Professional Documents
Culture Documents
Fentanyl-Induced Wooden Chest Syndrome Masquerading As Severe Res
Fentanyl-Induced Wooden Chest Syndrome Masquerading As Severe Res
Uploaded by
سلطان الحنبصيOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Fentanyl-Induced Wooden Chest Syndrome Masquerading As Severe Res
Fentanyl-Induced Wooden Chest Syndrome Masquerading As Severe Res
Uploaded by
سلطان الحنبصيCopyright:
Available Formats
Providence St.
Joseph Health
Providence St. Joseph Health Digital Commons
Providence Portland Medical Center Internal Providence Portland Medical Center Internal
Medicine 2021 Medicine
5-2021
Fentanyl-Induced Wooden Chest Syndrome Masquerading as
Severe Respiratory Distress Syndrome in COVID-19
Grace Judd
Rachael Starcher
David Hotchkin
Follow this and additional works at: https://digitalcommons.psjhealth.org/oaa_ppmc_21
Part of the Internal Medicine Commons
Fentanyl-Induced Wooden Chest Syndrome Masquerading as Severe
Respiratory Distress Syndrome in COVID-19
Grace Judd BS, Rachael Starcher MD, David Hotchkin MD
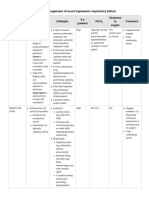
Case Presentation Wooden Chest Syndrome v. COVID-19 ARDS
Compliance is Inverse to Transpulmonary Pressure
History
• 47 yo M with no PMH presented with fever and respiratory distress ∆𝑣𝑣 ∆𝑣𝑣 c = lung compliance
Marked hypercarbia
• Admitted for COVID-19 pneumonia
𝑐𝑐 = = v = volume Marked hypoxia
Hospital Course ∆𝑝𝑝 𝑝𝑝𝑎𝑎𝑎𝑎 − 𝑝𝑝𝑝𝑝𝑙𝑙 pav = alveolar pressure
ppl = pleural pressure
Laryngospasm and
respiratory muscle
Ventilatory
failure Inflammatory
• Intubated for moderate acute respiratory distress syndrome alveolar damage
contraction
(ARDS) on hospital day 11 Poor lung
• Fentanyl infusion started Poor Compliance in both ARDS and WCS compliance Poor alveolar
• Hypoxia improved within 36 hrs but plateau pressures consistently Good alveolar
compliance compliance
>30 cm H2O despite minimizing dead space High airway
• Trial of airway pressure release ventilation worsened hypercarbia COVID-19 Wooden Chest pressures
• Bronchoscopy w/o mucous plugging, airway collapse, or purulent ARDS Syndrome Poor chest wall Good chest wall
secretions compliance compliance
• Lung compliance worsened (Pplat=50 on 4 cc/kg) w/o change in Plateau pressure High High
oxygenation
• Developed suspicion for wooden chest syndrome (WCS) and Lung compliance Low Low
discontinued fentanyl Takeaway Points
Alveolar pressure High Low
Outcome Pleural pressure Low High Fentanyl uniquely activates laryngeal and respiratory muscle
• Pplat nadired at 16 within one hour after stopping fentanyl potentially leading to a fatal syndrome known as Wooden Chest
• Pt successfully extubated on VD 10 Syndrome (WCS) manifested by poor ventilation
• It is likely more common than clinicians realize
Fentanyl Activates Muscles Likely Prevalence
Implications in practice:
Low Lung Compliance with Worsening Ventilation Frequency of Frequency
Opiates of Use Used in ICU†
• Maintain a high index of suspicion for alternate or overlying
pCO2 physiologies when treating persistent ventilatory failure in ARDS
Morphine & in COVID-19
Static Lung Compliance [normal 50-100 mL/cm H2O]
analogues Recommendation:
80
• Discontinue fentanyl if lung compliance and ventilatory failure
70 seem out of proportion to hypoxia
60
Fentanyl &
50 sk analogues References
40 Burry, Lisa D., David R. Williamson, Marc M. Perreault, Louise Rose, Deborah J. Cook, Niall D. Ferguson, Stephanie C. Lapinsky, and Sangheeta Mehta. “Analgesic, Sedative, Antipsychotic, and Neuromuscular Blocker Use in Canadian Intensive Care Units: A
Prospective, Multicentre, Observational Study.” Canadian Journal of Anaesthesia = Journal Canadien D’anesthesie 61, no. 7 (July 2014): 619–30. https://doi.org/10.1007/s12630-014-0174-1.
Buxton, Jane A., Tim Gauthier, Mai-Lei Woo Kinshella, and Jesse Godwin. “A 52-Year-Old Man with Fentanyl-Induced Muscle Rigidity.” CMAJ : Canadian Medical Association Journal 190, no. 17 (April 30, 2018): E539–41. https://doi.org/10.1503/cmaj.171468.
30
Camporota, Luigi, Davide Chiumello, Mattia Busana, Luciano Gattinoni, and John J. Marini. “Pathophysiology of COVID-19-Associated Acute Respiratory Distress Syndrome.” The Lancet Respiratory Medicine 0, no. 0 (November 13, 2020).
https://doi.org/10.1016/S2213-2600(20)30505-1.
Çoruh, Başak, Mark R. Tonelli, and David R. Park. “Fentanyl-Induced Chest Wall Rigidity.” Chest 143, no. 4 (April 2013): 1145–46. https://doi.org/10.1378/chest.12-2131.
Fentanyl is the most used analgesia Davis, Mellar P., and Bertrand Behm. “Reasons to Avoid Fentanyl.” Annals of Palliative Medicine 9, no. 2 (March 2020): 61124–624. https://doi.org/10.21037/apm.2020.01.12.
Freund, F. G., W. E. Martin, K. C. Wong, and T. F. Hornbein. “Abdominal-Muscle Rigidity Induced by Morphine and Nitrous Oxide.” Anesthesiology 38, no. 4 (April 1973): 358–62.
20
Gattinoni, Luciano, Silvia Coppola, Massimo Cressoni, Mattia Busana, Sandra Rossi, and Davide Chiumello. “COVID-19 Does Not Lead to a ‘Typical’ Acute Respiratory Distress Syndrome.” American Journal of Respiratory and Critical Care Medicine 201, no. 10
in ICU patients on mechanical
(May 15, 2020): 1299–1300. https://doi.org/10.1164/rccm.202003-0817LE.
Grasselli, Giacomo, Tommaso Tonetti, Alessandro Protti, Thomas Langer, Massimo Girardis, Giacomo Bellani, John Laffey, et al. “Pathophysiology of COVID-19-Associated Acute Respiratory Distress Syndrome: A Multicentre Prospective Observational Study.”
The Lancet Respiratory Medicine 8, no. 12 (December 1, 2020): 1201–8. https://doi.org/10.1016/S2213-2600(20)30370-2.
♦Grell, F. L., R. A. Koons, and J. S. Denson. “Fentanyl in Anesthesia: A Report of 500 Cases.” Anesthesia and Analgesia 49, no. 4 (August 1970): 523–32.
10 ventilation
Haudebourg, Anne-Fleur, François Perier, Samuel Tuffet, Nicolas de Prost, Keyvan Razazi, Armand Mekontso Dessap, and Guillaume Carteaux. “Respiratory Mechanics of COVID-19– versus Non–COVID-19–Associated Acute Respiratory Distress Syndrome.”
American Journal of Respiratory and Critical Care Medicine 202, no. 2 (June 1, 2020): 287–90. https://doi.org/10.1164/rccm.202004-1226LE.
Jacobi, Judith, Gilles L. Fraser, Douglas B. Coursin, Richard R. Riker, Dorrie Fontaine, Eric T. Wittbrodt, Donald B. Chalfin, et al. “Clinical Practice Guidelines for the Sustained Use of Sedatives and Analgesics in the Critically Ill Adult.” Critical Care Medicine 30,
no. 1 (January 2002): 119–41. https://doi.org/10.1097/00003246-200201000-00020.
Lucero, David, Shobha Mandal, and Apurwa Karki. “Lung Compliance in a Case Series of Four COVID-19 Patients at a Rural Institution.” Cureus 12, no. 7. Accessed December 18, 2020. https://doi.org/10.7759/cureus.9472.
0
† Payen, Jean-Francois, Gérald Chanques, Jean Mantz, Christiane Hercule, Igor Auriant, Jean-Luc Leguillou, Michèle Binhas, et al. “Current Practices in Sedation and Analgesia for Mechanically Ventilated Critically Ill Patients: A Prospective Multicenter Patient-
Based Study.” Anesthesiology 106, no. 4 (April 1, 2007): 687–95. https://doi.org/10.1097/01.anes.0000264747.09017.da.
99%♦ of people develop at least mild
Roan, Jeffrey P., Navin Bajaj, Field A. Davis, and Natalie Kandinata. “Opioids and Chest Wall Rigidity During Mechanical Ventilation.” Annals of Internal Medicine 168, no. 9 (May 1, 2018): 678. https://doi.org/10.7326/L17-0612.
Sokoll, M. D., J. L. Hoyt, and S. D. Gergis. “Studies in Muscle Rigidity, Nitrous Oxide, and Narcotic Analgesic Agents.” Anesthesia and Analgesia 51, no. 1 (February 1972): 16–20.
1 2 3 4 5 6 7 8 9 10 Torralva, Randy, Amy J. Eshleman, Tracy L. Swanson, Jennifer L. Schmachtenberg, William E. Schutzer, Shelley H. Bloom, Katherine M. Wolfrum, John F. Reed, and Aaron Janowsky. “Fentanyl but Not Morphine Interacts with Non-Opioid Recombinant Human
Neurotransmitter Receptors and Transporters.” Journal of Pharmacology and Experimental Therapeutics, January 1, 2020. https://doi.org/10.1124/jpet.120.265561.
muscle rigidity when given fentanyl Torralva, Randy, and Aaron Janowsky. “Noradrenergic Mechanisms in Fentanyl-Mediated Rapid Death Explain Failure of Naloxone in the Opioid Crisis.” Journal of Pharmacology and Experimental Therapeutics 371, no. 2 (November 1, 2019): 453–75.
Ventilator Day
https://doi.org/10.1124/jpet.119.258566.
Yasuda, Hideto, Tetsuro Nishimura, Tetsuro Kamo, Masamitsu Sanui, Eishu Nango, Takayuki Abe, Toru Takebayashi, Alan Kawarai Lefor, and Satoru Hashimoto. “Optimal Plateau Pressure for Patients with Acute Respiratory Distress Syndrome: A Protocol for a
Systematic Review and Meta-Analysis with Meta-Regression.” BMJ Open 7, no. 5 (May 29, 2017). https://doi.org/10.1136/bmjopen-2016-015091.
Yasuda, I., T. Hirano, T. Yusa, and M. Satoh. “Tracheal Constriction by Morphine and by Fentanyl in Man.” Anesthesiology 49, no. 2 (August 1978): 117–19. https://doi.org/10.1097/00000542-197808000-00012.
You might also like
- pg36-37 of Pneumothorax Case StudyDocument2 pagespg36-37 of Pneumothorax Case Studyikemas100% (1)
- Dyslexia BookletN PDFDocument33 pagesDyslexia BookletN PDFDr.V.Sivaprakasam100% (2)
- Pathophysiology of Chronic Obstructive Pulmonary DisorderDocument2 pagesPathophysiology of Chronic Obstructive Pulmonary DisorderBlessyl Mae EstenzoNo ratings yet
- Psychological ResilienceDocument37 pagesPsychological Resiliencedgavrile100% (3)
- Mechanical Ventilation: Dr. Shivam Mohan PandeyDocument150 pagesMechanical Ventilation: Dr. Shivam Mohan PandeyshivamNo ratings yet
- PEEP Positive End Expiratory Pressure and Its ConsequencesDocument2 pagesPEEP Positive End Expiratory Pressure and Its ConsequencesSadiq ZakariaNo ratings yet
- IOSH Working Safely v5 Course Syllabus 1Document3 pagesIOSH Working Safely v5 Course Syllabus 1pranavNo ratings yet
- 〈1229.1〉 Steam Sterilization by Direct ContactDocument3 pages〈1229.1〉 Steam Sterilization by Direct ContactAhckarawinThummaneeNo ratings yet
- Chronic Bronchitis and EmphesemaDocument2 pagesChronic Bronchitis and Emphesemanursing concept maps100% (2)
- NCP Impaired Gas ExchangeDocument2 pagesNCP Impaired Gas ExchangeGabriel Tolentino70% (10)
- Iv. Pathophysiology 1. Schematic Diagram Book Based Pathophysiology: Precipitating/Modifiable Factors Non Modifiable / Predisposing FactorsDocument2 pagesIv. Pathophysiology 1. Schematic Diagram Book Based Pathophysiology: Precipitating/Modifiable Factors Non Modifiable / Predisposing Factorsikemas67% (6)
- ARDS (Acute Respiratory Distress Syndrome) : EarlyDocument1 pageARDS (Acute Respiratory Distress Syndrome) : EarlyDora Elena HurtadoNo ratings yet
- Chapter 14 - Overview of The CirculationDocument26 pagesChapter 14 - Overview of The Circulationmuna sNo ratings yet
- Janeways Immunobiology 9th Edition Murphy Test BankDocument35 pagesJaneways Immunobiology 9th Edition Murphy Test Bankbrassepoiserwgjx5100% (23)
- NCP Difficulty of Breathing R/T SecretionDocument3 pagesNCP Difficulty of Breathing R/T Secretionherscentasiascribd50% (8)
- NCP For Cough 1Document3 pagesNCP For Cough 1Ro VinNo ratings yet
- The Narcissistic Masochistic CharacterDocument7 pagesThe Narcissistic Masochistic CharacterIrene IonescuNo ratings yet
- Covid - 19 NCPDocument4 pagesCovid - 19 NCPKrisianne Mae Lorenzo FranciscoNo ratings yet
- SARS PathophysioDocument2 pagesSARS PathophysioLouise BravoNo ratings yet
- ArdsDocument85 pagesArdsSiti KurniatiNo ratings yet
- Medical Surgical NursingDocument6 pagesMedical Surgical NursingzemmiphobiaNo ratings yet
- Respiratory Mechanics and Introduction To Respiratory PhysiologyDocument55 pagesRespiratory Mechanics and Introduction To Respiratory PhysiologyhariNo ratings yet
- 242 - Respiratory Pathology COPD - Clinical FeaturesDocument3 pages242 - Respiratory Pathology COPD - Clinical FeaturesPranav PunjabiNo ratings yet
- EAC BASIC Respiratory Pharmacology DrugsDocument130 pagesEAC BASIC Respiratory Pharmacology DrugsMARK RYAN HERNANDEZNo ratings yet
- PathophysiologyDocument1 pagePathophysiologyChua CandiceNo ratings yet
- ADAZA BSND 3 OR REQS Concept MAP 3 PDFDocument1 pageADAZA BSND 3 OR REQS Concept MAP 3 PDFKrizle AdazaNo ratings yet
- Acute Respiratory Distress SyndromeDocument7 pagesAcute Respiratory Distress SyndromeMicaNo ratings yet
- Covid NCPDocument6 pagesCovid NCPNathalia Cabalse100% (2)
- PulmonologyDocument39 pagesPulmonologyApsaraNo ratings yet
- Braga, Patricia 4B (NCM 118)Document4 pagesBraga, Patricia 4B (NCM 118)Jessica BragaNo ratings yet
- NCP Acute BrochitisDocument5 pagesNCP Acute BrochitisFrancine kimberlyNo ratings yet
- Flowchart 12 Dmts For AdultsDocument2 pagesFlowchart 12 Dmts For AdultsCristina SofiaNo ratings yet
- (PULMO) - ABG Interpretation PDFDocument7 pages(PULMO) - ABG Interpretation PDFKeith LajotNo ratings yet
- Pa Tho PhysiologyDocument1 pagePa Tho PhysiologyJoanne JelicaNo ratings yet
- (NS) AsthmaCOPDPneumonia Tutorial QuestionsDocument25 pages(NS) AsthmaCOPDPneumonia Tutorial QuestionsJoei “Jojo” GohNo ratings yet
- Flowchart DT For AdultsDocument3 pagesFlowchart DT For Adultsdr.mumtazhussain78No ratings yet
- Respiratory System GlossaryDocument3 pagesRespiratory System GlossaryFernanda AmigoNo ratings yet
- Emergencycarefor Acute Respiratory FailureDocument1 pageEmergencycarefor Acute Respiratory FailurekarenmstamNo ratings yet
- Ventilation-Perfusion RatioDocument34 pagesVentilation-Perfusion Rationeeba habeebNo ratings yet
- Cues Nursing Diagnosis Inference Planning Nursing Intervention Rationale EvaluationDocument3 pagesCues Nursing Diagnosis Inference Planning Nursing Intervention Rationale EvaluationNichol John MalabananNo ratings yet
- Asthma - Patho, Signs & SymptomsDocument1 pageAsthma - Patho, Signs & SymptomsBaebee LouNo ratings yet
- Pulmonary Edema Concept MapDocument3 pagesPulmonary Edema Concept MapGeraldine MagnanaoNo ratings yet
- Name of DrugDocument5 pagesName of DrugJoann BeriñoNo ratings yet
- Icu 3Document8 pagesIcu 3GemilleDaphneAndradaNo ratings yet
- PBL - RespiratoryDocument6 pagesPBL - Respiratorygie sarcedaNo ratings yet
- NCP Ineffective Airway Clearance PediaDocument2 pagesNCP Ineffective Airway Clearance PediaFaith CalimlimNo ratings yet
- NCP Rds 2Document1 pageNCP Rds 2Angelokeizer Gavino0% (1)
- Spiro Me TryDocument13 pagesSpiro Me TryfatimaabedulkhalikturkeyNo ratings yet
- Scenario 4 - NCPDocument15 pagesScenario 4 - NCPVian RiveraNo ratings yet
- NCPDocument3 pagesNCPNikki del Rosario100% (2)
- NCPDocument27 pagesNCPcuakialyannaNo ratings yet
- Ards Concept MapDocument1 pageArds Concept Mapchristine louise bernardoNo ratings yet
- ARDSDocument1 pageARDSBejinaruOanaSiCristiNo ratings yet
- BST NotesDocument26 pagesBST NotesshanggariNo ratings yet
- Assessment Diagnosis Planning Interventions Rationale Evaluation Problem: Difficulty of IndependentDocument5 pagesAssessment Diagnosis Planning Interventions Rationale Evaluation Problem: Difficulty of IndependentZabeth ZabNo ratings yet
- The Health Sciences CenterDocument5 pagesThe Health Sciences CenterStef ReyesNo ratings yet
- Hypoxemia 2Document3 pagesHypoxemia 2ganganakulan.nagavallyNo ratings yet
- ICU One Pager ARDS v1.1Document1 pageICU One Pager ARDS v1.1Michael LevitNo ratings yet
- Potential Conflicts of InterestDocument8 pagesPotential Conflicts of InterestLina GuerraNo ratings yet
- NCP PCDocument9 pagesNCP PCangelaNo ratings yet
- Esophageal Balloon Manometry RitzDocument37 pagesEsophageal Balloon Manometry RitzMichael LevitNo ratings yet
- Little Hans Case StudyDocument7 pagesLittle Hans Case StudyTammy Poe50% (2)
- SynthesisDocument1 pageSynthesisKenneth Von AllawiNo ratings yet
- Prevalence of Extended Spectrum Beta-Lactamase-Producing Escherchia Coli in Chicken MeatDocument8 pagesPrevalence of Extended Spectrum Beta-Lactamase-Producing Escherchia Coli in Chicken MeatIndian Journal of Veterinary and Animal Sciences RNo ratings yet
- Health 8 Q3 1 Stages of InfectionDocument25 pagesHealth 8 Q3 1 Stages of InfectionKimberly TanalasNo ratings yet
- Update Tim Tanggap DaruratDocument1 pageUpdate Tim Tanggap DaruratTeguh ArifinNo ratings yet
- UHC Slide Deck For Strat Planning of UISDocument78 pagesUHC Slide Deck For Strat Planning of UISIan Isaias ReclaNo ratings yet
- Esaote Dedicated-MRI-Factbook - 169004500MA - V04 - LRDocument12 pagesEsaote Dedicated-MRI-Factbook - 169004500MA - V04 - LREl DoNo ratings yet
- Synopsis: Title-Effect of Eccentric Training and Static Stretching On Calf Muscle Tightness Among Young AdultsDocument10 pagesSynopsis: Title-Effect of Eccentric Training and Static Stretching On Calf Muscle Tightness Among Young AdultsPoonam soniNo ratings yet
- Literature Review On Stress Management at WorkplaceDocument7 pagesLiterature Review On Stress Management at WorkplaceaflsswofoNo ratings yet
- SMRJ 2020 4 2 11591Document4 pagesSMRJ 2020 4 2 11591Isadora BuffonNo ratings yet
- Social Work in IndustryDocument19 pagesSocial Work in IndustryMd Ameer86% (29)
- Knowledge of Post Discharge Home Care Management Among Patients With Myocardial InfarctionDocument49 pagesKnowledge of Post Discharge Home Care Management Among Patients With Myocardial InfarctionRumela Ganguly ChakrabortyNo ratings yet
- Rosalinda Poot Morales: StudentDocument2 pagesRosalinda Poot Morales: StudentNewAccountMXNo ratings yet
- Eating Sweet Foods Produces Acid in The Mouth, Which Can Cause Tooth Decay. (High Acid Levels Are Measured by Low PH Values)Document19 pagesEating Sweet Foods Produces Acid in The Mouth, Which Can Cause Tooth Decay. (High Acid Levels Are Measured by Low PH Values)Munawir Rahman IslamiNo ratings yet
- Unit 301 Understanding The Principles and Practices of AssessmentDocument32 pagesUnit 301 Understanding The Principles and Practices of AssessmentحيدرالركابيNo ratings yet
- Employee BenefitsDocument28 pagesEmployee BenefitsJedea Joy LactaoenNo ratings yet
- Methylation Briget BriggsDocument61 pagesMethylation Briget BriggsBenjamin PeelNo ratings yet
- Social Psychology: Changing Attitudes Through PersuationDocument7 pagesSocial Psychology: Changing Attitudes Through PersuationChin SilverNo ratings yet
- База Тестів на ПМК2 з анатомії УКР і АНГDocument183 pagesБаза Тестів на ПМК2 з анатомії УКР і АНГAnzhelika BondarenkoNo ratings yet
- Ielts EssayDocument54 pagesIelts EssayHeyder Hiko HesenovNo ratings yet
- The Social Dilemma and Social NetworksDocument2 pagesThe Social Dilemma and Social NetworksJefferson Javier Barrera MontanezNo ratings yet
- MUCLecture 2022 4162747Document8 pagesMUCLecture 2022 4162747JamesNo ratings yet