Professional Documents
Culture Documents
Drug Study 1
Uploaded by
Sarah SalvaOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Drug Study 1
Uploaded by
Sarah SalvaCopyright:
Available Formats
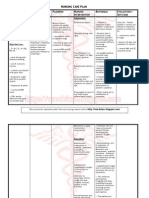
DRUG Classification: Antimetabolite
DOSAGE Acute lymphoblastic leukemia Adults and children: 3.3 mg/m2 P.O. or I.M. daily for 4 to 6 weeks, then 20 to 30 mg/m2 P.O. or I.M. weekly in two divided doses; given with corticosteroid. Alternatively, 2.5 mg/kg I.V. q 14 days. Meningeal leukemia Adult and children: 12 mg/m2 (maximum of 15 mg) intrathecally at intervals of 2 to 5 days, repeated until cerebrospinal fluid cell count is normal Burkitt's lymphoma Adults: In stages I and II, 10 to 25 mg P.O. daily for 4 to 8 days; in stage III, combined with other neoplastic drugs. Patients in all stages usually require several courses of therapy, with 7- to 10day rest periods between courses. Mycosis fungoides Adults: 2.5 to 10 mg/day P.O. or 50 mg I.M. q week or 25 mg I.M. twice weekly Osteosarcoma Adults: As part of adjunctive regimen with other antineoplastics, initially 12 g/m2 I.V. as 4-hour infusion, then 12 to 15 g/m2 I.V. in subsequent 4-hour infusions given at weeks 4, 5, 6, 7, 11, 12, 15, 16, 29, 30, 44, and 45 until peak blood level reaches 1,000 micromoles. Leucovorin rescue must start 24
PHARMACODYNA MICS
Adverse Reaction Administration Be aware that methotrexate is a highalert drug. Know that patient must be adequately hydrated before therapy and urine must be alkalized using sodium bicarbonate. Follow facility policy for handling, preparing, and administering carcinogenic, mutagenic, and teratogenic drugs. Be aware that oral administration is preferred. Give oral dose 1 hour before or 2 hours after meals. (Food decreases absorption of tablets and reduces peak blood level.) Reconstitute powder for injection with preservative-free solution, such as 5% dextrose solution or 0.9% sodium chloride injection. Reconstitute 20-mg and 50-mg vials to yield a concentration no greater than 25 mg/ml. Reconstitute 1g vial with 19.4 ml to yield a concentration of Contraindications Hypersensitivity to drug Psoriasis or rheumatoid arthritis in pregnant patients Breastfeeding Precautions Use cautiously in: severe myocardial, hepatic, or renal disease; decreased bone marrow reserve; active infection; hypotension; coma elderly patients patients with childbearing potential young children.
Route P.O. I.V. I.M. Peak 1-2 hr Immedi ate 0.5-1 hr
Interaction Drug-drug. Activated charcoal: decreased blood level of oral or I.V. methotrexate Folic acid derivatives: antagonism of methotrexate effects Fosphenytoin, phenytoin: decreased blood levels of these drugs Hepatotoxic drugs: increased risk of hepatotoxicity NSAIDs, phenylbutazone, probenecid, salicylates, sulfonamides: increased methotrexate toxicity Oral antibiotics: decreased methotrexate absorption Penicillin, sulfonamide: increased methotrexate blood level Procarbazine: increased nephrotoxicity Theophylline: increased theophylline level Vaccines: vaccine inefficacy Drug-diagnostic tests. Hemoglobin, platelets, red blood cells, white blood cells: decreased values Pregnancy tests: falsepositive result Protein-bound iodine, transaminases, uric acid: increased levels
Health Teaching Review dosing instructions carefully with patient to avoid toxicity. Tell patient with rheumatoid arthritis or psoriasis to take doses weekly. Advise patient to take oral doses 1 hour before or 2 hours after meals. Instruct patient to report diarrhea, abdominal pain, clay-colored or black tarry stools, fever, chills, sore throat, unusual bleeding or bruising, sores in or around mouth, cough or shortness of breath, yellowing of skin or eyes, dark or bloody urine, swelling of feet or legs, or joint pain. Tell patient to take temperature daily and to report fever or other signs or symptoms of infection. Instruct patient to drink 2 to 3 L of fluid each day. Advise male patients to use reliable contraception during and for at least 3 months after therapy. Advise female patients to use reliable contraception during and for one ovulatory cycle after therapy; also caution them not to breastfeed. Advise patient to avoid sun exposure and to use sunscreen and protective clothing (especially if he has psoriasis). Instruct patient to avoid alcohol. Tell patient he'll need to undergo blood tests during therapy. As appropriate, review all other significant and life-threatening adverse reactions and interactions, especially those related to the drugs, tests, foods, herbs, and behaviors
Generic: methotrexate sodium
Action Binds to dihydrofolate reductase, interfering with folic acid metabolism and inhibiting DNA synthesis and cellular replication
Pregnancy Classification: Pregnancy risk category X
Source: medicaldictionary
CNS: malaise, fatigue, drowsiness, dizziness, headache, aphasia, hemiparesis, demyelination, seizure s ,leukoencephalopath y , chemical arachnoiditis (with intrathecal use) EENT: blurred vision, pharyngitis GI: nausea, vomiting, stomatitis, hematemesis, melena, GI ulcers, enteritis, gingivitis, pharyngitis, anorexia,GI bleeding GU: hematuria, cystitis, infertility, menstrual dysfunction, defective spermatogenesis, abortion, tubular necrosis, severe nephropathy , renal failure Hematologic: anemia, l eukopenia, thrombocytopenia, severe bone marrow depression Hepatic: hepatotoxicity Metabolic: hyperurice mia, diabetes mellitus Musculoskeletal: joint pain, myalgia, osteonecrosis, osteoporosis (with
hours after methotrexate infusion begins; if patient can't tolerate oral leucovorin, dose must be given I.M. or I.V. on same schedule. Trophoblastic tumors (choriocarcinoma, hydatidiform mole) Adults: 15 to 30 mg P.O. or I.M. daily for 5 days. Repeat course three to five times as required, with rest periods of at least 1 week between courses, until toxic symptoms subside. Lymphosarcoma (stage III) Adults: 0.625 to 2.5 mg/kg/day P.O., I.M., or I.V. Psoriasis Adults: After test dose, 2.5 mg P.O. at 12-hour intervals for three doses weekly, to a maximum of 30 mg weekly. Alternatively, 10 to 25 mg P.O., I.M., or I.V. as a single weekly dose, to a maximum of 30 mg weekly; decrease dosage when adequate response occurs. Rheumatoid arthritis Adults: 7.5 mg P.O. weekly as a single dose or divided as 2.5 mg q 12 hours for three doses weekly. May gradually increase, if needed, up to 20 mg/week; decrease when adequate response occurs.
50 mg/ml. For high-dose I.V. infusion, dilute in 5% dextrose solution. Administer each 10 mg over 1 minute or by infusion over 30 minutes to 4 hours as directed. For intrathecal use, reconstitute immediately before administration, using preservative-free solution (such as 0.9% sodium chloride for injection), to a concentration of 1 mg/ml. For intrathecal or high-dose therapy, use preservative-free injection form. Avoid I.M. injections if platelet count is below 50,000/mm3. For osteosarcoma, make sure leucovorin rescue is used appropriately in patients receiving high methotrexate doses. Rescue usually starts 24 hours after methotrexate infusion begins.
long-term use in children) Respiratory: dry nonproductive cough, pneumonitis, pulmonary fibrosis, pulmonary interstitial infiltrates Skin: pruritus, rash, urticaria, alopecia, painful plaque erosions, photosensitivity Other: chills, fever, increased susceptibility to infection, septicemia, anaphylaxis , sudden death
Drug-food. Any food: delayed methotrexate absorption and decreased peak blood level Drug-herbs. Astragalus, echinacea, melatonin: interference with methotrexate-induced immunosuppression Drug-behaviors. Alcohol use: increased hepatotoxicity Sun exposure: photosensitivity
mentioned above. Patient monitoring Watch for vomiting, diarrhea, or stomatitis, which may cause dehydration. Know that high-dose therapy may cause nephrotoxicity. Monitor renal function, hydration status, urine alkalization (for pH above 6.5), and methotrexate blood level. Assess for fever, sore throat, bleeding, increased bruising, and other signs and symptoms of hematologic compromise or infection. With high-dose or intrathecal therapy, watch for CNS toxicity. Monitor creatinine and methotrexate blood levels 24 hours after therapy starts and then daily. Adjust leucovorin dosage as prescribed. Check hematologic studies at least monthly; blood or platelet transfusions may be necessary. Monitor liver and kidney function studies every 1 to 3 months. Evaluate uric acid levels. Watch for signs and symptoms of pulmonary toxicity, such as fever, dry nonproductive cough, dyspnea, hypoxemia, and infiltrates on chest Xray. Know that methotrexate exits slowly from third-space compartments (ascites, pleural effusions). Before therapy starts, fluid should be evacuated; during therapy, monitor drug blood level.
DRUG
DOSAGE
Pharmacodynamics
Adverse Reaction
Interaction
Health Teaching
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- FormulasDocument13 pagesFormulasSarah Salva100% (1)
- SAMPLE NCP For PneumoniaDocument3 pagesSAMPLE NCP For Pneumoniakana_mercado100% (6)
- NLE Compilation 1Document67 pagesNLE Compilation 1blazegomez91% (34)
- Etiopathogenesis of Biliary Atresia: Salva, Sarah Jane L. BSN 4JDocument4 pagesEtiopathogenesis of Biliary Atresia: Salva, Sarah Jane L. BSN 4JSarah SalvaNo ratings yet