Professional Documents
Culture Documents
Untitled
Uploaded by
herdian ariebowoCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Untitled
Uploaded by
herdian ariebowoCopyright:
Available Formats
Research
JAMA Oncology | Original Investigation
Comparison of Prophylactic Intravenous Antibiotic
Regimens After Endoprosthetic Reconstruction
for Lower Extremity Bone Tumors
A Randomized Clinical Trial
The Prophylactic Antibiotic Regimens in Tumor Surgery (PARITY) Investigators
Visual Abstract
IMPORTANCE The use of perioperative, prophylactic, intravenous antibiotics is standard Editorial page 340
practice to reduce the risk of surgical site infection after oncologic resection and complex
endoprosthetic reconstruction for lower extremity bone tumors. However, evidence guiding Supplemental content
the duration of prophylactic treatment remains limited.
OBJECTIVE To assess the effect of a 5-day regimen of postoperative, prophylactic,
intravenous antibiotics compared with a 1-day regimen on the rate of surgical site infections
within 1 year after surgery.
DESIGN, SETTING, AND PARTICIPANTS This randomized clinical superiority trial was performed
at 48 clinical sites in 12 countries from January 1, 2013, to October 29, 2019. The trial included
patients with a primary bone tumor or a soft tissue sarcoma that had invaded the femur or
tibia or oligometastatic bone disease of the femur or tibia with expected survival of at least 1
year who required surgical management by excision and endoprosthetic reconstruction. A
total of 611 patients were enrolled, and 7 were excluded for ineligibility.
INTERVENTIONS A 1- or 5-day regimen of postoperative prophylactic intravenous
cephalosporin (cefazolin or cefuroxime) that began within 8 hours after skin closure and was
administered every 8 hours thereafter. Those randomized to the 1-day regimen received
identical saline doses every 8 hours for the remaining 4 days; patients, care providers, and
outcomes assessors were blinded to treatment regimen.
MAIN OUTCOMES AND MEASURES The primary outcome in this superiority trial was a surgical
site infection (superficial incisional, deep incisional, or organ space) classified according to the
criteria established by the Centers for Disease Control and Prevention within 1 year after
surgery. Secondary outcomes included antibiotic-related complications, unplanned additional
operations, oncologic and functional outcomes, and mortality.
RESULTS Of the 604 patients included in the final analysis (mean [SD] age, 41.2 [21.9] years;
361 [59.8%] male; 114 [18.9%] Asian, 43 [7.1%] Black, 34 [5.6%] Hispanic, 15 [2.5%]
Indigenous, 384 [63.8%] White, and 12 [2.0%] other), 293 were randomized to a 5-day
regimen and 311 to a 1-day regimen. A surgical site infection occurred in 44 patients (15.0%)
allocated to the 5-day regimen and in 52 patients (16.7%) allocated to the 1-day regimen
(hazard ratio, 0.93; 95% CI, 0.62-1.40; P = .73). Antibiotic-related complications occurred in
15 patients (5.1%) in the 5-day regimen and in 5 patients (1.6%) allocated to the 1-day regimen
(hazard ratio, 3.24; 95% CI, 1.17-8.98; P = .02). Other secondary outcomes did not differ
significantly between treatment groups.
CONCLUSIONS AND RELEVANCE This randomized clinical trial did not confirm the superiority of
a 5-day regimen of postoperative intravenous antibiotics over a 1-day regimen in preventing Group Information: The members of
surgical site infections after surgery for lower extremity bone tumors that required an the PARITY Writing Committee
endoprosthesis. The 5-day regimen group had significantly more antibiotic-related appear at the end of the article. All
other members of the PARITY
complications. Investigators appear in
Supplement 3.
TRIAL REGISTRATION ClinicalTrials.gov Identifier: NCT01479283
Corresponding Author: Michelle
Ghert, MD, Division of Orthopaedic
Surgery, Department of Surgery,
McMaster University, 711 Concession
St, Section B, Level 3, Room 169A,
JAMA Oncol. 2022;8(3):345-353. doi:10.1001/jamaoncol.2021.6628 Hamilton, ON L8V 1C3, Canada
Published online January 6, 2022. (ghertm@mcmaster.ca).
(Reprinted) 345
Downloaded From: https://jamanetwork.com/ on 03/08/2023
Research Original Investigation Prophylactic Antibiotic Regimens After Endoprosthetic Reconstruction for Lower Extremity Bone Tumors
O
perations to remove malignant tumors of the femur
or tibia involve the resection of the affected bone Key Points
and surrounding soft tissue followed by complex re- Question Can a 5-day regimen of postoperative, prophylactic,
construction of the limb. The most common reconstruction intravenous antibiotics reduce the rate of surgical site infections in
involves the use of modular metallic and polyethylene endo- patients with a lower extremity bone tumor undergoing complex
prostheses to replace surgically resected bones and joints. Be- endoprosthetic reconstruction compared with a 1-day regimen?
cause of the length and intricacies of these procedures and the Findings In this randomized clinical trial including 604 patients in
medical complexity of these patients, the risk of a surgical site the primary analysis, the 5-day regimen did not reduce the rate of
infection is high.1-3 Attempts to eradicate the organism often surgical site infection compared with the 1-day regimen, although
it resulted in a higher rate of antibiotic-related complications,
fail and result in the eventual need for amputation in nearly
notably Clostridioides difficile–associated colitis.
50% of patients, thereby strongly affecting patient function
and quality of life and delaying the administration of adju- Meaning The results of this study suggest that prolonging use of
postoperative antibiotics beyond 1 day does not reduce the rate of
vant cancer therapies.1-4
surgical site infection but increases the risk of clinically significant
Strategies to minimize surgical site infections in this
antibiotic-related complications.
population include the administration of perioperative intra-
venous antibiotics. The most effective antibiotic regimen to
prevent surgical site infections remains uncertain and cur- study followed the Consolidated Standards of Reporting
rent clinical practice is highly varied, particularly with re- Trials (CONSORT) reporting guideline.
spect to antibiotic duration. Approximately 2 of every 3 sur-
geons prescribe prolonged courses well beyond the 24-hour Patients
recommended duration for standard total joint replacement From January 1, 2013, to October 29, 2019, investigators at 48
operations.5-8 However, overuse of antibiotics can lead to an- clinical sites across Canada, the US, Argentina, Australia, Aus-
tibiotic-related complications and antibiotic resistance; anti- tria, Brazil, Egypt, India, the Netherlands, Singapore, South
biotic stewardship, therefore, remains a salient issue.9 We con- Africa, and Spain recruited patients for the study. Eligible
ducted the Prophylactic Antibiotic Regimens in Tumor Surgery patients included all individuals 12 years or older with a pri-
(PARITY) trial to inform the effect of a 5-day regimen of post- mary bone tumor or a soft tissue sarcoma that had invaded
operative, prophylactic, intravenous antibiotics compared with the femur or tibia or oligometastatic bone disease of the
a 1-day regimen on the prevention of surgical site infections femur or tibia with expected survival of at least 1 year who
and on antibiotic adverse effects in patients requiring surgi- required surgical management by excision and endopros-
cal resection and endoprosthetic reconstruction for a lower thetic reconstruction. Patients with previous infections at
extremity bone tumor. the surgical site or who were known to be colonized with
methicillin-resistant Staphylococcus aureus or vancomycin-
resistant Enterococcus were excluded. A total of 895 patients
were screened for eligibility, and 7 patients were adjudicated
Methods to be ineligible at the time of randomization; thus, of the 611
Trial Design and Oversight patients randomized, 604 were included in the final analyses.
This intention-to-treat study was an investigator-initiated, The final 1-year assessments were completed in March 2021.
international, blinded (patients, surgeons, outcomes asses- Details on the eligibility criteria are available in the eAppendix
sors, and data analysts), parallel, superiority randomized in Supplement 2.
clinical trial. The rationale, design, and methods of the trial
have been previously published.10 Written informed con- Trial Interventions and Procedures
sent was required to participate in the study, and all data Surgical procedures were performed according to the stan-
were deidentified. Supplement 1 (the Trial Protocol) and dard practices at each clinical site. All patients received stan-
Supplement 2 provide information on eligibility criteria, dardized preoperative and intraoperative prophylactic in-
interventions, blinding, follow-up, outcomes definitions, travenous antibiotics. Patients were randomly allocated
and statistical analysis. The Hamilton Integrated Research perioperatively in a 1-to-1 ratio to receive a 1- or 5-day postop-
Ethics Board as well as the relevant local ethics committee erative prophylactic regimen of an intravenous cephalo-
at each participating site approved the trial protocol and its sporin (cefazolin or cefuroxime); they were blinded to the treat-
amendments before local study initiation. In addition, the ment regimen. Those randomized to the 1-day regimen received
following regulatory bodies also approved the trial protocol identical saline (placebo) doses for the remaining 4 days. Ran-
and its amendments: Health Canada, the Brazilian National domization, stratified according to tumor location (femur or
Health Surveillance Agency, the European Medicines tibia) and clinical site, was centralized through an internet-
Agency (including the competent authorities in Austria and based, computer-generated platform that concealed alloca-
Spain), the Indian Council of Medical Research, and the tion and used randomly permuted blocks of 2 or 4. An un-
Republic of South Africa’s Department of Health. The PAR- blinded member of the local investigational pharmacy
ITY Data and Safety Monitoring Board, composed of 2 performed the randomization. Patients began their ran-
orthopedic oncologists and 1 statistician who were indepen- domly allocated, postoperative, prophylactic antibiotic regi-
dent of the study team, reviewed the trial outcomes. This men within 8 hours after skin closure, and the doses were in-
346 JAMA Oncology March 2022 Volume 8, Number 3 (Reprinted) jamaoncology.com
Downloaded From: https://jamanetwork.com/ on 03/08/2023
Prophylactic Antibiotic Regimens After Endoprosthetic Reconstruction for Lower Extremity Bone Tumors Original Investigation Research
travenously administered every 8 hours. Clinical sites used mary outcome. The analysis included all patients in the groups
their own inventory to prepare the study antibiotics or pla- to which they were randomly allocated. Postoperative antibi-
cebo. Preparation, blinding of study antibiotics or placebo, and otic duration (treatment group) was the independent vari-
storage and administration of the study antibiotics were con- able, and the Cox proportional hazards regression included
ducted as per local procedures established at each clinical site tumor location and clinical site as stratification variables.
and the relevant manufacturers’ labels. Further details on the Patients who did not experience the primary outcome were
intravenous antibiotic regimens are available in the eAppen- censored at 1 year or at the time of last study visit. We tested
dix in Supplement 2. the proportional hazards assumption of the Cox proportional
hazards regression model by examining Schoenfeld residuals.
Outcome Measures We also performed several sensitivity analyses for the primary
The primary outcome was the development of a surgical site outcome, including a competing risks analysis that accounted
infection (superficial incisional, deep incisional, or organ for deaths and amputation as competing risks. We identified
space [deep prosthetic infection]) within 1 year of the date of the following 5 subgroups a priori, which we analyzed in
surgery. Surgical site infections were classified according the primary model to assess for possible effect modifica-
to the criteria established by the Centers for Disease Control tion: tumor type, tumor location, sex, age, and preoperative
and Prevention.11 Secondary outcomes included antibiotic- chemotherapy.
related complications, unplanned additional operations, death, We assessed the effect of postoperative antibiotic dura-
and oncologic and functional outcomes within 1 year after sur- tion on the secondary outcomes using Cox proportional haz-
gical resection and endoprosthetic reconstruction. Validated ards regressions with treatment group as the independent
functional assessments included the Musculoskeletal Tumor variable and tumor location and clinical site as stratification
Society 1987 (MSTS-87) (range, 0-35, with higher scores indi- variables. We also estimated the effect of postoperative antibi-
cating better function) and 1993 (MSTS-93) (range, 0-100, with otic duration on functional outcomes at 1 year using multiple
higher scores indicating better function) scores and the To- linear regression models that included treatment group,
ronto Extremity Salvage Score (TESS) (range, 0-100, with higher tumor location, clinical site, and baseline score as indepen-
scores indicating better function).12-14 dent variables. We used multiple imputation to address miss-
Patients were assessed for study events by their treating ing functional outcome data.
surgeon at 2 and 6 weeks, 3, 6, and 9 months, and 1 year post- The results are presented as hazard ratios (HRs) for
operatively. The functional assessments were completed be- time-to-event outcomes and mean difference for continuous
fore surgery and at the 1-year follow-up visit. The blinded Cen- outcomes, with corresponding 95% CIs and associated 2-sided
tral Adjudication Committee adjudicated all primary and key P values. No adjustments were made for multiple testing. Ka-
secondary outcome events identified during the 1-year study plan-Meier curves were constructed for the primary out-
follow-up as well as all instances when eligibility was in doubt. come. These analyses were first completed using blinded treat-
ment groups by the data analyst (D.H.-A.). Interpretations for
Statistical Analysis the effect of antibiotic duration were developed and docu-
The justification for the PARITY trial sample size has been pre- mented based on blinded group A vs B. The randomization code
viously published.10,15 At the trial’s onset, we calculated that was then broken, the correct a priori interpretation selected,
the definitive sample size would require a total of 920 pa- and the manuscript drafted. All analyses were conducted using
tients based on a between-group comparison of deep pros- SAS software, version 9.4 (SAS Institute Inc).
thetic infection. The sample size was calculated as a noninfe-
riority trial under the assumption of an overall 10% event rate
with an absolute difference of 5% in the risk of deep surgical
site infection within 1 year to define noninferiority. After ini-
Results
tiating enrollment and then transitioning from the vanguard Study Patients
to the definitive phase of the trial, we expanded the trial’s pri- Of the 604 patients included in the final analysis (mean [SD]
mary outcome from deep to any surgical site infection and age, 41.2 [21.9] years; 361 [59.8%] male; 114 [18.9%] Asian, 43
changed the study’s design to a superiority trial to increase the [7.1%] Black, 34 [5.6%] Hispanic, 15 [2.5%] Indigenous, 384
expected event rate and feasibility without compromising clini- [63.8%] White, and 12 [2.0%] other [3 Middle Eastern, 5 mixed
cal importance. The expanded definition of the primary out- race, 2 North African, 1 Polynesian, and 1 Turkish]), 293 were
come resulted in an overall vanguard phase event rate of 14%.16 randomized to a 5-day regimen and 311 to a 1-day regimen. Of
Therefore, with a presumed 50% or greater reduction in the the 527 patients alive at 1 year, 496 (94%) had 1-year fol-
relative risk of deep surgical site infection within 1 year and low-up data available. Figure 1 and the eAppendix (Section 5.0)
with a 2-sided α of .05 and study power of 80%, we planned and eTables 1 and 2 in Supplement 2 provide details regard-
the definitive trial’s sample size to include 300 patients per arm, ing patient flow and the reasons for exclusion.
for a total of 600 patients. Table 1 and eTables 3 to 5 in Supplement 2 present patient
When conducting the final analyses, we adhered to the characteristics and demonstrate similar characteristics in the
published statistical analysis plan.15 Briefly, for the primary 2 groups. The most common tumor type was a primary bone
analysis, we used a Cox proportional hazards regression model tumor located predominantly in the femur. A total of 290 pa-
with time from surgery to the surgical site infection as the pri- tients (48.0%) received preoperative chemotherapy; 22 (3.6%)
jamaoncology.com (Reprinted) JAMA Oncology March 2022 Volume 8, Number 3 347
Downloaded From: https://jamanetwork.com/ on 03/08/2023
Research Original Investigation Prophylactic Antibiotic Regimens After Endoprosthetic Reconstruction for Lower Extremity Bone Tumors
Figure 1. Patient Flow Diagram
895 Patients screened
252 Patients ineligible
643 Patients eligible
32 Patients eligible but not enrolled (missed)
611 Patients randomized
299 Patients allocated to 5-d regimen 312 Patients allocated to 1-d regimen
6 Patients ineligible per adjudication committee 1 Patient ineligible per adjudication committee
2 Did not provide informed consent 1 Unsuitable for treatment by surgical
1 Unsuitable for treatment by surgical excision and endoprosthetic reconstruction
excision and endoprosthetic reconstruction
1 Skin was known to be colonized with MRSA
or VRE 311 Patients included in primary analysis
1 Prior local infection within the surgical field
1 Known to have an immunologically deficient
disease condition 255 Patients with complete 1-y follow-up
293 Patients included in primary analysis
MRSA indicates methicillin-resistant
241 Patients with complete 1-y follow-up
Staphylococcus aureus; VRE,
vancomycin-resistant Enterococcus.
received preoperative radiotherapy. There was an imbalance Adjusted analyses yielded similar results to those in the pri-
between treatment groups, with 129 of 293 patients (44.0%) mary analysis. Subgroup analyses did not show any effect
allocated to the 5-day regimen having received preoperative modification, including when adjusted for preoperative
chemotherapy compared with 161 of 311 patients (51.8%) allo- chemotherapy. Figure 3 and eTables 7 and 8 in Supplement 2
cated to the 1-day regimen. provide details regarding the sensitivity and subgroup
analyses.
Adherence to the Allocated Intervention
Two patients (0.6%) who had originally been allocated to a Secondary Outcomes
1-day regimen received a 5-day regimen; no patients origi- Antibiotic-Related Complications, Unplanned Additional
nally allocated to a 5-day regimen crossed over to a 1-day regi- Operations, Oncologic Events, and Mortality
men. Protocol deviations primarily resulted from inpatient hos- Study-related antibiotic-related complications occurred in 15
pital discharge earlier than 5 days postoperatively and were patients (5.1%) allocated to the 5-day regimen and in 5 pa-
similar between groups. Of those allocated to the 5-day regi- tients (1.6%) allocated to the 1-day regimen (HR, 3.24; 95%
men, 248 patients (84.6%) received all but the final 3 doses of CI, 1.17-8.98; P = .02) (Table 2). The most common antibiotic-
intravenous infusions as did 256 patients (82.6%) allocated to related complication was Clostridioides difficile–associated coli-
the 1-day regimen. eTable 6 in Supplement 2 provides details tis (Table 2). Unplanned additional operations occurred in 75
regarding the administration of the antibiotics. patients (25.6%) allocated to the 5-day regimen and in 80 pa-
tients (25.7%) allocated to the 1-day regimen (HR, 1.06; 95%
Primary Outcome CI, 0.77-1.46) (eTable 9 in Supplement 2). The most common
A surgical site infection occurred within 1 year in 44 of 293 pa- types of additional operations were irrigation and debride-
tients (15.0%) allocated to the 5-day regimen and in 52 of 311 ment and implant exchange, most of which were to treat a deep
patients (16.7%) allocated to the 1-day regimen (HR, 0.93; 95% incisional or organ space surgical site infection. Oncologic
CI, 0.62-1.40; P = .73) (Figure 2 and Table 2). The Schoenfeld events (HR, 1.02; 95% CI, 0.75-1.39) and mortality (HR, 1.01;
residuals demonstrate that the assumption of proportional haz- 95% CI, 0.64-1.58) proved similar between the treatment
ards for the primary outcome was not violated. Table 2 pre- groups (Table 2 and eTable 9 in Supplement 2).
sents the incidence of superficial incisional, deep incisional,
and organ space surgical site infections for each group. The Functional Outcomes
most common causative organisms of surgical site infections Surgeon-reported function was similar between the treat-
were S aureus and coagulase-negative staphylococci. ment groups as measured by the MSTS-87 scores (mean dif-
The results were similar in the sensitivity analyses that ference, −0.49; P = .41) and MSTS-93 scores (mean differ-
accounted for deaths and amputation as competing risks. ence, −1.89; P = .34) as was patient-reported function between
348 JAMA Oncology March 2022 Volume 8, Number 3 (Reprinted) jamaoncology.com
Downloaded From: https://jamanetwork.com/ on 03/08/2023
Prophylactic Antibiotic Regimens After Endoprosthetic Reconstruction for Lower Extremity Bone Tumors Original Investigation Research
Table 1. Baseline Characteristics of the Study Patientsa
Characteristic 5-d Regimen (n = 293) 1-d Regimen (n = 311) Total (n = 604)
Patient demographic
characteristics and tumor
details
Age, mean (SD), y 42.6 (21.7) 39.9 (22.0) 41.2 (21.9)
Sex
Male 178 (60.8) 183 (58.8) 361 (59.8)
Female 115 (39.2) 128 (41.2) 243 (40.2)
Race and ethnicity
Asian 54 (18.4) 60 (19.4) 114 (18.9)
Black 21 (7.2) 22 (7.1) 43 (7.1)
Hispanic 14 (4.8) 20 (6.5) 34 (5.6)
Indigenous 4 (1.4) 11 (3.6) 15 (2.5)
White 194 (66.2) 190 (61.5) 384 (63.8)
Otherb 6 (2.0) 6 (1.9) 12 (2.0)
Unknown 0 2 2
Systemic metastases
No 244 (83.3) 255 (82.0) 499 (82.6)
Yes 49 (16.7) 56 (18.0) 105 (17.4)
Other cancer treatment modalities
No 157 (53.6) 138 (44.4) 295 (48.8)
Yes 136 (46.4) 173 (55.6) 309 (51.2)
Preoperative 129 (44.0) 161 (51.8) 290 (48.0)
chemotherapy
Preoperative radiation 10 (3.4) 12 (3.9) 22 (3.6)
Other 7 (2.4) 7 (2.3) 14 (2.3)
Location of tumor
Tibia 53 (18.1) 55 (17.7) 108 (17.9)
Femur 240 (81.9) 256 (82.3) 496 (82.1)
Type of tumor
Bone tumor 237 (80.9) 249 (80.1) 486 (80.5)
Soft tissue sarcoma 28 (9.6) 34 (10.9) 62 (10.3)
Oligometastatic bone 28 (9.6) 28 (9.0) 56 (9.3)
disease
c
Neutropenia at time of surgery
No. of patients 275 286 561
No 231 (84.0) 234 (81.8) 465 (82.9)
Yes 44 (16.0) 52 (18.2) 96 (17.1)
Surgical and perioperative management details
Length of procedure, median 270 (206-377) 270 (200-377) 270 (205-377)
(Q1-Q3), min
Antibiotic or silver-coated Abbreviation: Q1-Q3, quartile 1 to
prosthesis
quartile 3.
No. of patients 292 311 603
a
Data are presented as number
No 276 (94.5) 295 (94.9) 571 (94.7)
(percentage) of patients unless
Yes 16 (5.5) 16 (5.1) 32 (5.3) otherwise indicated.
Antibiotic 6 (2.1) 6 (1.9) 12 (2.0) b
Other ethnicity includes Middle
Silver-coated prosthesis 10 (3.4) 10 (3.2) 20 (3.3) Eastern (n = 3), mixed race (n = 5),
Suction drain used North African (n = 2), Polynesian
No. of patients 293 310 603 (n = 1), and Turkish (n = 1).
c
No 63 (21.5) 74 (23.9) 137 (22.7) Absolute neutrophil count of
1500/μL or less (to convert to
Yes 230 (78.5) 236 (76.1) 466 (77.3)
×109/L, multiply by 0.001).
the 2 groups as measured by the TESS (mean difference, 0.10; cephalosporins compared with a 1-day regimen in reducing sur-
P = .96) (eTable 10 in Supplement 2). gical site infections after surgical resection and endoprosthetic
reconstruction for a lower extremity bone tumor. However, 3
times as many patients allocated to the 5-day regimen experi-
enced serious antibiotic-related complications.
Discussion Our overall primary event rate is higher than previously
The PARITY randomized clinical trial failed to demonstrate a ben- published studies in the field.5,17 In a meta-analysis5 of retro-
efit of a 5-day prophylactic antibiotic regimen of intravenous spective data, the surgical site infection rate after lower ex-
jamaoncology.com (Reprinted) JAMA Oncology March 2022 Volume 8, Number 3 349
Downloaded From: https://jamanetwork.com/ on 03/08/2023
Research Original Investigation Prophylactic Antibiotic Regimens After Endoprosthetic Reconstruction for Lower Extremity Bone Tumors
associated diarrhea, not infrequently caused by C difficile. Al-
Figure 2. Kaplan-Meier Estimates of the Duration of Primary
Outcome-Free Survival at the Time of Final Assessment
though antibiotic-associated diarrhea is generally mild and self-
limiting, gut infection with C difficile is universally severe and
1.0 may lead to toxic megacolon, organ failure, or even death.27
5-d Regimen Our study found a significant increase in antibiotic-related com-
0.8
1-d Regimen plications in the 5-day regimen group, with most complica-
Proportion free of SSI
tions reported to be C difficile–associated colitis. To avoid this
0.6 complication, hospital antibiotic stewardship programs in the
UK have restricted the use of high-risk antibiotics, including
0.4 cephalosporins, with a subsequent clear reduction of nosoco-
mial C difficile infections.28-30
0.2
P = .73
Strengths and Limitations
0
0 3 6 9 12 Our trial has several strengths. Safeguards against potential
Time, mo bias included concealed randomization and blinding of
No. at risk
treatment allocation from patients, caregivers, outcomes
5-d Regimen 293 241 226 220 195
1-d Regimen 311 261 240 231 217 assessors, and data analysts. The diagnosis of surgical site
infection was independently adjudicated using well-
SSI indicates surgical site infection. established definitions, thus ensuring objective decision-
making and minimizing outcome assessment bias. By docu-
tremity endoprosthetic reconstruction was 10% (95% CI, 8%- menting our interpretations based on blinded results before
11%). This meta-analysis5 suggested that antibiotic prophylaxis breaking the randomization code, we safeguarded against
for longer than 24 hours postoperatively decreases the risk of interpretation bias.31 After accounting for the nearly 10%
infection, but the biases of observational research leave only mortality rate, true loss to follow-up was only 5%. Close
low-quality evidence. Our event rate may be higher than pre- clinical surveillance and rigorous study monitoring proce-
viously reported because of our broader definition of a surgi- dures resulted in this relatively small loss to follow-up. Our
cal site infection and the careful prospective collection of study study’s broad eligibility criteria and conduct in many health care
event data. systems strengthens its generalizability. Several of the study
Perioperative antibiotic prophylaxis is considered essen- outcomes are of unequivocal importance to both patients and
tial in minimizing surgical site infections in total joint arthro- health care systems. Finally, answering clinical questions in rare
plasty, in which the infection rate is much lower. 18-22 A conditions requires an immense international, collaborative
meta-analysis23 of randomized clinical trials that compared effort. To our knowledge, this trial was the first-ever collab-
only preoperative antibiotics with both preoperative and post- orative, interventional trial initiated and led by orthopedic
operative antibiotics in joint replacement surgery did not show oncologists.
efficacy of postoperative antibiotic prophylaxis. Because there Our trial also has limitations. The large number of partici-
is no evidence of additional benefit to a lengthened course, the pating clinical sites, combined with the rarity of bone tu-
Surgical Infection Prevention Project recommends the discon- mors, resulted in low enrollment at some sites. More patients
tinuation of use of prophylactic antibiotics 24 hours postop- in the shorter duration group received preoperative chemo-
eratively for all surgical cases.24 However, lower limb onco- therapy, which may have increased their risk of a surgical site
logic reconstructions are unique in their complexity and the infection. However, our subgroup and adjusted analyses
immunocompromised state of the affected patient popula- yielded results similar to our primary analysis. Protocol de-
tion; therefore, these recommendations may not be ap- viations, particularly doses not administered because of early
plicable in this particular setting. The second International hospital discharge, were not uncommon. Although the de-
Consensus Meeting on Musculoskeletal Infection recently iden- viations were balanced between groups, they would have
tified whether prolonging use of postoperative antibiotics affected the 5-day regimen group more than the 1-day regi-
would prevent surgical site infections in patients with bone tu- men. However, the discontinuation of antibiotics at hospital
mors undergoing endoprosthetic reconstruction as 1 of the discharge is standard procedure; thus, our results are appli-
most critical orthopedic oncology clinical questions.25 Their cable to actual clinical practice. The impact of the postopera-
recommendation acknowledged that although more than half tive prophylactic antibiotic regimens on late infections that pre-
of orthopedic oncologists prescribe prophylactic antibiotics for sent after the 1-year postsurgery timepoint cannot be inferred
longer than 24 hours postoperatively, there is insufficient from this study; however, these infections are not considered
evidence to support this practice.25 surgical site infections according to the definitions estab-
The overuse of antibiotics is a major public health con- lished by the Centers for Disease Control and Prevention. The
cern associated with increased health care costs from anti- diagnosis of a surgical site infection is challenging because
biotic-related complications and antibiotic resistance.26 The of the complexities of surgery and wound healing, a concern
increase in antibiotic-resistant organisms, particularly in a ameliorated by the rigor and blinding of the adjudication
nosocomial setting, is outpacing the development of new an- process. Finally, the lack of a statistically significant differ-
timicrobial agents. Antibiotic use often results in antibiotic- ence observed may be the result of insufficient study power.
350 JAMA Oncology March 2022 Volume 8, Number 3 (Reprinted) jamaoncology.com
Downloaded From: https://jamanetwork.com/ on 03/08/2023
Prophylactic Antibiotic Regimens After Endoprosthetic Reconstruction for Lower Extremity Bone Tumors Original Investigation Research
Table 2. Study Outcomes by Treatment Group (Primary and Secondary)
5-d Regimen 1-d Regimen
Study end point (n = 293) (n = 311) HR (95% CI) P value
Primary outcome
Any surgical site infection 44 (15.0) 52 (16.7) 0.93 (0.62-1.40) .73
Superficial incisional 13 (4.4) 12 (3.9) NR NR
Deep incisional 3 (1.0) 8 (2.6) NR NR
Organ or space 28 (9.6) 34 (10.9) 0.97 (0.59-1.62) .92
Secondary outcomes
Any antibiotic-related 15 (5.1) 5 (1.6) 3.24 (1.17-8.98) .02
complications
Clostridioides 11 (3.8) 4 (1.3) NR NR
difficile–associated colitis
Opportunistic fungal infection 0 1 (0.3) NR NR
Oral candidiasis 1 (0.3) 0 NR NR
Diarrhea (unrelated to C 3 (1.0) 0 NR NR
difficile) that required
intervention
Any unplanned additional 75 (25.6) 80 (25.7) 1.06 (0.77-1.46) .72
operation
Any oncologic events 85 (29.0) 89 (28.6) 1.02 (0.75-1.39) .90
Local recurrence 15 (5.1) 22 (7.1) 0.78 (0.40-1.51) .46
Distant metastases 69 (23.5) 79 (25.4) 0.90 (0.65-1.25) .53 Abbreviations: HR, hazard ratio;
Other oncologic event 7 (2.4) 8 (2.6) NR NR NR, not reported (these study end
points did not meet the threshold set
All-cause mortality 37 (12.6) 40 (12.9) 1.01 (0.64-1.58) .98
in the Statistical Analysis Plan for the
Death from disease 29 (9.9) 29 (9.3) 1.08 (0.64-1.81) .78 minimum number of events required
progression to conduct a statistical comparison).
Figure 3. Forest Plot for Subgroup Analyses
5-d 1-d Favors 5-d Favors 1-d Interaction
Subgroup Regimen Regimen HR (95% CI) regimen regimen P value
Tumor type
Bone tumor 38/237 43/249 1.02 (0.65-1.61)
Soft tissue sarcoma 5/28 7/34 0.49 (0.14-1.66) .54
Oligometastatic bone disease 1/28 2/28 0.73 (0.06-8.27)
Tumor location
Tibia 11/53 10/55 1.18 (0.50-2.80)
.56
Femur 33/240 42/256 0.88 (0.56-1.40)
Sex
Male 25/178 32/183 0.75 (0.44-1.29)
.17
Female 19/115 20/128 1.38 (0.72-2.66)
Age, y
<31 19/118 23/138 1.11 (0.59-2.09)
.48
≥31 25/175 29/173 0.82 (0.47-1.41)
Preoperative chemotherapy
No 28/164 22/150 1.18 (0.67-2.10)
.23
Yes 16/129 30/161 0.70 (0.37-1.32)
0.01 0.1 1 10
HR (95% CI)
HR indicates hazard ratio.
However, the observed absolute difference between the 2 treat- regimen. Although the results of this randomized clinical trial
ment groups was small, and the increased sample size needed do not definitively exclude an important benefit of post-
to show statistical significance would likely not be consid- operative prophylactic antibiotic therapy longer than 24
ered necessary by surgeons in the field. hours, the significantly higher risk of antibiotic-related com-
plications in the 5-day regimen represents a critical finding.
Clinicians should consider the uncertainty of the benefits and
the relative confidence in findings of harm to make an in-
Conclusions formed decision on antibiotic duration after surgical resec-
In this randomized clinical trial, the 5-day regimen did not re- tion and endoprosthetic reconstruction for lower extremity
duce the rate of surgical site infection compared with the 1-day bone tumors.
jamaoncology.com (Reprinted) JAMA Oncology March 2022 Volume 8, Number 3 351
Downloaded From: https://jamanetwork.com/ on 03/08/2023
Research Original Investigation Prophylactic Antibiotic Regimens After Endoprosthetic Reconstruction for Lower Extremity Bone Tumors
ARTICLE INFORMATION Khan, Sampath Kumar, McKay, Miller, van de Sande, Additional Information: The PARITY Steering
Accepted for Publication: October 7, 2021. Zumárraga, Bhandari. Committee designed the trial and prespecified the
Drafting of the manuscript: Ghert, Schneider. statistical analysis plan. The members of the
Published Online: January 6, 2022. Critical revision of the manuscript for important PARITY Steering Committee vouch for the
doi:10.1001/jamaoncol.2021.6628 intellectual content: Ghert, Guyatt, Thabane, Vélez, completeness and accuracy of the data and
Open Access: This is an open access article O’Shea, Randall, Turcotte, Wilson, Wunder, analyses reported and for the fidelity of the trial to
distributed under the terms of the CC-BY License. Baptista, Cheng, Doung, Ferguson, Giglio, Hayden, the protocol. The Methods Center at McMaster
© 2022 The Prophylactic Antibiotic Regimens in Heels-Ansdell, Khan, Sampath Kumar, McKay, University in Hamilton, Ontario, Canada, was
Tumor Surgery (PARITY) Investigators. JAMA Miller, van de Sande, Zumárraga, Bhandari. responsible for the trial randomization system, the
Oncology. Statistical analysis: Thabane, Heels-Ansdell. maintenance, validation, and analysis of the data
The Writing Committee for the PARITY Obtained funding: Ghert, Schneider, McKay, and the coordination of all clinical sites. The Central
Investigators: Michelle Ghert, MD; Patricia Bhandari. Adjudication Committee adjudicated all suspected
Schneider, BSc; Gordon Guyatt, MD, MSc; Lehana Administrative, technical, or material support: primary outcome events, as well as key secondary
Thabane, PhD; Roberto Vélez, MD, PhD; Timothy Schneider, Vélez, O’Shea, Randall, Turcotte, Wilson, outcome events and eligibility when in doubt.
O’Shea, MD, MPH; R. Lor Randall, MD; Robert Giglio, McKay, Zumárraga, Bhandari.
Turcotte, MD; David Wilson, MD, MASc; Jay S. Supervision: Ghert, Schneider, Guyatt, Thabane, REFERENCES
Wunder, MD; André Mathias Baptista, MD, PhD; Vélez, McKay, Bhandari. 1. Jeys L, Grimer R. The long-term risks of infection
Edward Y. Cheng, MD; Yee-Cheen Doung, MD; Conflict of Interest Disclosures: Dr Ghert reported and amputation with limb salvage surgery using
Peter C. Ferguson, MD; Victoria Giglio, MSc; James receiving grants from Canadian Institutes of Health endoprostheses. In: Tunn PU, ed. Treatment of
Hayden, MD, PhD; Diane Heels-Ansdell, MSc; Shah Research, Canadian Cancer Society Research Bone and Soft Tissue Sarcomas: Recent Results in
Alam Khan, MS (Ortho); Venkatesan Sampath Institute, Orthopaedic Research and Education Cancer Research. Springer; 2009:75-84. doi:10.
Kumar, MS (Ortho); Paula McKay, BSc; Foundation, Physician Services Incorporated, and 1007/978-3-540-77960-5_7
Benjamin Miller, MD, MS; Musculoskeletal Tumor Society during the conduct 2. Morii T, Yabe H, Morioka H, et al. Postoperative
Michiel van de Sande, MD, PhD; of the study and consulting and speaker fees from deep infection in tumor endoprosthesis
Juan P. Zumárraga, MD, PhD; Wright Medical outside the submitted work. reconstruction around the knee. J Orthop Sci. 2010;
Mohit Bhandari, MD, PhD. Dr O’Shea reported receiving grants from the 15(3):331-339. doi:10.1007/s00776-010-1467-z
Affiliations of The Writing Committee for the Canadian Cancer Society, Canadian Institutes of
Health Research, and Physicians Services Inc during 3. Jeys LM, Grimer RJ, Carter SR, Tillman RM. Risk
PARITY Investigators: Division of Orthopaedic of amputation following limb salvage surgery with
Surgery, Department of Surgery, McMaster the conduct of the study. Dr Cheng reported
serving as editor for the Journal of Bone and Joint endoprosthetic replacement, in a consecutive
University, Hamilton, Ontario, Canada (Ghert, series of 1261 patients. Int Orthop. 2003;27(3):
Schneider, Wilson, Giglio, McKay, Bhandari); Surgery Essential Surgical Techniques. Ms McKay
reported receiving personal fees from Global 160-163. doi:10.1007/s00264-003-0429-x
Department of Medicine, McMaster University,
Hamilton, Ontario, Canada (Guyatt, O’Shea); Research Solutions Inc and Platform Life Sciences 4. Akahane T, Shimizu T, Isobe K, Yoshimura Y,
Department of Health Research Methods, Evidence outside the submitted work. Dr Miller reported Fujioka F, Kato H. Evaluation of postoperative
and Impact, McMaster University, Hamilton, receiving grants from Canadian Institutes of Health general quality of life for patients with
Ontario, Canada (Guyatt, Thabane, Heels-Ansdell, Research during the conduct of the study. osteosarcoma around the knee joint. J Pediatr
Bhandari); Hospital Vall d’Hebron, Vall d’Hebron Dr Bhandari reported receiving grants from Orthop B. 2007;16(4):269-272. doi:10.1097/
Institut de Recerca, Barcelona, Spain (Vélez); Canadian Institutes of Health Research, National BPB.0b013e3280925670
Department of Orthopaedic Surgery, University of Institutes of Health, Michael G. DeGroote Institute 5. Racano A, Pazionis T, Farrokhyar F, Deheshi B,
California Davis Health, Sacramento (Randall); for Pain Research and Care, and Physicians’ Services Ghert M. High infection rate outcomes in long-bone
Division of Orthopaedic Surgery, Department of Inc Foundation, personal fees from Pendopharm, tumor surgery with endoprosthetic reconstruction
Surgery, McGill University, Montreal, Quebec, Bioventus, and Acumed, and nonfinancial support in adults: a systematic review. Clin Orthop Relat Res.
Canada (Turcotte); University of Toronto from Canadian Orthopaedic Association and Mayo 2013;471(6):2017-2027. doi:10.1007/
Musculoskeletal Oncology Unit, Mount Sinai Clinic Core Center for Clinical Research outside the s11999-013-2842-9
Hospital, Division of Orthopaedic Surgery, submitted work. No other disclosures were
reported. 6. Hasan K, Racano A, Deheshi B, et al.
Department of Surgery, University of Toronto, Prophylactic Antibiotic Regimens in Tumor Surgery
Toronto, Ontario, Canada (Wunder, Ferguson); Funding/Support: This research was supported by (PARITY) survey. BMC Musculoskelet Disord. 2012;
Instituto de Ortopedia e Traumatologia do Hospital operating grant 137104 from the Canadian 13:91. doi:10.1186/1471-2474-13-91
das Clínicas da Universidade de São Paulo, São Institutes of Health Research, innovation grant
Paulo, Brazil (Baptista, Zumárraga); Department of 701639 and innovation to impact grant 703398 7. Bratzler DW, Dellinger EP, Olsen KM, et al;
Orthopaedic Surgery, University of Minnesota, from the Canadian Cancer Society Research American Society of Health-System Pharmacists;
Minneapolis (Cheng); Department of Orthopaedics Institute, the Canadian Orthopaedic Foundation Infectious Disease Society of America; Surgical
and Rehabilitation, Oregon Health & Science 2018 J. Édouard Samson Award, the Orthopaedic Infection Society; Society for Healthcare
University, Portland (Doung, Hayden); Department Research and Education Foundation in conjunction Epidemiology of America. Clinical practice
of Orthopaedics, All India Institute of Medical with the Musculoskeletal Tumor Society (Clinical guidelines for antimicrobial prophylaxis in surgery.
Sciences, Delhi, India (Khan, Sampath Kumar); Research Grant in Orthopaedic Oncology 2011), and Am J Health Syst Pharm. 2013;70(3):195-283.
Department of Orthopaedics and Rehabilitation, the Physicians’ Services Incorporated (Clinical doi:10.2146/ajhp120568
University of Iowa, Iowa City (Miller); Department Research Grant 2012). This study was also funded, 8. Parvizi J, Gehrke T, Chen AF. Proceedings of the
of Orthopaedic Surgery, Leids Universitair Medisch in part, by generous donations from the International Consensus on Periprosthetic Joint
Centrum, Leiden, the Netherlands (van de Sande). Silverhearts Association and private donors. Infection. Bone Joint J. 2013;95-B(11):1450-1452.
Author Contributions: Dr Ghert had full access to Role of the Funder/Sponsor: The funding doi:10.1302/0301-620X.95B11.33135
all the data in the study and takes responsibility for organizations had no role in the design and conduct 9. Costelloe C, Metcalfe C, Lovering A, Mant D, Hay
the integrity of the data and the accuracy of the of the study; collection, management, analysis, and AD. Effect of antibiotic prescribing in primary care
data analysis. interpretation of the data; preparation, review, or on antimicrobial resistance in individual patients:
Concept and design: Ghert, Guyatt, Thabane, Vélez, approval of the manuscript; and decision to submit systematic review and meta-analysis. BMJ. 2010;
O’Shea, Randall, Turcotte, Wunder, Ferguson, the manuscript for publication. 340:c2096. doi:10.1136/bmj.c2096
McKay, Bhandari. Group Information: The PARITY Investigators are 10. Ghert M, Deheshi B, Holt G, et al; PARITY
Acquisition, analysis, or interpretation of data: listed in Supplement 3. Investigators. Prophylactic Antibiotic Regimens in
Ghert, Schneider, Guyatt, Thabane, Vélez, O’Shea, Tumour Surgery (PARITY): protocol for a
Randall, Turcotte, Wilson, Wunder, Baptista, Cheng, Data Sharing Statement: See Supplement 4.
multicentre randomised controlled study. BMJ Open.
Doung, Ferguson, Giglio, Hayden, Heels-Ansdell,
352 JAMA Oncology March 2022 Volume 8, Number 3 (Reprinted) jamaoncology.com
Downloaded From: https://jamanetwork.com/ on 03/08/2023
Prophylactic Antibiotic Regimens After Endoprosthetic Reconstruction for Lower Extremity Bone Tumors Original Investigation Research
2012;2(6):e002197. doi:10.1136/ malignant bone tumor surgery of the extremities. of post-operative infection, including surgical site
bmjopen-2012-002197 Anticancer Res. 2020;40(6):3551-3557. doi:10. infection. Surg Infect (Larchmt). 2011;12(3):163-168.
11. Horan TC, Gaynes RP, Martone WJ, Jarvis WR, 21873/anticanres.14344 doi:10.1089/sur.2010.083
Emori TG. CDC definitions of nosocomial surgical 18. Illingworth KD, Mihalko WM, Parvizi J, et al. 25. Strony J, Brown S, Choong P, Ghert M, Jeys L,
site infections, 1992: a modification of CDC How to minimize infection and thereby maximize O’Donnell RJ. Musculoskeletal infection in
definitions of surgical wound infections. Infect patient outcomes in total joint arthroplasty: orthopaedic oncology: assessment of the 2018
Control Hosp Epidemiol. 1992;13(10):606-608. a multicenter approach: AAOS exhibit selection. International Consensus Meeting on
doi:10.2307/30148464 J Bone Joint Surg Am. 2013;95(8):e50. doi:10.2106/ Musculoskeletal Infection. J Bone Joint Surg Am.
12. Tunn PU, Pomraenke D, Goerling U, JBJS.L.00596 2019;101(20):e107. doi:10.2106/JBJS.19.00182
Hohenberger P. Functional outcome after 19. Voigt J, Mosier M, Darouiche R. Systematic 26. Infectious Diseases Society of America (IDSA).
endoprosthetic limb-salvage therapy of primary review and meta-analysis of randomized controlled Combating antimicrobial resistance: policy
bone tumours: a comparative analysis using the trials of antibiotics and antiseptics for preventing recommendations to save lives. Clin Infect Dis.
MSTS score, the TESS and the RNL index. Int Orthop. infection in people receiving primary total hip and 2011;52(suppl 5):S397-S428. doi:10.1093/cid/cir153
2008;32(5):619-625. doi:10.1007/ knee prostheses. Antimicrob Agents Chemother. 27. Mullish BH, Williams HR. Clostridium difficile
s00264-007-0388-8 2015;59(11):6696-6707. doi:10.1128/AAC.01331-15 infection and antibiotic-associated diarrhoea. Clin
13. Davis AM, Wright JG, Williams JI, Bombardier C, 20. AAOS. Information statement: Med (Lond). 2018;18(3):237-241. doi:10.7861/
Griffin A, Bell RS. Development of a measure of recommendations for the use of intravenous clinmedicine.18-3-237
physical function for patients with bone and soft antibiotic prophylaxis in primary total joint 28. Aldeyab MA, Kearney MP, Scott MG, et al. An
tissue sarcoma. Qual Life Res. 1996;5(5):508-516. arthroplasty. Accessed June 4, 2021. https://www. evaluation of the impact of antibiotic stewardship
doi:10.1007/BF00540024 aaos.org/globalassets/about/bylaws-library/ on reducing the use of high-risk antibiotics and its
14. Schreiber D, Bell RS, Wunder JS, et al. information-statements/1027-recommendations- effect on the incidence of Clostridium difficile
Evaluating function and health related quality of life for-the-use-of-intravenous-antibiotic-prophylaxis- infection in hospital settings. J Antimicrob Chemother.
in patients treated for extremity soft tissue in-primary-total-joint-arthroplasy.pdf 2012;67(12):2988-2996. doi:10.1093/jac/dks330
sarcoma. Qual Life Res. 2006;15(9):1439-1446. 21. British Orthopaedic Association. Primary total 29. Talpaert MJ, Gopal Rao G, Cooper BS, Wade P.
doi:10.1007/s11136-006-0001-4 hip replacement: a guide to good practice. Impact of guidelines and enhanced antibiotic
15. Schneider P, Heels-Ansdell D, Thabane L, Ghert Accessed June 4, 2021. https://britishhipsociety. stewardship on reducing broad-spectrum antibiotic
M; PARITY Investigators. Prophylactic Antibiotic com/wp-content/uploads/2020/12/2012-Nov_ usage and its effect on incidence of Clostridium
Regimens In Tumor Surgery (PARITY): BOA-Blue-Book.pdf difficile infection. J Antimicrob Chemother. 2011;66
a multi-center randomized controlled study 22. New Zealand Orthopaedic Association. Total (9):2168-2174. doi:10.1093/jac/dkr253
comparing alternative antibiotic regimens in hip joint arthroplasty good practice guidelines. 30. Al-Obaydi W, Smith CD, Foguet P. Changing
patients undergoing tumor resections with Accessed June 4, 2021. https://nzoa.org.nz/sites/ prophylactic antibiotic protocol for reducing
endoprosthetic replacements-a statistical analysis default/files/Total_Hip_Joint_Arthroplasty_ Clostridium difficile-associated diarrhoeal
plan. Trials. 2021;22(1):223. doi:10.1186/ Guidelines_0.pdf infections. J Orthop Surg (Hong Kong). 2010;18(3):
s13063-021-05147-2 23. Thornley P, Evaniew N, Riediger M, Winemaker 320-323. doi:10.1177/230949901001800312
16. PARITY Investigators. Prophylactic Antibiotic M, Bhandari M, Ghert M. Postoperative antibiotic 31. Järvinen TLN, Sihvonen R, Bhandari M, et al.
Regimens in Tumour Surgery (PARITY): a pilot prophylaxis in total hip and knee arthroplasty: Blinded interpretation of study results can feasibly
multicentre randomised controlled trial. Bone Joint a systematic review and meta-analysis of and effectively diminish interpretation bias. J Clin
Res. 2015;4(9):154-162. doi:10.1302/ randomized controlled trials. CMAJ Open. 2015;3 Epidemiol. 2014;67(7):769-772. doi:10.1016/
2046-3758.49.2000482 (3):E338-E343. doi:10.9778/cmajo.20150012 j.jclinepi.2013.11.011
17. Langit MB, Miwa S, Yamamoto N, et al. Risk 24. Rosenberger LH, Politano AD, Sawyer RG. The
factors for postoperative deep infection after surgical care improvement project and prevention
jamaoncology.com (Reprinted) JAMA Oncology March 2022 Volume 8, Number 3 353
Downloaded From: https://jamanetwork.com/ on 03/08/2023
You might also like
- International Journal of Surgery: V. Gomathi Shankar, K. Srinivasan, Sarath C. Sistla, S. JagdishDocument4 pagesInternational Journal of Surgery: V. Gomathi Shankar, K. Srinivasan, Sarath C. Sistla, S. JagdishUswatun HasanahNo ratings yet
- AB Untuk FrakturDocument15 pagesAB Untuk FrakturRifda LatifaNo ratings yet
- Implantes en InmunosuprimidosDocument8 pagesImplantes en InmunosuprimidosLeandro PeraltaNo ratings yet
- Untitled 3Document10 pagesUntitled 3Satya AsatyaNo ratings yet
- Surgical Treatment of Peri-Implantitis: 3 - Year Results From A Randomized Controlled Clinical TrialDocument10 pagesSurgical Treatment of Peri-Implantitis: 3 - Year Results From A Randomized Controlled Clinical TrialFabian SanabriaNo ratings yet
- Dental Implant Procedures in Immunosuppressed Organ Transplant Patients: A Systematic ReviewDocument8 pagesDental Implant Procedures in Immunosuppressed Organ Transplant Patients: A Systematic ReviewjeeveshNo ratings yet
- Effectiveness of Glucocorticoids in Orthognathic Surgery - An Overview of Systematic ReviewsDocument15 pagesEffectiveness of Glucocorticoids in Orthognathic Surgery - An Overview of Systematic ReviewsBruno GuardieiroNo ratings yet
- Steinberg 2009Document7 pagesSteinberg 2009majedNo ratings yet
- An Enhanced Recovery After Surgery Protocol For FaDocument8 pagesAn Enhanced Recovery After Surgery Protocol For Faandrew250519No ratings yet
- First Page PDFDocument1 pageFirst Page PDFmpaivaecostaNo ratings yet
- Enhanced Recovery After Surgery For Cesarean Delivery Decreases Length of Hospital Stay and Opioid Consumption: A Quality Improvement InitiativeDocument9 pagesEnhanced Recovery After Surgery For Cesarean Delivery Decreases Length of Hospital Stay and Opioid Consumption: A Quality Improvement Initiativedina istianaNo ratings yet
- Surgery Paper 2Document15 pagesSurgery Paper 2Jonathan Billy ChristianNo ratings yet
- Effectiveness of Antibiotics On Post-Operative Com PDFDocument5 pagesEffectiveness of Antibiotics On Post-Operative Com PDFReshmaa RajendranNo ratings yet
- Burden of Adhesions in Abdominal and Pelvic SurgeryDocument15 pagesBurden of Adhesions in Abdominal and Pelvic SurgeryDian AdiNo ratings yet
- Clinical Study: Silver-Coated Hip Megaprosthesis in Oncological Limb Savage SurgeryDocument7 pagesClinical Study: Silver-Coated Hip Megaprosthesis in Oncological Limb Savage SurgeryEzhil AjithNo ratings yet
- Surgical Site InfectionDocument7 pagesSurgical Site InfectionCaxton ThumbiNo ratings yet
- Surgical Site Infection PreventionDocument9 pagesSurgical Site Infection PreventionRachmat HasanNo ratings yet
- Delmarmariscal Cazalla2020Document9 pagesDelmarmariscal Cazalla2020Andi Muhammad Imam RNo ratings yet
- Gentamicin-Collagen Sponge For Infection Prophylaxis in Colorectal SurgeryDocument12 pagesGentamicin-Collagen Sponge For Infection Prophylaxis in Colorectal SurgeryNurul ImaniarNo ratings yet
- Does An Antimicrobial Incision Drape Prevent.15Document9 pagesDoes An Antimicrobial Incision Drape Prevent.15Jimenez-Espinosa JeffersonNo ratings yet
- FS 162385Document4 pagesFS 162385Talha ZubairNo ratings yet
- Contemporary Management of Advanced Laryngeal CancDocument3 pagesContemporary Management of Advanced Laryngeal Cancandre halimNo ratings yet
- Oamjms 10b 1148Document5 pagesOamjms 10b 1148hanifNo ratings yet
- Antibiotic Prophylaxis For Traumatic Facial FracturesDocument10 pagesAntibiotic Prophylaxis For Traumatic Facial FracturesMaria Camila Castiblanco MolinaNo ratings yet
- 6037ASTR Astr 97 103Document9 pages6037ASTR Astr 97 103LuisNavarroHernandezNo ratings yet
- 46 Vol. 5 Issue 6 June 2014 IJPSR RA 3573 Paper 46Document6 pages46 Vol. 5 Issue 6 June 2014 IJPSR RA 3573 Paper 46Dr Meenakshi ParwaniNo ratings yet
- DAIRDocument12 pagesDAIRCris JiménezNo ratings yet
- Heigh2019 PDFDocument9 pagesHeigh2019 PDFVALENNo ratings yet
- English PB 23Document7 pagesEnglish PB 23shah hassaanNo ratings yet
- Green-Tsui2013 Article ImpactOfAnesthesiaForCancerSurDocument22 pagesGreen-Tsui2013 Article ImpactOfAnesthesiaForCancerSurNataNo ratings yet
- Post-Operative Wound Complications Following Emergency and Elective Abdominal SurgeriesDocument6 pagesPost-Operative Wound Complications Following Emergency and Elective Abdominal SurgeriesNurul Aini DamayantiNo ratings yet
- 12 BaruDocument8 pages12 BaruAnditha Namira RSNo ratings yet
- Preoperative Antibiotic Prophylaxis - StatPearls - NCBI BookshelfDocument7 pagesPreoperative Antibiotic Prophylaxis - StatPearls - NCBI BookshelfMikaela l100% (1)
- 2.effect of Perioperative Oral Management On The PreDocument5 pages2.effect of Perioperative Oral Management On The PreJambul Wak Wak WakNo ratings yet
- Short and Long-Term Outcomes After Surgical Procedures Lasting For More Than Six HoursDocument8 pagesShort and Long-Term Outcomes After Surgical Procedures Lasting For More Than Six HoursDickyNo ratings yet
- Comparing Erector Spinae Plane Block With Serratus Anterio - 2020 - British JourDocument9 pagesComparing Erector Spinae Plane Block With Serratus Anterio - 2020 - British JourtasyadelizaNo ratings yet
- Wormald 2019Document18 pagesWormald 2019araliNo ratings yet
- Antibiotic Prophylaxis in The Surgical ManagementDocument7 pagesAntibiotic Prophylaxis in The Surgical ManagementRAHUL SHINDENo ratings yet
- PterigiumDocument6 pagesPterigiumNdha SolidarityNo ratings yet
- Khan2014 PDFDocument4 pagesKhan2014 PDFtikaNo ratings yet
- Implantes en Pacientes Con RadioterapiaDocument7 pagesImplantes en Pacientes Con RadioterapiaLidise Hernandez AlonsoNo ratings yet
- Journal Homepage: - : IntroductionDocument10 pagesJournal Homepage: - : IntroductionIJAR JOURNALNo ratings yet
- Infection Following Bone Tumor Resection and Reconstruction With Tumoral Prostheses: A Literature Review F. CDocument9 pagesInfection Following Bone Tumor Resection and Reconstruction With Tumoral Prostheses: A Literature Review F. CWilson MartinezNo ratings yet
- Evidence-Based Strategies To Reduce Postoperative Complications in Plastic SurgeryDocument10 pagesEvidence-Based Strategies To Reduce Postoperative Complications in Plastic SurgeryAmanda HodelNo ratings yet
- Comparative Evaluation of Adjunctive Antibiotics Given Post Periodontal Flap SurgeryDocument7 pagesComparative Evaluation of Adjunctive Antibiotics Given Post Periodontal Flap SurgeryReshmaa RajendranNo ratings yet
- Knowledge of Chemotherapy and Occupational Safety Measures Among Nurses in Oncology UnitsDocument7 pagesKnowledge of Chemotherapy and Occupational Safety Measures Among Nurses in Oncology UnitsIOM BNSNo ratings yet
- Gynecology, 2020Document7 pagesGynecology, 2020Prameita Rahmawati MITNo ratings yet
- Japid 14 26Document6 pagesJapid 14 26rikaNo ratings yet
- Journal of Periodontology - 2022 - Monje - Significance of Barrier Membrane On The Reconstructive Therapy ofDocument13 pagesJournal of Periodontology - 2022 - Monje - Significance of Barrier Membrane On The Reconstructive Therapy of安西 泰規No ratings yet
- Malignant Bone Tumors - Sparing Vs AmpDocument13 pagesMalignant Bone Tumors - Sparing Vs AmpAnonymous wJTlxhINo ratings yet
- Prophylactic Antibiotics in Hip and Knee ArthroplastyDocument11 pagesProphylactic Antibiotics in Hip and Knee ArthroplastySara Aly YoussefNo ratings yet
- Bristow 2007Document11 pagesBristow 2007Diederick de JongNo ratings yet
- Paper 7 BellowsDocument10 pagesPaper 7 Bellowsmohmed addallaNo ratings yet
- Oral Oncology: Mark K. Wax, James AzziDocument4 pagesOral Oncology: Mark K. Wax, James Azzicr89omfNo ratings yet
- Froum-Rosen-Froum TX PDFDocument11 pagesFroum-Rosen-Froum TX PDFMark BisharaNo ratings yet
- Surgery: SciencedirectDocument5 pagesSurgery: Sciencedirectpolomska.kmNo ratings yet
- Wang 2021Document19 pagesWang 2021cikox21848No ratings yet
- Antibiotic Prophylaxis - Is It Necessary in Clean General Surgery?Document3 pagesAntibiotic Prophylaxis - Is It Necessary in Clean General Surgery?Jade Phoebe AjeroNo ratings yet
- Management of Peritoneal Metastases- Cytoreductive Surgery, HIPEC and BeyondFrom EverandManagement of Peritoneal Metastases- Cytoreductive Surgery, HIPEC and BeyondAditi BhattNo ratings yet
- Case Studies of Postoperative Complications after Digestive SurgeryFrom EverandCase Studies of Postoperative Complications after Digestive SurgeryNo ratings yet
- Technical Documentation IPM: Savina 300 Intensive Care VentilatorDocument166 pagesTechnical Documentation IPM: Savina 300 Intensive Care VentilatorhoudaNo ratings yet
- 150.66-RP4 YcalDocument92 pages150.66-RP4 YcalJosé RamosNo ratings yet
- JECFA Carrageenan MonographDocument5 pagesJECFA Carrageenan MonographSurya SaputraNo ratings yet
- ASTM C309: Do Liquid Hardeners Meet This Standard?Document2 pagesASTM C309: Do Liquid Hardeners Meet This Standard?Kishore Nayak kNo ratings yet
- Magat, Jescel-Anne Janea D. MED-2B A B C BDocument3 pagesMagat, Jescel-Anne Janea D. MED-2B A B C BJescel-Anne Janea MagatNo ratings yet
- Unit of PowerDocument9 pagesUnit of PowerSarathrv RvNo ratings yet
- iSF EClassRecord - NewNormal AdviserDocument254 pagesiSF EClassRecord - NewNormal AdviserYanara Delarama DayapNo ratings yet
- Quality Control Argex 0032/32.50.15.08 4/10 MM EN 13055: EN 15732 NL BSB K73820/01 (1/01/2004)Document1 pageQuality Control Argex 0032/32.50.15.08 4/10 MM EN 13055: EN 15732 NL BSB K73820/01 (1/01/2004)joe briffaNo ratings yet
- SECTION 03310-1 Portland Cement Rev 1Document10 pagesSECTION 03310-1 Portland Cement Rev 1Abdalrahman AntariNo ratings yet
- Formulating A Dental Treatment Plan: DR Tashnim BagusDocument33 pagesFormulating A Dental Treatment Plan: DR Tashnim BagustarekrabiNo ratings yet
- Birthday QuotesDocument24 pagesBirthday QuotesArniel CatubigNo ratings yet
- Escape From The Western Diet Summary RevisedDocument3 pagesEscape From The Western Diet Summary Revisedapi-385530863100% (1)
- Application of Statistical MethodsDocument5 pagesApplication of Statistical Methodsradquinineza0% (1)
- Hydraulic Seat Puller KitDocument2 pagesHydraulic Seat Puller KitPurwanto ritzaNo ratings yet
- Jeremiah's Law, Introduced by Assemblywoman Rodneyse BichotteDocument2 pagesJeremiah's Law, Introduced by Assemblywoman Rodneyse BichotteCity & State NYNo ratings yet
- WPPIL No. 43 of 2014 Uttrakhand High Court Orders For Animals - Abhishek KadyanDocument57 pagesWPPIL No. 43 of 2014 Uttrakhand High Court Orders For Animals - Abhishek KadyanNaresh KadyanNo ratings yet
- 94 175 1 SM PDFDocument8 pages94 175 1 SM PDFikaNo ratings yet
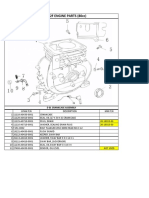
- Lifan 152F Engine Parts (80Cc) : E 01 Crankcase AssemblyDocument13 pagesLifan 152F Engine Parts (80Cc) : E 01 Crankcase AssemblySean MurrayNo ratings yet
- Bronce C90700Document2 pagesBronce C90700Luis Enrique CarranzaNo ratings yet
- Account Transfer Form: Fax Cover SheetDocument6 pagesAccount Transfer Form: Fax Cover SheetJitendra SharmaNo ratings yet
- Business ModelDocument3 pagesBusiness ModelEric AryeepahNo ratings yet
- 6 Ijasrjun20196Document8 pages6 Ijasrjun20196TJPRC PublicationsNo ratings yet
- Access To JusticeDocument9 pagesAccess To JusticeprimeNo ratings yet
- Material Data Sheet Durapro Asa: DescriptionDocument1 pageMaterial Data Sheet Durapro Asa: DescriptionAlexandru NeacsuNo ratings yet
- 2022 EDCS Weekly Surveillance Report No 5Document22 pages2022 EDCS Weekly Surveillance Report No 5Aesthetics MinNo ratings yet
- Chapter 10 Fitness Training PrinciplesDocument80 pagesChapter 10 Fitness Training Principlesapi-115744109No ratings yet
- Pressure Regulator FRSDocument6 pagesPressure Regulator FRSTobiasAngererNo ratings yet
- Static Var CompensatorDocument12 pagesStatic Var CompensatorBengal Gaming100% (1)
- Physical Assessment EquipmentDocument8 pagesPhysical Assessment EquipmentHannah TotohNo ratings yet
- Calinescu2017 PDFDocument38 pagesCalinescu2017 PDFElizabeth UrrutiaNo ratings yet