Professional Documents
Culture Documents
Hyperchloremic Acidosis Pathophysiology and Clinical Impact
Hyperchloremic Acidosis Pathophysiology and Clinical Impact
Uploaded by
Andri PurbiantoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hyperchloremic Acidosis Pathophysiology and Clinical Impact
Hyperchloremic Acidosis Pathophysiology and Clinical Impact
Uploaded by
Andri PurbiantoCopyright:
Available Formats
)
1778428x, 2003, 4, Downloaded from https://onlinelibrary.wiley.com/doi/10.1111/j.1778-428X.2003.tb00184.x by Nat Prov Indonesia, Wiley Online Library on [05/02/2023]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
TATM 2003;5(4):424-430
Hyperchloremic Acidosis:
(
Pathophysiology and
Clinical Impact
SUMMARY
Hyperchloremic acidosis is a predictable consequence of normal
saline-based fluid administration.The theoretical basis for this
E DWARD B URDETT, MA , MB BS , MRCP, 1
ANTONY M. ROCHE, MB ChB, FRCA, MMed (Anaes),1 is easily understood using Stewart’s model of acid-base
M ICHAEL G. M YTHEN , MB BS , FRCA , MD 2
homeostasis. Data are emerging which describe the consequences
RESEARCH FELLOW
1
of hyperchloremic acidosis in the surgical population.
UCL CENTRE FOR ANAESTHESIA
MIDDLESEX HOSPITAL
2
PORTEX PROFESSOR OF ANAESTHESIA AND CRITICAL CARE
UNIVERSITY COLLEGE LONDON
HEAD OF THE PORTEX ANAESTHESIA
INTENSIVE CARE AND RESPIRATORY UNIT
INSTITUTE OF CHILD HEALTH
UCL CENTRE FOR ANAESTHESIA • Hyperchloremic acidosis
MIDDLESEX HOSPITAL
• Fluid resuscitation
LONDON, UNITED KINGDOM
• Colloids
• Crystalloids
• Volume replacement
Transfusion Alternatives in Transfusion Medicine 424 ) VOLUME 5 NUMBER 4 OCTOBER 2003
( Page
1778428x, 2003, 4, Downloaded from https://onlinelibrary.wiley.com/doi/10.1111/j.1778-428X.2003.tb00184.x by Nat Prov Indonesia, Wiley Online Library on [05/02/2023]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
Hyperchloremic Acidosis: Pathophysiology and Clinical Impact E D WA R D B U R D E T T et al.
Hyperchloremic acidosis is a well-recognized entity, pertinent Note units of measurement:
to many areas of clinical practice. It is observed in diabetic HCO3- = mmol/L
ketoacidosis, and in some forms of renal tubular acidosis;1 it is pCO2 = kPa
also an important consequence of large-volume administration of From this, one can observe that any increase in pCO2 or decrease
some intravenous fluids.2 in bicarbonate would lead to a reduction in the pH, likely to be
Most hospital clinicians routinely administer large volumes of respiratory and metabolic acidosis respectively (depending on the
intravenous fluids, to support the circulation during significant primary disturbance and compensation). Conversely, when these
fluid shifts. Normal saline (0.9% sodium chloride solution), and variables display a rise in bicarbonate or a reduction in pCO2, one
colloids suspended in normal saline, are often infused because would find metabolic and respiratory alkaloses, respectively.
they are easily available, and are isotonic with plasma. Their non-
physiological levels of chloride and lack of buffer cause metabolic Base Excess
acidosis.2
The use of base excess was introduced to assist the quantification
The term “dilutional acidosis” has been used to describe this
of the metabolic components of acid-base disturbances. The most
effect; the term implying that plasma expansion and dilutional
notable developments in quantifying these were by Siggaard-
reduction of plasma bicarbonate are the underlying mechanisms.
Andersen and Severinghaus.3,4 Base excess quantifies the severity
This is not the whole story. More elegant, the Stewart model
of metabolic acidosis or alkalosis, and is defined as the amount
emphasizes the importance of hyperchloremia in reducing the
of base (or acid) that must be added to a sample of whole blood
strong-ion difference, with the consequent impairment of
in vitro in order to restore the pH of the sample to 7.40 (keeping
homeostatic mechanisms, including coagulation abnormalities
the pCO2 constant at 5.3 kPa).5
and renal hypoperfusion.
The value ranges from –30 to +30 mmol/L, with the normal
range being –2 to +2 mmol/L. Its measurement requires only a
small venous or arterial blood sample, and it is widely used in
Pathophysiology clinical practice. It has been established as an accurate indicator
of the metabolic component to any acid-base disturbance. Indeed,
Debate continues about the exact mechanism for acid-base
base excess derangement is an independent predictor of mortality
homeostasis in humans. The two main camps in the dispute follow
in critically ill patients.6
either the original Henderson-Hasselbalch and Siggaard-Andersen
Traditionally, it was suggested that pH is kept within a tight
line of thinking, or the more recent Stewart approach to acid-base
range by the body’s ability to buffer acid, using bicarbonate, plasma
physiology. Below, a brief overview of the original approach will
proteins and hemoglobin.
be covered, followed by a more in depth view of the Stewart theory
and its modifications.
Physicochemical Theory
pH is a logarithmic scale of the reciprocal of H+ ion
concentration. Both respiratory (e.g., CO2 tension) and metabolic How does a change in chloride concentration bring about such
factors (e.g., lactic acid) affect H+.3 Classically, decisions based on profound alteration in acid-base equilibrium? The answer is not
blood gas analysis are based on the apparent pH, in relation to obvious when analyzed using the Henderson-Hasselbalch
the pCO2 (carbon dioxide tension), further assisted by the equation. However, it can be explained by Stewart's method of
bicarbonate concentration (HCO3-) and base excess variables, can analysis of quantitative acid and base chemistry. Stewart turned
assess whether derangements are likely to be metabolic or the whole world of acid-base homeostasis upside down in the late
respiratory in origin. 1970s and early 1980s, when he published his mathematical
The first principle applied to acid-base physiology is as follows: theory of the body’s ability to regulate acid and base content.7,8
if the pCO2 rises, so too does the eventual H+ ion concentration. Stewart's approach shows the way to understanding plasma as a
This is due to the formation of carbonic acid by the combination physico-chemical system, and provides a basis for quantitative
of water and carbon dioxide. Carbonic acid then dissociates to analysis and rational manipulation of acid-base state, in vivo and
form H+ and HCO3-. It is a cornerstone to understanding the way in vitro.9
in which the body creates and handles acid. The Stewart theory rests on two important physicochemical
H20 + CO2 <—> H2CO2 <—> H+ + HCO3- principles, which describe the behavior of ions in fluids. Firstly,
all positively charged and all negatively charged ions in a solution
This was modified, originally by Henderson, then further by
must always be equal, the law of electro-neutrality. What this
Hasselbalch, into:
implies is that the sum of all positively and all negatively charged
The Henderson-Hasselbalch Equation
ions in a solution must equal zero. The second principle is the
pH = pK + log (HCO3-/pCO2 x 0.225)
conservation of mass, which means that the total amount of a
substance remains constant, unless it is added to or generated, or
Transfusion Alternatives in Transfusion Medicine 425 ) VOLUME 5 NUMBER 4 OCTOBER 2003
( Page
1778428x, 2003, 4, Downloaded from https://onlinelibrary.wiley.com/doi/10.1111/j.1778-428X.2003.tb00184.x by Nat Prov Indonesia, Wiley Online Library on [05/02/2023]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
Hyperchloremic Acidosis: Pathophysiology and Clinical Impact E D WA R D B U R D E T T et al.
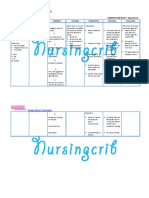
Table 1. In plasma, when all the strong ions
mentioned above, both anions and cations,
Electrolyte Hartmann’s Solution 0.9% NaCl Plasma Concentration
are added together, the result does not end
Sodium 131 154 135 - 146
up as zero. This accounts for what is known
Chloride 111 154 98 - 102 as the strong ion difference. Weak acids, for
Potassium 5 0 3.5 - 5.0 example, have not been taken into account in
Calcium 2 0 2.20 - 2.67 the equation. Stewart originally described the
Magnesium 0 0 0.7 - 1.1 equation as follows:
Phosphate 0 0 0.8 - 1.5
(Na+ + K+) – (Cl- + Lactate) = SID
Bicarbonate/lactate 27 0 22 - 30
The SID is determined by the charge of the
All values quoted are electrolyte concentration in mmol/L.
ions as well as the quantity; in healthy
volunteers it usually equals approximately 40-
49 milliequivalents per liter, and can therefore
removed or destroyed. Furthermore, the body is composed of 65- be affected by changes in plasma electrolyte concentrations. This
70% water, thereby providing an inexhaustible amount of H+ and SID, which is an independent mechanism of acid-base regulation,
OH- for bodily functions and processes.7-8,10 determines (along with CO2 and weak acids), what the plasma
According to Stewart, three main factors determine H+ ion hydrogen ion concentration will be. The electrochemical forces
concentration, namely carbon dioxide, weak acids in the body, generated by this SID determine water dissociation, hence H+ ion
and the strong ion difference. concentration required to “balance” plasma ionic charges. The net
As examined above, carbon dioxide directly affects H+ result always has to be a plasma ionic charge equal to zero
concentration by the mechanism of increasing or reducing (electrochemical neutrality). As one can see, H+ is not the driving
carbonic acid production, and thereby its dissociation into H+ and force of the reaction; it is the dependent variable, along with OH-
HCO3-. Complicating one’s understanding slightly is the body’s to a much lesser degree. To continually balance these
inexhaustible supply of H+ and OH-. Due to its dynamic nature, electrochemical forces, a decrease in H+ concentration is observed
the dissociation of water into these ions is also largely dictated by with increases in the SID, and H+ concentration increases as the
CO2 and the strong ions. This plays a further role in reactions SID decreases.8,12
observed in maintaining the acid-base and more importantly An increased plasma chloride ion concentration relative to
electrochemical neutrality. sodium and potassium concentrations will produce a smaller
Stewart’s second principle is that of weak acids (or weak plasma strong ion difference, leading to an increased hydrogen
electrolytes), which are acids or electrolytes in the body that are only ion concentration, and therefore acidosis.
partially ionized at pH levels encountered physiologically, such as Stewart's approach relates to how sodium bicarbonate corrects
plasma proteins like albumin, and phosphates. These play a role in the metabolic acidosis. The metabolic acidosis may be corrected
the mathematical model Stewart originally described, along with CO2 not so much by its bicarbonate content but by its sodium content.
and the Strong Ion Difference (SID, described below), and hence the The increased sodium concentration resulting from bicarbonate
final H+ ion concentration. As the total weak acid drops, in isolation, therapy corrects the reduced SID toward normal, thereby
an increase can be expected in the pH. Even though weak acids are correcting the acidosis. According to Stewart, bicarbonate is a
important in acid-base regulation, and noted in certain units, they dependent variable and therefore cannot bring about a change in
are not commonly used for clinical interpretations of acid-base another dependent variable like hydrogen ion concentration.
derangements. The observation that the only clinically relevant weak More recently, the SID equation was expanded to include Ca2+
acids are inorganic phosphate and albumin was later confirmed by and Mg2+, to account for further plasma ions.10,13
Fencl’s group, noting that a charge of approximately 12 mEq/L can
(Na+ + K+ + Ca2+ + Mg2+) – (Cl- + Lactate) = SID apparent
be attributed to these acids, and that globulins play a negligible role.11
Probably the most interesting discovery in Stewart’s theory was Many approaches to the management of critical care acid-base
that of the Strong Ion Difference (SID). This principle rests on the derangements use modified Stewart approaches. Below, we
chemistry of strong ions in the body (or aqueous solutions). Strong comment on the role of this technique in explaining pH
ions (or electrolytes) are almost completely ionized in aqueous derangements commonly observed with intravenous fluid
solutions. The most notable of the strong ions are Na+, K+, Ca2+, resuscitation.
Mg2+, Cl-, and Lactate.7 At this stage, it is prudent to remember
the basis of the physicochemical approach, which is firstly that of
electrochemical neutrality being maintained at all times, and
secondly the conservation of mass.
0Transfusion Alternatives in Transfusion Medicine 426 ) VOLUME 5 NUMBER 4 OCTOBER 2003
( Page
1778428x, 2003, 4, Downloaded from https://onlinelibrary.wiley.com/doi/10.1111/j.1778-428X.2003.tb00184.x by Nat Prov Indonesia, Wiley Online Library on [05/02/2023]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
Hyperchloremic Acidosis: Pathophysiology and Clinical Impact E D WA R D B U R D E T T et al.
If the patient lost 5 L of the plasma due to hemorrhage, the
Fluid Therapy
concentration of the various ions would be the same, but the total
content would be as follows (concentration multiplied by 10 L):
Understanding the role of intravenous fluid electrolyte content
• Na+ 1400 mmol
in affecting acid-base balance in vivo, one must first take note of
• K+ 40 mmol
normal plasma electrolyte content in healthy individuals. To
• Ca2+ 20 mmol
recapitulate on the concentrations of the plasma ions, see Table 1.
• Cl- 1000 mmol
Crystalloid intravenous fluids can be divided into resuscitation
If we chose to replace this lost volume of plasma with 5 L Saline,
fluids (e.g., 0.9% Sodium Chloride, Hartmann’s Solution) and
the electrolyte load would be 770 mmol of sodium and chloride
non-resuscitation fluids (e.g., 5% Dextrose, 4% Dextrose with
each (5 L x 154 mmol/L). This would take the total plasma ionic
0.18% Sodium Chloride). The main distinction between the two
content to the following:
groups can be described by the electrolytic component (versus
• Na+ 1400 mmol + 770 mmol = 2170 mmol
dextrose) providing the osmolar load. Although not identical to
• K+ 40 mmol
human plasma, intravenous solutions with a balanced electrolyte
• Ca2+ 20 mmol
formulation (such as Hartmann’s solution) match the biochemical
• Cl- 1000 mmol + 770 mmol = 1770 mmol
composition of human plasma more closely than saline-based
This would equate into the following concentrations:
fluids.
• Na+ 145 mmol/L
Saline-based fluids are non-physiological in three ways. Firstly,
• K+ 2.7 mmol/L
the level of chloride is significantly above that of plasma (154
• Ca 2+
1.3 mmol/L
mmol, as compared to 98-102 mmol); secondly they lack several
• Cl- 118 mmol/L
electrolytes present in normal plasma, including potassium,
In calculating the SID however, charge balance demands
calcium, glucose, and magnesium. Thirdly, they lack the
milliequivalents per liter, not millimol. The normal SID in healthy
bicarbonate or bicarbonate precursor buffer necessary to maintain
volunteers is 40-49 mEq/L. Bivalent ions such as calcium and
plasma pH within normal limits. Each of these may be responsible
magnesium, therefore, count double. When these variables are
for homeostatic disruption, and in particular the metabolic acidosis
examined using the SID, we would find the following:
produced by normal-saline infusion.14
As can be seen in Table 1, there are significant differences in the (Na+ + K+ + Ca2+ + Mg2+) – (Cl- + Lactate)
electrolyte content of 0.9% Sodium Chloride (Saline, and saline = (140 + 4 + 4 + 2) – (100 + 1)
based fluids, e.g. most colloid preparations) and balanced = 151 – 101
electrolyte fluid preparations (e.g., Hartmann’s, Lactated Ringers). = 49 mEq/L (before hemorrhage and transfusion)
Saline has a supra-physiological concentration of both sodium and
and chloride. This is of less importance for longer term = (145 + 2.7 + 2.6 + 2) – (118 + 1)
maintenance infusions, but very important in fluid resuscitation = 151.7 – 119
scenarios.8,15-17 = 32.7 mEq/L (after saline resuscitation)
Illustration of this concept with a simplified mathematical model The net result would be increased water dissociation, hence the
will demonstrate the effect of fluid resuscitation with a saline- H+ concentration would increase with saline resuscitation to
based fluid versus a balanced electrolyte fluid (Hartmann’s). Let’s maintain electrochemical neutrality. A fall in the pH would result.
consider an adult patient, with plasma electrolyte contents as This is commonly observed clinically as a hyperchloremic
follows (amongst others): metabolic acidosis associated with saline fluid resuscitation.
• Na+ 140 mmol/L If we resuscitated the same patient, but this time using
• K+ 4 mmol/L Hartmann’s solution, the SID after resuscitation would be 42.7
• Ca 2+
2 mmol/L mEq/L (146.7-104), assuming the lactate would be normally
• Cl- 100 mmol/L metabolised. Remember that these are only simplified examples
If we calculate the total electrolyte content of the entire of the role of SID in acid-base management, to help with the
extracellular fluid space (electrolyte concentrations roughly understanding of the principle involved.
constant across the space), by multiplying the respective
concentrations by 15 L (an average for a 70 kg male), we would
obtain the following results: Clinical Implications
• Na+ 2100 mmol
• K+ 60 mmol
The physiological risks of hyperchloremic metabolic acidosis
• Ca2+ 30 mmol
are not clear. It is fair to question whether hyperchloremic
• Cl- 1500 mmol
metabolic acidosis is benign and self-limiting, or whether it is
Transfusion Alternatives in Transfusion Medicine 427 ) VOLUME 5 NUMBER 4 OCTOBER 2003
( Page
1778428x, 2003, 4, Downloaded from https://onlinelibrary.wiley.com/doi/10.1111/j.1778-428X.2003.tb00184.x by Nat Prov Indonesia, Wiley Online Library on [05/02/2023]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
Hyperchloremic Acidosis: Pathophysiology and Clinical Impact E D WA R D B U R D E T T et al.
Table 2.
Summary of Clinical Trials Showing Intraoperative Estimated Blood Loss (EBL) clinically relevant. Metabolic
acidosis, whatever the etiology, can
With Balance Saline Based Fluid Administration
depress myocardial function, reduce
Trial author Fluids used Number in Patient group / op type Outcome (Balanced
cardiac output, and reduce renal
each arm compared to non-balanced)
and intestinal perfusion. Acidemia
Scheingraber16 NS/LR 12 Gynecologic Non-significant can inactivate membrane calcium
reduction in EBL channels, and inhibit the release of
McFarlane22 NS/ 15 General surgery No significant difference norepinephrine from sympathetic
plasmalyte148 nerve fibers. This may result in the
Waters18 NS/LR 33 Open AAA repair Non-significant redistribution of cardiac output
reduction in EBL away from internal organs.18
Whilst this may have little effect
Wilkes17 Hextend / Hespan 23 Surgical patients age > 60 Non-significant
on fit patients undergoing minor
increase in EBL
elective surgery, the concern is the
Martin21 Hextend / Surgical patients with Significant reduction effect of severe hyperchloremic
30
Hespan / LR EBL > 500 mL in EBL acidosis from aggressive fluid
Gan20 Hextend / Hespan 60 Surgical patients Significant reduction resuscitation in acutely ill patients
with EBL > 500 mL in EBL during major surgery, in particular
Boldt24 NS/LR 21 Abdominal cancer Non-significant reduction vascular surgery, and organ
surgery in EBL transplantation; or following
trauma or burns. After tourniquet
Takil25 NS/LR 15 Scoliosis repair Non-significant reduction
release, or in vascular surgery,
in EBL
lactate and carbonic acid load may
LR = Lactated Ringers solution; NS = Normal Saline; Hextend® is a hetastarch suspended in a balanced electrolyte formulation. be superimposed on the iatrogenic
Hespan® is a hetastarch suspended in normal saline.
hyperchloremic acidosis towards
the end of the procedure.
If an intraoperative metabolic
Table 3. acidosis becomes apparent during
fluid replacement, the clinician
Summary of Perioperative Clinical Trials Comparing Estimated Intraoperative may be misled into believing that
Urine Output (UO) With Balanced Saline Based Fluid Administration the patient is hypovolemic, or has
Trial author Fluids used Number in Patient group / op type Outcome (Balanced a surgical cause for their acidosis.
each arm compared to non-balanced) This may lead to inappropriate
Scheingraber16 NS / LR 12 Gynecologic Non-significant management, reports of which
increase in UO have been described in the clinical
setting.19 Further administration of
Waters18 NS / LR 33 Open AAA repair Non-significant
saline-based fluids will exacerbate
increase in UO
rather than relieve the problem. In
Wilkes17 Hextend / Hespan 23 Surgical patients age > 60 Significant improvement in UO this setting, a hyperchloremic
and post-op creatinine metabolic acidosis may not be
Bennett- Hextend / Hespan 50 Cardiac surgery Significant improvement in UO differentiated from lactic acidosis
Guerrero30 and post-op creatinine by the inexperienced anesthetist.
Gan20 Hextend / Hespan 60 Surgical patients No difference Below, we detail some specific
with EBL > 500 mL physiological mechanisms that
become disrupted in the presence
Boldt24 NS / LR 21 Abdominal cancer Non-significant
of hyperchloremia.
surgery decrease in UO
Takil25 NS / LR 15 Scoliosis repair Non-significant reduction Coagulation
decrease in UO
Coagulation, as any other
LR = Lactated Ringers solution; NS = Normal Saline; Hextend® is a hetastarch suspended in a balanced electrolyte formulation.
Hespan® is a hetastarch suspended in normal saline. physiologic system, has optimal
pH and electrolyte levels at which
Transfusion Alternatives in Transfusion Medicine 428 ) VOLUME 5 NUMBER 4 OCTOBER 2003
( Page
1778428x, 2003, 4, Downloaded from https://onlinelibrary.wiley.com/doi/10.1111/j.1778-428X.2003.tb00184.x by Nat Prov Indonesia, Wiley Online Library on [05/02/2023]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
Hyperchloremic Acidosis: Pathophysiology and Clinical Impact E D WA R D B U R D E T T et al.
it functions most effectively. What is less known in vivo, is the afferent arterioles at a chloride level of 110 mmol per liter, only
extent of minor to moderate acid-base and electrolyte disturbances slightly above normal plasma level.29 He suggested that a raised
on overall coagulation and hemostasis. One can assess clinical plasma chloride could increase renal sensitivity to angiotensin 2,
outcomes of coagulation or hemostatic function from a number and modulate the release of renin.
of well-conducted clinical trials of in vivo fluid therapy or Although the message is not as strong as with the coagulation
resuscitation, where balanced electrolyte formulations have been data, a number of clinical studies (Table 3) now suggest that renal
compared with saline-based fluids. indices are perturbed by normal saline infusion in the perioperative
Studies comparing saline-based versus balanced electrolyte setting. Bennett-Guerrero et al. showed a significant improvement
crystalloids or colloids have shown differences in bleeding and in urine output, serum creatinine, creatinine clearance in
coagulation, favoring reduced bleeding and less derangement of perioperative patients given balanced salt solution, when compared
coagulation function in the balanced electrolyte formulations.20,21 to a saline-based product.30 Similarly, Wilkes et al., in their elderly
Waters et al. showed a deleterious effect on hemostasis from surgical patient population, demonstrated a doubling of urine
infusion of normal saline based fluids, when compared to balanced output in their balanced fluid group, and a significant reduction
electrolyte solutions, in patients undergoing abdominal aortic in post-operative creatinine.17 Williams et al. in their healthy
aneurysm repair. Overall, the patients in the balanced fluid group volunteer study31 noted a significantly prolonged time to first
were exposed to significantly less blood products.18 urination in the group infused with 50ml per kg of normal saline
Other studies (see Table 2), underpowered for blood loss or as compared to the Ringer’s lactate group.
assessment of coagulation variables (where these have not been These trials are small, and not powered for patient outcome,
primary outcome variables), have shown no difference.16,17,22 and the overall data in this area are unclear. A recent systematic
Systematic review and meta-analysis of the available data of all review reveals a non-significant difference in intraoperative urine
randomized controlled trials investigating buffered versus non- output.32
buffered fluid therapy (cf. balanced electrolyte versus saline-based
fluids) has recently shown a significant reduction in blood loss in Other Clinical Implications
the pooled data of buffered fluids.23
Wilkes et al studied gastric tonometry in their trial, and noted a
Questions may be asked on why this should occur. Calcium
significant increase in the CO2 gap in their unbalanced group. This
may well play a role, albeit limited. Even when calcium has been
implies gastric hypoperfusion, and indeed there was a trend toward
controlled for with hemodilution with fluids in these two groups,
increased post-operative nausea and vomiting in the same group.
a difference still exists in blood coagulation as assessed by
These data tie-in well with the healthy volunteer study by Williams
thrombelastograph® analysis (TEG®, Haemoscope Corp).26 Calcium
et al. where normal saline infusion caused abdominal discomfort
does not have any further beneficial effects in enhancing blood
in significantly more volunteers than the same volume of Ringer’s
coagulation above ionized concentrations of 0.6 mmol/L.27 Further
lactate. The mechanism for this is unclear, but it might be
research will help in understanding the role of other electrolytes
hypothesized that metabolic acidosis itself causes gut hypoperfusion,
in the coagulation process.
or that chloride acts on the splanchnic vasculature in the same
vasoconstricive in the same way as on the renal arterioles.
Renal Effects
The respiratory response to perioperative intravenous fluid
Animal studies suggest that hyperchloremia causes renal administration was noted by Takil et al.25 in their study of ASA 1
vasoconstriction: Wilcox, in a canine model, has shown that renal and 2 patients undergoing scoliosis repair. They discovered a
blood flow and glomerular filtration rate are regulated by plasma significantly increased post-operative hypercarbia in their Ringer’s
chloride.28 He demonstrated that hyperchloremia produces a lactate group (44 mmHg) as compared to their normal saline group
progressive renal vasoconstriction by inhibiting the intrarenal (40 mmHg). They concluded that this hypercarbia may lead to
release of renin and angiotensin II; and a decrease in glomerular reduced opiate administration, and inadequate pain control. It is
filtration rate and renal blood flow that was independent of renal fair to hypothesize that the metabolic acidosis found in their normal
innervation, enhanced by prior salt depletion, and related to a saline group caused these patients to overbreathe in compensation
tubular reabsorption mechanism involving chloride. He went on post-operatively. The clinical effects of this are unclear.
to show that chloride-induced vasoconstriction appears specific
for the renal vessels.
Renal afferent arterioles are major regulatory sites of renal Conclusion
vascular resistance. Hansen showed that plasma chloride levels
directly affect renal afferent arteriolar tone through calcium In the field of anesthesia and perioperative medicine, it has now
activated chloride channels in the afferent arteriolar smooth muscle firmly been established that hyperchloremic metabolic acidosis is
in rabbits. He demonstrated a total occlusion of rabbit renal a predictable consequence of saline-based, non-balanced
Transfusion Alternatives in Transfusion Medicine 429 ) VOLUME 5 NUMBER 4 OCTOBER 2003
( Page
1778428x, 2003, 4, Downloaded from https://onlinelibrary.wiley.com/doi/10.1111/j.1778-428X.2003.tb00184.x by Nat Prov Indonesia, Wiley Online Library on [05/02/2023]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
Hyperchloremic Acidosis: Pathophysiology and Clinical Impact E D WA R D B U R D E T T et al.
intravenous fluid administration. Current evidence suggests that Conflicts of Interest
it is a clinically relevant and easily avoidable condition. The authors have received unrestricted educational grants
Clearly, further studies are needed to better understand the from the following: Abbott Laboratories USA; Biotime, Inc. USA;
pathophysiology and effects of hyperchloremic metabolic acidosis Fresenius UK; B Braun UK.
in acutely ill patients. We think that until such data are available,
the logical approach should be to avoid iatrogenic hyperchloremia.
Acknowledgements
This is more easily achieved if a fluid that is more normal than
The authors wish to thank Dr. Mark Hamilton for his help
“normal” saline is utilized. We advocate the use of intravenous
and background research, and Dr. Marika Davies for her patience
fluids that have a more balanced composition.
and inspiration.
R E F E R E N C E S
1. Brivet F, Bernardin M, Dormont J. [Hyperchloremic acidosis 16. Scheingraber S, Rehm M, Sehmisch C, Finsterer U. Rapid 25. Takil A, Eti Z, Irmak P, Yilmaz Gogus F. Early
in metabolic acidosis with anion gap excess. Comparison with saline infusion produces hyperchloraemic acidosis in patients postoperative respiratory acidosis after large intravascular
diabetic ketoacidosis]. Presse Med 1991;20:413-7. undergoing gynecologic surgery. Anesthesiology volume infusion of lactated ringer's solution during major
2. Burdett E, Roche T, Donnelly T, Moulding R, Mythen M. 1999;90:1265-70. spine surgery. Anesth Analg 2002;95:294-8.
Saline-based fluid resuscitation is associated with metabolic 17. Wilkes NJ, Woolf R, Mutch M, et al. The effects of balanced 26. Roche AM, James MF, Mythen MG. In vitro addition of
acidosis in surgical patients. Eur J Anaesthesiology 2003; in versus saline-based hetastarch and crystalloid solutions on calcium to saline-based intravenous fluids only partially
press. acid-base and electrolyte status and gastric mucosal perfusion compensates for TEG pictures observed during
3. Astrup P, Jorgensen K, Siggaard-Andersen O, et al. Acid- in elderly surgical patients. Anesth Analg 2001;93:811-16. haemodilution. Anesth Analg 2002;94:S73.
base metabolism: a new approach. Lancet 1960;1:1035-9. 18. Waters JH, Gottlieb A, Schoenwald P, Popovich MJ, 27. James MF, Roche AM. Dose-response relationship between
4. Severinghaus JW. Acid-base balance nomogram--a Boston- Sprung J, Nelson DR. Normal saline versus lactated Ringer's calcium and thrombelastography. Anesthesiology
Copenhagen detente. Anesthesiology 1976;45:539-41. solution for intraoperative fluid management in patients 2001;95:A185.
undergoing abdominal aortic aneurysm repair: an outcome 28. Wilcox CS. Regulation of renal blood flow by plasma
5. Siggaard-Andersen O. The pH-log pCO2 blood acid-base study. Anesth Analg 2001;93:817-22.
nomogram revisited. Scand J Lab Invest 1962;14:598-604. chloride. J Clin Invest 1983;71:726-35.
19. Parekh N. Hyperchloremic acidosis. Anesth Analg 29. Hansen PB, Jensen BL, Skott O. Chloride regulates afferent
6. Neugebauer E, Zander R. Clinical relevance of base excess 2002;95:1821.
and lactate concentration. Anasthesiol Intensivmed arteriolar contraction in response to depolarization.
Notfallmed Schmerzther 2002;37:341-2. 20. Gan TJ, Bennett-Guerrero E, Phillips-Bute B, et al. Hypertension 1998;32:1066-70.
Hextend, a physiologically balanced plasma expander for 30. Bennett-Guerrero E, Frumento RJ, Mets B, Manspeizer
7. Stewart PA. Independent and dependent variables of acid- large volume use in major surgery: a randomized phase III
base control. Respir Physiol 1978;33:9-26. HE, Hirsh AL. Impact of normal saline based versus
clinical trial. Hextend Study Group. Anesth Analg balanced-salt intravenous fluid replacement on clinical
8. Stewart PA. How to Understand Acid-Base. New York: 1999;88:992-8. outcomes: a randomized blinded clinical trial. Anesthesiology
Elsevier, 1981. 21. Martin G, Bennett-Guerrero E, Wakeling H, et al. 2001;95:A147.
9. Fencl V, Leith DE. Stewart's quantitative acid-base chemistry: A prospective, randomized comparison of 31. Williams EL, Hildebrand KL, McCormick SA, Bedel MJ.
applications in biology and medicine. Respiration Physiol thromboelastographic coagulation profile in patients The effect of intravenous lactated Ringer's solution versus
1993;91:1-16. receiving lactated Ringer's solution, 6% hetastarch in a 0.9% sodium chloride solution on serum osmolality in human
10. Stewart PA. Modern quantitative acid-base chemistry. Can J balanced-saline vehicle, or 6% hetastarch in saline during volunteers. Anesth Analg 1999;88:999-1003.
Physiol Pharmacol 1983;61:1444-61. major surgery. J Cardiothorac Vasc Anesth 2002;16:441-6.
32. Burdett E, Roche AM, Fong K, Grocott M, Mythen MG.
11. Figge J, Rossing TH, Fencl V. The role of serum proteins in 22. McFarlane C, Lee A. A comparison of Plasmalyte 148 and A systematic review of buffered versus non-buffered
acid-base equilibria. J Lab Clin Med 1991;117:453-67. 0.9% saline for intra-operative fluid replacement. perioperative fluid resuscitation and urine output.
12. Kellum JA. Determinants of blood pH in health and disease. Anaesthesia 1994;49:779-81. Anesthesiology 2002;96:A201.
Crit Care 2000;4:6-14. 23. Fong K, Roche AM, Burdett E, Mythen MG. Meta-analysis
13. Figge J, Mydosh T, Fencl V. Serum proteins and acid-base of estimated peri-operative blood loss for buffered versus
equilibria: a follow-up. J Lab Clin Med 1992;120:713-9. non-buffered IV fluid Resuscitation. Anesthesiology
2002;96:A197.
14. O'Connor MF, Roizen MF. Lactate versus chloride: which is
better? Anesth Analg 2001;93:809-10. 24. Boldt J, Haisch G, Suttner S, Kumle B, Schellhase F. Are
lactated Ringer's solution and normal saline solution equal
15. Kellum JA. Saline-induced hyperchloraemic metabolic with regard to coagulation? Anesth Analg 2002;94:378-84.
acidosis. Crit Care Med 2002;30:259-61.
Transfusion Alternatives in Transfusion Medicine is published bimonthly by LMS Group, 70/86, avenue de la République 92325 Châtillon Cedex FRANCE – S.A.R.L. au capital de 50,000 FF. • Phone: + 33 1 42 53 03 03
• Fax: + 33 1 42 53 03 02 • Printed in France, De Chabrol, 189 rue d’Aubervilliers, 75886 Paris Cedex 18 FRANCE • Numéro ISSN: 1295-9022 • All rights reserved • Copyright LMS Group • Advertising: For details on
media opportunities within this journal, please contact the advertising sales department (phone: + 33 1 42 53 03 03)• Dépôt légal 3e trimestre 2003.
Transfusion Alternatives in Transfusion Medicine 430 ) VOLUME 5 NUMBER 4 OCTOBER 2003
( Page
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- The PINEAL GLAND & Symbol of Manifestation - The SRI YANTRADocument7 pagesThe PINEAL GLAND & Symbol of Manifestation - The SRI YANTRAscriberone100% (3)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (842)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5807)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- (A. McLuckie) Respiratory Disease and Its Manageme PDFDocument169 pages(A. McLuckie) Respiratory Disease and Its Manageme PDFDerison MarsinovaNo ratings yet
- Butyric AcidDocument17 pagesButyric AcidBiswajit MohantyNo ratings yet
- Testicular Torsion Torsio TestisDocument34 pagesTesticular Torsion Torsio TestisAira Kelly50% (2)
- Acute Limb IschemiaDocument16 pagesAcute Limb IschemiaMohammad Husni BanisalmanNo ratings yet
- Adhf NCPDocument3 pagesAdhf NCPkristine keen buanNo ratings yet
- Pathophysiology BFSDocument1 pagePathophysiology BFSPatricia MonzonNo ratings yet
- Gordon's AssessmentDocument2 pagesGordon's AssessmentNikka GutierrezNo ratings yet
- Biology 1 - 12 - Q1 - M6Document15 pagesBiology 1 - 12 - Q1 - M6Artlyne BunuanNo ratings yet
- 576 A3sDocument3 pages576 A3sastige100% (1)
- Lesson1DIGESTIVESYSTEM DLPDocument11 pagesLesson1DIGESTIVESYSTEM DLPDen Angelica DungoNo ratings yet
- MAA Final / Orthodontic Courses by Indian Dental AcademyDocument93 pagesMAA Final / Orthodontic Courses by Indian Dental Academyindian dental academyNo ratings yet
- Skill Lab Checking Vital Signs OriginalDocument3 pagesSkill Lab Checking Vital Signs OriginalLuthi PratiwiNo ratings yet
- 7 - Chapter 2 - The Biology of MindDocument98 pages7 - Chapter 2 - The Biology of MindCikgu Diana IbnoNo ratings yet
- Against All Odds Preventing Pressure Ulcers in High-Risk Cardiac Surgery PatientsDocument8 pagesAgainst All Odds Preventing Pressure Ulcers in High-Risk Cardiac Surgery PatientsjokoNo ratings yet
- Review On Animal Tissues PDFDocument7 pagesReview On Animal Tissues PDFTitiNo ratings yet
- Modulacion Descendente Del DolorDocument9 pagesModulacion Descendente Del DolorCoke Cifuentes EsparzaNo ratings yet
- Health Ed II Module 4Document17 pagesHealth Ed II Module 4saturnino corpuzNo ratings yet
- Metabolisme IronDocument15 pagesMetabolisme IronERNI FORWATYNo ratings yet
- Student Nurses' Community: NURSING CARE PLAN AppendicitisDocument2 pagesStudent Nurses' Community: NURSING CARE PLAN AppendicitisJamaica Leslie NovenoNo ratings yet
- Bluff EnzymesDocument51 pagesBluff EnzymesJay Andrea Vea Dayuday-IsraelNo ratings yet
- IBO 2014 Theory Part A - CCLDocument50 pagesIBO 2014 Theory Part A - CCLimranq02No ratings yet
- Poster SpecCircs Anaphylaxis Treatment Algorithm ENG V20151001 HRES Site PDFDocument1 pagePoster SpecCircs Anaphylaxis Treatment Algorithm ENG V20151001 HRES Site PDFPetrarkina LauraNo ratings yet
- PPTDocument30 pagesPPTAimanNo ratings yet
- Haemopoiesis and Clinical ApplicationDocument42 pagesHaemopoiesis and Clinical Applicationtamer273No ratings yet
- Section C: Half Yearly Examination 2022-23 Biotechnology Paper-1 (Theory)Document6 pagesSection C: Half Yearly Examination 2022-23 Biotechnology Paper-1 (Theory)xipilev161No ratings yet
- NLE - CGFNS - Nclex Review Materials 1Document2 pagesNLE - CGFNS - Nclex Review Materials 1ChieChay Dub100% (1)
- UremiaDocument4 pagesUremiaMilnalyn Muammil100% (1)
- Generation of Gene-Modified Cynomolgus Monkey Via Cas9Document37 pagesGeneration of Gene-Modified Cynomolgus Monkey Via Cas9onimushaNo ratings yet
- Basal GangliaDocument48 pagesBasal GangliaMudassar Roomi100% (1)