potential trigger for his reactive arthritis. Can
you tell me about the potential triggers for reactive arthritis?
o Diarrhoeal illnesses principally caused by Salmonella, is particularly common, as
are streptococcal infections.
o Sexually transmitted infections can be a precipitant to reactive arthritis,
particularly Chlamydia.
What about a gonococcal infection?
o Whilst Gonococcus can cause reactive arthritis, it is more likely to cause a septic
joint.
How would you investigate this gentleman?
o I would not expect X-rays to be of any help.
o I would do some blood tests.
o I would like to check the inflammatory markers to get an idea of the active
inflammation ongoing, so a CRP (C-reactive protein) and ESR (erythrocyte
sedimentation rate).
o I would do U&Es (urea and electrolytes) to make sure the kidney function is okay
given his use of NSAIDs (non-steroidal anti-inflammatory drugs).
o I would also do a rheumatoid factor, an anti-CCP *(cyclic citrullinated peptides)
antibody, and if they were borderline, we could consider looking at HLA (human
leukocyte antigen)-B27.
Did you think he had an effusion?
o I did not, but if there was an effusion present, then I would like to do an
aspiration, send that for culture and sensitivity, cytology and for crystals.
Integrated clinical assessment
Reactive arthritis:
Key Words and Phrases
This gentleman has a classic history of reactive arthritis. He has symptoms of
asymmetrical oligoarthritis preceded by a diarrhoeal illness.
However, you do have to consider other differential diagnoses, such as first presentation
of rheumatoid arthritis, other spondyloarthritidies, such as psoriatic arthropathy if he
had a personal or family history of psoriasis, and you could consider gout, meniscal lesion
or septic arthritis, but I agree with the candidate with this history and examination that
these are all less likely.
Good candidates will know that Gonococcus causes septic arthritis (and so the patients
typically present with purulent urethral discharge and concurrent joint pain and also
fever) while Chlamydia, Salmonella, Campylobacter and Streptococcus are the classic
causes of reactive arthritis – the joint symptoms usually post-date the initial infection by
some weeks (typically 4–8).
Candidates should examine the patient, specifically examining the knees and ankles to
assess for the presence of a hot/swollen joint, plus any effusion. The joint examination
should include inspection, palpation, and an assessment of range of movement.
Appropriate investigations would include Blood tests for urate, CRP, ESR, full blood
count (FBC), rheumatoid factor (RF) and CCP antibody.
You could consider HLA-B27 testing, it’s positive in up to 50% patients with reactive
arthritis.
If there are any suspicions of a sexually transmitted infection, then urine and genital
swab testing for Gonnorhoea and Chlamydia in particular would be indicated.
There are no specific findings on plain X-rays in reactive arthritis that can confirm the
diagnosis, so these would not be helpful.
If there was any effusion, then joint aspiration would be appropriate for cell count,
crystals, culture, and sensitivity.
Rheumatology referral is appropriate here.
Acute management of reactive arthritis would be with simple analgesics, NSAIDs unless
contraindicated. The condition is usually self-limiting. Most patients will not require
steroids or disease-modifying antirheumatic agents to control inflammation or to
prevent erosive joint changes.
You might also like
- Diagnosis and Differential Diagnosis of Rheumatoid Arthritis - UpToDateDocument25 pagesDiagnosis and Differential Diagnosis of Rheumatoid Arthritis - UpToDatehochanh199xNo ratings yet
- Case 17: 4-Year-Old Refusing To Walk-EmilyDocument6 pagesCase 17: 4-Year-Old Refusing To Walk-Emilyarlene-bury-fiol-6287No ratings yet
- Diagnosis and Differential Diagnosis of Rheumatoid ArthritisDocument12 pagesDiagnosis and Differential Diagnosis of Rheumatoid ArthritisAnghelo Aldair Velásquez CarrilloNo ratings yet
- Diagnosis and Differential Diagnosis of Rheumatoid Arthritis - UpToDateDocument20 pagesDiagnosis and Differential Diagnosis of Rheumatoid Arthritis - UpToDateDannyGutierrezNo ratings yet
- Differential Polyarthritis: Diagnosis ofDocument5 pagesDifferential Polyarthritis: Diagnosis ofKaran ChauhanNo ratings yet
- MedicalDocument29 pagesMedicalZia Ur RehmanNo ratings yet
- Rheumatoid ArthritisDocument37 pagesRheumatoid ArthritisPetit NacarioNo ratings yet
- Case Study OrthoDocument21 pagesCase Study Orthojoshua_santiago_5No ratings yet
- Station 5 Case 10 Extra Case InformationDocument3 pagesStation 5 Case 10 Extra Case InformationSarah CrausNo ratings yet
- Artritis ReumatoideDocument73 pagesArtritis ReumatoideCastillo DiegoNo ratings yet
- All Topics Are Updated As New Evidence Becomes Available and Our Peer Review Process Is CompleteDocument88 pagesAll Topics Are Updated As New Evidence Becomes Available and Our Peer Review Process Is CompleteJaime BarraganNo ratings yet
- Musculoskeletal SystemDocument25 pagesMusculoskeletal Systembessan alfqeatNo ratings yet
- ASCP Recall (June 21 2017)Document8 pagesASCP Recall (June 21 2017)Joanna Carel Lopez100% (3)
- The Sexual Instinct and its Morbid Manifestations from the Standpoint of Jurisprudence & PsychiatryFrom EverandThe Sexual Instinct and its Morbid Manifestations from the Standpoint of Jurisprudence & PsychiatryNo ratings yet
- Inflamed Aorta, (Aortitis) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandInflamed Aorta, (Aortitis) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Psoriatic ArthritisDocument14 pagesPsoriatic ArthritisRoberto López Mata100% (2)
- Spond Ylo ArthritisDocument58 pagesSpond Ylo ArthritisirsyadilfikriNo ratings yet
- Reactive ArthritisDocument4 pagesReactive ArthritisMisael ClintonNo ratings yet
- Rheumatology Year 4Document90 pagesRheumatology Year 4Abdalla SamatarNo ratings yet
- Diagnosis of Reactive ArhtritisDocument8 pagesDiagnosis of Reactive ArhtritisJayricDepalobosNo ratings yet
- Case Psoriatic ArthritisDocument5 pagesCase Psoriatic ArthritisAyuNo ratings yet
- ArthritisDocument14 pagesArthritisSherley Meiske Pakasi100% (1)
- Annals of The 680: Rheumatic DiseasesDocument2 pagesAnnals of The 680: Rheumatic DiseasesAnonymous hvOuCjNo ratings yet
- Dr. Paul McCutcheon Expert Report (Plaintiff)Document35 pagesDr. Paul McCutcheon Expert Report (Plaintiff)Osiris-KhentamentiuNo ratings yet
- What Tests Are Used To Diagnose Rheumatoid Arthritis?Document7 pagesWhat Tests Are Used To Diagnose Rheumatoid Arthritis?sadia younasNo ratings yet
- Mesothelioma 20.3.19Document33 pagesMesothelioma 20.3.19PradeepNo ratings yet
- Arthritis FulltextDocument6 pagesArthritis FulltextAnuj Gupta100% (1)
- Differential Diagnosis of Polyarticular ArthritisDocument7 pagesDifferential Diagnosis of Polyarticular ArthritismedicabrujaNo ratings yet
- Yusuf Brilliant M.Jauharil WafiDocument29 pagesYusuf Brilliant M.Jauharil WafiJauharil Wafi MuhammadNo ratings yet
- Human Atheroma: With Particular Reference to Endocrine Aspects of ÆtiologyFrom EverandHuman Atheroma: With Particular Reference to Endocrine Aspects of ÆtiologyNo ratings yet
- CASE SCENARIO - SerologyDocument4 pagesCASE SCENARIO - Serologysanjeev09122005No ratings yet
- Acutely Swollen JointDocument7 pagesAcutely Swollen JointHossein VakiliNo ratings yet
- Self Assessment in Musculoskeletal Pathology X-raysFrom EverandSelf Assessment in Musculoskeletal Pathology X-raysRating: 5 out of 5 stars5/5 (2)
- Yousaf Ali (Auth.) - Self Assessment Questions in Rheumatology-Humana Press (2009)Document147 pagesYousaf Ali (Auth.) - Self Assessment Questions in Rheumatology-Humana Press (2009)Amr AmalNo ratings yet
- Approach Patient With ArthritisDocument45 pagesApproach Patient With ArthritisAli TawbeNo ratings yet
- Approach To Rheum PTDocument44 pagesApproach To Rheum PTjiojimalaniNo ratings yet
- Reiter's Syndromeنور حيدر قيس الرابع مسائيDocument8 pagesReiter's Syndromeنور حيدر قيس الرابع مسائيصفا رياض محمد /مسائيNo ratings yet
- Approach To ARTHRITISDocument46 pagesApproach To ARTHRITISkalfNo ratings yet
- Attending Osteomyelitis ModuleDocument9 pagesAttending Osteomyelitis ModuleMrLarry DolorNo ratings yet
- Rheumatoid FactorDocument21 pagesRheumatoid FactorMuhamad Wirawan AdityoNo ratings yet
- Orthopedic Infections: Anil Arora, Anil AgarwalDocument22 pagesOrthopedic Infections: Anil Arora, Anil AgarwalaninnaNo ratings yet
- Case Presentations in Arterial DiseaseFrom EverandCase Presentations in Arterial DiseaseRating: 5 out of 5 stars5/5 (1)
- Diagnostic Principles and Applications: Avoiding Medical Errors, Passing Board Exams, and Providing Informed Patient CareFrom EverandDiagnostic Principles and Applications: Avoiding Medical Errors, Passing Board Exams, and Providing Informed Patient CareNo ratings yet
- A Case of Male Sle: An Unusual PresentationDocument4 pagesA Case of Male Sle: An Unusual PresentationIJAR JOURNALNo ratings yet
- Rheumatoid ArthritisDocument6 pagesRheumatoid ArthritisJayson Cruz100% (2)
- Care 2008 38-60Document30 pagesCare 2008 38-60yateema4ever100% (2)
- Avoiding Common Errors in The Emergency Department-801-1002Document200 pagesAvoiding Common Errors in The Emergency Department-801-1002Hernando CastrillónNo ratings yet
- Acute Renal FailureDocument8 pagesAcute Renal FailureLuis Hernán Guerrero LoaizaNo ratings yet
- Laboratory Investigations in RheumatologyDocument43 pagesLaboratory Investigations in RheumatologyBahaa Shaaban100% (1)
- Case Study 3 - Knee PainDocument12 pagesCase Study 3 - Knee PainElizabeth Ho100% (9)
- GS 201-250Document19 pagesGS 201-250Sara Abdul RahmanNo ratings yet
- Definition of Osteomyelitis in Children: Acute Inflammation of The Bone Bacterial PathogenDocument6 pagesDefinition of Osteomyelitis in Children: Acute Inflammation of The Bone Bacterial PathogenEdrian IndraNo ratings yet
- Raynaud’s Phenomenon: A Guide to Pathogenesis and TreatmentFrom EverandRaynaud’s Phenomenon: A Guide to Pathogenesis and TreatmentFredrick M. WigleyNo ratings yet
- A 31-Year-Old Man With Chronic Cough and HemoptysisDocument6 pagesA 31-Year-Old Man With Chronic Cough and HemoptysiscocomilkNo ratings yet
- Surgery - Orthopedic Surgery and NeurosurgeryDocument88 pagesSurgery - Orthopedic Surgery and Neurosurgeryteena6506763No ratings yet
- What Is Henoch-Schönlein Purpura (HSP) ?Document4 pagesWhat Is Henoch-Schönlein Purpura (HSP) ?Ila Daril FadhilahNo ratings yet
- Mark Sheet Station 05Document2 pagesMark Sheet Station 05Theepan ThuraiNo ratings yet
- Mark Sheet Station 02Document2 pagesMark Sheet Station 02Theepan ThuraiNo ratings yet
- Demititis HerpitiformisDocument2 pagesDemititis HerpitiformisTheepan ThuraiNo ratings yet
- 9635 34327 1 PBDocument2 pages9635 34327 1 PBTheepan ThuraiNo ratings yet
- GLP1 Analogue TreatmentDocument7 pagesGLP1 Analogue TreatmentTheepan ThuraiNo ratings yet
- GLP-1 Analog Dosing ChartDocument1 pageGLP-1 Analog Dosing ChartTheepan Thurai100% (1)
- Icd 10Document3 pagesIcd 10irmayantinur22No ratings yet
- Diagnosis Dan Terapi Ilmu Bedah RSUD Dr. Soetomo. Surabaya.2008Document2 pagesDiagnosis Dan Terapi Ilmu Bedah RSUD Dr. Soetomo. Surabaya.2008tafwidiqbalNo ratings yet
- Cross Sectional Purposive Sampling (Checklist) .: Keyword: Phlebitis, Intravenous Medicine Application, Aseptic TechniqueDocument10 pagesCross Sectional Purposive Sampling (Checklist) .: Keyword: Phlebitis, Intravenous Medicine Application, Aseptic TechniqueFebri NgestiutamaNo ratings yet
- 7985 - Jadwal GIS 1920Document12 pages7985 - Jadwal GIS 1920amelia rahayuNo ratings yet
- IBDDocument31 pagesIBDEdwardArielTadeaNo ratings yet
- Rheumatology SBIM Part 1Document5 pagesRheumatology SBIM Part 1Gousay AlkhazmariNo ratings yet
- 275 1057 1 PBDocument14 pages275 1057 1 PBLuckytyasNo ratings yet
- Daftar PustakaDocument2 pagesDaftar PustakarisdaauliaputriNo ratings yet
- ARTHRITISDocument12 pagesARTHRITISram krishna100% (1)
- Althazar Score: Grading of PancreatitisDocument1 pageAlthazar Score: Grading of PancreatitisJuan GomezNo ratings yet
- 1526931449Document123 pages1526931449Lika KipshidzeNo ratings yet
- Approach To Joint PainDocument44 pagesApproach To Joint PainKavya Anoop100% (1)
- Multiple Choice Questions Pediatric Rheumatology1Document13 pagesMultiple Choice Questions Pediatric Rheumatology1Riham Abu ZahirNo ratings yet
- Rheumatology Handout - c2fDocument1 pageRheumatology Handout - c2fapi-195799092No ratings yet
- BlepharitisDocument11 pagesBlepharitismohamadNo ratings yet
- Chronic Pancreatitis - AMBOSSDocument13 pagesChronic Pancreatitis - AMBOSSMdacNo ratings yet
- Diagnosa Ri Dan Kode Ina CBGDocument7 pagesDiagnosa Ri Dan Kode Ina CBGUjang YayaNo ratings yet
- Hepatitis in Children (Hep A, B, C)Document26 pagesHepatitis in Children (Hep A, B, C)sarNo ratings yet
- BlepharitisDocument11 pagesBlepharitismohamadNo ratings yet
- MaretDocument132 pagesMarettipanoesaNo ratings yet
- Trigger Finger: Dr. Aswedi Putra, SP - OT, FICS Universitas MalahayatiDocument9 pagesTrigger Finger: Dr. Aswedi Putra, SP - OT, FICS Universitas MalahayatiJessy WidiyantiNo ratings yet
- Pembimbing Diskusi Kasus Minor November 2020Document1 pagePembimbing Diskusi Kasus Minor November 2020Yosia ChristiNo ratings yet
- Juli 21Document15 pagesJuli 21Asam CemaraNo ratings yet
- Rheumatoid ArthritisDocument2 pagesRheumatoid ArthritisRiena Austine Leonor NarcillaNo ratings yet
- Checklist UKMPPD NovemberDocument6 pagesChecklist UKMPPD Novemberuci marley100% (1)
- Data Pasien Umum Poli Gigi Klinik Vita Medika: TGL NO. Nama No RM Diagnosa Terapi Tarif KetDocument4 pagesData Pasien Umum Poli Gigi Klinik Vita Medika: TGL NO. Nama No RM Diagnosa Terapi Tarif KetDiana PuspitasariNo ratings yet
- Jurnal PENGARUH KOMPRES SEREI HANGAT TERHADAP INTENSITAS NYERI ARTRITIS RHEUMATOID PADA LANJUT USIA (2020)Document8 pagesJurnal PENGARUH KOMPRES SEREI HANGAT TERHADAP INTENSITAS NYERI ARTRITIS RHEUMATOID PADA LANJUT USIA (2020)nauranazifa1No ratings yet
- Meningitis ??? Meningitis: Meningitis Jamur (Fungal Meningitis) - Disebabkan Oleh JamurDocument2 pagesMeningitis ??? Meningitis: Meningitis Jamur (Fungal Meningitis) - Disebabkan Oleh JamurHendraLiyusmanNo ratings yet
- NIS Dissertation TopicsDocument3 pagesNIS Dissertation TopicsMaha RajaNo ratings yet
- DermatitisDocument50 pagesDermatitisbosNo ratings yet