Professional Documents
Culture Documents
Ethic and Legal Aspects in Bio Medical Research Involving Human Beings
Ethic and Legal Aspects in Bio Medical Research Involving Human Beings
Uploaded by
luminitasimionOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ethic and Legal Aspects in Bio Medical Research Involving Human Beings
Ethic and Legal Aspects in Bio Medical Research Involving Human Beings
Uploaded by
luminitasimionCopyright:
Available Formats
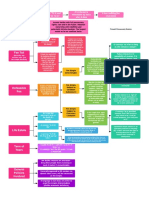
ETHIC AND LEGAL ASPECTS IN BIOMEDICAL RESEARCH INVOLVING HUMAN BEINGS
Toader Elena Gr.T. Popa University of Medicine and Pharmacy / Institute of Gastroenterology and Hepatology str. Costache Negri nr.60.bl.C1, sc.B et.2, ap.6, Iasi, Romnia toader.elena@yahoo.com / www.bioinginerie.ro
Damir Daniela Gr.T. Popa University of Medicine and Pharmacy str.Independenei nr.2, bl. C, et.6 ap. 26, Iai, Romnia, danadamir@yahoo.com / www.bioinginerie.ro
Abstract
The observation of the ethical and juridical standards is the premise without which the applications of biomedical research involving human beings are forbidden. Taking this into consideration, the ethical aspects of biomedical research, are evaluated by the european group for deontology, whereas juridical aspects are regulated by national and community law. The complementarity of the two categories of rules, that is ethical and legal, shows that there are the processes the application of which constitutes an offence to human dignity. The ethical principles and legal aspects laid down in the instruments and guidance covering biomedical research aim to protect the dignity, rights, safety and well being of the research participants.
confidence that the materials will be handled and used sensitively and responsibly. It is likewise important that any collections of human biological materials are used optimally and that unnecessary collection of new materials is avoided. The materials that are taken from human beings for research must/should fall into two broad categories: those that are destined for immediate use in a specific research project; those that are to be stored for future use. The ethical issues for research involving human biological materials are two-fold: issues concerning initial removal of the material, which necessitates a physical intervention this is the only time when the physical integrity of a person is at stake and the general protective provisions concerning biomedical research apply as for any other research intervention; issues of consent/authorisation and confidentiality concerning use and/or storage of the materials that have been removed.
1. Introduction
The use of human biological materials is increasingly important for biomedical research. Consequently, research participants and the public should have
Page 1 of 3
Research may be conducted at local/regional, national, or, international level. The growing international dimension has prompted the development of internationally accepted ethical principles for biomedical research for example, as set out in the Council of Europe Convention on Human Rights and Biomedicine and its Additional Protocols as well as in other legally binding instruments. Furthermore other sources of ethical guidance are internationally widely accepted, foremost among these being the World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects and the Council for International Organizations of Medical Sciences (CIOMS) International Ethical Guidelines for Biomedical Research Involving Human Subjects.
research project must always be justified specifically. Special provisions are also needed, to ensure appropriate protection of persons who, according to law, are not able to give valid consent because of their age (minors), a mental disability, a disease or for other reasons. Research on stored human biological materials may raise particular problems with regard to consent.
2.2 Beneficence and non-maleficence
The principles of beneficence and non maleficence [2,3] encapsulate the moral obligation to maximise potential benefit and minimize potential harm. There ensure appropriate protection of the research participants. The balance between harms and benefits is therefore critical to the ethics of biomedical research. In practice, this means that all research projects must undergo a thorough comparative risk/benefit assessment. Risks must always be minimized.
2. Ethical principles
All research involving human beings should be conducted according to ethical principles: autonomy; beneficence and the related principle of nonmaleficence; justice. Ensuring respect for ethical principles independent scientific and ethical evaluation. The ethical principles laid down in the instruments and guidance covering biomedical research aim to protect the dignity, rights, safety and well being of the research participants. Independent examination of the scientific merit of a research project and review of its ethical acceptability are central to ensuring respect for these principles Underpinning these principles, from which other ethical considerations flow, is the need to respect and protect human dignity and the corollary principle of primacy of the human being.
2.3 Justice
The principle of justice [4] encompasses fairness and equity. This principle has been generally defined in relation to biomedicine, but also has particular relevance for research. In biomedical research involving human beings, this implies that the distribution of risk and burden on the one hand and benefit on the other be fair a principle known as distributive justice. The key question is who ought to receive the benefits of research and bear its risk and burden.
3. Legal aspects
From a legal standpoint, research projects must comply with the national law of the country where the research will be carried out. In turn, the national law of each country must fulfill the requirements of any international laws/treaties to which the countries concerned have subscribed. Various standard-setting instruments deal with biomedical research, whether at world, European or national level; these are thus classified according to their legally non-binding or binding character [5,6]. Non legally binding instruments: Declaration of Helsinki, drawn up by of the World Medical Association and adopted for the first time in 1964 with several subsequent amendments. The Universal Declaration on bioethics and human rights, drawn up within UNESCO, contains certain provisions on research. The CIOMS International Ethical Guidelines for Biomedical Research Involving Human Subjects and the ICH, E6 Good Clinical
2.1 Autonomy
Respect for autonomy of the persons capacity to make personal choices. In the context of biomedicine there are further implications [1]: that an individual should be provided with the necessary conditions to exercise his or her autonomy; that a person whose autonomy is diminished or impaired should be protected from harm and abuse. In biomedical research, the principle of autonomy is exercised in particular through the process of free and informed consent. Particular attention must be paid to dependent and vulnerable people whose proposed participation in a
Page 2 of 3
Practice guidelines, drawn up by the International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use are also of special interest.
3.1 Legally binding instruments
Directive 2001/20/EC of the European Parliament and of the Council of 4 April 2001 Convention on Human Rights and Biomedicine (Oviedo Convention) drawn up within the Council of Europe Article 7 of the Covenant on Civil and Political Rights, drawn up within the United Nations. 3.1.1 The Oviedo Convention and Additional Protocol concerning Biomedical Research. Drawn up within the Council of Europe by the Steering Committee on Bioethics, the Oviedo Convention and its Additional Protocol concerning Biomedical Research constitute international treaties [7]. Their provisions are legally binding in respect of the countries which have ratified them. The Convention provisions apply to research projects in the sphere of health where such research involves an intervention on a human being. This includes, in particular, research on medicines, but also other types of research such as fundamental research. 3.1.2 Directive 2001/20/EC. Directive 2001/20/EC [8] is applicable to the Member States of the European Union and the contracting States of the European Economic Area (EEA). The Directives provisions apply to clinical trials on medicinal products for human use, performed in any Member State of the EU/EEA. Non-interventional trials as defined in Article 2(c) of the Directive are not covered. (EC). The Convention (Article 22) requires participants free informed consent for the storage and use of materials for a purpose other than that for which it was removed. It further stipulates (Article 21) that the human body and its parts shall not, as such, give rise to financial gain. This does not of itself preclude the licensing/selling of intellectual property rights arising from research in
which the samples are used (i.e. this is the same as for other intellectual property rights) but it does mean that those who donate their materials should be informed if those materials might be used for commercial purposes. It also means that researchers should not sell the materials per se for a profit, and that donors of materials should not be offered financial inducement to donate samples (reimbursement of reasonable expenses would be permissible).
4. Conclusion
In conclusion todays research is tomorrows healthcare this simple statement encapsulates the ultimate justification for biomedical research.
5. References
[1] Cohen J., Patient autonomy and social fairness, Cambridge Quarterly of healthcare ethics 9, 391-399, 2000. [2] Beauchamp T.L., Childress J.F. Beneficience, in Principles of Biomedical Ethics, p 165-214, Oxford University Press, 2001. [3] Beauchamp T.L., Childress J.F. Nonmaleficience, in Principles of Biomedical Ethics, p 113-157, Oxford University Press ,2001. [4] Rawls J., Chapter II The principles of Justice, A Theory of Justice, Harvard University Press, p 34-114, 2005. [5] The Helsinki Declaration, www.wma.net [6] Council for International Organizations of Medical Sciences (CIOMS) [7] The Oviedo Convention www.coe.int/bioethics [8] Directive 2001/20/EC and its Protocols,
Page 3 of 3
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5814)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (845)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Property Present EstatesDocument1 pageProperty Present EstatesBrat Wurst100% (1)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Motion For Reconsideration FormatDocument3 pagesMotion For Reconsideration FormatKendrick SiaoNo ratings yet
- READMEDocument3 pagesREADMEDarryn BendykNo ratings yet
- SOLO PARENT ID Application FormDocument1 pageSOLO PARENT ID Application FormRoselyn Padernal100% (1)
- Neville - V - Trafford PLCDocument2 pagesNeville - V - Trafford PLCRed HoodNo ratings yet
- Sps. Valenzuela v. Sps. Mano, G.R. No. 172611, July 9, 2010Document2 pagesSps. Valenzuela v. Sps. Mano, G.R. No. 172611, July 9, 2010EPZ RELANo ratings yet
- Sales ParasDocument162 pagesSales ParasZydalgLadyz Nead100% (2)
- C7. Licaros vs. SandiganbayanDocument2 pagesC7. Licaros vs. SandiganbayanAlit Dela Cruz100% (1)
- Contract For The Long TermDocument7 pagesContract For The Long TermWendimagen Meshesha FantaNo ratings yet
- 77 People v. WagasDocument6 pages77 People v. WagasTricia MontoyaNo ratings yet
- The Legal Representative Suits Act, 1855Document1 pageThe Legal Representative Suits Act, 1855Rizwan Niaz RaiyanNo ratings yet
- WillsDocument99 pagesWillsDR100% (2)
- Patrice Mansell v. Frederic N. Smalkin, 91 F.3d 131, 4th Cir. (1996)Document1 pagePatrice Mansell v. Frederic N. Smalkin, 91 F.3d 131, 4th Cir. (1996)Scribd Government DocsNo ratings yet
- United States v. Sherry Taylor, 4th Cir. (2012)Document11 pagesUnited States v. Sherry Taylor, 4th Cir. (2012)Scribd Government DocsNo ratings yet
- Sitaca v. PalomaresDocument10 pagesSitaca v. PalomaresAlyssa Bianca OrbisoNo ratings yet
- Diplomatic and Consular Immunity On Law Enforcement and Judicial AuthoritiesDocument52 pagesDiplomatic and Consular Immunity On Law Enforcement and Judicial AuthoritiesGregory A WallaceNo ratings yet
- Lawsuit: June Rodgers v. Chris Christie Et Al.Document45 pagesLawsuit: June Rodgers v. Chris Christie Et Al.jalt61No ratings yet
- Martin Joseph Kilcoyne v. Robert Morgan, Chairman, Board of Trustees, East Carolina University, Etc., 664 F.2d 940, 4th Cir. (1981)Document4 pagesMartin Joseph Kilcoyne v. Robert Morgan, Chairman, Board of Trustees, East Carolina University, Etc., 664 F.2d 940, 4th Cir. (1981)Scribd Government DocsNo ratings yet
- People v. Abordo, 58 Phil. 350 (1933)Document1 pagePeople v. Abordo, 58 Phil. 350 (1933)faithNo ratings yet
- Company Law-I, Promotion Activities & Formation of A Company - IDocument6 pagesCompany Law-I, Promotion Activities & Formation of A Company - IAbid CoolNo ratings yet
- Potential Participants, AnalysisDocument63 pagesPotential Participants, AnalysisZuzi RadičováNo ratings yet
- Case Digest - People v. Pajares (1992)Document2 pagesCase Digest - People v. Pajares (1992)Nicole DeocarisNo ratings yet
- Facts of Case: United States Supreme Court MCNABB v. U.S., (1943)Document5 pagesFacts of Case: United States Supreme Court MCNABB v. U.S., (1943)Hakim Ali HotianaNo ratings yet
- Joseph P. Haddad, Administrator v. Border Express, Inc., 300 F.2d 885, 1st Cir. (1962)Document2 pagesJoseph P. Haddad, Administrator v. Border Express, Inc., 300 F.2d 885, 1st Cir. (1962)Scribd Government DocsNo ratings yet
- Marcoso v. CADocument2 pagesMarcoso v. CAPrincess Samantha SarcedaNo ratings yet
- Hanlon V Hausserman and BeamDocument2 pagesHanlon V Hausserman and Beamsmtm06No ratings yet
- Doe V Dirty World Entertainment ComplaintDocument7 pagesDoe V Dirty World Entertainment ComplaintEric GoldmanNo ratings yet
- Agency DigestsDocument6 pagesAgency DigestsWilliam GriffinNo ratings yet
- Ernesto M. Maceda, vs. Hon. Catalino Macaraig, JR., in His Capacity As Executive SecretaryDocument1 pageErnesto M. Maceda, vs. Hon. Catalino Macaraig, JR., in His Capacity As Executive SecretaryI.G. Mingo MulaNo ratings yet
- Chapter 18 National Sex Offender RegistryDocument25 pagesChapter 18 National Sex Offender RegistryAndrew Charles HendricksNo ratings yet