Professional Documents
Culture Documents
2012 - Catatonia Emergency Department
Uploaded by
sirodimOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
2012 - Catatonia Emergency Department
Uploaded by
sirodimCopyright:
Available Formats
Downloaded from http://emj.bmj.com/ on February 27, 2015 - Published by group.bmj.
com
Review
Catatonia in the emergency department
Walter Jaimes-Albornoz,1,2 Jordi Serra-Mestres2
1
Department of Psychiatry, ABSTRACT in an inadequate management and important
Complejo Hospitalario de Disturbances of the level of awareness are a frequent morbidity and mortality.11 12
Navarra, Pamplona, Spain
2 motive of attendance to emergency departments where Given the frequent acute presentation of cata-
Central and North West
London NHS Foundation Trust, the initial assessment and management will determine tonia in which stupor is a prominent feature, it is
London, UK the direction of their outcome. The syndrome of often the case that patients with this condition first
catatonia must be taken into consideration and although come into contact with medical practitioners in
Correspondence to it is normally associated with psychiatric diagnoses, it is emergency departments where catatonia is seldom
Dr Jordi Serra-Mestres,
also very often found in a great variety of neurological identified or managed adequately and where the
Woodland Centre, Hillingdon
Hospital, Central & North West and medical conditions. Due to the clinical complexity of presentation is often attributed to psychological
London NHS Foundation Trust, catatonia, there are still difficulties in its correct problems.13e15
Uxbridge, Middlesex UB8 3NN, identification and initial management, something that
UK;
jordi.serra-mestres@nhs.net
leads to diagnostic delays and increased morbidity and METHODS
mortality. In this article, a review of the literature on A literature search of MEDLINE/PubMed was
Accepted 10 January 2012 catatonia is presented with the aim of assisting undertaken, ranging from its first registers to July
Published Online First emergency department doctors (and clinicians assessing 2011. The following key words were cross-refer-
2 March 2012 patients in emergency situations) in considering this enced: ‘catatonia’ and/or ‘catatonic syndrome’ with
condition in the differential diagnosis of stupor due to its ‘organic’, ‘complications’, ‘emergency’ and ‘treat-
high frequency of association with organic pathology. ment’. Additionally, a manual revision of the liter-
ature referred to in the identified articles was
undertaken in order to obtain old or non-indexed
references. All articles were considered for inclusion
INTRODUCTION if their content was felt to be relevant to this review.
Catatonia is a neuropsychiatric syndrome charac-
terised by psychomotor abnormalities that is CLINICAL FEATURES
observed in a variety of medical, neurological and Catatonia usually presents acutely although some
psychiatric disorders. The concept was introduced forms adopt a chronic course and is characterised
by Karl Ludwig Kahlbaum in 1874 who described by motor, behavioural, affective and autonomic
the presence of stupor, mutism, rigidity, nega- signs. Around 40 signs of catatonia have been
tivism, catalepsy and echophenomena in a group of described16 and they can be grouped in two clinical
patients with depression, mania, epilepsy, neuro- forms: a retarded-stuporous variety, which is the
syphilis and tuberculosis.1 Catatonia was later most common, and an excited one. The former
incorporated into the nosological entity of schizo- presents with stupor, mutism, rigidity, immobility,
phrenia, first by Kraepelin and later by Bleuler, negativism, catalepsy (and waxy flexibility or
although both described catatonia in various rigidity), posturing and echophenomena. Excite-
organic disorders. However, this observation did ment, aggressivity and impulsivity are the main
not seem to transcend into a wider understanding hallmarks of the excited form of catatonia. These
of catatonia.2 From its original description, reports two clinical forms may occur in the same patient
of catatonia associated with organic disease were during the same episode. The underlying cause does
abundant but this did not succeed in removing not seem to determine the form of presentation but
catatonia from its association with schizophrenia,2 it does seem to determine its prognosis. For
and this is maintained to date in the various disease example, among the catatonia secondary to medical
classification systems. More modernly, the publi- causes, structural brain damage is associated with
cation of clinical series of cases of catatonia with an a poorer prognosis than other organic disorders.11 17
organic aetiology has been frequent, and its preva- Catatonia can also adopt a very severe form
lence has been reported to range from 7% to 45% in called lethal or malignant when it is associated
various clinical settings (20%e25% in psychiatric with hyperthermia, tachycardia, tachypnoea,
units).3e7 In 1991, it was proposed that catatonia hypertension or labile blood pressure, diaphoresis
be considered a distinct diagnostic category8 and and alternating excitement and stupor. This form
in the Diagnostic and Statistical Manual-IV of catatonia is life threatening,18 and though not
(DSM-iV), catatonia appears as an entity secondary very frequent, it is secondary to a variety of general
to a general medical condition for the first time,9 medical or psychiatric causes, or to drugs and toxic
although its phenomena are not clearly described substances,19 especially antidopaminergic drugs
and their severity not considered. (neuroleptic malignant syndrome)19 and seroto-
It has been postulated that the problem relating nergic compounds (serotonergic syndrome where,
to the classification of catatonia is one of the in addition, abdominal pain and diarrhoea, myoc-
reasons why it remains relatively unrecognised by lonus, ataxia, tremor and convulsions are noted).20
both psychiatrists and other medical practi- Most patients in a catatonic state, although
tioners.10 This causes diagnostic delays that result often demonstrating a flattened affective state,
Emerg Med J 2012;29:863–867. doi:10.1136/emermed-2011-200896 863
Downloaded from http://emj.bmj.com/ on February 27, 2015 - Published by group.bmj.com
Review
experience an intense emotional state with high levels of anxiety disorders, diffuse lesions or dysfunction seem to be more
and fear sometimes thinking they are dead or about to die.21 frequently associated with catatonia than localised lesions. This,
They often do not recognise the motor abnormalities affecting together with the fact that catatonia occurs in primary
them, something known as motor or postural anosognosia.22 psychiatric disorders where no specific brain lesion has been
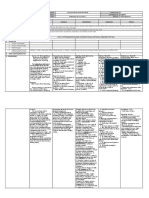
The assessment of catatonia is undertaken by a clinical identified, suggests that catatonia is the result of dysregulation
interview, observation and direct examination to elicit its of specific neural pathways affecting motor function rather than
signs.17 23 24 In table 1, there is a description of the main cata- the result of a single local lesion.24 These neurochemical path-
tonic signs, together with an indication of how to assess them. ways relate to circuitry linking the medial frontal and inferior
It is important to consider that catatonia is associated with orbital cortices to the basal ganglia and thalami, with connec-
a number of medical complications if not treated and managed tions to parietal lobes, cerebellum and limbic system,17 22 24
adequately, and that some of these complications are serious and mainly in the right hemisphere.
life threatening. Pulmonary thromboembolism is a frequent It has been proposed that the initial neurochemical abnor-
cause of death in this patient group.11 12 Box 1 shows the most mality would take place in the gamma-aminobutyric acid-A
frequent medical complications of catatonia. (GABA-A) receptors in cortical areas of the frontal lobes that
would cause hypoactivity of this inhibitory neurotransmitter
PATHOPHYSIOLOGY system. In turn, this would cause hypoactivity of dopaminergic
Given the fact that catatonia has multiple aetiologies, a unique transmission in subcortical areas. This top-down or corticoe
pathophysiological mechanism to explain the whole syndromic subcortical dopaminergic dysfunction would cause catatonia
complex is lacking. In relation to catatonia secondary to brain and also its malignant form. The neuroleptic malignant
Table 1 Catatonic semiology and its evaluation*
Sign Definition Mode of evaluation
Excitement Extreme and constant hyperactivity without aim Observation
Immobility and stupor Extreme hypoactivity, complete immobility, minimal response to stimuli Observation
Stimulation
Mutism Minimal or absent verbal response Observation
Conversation
Fixation of gaze Fixed gaze with little or absent response to environment and reduced blinking Observation
Posturing Maintenance of a mundane or bizarre posture for long periods of time, even Observation
when uncomfortable
Catalepsy Same as above but patient is positioned by the examiner Placing arm, leg or body of patient in a particular position
Grimacing Production and maintenance of bizarre facial expressions Observation
Echopraxia and echolalia Imitation of the movements or speech of a third party or of the examiner Observation
Conversation
Examiner scratches own head in an exaggerated manner
Stereotypies Aimless and repetitive motor activity (the abnormality is not inherent to the Observation
act but to its frequency)
Mannerisms Directed motor activity undertaken in a strange or exaggerated form (eg, Observation
jumping, tiptoeing, waving at passersby)
Verbigeration Production and repetition of sentences or words Observation
Conversation
Rigidity Maintenance of a rigid posture despite attempts to being moved (exclude if Examination of muscle tone
tremor or cogwheeling exist)
Negativism Unmotivated resistance to instructions or attempts to move or examine the Examination of muscle tone
patient, or conduct opposite to that required Verbal instructions
Waxy flexibility (flexibilitas Initial resistance to passive movement of a limb followed by a facilitation of Examination of muscle tone
cerea) or waxy rigidity the movement (similar to the feeling of folding a hot candle)
Withdrawal Refusal to eat, drink or to sustain others’ gaze Observation
Feeding
Impulsivity The patient suddenly behaves inappropriately without reason (undressing, Observation
running down the corridor, shouting). After the event, unable to explain his
or her behaviour
Automatic obedience Exaggerated cooperation with the examiner’s requests, or repetition of Examiner puts hand in pocket while saying to patient:
movements or actions that were only required once ‘stick out your tongue; I am going to prick it with a pin’
Passive obedience (Mitgehen) Raising of the arm in response to a slight pressure by the examiner’s finger Ask patient to extend the arm, place finger under patient’s
despite the instruction not to raise it palm and try to raise the arm by gentle pressure while
giving the instruction: ‘Don’t raise your arm’
Gegenhalten Resistance to passive movement that is proportional to the strength of the Passive mobilisation of a limb
stimulus
Ambitendency The patient seems to get stuck in indecisive conduct or movements Observation
Give hand to patient as intending to shake his or her hand
while instructing: ‘don’t shake my hand’
Grasping Grasping reflex that occurs when the patient’s palm is stimulated Examination of the grasping reflex
Perseveration Repetitive returning to the same topic or movement Observation
Conversation
Giving instructions
Combativeness Unmotivated, undirected and unexplained combative behaviour Observation
Autonomic abnormalities In temperature, blood pressure, pulse, respiratory frequency; also, Observation
inappropriate perspiration Checking of vital signs
Incontinence (urine/faecal)
*Based on the BusheFrancis catatonia rating scale.23
864 Emerg Med J 2012;29:863–867. doi:10.1136/emermed-2011-200896
Downloaded from http://emj.bmj.com/ on February 27, 2015 - Published by group.bmj.com
Review
diagnostic confidence while in inpatient cases or in those in
Box 1 Medical complications of catatonia emergency departments, two signs would suffice.28 The
majority of authors agree that two or more signs of catatonia
Cardiac and respiratory present during 1 h or more, or that can be reproduced in two or
Myocardial infarction, cardiac or respiratory arrest, aspiration, more occasions, are sufficient to diagnose catatonia.17 24
pneumonia, pneumonitis, pulmonary thromboembolism In any clinical situation, the presence of one catatonic sign
should raise the suspicion of catatonia and a full clinical
Gastrointestinal, endocrine and electrolytical assessment should be undertaken, preferably using a stand-
Haemorrhage, dehydration, hypernatraemia, hyponatraemia, ardised rating scale such as the BusheFrancis Catatonia Rating
malnutrition, chachexis, liver damage, hypoglycaemia Scale that also measures the severity of the signs.23 The use of
such scales improves the detection and diagnosis of catatonia.
Vascular The BusheFrancis Catatonia Rating Scale has also been shown
Thrombophlebitis, deep venous thrombosis, disseminated intra- to be sensitive to changes in the severity of catatonia during
vascular coagulation treatment.29 Thus, the diagnosis of catatonia is twofold: first
Neurological and muscular syndromic and second aetiological.
Muscle contractures, rhabdomyolisis, neuropathies secondary to As previously mentioned, catatonia has been observed in
posture, convulsions a wide variety of general medical, neurological and psychiatric
disorders as well as associated with drugs and toxic
Renal and urinary substances2 17 24 30 31 (box 2). When the patient is initially seen
Renal failure, urinary retention, urinary incontinence, bacteriuria, at the emergency department, apart from obtaining a clinical
urinary tract infection history and details on the patient’s past medical, psychiatric and
drug/toxic history, a full physical and neurological examination
Other will be needed, as well as a phenomenological description of
Sepsis, oral candidiasis, skin infections, pressure ulcers, burns
the clinical signs of catatonia. Since the patient will be, more
often than not, unable to assist clinical staff with the above,
the interview with relatives, friends or carers of the patient will
syndrome would be caused by subcortical dopaminergic dysre- be of great importance to establish the history and chronology
gulation (related to dopamine blockade) that would then cause of events and symptoms.
a bottom-up or subcorticoecortical dysfunction in GABA-A In relation to laboratory tests, it is important to undertake
transmission in the frontal cortex.22 Autonomic symptoms in a wide haematological and biochemical screening comprising
catatonia would be the result of similar GABA-A/dopamine a full blood count, markers of inflammatory processes such as C
dysregulation in fronto-hypothalamic circuits.24 reactive protein, glucose, urea and electrolytes, liver function tests,
The good response of catatonia to benzodiazepines (positive proteins, calcium, thyroid function, and creatinin-phosphokinase
modulators of the benzodiazepine/GABA receptor)25 and to and any other test that may be necessary according to the findings
electroconvulsive therapy (ECT) (that increases brain concen- of the examination.17 32 33
trations of GABA)26 is very suggestive of the primary involve- There are no specific abnormalities related to catatonia, but in
ment of the GABAergic system in the genesis of catatonia. its malignant form and in the neuroleptic malignant syndrome,
Glutamate would also have a role in its pathophysiology, being raised leucocytes and creatinin-phosphokinase and low serum
a biological antagonist of GABA, and given the fact that drugs iron have been often described.24 In simple catatonia, leukocytosis
that reduce glutamatergic transmission such as memantine and is generally not seen.24
amantadine have been shown to improve catatonia.27 Finally, it A blood or urine drug/toxic screen will often be needed. In
has been reported that serotonergic and cholinergic hyperac- addition, and when neurological disease is suspected, a test of
tivity could also be involved in the production of catatonic structural neuroimaging such as a CT or MRI scan will be indi-
phenomena,22 but the role of these neurotransmitters is less well cated. An EEG is also paramount in the investigation of unre-
understood. sponsive patients, helping with the diagnosis of seizure activity,
Catatonia has also been conceptualised as an evolutionary particularly nonconvulsive status epilepticus34 that can present
response to extreme fear (including that induced by psycho- with ictal catatonia. It is also of assistance in detecting enceph-
pathological phenomena such as hallucinations and delusions) alopathic states and in distinguishing normal wakefulness from
that would cause freezing of the individual to protect himself or sleep.
herself from predators stimulated by movement.21 This freezing It is important that clinicians distinguish between medical
would be analogous to immobility, catalepsy, stupor and causes of catatonia and medical complications of catatonia and,
mutism. The catatonic excitement would be analogous to the hence, that they rule out an organic cause and that they detect
flightefight response mediated by the sympathetic nervous possible complications as soon as possible.
system that precedes or follows the freezing.
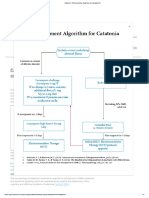
DIAGNOSIS MANAGEMENT
There is no consensus on the number of clinical signs needed to Once identified, the treatment of catatonia can be rapidly and
diagnose catatonia, although most authors tend to agree that dramatically effective, with a complete resolution of clinical
between one and four signs are necessary.6 9 17 23 24 In a study of signs in 60%e80% of acute cases.25 35 Due to the clinical signs of
catatonia in patients with psychotic symptoms, it was found acute catatonia, patients are often unable to provide informed
that with three or more signs a sensitivity and specificity of 99% consent to the proposed treatment, and so clinicians will need to
was reached.28 The optimal cut-off point could vary according assess their mental capacity and to undertake a best interests
to the clinical setting; in community cases where the prevalence assessment as the consequences of untreated catatonia may be
of catatonia is lower, four signs would confer reasonable very serious indeed.
Emerg Med J 2012;29:863–867. doi:10.1136/emermed-2011-200896 865
Downloaded from http://emj.bmj.com/ on February 27, 2015 - Published by group.bmj.com
Review
Box 2 Aetiologies of catatonia
Neurological
< Bilateral infarction of the parietal lobes, temporal infarcts, thalamic lesions, bilateral lesions in globus pallidus
< Anterior cerebral and anterior communicating artery aneurysms and haemorrhagic infarcts, subdural haematoma
< Hydrocephalus
< Frontal lobe traumatic contusions and neoplasms, paraneoplastic encephalopathy and malignant and benign central nervous system
(CNS) tumours
< Encephalitis (including herpes, HIV, postimmunisation and encephalitis lethargica), meningitis and cerebral abscesses
< Postencephalitic states, especially with Parkinsonism, progressive multifocal encephalopathy
< Neurosyphilis, other CNS infections: typhoid fever, tuberculosis, borreliosis, malaria, trypanosomiasis, hidatidosis
< Parkinson’s disease and Lewy body disease
< Frontotemporal dementia, Alzheimer’s disease, vascular dementia, CreutzfelteJakob disease, fatal familial insomnia
< Motor neuron disease, Wilson’s disease, Huntington’s disease, multiple sclerosis
< Epilepsy (absence seizures, complex partial seizures, generalised and complex partial (focal) status epilepticus, postictal states)
< Brain trauma acute and sequelae, Wernicke’s encephalopathy, hepatic encephalopathy, central pontine myelinolisis
< Narcolepsy, TayeSachs disease, tuberous sclerosis
Metabolic and endocrine, haematological and immune
< Diabetic ketoacidosis, hypercalcaemia, renal failure, liver failure
< Acute intermittent porphyria, homocystinuria, membranous glomerulonephritis, hyponatraemia and hypernatraemia
< Lysosomal disease, hypothyroidism, hyperthyroidism, hyperparathyroidism, hypoglycaemia, Sheehan’s syndrome
< Addison’s disease, Cushing’s disease, syndrome of inappropriate antidiuretic hormone secretion
< Vitamin B12 deficiency, nicotinic acid deficiency, pellagra
< Systemic lupus erythematosus, Paediatric Autoimmune Neuropsychiatric Disorder Associated with Streptoccocus (PANDAS),
antiphospholipid syndrome, renal and hepatic transplant, Langerhans carcinoma
Pharmacological, toxic and other
< Typical and atypical antipsychotics (use and withdrawal) including clozapine, levodopa, amantadine, serotonergic drugs, Selective
Serotonin Re-uptake Inhibitors ((SSRIs) trazodone, venlafaxine, etc), lithium
< Cephalosporines, ciprofloxacin, levofloxacin, azitromicine, levetiracetam, sodium valproate, gabapentin
< Disulfiram, paracetamol, aspirin, tramadol, hydroxicine, antitretrovirals, Adrenocorticotropic Hormone (ACTH), steroids
< Ciclosporin, chlorphenamine, methylphenidate, morphine, methadone, meperidene, allopurinol
< Benzodiazepines, cocaine, cannabis, lysergic acid diethylamide (LSD), mescalin, ketamine, phenylcyclidine, amphetamines,
organophosphates, ethylene, carbon monoxide, severe burns
Psychiatric and neurodevelopmental
< Mania and depression (bipolar disorder), unipolar depression, late-onset depression, schizophrenia and chronic psychoses
< Anxiety disorder, dissociative disorder and Ganser syndrome, adjustment disorders, acute stress reactions, obsessive-compulsive
disorder, PradereWilli syndrome, autistic spectrum disorders
The aetiology, pattern and severity of catatonic signs do not topiramate, but they are usually slower than lorazepam in their
affect response to treatment.11 The treatment of catatonia action.27 For patients unresponsive to lorazepam and who are in
should be provided in a hospital setting by a multidisciplinary a serious clinical condition, ECT can be very beneficial.17 40
team and with psychiatric support.32 33 Benzodiazepines, and It is also very important that in addition to treating the signs
especially lorazepam, are the drugs of choice for the acute of catatonia the treatment of the cause of the catatonia be
management of catatonia, and they are widely used for this started as soon as possible in order to ensure a complete reso-
purpose17 given their mechanism of action through the GABA-A lution of the syndrome and to avoid early recurrences.
receptor. There is plenty of literature on the effectiveness of A lorazepam trial is the treatment of choice in cata-
lorazepam in catatonia of various aetiologies, mainly case tonia,17 24 25 27 32 especially in the retarded or stuporous forms.32
reports, series and open label studies,27 36 37 but to date there is It should start with the administration of lorazepam 1e2 mg
no evidence from randomised controlled trials of its use in intramuscular or orally. After 3 h, and if there is no response or if
catatonia secondary to schizophrenia.38 In this illness, there is this is partial, lorazepam 1e2 mg intramuscular or orally are
controversy on the role of antipsychotic drugs in the manage- administered. This dose can be repeated after another 3 h.32 An
ment of catatonia, with some authors suggesting that they initial positive response usually predicts a more sustained
worsen the latter (except for clozapine)37 while others reporting response with further doses of treatment25 and would confirm
that they can be beneficial.27 39 It would appear that antipsy- the diagnosis of catatonia in 80% of cases.41 The final effective
chotics with strong D2 receptor antagonism should be avoided dose of lorazepam that achieved a complete resolution of the
in patients with psychosis and catatonia.37 There are also catatonic signs will then be maintained for some days until the
reports of other drugs being helpful and effective, sometimes in treatment of the cause of catatonia is well under way.32 The
refractory cases, such as zolpidem, amantadine, memantine, dose should be titrated against sedation.32 Lorazepam should be
bromocriptine, levodopa, sodium valproate, carbamazepine and switched to oral administration as soon as possible. A premature
866 Emerg Med J 2012;29:863–867. doi:10.1136/emermed-2011-200896
Downloaded from http://emj.bmj.com/ on February 27, 2015 - Published by group.bmj.com
Review
suspension of treatment with lorazepam is likely to provoke 6. Rosebush PI, Hildebrand AM, Furlong BG, et al. Catatonic syndrome in a general
a recurrence of the symptoms.6 32 psychiatric inpatient population: frequency, clinical presentation, and response to
lorazepam. J Clin Psychiatry 1990;51:357e62.
In patients with lethal or malignant catatonia, the dose of 7. Carroll BT, Anfinson TJ, Kennedy JC, et al. Catatonic disorder due to general
lorazepam will be higher and ECT may be needed much earlier.17 medical condition. J Neuropsychiatry Clin Neurosci 1994;6:122e33.
The initial and subsequent doses of lorazepam may need to be 8. Fink M, Taylor AM. Catatonia: a separate category for DSM-IV? Integr Psychiatry
1991;7:2e10.
lower in elderly patients32 or in those with obesity or known 9. American Psychiatric Association. Diagnostic and Statistical Manual of Mental
respiratory disease. Disorders. 4th edn. Washington: American Psychiatric Association, 1994.
ECT is considered in those cases in which response to an 10. Van der Heijden FM, Tuinier S, Arts NJ, et al. Catatonia: disappeared or under-
diagnosed? Psychopathology 2005;38:3e8.
adequate trial of treatment with lorazepam is not achieved after 11. Levenson J. Medical aspects of catatonia. Prim psychiatry 2009;16:23e6.
5 days or in those with lethal catatonia.17 In the UK, the 12. Gross AF, Smith FA, Stern TA. Dread complications of catatonia: a case discussion
National Institute of Clinical Excellence includes catatonia as and review of the literature. Prim Care Companion J Clin Psychiatry 2008;10:153e5.
one of the few indications for ECT in its technology appraisal of 13. Seethalakshmi R, Dhavale S, Suggu K, et al. Catatonic syndrome: importance of
detection and treatment with lorazepam. Ann Clin Psychiatry 2008;20:5e8.
this treatment modality.42 ECT can only be administered by 14. Valenstein M, Maltbie A, Kaplan P. Catatonia in the emergency department. Ann
trained psychiatrists with anaesthetic support in accredited Emerg Med 1985;14:359e61.
services. 15. Swartz C, Galang RL. Adverse outcome with delay in identification of catatonia in
elderly patients. Am J Geriatr Psychiatry 2001;9:78e80.
During the treatment of catatonia, it is important to ensure 16. Rogers D. Motor Disorder in Psychiatry: Towards a Neurological Psychiatry.
that the patient is well hydrated and nursed and that adequate Chichester: John Wiley & Sons, 1992.
prevention of poor nutrition, infection and thrombosis is given. 17. Fink M, Taylor AM. Catatonia: A Clinician’s Guide to Diagnosis and Treatment.
With improvement, the risk of falls secondary to sedation, espe- Cambridge: Cambridge University Press, 2003.
18. Mann SC, Caroff SN, Bleier HR, et al. Lethal catatonia. Am J Psychiatry
cially in older patients, will need to be managed appropriately. 1986;143:1374e81.
19. Strawn JR, Keck PE Jr, Caroff SN. Neuroleptic malignant syndrome. Am J
CONCLUSION Psychiatry 2007;164:870e6.
20. Ables AZ, Nagubilli R. Prevention, recognition, and management of serotonin
Catatonia is a neuropsychiatric syndrome associated with syndrome. Am Fam Physician 2010;81:1139e42.
a wide variety of general medical, neurological and primary 21. Moskowitz AK. “Scared stiff”: catatonia as an evolutionary-based fear response.
psychiatric conditions. It is mainly characterised by stupor, Psychol Rev 2004;111:984e1002.
mutism, catalepsy, posturing and immobility. It is not infre- 22. Northoff G. What catatonia can tell us about “top-down modulation”:
a neuropsychiatric hypothesis. Behav Brain Sci 2002;25:555e77; discussion
quent and its presence does not automatically imply a psychi- 578e604.
atric cause. The clinical presentation is easily identifiable by the 23. Bush G, Fink M, Petrides G, et al. Catatonia I: rating scale and standardized
knowledgeable clinician through observation, clinical examina- examination. Acta Psychiatr Scand 1996;93:129e36.
24. Caroff SN, Mann SC, Francis A, et al. Catatonia: From Psychopathology to
tion and interview. Most patients with acute catatonia will Neurobiology. Washington: American Psychiatric Publishing, 2004.
present to accident and emergency departments where it is 25. Bush G, Fink M, Petrides G, et al. Catatonia II: treatment with lorazepam and
crucial that catatonia be diagnosed and where the work up to electroconvulsive therapy. Acta Psychiatr Scand 1996;93:137e43.
ascertain an aetiological diagnosis be started. Delays in diagnosis 26. Sanacora G, Mason GF, Rothman DL, et al. Increased cortical GABA concentrations
in depressed patients receiving ECT. Am J Psychiatry 2003;160:577e9.
and initial management are associated with increased morbidity 27. Carroll B, Lee JW, Appiani F, et al. The pharmacotherapy of catatonia. Prim
and complications, especially when catatonia is wrongly Psychiatry 2010;17:41e7.
attributed to psychiatric disease. 28. Peralta V, Cuesta MJ. Motor features in psychotic disorders II. Schizophr Res
2001;47:117e26.
Given that there is no consistent pattern in the semiology of 29. Sienaert P, Rooseleer J, De Fruyt J. Measuring catatonia: a systematic review of
catatonia to distinguish medical from psychiatric causes, the rating scales. J Affect Disord 2011;135:1e9.
advice given by Gelenberg to consider medical aetiologies in all 30. Ahuja N. Organic catatonia: a review. Indian J Psychiatry 2000;42:327e46.
31. Duggal HS, Singh I. Drug-induced catatonia. Drugs Today (Barc) 2005;41:599e607.
patients presenting with acute catatonia regardless of any
32. Rosebush PI, Mazurek MF. Catatonia and its treatment. Schizophr Bull
psychiatric diagnosis still stands.2 2010;36:239e42.
Treatment with lorazepam is usually effective and improves 33. Lahutte B, Cornic F, Bonnot O, et al. Multidisciplinary approach of organic catatonia
the patient’s clinical condition rapidly in a high proportion of in children and adolescents may improve treatment decision making. Prog
Neuropsychopharmacol Biol Psychiatry 2008;32:1393e8.
cases. 34. Kaplan PW. Nonconvulsive status epilepticus in the emergency room. Epilepsia
Catatonia should be considered in the differential diagnosis of 1996;37:643e50.
altered states of awareness in the emergency department. 35. Daniels J. Catatonia: clinical aspects and neurobiological correlates. J
Neuropsychiatry Clin Neurosci 2009;21:371e80.
Contributors WJA jointly designed the study, reviewed, read and analysed the 36. Ungvari GS, Leung CM, Wong MK, et al. Benzodiazepines in the treatment of
relevant literature, and jointly wrote the manuscript. JSM jointly designed the study, catatonic syndrome. Acta Psychiatr Scand 1994;89:285e8.
read and analysed relevant literature, and jointly wrote the manuscript. 37. England ML, Ongür D, Konopaske GT, et al. Catatonia in psychotic patients:
clinical features and treatment response. J Neuropsychiatry Clin Neurosci
Competing interests None. 2011;23:223e6.
Provenance and peer review Not commissioned; externally peer reviewed. 38. Gibson RC, Walcott G. Benzodiazepines for catatonia in people with schizophrenia
and other serious mental illnesses. Cochrane Database Syst Rev 2008;(4):CD006570.
39. Peralta V, Campos MS, de Jalon EG, et al. DSM-IV catatonia signs and criteria in
REFERENCES first-episode, drug-naive, psychotic patients: psychometric validity and response to
1. Kahlbaum KL. Catatonia. Baltimore: John Hopkins University Press, 1973. antipsychotic medication. Schizophr Res 2010;118:168e75.
2. Fink M, Shorter E, Taylor MA. Catatonia is not schizophrenia: Kraepelin’s error and 40. Zisselman MH, Jaffe RL. ECT in the treatment of a patient with catatonia: consent
the need to recognize catatonia as an independent syndrome in medical and complications. Am J Psychiatry 2010;167:127e32.
nomenclature. Schizophr Bull 2010;36:314e20. 41. Fink M, Taylor AM. Catatonia: subtype or syndrome in DSM? Am J Psychiatry
3. Gelenberg AJ. The catatonic syndrome. Lancet 1976;1:1339e41. 2006;163:1875e6.
4. Huang TL, Ree SC, Huang YC, et al. Catatonic features: differential diagnosis and 42. National Institute of Clinical Excellence. Technology Appraisal No 59: The
treatments at an emergency unit. Psychiatry Clin Neurosci 1999;53:63e6. clinical effectiveness and cost effectiveness of electroconvulsive therapy (ECT) for
5. Barnes MP, Saunders M, Walls TJ, et al. The syndrome of Karl Ludwig Kahlbaum. depressive illness, schizophrenia, catatonia and mania. http://www.nice.org.uk/
J Neurol Neurosurg Psychiatry 1986;49:991e6. TA059
PAGE fraction trail=5
Emerg Med J 2012;29:863–867. doi:10.1136/emermed-2011-200896 867
Downloaded from http://emj.bmj.com/ on February 27, 2015 - Published by group.bmj.com
Catatonia in the emergency department
Walter Jaimes-Albornoz and Jordi Serra-Mestres
Emerg Med J 2012 29: 863-867 originally published online March 2, 2012
doi: 10.1136/emermed-2011-200896
Updated information and services can be found at:
http://emj.bmj.com/content/29/11/863
These include:
References This article cites 35 articles, 3 of which you can access for free at:
http://emj.bmj.com/content/29/11/863#BIBL
Email alerting Receive free email alerts when new articles cite this article. Sign up in the
service box at the top right corner of the online article.
Notes
To request permissions go to:
http://group.bmj.com/group/rights-licensing/permissions
To order reprints go to:
http://journals.bmj.com/cgi/reprintform
To subscribe to BMJ go to:
http://group.bmj.com/subscribe/
You might also like
- Movement Disorders in Catatonia: Subhashie Wijemanne, Joseph JankovicDocument9 pagesMovement Disorders in Catatonia: Subhashie Wijemanne, Joseph JankovicTri Santi GhozaliNo ratings yet
- Catatonia From The First Descriptions To DSM 5Document7 pagesCatatonia From The First Descriptions To DSM 5Monika LangngagNo ratings yet
- Catatonia Revived. A Unique Syndrome UpdatedDocument10 pagesCatatonia Revived. A Unique Syndrome UpdatedElisa PavezNo ratings yet
- The Diagnosis and Treatment of CatatoniaDocument4 pagesThe Diagnosis and Treatment of Catatonia崔雍建No ratings yet
- Anand 2019Document5 pagesAnand 2019DhayenaurasNo ratings yet
- Using A Systematic Approach To Assess An Acutely Unwell Patient With Catatonia: A Case StudyDocument9 pagesUsing A Systematic Approach To Assess An Acutely Unwell Patient With Catatonia: A Case StudynasimhsNo ratings yet
- Catatonia - Pathophysiology, Diagnosis and ManagementDocument17 pagesCatatonia - Pathophysiology, Diagnosis and ManagementFahrunnisa NurdinNo ratings yet
- The Many Varieties of Catatonia: Max Fink Michael A. TaylorDocument7 pagesThe Many Varieties of Catatonia: Max Fink Michael A. TaylorRoy FloresNo ratings yet
- Catatonia: Clinical Aspects and Neurobiological Correlates: Jessica Daniels, M.DDocument10 pagesCatatonia: Clinical Aspects and Neurobiological Correlates: Jessica Daniels, M.DCarol ArtigasNo ratings yet
- Jurnal PsiDocument5 pagesJurnal PsisamiaNo ratings yet
- Catatonia Kaplan PDFDocument3 pagesCatatonia Kaplan PDFJuan Sebastian LozanoNo ratings yet
- Catatonia 1Document12 pagesCatatonia 1rafuxu22No ratings yet
- CP 01708016Document11 pagesCP 01708016telur_kudaNo ratings yet
- Catatonia - APM EAPM - 2015 04 17 PDFDocument51 pagesCatatonia - APM EAPM - 2015 04 17 PDFImon PaulNo ratings yet
- Cureus 0014 00000021662Document5 pagesCureus 0014 00000021662Luis Cesar RochaNo ratings yet
- Catatonia MalignaDocument7 pagesCatatonia MalignaAlden García GonzálezNo ratings yet
- Brain Mechanisms Underlying Apathy: Campbell Le Heron, Clay B Holroyd, John Salamone, Masud HusainDocument11 pagesBrain Mechanisms Underlying Apathy: Campbell Le Heron, Clay B Holroyd, John Salamone, Masud HusainMuhammad UsmanNo ratings yet
- Epilepsia - 2018 - Shorvon - Regulatory Aspects of Status EpilepticusDocument7 pagesEpilepsia - 2018 - Shorvon - Regulatory Aspects of Status EpilepticusKikie Rizky HeningNo ratings yet
- Emergency Presentations of MDDocument10 pagesEmergency Presentations of MDGustavo PestanaNo ratings yet
- Delirium en Cuidados Paliativos Oncológicos: Revisión: Psicooncologia January 2004Document19 pagesDelirium en Cuidados Paliativos Oncológicos: Revisión: Psicooncologia January 2004Katerina BellostaNo ratings yet
- Catatonia in Adults - Epidemiology, Clinical Features, Assessment, and Diagnosis - UpToDateDocument15 pagesCatatonia in Adults - Epidemiology, Clinical Features, Assessment, and Diagnosis - UpToDatedaveNo ratings yet
- CatatoniaDocument8 pagesCatatoniaElysium MindsNo ratings yet
- Delirium Disorder Unity in DiversityDocument7 pagesDelirium Disorder Unity in DiversityPsiquiatría CESAMENo ratings yet
- 2018 DystoniaDocument23 pages2018 DystoniaTony NgNo ratings yet
- DistoniaDocument23 pagesDistoniaOsvaldo CortésNo ratings yet
- Postoperative DeliriumDocument13 pagesPostoperative DeliriumEndah Augina BudiartiNo ratings yet
- Ciurli NPI2011Document11 pagesCiurli NPI2011colomba cosignaniNo ratings yet
- Catatonía HistoriaDocument48 pagesCatatonía HistoriaW Andrés S MedinaNo ratings yet
- Catatonia From Its Creation To DSM-V: Considerations For ICDDocument4 pagesCatatonia From Its Creation To DSM-V: Considerations For ICDMariano OutesNo ratings yet
- Catatonia PDFDocument9 pagesCatatonia PDFDanilo RibeiroNo ratings yet
- CatatoniaDocument5 pagesCatatoniacarolina ferranteNo ratings yet
- Neurometabolic Hereditary Diseases of AdultsFrom EverandNeurometabolic Hereditary Diseases of AdultsAlessandro P. BurlinaNo ratings yet
- Out PDFDocument6 pagesOut PDFMaria RenjaanNo ratings yet
- PIIS0885392412001224Document12 pagesPIIS0885392412001224Catinca DobroghiiNo ratings yet
- A Case Series of Catatonia: Lessons To Learn: June 2015Document4 pagesA Case Series of Catatonia: Lessons To Learn: June 2015Mariano OutesNo ratings yet
- Catatonia: Sebastian Walther and Werner StrikDocument8 pagesCatatonia: Sebastian Walther and Werner StrikvgkdgkiajgvikaNo ratings yet
- Autism: Catatonia: The Ultimate Yet Treatable Motor Reaction To Fear in AutismDocument5 pagesAutism: Catatonia: The Ultimate Yet Treatable Motor Reaction To Fear in AutismMariano OutesNo ratings yet
- Catatonia in Adults - Epidemiology, Clinical Features, Assessment, and Diagnosis - UpToDateDocument21 pagesCatatonia in Adults - Epidemiology, Clinical Features, Assessment, and Diagnosis - UpToDateJéssica ChavesNo ratings yet
- 1 s2.0 S0920996422004315 MainDocument10 pages1 s2.0 S0920996422004315 MainAndrea SalazarNo ratings yet
- The Mental Illness SpectrumDocument4 pagesThe Mental Illness Spectrumfrancesca_valdiviaNo ratings yet
- Abram Hoffer - Prousky - Orthomolecular Treatment of Anxiety DisordersDocument7 pagesAbram Hoffer - Prousky - Orthomolecular Treatment of Anxiety DisordersEbook PDFNo ratings yet
- Catatonia FarmacoterapiaDocument8 pagesCatatonia FarmacoterapiaW Andrés S MedinaNo ratings yet
- Mellers 2005Document8 pagesMellers 2005esckere papas fritasNo ratings yet
- AJGP 12 2019 Focus Patel Palliative Sedation WEB PDFDocument8 pagesAJGP 12 2019 Focus Patel Palliative Sedation WEB PDFFrancisco Rodriguez de NarvaezNo ratings yet
- Ataxia en AdultosDocument12 pagesAtaxia en AdultosOsvaldo CortésNo ratings yet
- Benign Stupors: A Study of a New Manic-Depressive Reaction TypeFrom EverandBenign Stupors: A Study of a New Manic-Depressive Reaction TypeNo ratings yet
- Factitious DisorderDocument6 pagesFactitious Disorderayu yuliantiNo ratings yet
- Management of The Agitated Patient in The Emergency DepartmentDocument11 pagesManagement of The Agitated Patient in The Emergency Departmentkittykat4144321No ratings yet
- Frailty For Neurologists - A Practical GuideDocument8 pagesFrailty For Neurologists - A Practical GuideAlphaNo ratings yet
- Balint 2018Document23 pagesBalint 2018Ovidiu-Lucian BajenaruNo ratings yet
- Review of CimDocument8 pagesReview of CimMuhammad Imran MirzaNo ratings yet
- Catatonia DSM 5Document5 pagesCatatonia DSM 5vinodksahuNo ratings yet
- Bipolaridad 1Document12 pagesBipolaridad 1JambisNo ratings yet
- Dissociative Identity Disorder A Case of Three SelDocument2 pagesDissociative Identity Disorder A Case of Three SelMartín SalamancaNo ratings yet
- Case Report On Antipsychotic Induced Catatonia in An Incarcerated PatientDocument7 pagesCase Report On Antipsychotic Induced Catatonia in An Incarcerated Patientazadparis66No ratings yet
- Evaluation and Management of The Dizzy Patient: L M LuxonDocument8 pagesEvaluation and Management of The Dizzy Patient: L M LuxonCarolina Sepulveda RojasNo ratings yet
- Epilspia y Comobilidad PsiquiatricaDocument17 pagesEpilspia y Comobilidad PsiquiatricaManuel Alejandro Pinzon OlmosNo ratings yet
- Evaluation and Management of The Dizzy PatientDocument9 pagesEvaluation and Management of The Dizzy Patientsara mohamedNo ratings yet
- Cognitive Disorders: Delirium EpidemiologyDocument5 pagesCognitive Disorders: Delirium EpidemiologyJupiter ZangelNo ratings yet
- Adherence, Anxiety and Depression Associated With Hemodialysis Treatment in Patients With Chronic Kidney DiseaseDocument11 pagesAdherence, Anxiety and Depression Associated With Hemodialysis Treatment in Patients With Chronic Kidney DiseaseInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- DLL English 5 Q3W2Document3 pagesDLL English 5 Q3W2Mark Daniel L. SalvadorNo ratings yet
- State of Lung Cancer 2021Document16 pagesState of Lung Cancer 2021Honolulu Star-AdvertiserNo ratings yet
- New Patient FormDocument7 pagesNew Patient FormajNo ratings yet
- ASCOT Hypertension StudyDocument12 pagesASCOT Hypertension StudyAnonymous NeRC5JYiSNo ratings yet
- 2024self-Report of Medical ConditionsDocument3 pages2024self-Report of Medical Conditionsdiolanto5No ratings yet
- Clinical SummaryDocument4 pagesClinical Summaryvetdimples.29No ratings yet
- Heat Illness Prevention ProgramDocument7 pagesHeat Illness Prevention ProgramSPIQCNo ratings yet
- Renal Transplantation in ChildrenDocument9 pagesRenal Transplantation in ChildrenJhomines NialaNo ratings yet
- Itls 9th Edition Prep Packet Advanced Provider VersionDocument19 pagesItls 9th Edition Prep Packet Advanced Provider VersionUmidagha BaghirzadaNo ratings yet
- Mcn-Rle-Ncp Postpartum Narce Bsn2aDocument3 pagesMcn-Rle-Ncp Postpartum Narce Bsn2aAlmera Rose NarceNo ratings yet
- Dulcolax Paracetamol Duvadilan Ferrous SulfateDocument32 pagesDulcolax Paracetamol Duvadilan Ferrous SulfateAdrianne BastasaNo ratings yet
- POULTRY PATHO - Marek's DiseaseDocument31 pagesPOULTRY PATHO - Marek's DiseaseArooma KhalidNo ratings yet
- RapeDocument8 pagesRapeVida MarieNo ratings yet
- Lung Adenocarcinoma With Solitary MetastDocument88 pagesLung Adenocarcinoma With Solitary MetastMikmik bay BayNo ratings yet
- Challenging Neurological Manifestations in Large Cell Neuroendocrine Carcinoma Lcnec A Case Study of Extensive Intracranial and Intradural MetastasesDocument3 pagesChallenging Neurological Manifestations in Large Cell Neuroendocrine Carcinoma Lcnec A Case Study of Extensive Intracranial and Intradural MetastasesHerald Scholarly Open AccessNo ratings yet
- HISTORY TAKING Anterior Neck MassDocument10 pagesHISTORY TAKING Anterior Neck MassWispy NotesNo ratings yet
- Global Oncology Trends 2021-2025Document70 pagesGlobal Oncology Trends 2021-2025Deepak MakkarNo ratings yet
- Kendigs Disorders of The Respiratory Tract in Children 9Th Edition Robert W Wilmott Full ChapterDocument50 pagesKendigs Disorders of The Respiratory Tract in Children 9Th Edition Robert W Wilmott Full Chapterernest.guzman635100% (5)
- Hsa Questions 1Document13 pagesHsa Questions 1felixohxinganoNo ratings yet
- CKD Case StudyDocument27 pagesCKD Case StudyMary Rose Vito100% (1)
- Curriculum Vitae of Oluwakemi Ayomidr Adekunrun 2023 4Document7 pagesCurriculum Vitae of Oluwakemi Ayomidr Adekunrun 2023 4Musa IbrahimNo ratings yet
- Ref 4Document13 pagesRef 4Tiago BaraNo ratings yet
- Case Report A Chinese Patient With Spinocerebellar Ataxia Finally Confirmed As Gerstmann-Sträussler-Scheinker Syndrome With P102L MutationDocument16 pagesCase Report A Chinese Patient With Spinocerebellar Ataxia Finally Confirmed As Gerstmann-Sträussler-Scheinker Syndrome With P102L MutationLídia YoshiharaNo ratings yet
- Cervical Disc Disease and Spondylosis: Rabia Qureshi, Jason A. Horowitz, Hamid HassanzadehDocument7 pagesCervical Disc Disease and Spondylosis: Rabia Qureshi, Jason A. Horowitz, Hamid HassanzadehMasithaNo ratings yet
- Adolescent Substance AbuseDocument5 pagesAdolescent Substance AbuseHamza DouichiNo ratings yet
- Palliative Care - Overview of Cough, Stridor, and Hemoptysis - UpToDateDocument19 pagesPalliative Care - Overview of Cough, Stridor, and Hemoptysis - UpToDateThaísa NogueiraNo ratings yet
- Health Certificate PDFDocument2 pagesHealth Certificate PDFPedro KunstNo ratings yet
- Bacterio BilityDocument8 pagesBacterio BilityAbdul Rehman SafdarNo ratings yet
- The Benefits of Immunotherapy CombinationsDocument1 pageThe Benefits of Immunotherapy CombinationsMicheleFontanaNo ratings yet
- Principles of Emergency NursingDocument4 pagesPrinciples of Emergency NursingShamera MahabassalNo ratings yet