Professional Documents
Culture Documents
Ozonearticle
Uploaded by
سامر مضحيOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ozonearticle
Uploaded by
سامر مضحيCopyright:
Available Formats
See discussions, stats, and author profiles for this publication at: https://www.researchgate.
net/publication/340889776
Efficacy of Subgingival Ozone Irrigation for Management of Chronic
Periodontitis – A Clinical, Microbiological and Biochemical study
Article · January 2020
CITATION READS
1 189
5 authors, including:
Thayyil Sivaraman Hrishi Pratibha Kundapur
Government Dental College Calicut Manipal Academy of Higher Education
14 PUBLICATIONS 40 CITATIONS 18 PUBLICATIONS 238 CITATIONS
SEE PROFILE SEE PROFILE
Some of the authors of this publication are also working on these related projects:
Implant View project
soft tissue regeneration View project
All content following this page was uploaded by Thayyil Sivaraman Hrishi on 02 June 2020.
The user has requested enhancement of the downloaded file.
Thayyil S Hrishi et al; Subgingival Ozone Irrigation in Management of Chronic Periodontitis
ORIGINAL ARTICLE DENTISTRY
ISSN [P-2347-4513]
Journal of Contemporary Medicine ISSN [O-2349-0799]
Year: 2020
and Dentistry Volume: 8
www.jcmad.com Issue:1
64-71
Efficacy of Subgingival Ozone Irrigation for Management of Chronic
Periodontitis – A Clinical, Microbiological and Biochemical study
Thayyil Sivaraman Hrishi 1, Pratibha Pandurang Kundapur 2, Giliyar Subraya Bhat 3,
Shashidhar Vishwanath 4, Shoba Kamath5
1. Assistant Professor, Department of Periodontology, Government Dental College, Calicut
2. Professor and Head, Department of Periodontology Manipal College of Dental Sciences, Manipal, Karnataka
3. Professor, Department of Periodontology Manipal College of Dental Sciences, Manipal, Karnataka
4. Associate Professor, Department of Microbiology, Kasturba Medical College, Manipal, Karnataka
5. Professor, Department of Biochemistry, Kasturba Medical College, Manipal, Karnataka
Abstract
Purpose: Ozone, both gaseous and aqueous forms, is gaining significance among the dental fraternity as a
possible alternative oral antiseptic agent. It is strongly antimicrobial and does not induce microbial resistance.
The purpose of the present study was to evaluate the efficacy of subgingival irrigation of ozonated water as an
adjunct to scaling and root planing (SRP) compared to SRP alone in the management of mild to moderate
periodontitis patients. Methods and Material: The study was a randomized controlled trial; sixty patients were
allocated to two groups, the ozone group (test group) and the scaling group (control group). All patients were
subjected to scaling and root planing (SRP) in a single visit followed by irrigation with ozone water in the test
group and distilled water in the control group at baseline and 14 days. The clinical parameters of Gingival Index
(GI), Plaque Index (PI), percentage of sites with bleeding on probing (BOP), probing depth (PD) and clinical
attachment level (CAL), total microbiologic count, differential microbial count of Porphyromonas spp.,
Fusobacterium spp., Prevotella spp. &Veillonella spp., and biochemical parameter of total antioxidant capacity
(TAOC) in gingival crevicular fluid (GCF) were recorded at baseline and after 6 weeks. Results: Statistically
significant improvements in clinical, microbiological and biochemical parameters were observed in both groups
following therapy. At 6 weeks it was observed that adjunctive ozone irrigation resulted in significant reductions
in GI, BOP, CAL and total microbial count compared to scaling and adjunctive distilled water irrigation while the
changes in PI and antioxidant levels did not reach statistical significance. Conclusions: The adjunctive use of
subgingival irrigation ozonated water showed promising short-term results.
Keywords: Ozone, Periodontitis, antimicrobial, subgingival irrigation, non-surgical therapy
Address for correspondence: Dr. Thayyil Sivaraman Hrishi, Assistant Professor, Department of Periodontology,
Government Dental College Calicut, Kerala, India- Phone- 9846772531 Email- hrishisivram@hotmail.com
Date of Acceptance: 23/04/2020
response to these accumulations. [1] Therefore,
Introduction removal and control of microbial deposits is
critical for successful periodontal therapy.
Periodontitis is an inflammatory disease
Clinical evidence shows that plaque control
affecting the supporting tissues of the teeth. It is
combined with scaling and root planning is
caused by specific microflora leading to
effective as a therapeutic modality for arresting
destruction of the periodontal ligament and
periodontitis, but certain factors can limit the
alveolar bone. The pathophysiology of
effectiveness of scaling and root planning, for
periodontal disease is related to microbial
example, deep developmental grooves,
plaque which accumulate on teeth and host’s
furcations, operator skills, tortuous pockets,
J Cont Med A Dent Jan-Apr2020 Volume 8 Issue 1 64
Thayyil S Hrishi et al; Subgingival Ozone Irrigation in Management of Chronic Periodontitis
osseous defects etc.[2] Hence, use of adjunctive Materials and Methods
modalities like local and systemic
chemotherapeutics,[3-7]host modulatory The present study followed a randomized
agents,[8,9] lasers [10,11] and photodynamic controlled clinical trial design. A total of one
therapy[12] has been advocated to overcome hundred twenty four patients within the age
these limitations. Chemotherapeutics can be group of 18 to 60 years of both sexes reporting
delivered to the periodontal pockets in many to the Department of Periodontology were
ways such as irrigation, mouth rinses, fibers, screened for eligibility for participation in the
membranes, gels, chips etc.[13] Irrigation (supra study. Out of these, sixty patients having at least
and subgingival irrigation) has the potential to 6 sites with probing pocket depth of >4mm with
be a cost effective method that can be used by Clinical Attachment Loss (CAL) of 1 - 2 mm
clinicians and patients to help suppress bacterial (mild periodontitis) or CAL of 3 – 4mm
etiologic agents causing periodontitis.[14]The (moderate periodontitis) were included in the
biologic rationale for performing supra and study. [21] Patients who had undergone any
subgingival irrigation is to nonspecifically surgical or non-surgical periodontal therapy in
reduce microbial deposits and count the past 6 months or patients with Diabetes
respectively, thereby reducing the pocket mellitus, Rheumatoid arthritis, Osteoporosis and
microflora to prevent initiation of periodontitis bleeding disorders, pregnant and lactating
or to facilitate its reduction [15] The conventional women, smokers and patients with less than 20
antimicrobial or antiseptic agents may allow for teeth or history of use of antibiotics, anti-
development of bacterial resistance following inflammatory agents and any chemotherapeutics
long term use.[16] Presently, ozone, O3 is in the past 3 months were excluded from the
contemplated as a possible alternative oral study. The study design and purpose was
antiseptic agent owing to its strong explained to the patients and a written consent
antimicrobial property and incidence of no was obtained. Ethical approval for the study was
microbial resistance. Evidence has shown that obtained from the Hospital Ethics Committee.
both aqueous and gaseous forms of ozone are Subjects were randomly divided into two
detrimental to oral pathogens. [17, 18] Ozonated groups, the test group and control group, with
water (0.5-4 mg/L) was found to be highly 30 subjects in each group. Patients in test group
effective in killing both gram-positive and received scaling and root planing in a single
gram-negative microorganisms. Even lower visit using ‘EMS Piezon Master 150’ ultrasonic
concentrations of ozone water (0.12 to 0.19 scaler with 0.1 mg/L ozone water (produced by
mg/L) were found to be effective against “Kent ozone Dental Jet TY-820”, Kent Ro
bacteria. [19] Ozone, therefore, may have a Systems Ltd., Noida, India) (figure:1) used as
potential role in the treatment of periodontal the coolant and hand instruments (Gracey
disease. Administration of ozone into Curettes; Hu Friedy, Chicago, IL, USA).
periodontal pockets would conceivably reduce Following thispockets were irrigated with ozone
the bacterial load in periodontal pockets. Ozone water using a sterile 5 cc syringe with a blunt 21
water could either be used as a coolant in gauge needle for 3 min (figure 2). Repeated
ultrasonic scalers or as an irrigant along with irrigation ensured that irrigants filled up pockets
scaling and root planing. Clinical evidence is for a period of 3 min.In the control group,
however, limited in this area. Kshitish et al. [20] scaling and root planing was performed and
in a study used ozonated water in the treatment pockets were irrigated with distilled water using
of periodontitis patients and observed that ozone blunt 21 gauge needle. Patients were instructed
water (0.1mg/L) was effective against to brush with Modified Bass method twice daily
periodonto-pathogenic bacteria. The purpose of using a standard tooth paste and were recalled
this study is to evaluate the efficacy of ozone after 2 weeks to repeat the irrigations. During
water irrigation as an adjunct to scaling and root this visit personal plaque control of patients was
planing in improving the clinical, monitored and oral hygiene instructions were
microbiological and biochemical parameters in reinforced. Clinical, microbiological &
mild to moderate periodontitis patients. biochemical parameters were evaluated at
baseline and the sixth week.
J Cont Med A Dent Jan-Apr2020 Volume 8 Issue 1 65
Thayyil S Hrishi et al; Subgingival Ozone Irrigation in Management of Chronic Periodontitis
and gently air dried. Standardized Whatman’s
Clinical parameters
filter paper strips of dimensions 2x8 mm
Gingival Index, [22] Plaque Index[23] probing
dimensions were used, 6 strips of filter paper
pocket depth (PPD), number of teeth which bled
were placed in the pocket and atotal of 4 pockets
on probing and clinical attachment level (CAL)
were sampled. The filter paper were removed
were recorded prior to SRP and at 6 weeks
after 60 seconds and transferred to Eppendorf
recall visits. Probing depth was measured from
vials containing phosphate buffered saline
the gingival margin to the base of the pocket
(pH=7.4).
only in areas where the depth was more than
The TAOC in GCF was measured using Ferric
3mm and CAL attachment was measured from
Reducing Antioxidant Power Assay(FRAP).
the CEJ to base of the pocket using William’s
FRAP measures antioxidant reduction of ferric
periodontal probe.
tripyridyltriazine complex to intense blue
Microbiological Evaluation colored ferrous tripyridyltriazine, which is
Microbiological parameters evaluated included monitored by measuring the change in
total anaerobic bacterial count & differential absorption at 593nm.[24]
count of Porphyromonas spp., Fusobacterium
spp., Prevotella spp. &Veillonella spp. Statistical Analysis
Statistical analysis was performed by SPSS 19
Plaque samples were collected from 4 deepest
software. Shapiro Wilk test was utilized to
periodontal pocket prior to SRP. The
determine the normality of variables. The
supragingival plaque was removed from the
variables were expressed in Mean ± Std.
tooth surface using a gauze piece, tooth was
deviation. Paired t-test was used to compare the
isolated, air dried before collection. The same
variables which showed normal distribution (GI,
sites were used for sampling during final visit.
PI, CAL, PD) between baseline and follow up in
The collected samples were transported in 10 ml
both groups and the intergroup comparisons
thioglycollate broth immediately to Department
were made by independent t-test. Non-
of Microbiology and culturing was done within
parametric Wilcoxon test was used to compare
30 minutes. Neomycin Blood Agar which is a
baseline and follow up values of parameters
selective media for obligate anaerobes
which didn’t show normal distribution (BOP,
(Peptostreptococcus, Treponema,
TAOC, Total anaerobic count) and Mann-
Fusobacterium, Porphyromonas, Veillonella,
Whitney U Test was used for intergroup
and Actinomycesspecies) was used for culture.
comparisons.
The plaque samples were vortexed and serially
diluted up to 10-3 . The different dilutions i.e.,
undiluted, 1:10, 1:100 & 1:1000 were inoculated
Results
on the culture plates by means of loop. The The present study was a randomized controlled
plates were incubated in anaerobic jars with clinical trial. A total of 60 subjects including 23
GasPak™ EZ Anaerobe Container System male and 37 females were enrolled in the study.
Sachets for 5 days. Metronidazole discs were The mean age of the patients was 38.6 years.
placed on the agar plates before incubation, for
Clinical Parameters
identification of anaerobes. Specific species
The mean gingival index score showed
were recognized from colony morphology, gram
significant reduction at 6 weeks in both ozone
staining and biochemical differentiation tests
and scaling group compared to baseline values
using kanamycin 1mg, Vancomycin 5 mg,
(table 1 & 3) and intergroup comparison at 6
collistin10mg discs.
weeks showed significant mean GI reduction in
Biochemical Parameter ozone group compared to scaling group. The
Gingival crevicular fluid was collected from all mean plaque index scores showed statistically
subjects for biochemical analysis of total significant reduction in both ozone and scaling
antioxidant capacity. GCF samples were taken groups from baseline to 6 weeks follow up visits
prior to plaque collection to avoid bleeding from (table 1 & 3), but the mean reduction between
pockets during GCF collection, from same sites the groups were not significant. (table 5). The
where plaque samples were intended to be
collected. Teeth were isolated with cotton rolls
J Cont Med A Dent Jan-Apr2020 Volume 8 Issue 1 66
Thayyil S Hrishi et al; Subgingival Ozone Irrigation in Management of Chronic Periodontitis
reduction in percentage of bleeding sites were group (table 1 &3), but this change was not
statistically significant in both control and test significant between the groups (table 5). The
groups from baseline to 6 weeks (table 1 & 3). mean attachment level gain was statistically
The reduction in ozone group was statistically significant in both the groups after 6 weeks
significant than scaling group on intergroup (table 1 & 3) and Intergroup comparison showed
comparison (table 5). At 6 weeks follow up significant change in ozone group (table 5).
significant reduction in mean probing depth was
observed in both the ozone and the scaling
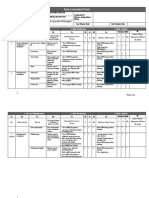
Table 1: Changes in Clinical, Microbiological & Biochemical Parameters in Ozone Group
Parameters Baseline 6 weeks Mean change P value
Gingival index† 1.73±0.14 0.84±0.18 0.89±0.14 <0.001
Plaque index† 1.62±0.20 0.97±.17 0.67±0.23 <0.001
Bleeding on probing %* 82.03±10.2 26.03±13.75 56.00±14.02 <0.001
Probing depth† 5.34±0.34 3.87±0.51 1.47±0.45 <0.001
Clincal attachment level† 3.43±0.54 2.04±0.60 1.39±0.36 <0.001
Totalantioxidant capacity* 237.33±74.0 307.63±40.32 70.3±68.6 <0.001
(µmol/l)
Anaerobes*(log of cfus) 6.57±0.44 5.16±0.75 1.41±0.50 <0.001
†Evaluate by Paired t test, *Evaluated by non-parametric Wilcoxon’s test.
Table 2: Reduction in Count of Different Bacterial Species (in Log Cfus) in Ozone Group
Species Prevalence Baseline 6 weeks Mean change
Porphyromonas 7(23%) 5.16±.65 4.5±0.77 0.66±0.34
Fusobacterium 10(33%) 5.49±0.1 4.14±1.22 1.34±1.25
Veillonella 12(40%) 4.88±0.68 4.37±0.59 0.51±0.41
Prevotella 9(27%) 5.02±0.61 4.11±0.70 0.91±0.29
Table 3: Comparison of Parameters at Baseline & 6 Weeks in Scaling Group
Parameter Base line 6 weeks Mean change P value
Gingival index† 1.63±.19 1.06±0.22 0.57±0.03 <0.001
Plaque index† 1.65±0.19 1.09±0.20 0.55±0.03 <0.001
Bleeding on probing %* 78.87±10.64 40.17±16.81 38.70±14.92 <0.001
Probing depth† 5.32±0.35 4.03±0.51 1.29±0.06 <0.001
Clinical attachment 3.50±0.69 2.39±0.75 0.80±0.18 <0.001
level†
Totalantioxidant 239.00±33.7 292.50±40.3 53.50±33.12 <0.001
capacity (µmol/l)*
Anaerobs* (log of 6.36±0.50 5.37±0.48 0.99±0.48 0.003
CFUs)
†Evaluated by paired t test, *Evaluated by non-parametric wilcoxon’s test
Table 4: Comparison of CFUs of Different Microorganisms at Baseline and 6 Weeks in Scaling Group
Species prevalence Baseline 6 weeks Mean change
Porphyromonas 6 (20%) 3.97±0.62 3.39±0.34 0.58±0.32
Fusobacterium 9 (30%) 5.44±0.59 4.54±0.59 0.90±0.19
Veillonella 13 (43.33%) 4.76±0.69 4.25±0.70 0.50±0.38
Prevotella 12(40 %) 5.14±0.55 4.37±0.70 0.76±0.40
J Cont Med A Dent Jan-Apr2020 Volume 8 Issue 1 67
Thayyil S Hrishi et al; Subgingival Ozone Irrigation in Management of Chronic Periodontitis
Table 5: Comparison of mean changes at 6 Weeks
Parameters Ozone Scaling Ozone v/s scaling
Gingival index† 0.89±0.14 0.57±0.03 P<0.001
Plaque index † 0.67±0.23 0.31±0.23 NS
Bleeding on probing %* 56.00±14.0 38.70±14.92 P<0.001
Pocket depth† 1.47±0.45 1.29±0.06 NS
Clinical attachment level† 1.39±0.03 0.80±0.04 P=0.006
Total antioxidant capacity * 70.3±68.6 53.50±33.12 NS
Anaerobes * 1.41±0.50 0.99±0.48 P=0.05
Porphyromonas 0.66±0.34 0.58±0.32 -
Fusobacterium 1.34±1.25 0.90±0.19 -
Veillonella 0.51±0.41 0.50±0.38 -
Prevotella 0.91±0.29 0.76±0.40 -
†Evaluated by independent t test, *Evaluated by Mann-Whitney U Test
Microbiologic Parameters the size of samples of different bacteria was not
The total anaerobic count and differential count sufficient. At follow up, the ozone group
of anaerobic bacteria was expressed in log of showed increased reduction in CFUs of
colony forming units (Log CFUs). At 6 weeks Porphyromonasspp, Fusobacterium
follow up the mean log CFUs of total anaerobic spp&Prevotellasppcompared to scaling group
bacteria showed significant reduction in both the
Biochemical Parameter
ozone and the scaling groups (figure 3 &
The total antioxidant capacity (TAOC) was
4,table1 & 3). Comparison between groups
evaluated at baseline & 6 weeks in both the
showed statistically significant reduction in the
groups. At 6 weeks, TAOC showed significant
ozone group compared to the scaling group
increase in both the groups (table 1 & 3). Even
(table 5). The differential bacterial count in both
though the mean increase in Ozone group was
the groups was expressed in log of CFUs (table
more compared to the Scaling group, intergroup
2 & 4). The changes in differential count at 6
comparison at 6 weeks showed no statistically
weeks between the various counts was
significant differences (table 5).
represented in mean differences ± Standard
deviations, p values were not calculated because
J Cont Med A Dent Jan-Apr2020 Volume 8 Issue 1 68
Thayyil S Hrishi et al; Subgingival Ozone Irrigation in Management of Chronic Periodontitis
Discussion ozone group and 0.31±0.23 in the scaling group)
was not statistically significant, this may be due
Adjunctive use of local agents with SRP has met to strict oral hygiene maintained by the patients
with moderate success. [4] Considering possible during the study period, which was evaluated
development of resistant bacteria and adverse and reinforced every 2 weeks by the examiners.
host reactions, the use of a broad-spectrum The ozone concentration used in the present
antiseptic agent with low potential for adverse study was 0.1mg/m. Kshitish& Laxman in a
reactions seems a desirable choice than topical short term comparative study of 21 days used
antibiotics. [25, 26] Ozone is an interesting the same concentration of ozone water as an
prospect because of its strong antimicrobial irrigant in the treatment of periodontitis patients.
activity and reduced risk of bacterial resistance. It was observed that irrigation with ozone water
In the present study, the efficacy of adjunctive resulted in higher percentage reduction of
subgingival irrigation of 0.1 mg/L ozone water Plaque Index (12%), Gingival Index (29%) and
with SRP was compared to SRP and adjunctive bleeding sites (26%) compared to chlorhexidine.
[20]
distilled water irrigation. Clinical, It has also been observed that ozonated water
microbiological and biochemical parameters at 0.1 ppm concentration is found to be effective
were recorded at baseline and 6 weeks. in reducing the load of 24-hour plaque bacteria
Significant improvements in clinical, but it did not eliminate them completely. [35]
microbiological and biochemical parameters The total anaerobic counts (expressed in log of
were observed in both groups following therapy. CFUs) were significantly reduced from baseline
At 6 weeks it was observed that adjunctive to 6 weeks in both the groups and the
ozone irrigation resulted in significant comparison of total anaerobic count among the
reductions in GI, BOP, CAL and Total groups showed a statistically significant
Microbial count compared to scaling and reduction in the ozone group (1.41±0.50)
adjunctive distilled water irrigation while the compared to the scaling group (0.99±0.48).
changes in PI and antioxidant levels did not These results are consistent with a study by
reach statistical significance. The improvements Ramzy et al., 2005, who noticed significant
at 6 weeks in all groups can be attributed improvements regarding bacterial count in
primarily to removal of local factors and aggressive periodontitis patients following
diseased cementum by SRP and thereby SRP& irrigation with ozone water compared to
reduction of microbial load from periodontal SRPalone.[36] The mechanism by which ozone
pockets. Various authors have reported kills bacteria is by oxidation of cell walls and
improvements in clinical [27-31]and microbiologic cytoplasmic membranes of microorganisms.
parameters following SRP.[32-34] Microorganisms will have different
The greater reduction in GI & percentage of susceptibility to ozonated water due to
bleeding sites in the ozone group can be differences in the structure of the cell walls of
attributed to the antimicrobial properties of microorganisms. After the membrane is
ozone water, which would result in resolution of damaged by oxidation, the permeability of the
inflammation in periodontal tissues by reducing membrane increases, and ozone molecules can
the pathogenic bacterial count. Nagayoshiet readily enter the cells and cause lysis. This
al.,[18]observed that ozone is highly effective action is non-specific and selective to microbial
against oral microorganisms, the viability of S. cells; it does not damage human body cells
mutans, P. gingivalis, P. endodontalis, and A. because of their major antioxidative ability.[37]
actinomycetemcomitans was found to be In the present study total antioxidant status was
significantly decreased when treated with evaluated in order to determine the oxidative
ozonated water of concentration 0.5mg/L. stress in periodontal tissue and to evaluate the
Hence it can be implied that Ozone may have effect of various treatment modalities on
antibacterial properties against gram negative oxidative stress. Oxidative stress has been
periodontopathogens like P gingivalis, implicated in the pathobiology of many human
Tannerella forsythia and Treponemadenticola diseases including periodontitis. In periodontal
which are associated with bleeding on probing. disease, the exaggerated inflammatory and
The change in plaque index (0.67±0.23 in the immune response to the presence of specific
J Cont Med A Dent Jan-Apr2020 Volume 8 Issue 1 69
Thayyil S Hrishi et al; Subgingival Ozone Irrigation in Management of Chronic Periodontitis
periodontal pathogens results in elevated levels antioxidant concentrations. Supplemental
of local neutrophil-derived degradative estimation of the pro-oxidant levels would have
enzymes, circulating cytokines and C-reactive been more ideal.
protein (CRP). Binding of bacteria directly or
indirectly by the surface receptors, such as Toll- Conclusion
like receptors [TLR] and Fcγ-receptors of
In the present study, it was observed that the
neutrophils, triggers phagocytosis and
adjunctive use of subgingival irrigation of 0.1
superoxide radical formation which may
ppm ozone produced significant improvement in
subsequently be converted to hydrogen peroxide
clinical and microbiological parameters in
and highly reactive hydroxyl radicals.[38]Hence
periodontitis patients. Within the limits of the
in periodontitis the balance between pro-
study, we can conclude that subgingival ozone
oxidants and antioxidants is disturbed with more irrigation can be effectively used as an
production of reactive oxygen species resulting
adjunctive therapy for management of
in destruction of host tissue.[39] The antioxidant
periodontal disease. It may be likely that the use
defense system scavenges the increased ROS
of ozonated water as a coolant along with
and in this process the antioxidant levels are
ultrasonic scalers, instead of distilled water,
depleted. Similarly a reduction in oxidative
would provide substantial therapeutic benefits,
stress restores the antioxidant levels
especially in those patients for whom surgical
representing the healthy state of tissue. Based on
therapy may not be a feasible option.
this concept many authors have suggested that
antioxidant levels and pro-oxidant levels in GCF References
can be utilized as biomarkers of periodontal
disease.[40] 1. Hinrichs J, Kotsakis G. “Classification of Diseases
In the present study, the total antioxidant levels and Conditions Affecting the Periodontium” In:
Newman M, Takei H, Klokkevold P, Carranza F.
increased significantly in all groups from Clinical Periodontology, 2014, Chapter 3, 12th
baseline to 6weeks follow up which is in Edition published by Elsevier, pp 45-67
accordance to various studies that have 2. Lowenguth RA, Greenstein G. Clinical and
demonstrated improvement in total antioxidant microbiological response to nonsurgical mechanical
levels in GCF following non-surgical periodontal therapy. Periodontol 2000; 1995; 9:14-
periodontal therapy.[40, 41] Intergroup comparison 22.
3. Goodson JM, Offenbacher S, Farr DH, Hogan PE.
among the groups demonstrated that the ozone
Periodontal disease treatment by local drug delivery.
group showed slight improvement over the JPeriodontol1985;56:265-72
scaling group but these changes were not 4. Greenstein G, Polson A. The role of local drug
statistically significant. The improvement in delivery in the management of periodontal diseases:
TAOC levels is likely due to the reduction in a comprehensive review. J Periodontol1998;69:507-
oxidative stress in periodontal tissues following 20
non-surgical therapy which indirectly results 5. Greenstein G. Local drug delivery in the treatment
of periodontal diseases: assessing the clinical
from reduction in the microbial load. The significance of the results. JPeriodontol.
additional improvement in the ozone can be due 2006;77:565-78
to the additional antimicrobial effect when used 6. Haffajee AD, Socransky SS, Gunsolley JC.
as an adjunct to SRP. The present study was Systemic anti-infective periodontal therapy. A
carried out as a short term clinical trial to systematic review. Ann Periodontol2003;8;115–181
evaluate the effect of adjunctive ozone irrigation 7. Slot J, Rams T E. Antibiotics in periodontal therapy:
advantages and disadvantages. J. Clin. Periodontol
in treating mild to moderate periodontitis and 1990; 17:479–493.
our results should be confirmed by long term 8. Preshaw PM. Host response modulation in
follow up studies. Although, microbial culture is periodontics. Periodontol 2000 2008;48:92–110
considered as the gold standard, it cannot detect 9. Giannobile WV. Host-Response Therapeutics for
non-viable organisms. Therefore, newer Periodontal Diseases. J Periodontol 2008; 79:1592–
diagnostic methods like PCR would have been a 1600.
10. Walsh L. The current status of laser applications in
better choice for consideration of the non-viable
dentistry. Aust Dent J 2003; 48:146–155.
organisms killed during sampling. Oxidative 11. Ishikawa I, Aoki A, Takasaki AA, Mizutani K,
stress was determined indirectly, in terms of Sasaki KM, Izumi Y. Application of lasers in
J Cont Med A Dent Jan-Apr2020 Volume 8 Issue 1 70
Thayyil S Hrishi et al; Subgingival Ozone Irrigation in Management of Chronic Periodontitis
12. periodontics: true innovation or myth? Periodontol periodontal therapy: Mean probing depth probing
2000 2009; 50: 90–126. attachment levels and recession changes. J.
13. Braham P, Herron C, Street C, Darveau R. Periodontol1988;59:783-793
Antimicrobial photodynamic therapy may promote 30. Haffajee AD, Cugini, MA, Dibart S, Smith C, Kent
periodontal healing through multiple mechanisms. J RL, Socransky SS. The effect of SRP on the clinical
Periodontol 2009; 80:1790-1798. and microbiological parameters of periodontal
14. Rams TE, Slots J. Local delivery of antimicrobial diseases. J ClinPeriodontol 1997; 24: 324–334.
agents in the periodontal pocket. Periodontol 2000 31. Cobb CM Clinical significance of non-surgical
1996; 10:139–159. periodontal therapy: an evidence-based perspective
15. Hoang T, Jorgensen MG, Keim RG, Pattison AM, of scaling and root planing. J ClinPeriodontol.
Slots J. Povidone-iodine as a periodontal pocket 2002;29:6-16
disinfectant. J Periodontal Res 2003; 38:311–317. 32. Goodson JM, Haffajee AD, Socransky SS, Kent R,
16. Greenstein G. The role of supra- and subgingival Teles R, Hasturk, H et al. Control of periodontal
irrigation in the treatment of periodontal diseases. J infections: A randomized controlled trial I. The
Periodontol. 2005; 76:2015-2027. primary outcome attachment gain and pocket depth
17. Rodrigues RMJ, Gonçalves C, SoutoR, Feres-Filho reduction at treated sites. J
EJ, Uzeda M, Colombo APV. Antibiotic resistance ClinPeriodontol2012;39:526–536
profile of the subgingivalmicrobiota following 33. Mousquéegs T, Listgarten MA, Phillips RW. Effect
systemic or local tetracycline therapy. Journal of of scaling and root planing on the composition of
Clinical Periodontology 2004; 31:420–427. the human subgingival microbial flora. J Periodontal
18. Baysan A, Whiley RA, Lynch E. Antimicrobial Res 1980; 15: 144–151.
effect of a novel ozone-generating device on 34. Haffajee AD, Cugini MA, Dibart S, Smith C, Kent
microorganisms associated with primary root RL, Socransky, SS. The effect of SRP on the
carious lesions in vitro. Caries Res 2000; 34:498– clinical and microbiological parameters of
501 periodontal diseases. J ClinPeriodontol 1997;
19. Nagayoshi M, Fukuizumi T, Kitamura C, Yano J, 24:324–334.
Terashita M, Nishihara T. Efficacy of ozone on 35. Haffajee AD, Teles RP, Socransky SS. The effect of
survival and permeability of oral microorganisms. periodontal therapy on the composition of the
Oral Microbiol Immunol 2004; 19: 240–246. subgingivalmicrobiota. Periodontol 2000 2006;
20. Broadwater WT, Hoehn RC, King PH. Sensitivity of 42:219-58.
three selected bacterial species to ozone. 36. Mohamed Syed Sadatullah N, Razak FA. The
ApplMicrobiol. , 1973; 26:391-393. antimicrobial effect of 0.1 ppm ozonated water on
21. Kshitish D, Laxman VK. The use of ozonated water 24-hour plaque microorganisms in situ. Braz Oral
and 0.2% chlorhexidine in the treatment of Res 2012; 26:126-131.
periodontitis patients: a clinical and microbiologic 37. Ramzy MI, Gomaa HE, Mostafa MI, Management
study. Indian J Dent Res. 2010;21:341-348 of Aggressive Periodontitis Using Ozonized Water.
22. Armitage GC. Development of a classification Egypt. Med. J. N R C. 2005; 6:229–245.
system for periodontal diseases and conditions. Ann 38. Rojas‑Valencia MN, Research on ozone application
Periodontol 1999; 4: 1–6. as disinfectant and action mechanisms on
23. Löe H, Silness, J Periodontal disease in pregnancy. wastewater microorganisms. In: Science against
Acta Odontol Scand. 1963 21:533-551 microbial pathogens: communicating current
24. Silness J, Loe H. Periodontal disease in pregnancy. research and technological advances. Méndez‑Vilas
II. Correlation between oral hygiene and periodontal A edFormatex, p. 263, 2011
condition. Acta OdontolScand 1964; 22:121-135. 39. Allen EM, Matthews JB, O'Connor R, O'Halloran
25. Benzie Iris FF, Strain JJ. The ferric reducing ability D, Chapple IL. Periodontitis and type 2 diabetes: is
of plasma (FRAP) as a measure of “antioxidant oxidative stress the mechanistic link? Scott Med J.
power”—the FRAP assay. Anal Biochem. 2009;54: 41-47
1996;239:70–76 40. Chapple IL, Matthews JB. The role of reactive
26. Hoang T, Jorgensen MG, Keim, RG, Pattison AM, oxygen and anti-oxidant species in periodontal
Slots J. Povidone-iodine as a periodontal pocket tissue destruction. Periodontol 2000 2007;43;160-
disinfectant. J Periodontal Res 2003;38:311–317 232
27. Slots J, Ting M. Systemic antibiotics in the 41. Chapple IL, Brock GR, Milward MR Ling N,
treatment of periodontal disease. Periodontol 2000 Matthews JB. Compromised GCF total antioxidant
2002; 28:106–176. capacity in periodontitis: cause or effect? J
28. Badersten A, Nilvéus R, Egelberg J. Effect of ClinPeriodontol. 2007; 34:103-10.
nonsurgical periodontal therapy. I. Moderately 42. Akpinar A, Toker H, Ozdemir H, Bostanci V,
advanced periodontitis. J ClinPeriodontol. 1981; Aydin, H. The effects of non-surgical periodontal
8:57-72. therapy on oxidant and anti-oxidant status in
29. Kaidahl WB, Kalkwarf KL, Patii, KD, Dyer JK, smokers with chronic periodontitis. Arch Oral
Bates RE. Jr.Evaluation of four modalities of Biol2013;58:717-723
J Cont Med A Dent Jan-Apr2020 Volume 8 Issue 1 71
View publication stats
You might also like
- Periodontal Tray Application of Chlorine Dioxide Gel As An Adjunct To Scaling and Root Planing in The Treatment of Chronic PeriodontitisDocument6 pagesPeriodontal Tray Application of Chlorine Dioxide Gel As An Adjunct To Scaling and Root Planing in The Treatment of Chronic PeriodontitisPhuong ThaoNo ratings yet
- LDD in Period On TicsDocument6 pagesLDD in Period On TicsAstridNo ratings yet
- Non Surgical Management of Periapical Lesions Using Calcium HydroxideDocument6 pagesNon Surgical Management of Periapical Lesions Using Calcium HydroxideVinisha Vipin SharmaNo ratings yet
- Prevention of Peri Implantitis A Narrative Review1Document7 pagesPrevention of Peri Implantitis A Narrative Review1asdNo ratings yet
- Microorganisms 10 00337 1Document16 pagesMicroorganisms 10 00337 1Maysaa mahdiNo ratings yet
- Comparative evaluation of curcumin and chlorhexidine irrigation for chronic periodontitisDocument7 pagesComparative evaluation of curcumin and chlorhexidine irrigation for chronic periodontitissamanvi badriNo ratings yet
- 63-D22 1737 Siti Sopiatin IndonesiaDocument9 pages63-D22 1737 Siti Sopiatin Indonesiajassi pwarkNo ratings yet
- Wjoud 11 221Document5 pagesWjoud 11 221ReshmaaRajendranNo ratings yet
- Treatment Stage I-Iii J Clinic Periodontology - 2020 - Sanz - Treatment of Stage I III Periodontitis The EFP S3 Level Clinical Practice GuidelineDocument57 pagesTreatment Stage I-Iii J Clinic Periodontology - 2020 - Sanz - Treatment of Stage I III Periodontitis The EFP S3 Level Clinical Practice GuidelineSofia Zaematul ArifahNo ratings yet
- Effect of Probiotics As A Complement To Non Surgical Periodontal Therapy in Chronic Periodontitis A Systematic RevieDocument7 pagesEffect of Probiotics As A Complement To Non Surgical Periodontal Therapy in Chronic Periodontitis A Systematic RevieMohammedNo ratings yet
- Tikrit Journal For Dental Sciences 6 (2) (2018) 64-71Document8 pagesTikrit Journal For Dental Sciences 6 (2) (2018) 64-71Mudur AdamNo ratings yet
- J Clinic Periodontology - 2020 - Sanz - Treatment of Stage I III Periodontitis The EFP S3 Level Clinical Practice GuidelineDocument57 pagesJ Clinic Periodontology - 2020 - Sanz - Treatment of Stage I III Periodontitis The EFP S3 Level Clinical Practice GuidelineKeHuyDietNo ratings yet
- Treatment Trends in PeriodonticsDocument8 pagesTreatment Trends in Periodonticspatricia sotoNo ratings yet
- Jctres07202105003 EpubDocument18 pagesJctres07202105003 Epubسامر مضحيNo ratings yet
- Effect of Fixed: Orthodontic Treatment On Salivary Flow, PH and Microbial CountDocument5 pagesEffect of Fixed: Orthodontic Treatment On Salivary Flow, PH and Microbial CountAndré FonsecaNo ratings yet
- Treatment of Stage I-III Periodontitis-The EFP S3 Level Clinical Practice GuidelineDocument57 pagesTreatment of Stage I-III Periodontitis-The EFP S3 Level Clinical Practice GuidelinePaulina Müller100% (1)
- Int J Dental Hygiene - 2023 - Tahery - Microbiological Status at Intake in Relation To Clinical Periodontal Status atDocument12 pagesInt J Dental Hygiene - 2023 - Tahery - Microbiological Status at Intake in Relation To Clinical Periodontal Status atmisulica2010No ratings yet
- Propolis Chronic PeriodontitisDocument11 pagesPropolis Chronic PeriodontitisZoita MandilaNo ratings yet
- Herrera 2012 at BDocument11 pagesHerrera 2012 at BOfara PachecoNo ratings yet
- Comparative Evaluation of Chlorhexidine and Hydrogen Peroxide Mouth Wash Among Patients With GingivitisDocument5 pagesComparative Evaluation of Chlorhexidine and Hydrogen Peroxide Mouth Wash Among Patients With GingivitisInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- 18 - Clinical, Inflammatory and Microbiological Outcomes of Full-Mouth Scaling With Adjunctive Glycine Powder Air-Polishing - A Randomized TrialDocument25 pages18 - Clinical, Inflammatory and Microbiological Outcomes of Full-Mouth Scaling With Adjunctive Glycine Powder Air-Polishing - A Randomized TrialPietro SanzNo ratings yet
- Management of Deep Carious LesionsFrom EverandManagement of Deep Carious LesionsFalk SchwendickeNo ratings yet
- Desarrollo 15Document11 pagesDesarrollo 15SofiaNo ratings yet
- 11th JC - SINDHUDocument22 pages11th JC - SINDHUDadi SindhuNo ratings yet
- Pathogens: Microbial Etiology and Prevention of Dental Caries: Exploiting Natural Products To Inhibit Cariogenic BiofilmsDocument15 pagesPathogens: Microbial Etiology and Prevention of Dental Caries: Exploiting Natural Products To Inhibit Cariogenic BiofilmsGinoNo ratings yet
- 1 s2.0 S1882761618300085 Main PDFDocument8 pages1 s2.0 S1882761618300085 Main PDFIonela MadalinaNo ratings yet
- Evidence-Based Strategy For Dental Biofilms: Current Evidence of Mouthwashes On Dental Biofilm and GingivitisDocument8 pagesEvidence-Based Strategy For Dental Biofilms: Current Evidence of Mouthwashes On Dental Biofilm and GingivitisIonela MadalinaNo ratings yet
- Art. 1.2Document8 pagesArt. 1.2laura ojedaNo ratings yet
- Efectele IrigatieiDocument9 pagesEfectele IrigatieiKlaudynhooq JaudyNo ratings yet
- 04 Ravneet KRandhawapolishingDocument9 pages04 Ravneet KRandhawapolishingLatifa Hanif ZuhriNo ratings yet
- Hyaluronic Acid: A New Approach For The Treatment of Gingival Recession-A Systematic ReviewDocument11 pagesHyaluronic Acid: A New Approach For The Treatment of Gingival Recession-A Systematic ReviewGali Alfaro ZagalNo ratings yet
- Non-Surgical Treatment of Chronic PeriodontitisDocument4 pagesNon-Surgical Treatment of Chronic PeriodontitisEmaNo ratings yet
- The Microbial Changes in Subgingival Plaques of Orthodontic Patients: A Systematic Review and Meta-Analysis of Clinical TrialsDocument10 pagesThe Microbial Changes in Subgingival Plaques of Orthodontic Patients: A Systematic Review and Meta-Analysis of Clinical TrialsRaji MurthyNo ratings yet
- Ar Weiler 2017Document16 pagesAr Weiler 2017Alfredo LunaNo ratings yet
- Intracanal - Medication PROPOSAL-2Document9 pagesIntracanal - Medication PROPOSAL-2khaled.s.alformNo ratings yet
- 2922 ArticleText 12555 1 10 20221211Document11 pages2922 ArticleText 12555 1 10 20221211garciadeluisaNo ratings yet
- Plants: Effect of Propolis Paste and Mouthwash Formulation On Healing After Teeth Extraction in Periodontal DiseaseDocument12 pagesPlants: Effect of Propolis Paste and Mouthwash Formulation On Healing After Teeth Extraction in Periodontal DiseaseSalsabila Tri YunitaNo ratings yet
- Journal Homepage: - : IntroductionDocument6 pagesJournal Homepage: - : IntroductionIJAR JOURNALNo ratings yet
- Antibiotics 11 00118Document13 pagesAntibiotics 11 00118ruxandra.lipanNo ratings yet
- Estado Periodontal AlineadoresDocument7 pagesEstado Periodontal AlineadoresCLAUDIA PATRICIA ROSALES BASANTENo ratings yet
- ArtigoDocument10 pagesArtigoRuanPabloNo ratings yet
- Supportive Periodontal Therapy: Maintaining Oral HealthDocument8 pagesSupportive Periodontal Therapy: Maintaining Oral HealthAlaghen VespanathanNo ratings yet
- Efficacy of Xanthan Based Chlorhexidine Gel As AnDocument5 pagesEfficacy of Xanthan Based Chlorhexidine Gel As AnMai ThúyNo ratings yet
- Eksperimental 2021Document8 pagesEksperimental 2021Putri NurhadizahNo ratings yet
- 7 DB 6Document6 pages7 DB 6AamirNo ratings yet
- Dehghan IDocument7 pagesDehghan IincisivusNo ratings yet
- MainDocument5 pagesMainRaji MurthyNo ratings yet
- Acta Odontologica Scandinavica: Shweta Sharda, Arpit Gupta, Ashima Goyal & Krishan GaubaDocument17 pagesActa Odontologica Scandinavica: Shweta Sharda, Arpit Gupta, Ashima Goyal & Krishan GaubaAnonymous tIwg2AyNo ratings yet
- MainDocument5 pagesMainRaji MurthyNo ratings yet
- Chen 2012Document8 pagesChen 2012Hamza GaaloulNo ratings yet
- Administration of Systemic Antibiotics During Non-Surgical Periodontal Therapy - A Consensus ReportDocument13 pagesAdministration of Systemic Antibiotics During Non-Surgical Periodontal Therapy - A Consensus ReportRizki Yuli amandaNo ratings yet
- 41 ST JC - SindhuDocument8 pages41 ST JC - SindhuDadi SindhuNo ratings yet
- 3 - Pone 0128657Document20 pages3 - Pone 0128657ingarionNo ratings yet
- Malondialdehyde As A Marker of Oxidative Stress in Periodontitis PatientsDocument6 pagesMalondialdehyde As A Marker of Oxidative Stress in Periodontitis PatientsRimaNo ratings yet
- Evaluation of Effects of 1.2% Atorvastatin As A Local Drug Delivery: A Randomized Controlled Clinical StudyDocument8 pagesEvaluation of Effects of 1.2% Atorvastatin As A Local Drug Delivery: A Randomized Controlled Clinical StudyIJAR JOURNALNo ratings yet
- JIAP October 2020 - Comparative Evaluation of Chitosan Chlorhexidine Mouthwash in Plaque Control - A Preliminary Randomized Controlled Clinical TrialDocument8 pagesJIAP October 2020 - Comparative Evaluation of Chitosan Chlorhexidine Mouthwash in Plaque Control - A Preliminary Randomized Controlled Clinical TrialANUMULA MANASANo ratings yet
- Clinically Proven Herbal Toothpaste in Sri LankaDocument7 pagesClinically Proven Herbal Toothpaste in Sri LankaYoga ChanNo ratings yet
- Journal of Prosthodontic Research: Yuya Baba, Yusuke Sato, Gaku Owada, Shunsuke MinakuchiDocument6 pagesJournal of Prosthodontic Research: Yuya Baba, Yusuke Sato, Gaku Owada, Shunsuke MinakuchiSayed RustiaNo ratings yet
- Polak Et Al-2015-Journal of Clinical Periodontology PDFDocument13 pagesPolak Et Al-2015-Journal of Clinical Periodontology PDFChristine HacheNo ratings yet
- AnalgesicsDocument14 pagesAnalgesicsسامر مضحيNo ratings yet
- 11IJDEJul Sep2017Document45 pages11IJDEJul Sep2017Yady S. Londoño L.No ratings yet
- Jctres07202105003 EpubDocument18 pagesJctres07202105003 Epubسامر مضحيNo ratings yet
- Jurnal Kedokteran GigiDocument7 pagesJurnal Kedokteran GigiMochamad Haldi Tri HutamaNo ratings yet
- JCDR 9 ZC29Document5 pagesJCDR 9 ZC29سامر مضحيNo ratings yet
- MAPEH 6- WEEK 1 ActivitiesDocument4 pagesMAPEH 6- WEEK 1 ActivitiesCatherine Renante100% (2)
- Lim Meng Heck (SR - Operation Manager) : ISK Ssessment ORMDocument2 pagesLim Meng Heck (SR - Operation Manager) : ISK Ssessment ORMVaradaraju ThirunavukkarasanNo ratings yet
- [1479683X - European Journal of Endocrinology] Management of Graves' hyperthyroidism in pregnancy_ focus on both maternal and foetal thyroid function, and caution against surgical thyroidectomy in pregnancyDocument8 pages[1479683X - European Journal of Endocrinology] Management of Graves' hyperthyroidism in pregnancy_ focus on both maternal and foetal thyroid function, and caution against surgical thyroidectomy in pregnancyClaudia IrimieNo ratings yet
- ARBR 2806 Edit ReportDocument5 pagesARBR 2806 Edit ReportJosé Manuel Valencia GallardoNo ratings yet
- Ibm India Benefits - Covid-19 Help Line & Doctor Tele-ConsultationDocument4 pagesIbm India Benefits - Covid-19 Help Line & Doctor Tele-ConsultationSushovan NandiNo ratings yet
- Ectopic PregnancyDocument54 pagesEctopic Pregnancypatriciaatan1497No ratings yet
- NCP-Deficient Fluid VolumeDocument1 pageNCP-Deficient Fluid Volumejanmichael8No ratings yet
- Higado Graso No Alcoholico y Niveles de PCRDocument6 pagesHigado Graso No Alcoholico y Niveles de PCRperuliz19No ratings yet
- Metformin Use in Polycystic Ovary Syndrome (PCOS)Document2 pagesMetformin Use in Polycystic Ovary Syndrome (PCOS)matasatuNo ratings yet
- Stress Management Strategies: Individual Approaches Organizational ApproachesDocument13 pagesStress Management Strategies: Individual Approaches Organizational ApproachesYakshit GoelNo ratings yet
- Shatavari - Benefits, Precautions and DosageDocument13 pagesShatavari - Benefits, Precautions and Dosagenvenkatesh485No ratings yet
- No. Nama Penyakit Kode Dan Nama Diagnosa ICD 10Document16 pagesNo. Nama Penyakit Kode Dan Nama Diagnosa ICD 10Sari Eka RahayuNo ratings yet
- Case Write Up - Dengue FeverDocument22 pagesCase Write Up - Dengue FevervijayaNo ratings yet
- Abnormal Psychology Beidel 3rd Edition Test BankDocument4 pagesAbnormal Psychology Beidel 3rd Edition Test BankChuck Simmons100% (25)
- AWWA M3 Safety Mangement For Utilities 7th Ed 2014Document164 pagesAWWA M3 Safety Mangement For Utilities 7th Ed 2014Harold Fernando Guavita ReyesNo ratings yet
- Gym PlanDocument56 pagesGym PlanAlize Ch0% (1)
- Browne2018-A Guide To Policy Analysis As A Research MethodDocument14 pagesBrowne2018-A Guide To Policy Analysis As A Research MethodIzza Dinalhaque PranatasariNo ratings yet
- BPH treatment options and assessmentDocument7 pagesBPH treatment options and assessmentVon BellosilloNo ratings yet
- Diabetes Type 2 BasicsDocument44 pagesDiabetes Type 2 BasicsMasunji EmanuelNo ratings yet
- Flowchart For Drug Surrender: Pnp/PdeaDocument2 pagesFlowchart For Drug Surrender: Pnp/PdeaLuppo PcaduNo ratings yet
- SterileProcessing SkillschecklistDocument2 pagesSterileProcessing SkillschecklistJose TiradoNo ratings yet
- Fibroids (Uterine Myomas) - ClinicalKeyDocument25 pagesFibroids (Uterine Myomas) - ClinicalKeyfebri febiNo ratings yet
- Internship ReportDocument15 pagesInternship Reportpreethi balakrishnanNo ratings yet
- Reading Unit 3Document2 pagesReading Unit 3estefania aranda jimenezNo ratings yet
- Evidence Based Chinese Medicine HypertensionDocument13 pagesEvidence Based Chinese Medicine Hypertensionpranaji100% (2)
- Population Trends in INDIADocument8 pagesPopulation Trends in INDIAcheedikrishnaNo ratings yet
- Actividad Unidad 1 Ingles IDocument4 pagesActividad Unidad 1 Ingles Iyohi100% (3)
- Self-Injection Classes: Empowering Patients and Decreasing Nursing WorkloadDocument5 pagesSelf-Injection Classes: Empowering Patients and Decreasing Nursing WorkloadIlvita MayasariNo ratings yet
- ECardDocument2 pagesECardsivaNo ratings yet
- Sample: Georgia Department of Public HealthDocument1 pageSample: Georgia Department of Public HealthWSB-TV Assignment DeskNo ratings yet

































































![[1479683X - European Journal of Endocrinology] Management of Graves' hyperthyroidism in pregnancy_ focus on both maternal and foetal thyroid function, and caution against surgical thyroidectomy in pregnancy](https://imgv2-1-f.scribdassets.com/img/document/552054434/149x198/0ad7f435ea/1710545307?v=1)


























