Professional Documents
Culture Documents
WNF 0000000000000401 PDF
Uploaded by
FRANCISCO JOSUÉ CORDERO PÉREZOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
WNF 0000000000000401 PDF
Uploaded by
FRANCISCO JOSUÉ CORDERO PÉREZCopyright:
Available Formats
REVIEW ARTICLE
The Efficacy and Safety of DFN-15 for the Treatment of
Migraine: A Meta-Analysis of Randomized Controlled Studies
Yili Deng, MD,* Yang Chen, MD,† Zeyan Peng, MD,† and Heng Yang, MD†
meta-analysis of randomized controlled trials (RCTs) aims to as-
Objectives: The efficacy of DFN-15 for pain control of migraine remains sess the efficacy and safety of DFN-15 versus placebo on pain
controversial. We conduct a systematic review and meta-analysis to explore control in migraine patients.
the influence of DFN-15 versus placebo on pain control in migraine patients.
Patients and Methods: We search PubMed, Embase, Web of Science,
EBSCO, and Cochrane Library databases through November 2019 for ran- MATERIALS AND METHODS
Downloaded from http://journals.lww.com/clinicalneuropharm by BhDMf5ePHKbH4TTImqenVHVWbIH6TTJXt+6jQbRDfKBmKA6t1O34KUxLV9xApgjoPLgRuwiiYmg= on 07/26/2020
domized controlled trials assessing the effect of DFN-15 versus placebo on This systematic review and meta-analysis are performed
pain control in migraine patients. This meta-analysis is performed using the based on the guidance of the Preferred Reporting Items for Sys-
random-effects model. tematic Reviews and Meta-analysis statement and Cochrane
Results: Three randomized controlled trials are included in the meta- Handbook for Systematic Reviews of Interventions.17,18 No ethical
analysis. Overall, compared with the control group in migraine patients, approval and patient consent are required because all analyses are
lasmiditan treatment shows a positive impact on pain freedom at 2 hours (risk based on previous published studies.
ratio [RR], 1.96; 95% confidence interval, 1.61–2.40; P < 0.00001), head-
ache response at 2 hours (RR, 1.40; 95% CI, 1.25–1.57; P < 0.00001), and Literature Search and Selection Criteria
pain freedom at 24 hours (RR, 1.87; 95% CI, 1.33–2.62; P = 0.0003), but
We systematically search several databases including
has no obvious influence or no substantial impact on no or mild disability
PubMed, Embase, Web of Science, EBSCO, and the Cochrane Li-
level (RR, 1.21; 95% CI, 0.97–1.52; P = 0.09) or nausea (RR, 2.42; 95%
brary from inception to November 2019 with the following key-
CI, 0.53–11.01; P = 0.25). In addition, lasmiditan seems to result in the in-
words: DFN-15 and migraine. The reference lists of retrieved
crease in dizziness (RR, 7.33; 95% CI, 1.83–29.30; P = 0.005) and paresthe-
studies and relevant reviews are also hand-searched, and the afore-
sia (RR, 5.17; 95% CI, 2.08–12.86; P = 0.0004).
mentioned process is performed repeatedly in order to include ad-
Conclusions: DFN-15 treatment may be effective and safe for pain con-
ditional eligible studies.
trol in migraine patients.
The inclusion criteria are presented as follows: (1) study de-
Key Words: DFN-15, migraine, pain control, randomized controlled trials sign is RCT, (2) patients are diagnosed with migraine, and (3) in-
(Clin Neuropharm 2020;43: 107–111)
tervention treatments are DFN-15 versus placebo.
Data Extraction and Outcome Measures
M igraine is one common neurological disorder and is regarded
as the world's second leading cause of disability.1–5 Inflam-
matory mediators have important roles in the pathophysiology of
Some baseline information is extracted from the original
studies, including first author, number of patients, age, body mass
migraine.6–8 Certain nonsteroidal anti-inflammatory drugs (eg, as- index, and detailed methods in 2 groups. Data are extracted inde-
pirin, diclofenac, ibuprofen, and naproxen) are currently used for pendently by 2 investigators, and discrepancies are resolved by
the acute treatment of migraine by inhibiting the synthesis of pros- consensus. We have contacted the corresponding author to obtain
taglandins by blocking the effects of cyclooxygenase (COX)-1 and the data when necessary.
COX-2 on arachidonic acid.9–11 The primary outcome is 2-hour pain freedom. Secondary
Celecoxib, a selective COX-2 inhibitor, demonstrates lower outcomes include freedom from MBS, adverse event, dysgeusia,
risk of gastrointestinal events than naproxen or ibuprofen and nausea.
(P = 0.002), and lower risk of renal events than ibuprofen for os-
teoarthritis and rheumatoid arthritis.12,13 Celecoxib is also indi- Quality Assessment in Individual Studies
cated for the control of acute pain in patients with ankylosing The methodological quality of each RCT is assessed using the
spondylitis and primary dysmenorrhea. DFN-15, an oral liquid Jadad scale, which consists of 3 evaluation elements: randomization
solution of celecoxib, has some potential in the acute treatment (0–2 points), blinding (0–2 points), and dropouts and withdrawals
of migraine. During the acute treatment of migraine, 120 mg (0–1 points).19 One point would be allocated to each element if they
DFN-15 can remarkably improve pain freedom at 2 hours and have been conducted and mentioned appropriately in the original
freedom from the most bothersome symptom (MBS).14 article. The Jadad scale score varies from 0 to 5 points. An article
Several studies have investigated the effects of DFN-15 on with Jadad score ≤2 is considered to be of low quality. The study
pain relief for migraine patients.14–16 This systematic review and is thought to be of high quality if the Jadad score is ≥3.20
*Department of Cardiology, Xinxin Hospital of Qijiang District; and †Department Statistical Analysis
of Neurology, Daping Hospital, Army Medical University, Chongqing, China.
Address correspondence and reprint requests to Heng Yang, MD, Department of
We assess risk ratios (RRs) with 95% confidence intervals
Neurology, Daping Hospital, Army Medical University, Chongqing (CIs) for dichotomous outcomes (2-hour pain freedom, freedom
400042, China; E‐mail: cyfy776655@163.com from MBS, adverse event, dysgeusia, and nausea). Heterogeneity
Conflicts of Interest and Source of Funding: The authors have no conflict of is evaluated using the I2 statistic, and I2 > 50% indicates signifi-
interest to declare.
Research involving human participants and/or animals: not applicable.
cant heterogeneity.21 The random-effects model is used for all
Copyright © 2020 Wolters Kluwer Health, Inc. All rights reserved. meta-analyses. We search for potential sources of significant het-
DOI: 10.1097/WNF.0000000000000401 erogeneity. Sensitivity analysis is performed to detect the
Clinical Neuropharmacology • Volume 43, Number 4, July/August 2020 www.clinicalneuropharm.com 107
Copyright © 2020 Wolters Kluwer Health, Inc. All rights reserved.
Deng et al Clinical Neuropharmacology • Volume 43, Number 4, July/August 2020
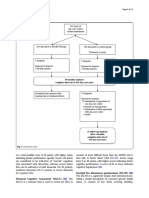
FIGURE 1. Flow diagram of study searching and selection process.
influence of a single study on the overall estimate via omitting one initially, and 2 RCTs and 1 abstract are included in the meta-
study in turn or performing the subgroup analysis. Because of the analysis.14–16
limited number (<10) of included studies, publication bias is not The baseline characteristics of 3 included RCTs are shown in
assessed. Results are considered statistically significant for Table 1. These studies are published between 2017 and 2019, and
P < 0.05. All statistical analyses are performed using Review the total sample size is 711. DFN-15 is administered by a single
Manager Version 5.3 (The Cochrane Collaboration, Software Up- dose of DFN-15 120 mg. Three RCTs report 2-hour pain freedom
date, Oxford, United Kingdom). and freedom from MBS,14–16 and 2 RCTs report adverse events,
dysgeusia and nausea.14,16 The Jadad scores of the 3 included
studies vary from 3 to 5, and all 3 studies have high quality based
RESULTS on the quality assessment.
Literature Search, Study Characteristics, and Primary Outcome: 2-Hour Pain Freedom
Quality Assessment The random-effects model is used for the analysis of primary
Figure 1 shows the detailed flowchart of the search and selec- outcomes. The results find that compared with the control group
tion results. Forty-five potentially relevant articles are identified in migraine patients, a single dose of DFN-15 120 mg is
TABLE 1. Characteristics of Included Studies
DFN-15 Group Control Group
Female, Female, Jada
No. Author No. Age, y n BMI, kg/m2 Methods No. Age, y n BMI, kg/m2 Methods Scores
1 Bennett and 20 — — — 120 mg DFN-15 daily 20 — — — Placebo 3
Munjal15
2 Lipton et al14 285 41 (11) 252 30.6 (7.8) 120 mg DFN-15 daily 282 40 (12) 242 30.0 (7.9) Placebo 5
3 Munjal and 51 43.6 — 28.48 Single dose of 53 43.6 — 28.48 Placebo 4
Bennett16 DFN-15 120 mg
BMI, body mass index.
108 www.clinicalneuropharm.com © 2020 Wolters Kluwer Health, Inc. All rights reserved.
Copyright © 2020 Wolters Kluwer Health, Inc. All rights reserved.
Clinical Neuropharmacology • Volume 43, Number 4, July/August 2020 DFN-15 for Migraine Treatment
FIGURE 2. Forest plot of the meta-analysis of 2-hour pain freedom.
FIGURE 3. Forest plot of the meta-analysis of freedom from MBS.
associated with significantly improved 2-hour pain freedom (RR, celecoxib oral capsules20 and may result in low incidence of ad-
1.65; 95% CI, 1.28–2.12; P = 0.0001) with no heterogeneity verse events.22
among the studies (I2 = 0%; heterogeneity, P = 0.98; Fig. 2). Our meta-analysis suggests that DFN-15 at a single dose of
120 mg is associated with substantially improved 2-hour pain
Sensitivity Analysis freedom and freedom from MBS for the acute treatment for mi-
There is no heterogeneity for the primary outcome, and thus, graine patients. In addition, DFN-15 is also documented to pro-
we do not perform the meta-analysis via omitting one study or vide significantly benefit to change in functional disability, relief
subgroup analysis to detect the heterogeneity. of photophobia, 24-hour satisfaction with treatment, use of rescue
medication, and sustained pain relief and pain freedom.14
Secondary Outcomes Migraine patients commonly have some problems of cardio-
vascular conditions, events, and procedures.24–28 Widely used
In comparison with the control intervention for migraine, triptans may even increase the risk of serious cardiovascular ad-
DFN-15 treatment can substantially increase freedom from MBS verse events by vasoconstriction and the activation of 5-HT1B
(RR, 1.40; 95% CI, 1.12–1.76; P = 0.003; Fig. 3), but has no sub- receptors.29–31 Long-term use of nonsteroidal anti-inflammatory
stantial impact on adverse events (RR, 1.34; 95% CI, 0.88–2.04; drugs (eg, COX-2–selective drugs) should be used with caution
P = 0.17; Fig. 4), dysgeusia (RR, 2.20; 95% CI, 0.97–5.00; in patients with cardiovascular risk factors. Two cardiovascular
P = 0.06; Fig. 5), or nausea (RR, 1.44; 95% CI, 0.54–3.85; events (eg, palpitation and hypertension) were reported to be very
P = 0.47; Fig. 6). low and similar between DFN-15 and placebo for migraine
patients.16
DISCUSSION Furthermore, this meta-analysis finds no statistical difference
Compared with the oral capsule formulation of celecoxib, of adverse events, dysgeusia, or nausea between the 2 groups.
120 mg DFN-15 (50 mg/mL) has a faster median time to peak Dysgeusia and nausea are the most common adverse events dur-
concentration (within 1 vs 2.5 hours), which affords more rapid ing DFN-15 treatment. The tolerability and safety of DFN-15
onset of pain relief and a treatment priority for people with mi- are generally favorable, with mostly mild adverse events. Several
graine.22,23 DFN-15 120 mg had a relative bioavailability of limitations exist in this meta-analysis. First, our analysis is based
144% (ie, 44% greater) compared with a 400-mg dose of on only 3 RCTs, and more RCTs with large sample size should
FIGURE 4. Forest plot of the meta-analysis of adverse events.
© 2020 Wolters Kluwer Health, Inc. All rights reserved. www.clinicalneuropharm.com 109
Copyright © 2020 Wolters Kluwer Health, Inc. All rights reserved.
Deng et al Clinical Neuropharmacology • Volume 43, Number 4, July/August 2020
FIGURE 5. Forest plot of the meta-analysis of dysgeusia.
FIGURE 6. Forest plot of the meta-analysis of nausea.
be conducted to explore this issue. Next, although there is no het- Subcommittee of the American Academy of Neurology. Neurology 2000;
erogeneity, different patient population may lead to some bias. Fi- 55(6):754–762.
nally, some unpublished and missing data may induce some bias 11. Marmura MJ, Silberstein SD, Schwedt TJ. The acute treatment of migraine
to the pooled effect. in adults: the American Headache Society evidence assessment of migraine
pharmacotherapies. Headache 2015;55(1):3–20.
12. Moore RA, Derry S, Makinson GT, et al. Tolerability and adverse events in
CONCLUSIONS clinical trials of celecoxib in osteoarthritis and rheumatoid arthritis:
DFN-15 treatment may be effective and safe for pain control systematic review and meta-analysis of information from company clinical
in migraine patients. trial reports. Arthritis Res Ther 2005;7(3):R644–R665.
13. Nissen SE, Yeomans ND, Solomon DH, et al. Cardiovascular safety of
celecoxib, naproxen, or ibuprofen for arthritis. N Engl J Med 2016;375:
REFERENCES
2519–2529.
1. MacGregor EA. Migraine. Ann Intern Med 2017;166(7):ITC49–ITC64.
14. Lipton RB, Munjal S, Brand-Schieber E, et al. Efficacy, tolerability, and
2. Schwedt TJ. Chronic migraine. BMJ 2014;348:g1416. safety of DFN-15 (celecoxib oral solution, 25 mg/mL) in the acute
3. Dodick DW, Silberstein SD, Lipton RB, et al. Early onset of effect of treatment of episodic migraine: a randomized, double-blind,
onabotulinumtoxinA for chronic migraine treatment: analysis of placebo-controlled study. Headache 2019;60(1):58–70.
PREEMPT data. Cephalalgia 2019;39(8):945–956. 15. Bennett A, Munjal S. A multi-center, randomized, placebo-controlled,
4. Tao H, Wang T, Dong X, et al. Effectiveness of transcutaneous electrical double-blind, crossover study evaluating DFN-15, a liquid celecoxib
nerve stimulation for the treatment of migraine: a meta-analysis of formulation, for the acute treatment of migraine with or without aura in
randomized controlled trials. J Headache Pain 2018;19(1):42. adults. Neuropsychiatr Dis Treat 2019;92: P2. 10-019.
5. Zhang H, Yang X, Lin Y, et al. The efficacy of greater occipital nerve block 16. Munjal S, Bennett A. Efficacy and safety of DFN-15, an oral liquid
for the treatment of migraine: a systematic review and meta-analysis. Clin formulation of celecoxib, in adults with migraine: a multicenter,
Neurol Neurosurg 2018;165:129–133. randomized, placebo-controlled, double-blind, crossover study.
6. Levy D, Strassman A. Distinct sensitizing effects of the cAMP-PKA Neuropsychiatr Dis Treat 2017;13:2797–2802.
second messenger cascade on rat dural mechanonociceptors. J Physiol 17. Moher D, Liberati A, Tetzlaff J, et al, P. Group. Preferred reporting items for
2002;538(2):483–493. systematic reviews and meta-analyses: the PRISMA statement. BMJ 2009;
7. Levy D, Strassman AM. Modulation of dural nociceptor 339:b2535.
mechanosensitivity by the nitric oxide-cyclic GMP signaling cascade. 18. Higgins JP. Cochrane Handbook for Systematic Reviews of Interventions
J Neurophysiol 2004;92(2):766–772. version 5.1. 0 [updated March 2011], The Cochrane Collaboration. 2011.
8. Chaudhry SR, Lendvai IS, Muhammad S, et al. Inter-ictal assay of Available at: http://handbook-5-1.cochrane.org. Accessed October 2, 2019.
peripheral circulating inflammatory mediators in migraine patients under 19. Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of
adjunctive cervical non-invasive vagus nerve stimulation (nVNS): a randomized clinical trials: is blinding necessary? Control Clin Trials 1996;
proof-of-concept study. Brain Stimul 2019;12(3):643–651. 17(1):1–12.
9. Law S, Derry S, Moore RA. Sumatriptan plus naproxen for the treatment 20. Kjaergard LL, Villumsen J, Gluud C. Reported methodologic quality and
of acute migraine attacks in adults. Cochrane Database Syst Rev discrepancies between large and small randomized trials in meta-analyses.
2016;4(4):CD008541. Ann Intern Med 2001;135(11):982–989.
10. Silberstein SD. Practice parameter: evidence-based guidelines for migraine 21. Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis.
headache (an evidence-based review): report of the Quality Standards Stat Med 2002;21(11):1539–1558.
110 www.clinicalneuropharm.com © 2020 Wolters Kluwer Health, Inc. All rights reserved.
Copyright © 2020 Wolters Kluwer Health, Inc. All rights reserved.
Clinical Neuropharmacology • Volume 43, Number 4, July/August 2020 DFN-15 for Migraine Treatment
22. Pal A, Shenoy S, Gautam A, et al. Pharmacokinetics of DFN-15, a novel oral 27. Rist PM, Winter AC, Buring JE, et al. Migraine and the risk of incident
solution of celecoxib, versus celecoxib 400-mg capsules: a randomized crossover hypertension among women. Cephalalgia 2018;38(12):
study in fasting healthy volunteers. Clin Drug Investig 2017;37(10):937–946. 1817–1824.
23. Lipton RB, Hamelsky SW, Dayno JM. What do patients with migraine 28. Al-Hassany L, Linstra K, Terwindt G, et al. Cardiovascular risk of migraine
want from acute migraine treatment? Headache 2002;42:3–9. in men and women. In: Gender and Migraine. Cham, Switzerland:
24. Buse DC, Reed ML, Fanning KM, et al. Cardiovascular events, conditions, Springer; 2019:17–29.
and procedures among people with episodic migraine in the US population: 29. Dodick DW, Martin VT, Smith T, et al. Cardiovascular tolerability and
results from the American Migraine Prevalence and Prevention (AMPP) safety of triptans: a review of clinical data. Headache 2004;44(Suppl 1):
study. Headache 2017;57(1):31–44. S20–S30.
25. Lipton RB, Reed ML, Kurth T, et al. Framingham-based cardiovascular risk 30. Nilsson T, Longmore J, Shaw D, et al. Characterisation of 5-HT receptors in
estimates among people with episodic migraine in the US population: human coronary arteries by molecular and pharmacological techniques.
results from the American Migraine Prevalence and Prevention (AMPP) Eur J Pharmacol 1999;372(1):49–56.
study. Headache 2017;57(10):1507–1521. 31. Kurth T, Winter AC, Eliassen AH, et al. Migraine and risk of cardiovascular
26. Linstra KM, Ibrahimi K, Terwindt GM, et al. Migraine and cardiovascular disease in women: prospective cohort study.
disease in women. Maturitas 2017;97:28–31. BMJ 2016;353:i2610.
© 2020 Wolters Kluwer Health, Inc. All rights reserved. www.clinicalneuropharm.com 111
Copyright © 2020 Wolters Kluwer Health, Inc. All rights reserved.
You might also like
- Asbestos FibreDocument20 pagesAsbestos FibreHasanuzzaman SumonNo ratings yet
- Hypertension: Unit-5 - Non-Communicable Disease Community Health Nursing - IDocument19 pagesHypertension: Unit-5 - Non-Communicable Disease Community Health Nursing - IPrabhakaran AranganathanNo ratings yet
- NCM 112 Lecture Module 4 Cellular AberrationDocument16 pagesNCM 112 Lecture Module 4 Cellular AberrationMeryville JacildoNo ratings yet
- Williams Study Guide Maternal AnatomyDocument5 pagesWilliams Study Guide Maternal AnatomyCarl Vin Pasion100% (1)
- Animal Flow TrainingDocument3 pagesAnimal Flow TrainingOmar CiauNo ratings yet
- Journal of Hand Therapy: Hayat Hamzeh PT, MSC, Mohammad Madi PT, PHD, Alia A. Alghwiri PT, PHD, Ziad Hawamdeh MD, PHDDocument9 pagesJournal of Hand Therapy: Hayat Hamzeh PT, MSC, Mohammad Madi PT, PHD, Alia A. Alghwiri PT, PHD, Ziad Hawamdeh MD, PHDWinda FRNo ratings yet
- Pharmacology in Drug Discovery: Understanding Drug ResponseFrom EverandPharmacology in Drug Discovery: Understanding Drug ResponseNo ratings yet
- Programmed - Intermittent - Epidural - Bolus - in Metanalisis Wang Et AlDocument17 pagesProgrammed - Intermittent - Epidural - Bolus - in Metanalisis Wang Et AlAlice MironesNo ratings yet
- Efficacy of Acupuncture For Generalized Anxiety.108Document10 pagesEfficacy of Acupuncture For Generalized Anxiety.108JonasMarçaloNo ratings yet
- Medicine: Comparison Between Acupuncture and Cognitive Behavioral Therapy For Primary InsomniaDocument5 pagesMedicine: Comparison Between Acupuncture and Cognitive Behavioral Therapy For Primary InsomniaJoão PauloNo ratings yet
- Linetzky Et Al 2015 Depression and AnxietyDocument9 pagesLinetzky Et Al 2015 Depression and AnxietyFaisal khanNo ratings yet
- Using Psychometric Techniques To Improve The Balance Evaluation Systems Test: The Mini-BestestDocument9 pagesUsing Psychometric Techniques To Improve The Balance Evaluation Systems Test: The Mini-BestestMochammad Syarif HidayatNo ratings yet
- Journal of Affective Disorders: Review ArticleDocument11 pagesJournal of Affective Disorders: Review Article賀立安No ratings yet
- Protocol NMA For TRDDocument8 pagesProtocol NMA For TRDNut SamprasitNo ratings yet
- Augmentation Therapies For Treatment-Resistant Depression: Systematic Review and Meta-AnalysisDocument10 pagesAugmentation Therapies For Treatment-Resistant Depression: Systematic Review and Meta-AnalysisjonascarvNo ratings yet
- ESA Prospect Thoracotomy Poster v10Document1 pageESA Prospect Thoracotomy Poster v10Andreea ShalidaNo ratings yet
- A Guide To Understanding Meta-AnalysisDocument14 pagesA Guide To Understanding Meta-AnalysisJesusNavarrete97No ratings yet
- NDT 12531 Comparative Efficacy of Escitalopram in The Treatment of Maj - 012811Document11 pagesNDT 12531 Comparative Efficacy of Escitalopram in The Treatment of Maj - 012811pantea_mihai_1No ratings yet
- Effect of Different Types of Anesthesia On.23 PDFDocument5 pagesEffect of Different Types of Anesthesia On.23 PDFHelsie DahokloryNo ratings yet
- Guia Entender MetaanalisisDocument14 pagesGuia Entender MetaanalisisResidentes urologiaNo ratings yet
- Courtney - 2022 - Oi - 211279 - 1643056684.29546 1Document22 pagesCourtney - 2022 - Oi - 211279 - 1643056684.29546 1U of T MedicineNo ratings yet
- Journal Reading: Dr. Said Shofwan, SP - An Ria Dewi Pranastuti 30101206720 Hesti Hermawati 3010120Document23 pagesJournal Reading: Dr. Said Shofwan, SP - An Ria Dewi Pranastuti 30101206720 Hesti Hermawati 3010120Nurmalita CaesarliaNo ratings yet
- A Guide To Understanding Meta-AnalysisDocument9 pagesA Guide To Understanding Meta-AnalysisTadesse MenjettaNo ratings yet
- Israel Richter 2011 A Guide To Understanding Meta AnalysisDocument16 pagesIsrael Richter 2011 A Guide To Understanding Meta AnalysisDavid AlarconNo ratings yet
- Fpubh 11 1187382Document10 pagesFpubh 11 1187382Utami NadyaNo ratings yet
- Mediators and Moderators of Treatment Effects in Randomized Clinical TrialsDocument7 pagesMediators and Moderators of Treatment Effects in Randomized Clinical TrialsCoordinacionPsicologiaVizcayaGuaymasNo ratings yet
- Evaluation of Scientific Publications - Part 20 - Establishing Equivalence or Non-Inferiority in Clinical Trials PDFDocument6 pagesEvaluation of Scientific Publications - Part 20 - Establishing Equivalence or Non-Inferiority in Clinical Trials PDFPhoNo ratings yet
- Matrix 1Document2 pagesMatrix 1josephmainam9No ratings yet
- Meta-Analisis Paracetamol TunggalDocument8 pagesMeta-Analisis Paracetamol TunggalAlexander KwaitotaNo ratings yet
- Clinical Trial DesignDocument16 pagesClinical Trial Designsorianokristine12No ratings yet
- Sugammadex For Reversal of Rocuronium-Induced Neuromuscular Blockade in Pediatric PatientsDocument7 pagesSugammadex For Reversal of Rocuronium-Induced Neuromuscular Blockade in Pediatric PatientsAllonsiny GutierrezNo ratings yet
- BR J Sports Med - 23 - Exercise As Medicine For Depressive Symptoms - A Systematic Review and Meta-Analysis With Meta-RegressionDocument10 pagesBR J Sports Med - 23 - Exercise As Medicine For Depressive Symptoms - A Systematic Review and Meta-Analysis With Meta-RegressionVictoria AlmeidaNo ratings yet
- Efficacy Corticosteroid On GBSDocument11 pagesEfficacy Corticosteroid On GBSRestu TriwulandaniNo ratings yet
- The Efficacy of Kinesio Taping As An Adjunct To.72 PDFDocument9 pagesThe Efficacy of Kinesio Taping As An Adjunct To.72 PDFMenna Allah MohammedNo ratings yet
- Expermintal EpidDocument9 pagesExpermintal EpidHannan AliNo ratings yet
- Efficacy and Safety of Transcranial Magnetic Stimulation For T - 2023 - ClinicalDocument15 pagesEfficacy and Safety of Transcranial Magnetic Stimulation For T - 2023 - Clinicalo122811027No ratings yet
- A Guide To UnderstandingDocument9 pagesA Guide To UnderstandingΚυριάκος ΠαπαδόπουλοςNo ratings yet
- OSTEOPATIADocument15 pagesOSTEOPATIAKarina MoroNo ratings yet
- E300630 FullDocument8 pagesE300630 FullAbdualaziz AlmalkiNo ratings yet
- Medicine: Pharmacological and Psychotherapeutic Interventions For Management of Poststroke DepressionDocument5 pagesMedicine: Pharmacological and Psychotherapeutic Interventions For Management of Poststroke DepressionaditNo ratings yet
- Interventional Study DesignsDocument11 pagesInterventional Study DesignshalimNo ratings yet
- Iosifescu (2011) - Electroencephalography-Derived Biomarkers of Antidepressant Response.Document11 pagesIosifescu (2011) - Electroencephalography-Derived Biomarkers of Antidepressant Response.Julieht RodriguezNo ratings yet
- Meta-Analysis Random Effects Riley Higgins BMJ 2011Document4 pagesMeta-Analysis Random Effects Riley Higgins BMJ 2011Fellow HumanNo ratings yet
- Maas2020 Article TranexamicAcidInTraumaticBrainDocument3 pagesMaas2020 Article TranexamicAcidInTraumaticBrainMiguel Ángel Ramírez AmbrízNo ratings yet
- Efficacy and Safety of Electroconvulsive Therapy in Depressive D 2003 1Document10 pagesEfficacy and Safety of Electroconvulsive Therapy in Depressive D 2003 1Gonzalo VeizagaNo ratings yet
- Endogenous Pain Modulation in Chronic Orofacial.4Document15 pagesEndogenous Pain Modulation in Chronic Orofacial.4prokin_martinezNo ratings yet
- Neu 2015 4192Document14 pagesNeu 2015 4192Dea RitungNo ratings yet
- Exercise and Sleep: A Systematic Review of Previous Meta-AnalysesDocument11 pagesExercise and Sleep: A Systematic Review of Previous Meta-AnalysesAlexPsrNo ratings yet
- Z Al-Roubaie - 2020Document12 pagesZ Al-Roubaie - 2020Kossay ZaouiNo ratings yet
- Classification of ResearchDocument41 pagesClassification of ResearchMuhammad Arslan AslamNo ratings yet
- Biologic Therapy For Psoriatic Arthritis or Moderate To Severe Plaque Psoriasis: Systematic Review With Pairwise and Network Meta-AnalysisDocument14 pagesBiologic Therapy For Psoriatic Arthritis or Moderate To Severe Plaque Psoriasis: Systematic Review With Pairwise and Network Meta-AnalysislilingNo ratings yet
- Medicine: The Effectiveness of Acupuncture For Chronic Pain With DepressionDocument6 pagesMedicine: The Effectiveness of Acupuncture For Chronic Pain With DepressionRatrika SariNo ratings yet
- Pharmacological Therapy For Acute Spinal Cord Injury. in Guidelines For The Management of Acute Cervical Spine and Spinal Cord Injuries.Document10 pagesPharmacological Therapy For Acute Spinal Cord Injury. in Guidelines For The Management of Acute Cervical Spine and Spinal Cord Injuries.Madalina TalpauNo ratings yet
- Acm 2019 0113 PDFDocument9 pagesAcm 2019 0113 PDFFirda UfairahNo ratings yet
- Systemic Nonsteroidal Anti Inflammatories For.6Document11 pagesSystemic Nonsteroidal Anti Inflammatories For.6Edward ElBuenoNo ratings yet
- Jurnal Reading 2Document6 pagesJurnal Reading 2dezafarista_44587428No ratings yet
- Comparative Effectiveness and Safety of Analgesic Medicines For Adults With Acute Non-Specific Low Back PainDocument15 pagesComparative Effectiveness and Safety of Analgesic Medicines For Adults With Acute Non-Specific Low Back PainRachel PutriNo ratings yet
- Triptans in Prevention of Menstrual Migraine: A Systematic Review With Meta-AnalysisDocument9 pagesTriptans in Prevention of Menstrual Migraine: A Systematic Review With Meta-AnalysisRadiTriHadrianNo ratings yet
- Co Administration of Dexamethasone With Peripheral Nerve Bloc 2018 British JDocument16 pagesCo Administration of Dexamethasone With Peripheral Nerve Bloc 2018 British JSeveNNo ratings yet
- Jackson2017 Article TricyclicAndTetracyclicAntidepDocument8 pagesJackson2017 Article TricyclicAndTetracyclicAntidepAndreas NatanNo ratings yet
- The - Erlangen - Test - of - Activities - of - Daily - Living - in BDocument2 pagesThe - Erlangen - Test - of - Activities - of - Daily - Living - in Bkwstas79No ratings yet
- Complementary Therapies in Clinical PracticeDocument7 pagesComplementary Therapies in Clinical PracticeBkash ShahNo ratings yet
- Part 17 PDFDocument6 pagesPart 17 PDFKarolina PolskaNo ratings yet
- Cheung Et Al - Overview of Systematic Reviews of The Effectiveness of Reminders in Improving Healthcare Professional BehaviorDocument8 pagesCheung Et Al - Overview of Systematic Reviews of The Effectiveness of Reminders in Improving Healthcare Professional BehaviorabcNo ratings yet
- Benefits and Harms of Spinal Manipulative Therapy For The Treatment of Chronic Low Back PainDocument15 pagesBenefits and Harms of Spinal Manipulative Therapy For The Treatment of Chronic Low Back PainRachel PutriNo ratings yet
- Mosso's Ergography With VideoDocument21 pagesMosso's Ergography With VideoRavi DuttNo ratings yet
- Livestock Product TechnologyDocument3 pagesLivestock Product TechnologyRajat SinghNo ratings yet
- Ucat Planner: The Ultimate Guide To Scoring in The Top 1%Document16 pagesUcat Planner: The Ultimate Guide To Scoring in The Top 1%AyaNo ratings yet
- CWTS LTS Specific Module 3 Introduction To Community Based Management 2Document16 pagesCWTS LTS Specific Module 3 Introduction To Community Based Management 2kingluffy244466666No ratings yet
- The Study of Knowledge, Attitude and Practice Among Diabetic Patients During Ramadan at Hospital Tengku Ampuan AfzanDocument10 pagesThe Study of Knowledge, Attitude and Practice Among Diabetic Patients During Ramadan at Hospital Tengku Ampuan AfzanIzzul HafiyNo ratings yet
- ENVPEP1406022EN PM8243 Power and Energy Meter Life CycleDocument5 pagesENVPEP1406022EN PM8243 Power and Energy Meter Life CycleSamsung JosephNo ratings yet
- Appropriate Conservatism in Safety Cases: The UK Nuclear Industry Good Practice Guide ToDocument16 pagesAppropriate Conservatism in Safety Cases: The UK Nuclear Industry Good Practice Guide ToEm GerNo ratings yet
- AnemiaDocument10 pagesAnemiaRamesh VaradharajanNo ratings yet
- Never Give Up EssayDocument8 pagesNever Give Up Essayfz640x4t100% (2)
- Prostitution: A Feminist Perspective: Hidayatullah National Law UniversityDocument24 pagesProstitution: A Feminist Perspective: Hidayatullah National Law UniversityApoorvaChandraNo ratings yet
- Clendario 2023Document1 pageClendario 2023Edgar SanaNo ratings yet
- On Becoming A Teacher: Field Study 6Document3 pagesOn Becoming A Teacher: Field Study 6Marvin Dagdag MoralesNo ratings yet
- Write - Up - Adhoc Data SourcesDocument12 pagesWrite - Up - Adhoc Data SourcesRaju BaiNo ratings yet
- Minipar Breast-Fibroadenoma Group2 n21Document71 pagesMinipar Breast-Fibroadenoma Group2 n21Kristine AcasioNo ratings yet
- Speaking Presentations Past Paper Sample ScriptsDocument3 pagesSpeaking Presentations Past Paper Sample ScriptsbillkiNo ratings yet
- Retrocuspid Papilla Presenting As A Giant Cell F - 2022 - Journal of Dental ScieDocument2 pagesRetrocuspid Papilla Presenting As A Giant Cell F - 2022 - Journal of Dental ScieDavid ABCNo ratings yet
- Ta2 Speaking WritingDocument3 pagesTa2 Speaking Writingvohiep14122004No ratings yet
- Dry Needling Versus Trigger Point Injection For Neck PainDocument11 pagesDry Needling Versus Trigger Point Injection For Neck PainDavid ElirazNo ratings yet
- Quiz - 7024 - de Thi Vao Lop 10 Chuyen Anh Truong THPT Chuyen DH Su Pham Ha Noi - 2021Document17 pagesQuiz - 7024 - de Thi Vao Lop 10 Chuyen Anh Truong THPT Chuyen DH Su Pham Ha Noi - 2021TiengAnhK12 HTKHNo ratings yet
- Fatalities Nursing Home AcfDocument11 pagesFatalities Nursing Home AcfNewsChannel 9No ratings yet
- Asphalt - MC 3000 (Superior) - Superior Refining Company, LLC (Husky Energy)Document10 pagesAsphalt - MC 3000 (Superior) - Superior Refining Company, LLC (Husky Energy)Lindsey BondNo ratings yet
- Nursing Management: Nutritional Problems (Chapter 40) : MalnutritionDocument2 pagesNursing Management: Nutritional Problems (Chapter 40) : MalnutritionPrince K. TaileyNo ratings yet
- GPA One Pager - Mail - Savings AccountDocument2 pagesGPA One Pager - Mail - Savings Accountsumit kumarNo ratings yet
- Communication: Improving Patient Safety With SbarDocument7 pagesCommunication: Improving Patient Safety With Sbarria kartini panjaitanNo ratings yet
- Reading Love and AttractionDocument3 pagesReading Love and AttractionLaura Elena HernándezNo ratings yet