Professional Documents
Culture Documents
Week 6 Case B 2022
Uploaded by
Charity Asprer OsorioOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Week 6 Case B 2022
Uploaded by
Charity Asprer OsorioCopyright:
Available Formats
Week 6 Case B
RM a 6 year old male child was brought to SWU-MC for the first time with chief complaint of swelling in
the face, legs and scrotal area.
HPI:
1 week PTA, mother noted puffy eyelids of the patient, no consult was done. Condition was tolerated,
until a few days PTA aside from the puffy eyelids the patient had swelling of the lower extremities and
scrotal area. She also observed that the patient had decrease frequency of urination and later told her
that her urine looks like ice tea. Persistence of condition prompted admission.
PE: awake, afebrile, not in respiratory distress
BP: 140/ 80mmHg HR: 100bpm RR: 20cpm O2 sat: 98% at room air Wt: 25kg
Skin: + multiple skin lesion with yellowish brown crust on the lower extremities
HEENT: supple neck, anicteric sclera, (-) cervical lymphadenopathy, grade II tonsils non erythematous
C/L: clear breath sounds
CVS: no murmur
Abd: globular, soft, NABS
GUT: scrotal swelling, + transillumination
Ext: grade 2 pretibial edema, strong pulses
Questions:
1. What other pertinent information should be elicited in the history? Physical examination?
2. Discuss the approach to hematuria and proteinuria?
3. What are the appropriate laboratory examination that should be performed to establish the
diagnosis?
4. Identify the logical diagnosis/ differential diagnosis based on the signs and symptoms of the
given case
5. Discuss the primary impression/diagnosis of the given case as to
a. Pathogenesis
b. Clinical manifestation
c. Appropriate diagnostic examination to establish the diagnosis
d. Management
e. Prognosis and Prevention
You might also like
- Chronic Diseases - Lymes, Hpv, Hsv Mis-Diagnosis and Mistreatment: A New Approach to the EpidemicFrom EverandChronic Diseases - Lymes, Hpv, Hsv Mis-Diagnosis and Mistreatment: A New Approach to the EpidemicRating: 5 out of 5 stars5/5 (1)
- PediatricsDocument84 pagesPediatricsMoataz TrabehNo ratings yet
- Headsss 3.0 &Phq9Document39 pagesHeadsss 3.0 &Phq9Charity Asprer OsorioNo ratings yet
- A Case Study On Dengue FeverDocument10 pagesA Case Study On Dengue FeverRinrin de BelenNo ratings yet
- Clinical Case Report on Dengue FeverDocument16 pagesClinical Case Report on Dengue FeverAimanazrul ZainudinNo ratings yet
- MCQ Tropmed 25 Maret 2010 PublishDocument27 pagesMCQ Tropmed 25 Maret 2010 PublishDapot Sianipar100% (1)
- Kawasaki DiseaseDocument22 pagesKawasaki DiseaseMax LocoNo ratings yet
- Liver Abscess Risk FactorsDocument7 pagesLiver Abscess Risk FactorsJoan junioNo ratings yet
- Soal Ika MCQ NasionalDocument27 pagesSoal Ika MCQ NasionalElly LutfiasariNo ratings yet
- Week 7 Case A 2022Document1 pageWeek 7 Case A 2022Charity Asprer OsorioNo ratings yet
- San Juan de Dios Educational Foundation, Inc. Department of Pediatrics 4th Floor Jaime Cardinal L. Sin Bldg. 2772 Roxas BLVD., Pasay CityDocument5 pagesSan Juan de Dios Educational Foundation, Inc. Department of Pediatrics 4th Floor Jaime Cardinal L. Sin Bldg. 2772 Roxas BLVD., Pasay CityNiña AmatNo ratings yet
- Fever in A ChildDocument46 pagesFever in A ChildSujeet ShahNo ratings yet
- ASD Internship ReportingDocument14 pagesASD Internship ReportingPernel Jose Alam MicuboNo ratings yet
- Pamantasan NG Lungsod NG Maynila College of Medicine Depatment of Microbiology and Parasitology Case Discussion in Virology CASE No.1: Group 1Document2 pagesPamantasan NG Lungsod NG Maynila College of Medicine Depatment of Microbiology and Parasitology Case Discussion in Virology CASE No.1: Group 1Maikka IlaganNo ratings yet
- Mohammad Hamid Sabibi - 720621465Document11 pagesMohammad Hamid Sabibi - 720621465Farida Trinovita SariNo ratings yet
- Clinical Abstract of 4-Month-Old Male with PneumoniaDocument3 pagesClinical Abstract of 4-Month-Old Male with PneumoniaSamuelNo ratings yet
- 4 Year Paediatrics Examination 2 SEMESTER SESSION 2009/2010 OBADocument11 pages4 Year Paediatrics Examination 2 SEMESTER SESSION 2009/2010 OBAMuhammad AzrinNo ratings yet
- PCC CaseDocument9 pagesPCC CaseKaila AbeledaNo ratings yet
- Leukemia Case StudyDocument3 pagesLeukemia Case StudyMaria Victoria A. PraxidesNo ratings yet
- 2nd Yr SGD Immuno Week 1 For StudentsDocument3 pages2nd Yr SGD Immuno Week 1 For StudentsRaya LuNo ratings yet
- 2B - Askep TB Paru - R.teratai A enDocument46 pages2B - Askep TB Paru - R.teratai A enPutri MeylisaNo ratings yet
- Ske BDocument3 pagesSke Bwindy ulfa gialiniNo ratings yet
- Clinical cases of Diphtheria and CroupDocument1 pageClinical cases of Diphtheria and CroupBeni KelnerNo ratings yet
- DRMC Grand Rounds: Case of Myxedema ComaDocument9 pagesDRMC Grand Rounds: Case of Myxedema ComaKristiannlae DanoNo ratings yet
- Case Management Protocol-Ong-Centipede Envenomation FINALDocument5 pagesCase Management Protocol-Ong-Centipede Envenomation FINALSamuel WibowoNo ratings yet
- TBL PaedsDocument10 pagesTBL PaedsHo Yong WaiNo ratings yet
- Lupus Nephritis Case Presentations - Clinical Features and ManagementDocument33 pagesLupus Nephritis Case Presentations - Clinical Features and ManagementBharath D sNo ratings yet
- Morning Report Sunday Night, July 7 2019: Iss/Ris/KhiDocument18 pagesMorning Report Sunday Night, July 7 2019: Iss/Ris/KhimariaNo ratings yet
- SGD 3 Case ProtocolDocument2 pagesSGD 3 Case ProtocolJulie Ann TrinidadNo ratings yet
- CC 2 Mei 2017 PneumoniaDocument37 pagesCC 2 Mei 2017 PneumoniaAhimsa Yoga AninditaNo ratings yet
- Joy N. Saquibal, M.DDocument78 pagesJoy N. Saquibal, M.DJoy AlmondsNo ratings yet
- Askep CKD Bhs InggrisDocument15 pagesAskep CKD Bhs InggrisFitri MulyaNo ratings yet
- Cirrhosis Case For PrintingDocument12 pagesCirrhosis Case For PrintingSean Mercado100% (1)
- Case Management NICU July 2020 Sam WibowoDocument6 pagesCase Management NICU July 2020 Sam WibowoSamuel WibowoNo ratings yet
- Lupus Primary CareDocument22 pagesLupus Primary Carewoopdeedoo903No ratings yet
- Hand infection in automotive technicianDocument10 pagesHand infection in automotive technicianP D Spencer0% (1)
- Case Presentation and Discussion On Dengue: Bedside Rounds OutputDocument5 pagesCase Presentation and Discussion On Dengue: Bedside Rounds OutputCalingalan Hussin CaluangNo ratings yet
- BANGSAJA Case Presentation and Discussion On DengueDocument17 pagesBANGSAJA Case Presentation and Discussion On DengueCalingalan Hussin CaluangNo ratings yet
- Alg OnesDocument2 pagesAlg OnesrendererichmadarangNo ratings yet
- Крок-2 - студ - 18 - англDocument8 pagesКрок-2 - студ - 18 - англAimeeNo ratings yet
- History Taking: 1. DemographicsDocument12 pagesHistory Taking: 1. Demographicsanis jannahNo ratings yet
- DR Ashiq Tutorials Base 2024Document49 pagesDR Ashiq Tutorials Base 2024cotoge7880No ratings yet
- The Problem List: Angkor Hospital For Children Faculty Development CourseDocument6 pagesThe Problem List: Angkor Hospital For Children Faculty Development CoursednaritaNo ratings yet
- ROSIMO - AUG 2021 NB VomitingDocument5 pagesROSIMO - AUG 2021 NB VomitingcarlosNo ratings yet
- Family and Clinical Case Presentation - DOCU - NEW CASEDocument8 pagesFamily and Clinical Case Presentation - DOCU - NEW CASERyan Joseph BalmacedaNo ratings yet
- Case Conference Friday Shift, June 30 2017Document49 pagesCase Conference Friday Shift, June 30 2017Izni AyuniNo ratings yet
- 5th Sem Internal Mid TermDocument17 pages5th Sem Internal Mid TermIashdip iashdipNo ratings yet
- CC 13 October 2017 (Demam Neutropenia) 2Document35 pagesCC 13 October 2017 (Demam Neutropenia) 2febrydwiNo ratings yet
- CA - CACAODocument2 pagesCA - CACAOISRAEL JULIANO SALGADONo ratings yet
- Anp Case Presentation of Icu 103 Sem IiDocument26 pagesAnp Case Presentation of Icu 103 Sem IiShilpa JoshiNo ratings yet
- CLS 400 - Test 4 (Extra Credit)Document8 pagesCLS 400 - Test 4 (Extra Credit)McNeeseInsiderNo ratings yet
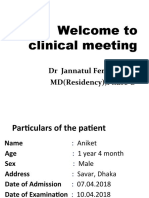
- Welcome To Clinical Meeting: DR Jannatul Ferdaus MD (Residency), Phase-BDocument37 pagesWelcome To Clinical Meeting: DR Jannatul Ferdaus MD (Residency), Phase-Bmd shadadNo ratings yet
- 1839-Article Text-5892-2-10-20200229Document13 pages1839-Article Text-5892-2-10-20200229MeliNo ratings yet
- Labrato - Kayla AHN596-801 SOAP#1Document10 pagesLabrato - Kayla AHN596-801 SOAP#1Kayla LabratoNo ratings yet
- PEDIA CASE 3 FinalDocument9 pagesPEDIA CASE 3 FinalXandra BnnNo ratings yet
- Daily Platelet Monitoring in DengueDocument52 pagesDaily Platelet Monitoring in DengueIrfan Dzakir NugrohoNo ratings yet
- Renal Disorders Case 5Document2 pagesRenal Disorders Case 5Geriz Daniella VigoNo ratings yet
- 5_6156702096872703940 (2)Document21 pages5_6156702096872703940 (2)Yohannes Kurniawan SoeparnoNo ratings yet
- Cwu 1 OrthoDocument14 pagesCwu 1 OrthoHakimah K. Suhaimi100% (1)
- Paediatrics 2014: DECEMBER 11, 2014 TIME ALLOWED: 11:00-1:00Document2 pagesPaediatrics 2014: DECEMBER 11, 2014 TIME ALLOWED: 11:00-1:00Ahmad Zulfitri AzmiNo ratings yet
- Chronic Cough CaseDocument2 pagesChronic Cough CaseCharity Asprer OsorioNo ratings yet
- C Ssrs Pediatric SLC 11.14.16Document4 pagesC Ssrs Pediatric SLC 11.14.16Charity Asprer OsorioNo ratings yet
- Taking care of your health and safety as a teenagerDocument2 pagesTaking care of your health and safety as a teenagerCharity Asprer OsorioNo ratings yet