Professional Documents
Culture Documents
Seizures, Status Epilepticus, and Continuous EEG in The Intensive Care Unit
Uploaded by
ednasu1Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Seizures, Status Epilepticus, and Continuous EEG in The Intensive Care Unit
Uploaded by
ednasu1Copyright:
Available Formats
Seizures, Status REVIEW ARTICLE
Epilepticus, and C O N T I N U UM A U D I O
INTERVIEW AVAILABLE
ONLINE
Continuous EEG in the
Intensive Care Unit
By Eric S. Rosenthal, MD
ABSTRACT
PURPOSE OF REVIEW: Thisarticle discusses the evolving definitions of seizures
and status epilepticus in the critical care environment and the role of
critical care EEG in both diagnosing seizure activity and serving as a
predictive biomarker of clinical trajectory. CITE AS:
CONTINUUM (MINNEAP MINN)
2021;27(5, NEUROCRITICAL CARE):
RECENT FINDINGS:Initial screening EEG has been validated as a tool to 1321–1343.
predict which patients are at risk of future seizures. However, accepted
definitions of seizures and nonconvulsive status epilepticus encourage a Address correspondence to
Dr Eric S. Rosenthal, Department
treatment trial when the diagnosis on EEG is indeterminate because of of Neurology, Massachusetts
periodic or rhythmic patterns or uncertain clinical correlation. Similarly, General Hospital, 55 Fruit St,
recent data have demonstrated the diagnostic utility of intracranial EEG Lunder 644, Boston, MA 02114,
erosenthal@mgh.harvard.edu.
in increasing the yield of seizure detection. EEG has additionally been
validated as a diagnostic biomarker of covert consciousness, a predictive RELATIONSHIP DISCLOSURE:
biomarker of cerebral ischemia and impending neurologic deterioration, Dr Rosenthal serves on
scientific advisory boards for
and a prognostic biomarker of coma recovery and status epilepticus Ceribell, Inc and UCB, Inc and
resolution. A recent randomized trial concluded that patients allocated to has received personal
compensation for speaking
continuous EEG had no difference in mortality than those undergoing engagements from UCB, Inc.
intermittent EEG but could not demonstrate whether this lack of Dr Rosenthal receives
difference was because of studying heterogeneous conditions, examining research/grant support from
Moberg Analytics, Inc (DoD
a monitoring tool rather than a therapeutic approach, or examining an W81XWH-18-DMRDP-PTCRA)
outcome measure (mortality) perhaps more strongly associated with early and the National Institutes of
withdrawal of life-sustaining therapy than to a sustained response to Health/National Institute of
Neurological Diseases and
pharmacotherapy. Stroke (1R01NS117904,
1R01NS113541, 1K23NS105950,
U54NS100064, DoD
SUMMARY: Seizures and status epilepticus are events of synchronous
W81XWH-BAA-15-1).
hypermetabolic activity that are either discrete and intermittent or,
alternatively, continuous. Seizures and status epilepticus represent the far UNLABELED USE OF
PRODUCTS/INVESTIGATIONAL
end of a continuum of ictal-interictal patterns that include lateralized USE DISCLOSURE:
rhythmic delta activity and periodic discharges, which not only predict Dr Rosenthal discusses the
future seizures but may be further classified as status epilepticus on the unlabeled/investigational use of
IV injection of ketamine,
basis of intracranial EEG monitoring or a diagnostic trial of antiseizure midazolam, and propofol for the
medication therapy. In particularly challenging cases, neuroimaging or treatment of seizures.
multimodality neuromonitoring may be a useful adjunct documenting
metabolic crisis. Specialized uses of EEG as a prognostic biomarker have © 2021 American Academy
of Neurology.
CONTINUUMJOURNAL.COM 1321
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
SEIZURES, STATUS EPILEPTICUS, AND CONTINUOUS EEG IN THE ICU
emerged in traumatic brain injury for predicting language function and
covert consciousness, cardiac arrest for predicting coma recovery, and
subarachnoid hemorrhage for predicting neurologic deterioration due to
delayed cerebral ischemia.
INTRODUCTION
T
his article discusses how to define, diagnose, and manage seizures,
status epilepticus, and indeterminate findings on the ictal-interictal
continuum within the critical care environment. Additionally, the
recent expansion of the utility of continuous EEG as a predictive
biomarker in a variety of critical care populations is discussed, such as
in predicting secondary ischemia after subarachnoid hemorrhage, diagnosing
covert consciousness in patients who are comatose, and predicting neurologic
recovery after structural brain injury or status epilepticus.
DEFINING AND DETECTING SEIZURES AND STATUS EPILEPTICUS IN
THE INTENSIVE CARE UNIT
The detection of seizures in the critical care setting is the subject of much
attention because they are common (found in 10% to 25% of patients recorded),1,2
represent a potentially reversible cause of encephalopathy or coma,3 and are
associated with poor outcome.4-6 The American Clinical Neurophysiology
Society (ACNS) has issued consensus recommendations regarding indications
for prolonged continuous EEG monitoring7:
u Persistently abnormal mental status following generalized convulsive status epilepticus or
other clinically evident seizures
u Acute supratentorial brain injury with altered mental status
u Fluctuating mental status or unexplained alteration of mental status without known acute
brain injury
u EEG patterns along the ictal-interictal continuum such as periodic discharges and
lateralized rhythmic delta activity
u Clinical risk for seizures potentially masked by the requirement for pharmacologic
paralysis during conditions such as extracorporeal membrane oxygenation (ECMO) or
targeted temperature management for cardiac arrest
u Paroxysmal clinical events suspected to be possible seizures
These indications nearly universally include patients with altered mental
status, encephalopathy, coma, or other disorders of consciousness following
traumatic brain injury, spontaneous subdural hematoma, subarachnoid
hemorrhage, intracerebral hemorrhage, meningoencephalitis, brain tumors,
recent neurologic surgery, cardiac arrest, and sepsis, as rates of seizure
exceed 15% among these patients when referred for EEG.4-6 Other
populations with a high risk may include patients with cerebral venous
sinus thrombosis.
Of note, a provider’s suspicion for seizure is likely not a substitute for active
surveillance, as patients not referred for EEG monitoring may be having occult
seizures. For example, in a cohort of patients with subarachnoid hemorrhage
monitored solely as part of an ischemia monitoring protocol to predict delayed
1322 OCTOBER 2021
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
cerebral ischemia, seizures occurred with a similar rate as in those patients KEY POINTS
referred with a concern for subclinical or clinical seizures (ie, even when the
● Electrographic seizures
provider lacked suspicion for seizure and would not otherwise have ordered and status epilepticus can
an EEG).8 be diagnosed by an
The diagnosis of seizures in the critically ill population has three electroclinical response to
main challenges: antiseizure medication.
● Although most seizures
u Seizures are commonly nonconvulsive, subtle, or obscured by a primary neurologic deficit are detected in the first
or sedation 48 hours of monitoring,
u Seizures may be occult on scalp EEG and only detected by an intracranial electrode shorter-duration monitoring
may be sufficient in patients
u Seizures, as status epilepticus, may only be diagnosed in retrospect after electroclinical without any epileptiform
improvement following treatment abnormalities and
longer-duration monitoring
Current consensus definitions of electrographic and electroclinical seizures may be required in patients
have coalesced around the Salzburg Consensus Criteria9-11 and have been with subarachnoid
hemorrhage.
adopted by the ACNS.12 In the updated 2021 ACNS Standardized Critical Care
EEG Terminology, electrographic seizures are defined as either epileptiform
discharges averaging more than 2.5 Hz for at least 10 seconds or a pattern with
definite evolution and lasting at least 10 seconds. Similarly, electrographic status
epilepticus is defined as an electrographic seizure for at least 10 continuous
minutes or for at least 20% of any 60-minute period.
Other electrographic activity not meeting these criteria may qualify as
“possible” electrographic seizure or electrographic status epilepticus when the
activity consists of periodic discharges, spike-wave activity, or rhythmic delta
activity on the ictal-interictal continuum. Uncertainty about whether
ictal-interictal continuum activity in an individual patient is indeed
nonconvulsive status epilepticus can be resolved, according to the ACNS
Standardized Critical Care EEG Terminology and Salzburg Consensus Criteria,9-12
when the electroclinical activity has a time-locked clinical correlate (eg,
thumb-twitching synchronous with each discharge despite lack of electrographic
evolution) or, alternatively, has combined EEG and clinical improvement
following antiseizure medication.12
The duration of EEG necessary for exhaustive detection of seizures in a
patient remains uncertain, given inherent biases in referring patients to
short-term EEG versus longer-duration continuous EEG monitoring.
However, retrospective research has led to validated risk scores that may be
applied on initial screening EEG to predict which patients will go on to have
seizures detected by continuous EEG monitoring. One method, the 2HELPS2B
score13,14 (FIGURE 6-1) has been tested and validated in separate inpatient
populations, accurately predicting the probability of subsequent seizures
across a range of predicted risk. Overall, 93% of patients with seizures had
detected events in the first 48 hours, and an absence of epileptiform
abnormalities in the first 2 hours was associated with a 72-hour seizure risk
lower than 5%.2 Similarly, in critically ill children with encephalopathy who
were at least 1 year of age, a seizure risk lower than 5% was observed if no prior
seizures were present and no epileptiform discharges and ictal-interictal
continuum patterns were present by 6 hours of recording; 1 day of monitoring
was required if EEG risk factors or prior seizures were evident, and 2 days
were required if both EEG risk factors and prior seizures were evident.15
Specific illnesses, however, may have an increased diagnostic yield from
CONTINUUMJOURNAL.COM 1323
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
SEIZURES, STATUS EPILEPTICUS, AND CONTINUOUS EEG IN THE ICU
FIGURE 6-1
2HELPS2B risk score system for prediction of subsequent electrographic seizures during
an initial screening EEG. Predicted seizure risk using this tool is well calibrated to the actual
seizure risk observed.
a
Range across the development and validation cohorts.
Data from Struck AF, et al, JAMA Neurol.14
longer-duration monitoring. For example, the median duration until seizure
detection following subarachnoid hemorrhage has been observed to be as long
as 5.6 days, whereas 7.3 days was required to detect 75% of patients
with seizures.8
These risk estimates, however, only apply to the detection of seizures by scalp
EEG. Additional seizures may be detected when recording intracranially by
electrocorticography, using either an orthogonally inserted mini–depth electrode
or a subdural strip electrode (CASE 6-1). Experience using an orthogonal
mini–depth electrode has been reported to increase the yield of seizure detection
from 14.7% to 23.5% in patients with traumatic brain injury16 and from 8% to 38%
in patients with subarachnoid hemorrhage.17 It is not known which scalp EEG
features best predict depth seizures, although the occurrence of depth seizures is
greatest ipsilateral to the side of dominant injury in patients with traumatic
brain injury.16
TREATMENT APPROACHES TO SEIZURES, REFRACTORY STATUS
EPILEPTICUS, AND SUPER-REFRACTORY STATUS EPILEPTICUS
Although the treatment of occult nonconvulsive seizures remains controversial,
antiseizure medication is commonly administered, and clinical trials examining
optimal dosing strategies have typically been performed without a placebo. In
one study, lacosamide was found to be noninferior to fosphenytoin for
controlling nonconvulsive seizures.18 When using fosphenytoin or phenytoin,
therapeutic drug monitoring requires assessment of free phenytoin levels in
patients who are critically ill or the use of more complex correction equations to
estimate a free phenytoin level or else high-magnitude errors can occur when
applying historical correction equations in critically ill patients to estimate free
phenytoin levels.19
1324 OCTOBER 2021
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
For convulsive seizures, the treatment approach is more straightforward. KEY POINTS
Benzodiazepines, specifically IV lorazepam or IM midazolam, are first-line
● Seizure detection is
agents,20,21 with IV lorazepam preferred for its rapidity of seizure control if an IV significantly augmented by
catheter is already in place.22 However, benzodiazepines are commonly the implantation of a single
underdosed after status epilepticus,23 despite their use being associated with intraparenchymal or
decreased rates of endotracheal intubation.24 When seizures are refractory to subdural strip electrode.
benzodiazepines, similar rates of terminating established status epilepticus were
● Because of changes in
observed with levetiracetam, fosphenytoin, or valproate. Of note, dosing was protein binding,
robust compared to doses commonly administered, particularly for levetiracetam large-magnitude errors are
(TABLE 6-125).26,27 However, antiseizure medications did not have a high rate of common when estimating
terminating clinically apparent seizures and improving consciousness without free phenytoin applying
standard phenytoin
need for additional antiseizure medication; success rates were approximately correction equations to
52% in children, 44% in adults, and 37% in older adults with established patients who are critically
status epilepticus.26 ill; correction equations
Patients for whom these therapies fail because of continued seizures are adjusting for age, renal
function, hepatic function,
commonly treated with anesthetic seizure suppression or burst suppression; and critical illness are
however, no randomized controlled trials are available to guide drug selection or necessary to avoid
dose. Trends embracing therapies other than traditional anesthetics include significant errors if free
increasing use of IV ketamine25 and ketogenic or low-glycemic diet therapy,28 in phenytoin levels are
unavailable.
addition to rational polytherapy aimed at avoiding the complications of status
epilepticus that are independently associated with mortality at 1 year.29 In the ● High-frequency periodic
absence of comparative effectiveness studies, the selection of antiseizure discharges may be transient
medications in refractory and super-refractory status epilepticus remains when weaning patients from
anesthetic coma following
focused on rational polytherapy targeting different mechanisms of action while
status epilepticus; pausing
managing and preventing complications (TABLE 6-2). and observing the patient
and EEG, evaluating
EEG NEUROMONITORING TO GUIDE LIBERATION FROM ANESTHETIC background activity, and
COMA AFTER STATUS EPILEPTICUS examining for frank seizures
may avoid delaying
EEG is used routinely in the treatment and monitoring of status epilepticus. anesthetic liberation.
Following convulsive status epilepticus, 48% of patients demonstrated persistent
seizures, including 14% with nonconvulsive status epilepticus. Those with
nonconvulsive status epilepticus had a mortality greater than 50% compared
with less than 15% among those without ictal discharges, conferring 1.9-fold risk
of mortality even when adjusted for age and etiology.30 Rapid EEG has not been
used to date in interventional clinical trials in the emergency department; thus,
primary end points in acute status epilepticus clinical effectiveness trials have
been limited to absence of clinically apparent seizures with improved
consciousness and without additional antiseizure medication.26,27 Without an
end point that includes EEG monitoring, patients intubated for neuroimaging or
progression of a structural brain injury have been considered to have failed status
epilepticus therapy regardless of the reason for intubation, a major limitation
given that the rate of intubation has nearly doubled over the past 2 decades.31
In critical care studies of status epilepticus utilizing continuous EEG, an
aggressive approach to anesthetic weaning has demonstrated EEG normalization
and clinical improvement despite initial increases in periodic discharges.32
Although the literature suggests that metabolic crisis is associated with these
high-frequency periodic discharges,33 the emergence of ictal-interictal
continuum activity may be transient in the setting of weaning from anesthetic
coma.34 In this setting, other clinical and quantitative features may be of use to
determine which patients are likely to be liberated from anesthetic coma. For
CONTINUUMJOURNAL.COM 1325
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
SEIZURES, STATUS EPILEPTICUS, AND CONTINUOUS EEG IN THE ICU
example, in a population without cardiac arrest, unsuccessful anesthetic
liberation after refractory status epilepticus was associated with the presence of
highly epileptiform bursts (multiple discharges in the majority of bursts)35 as
well as with bursts that were monomorphic, exceeded 125 μV amplitude, or
(more often than not) demonstrated epileptiform features.36 A quantitative
approach using spectral power in frequency bands and functional connectivity
measures, including network density, yielded a testing accuracy of 75% in a
holdout cohort and in a secondary external validation cohort, with an area under
the curve of 83% for predicting successful anesthetic liberation. These features
add information about the potential success or failure of a wean up to 12 hours
before a wean is clinically terminated. Thus, many hours before anesthesia
weaning is determined to be a success or failure based on recurrence of status
epilepticus, emerging network connectivity is evident in patients who were
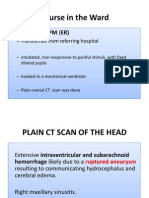
CASE 6-1 A 61-year-old man was admitted to the neurocritical care unit after
craniotomy for aneurysmal subarachnoid hemorrhage. He was comatose,
and continuous EEG monitoring with electrocorticography recording
activity from a 6-contact subdural strip electrode was initiated
immediately after the craniotomy. He was found to have seizures
consisting of periodic discharges with evolution on the subdural strip
electrode while on levetiracetam 500 mg every 12 hours (FIGURE 6-2A). He
had no evident seizures on the scalp EEG channels, which showed only
rhythmic delta activity. After two doses of levetiracetam 1500 mg every
12 hours (FIGURE 6-2B), his EEG improved to an alpha background without
epileptiform activity and his clinical examination had improved to
conversational.
COMMENT This case illustrates the discordant findings between scalp EEG and
intracranial electrocorticography. The scalp EEG showed rhythmic delta
activity, but the subdural strip electrode showed a mix of rhythmic delta
activity with embedded sharp waves as well as periodic discharges with
evolution. Additionally, the case demonstrates how changes over time in
the context of treatment may be interpreted clinically according to the
Salzburg Consensus Criteria.10 Both the rhythmic delta activity on the scalp
and the activity on the strip electrode with evolution resolved after
treatment, coincident with improvement of arousal, orientation, and verbal
functioning. Although this patient’s electroclinical improvement was
consistent with a post hoc diagnosis of nonconvulsive status epilepticus
according to the American Clinical Neurophysiology Society Standardized
Critical Care EEG Terminology and Salzburg Consensus Criteria, clinical
trials are necessary to determine whether antiseizure medication
escalation itself improves clinical outcomes.
1326 OCTOBER 2021
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
successfully liberated from anesthesia without seizure recurrence.37 Accordingly,
future efforts may be aimed at hastening anesthetic liberation and coma recovery
in patients with status epilepticus based on EEG measures.
BALANCING THE RISKS AND BENEFITS OF TREATING NONCONVULSIVE
SEIZURES AND ICTAL-INTERICTAL CONTINUUM ACTIVITY
When considering the risks of nonconvulsive seizure activity and status
epilepticus, a measure of overall burden (percent prevalence multiplied by time
observed) has been introduced as part of the ACNS Standardized Critical Care
EEG Terminology. When considering the risks of ictal-interictal activity, an
additional measure, index (burden multiplied by the frequency of periodic
discharges or lateralized rhythmic delta activity) can be used as a composite
measure combining both duration and intensity.12
FIGURE 6-2
Continuous EEG monitoring with intracranial electrocorticography from a six-electrode
subdural strip (red boxes) of the patient in CASE 6-1 after craniotomy for aneurysmal
subarachnoid hemorrhage while on levetiracetam 500 mg every 12 hours on hospital day 1 (A)
and on day 2 (B) after two doses of levetiracetam 1500 mg every 12 hours.
CONTINUUMJOURNAL.COM 1327
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
SEIZURES, STATUS EPILEPTICUS, AND CONTINUOUS EEG IN THE ICU
Nonconvulsive seizures and ictal-interictal continuum activity have
demonstrated an impact on outcome independent of potential confounders such
as disease severity, which itself may be associated with both seizure incidence
and outcome. In multivariate regression analysis, periodic discharges are
associated with an 18.8-fold risk of poor functional outcome on the modified
Rankin Scale in patients with subarachnoid hemorrhage.5 Although one study
demonstrated little difference between brief or prolonged periodic discharges on
functional outcome in a mixed population,38 more recent studies using burden
measures have demonstrated that patients with ischemic stroke with a peak daily
burden of epileptiform activity exceeding 10% have a 23-fold risk of poor
outcome and that the interaction of increasing epileptiform activity burden with
frequency reaching 1.5 Hz conferred a 1.6-fold risk of poor outcome.39 Similarly,
in subarachnoid hemorrhage, the burden of epileptiform activity on the first
day of monitoring and the peak daily burden of epileptiform activity were each
associated with poor functional and cognitive outcomes.40,41 In a cohort of
patients with traumatic brain injury in the INTREPID2566 (Study of NNZ-2566 in
Patients With Traumatic Brain Injury) study, ictal-interictal activity did not have
an association with poor outcome when patients with moderate (including
sub–1.5-Hz lateralized rhythmic delta activity or sub–1.5-Hz generalized periodic
discharges; 45% of patients) and severe ictal-interictal continuum activity (14%
of patients) were grouped together, with the latter underrepresented.42
Given these effects on outcome, antiseizure medication escalation to suppress
events on the ictal-interictal continuum other than generalized rhythmic delta
activity has been investigated, including retrospective studies examining
triphasic-appearing generalized periodic discharges, historically considered
metabolic in origin.3 Recognizing that unequivocal responses to antiseizure
medication escalation (resolution of both the abnormal EEG pattern and
improvement of EEG background or encephalopathy) are common has
encouraged a more proactive approach to treatment. The historic
characterization of triphasic waves as being synonymous with a metabolic
etiology needing treatment of the underlying condition has been updated by data
showing that intervening by treating patients with triphasic discharges with
benzodiazepines or antiseizure medication results in commensurate
electrographic and clinical improvement in a number of patients.3 However,
questions remain about the clinical benefit of routine antiseizure medication
escalation in patients with ictal-interictal continuum activity. One potential
TABLE 6-1 Dosing Administered in the Established Status Epilepticus Treatment Triala
Drug Dose Administration
Levetiracetam 60 mg/kg (maximum 4500 mg) 10-min infusion
Fosphenytoin 20 mg PE/kg (maximum 1500 mg PE) 10-min infusion
Valproate 40 mg/kg (maximum 3000 mg) 10-min infusion
PE = phenytoin sodium equivalent.
a
Data from Gaspard N, et al, Epilepsia.25 and Chamberlain JM, et al, Lancet.26
1328 OCTOBER 2021
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
strategy is a 48-hour trial of therapy to assess for electrographic response as well KEY POINTS
as sufficient time for a clinical response that may require recovery from a
● The quantified initial or
postictal period. peak burden of
ictal-interictal continuum
POSTACUTE ANTISEIZURE MEDICATION MANAGEMENT activity and electrographic
The negative effects of antiseizure medication on cognition have been seizures are independently
associated with outcome.
demonstrated in subarachnoid hemorrhage and intracerebral hemorrhage.43 As a
result, patients with symptomatic or reversible causes of seizures may be ● Even generalized periodic
considered for withdrawal of antiseizure medications at several weeks following discharges with a triphasic
critical care. These decisions must be balanced against the risks of recurrent morphology, historically
seizures, particularly in patients with seizures attributable to a focal lesion, associated with metabolic
disturbances, may
persistent epileptiform discharges after trauma, or status epilepticus.44,45 One commonly have an
strategy is to perform outpatient EEG after withdrawing seizure medications, electroclinical response to
although it is unclear whether this strategy optimizes the use of antiseizure escalation of antiseizure
medications or cognitive outcomes. medication.
● Electrometabolic status
EEG FOR DETECTION AND PREDICTION OF SECONDARY BRAIN INJURY epilepticus is increasingly
Whether epileptiform activity on the ictal-interictal continuum is a cause or appreciated as
effect of injury and ischemia has been of interest since the specific association of ictal-interictal continuum
activity of high frequency in
generalized or lateralized periodic epileptiform discharges with brain injury was
association with exhaustive
first noted as “paroxysmal high-voltage and rhythmic low-voltage discharges” by metabolic crisis measured
Echlin and colleagues46 following surgical isolation or partial isolation of human by cerebral hyperglycolysis
cortex; by Chatrian and colleagues47-49 beginning in 1952 as periodic lateralized during positron emission
tomography, increasing
epileptiform discharges associated with ischemia, malignancy, or infection; and
lactate to pyruvate ratio
by Alajouanine and colleagues50 in 1955 as generalized and lateralized periodic evident from cerebral
discharges associated with infectious and inflammatory maladies. microdialysis sampling, or
There are multiple potential mechanisms by which epileptiform activity is brain tissue hypoxia
independently associated with poor outcome: (1) association of epileptiform identified during brain tissue
oxygenation monitoring.
activity with exhaustive hypermetabolism and metabolic crisis, (2) association of
epileptiform activity with subsequent cortical spreading depolarization, (3)
association of epileptiform activity with inflammation, and (4) potential
medication toxicity related to escalating antiseizure medication to treat
epileptiform activity.
Numerous modalities have documented the temporal and regional association
of epileptiform activity with exhaustive hypermetabolism and metabolic crisis.
Ictal-interictal activity is associated with regional hyperglycolysis51 that is
frequency dependent33 and decreases with anesthetic burst suppression.51,52 In
patients with subarachnoid hemorrhage, periodic discharges have been shown to
have a regional and temporal frequency-dependent association with decreases in
brain tissue oxygenation53: median partial pressure of brain tissue oxygenation
was 23 mm Hg without periodic discharges, 16 mm Hg when periodic discharges
reached 2.0 Hz, and 14 mm Hg when discharges reached 2.5 Hz.53 In traumatic
brain injury, elevated lactate to pyruvate ratio is associated with either seizures or
periodic discharges16 and subsequent ipsilateral cortical atrophy.6 In
intracerebral hemorrhage, electrographic seizures have been linked to a
subsequent increase in midline shift of 2.7 mm (compared to a decrease of
2.4 mm in patients without seizure over the first 72 hours of admission).54
Patients with in-hospital nonconvulsive seizures after subarachnoid
hemorrhage have a 1.9-fold risk of a systemic inflammatory response syndrome
and higher levels of high-sensitivity C-reactive protein and tumor necrosis factor
CONTINUUMJOURNAL.COM 1329
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
SEIZURES, STATUS EPILEPTICUS, AND CONTINUOUS EEG IN THE ICU
TABLE 6-2 Antiseizure Medications Commonly Used On-label and Off-label in
Patients Who Are Critically Ill
Drug Proposed mechanism and rationale Monitoring Considerations
Brivaracetam Synaptic vesicle glycoprotein 2A Complete blood cell count, Prior authorization may be
(SV2A) binding; IV available; liver function tests required as outpatient
dependable and rapid kinetics; higher
binding affinity than levetiracetam
Carbamazepine Voltage-gated sodium channel Trough levels; complete No long-term IV option;
binding, inactivation blood cell count, liver function associated with higher risk of
tests/drug reaction with Stevens-Johnson syndrome in
eosinophilia and systemic certain Asian patients with
symptoms (DRESS); degraded HLA-B*15:02
by cytochrome P450 (CYP)
3A4; strong, broad enzyme
inducer of CYP3A4
Clobazam γ-Aminobutyric acid A (GABAA) partial Arousal, hypopnea; degraded Long elimination half-life; use
agonist selective α1β3γ2 with lower by CYP3A4 with caution in patients with
affinity for α1β2γ2 receptor; increase hepatic dysfunction
in calcium ion conduction; selective
receptor binding to reduce sedative
side effects with increased
antiseizure effects compared to other
benzodiazepines
Lacosamide Sodium channel selective ECG PR interval, bradycardia, IV; avoid in second- and
enhancement of slow inactivation, heart block third-degree heart block or sick
collapsin response mediator protein 2 sinus syndrome; prior
(CRMP-2) binding; IV available; authorization may be required
therapeutic drug monitoring not as outpatient
routinely required; minimal drug
interactions; noninferior to
fosphenytoin in patients with
nonconvulsive seizures
Levetiracetam Binding to SV2A; partial inhibition of Complete blood cell count, IV; dosing in clinical trials higher
N-type calcium ion currents; IV liver function tests; behavioral than commonly prescribed
available; therapeutic drug monitoring dysfunction
not routinely required; highly studied
in status epilepticus
Oxcarbazepine Binding to voltage-gated sodium Trough levels; complete No IV option; associated with
channels; inhibition of glutamate blood cell count, sodium; liver higher risk of Stevens-Johnson
release; easily titrated; less function tests/DRESS; weakly syndrome in Asian patients with
hyponatremia than carbamazepine; induces CYP3A4, weakly HLA-B*15:02, although lower risk
secondary use in mood disorders inhibits CYP2C19 than carbamazepine
Perampanel Noncompetitive α-Amino-3-hydroxy- DRESS, mood dysfunction;
5-methylisoxazole-4-proprionic acid degraded by CYP3A4
(AMPA) receptor antagonist; IV
available; unique mechanism
Phenobarbital GABAA receptor β-subunit binding; Complete blood cell count, May enhance beta activity,
increase in calcium ion channel liver function tests; induces sharpness of EEG
conduction; IV available; secondary CYP3A4, CYP2C9, CYP1A2;
use in treating alcohol withdrawal; degraded by CYP2C9,
historic data in status epilepticus CYP2C19, CYP2E1
CONTINUED ON PAGE 1331
1330 OCTOBER 2021
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
CONTINUED FROM PAGE 1330
Drug Proposed mechanism and rationale Monitoring Considerations
Phenytoin/ Blockade of voltage-dependent Complete blood cell count, Zero-order kinetics can result in
fosphenytoin sodium channels; IV available; highly liver function tests, albumin; toxicity; free levels in patients in
studied in status epilepticus and strong, broad enzyme inducer the intensive care unit poorly
seizure prophylaxis studies of patients of CYP3A4, CYP2C9, CYP1A2; estimated by historic equations
with traumatic brain injury degraded by CYP2C9,
CYP2C19
Topiramate GABAA nonbenzodiazepine receptor pH, bicarbonate; weakly Alternatives preferred when
site binding; AMPA and kainate induces CP3A4, weakly possible in patients with
receptor binding/inhibition; inhibits CYP2C19 first-term pregnancies
voltage-dependent sodium channel
binding; IV available; case series in
refractory status epilepticus
Valproate GABA transaminase inhibition and Liver function tests, albumin, IV; may have effect on platelet
reduced GABA metabolism; amylase/lipase in patients at dysfunction even without
voltage-gated sodium channel high risk; blood cell counts, thrombocytopenia; free levels
suppression; IV available; may have albumin; inhibits CYP2C9; may be needed if
secondary benefit for mood degraded by CYP2A6, hypoalbuminemia or
stabilization or headache CYP2C9, CYP2C19, CYP2B6 concomitant phenytoin/
fosphenytoin therapy;
alternatives preferred when
possible in patients who are
pregnant; consider free levels in
patients with low albumin
Ketamine Noncompetitive N-methyl-D- Heart rate, respiratory Increasing use as earlier option
aspartate (NMDA); HCN1 receptor function, liver function tests, in patients with refractory
blockade and commensurate laryngospasm; postanesthetic seizures
decrease in AMPA receptor-mediated emergence reaction;
transmission; IV dissociative degraded by CYP2B6 and
anesthetic; reduced withdrawal CYP3A4
symptoms; well tolerated without
hemodynamic effects
Midazolam GABAA benzodiazepine binding site; Blood pressure, respiratory May require vasopressor
IV, IM, and intranasal routes; first-line function support
agent in prehospital setting;
anesthetic third-line agent
Pentobarbital GABAA β-subunit binding; IV Heart rate; respiratory Need for vasopressor support;
anesthetic third-line agent; silencing function; complete blood cell risk for bowel perforation
of cerebral metabolism at high doses count, liver function tests,
ileus; degraded by CYP2B6,
partially by CYP3A4
Propofol GABAA β2 and β3 receptor subunit Respiratory function; liver May require vasopressor
binding. IV anesthetic third-line agent; function tests, triglycerides, support; risk for propofol
rapid onset and offset creatine kinase, pH, potential infusion syndrome in children or
CYP3A4 inhibitor in patients with low body
weight; need for adjusting
nutrition to prevent
hypertriglyceridemia
ECG = electrocardiogram; EEG = electroencephalogram; IM = intramuscular; IV = intravenous.
CONTINUUMJOURNAL.COM 1331
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
SEIZURES, STATUS EPILEPTICUS, AND CONTINUOUS EEG IN THE ICU
receptor 1; a mediation analysis demonstrated that the association between
inflammatory markers and outcome was mediated in part through
nonconvulsive seizures.55 The emergence of new or worsening epileptiform
activity (lateralized rhythmic delta activity, generalized periodic discharges, or
lateralized periodic discharges) was also associated with inflammatory marker
soluble ST2 both in blood and CSF,56 suggesting that inflammation is associated
with ictal-interictal activity in addition to frank electrographic seizures.
EEG ISCHEMIA MONITORING AFTER SUBARACHNOID HEMORRHAGE
Because EEG demonstrates increased delta and decreased alpha activity during
ischemia, continuous EEG has been retrospectively examined for the ability to
predict delayed cerebral ischemia after subarachnoid hemorrhage using
continuous EEG spectral features,57,58 including decreases in the alpha to delta
power ratio57,59,60 or relative alpha power variability.60,61 Specifically, clinically
useful cutoffs in alpha to delta ratio were identified, including six consecutive
recordings with a greater than 10% decrease from baseline (sensitivity 100%,
specificity 76%) and any single measurement with a greater than 50% decrease
(sensitivity 89%, specificity 84%).59 A decrease in relative alpha variability was
100% sensitive but only 50% specific for vasospasm.61
Other findings historically associated with cerebral ischemia include
epileptiform discharges, rhythmic and periodic ictal-interictal continuum
patterns,49,62-64 and isolated alpha suppression.65 In subarachnoid hemorrhage,
new or worsening epileptiform activity has been associated with subsequent
delayed cerebral ischemia.66,67 Using change-point detection, the temporal onset
of brain tissue hypoxia was associated with increases of periodic discharge
frequency exceeding 2.0 Hz, supporting the hypothesis that secondary ischemia
is associated with subarachnoid hemorrhage.53
The findings of spectral frequency change and new epileptiform activity on
continuous EEG have been examined prospectively in both a feasibility study
(demonstrating that more than 90% of delayed cerebral ischemia events
occurred during the mean 6.9 days of continuous EEG monitoring68) and a
TABLE 6-3 Accuracy Results for Continuous EEG Prediction of Delayed Cerebral
Ischemia After Subarachnoid Hemorrhage (n = 103)a
Low risk Medium risk High risk
[risk score = 1] [risk score = 2.5] [risk score = 4]
Sensitivity (%) 91 [81-98] 94 [88-99] 95 [87-99]
Specificity (%) 83 [71-93] 80 [69-90] 77 [36-99]
Pretest probability of delayed cerebral ischemia (%) 37 [25-50] 58 [50-66] 79 [61-92]
Delayed cerebral ischemia risk (continuous EEG deterioration) (%) 76 [58-90] 87 [79-94] 94 [79-100]
Delayed cerebral ischemia risk (no continuous EEG deterioration) (%) 6 [1-13] 10 [2-19] 9 [3-53]
Number needed to monitor 2.6 [2.0-3.8] 3.5 [2.8-4.8] 6.7 [3.6-25.3]
a
Modified with permission from Rosenthal ES, et al, Ann Neurol.67 © 2018 American Neurological Association.
1332 OCTOBER 2021
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
diagnostic accuracy study (validating the high sensitivity and specificity of an KEY POINTS
EEG “alarm” in patients with low, medium, or high baseline risk) (TABLE 6-3).67
● Seizure activity is
These EEG alarms were prespecified as a change from baseline consisting of increasingly appreciated as
any of the following not explained by sedation, hydrocephalus, or other clinical associated with an
confounders: (1) 10% decrease in alpha to delta ratio persisting 6 hours or a 50% inflammatory complex
decrease persisting longer than 1 hour, (2) a one-grade decrease in relative alpha of biomarkers in blood
and CSF.
variability over an 8-hour epoch, (3) new focal slowing identified on regional
spectrograms or raw EEG, or (4) new or worsening epileptiform activity. ● A battery of continuous
Because patients with an EEG alarm as described above have a subsequent risk of EEG findings, including
delayed cerebral ischemia of 76% (patients at low risk), 87% (patients at medium decrease in alpha to delta
risk), and 94% (patients at high risk), these methods of ischemia monitoring may ratio of frequency-band
power, one-grade decrease
be useful as patient selection criteria for enrichment strategies in future clinical in relative alpha variability,
trials or as triggers for higher-risk diagnostic or treatment studies such as and new or worsening
cerebral angiography with endovascular vasodilator therapy. Of interest, a epileptiform activity, have
single-center study found that EEG delayed cerebral ischemia biomarkers of new been prospectively
validated as a method of
or worsening epileptiform activity were strongly associated with longitudinal predicting subsequent
functional outcomes following subarachnoid hemorrhage, whereas EEG ischemia in patients with
background deterioration was not.69 This discrepancy may be related to a subarachnoid hemorrhage.
differential response to clinically available interventions. A patient with a
● Cortical spreading
commensurate decrease in both alpha to delta ratio and invasively measured
depolarizations are
cerebral blood flow followed by a response to endovascular intraarterial increasingly being
administration of calcium channel blockers directly at the site of cerebral monitored in clinical
vasospasm is depicted in CASE 6-2. practice as brain activity
associated with unexplained
coma and poor neurologic
CORTICAL SPREADING DEPOLARIZATION MONITORING ACROSS outcome.
ACUTE BRAIN INJURIES
Cortical spreading depolarizations similar to those seen in migraine are present in
acute brain injury. These depolarizations spread slowly and typically have a
magnitude greater in amplitude than seizure activity; when they occur in
vulnerable parenchyma after acute brain injury, they result in severe metabolic
crisis, which is often irreversible when depolarizations occur repeatedly in
clusters. Intracranial electrocorticography has traditionally been required for the
detection of cortical spreading depolarization.70,71 However, evaluation of
examples of simultaneous scalp and subdural electrode recordings suggested that
depression of fast activity over the scalp may be a signature of underlying
spreading depolarization.72 The association of spreading depolarizations with
neurologic deterioration and poor outcome in patients with subarachnoid
hemorrhage, traumatic brain injury,73-76 and surgically managed subdural
hematoma, combined with the reduction of these events by ketamine,77-83 has led
to a trend of both increased clinical use of intracranial monitoring of
low-frequency activity in patients with acute brain injuries and increased interest
in future therapies targeted at treating these events.84
DETECTION OF DELIRIUM, ENCEPHALOPATHY, AND COVERT
CONSCIOUSNESS AND PREDICTION OF COMA RECOVERY
In addition to predicting anesthetic liberation after status epilepticus, EEG has
also gained attention for its ability to diagnose and monitor delirium and
disorders of consciousness in patients who are critically ill and to predict coma
recovery. The depth and severity of delirium is highly correlated with the
prevalence of EEG slowing. The EEG finding most strongly associated with the
CONTINUUMJOURNAL.COM 1333
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
SEIZURES, STATUS EPILEPTICUS, AND CONTINUOUS EEG IN THE ICU
presence of delirium in one study was a composite of generalized theta or delta
slowing, conferring a tenfold risk (95% confidence interval, 5.3-20.1). Slowing is
present even in patients with delirium who have preserved arousal.85 In clinical
practice, EEG in patients with delirium can be useful to trend improvement from
delirium as an intermediate biomarker of recovery after treatment of potential
underlying causes, such as infection, sedation, toxic-metabolic effects, or
organ dysfunction.
As a tool for patients with disorders of consciousness, EEG is useful to detect
covert consciousness. EEG performed in the background of various stimuli
(audio recordings alternating as a stimulus battery) at a mean of 10 days after
CASE 6-2 A 74-year-old woman presented with a Hunt and Hess Scale grade 4 and
Fisher Scale grade 4 subarachnoid hemorrhage due to a right supraclinoid
internal carotid artery aneurysm. Examination demonstrated delayed
response to commands but no overt focal symptoms of delayed cerebral
ischemia. The patient was considered uncertain to benefit from
catheter-based intraarterial vasodilator therapy. Over a 2-day period, a
depth electrode demonstrated a decline in the alpha to delta ratio that
was concordant with a decline in cerebral blood flow monitoring from
30 mL/100 g/min to 10 mL/100 g/min measured from a nearby probe
(FIGURE 6-3A). Based on these data, the patient was referred for
endovascular intraarterial calcium channel blocker therapy (FIGURE 6-3B),
which was associated with an increase in cerebral blood flow (FIGURE 6-3B)
from 10 mL/100 g/min to 15 mL/100 g/min and concordant emergence of
an EEG alpha rhythm measured from the colocated depth electrode
(FIGURE 6-3B).
COMMENT This case demonstrates that when changes in EEG spectral activity (such as
decrease of the alpha to delta ratio) are concordant with other modalities
(such as cerebral blood flow or brain tissue oxygenation), there may be
increased confidence of vasospasm as a treatable mechanism of
metabolic crisis, manifest as EEG background deterioration.
1334 OCTOBER 2021
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
traumatic coma was part of a multimodal assessment, also incorporating
functional MRI (fMRI), that was able to identify cognitive-motor dissociation in
four of 16 subjects and higher-order cortical processing in two additional
patients.86 Patients with EEG differences demonstrated by a machine learning
classifier comparing alternating blocks of auditory stimulation and rest were
more likely to have intact language function as measured by either the Coma
Recovery Scale-Revised or a composite that included fMRI.87 A manual method
examining EEG background had almost as good agreement with the behavioral
language examination as did the machine learning stimulus-based EEG classifier,
and a method employing both background and reactivity had significant
FIGURE 6-3
Findings for the patient in CASE 6-2. A, Depth electrode tracings demonstrate a decline in the
alpha to delta ratio that is discordant with a decline in cerebral blood flow monitoring from
30 mL/100 g/min to 10 mL/100 g/min measured from a nearby probe (sixth tracing from the
top). B, Tracings before (left image) and after (right image) catheter-based intraarterial
vasodilator therapy demonstrate an increase in cerebral blood flow (top image) of
10 mL/100 g/min to 15 mL/100 g/min, concordant with the emergence of an alpha rhythm
measured from the colocated depth electrode (B, bottom tracing).
CONTINUUMJOURNAL.COM 1335
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
SEIZURES, STATUS EPILEPTICUS, AND CONTINUOUS EEG IN THE ICU
agreement with the composite standard for detecting language function by either
fMRI or behavioral evidence of language.87 In addition to studies of patients with
traumatic brain injury, a prospective study evaluating EEG responses in patients
with a wide variety of acute brain injuries demonstrated that brain activation in
response to auditory stimulation was evident in 15% of 104 patients, conferring
nearly twice the rate (50% compared to 26%) of following commands before
discharge and 4.6-fold odds of achieving a good Glasgow Outcome
Scale-Extended score at 12 months (44% compared to 14%).88 EEG may also be
useful in differentiating patients in an unresponsive wakefulness state from those
in a locked-in state even without preserved eye movements, such that EEG may
demonstrate normal cortical rhythms and reactivity in the locked-in state.89,90
Prognostic information about coma recovery is also evident in patients with
cardiac arrest. Treatment with therapeutic hypothermia significantly affects the
prognostic significance of these findings.91 The occurrence of monomorphic
“identical” bursts has been linked with near uniformly poor outcome in studies
seeking to minimize biases from self-fulfilling prophecies by examining a cohort
in which limitation of life-sustaining therapy did not occur in the first 72 hours,
even though an unfavorable EEG pattern at 12 hours was the factor most strongly
associated with poor outcome.92 A prediction model including the presence of
status epilepticus, suppression-burst pattern alone, and lack of background
reactivity had an area under the curve of 0.92 for predicting poor functional
outcome in a cohort of 373 patients.93 Alternatively, patients with continuous
EEG activity are more likely to respond to antiseizure medication or therapeutic
hypothermia with a resolution of epileptiform activity,94 and the combination of
EEG continuity and lack of anoxic injury on MRI was associated with coma
recovery at a sensitivity of 91% and specificity of 99%. Other more quantitative
tools include a Cerebral Recovery Index (consisting of alpha to delta ratio of
power, standard deviation, coherence in delta activity, Shannon entropy, and
regularity)95-98 and time-varying models containing features of complexity,
category, and connectivity.99
Similarly, in intracerebral hemorrhage, the absence of an anteroposterior
gradient was associated with poor outcome and the presence of stage II sleep
activity was independently associated with good functional outcome.100 In
traumatic brain injury, absence of a posterior dominant rhythm, absence of N2
sleep transients, presence of predominant delta activity, and presence of a
discontinuous background were associated with poor outcome when evident in
the initial 72 hours.42
RESOURCE UTILIZATION
The use of EEG in the emergency and critical care environment has historically
required the availability of both EEG equipment and technologist resources.
The increasing availability of rapid EEG devices that can be placed by physicians
and nurses has enabled EEG placement at a median of 5 minutes, with only
25% of studies requiring greater than 10 minutes before recording could
commence.101 These techniques may also allow for screening neurotelemetry
that may enable examining the rate of seizures in the hyperacute phase as well as
assessing whether ictal-interictal activity is commonly preceded by progression
from sustained seizure activity.102
The use of continuous EEG has increased significantly over time, with critical
care neurophysiologists using quantitative aspects of EEG for seizure detection in
1336 OCTOBER 2021
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
over 90% of users, pharmacologic titration to burst suppression in nearly 60% of KEY POINTS
users, and a variety of other uses in 20% to 30% of users, including monitoring
● Covert consciousness is
the depth of sedation, detecting ischemia, detecting vasospasm, and prognosis frequently seen in patients
after cardiac arrest,103 with costs and resource utilization commensurate with who are critically ill with
intermittent EEG. Challenges with the availability and cost of continuous EEG acute brain injury; wider
monitoring compared to intermittent EEG monitoring have led to analyses availability of
stimulus-based EEG
examining differences in yield and outcomes. In patients with cardiac arrest
monitoring (in addition to
undergoing therapeutic hypothermia, for example, a high degree of agreement functional MRI) may not only
was reported between continuous and intermittent EEG methods, and an improve the accuracy of
observational study reported that continuous EEG did not confer a benefit over diagnosing patients with
disorders of consciousness
intermittent EEG in patients with cardiac arrest,104 although decisions to limit
but also improve the
life-sustaining therapy and physician biases may also have explained the lack of information available to
differences. A follow-up randomized controlled trial reported no difference in surrogate decision makers.
outcomes among patients undergoing continuous EEG compared to intermittent
EEG, but the conclusions were limited by a highly heterogeneous population, ● Assessment of the EEG
background rhythm,
lack of a specified treatment protocol during the monitoring, and the potential including sleep features and
for continuous monitoring to inform goals-of-care conversations and thereby continuity, provides
influence the rate of withdrawal of life-sustaining therapy.105 Other studies prognostic information in
reporting improved outcomes when continuous EEG was performed in patients addition to the presence of
activity on the
who were critically ill106 similarly lack an interventional approach to determine ictal-interictal continuum.
whether these effects are related to treatment effects.
● Although one randomized
study concluded that
continuous EEG showed no
CONCLUSION
benefit compared to
The advancement of consistent nomenclature and definitions has improved the intermittent EEG, a definitive
reliability of definitions for seizures, status epilepticus, and indeterminate study would require
patterns on the ictal-interictal continuum. A consolidated approach to diagnosis examining a specific
and management reflecting these many applications of EEG neuromonitoring in population expected to
have a homogeneous
neurocritical care is depicted in FIGURE 6-4. Management of clinically apparent pathophysiology, defining a
and convulsive status epilepticus (FIGURE 6-4A) has evidence-based literature treatment protocol that
guiding management along the continuum of prehospital, emergency, and makes use of
critical care, but continuous EEG may improve diagnostic accuracy and precision neuromonitoring findings,
and controlling for changes
of management at an early phase. Management of encephalopathy, coma, and in life-sustaining treatment
other disorders of consciousness requires a consideration of more diverse resulting from differences in
etiologies and multimodality neuromonitoring to improve diagnostic precision. available prognostic
Monitoring requires serial assessment and iterative management changes information.
(FIGURE 6-4B). Specifically, trends in using adjunctive tools to document both
scalp-negative seizures and the metabolic burden of epileptiform activity have
expanded the recognition that increasing seizure burden and increasing
burden and intensity of periodic and rhythmic patterns on the ictal-interictal
continuum are both associated with cerebral metabolic crisis related to
exhaustive cerebral hypermetabolism. When seizure activity is indeterminate,
intracranial EEG and empiric treatment trials with antiseizure medication have
been used to demonstrate clinical improvement in a substantial portion of
patients, thereby improving diagnostic precision. When seizures are continuous
and refractory in the form of status epilepticus, the current approach is to
optimize antiseizure medications during a structured course of anesthetic
management. Approaches including seizure suppression and burst suppression
with anesthetics have grown to incorporate medications including ketamine as
well as ketogenic or low-glycemic diet therapy and neuromodulation.
CONTINUUMJOURNAL.COM 1337
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
SEIZURES, STATUS EPILEPTICUS, AND CONTINUOUS EEG IN THE ICU
FIGURE 6-4
EEG monitoring guides the approach to both clinically apparent and convulsive status
epilepticus in the emergency and critical care settings (A) and to a broad differential
diagnosis considered in the evaluation of a patient with encephalopathy, coma, or other
disorder of consciousness (B). Increasing availability of EEG in the emergency setting (A) may
enable more precise management of the patient with established convulsive status
epilepticus by distinguishing pharmacologic sedation, progression to refractory
nonconvulsive seizures, and nonepileptic spells. EEG has numerous roles in patients who are
critically ill with encephalopathy, coma, and disorders of consciousness (B), including
detection of nonconvulsive seizures or nonconvulsive status epilepticus, evaluation for
ictal-interictal continuum activity consistent with possible nonconvulsive status, tissue
dysfunction due to secondary brain injury or delayed cerebral ischemia, and cognitive-motor
dissociation, in which consciousness is only evident through advanced monitoring. For all
these scenarios, complementary multimodality monitoring data can add contextual
information, which can be evaluated along with EEG monitoring for concordance and
iterative response to treatment.
EEG = electroencephalography; FDG CT-PET = fludeoxyglucose computed tomography positron emission
tomography; Rx = pharmacologic management; SAH = subarachnoid hemorrhage; SE = status epilepticus;
TBI = traumatic brain injury.
1338 OCTOBER 2021
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
Apart from diagnosing and monitoring seizure activity, other diagnostic roles for
EEG have been demonstrated recently in diverse patient cohorts: monitoring for
ischemia after subarachnoid hemorrhage; diagnosing covert consciousness in
patients who are apparently comatose; and predicting neurologic recovery after
cardiac arrest, primary acute brain injury, or resolution of status epilepticus.
ACKNOWLEDGMENT
This work was supported by a grant from the National Institutes of Health/
National Institute of Neurological Disorders and Stroke (1K23NS105950).
REFERENCES
1 Claassen J, Mayer SA, Kowalski RG, et al. 9 Beniczky S, Hirsch LJ, Kaplan PW, et al. Unified
Detection of electrographic seizures with EEG terminology and criteria for nonconvulsive
continuous EEG monitoring in critically ill status epilepticus. Epilepsia 2013;54(suppl 6):
patients. Neurology 2004;62(10):1743-1748. 28-29. doi:10.1111/epi.12270
doi:10.1212/01.wnl.0000125184.88797.62
10 Leitinger M, Beniczky S, Rohracher A, et al.
2 Westover MB, Shafi MM, Bianchi MT, et al. The Salzburg consensus criteria for non-convulsive
probability of seizures during EEG monitoring in status epilepticus—approach to clinical
critically ill adults. Clin Neurophysiol 2015;126(3): application. Epilepsy Behav 2015;49:158-163.
463-471. doi:10.1016/j.clinph.2014.05.037 doi:10.1016/j.yebeh.2015.05.007
3 O'Rourke D, Chen PM, Gaspard N, et al. Response 11 Leitinger M, Trinka E, Gardella E, et al. Diagnostic
rates to anticonvulsant trials in patients with accuracy of the Salzburg EEG criteria for
triphasic-wave EEG patterns of uncertain non-convulsive status epilepticus: a
significance. Neurocrit Care 2016;24(2):233-239. retrospective study. Lancet Neurol 2016;15(10):
doi:10.1007/s12028-015-0151-8 1054-1062. doi:10.1016/S1474-4422(16)30137-5
4 Vespa PM, Nuwer MR, Nenov V, et al. Increased 12 Hirsch LJ, Fong MWK, Leitinger L, et al. American
incidence and impact of nonconvulsive and Clinical Neurophysiology Society's Standardized
convulsive seizures after traumatic brain Critical Care EEG Terminology: 2021 version. J Clin
injury as detected by continuous Neurophysiol 2021;38(1):1-29. doi:10.1097/
electroencephalographic monitoring. WNP.0000000000000806
J Neurosurg 1999;91(5):750-760.
13 Struck AF, Ustun B, Ruiz AR, et al. Association of
doi:10.3171/jns.1999.91.5.0750
an electroencephalography-based risk score
5 Claassen J, Hirsch LJ, Frontera JA, et al. with seizure probability in hospitalized patients.
Prognostic significance of continuous EEG JAMA Neurol 2017;74(12):1419-1424.
monitoring in patients with poor-grade doi:10.1001/jamaneurol.2017.2459
subarachnoid hemorrhage. Neurocrit Care 2006;
14 Struck AF, Tabaeizadeh M, Schmitt SE, et al.
4(2):103-112. doi:10.1385/NCC:4:2:103
Assessment of the validity of the 2HELPS2B
6 Vespa PM, McArthur DL, Xu Y, et al. score for inpatient seizure risk prediction.
Nonconvulsive seizures after traumatic brain JAMA Neurol 2020;77(4):500-507.
injury are associated with hippocampal doi:10.1001/jamaneurol.2019.4656
atrophy. Neurology 2010;75(9):792-798.
15 Fung FW, Fan J, Vala L, et al. EEG monitoring
doi:10.1212/WNL.0b013e3181f07334
duration to identify electroencephalographic
7 Herman ST, Abend NS, Bleck TP, et al. Consensus seizures in critically ill children.
statement on continuous EEG in critically ill Neurology 2020;95(11):e1599-e1608.
adults and children, part I: indications. doi:10.1212/WNL.0000000000010421
J Clin Neurophysiol 2015;32(2):87-95.
16 Vespa P, Tubi M, Claassen J, et al. Metabolic
doi:10.1097/WNP.0000000000000166
crisis occurs with seizures and periodic
8 O'Connor KL, Westover MB, Phillips MT, et al. discharges after brain trauma. Ann Neurol 2016;
High risk for seizures following subarachnoid 79(4):579-590. doi:10.1002/ana.24606
hemorrhage regardless of referral bias.
17 Claassen J, Perotte A, Albers D, et al.
Neurocrit Care 2014;21(3):476-482.
Nonconvulsive seizures after subarachnoid
doi:10.1007/s12028-014-9974-y
hemorrhage: multimodal detection and
outcomes. Ann Neurol 2013;74(1):53-64.
doi:10.1002/ana.23859
CONTINUUMJOURNAL.COM 1339
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
SEIZURES, STATUS EPILEPTICUS, AND CONTINUOUS EEG IN THE ICU
18 Husain AM, Lee JW, Kolls BJ, et al. Randomized 30 DeLorenzo RJ, Waterhouse EJ, Towne AR, et al.
trial of lacosamide versus fosphenytoin for Persistent nonconvulsive status epilepticus
nonconvulsive seizures. Ann Neurol 2018;83(6): after the control of convulsive status
1174-1185. doi:10.1002/ana.25249 epilepticus. Epilepsia 1998;39(8):833-840.
doi:10.1111/j.1528-1157.1998.tb01177.x
19 Barra ME, Phillips KM, Chung DY, Rosenthal ES. A
novel correction equation avoids 31 Alkhachroum AM, Rubinos C, Chatterjee A, et al.
high-magnitude errors in interpreting therapeutic Rates and trends of endotracheal intubation in
drug monitoring of phenytoin among critically ill patients with status epilepticus. Neurohospitalist
patients. Ther Drug Monit 2020;42(4):617-625. 2019;9(4):190-196. doi:10.1177/1941874419830496
doi:10.1097/FTD.0000000000000739
32 Rosenthal ES, Claassen J, Wainwright MS, et al.
20 Treiman DM, Meyers PD, Walton NY, et al. A Brexanolone as adjunctive therapy in
comparison of four treatments for generalized super-refractory status epilepticus. Ann Neurol
convulsive status epilepticus. Veterans Affairs 2017;82(3):342-352. doi:10.1002/ana.25008
Status Epilepticus Cooperative Study
33 Subramaniam T, Jain A, Hall LT, et al. Lateralized
Group. N Engl J Med 1998;339(12):792-798.
periodic discharges frequency correlates with
doi:10.1056/NEJM199809173391202
glucose metabolism. Neurology 2019;92(7):
21 Alldredge BK, Gelb AM, Isaacs SM, et al. A e670-e674. doi:10.1212/WNL.0000000000006903
comparison of lorazepam, diazepam, and
34 Das AS, Lee JW, Rosenthal ES, Vaitkevicius H.
placebo for the treatment of out-of-hospital
Successful wean despite emergence of
status epilepticus. N Engl J Med 2001;345(9):
ictal-interictal EEG patterns during the weaning
631-637. doi:10.1056/NEJMoa002141
of prolonged burst-suppression therapy for
22 Silbergleit R, Durkalski V, Lowenstein D, et al. super-refractory status epilepticus.
Intramuscular versus intravenous therapy for Neurocrit Care 2018;29(3):452-462.
prehospital status epilepticus. N Engl J Med 2012; doi:10.1007/s12028-018-0552-6
366(7):591-600. doi:10.1056/NEJMoa1107494
35 Thompson SA, Hantus S. Highly epileptiform
23 Sathe AG, Tillman H, Coles LD, et al. Underdosing bursts are associated with seizure recurrence.
of benzodiazepines in patients with status J Clin Neurophysiol 2016;33(1):66-71.
epilepticus enrolled in established status doi:10.1097/WNP.0000000000000232
epilepticus treatment trial. Acad Emerg Med
36 Johnson EL, Martinez NC, Ritzl EK. EEG
2019;26(8):940-943. doi:10.1111/acem.13811
characteristics of successful burst suppression
24 Alldredge BK, Lowenstein DH, Simon RP. for refractory status epilepticus. Neurocrit Care
Placebo-controlled trial of intravenous 2016;25(3):407-414. doi:10.1007/s12028-016-0294-2
diphenylhydantoin for short-term treatment of
37 Rubin DB, Angelini B, Shoukat M, et al.
alcohol withdrawal seizures. Am J Med 1989;
Electrographic predictors of successful weaning
87(6):645-648. doi:10.1016/s0002-9343(89)80397-3
from anaesthetics in refractory status
25 Gaspard N, Foreman B, Judd LM, et al. epilepticus. Brain 2020;143(4):1143-1157.
Intravenous ketamine for the treatment of doi:10.1093/brain/awaa069
refractory status epilepticus: a retrospective
38 Ong C, Gilmore E, Claassen J, et al. Impact of
multicenter study. Epilepsia 2013;54(8):1498-1503.
prolonged periodic epileptiform discharges on
doi:10.1111/epi.12247
coma prognosis. Neurocrit Care 2012;17(1):39-44.
26 Chamberlain JM, Kapur J, Shinnar S, et al. doi:10.1007/s12028-012-9728-7
Efficacy of levetiracetam, fosphenytoin, and
39 Tabaeizadeh M, Aboul Nour H, Shoukat M, et al.
valproate for established status epilepticus
Burden of epileptiform activity predicts
by age group (ESETT): a double-blind,
discharge neurologic outcomes in severe acute
responsive-adaptive, randomised controlled
ischemic stroke. Neurocrit Care 2020;32(3):
trial. Lancet 2020;395(10231):1217-1224.
697-706. doi:10.1007/s12028-020-00944-0
doi:10.1016/S0140-6736(20)30611-5
40 De Marchis GM, Pugin D, Meyers E, et al. Seizure
27 Kapur J, Elm J, Chamberlain JM, et al. Randomized
burden in subarachnoid hemorrhage associated
trial of three anticonvulsant medications for
with functional and cognitive outcome.
status epilepticus. N Engl J Med 2019;381(22):
Neurology 2016;86(3):253-260. doi:10.1212/
2103-2113. doi:10.1056/NEJMoa1905795
WNL.0000000000002281
28 Cervenka MC, Hocker S, Koenig M, et al. Phase
41 Zafar SF, Postma EN, Biswal S, et al. Effect of
I/II multicenter ketogenic diet study for adult
epileptiform abnormality burden on neurologic
superrefractory status epilepticus.
outcome and antiepileptic drug management
Neurology 2017;88(10):938-943.
after subarachnoid hemorrhage. Clin
doi:10.1212/WNL.0000000000003690
Neurophysiol 2018;129(11):2219-2227.
29 Tuppurainen KM, Ritvanen JG, Mustonen H, doi:10.1016/j.clinph.2018.08.015
Kamppi LS. Predictors of mortality at one year
42 Lee H, Mizrahi MA, Hartings JA, et al. Continuous
after generalized convulsive status epilepticus.
electroencephalography after moderate to
Epilepsy Behav 2019;101(pt B):106411.
severe traumatic brain injury. Crit Care
doi:10.1016/j.yebeh.2019.07.012
Med 2019;47(4):574-582.
doi:10.1097/CCM.0000000000003639
1340 OCTOBER 2021
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
43 Naidech AM, Kreiter KT, Janjua N, et al. Phenytoin 56 Lissak IA, Zafar SF, Westover MB, et al. Soluble
exposure is associated with functional and ST2 is associated with new epileptiform
cognitive disability after subarachnoid abnormalities following nontraumatic
hemorrhage. Stroke 2005;36(3):583-587. subarachnoid hemorrhage. Stroke 2020;51(4):
doi:10.1161/01.STR.0000141936.36596.1e 1128-1134. doi:10.1161/STROKEAHA.119.028515
44 Kim JA, Boyle EJ, Wu AC, et al. Epileptiform 57 Labar DR, Fisch BJ, Pedley TA, et al. Quantitative
activity in traumatic brain injury predicts EEG monitoring for patients with subarachnoid
post-traumatic epilepsy. Ann Neurol 2018;83(4): hemorrhage. Electroencephalogr Clin
858-862. doi:10.1002/ana.25211 Neurophysiol 1991;78(5):325-332. doi:
10.1016/0013-4694(91)90094-k
45 Chen DF, Kumari P, Haider HA, et al. Association
of epileptiform abnormality on 58 Gollwitzer S, Groemer T, Rampp S, et al. Early
electroencephalography with development of prediction of delayed cerebral ischemia in
epilepsy after acute brain injury. Neurocrit Care subarachnoid hemorrhage based on quantitative
2021. doi:10.1007/s12028-020-01182-0 EEG: a prospective study in adults.
Clin Neurophysiol 2015;126(8):1514-1523.
46 Echlin FA, Arnett V, Zoll J. Paroxysmal high
doi:10.1016/j.clinph.2014.10.215
voltage discharges from isolated and partially
isolated human and animal cerebral cortex. 59 Claassen J, Hirsch LJ, Kreiter KT, et al.
Electroencephalogr Clin Neurophysiol 1952;4(2): Quantitative continuous EEG for detecting
147-164. doi:10.1016/0013-4694(52)90004-7 delayed cerebral ischemia in patients with
poor-grade subarachnoid hemorrhage. Clin
47 Chatrian GE, Vizioli R. [Case of degenerative
Neurophysiol 2004;115(12):2699-2710.
disease of uncertain nosographical
doi:10.1016/j.clinph.2004.06.017
systematization]. Riv Neurol 1952;22:715-720.
60 Rots ML, van Putten MJAM, Hoedemaekers CWE,
48 Chatrian GE, Shaw CM, Leffman H. The
Horn J. Continuous EEG monitoring for early
significance of periodic lateralized epileptiform
detection of delayed cerebral ischemia in
discharges in EEG: an electrographic, clinical and
subarachnoid hemorrhage: a pilot study.
pathological study. Electroencephalogr Clin
Neurocrit Care 2016;24(2):207-216.
Neurophysiol 1964;17:177-193. doi:10.1016/0013-
doi:10.1007/s12028-015-0205-y
4694(64)90149-x
61 Vespa PM, Nuwer MR, Juhasz C, et al. Early
49 Chatrian GE, Shaw CM, Luttrell CN. Focal
detection of vasospasm after acute
electroencephalographic seizure discharges in
subarachnoid hemorrhage using continuous EEG
acute cerebral infarction. Electrographic, clinical,
ICU monitoring. Electroencephalogr Clin
and pathological observations. Neurology 1965;
Neurophysiol 1997;103(6):607-615.
15:123-131. doi:10.1212/wnl.15.2.123
doi:10.1016/s0013-4694(97)00071-0
50 Alajouanine T, Lecasble R, Remond A. Slow
62 Echlin FA, Arnett V, Zoll J. Paroxysmal high
graphic paroxystic elements of periodic
voltage and rhythmic low voltage discharges
occurrence; electrical and clinical correlations [in
from isolated and partially isolated human
French]. Rev Neurol (Paris) 1955;93(2):477-478.
cortex. J Nerv Ment Dis 1952;116(1):65-72.
51 Struck AF, Westover MB, Hall LT, et al. Metabolic
63 Hartings JA, Williams AJ, Tortella FC. Occurrence
correlates of the ictal-interictal continuum:
of nonconvulsive seizures, periodic epileptiform
FDG-PET during continuous EEG. Neurocrit Care
discharges, and intermittent rhythmic delta
2016;24(3):324-331. doi:10.1007/s12028-016-0245-y
activity in rat focal ischemia. Exp Neurol 2003;
52 Akbik F, Robertson M, Das AS, et al. The PET 179(2):139-149. doi:10.1016/s0014-4886(02)00013-4
sandwich: using serial FDG-PET scans with
64 Dreier JP, Major S, Pannek HW, et al. Spreading
interval burst suppression to assess ictal
convulsions, spreading depolarization and
components of disease. Neurocrit Care 2020;
epileptogenesis in human cerebral cortex. Brain
33(3):657-669. doi:10.1007/s12028-020-00956-w
2012;135(pt 1):259-275. doi:10.1093/brain/awr303
53 Witsch J, Frey HP, Schmidt JM, et al.
65 Nuwer MR, Jordan SE, Ahn SS. Evaluation of
Electroencephalographic periodic discharges
stroke using EEG frequency analysis and
and frequency-dependent brain tissue hypoxia
topographic mapping. Neurology 1987;37(7):
in acute brain injury. JAMA Neurol 2017;74(3):
1153-1159. doi:10.1212/wnl.37.7.1153
301-309. doi:10.1001/jamaneurol.2016.5325
66 Kim JA, Rosenthal ES, Biswal S, et al. Epileptiform
54 Vespa PM, O'Phelan K, Shah M, et al. Acute
abnormalities predict delayed cerebral ischemia
seizures after intracerebral hemorrhage: a factor
in subarachnoid hemorrhage. Clin Neurophysiol
in progressive midline shift and outcome.
2017;128(6):1091-1099. doi:10.1016/j.
Neurology 2003;60(9):1441-1446.
clinph.2017.01.016
doi:10.1212/01.wnl.0000063316.47591.b4
67 Rosenthal ES, Biswal S, Zafar SF, et al. Continuous
55 Claassen J, Albers D, Schmidt JM, et al.
electroencephalography predicts delayed
Nonconvulsive seizures in subarachnoid
cerebral ischemia after subarachnoid
hemorrhage link inflammation and
hemorrhage: a prospective study of diagnostic
outcome. Ann Neurol 2014;75(5):771-781.
accuracy. Ann Neurol 2018;83(5):958-969.
doi:10.1002/ana.24166
doi:10.1002/ana.25232
CONTINUUMJOURNAL.COM 1341
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
SEIZURES, STATUS EPILEPTICUS, AND CONTINUOUS EEG IN THE ICU
68 Muniz CF, Shenoy AV, O'Connor KL, et al. Clinical 79 Sanchez-Porras R, Zheng Z, Sakowitz OW.
development and implementation of an Pharmacological modulation of spreading
institutional guideline for prospective EEG depolarizations. Acta Neurochir Suppl 2015;120:
monitoring and reporting of delayed cerebral 153-157. doi:10.1007/978-3-319-04981-6_26
ischemia. J Clin Neurophysiol 2016;33(3):217-226.
80 Sanchez-Porras R, Santos E, Scholl M, et al.
doi:10.1097/WNP.0000000000000281
Ketamine modulation of the haemodynamic
69 Lissak IA, Locascio JJ, Zafar SF, et al. response to spreading depolarization in the
Electroencephalography, hospital complications, gyrencephalic swine brain. J Cereb Blood Flow
and longitudinal outcomes after subarachnoid Metab 2017;37(5):1720-1734.
hemorrhage. Neurocrit Care 2021;1-12. doi:10.1177/0271678X16646586
doi:10.1007/s12028-020-01177-x
81 Carlson AP, Abbas M, Alunday RL, et al.
70 Hartings JA, Shuttleworth CW, Kirov SA, et al. The Spreading depolarization in acute brain injury
continuum of spreading depolarizations in acute inhibited by ketamine: a prospective,
cortical lesion development: examining Leao's randomized, multiple crossover trial. J Neurosurg
legacy. J Cereb Blood Flow Metab 2017;37(5): 2018;1-7. doi:10.3171/2017.12.JNS171665
1571-1594. doi:10.1177/0271678X16654495
82 Reinhart KM, Shuttleworth CW. Ketamine
71 Dreier JP, Fabricius M, Ayata C, et al. Recording, reduces deleterious consequences of spreading
analysis, and interpretation of spreading depolarizations. Exp Neurol 2018;305:121-128.
depolarizations in neurointensive care: review doi:10.1016/j.expneurol.2018.04.007
and recommendations of the COSBID research
83 Santos E, Olivares-Rivera A, Major S, et al. Lasting
group. J Cereb Blood Flow Metab 2017;37(5):
s-ketamine block of spreading depolarizations in
1595-1625. doi:10.1177/0271678X16654496
subarachnoid hemorrhage: a retrospective
72 Drenckhahn C, Winkler MK, Major S, et al. cohort study. Crit Care 2019;23(1):427.
Correlates of spreading depolarization in human doi:10.1186/s13054-019-2711-3
scalp electroencephalography. Brain 2012;
84 Mohammad LM, Abbas M, Shuttleworth CW,
135(pt 3):853-868. doi:10.1093/brain/aws010
et al. Spreading depolarization may represent a
73 Hartings JA, Watanabe T, Bullock MR, et al. novel mechanism for delayed fluctuating
Spreading depolarizations have prolonged direct neurological deficit after chronic subdural
current shifts and are associated with poor hematoma evacuation. J Neurosurg 2020;1-9.
outcome in brain trauma. Brain 2011;134(pt 5): doi:10.3171/2020.1.JNS192914
1529-1540. doi:10.1093/brain/awr048
85 Kimchi EY, Neelagiri A, Whitt W, et al. Clinical
74 Strong AJ, Macdonald RL. Cortical spreading EEG slowing correlates with delirium severity
ischemia in the absence of proximal vasospasm and predicts poor clinical outcomes.
after aneurysmal subarachnoid hemorrhage: Neurology 2019;93(13):e1260-e1271.
evidence for a dual mechanism of delayed doi:10.1212/WNL.0000000000008164
cerebral ischemia. J Cereb Blood Flow Metab
86 Edlow BL, Chatelle C, Spencer CA, et al. Early
2012;32(2):201-202. doi:10.1038/jcbfm.2011.170
detection of consciousness in patients with
75 Drenckhahn C, Windler C, Major S, et al. acute severe traumatic brain injury. Brain 2017;
Complications in aneurysmal subarachnoid 140(9):2399-2414. doi:10.1093/brain/awx176
hemorrhage patients with and without subdural
87 Chatelle C, Rosenthal ES, Bodien YG, et al. EEG
electrode strip for electrocorticography. J Clin
correlates of language function in traumatic
Neurophysiol 2016;33(3):250-259.
disorders of consciousness. Neurocrit Care
doi:10.1097/WNP.0000000000000274
2020;33(2):449-457. doi:10.1007/s12028-019-
76 Hartings JA, Andaluz N, Bullock MR, et al. 00904-3
Prognostic value of spreading depolarizations in
88 Claassen J, Doyle K, Matory A, et al. Detection of
patients with severe traumatic brain injury.
brain activation in unresponsive patients with
JAMA Neurol 2020;77(4):489-499.
acute brain injury. N Engl J Med 2019;380(26):
doi:10.1001/jamaneurol.2019.4476
2497-2505. doi:10.1056/NEJMoa1812757
77 Hertle DN, Dreier JP, Woitzik J, et al. Effect of
89 Malinowska U, Chatelle C, Bruno MA, et al.
analgesics and sedatives on the occurrence of
Electroencephalographic profiles for
spreading depolarizations accompanying acute
differentiation of disorders of consciousness.
brain injury. Brain 2012;135(pt 8):2390-2398.
Biomed Eng Online 2013;12:109.
doi:10.1093/brain/aws152
doi:10.1186/1475-925X-12-109
78 Sanchez-Porras R, Santos E, Scholl M, et al. The
90 Lesenfants D, Habbal D, Chatelle C, et al. Toward
effect of ketamine on optical and electrical
an attention-based diagnostic tool for patients
characteristics of spreading depolarizations in
with locked-in syndrome. Clin EEG Neurosci 2018;
gyrencephalic swine cortex.
49(2):122-135. doi:10.1177/1550059416674842
Neuropharmacology 2014;84:52-61.
doi:10.1016/j.neuropharm.2014.04.018 91 Greer DM, Rosenthal ES, Wu O.
Neuroprognostication of hypoxic-ischaemic
coma in the therapeutic hypothermia era.
Nat Rev Neurol 2014;10(4):190-203. doi:10.1038/
nrneurol.2014.36
1342 OCTOBER 2021
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
92 Hofmeijer J, Tjepkema-Cloostermans MC, van 100 Purandare M, Ehlert AN, Vaitkevicius H, et al. The
Putten MJ. Burst-suppression with identical role of cEEG as a predictor of patient outcome
bursts: a distinct EEG pattern with poor outcome and survival in patients with intraparenchymal
in postanoxic coma. Clin Neurophysiol 2014; hemorrhages. Seizure 2018;61:122-127.
125(5):947-954. doi:10.1016/j.clinph.2013.10.017 doi:10.1016/j.seizure.2018.08.014
93 Amorim E, Rittenberger JC, Zheng JJ, et al. 101 Vespa PM, Olson DM, John S, et al. Evaluating
Continuous EEG monitoring enhances the clinical impact of rapid response
multimodal outcome prediction in electroencephalography: the DECIDE
hypoxic-ischemic brain injury. Multicenter Prospective Observational Clinical
Resuscitation 2016;109:121-126. Study. Crit Care Med 2020;48(9):1249-1257.
doi:10.1016/j.resuscitation.2016.08.012 doi:10.1097/CCM.0000000000004428
94 Solanki P, Coppler PJ, Kvaloy JT, et al. Association 102 Treiman DM, Walton NY, Kendrick C. A
of antiepileptic drugs with resolution of progressive sequence of
epileptiform activity after cardiac arrest. electroencephalographic changes during
Resuscitation 2019;142:82-90. generalized convulsive status epilepticus.
doi:10.1016/j.resuscitation.2019.07.007 Epilepsy Res 1990;5(1):49-60. doi:10.1016/0920-
1211(90)90065-4
95 Tjepkema-Cloostermans MC, van Meulen FB,
Meinsma G, van Putten MJAM. A Cerebral 103 Swisher CB, Sinha SR. Utilization of quantitative
Recovery Index (CRI) for early prognosis in EEG trends for critical care continuous EEG
patients after cardiac arrest. Crit Care 2013;17(5): monitoring: a survey of neurophysiologists.
R252. doi:10.1186/cc13078 J Clin Neurophysiol 2016;33(6):538-544.
doi:10.1097/WNP.0000000000000287
96 Ghassemi MM, Amorim E, Pati SB, et al. An
enhanced Cerebral Recovery Index for coma 104 Fatuzzo D, Beuchat I, Alvarez V, et al. Does
prognostication following cardiac arrest. Annu continuous EEG influence prognosis in patients
Int Conf IEEE Eng Med Biol Soc 2015;2015: after cardiac arrest? Resuscitation 2018;132:
534-537. doi:10.1109/EMBC.2015.7318417 29-32. doi:10.1016/j.resuscitation.2018.08.023
97 Tjepkema-Cloostermans MC, Hofmeijer J, 105 Rossetti AO, Schindler K, Sutter R, et al.
Beishuizen A, et al. Cerebral Recovery Index: Continuous vs routine electroencephalogram in
reliable help for prediction of neurologic critically ill adults with altered consciousness
outcome after cardiac arrest. Crit Care Med 2017; and no recent seizure: a multicenter randomized
45(8):e789-e797. doi:10.1097/ clinical trial. JAMA Neurol 2020;77(10):1-8.
CCM.0000000000002412 doi:10.1001/jamaneurol.2020.2264
98 Nagaraj SB, Tjepkema-Cloostermans MC, Ruijter 106 Hill CE, Blank LJ, Thibault D, et al. Continuous EEG
BJ, et al. The revised Cerebral Recovery Index is associated with favorable hospitalization
improves predictions of neurological outcome outcomes for critically ill patients.
after cardiac arrest. Clin Neurophysiol 2018; Neurology 2019;92(1):e9-e18.
129(12):2557-2566. doi:10.1016/j.clinph.2018.10.004 doi:10.1212/WNL.0000000000006689
99 Ghassemi MM, Amorim E, Alhanai T, et al.
Quantitative electroencephalogram trends
predict recovery in hypoxic-ischemic
encephalopathy. Crit Care Med 2019;47(10):
1416-1423. doi:10.1097/CCM.0000000000003840
CONTINUUMJOURNAL.COM 1343
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
You might also like
- Management of Status Epilepticus, Refractory Status Epilepticus, and Super-Refractory Status EpilepticusDocument44 pagesManagement of Status Epilepticus, Refractory Status Epilepticus, and Super-Refractory Status EpilepticusOlga Manco GuzmánNo ratings yet
- Surgical Approaches To EpilepsyDocument13 pagesSurgical Approaches To EpilepsyJames E. WalkerNo ratings yet
- Edo Epileptico No ConvulsivoDocument10 pagesEdo Epileptico No Convulsivosprnv2No ratings yet
- TreatmentofStatusEpilepticus PDFDocument14 pagesTreatmentofStatusEpilepticus PDFAnonymous 7wo4ZBVaEvNo ratings yet
- ACNS Guideline Continuous Electroencephalography Monitoring in NeonatesDocument7 pagesACNS Guideline Continuous Electroencephalography Monitoring in NeonatesShanaHNo ratings yet
- Are We Prepared To Detect Subtle and Nonconvulsive Status Epilepticus in Critically Ill Patients?Document7 pagesAre We Prepared To Detect Subtle and Nonconvulsive Status Epilepticus in Critically Ill Patients?succa07No ratings yet
- Update On The Management of Status Epilepticus: Learning ObjectivesDocument4 pagesUpdate On The Management of Status Epilepticus: Learning Objectivesmoy9616No ratings yet
- Status Epilepticus in Adults A Brief Commentary For A Critical Care Nursingperspective Jpcic 1000117Document3 pagesStatus Epilepticus in Adults A Brief Commentary For A Critical Care Nursingperspective Jpcic 1000117Constanza Andrea Saldivia Blanco(RedSalud Magallanes)No ratings yet
- J Clinph 2013 03 031Document7 pagesJ Clinph 2013 03 031Andres Rojas JerezNo ratings yet
- G. Rees Cosgrove, M.D., F.R.C.S. (C) and Andrew J. Cole M.D., FRCP (C)Document11 pagesG. Rees Cosgrove, M.D., F.R.C.S. (C) and Andrew J. Cole M.D., FRCP (C)Jean Costan RNNo ratings yet
- The EEG of Status Epilepticus: Peter W. KaplanDocument9 pagesThe EEG of Status Epilepticus: Peter W. KaplanNathaly LapoNo ratings yet
- Status EpilepticusDocument10 pagesStatus Epilepticusabdi syahputraNo ratings yet
- Epilepsia - 2019 - Hanin - Cerebrospinal Fluid and Blood Biomarkers of Status EpilepticusDocument13 pagesEpilepsia - 2019 - Hanin - Cerebrospinal Fluid and Blood Biomarkers of Status EpilepticusAmira GharbiNo ratings yet
- Ref 5Document15 pagesRef 5Neha BhatiNo ratings yet
- Status Epilepticus in Critically Ill PatientsDocument11 pagesStatus Epilepticus in Critically Ill PatientsAkbal Nur KarimNo ratings yet
- So 2010Document10 pagesSo 2010Pablo Sebastián SaezNo ratings yet
- Lattanzi 2021Document6 pagesLattanzi 2021Ivan MihailovicNo ratings yet
- Muhlhofer 2018Document15 pagesMuhlhofer 2018bozasnachoNo ratings yet
- Sedatives in Neurocritical Care 2019 Curr Opin Crit CareDocument8 pagesSedatives in Neurocritical Care 2019 Curr Opin Crit CareCAMILO ERNESTO DAZA PERDOMONo ratings yet
- Posterior Reversible Encephalopathy Syndrome After Lumbar PunctureDocument2 pagesPosterior Reversible Encephalopathy Syndrome After Lumbar PunctureMedtext PublicationsNo ratings yet
- Awake CraniotomyDocument28 pagesAwake CraniotomyBeba EchevarriaNo ratings yet
- PN0520 EE PostanoxicMyoclonusDocument2 pagesPN0520 EE PostanoxicMyoclonusGian Franco Oneto TapiaNo ratings yet
- Anesthesia Related Seizure DisordersDocument9 pagesAnesthesia Related Seizure DisordersBudiBoyPratamaNo ratings yet
- Status Epilepticus Work-Up and Management in AdultsDocument9 pagesStatus Epilepticus Work-Up and Management in AdultsAnonymous QLadTClydkNo ratings yet
- NIH Public Access: Management of Pediatric Status EpilepticusDocument16 pagesNIH Public Access: Management of Pediatric Status EpilepticusDiego CedamanosNo ratings yet
- Spect PDFDocument14 pagesSpect PDFhalamadrid77No ratings yet
- Epilepsy: ACR Appropriateness CriteriaDocument3 pagesEpilepsy: ACR Appropriateness CriteriaLuwinda SariNo ratings yet
- Clinical-Neurophysiology 2016 MedicineDocument5 pagesClinical-Neurophysiology 2016 MedicinemateoNo ratings yet
- Pleds 2009 JamaDocument7 pagesPleds 2009 JamaRosiane Da Silva FontanaNo ratings yet
- Status Epileptikus HUT IDI 2017Document31 pagesStatus Epileptikus HUT IDI 2017Aulia Ayu PuspitaNo ratings yet
- Treatment Options For Posttraumatic Epilepsy: ReviewDocument7 pagesTreatment Options For Posttraumatic Epilepsy: ReviewOmarJoseCuberosMarcanoNo ratings yet
- Adult NCSE Power KN 2015Document5 pagesAdult NCSE Power KN 2015Hendra PermanaNo ratings yet
- Clinical Neurophysiology: Key PointsDocument5 pagesClinical Neurophysiology: Key PointsAndres AceroNo ratings yet
- Crise Convulsiva Provocada - ManejoDocument11 pagesCrise Convulsiva Provocada - Manejorafael rocha novaesNo ratings yet
- Fneur 11 00071Document10 pagesFneur 11 00071Nurvia AndrianiNo ratings yet
- Contents NCLDocument3 pagesContents NCLdewi najiraNo ratings yet
- Epilepsy: Ever-Changing States of Cortical Excitability: R. A. B. Badawy, D. R. Freestone, A. Lai AND M. J. CookDocument11 pagesEpilepsy: Ever-Changing States of Cortical Excitability: R. A. B. Badawy, D. R. Freestone, A. Lai AND M. J. CooknurhikmahNo ratings yet
- Fnana 12 00025Document11 pagesFnana 12 00025Mohamed TahaNo ratings yet
- An Update On The Management of Status Epilepticus in Adults 2016Document8 pagesAn Update On The Management of Status Epilepticus in Adults 2016Farmacia SantamariaNo ratings yet
- Schmitt 2012Document8 pagesSchmitt 2012nurdiansyahNo ratings yet
- MainDocument12 pagesMainbozasnachoNo ratings yet
- Continuous Amplitude-Integrated Electroencephalographic Monitoring Is A Useful Prognostic Tool For Hypothermia-Treated Cardiac Arrest PatientsDocument10 pagesContinuous Amplitude-Integrated Electroencephalographic Monitoring Is A Useful Prognostic Tool For Hypothermia-Treated Cardiac Arrest PatientsSachin DangiNo ratings yet
- Bravo 2021Document22 pagesBravo 2021Ivan MihailovicNo ratings yet
- Ene 12372Document7 pagesEne 12372Andres Rojas JerezNo ratings yet
- Continuous EEG Monitoring in The Intensive Care UnDocument7 pagesContinuous EEG Monitoring in The Intensive Care UnSara MendesNo ratings yet
- Neonatal Seizures: Alan Hill, MD, PHDDocument5 pagesNeonatal Seizures: Alan Hill, MD, PHDcainzkeinzNo ratings yet
- Review: Hartmut Meierkord, Martin HoltkampDocument11 pagesReview: Hartmut Meierkord, Martin HoltkampMelissa Peña LópezNo ratings yet
- Status Epileptic in Pediatric PDFDocument12 pagesStatus Epileptic in Pediatric PDFHanna SimbolonNo ratings yet
- 10.1016@B978 0 444 64032 1.00009 6Document18 pages10.1016@B978 0 444 64032 1.00009 6ilonaskorinNo ratings yet
- Back To Basics: The Pathophysiology of Epileptic Seizures: A Primer For PediatriciansDocument12 pagesBack To Basics: The Pathophysiology of Epileptic Seizures: A Primer For Pediatriciansgerson altamiranoNo ratings yet
- Heterotopia PV GruposDocument12 pagesHeterotopia PV GruposJuan D. HoyosNo ratings yet
- Long QT Syndrome and Seizures: Editorial CommentDocument2 pagesLong QT Syndrome and Seizures: Editorial CommentР. МөнхжинNo ratings yet
- Coma and Brain DeathDocument24 pagesComa and Brain DeathDean AccountNo ratings yet
- Current Status of Continuous Electroencephalographic Monitoring in Critically Ill ChildrenDocument7 pagesCurrent Status of Continuous Electroencephalographic Monitoring in Critically Ill ChildrenMauricio RiveraNo ratings yet
- Jurnal EEGDocument17 pagesJurnal EEGNurul FajriNo ratings yet
- Mcanism B NeurodegenerativeDocument13 pagesMcanism B NeurodegenerativeAlin CiubotaruNo ratings yet
- Utility of Routine EEG in Emergency Room and Inpatient ServiceDocument16 pagesUtility of Routine EEG in Emergency Room and Inpatient Servicefedcaf18No ratings yet
- Chronic Immune-Mediated Demyelinating NeuropathiesDocument21 pagesChronic Immune-Mediated Demyelinating NeuropathiesArbey Aponte PuertoNo ratings yet
- 1 5136382648058380752Document11 pages1 5136382648058380752ednasu1No ratings yet
- Antibiotic Prophylaxis in Open Fractures: Evidence, Evolving Issues, and RecommendationsDocument7 pagesAntibiotic Prophylaxis in Open Fractures: Evidence, Evolving Issues, and RecommendationsEstefany Almonte MatiasNo ratings yet
- 8 Fases en IAMDocument14 pages8 Fases en IAMednasu1No ratings yet
- October Sodium DisordersDocument20 pagesOctober Sodium DisordersAngel GarciaNo ratings yet
- Nacl Kad 2Document12 pagesNacl Kad 2Ida LemonNo ratings yet
- 2015 Sodium Bicarbonate in The Treatment of Acidosis in SepsisDocument8 pages2015 Sodium Bicarbonate in The Treatment of Acidosis in Sepsisednasu1No ratings yet
- Ureteroureterostomy For Reflux Duplex SystemsDocument5 pagesUreteroureterostomy For Reflux Duplex Systemsjithin rNo ratings yet
- Cases Journal: Acquired Nonobstructive Urinary Bladder Diverticulum: A CaseDocument3 pagesCases Journal: Acquired Nonobstructive Urinary Bladder Diverticulum: A CaseIrma Suriani DarwisNo ratings yet
- Pathophysiology of Severe AnemiaDocument3 pagesPathophysiology of Severe AnemiaChrizley Shawn DeroniaNo ratings yet
- Clinico-Radiological Profile in Covid - 19 PatientsDocument6 pagesClinico-Radiological Profile in Covid - 19 PatientsInternational Journal of Innovative Science and Research Technology100% (1)
- Drug Study MethimazoleDocument2 pagesDrug Study MethimazoleEricka MunsayacNo ratings yet
- Clinical Chemsitry AnsweredDocument4 pagesClinical Chemsitry AnsweredStephany Mae ChiNo ratings yet
- Benemérita Universidad Autónoma de Puebla: Preparatoria 2 de Octubre de 1968Document16 pagesBenemérita Universidad Autónoma de Puebla: Preparatoria 2 de Octubre de 1968martinNo ratings yet
- Calcium Gluconate Dosage PlusDocument8 pagesCalcium Gluconate Dosage PlusJaved ArifNo ratings yet
- Seyfert 2009Document6 pagesSeyfert 2009yane sofNo ratings yet
- Xeljanz Initiation ChecklistDocument8 pagesXeljanz Initiation ChecklistRawan ZayedNo ratings yet
- Day 12 - Ncm-109 7b InfancyDocument59 pagesDay 12 - Ncm-109 7b InfancySheena Patricia ArasulaNo ratings yet
- Cerebral Salt Wasting Syndrome - StatPearls - NCBI BookshelfDocument4 pagesCerebral Salt Wasting Syndrome - StatPearls - NCBI BookshelfOnggo WiliyantoNo ratings yet
- Patient & Family EducationDocument3 pagesPatient & Family EducationJenjendeuk kimNo ratings yet
- Medical Terminology: Study GuideDocument143 pagesMedical Terminology: Study GuideRaniel ChuaNo ratings yet
- Diagnosis and Management of Blepharitis: An Optometrist's PerspectiveDocument8 pagesDiagnosis and Management of Blepharitis: An Optometrist's PerspectiveMutiara Permata SariNo ratings yet
- Peds Ati ReviewDocument32 pagesPeds Ati ReviewMorgan100% (41)
- Lincomycin: Drug Information: ALERT: US Boxed WarningDocument12 pagesLincomycin: Drug Information: ALERT: US Boxed WarningsadiaNo ratings yet
- BMJ k2693 FullDocument9 pagesBMJ k2693 FullFirman SyahNo ratings yet
- Penis & DisordersDocument54 pagesPenis & Disordersshivay100% (1)
- Chapter One - InclusivenessDocument22 pagesChapter One - InclusivenessAshenafi PaulosNo ratings yet
- College Final Paper 1Document6 pagesCollege Final Paper 1Rita PrinceNo ratings yet
- MEDBIO KROK-1 English 2019-2020Document65 pagesMEDBIO KROK-1 English 2019-2020Катерина КабишNo ratings yet
- Hema Lec Week 16 Leukocyte Disorders Part 2Document4 pagesHema Lec Week 16 Leukocyte Disorders Part 2Max RuideraNo ratings yet
- Wilson Disease - Treatment and Prognosis - UpToDateDocument13 pagesWilson Disease - Treatment and Prognosis - UpToDatericanoy191No ratings yet
- Case Study GonorrheaDocument19 pagesCase Study GonorrheaErika ThereseNo ratings yet
- Classification SystemsDocument11 pagesClassification SystemsKelli StevensNo ratings yet
- Juhairina: Medical Nutrition Therapy For Disorders of The Lower Gastrointestinal TractDocument82 pagesJuhairina: Medical Nutrition Therapy For Disorders of The Lower Gastrointestinal Tractdesy100% (1)
- Pedia Uworld DrillsDocument9 pagesPedia Uworld DrillsMhing's Printing ServicesNo ratings yet
- A Case of Brain Death During PregnancyDocument52 pagesA Case of Brain Death During PregnancyMa Pilar Peñaflor AñonuevoNo ratings yet
- NAN KE ANDROLOGY Yang Wei - Erectile Dysfunction From Chinese Medicine and BiomedicalDocument100 pagesNAN KE ANDROLOGY Yang Wei - Erectile Dysfunction From Chinese Medicine and BiomedicalLeo100% (1)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (6)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (28)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (1)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (404)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (81)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (3)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningFrom EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningRating: 4 out of 5 stars4/5 (3)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)From EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)No ratings yet
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- Gut: the new and revised Sunday Times bestsellerFrom EverandGut: the new and revised Sunday Times bestsellerRating: 4 out of 5 stars4/5 (392)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (44)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- The Marshmallow Test: Mastering Self-ControlFrom EverandThe Marshmallow Test: Mastering Self-ControlRating: 4.5 out of 5 stars4.5/5 (58)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- Dark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingFrom EverandDark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingRating: 4 out of 5 stars4/5 (1138)
- Troubled: A Memoir of Foster Care, Family, and Social ClassFrom EverandTroubled: A Memoir of Foster Care, Family, and Social ClassRating: 4.5 out of 5 stars4.5/5 (26)