Professional Documents
Culture Documents
Characteristics and Causes of Diarrhea in Indonesian Children
Uploaded by
DrnOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Characteristics and Causes of Diarrhea in Indonesian Children
Uploaded by
DrnCopyright:
Available Formats
Original Article
Characteristics of Pediatric Patients with Diarrhea in
Indonesia: A Laboratory-based Report
Lia Amanda1, Karin Nadia Utami1, Andria Amanda Pulungan1, Diar Riyanti Rudiatmoko1, Fatima
Safira Alatas2
1
Faculty of Medicine, Universitas Indonesia, Jakarta, Indonesia
2
Department of Child Health, Faculty of Medicine, Universitas Indonesia, Cipto Mangunkusumo Hospital, Jakarta,
Indonesia
Corresponding author:
Fatima Safira Alatas, MD, PhD
Abstract:
safiraalatas@gmail.com
Background: Diarrhea is still a common health problem in Indonesia, with high
morbidity and mortality rate. The severity of diarrhea is associated with age, nutritional
status, and cause of diarrhea. This study aims to describe the characteristics and
laboratory findings, particularly stool analysis, in pediatric patients with diarrhea.
Published: Methods: A retrospective study was conducted using data from patients aged 0 to 18
25 August 2022 with diarrhea who underwent stool analysis in Cipto Mangunkusumo Hospital
between 2012 and 2016.
DOI:
https://doi.org/10.58427/apg Results: The average age of children with diarrhea was 45 months, with most patients
hn.1.2.2022.8-15 (55,6%) being under two years old children. More than half of the patients were boys
(58.8%). Two-thirds of the patients (67%) presented with watery stool diarrhea. The
interpretation of stool analysis indicated that nearly half of the patients (48%)
experienced diarrhea due to bacterial infection, followed by fat malabsorption
(20.8%). Similar results were also seen in the stool analysis of children aged 0-24
Citation:
months, with the prevalence of bacterial infection (35.2%) and fat malabsorption
Amanda L, Utami KN,
Pulungan AA, and Alatas FS. (30.2%) being the most commonly identified etiology of diarrhea.
Characteristics of Pediatric Conclusion: In Indonesia, children under two and male gender were more frequently
Patients with Diarrhea in reported to experience diarrhea. The primary manifestation of pediatric diarrhea was
Indonesia: A laboratory-based
Report. Arch Pediatr Gastr watery stools, while the most common etiology was bacterial infections.
Hepatol Nutr. 2022(2):8-15
Keywords: diarrhea, stool analysis, pediatric patients
Introduction
The high morbidity and mortality rates of diarrhea remain a major concern in
developing countries, including Indonesia. Diarrhea is the recurrent passage of watery
stools that occurs at least three times in 24 hours. The disease is further classified as
acute diarrhea, which occurs for less than seven days; prolonged diarrhea, occurring
for 7-14 days; and persistent diarrhea that last for more than 14 days.1
APGHN | www.agphn.com Vol 1| August 2022 | Page 8
The severity of diarrhea is associated with the age of the patient, nutritional status, and
the underlying cause of diarrhea.1 According to RISKESDAS 2013, infant is the main
age group that suffered from diarrhea. In addition, diarrhea in this particular age group
primarily occurred at the age of 12-23 months (7.6%), majorly in the male gender
(5.5%), and commonly in patients who lived in the countryside (6.2%). 2
A cross-sectional study conducted by Hendrawati et al. reported that more than 25%
of children with diarrhea also suffered from malabsorption syndrome, with the
prevalence of lactose and fat malabsorption were 11% and 51%, respectively.
Furthermore, this study found that 19% of 3480 stool specimens of pediatric patients
show signs of maldigestion. Food allergy may also lead to malabsorption. In addition,
previous study found that the prevalence of cow’s milk allergy in patients with diarrhea
in Indonesia was 3%.3,4
The purpose of this study was to identify the characteristics and laboratory findings
of pediatric patients based on their stool analysis profile treated in Cipto
Mangunkusumo Hospital.
Methods
This research was a retrospective, cross-sectional study conducted in Cipto
Mangunkusumo Hospital, Jakarta, Indonesia. Patients aged 0 to 18 years old who
suffered from diarrhea and underwent stool examination in the Laboratory of
Gastrohepatology Division, Department of Child Health, Cipto Mangunkusumo
Hospital were included in this study. Meanwhile, subjects with incomplete medical
records were excluded. Stool analysis and other supporting data were obtained from
the medical records documented in 2012 – 2016. Other supporting data include age,
gender, history of bacterial infection, fungal infection, food maldigestion,
carbohydrate maldigestion, protein maldigestion, lactose malabsorption, fat
malabsorption, and suspected cow milk allergy.
Bacterial infection was considered positive if the stool leucocyte count was higher than
+2 or 10-20 leucocytes per high magnification field. 3 Meanwhile, the diagnosis of
fungal infection was noted in samples with positive appearance of fungal. Food
maldigestion was indicated by the presence of meat or vegetable fibers in the stool,
while carbohydrate maldigestion was considered positive in the existence of amylum.3,5
The presence of the protein molecule indicated protein maldigestion. 5 Furthermore,
the diagnosis of lactose malabsorption was established in samples with fecal pH less
than 6, or if the fecal reducing substance results read as 0, trace (1/4% glucose), +
(1/2% glucose), ++ (3/4% glucose), +++ (1% glucose), and ++++ (2% glucose).6,7
Fat malabsorption was confirmed if the amount of fat exhibited positive 2 (++) in the
microscopic examination.3 Lastly, cow’s milk allergies were suspected in patients with
APGHN | www.agphn.com Vol 1| August 2022 | Page 9
erythrocyte counts in stool > 5. The data collected were then quantified using SPSS
version 21.
All data, including other personal information provided and gathered, was kept
confidential. This research had received ethical permission no.
964/UN2.F1.D1/KBK/PDP.01/2016.
Result
Subjects Demographics
From 2012 until 2016, stool analysis was performed on 1031 pediatric patients with
diarrhea in Cipto Mangunkusumo Hospital. The age ranged between 0 to 18 years old,
with the average age of 45 months. Most of the patients were children under two years
old (55.6%). Furthermore, more than half of the patients (58.8%) were male.
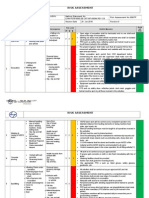
Table 1. Characteristics of study subjects
Characteristics n (%)
Gender
Male 606 (58.8)
Female 423 (41)
Age
<24 months 573 (55.6)
24-59 months 191 (18.5)
>60 months 262 (25.4)
Consistency of the Stool
The stool analysis results demonstrated various stool characteristics such as
consistency, and laboratory findings. Among the 857 patients, 67% of the patients
presented with watery stool diarrhea.
Table 2. Consistency of stool analysis in this study
Consistency n (%)
Normal 155 (15)
Solid 11 (1.1)
Liquid 691 (67)
Laboratory Findings and Interpretation
Various laboratory examinations of the stool samples were performed to determine
the cause of diarrhea. Each etiology presented distinct characteristics, which were
mentioned in the methodology. One patient might have more than one significant
laboratory findings and hence was diagnosed with more than one causes of diarrhea.
APGHN | www.agphn.com Vol 1| August 2022 | Page 10
Most of the samples demonstrated the presence of leucocytes, erythrocytes, and fat.
Positive results with a low number of these components in stool can be considered
normal. However, excessive amounts may indicate various conditions such as bacterial
infection, dysentery, or fat malabsorption.
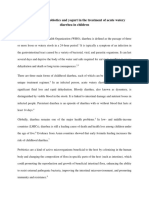
Table 3. Stool analysis profile of the study subjects
Laboratory Findings* n (%)
Mucus 536 (52)
Blood 25 (2.4)
Leucocyte
+1 273 (26.5)
+2 395 (38.3)
+3 198 (19.2)
Erythrocyte
+1 471 (45.7)
+2 200 (19.4)
+3 82 (8.0)
Fat
+1 347 (33.7)
+2 188 (18.2)
+3 63 (6.1)
Amylum 129 (12.5)
Plant fibers 192 (18.6)
Muscle fibers 34 (3.3)
Occult blood 337 (32.7)
pH
6 or more 951 (92.2)
Less than 6 80 (7.8)
Glucose
0.25% 22 (2.1)
0.50% 36 (3.5)
0.75% 8 (0.8)
1% 16 (1.6)
2% 3 (0.3)
Parasites 6 (0.6)
Fungi 216 (21)
*One participant might present with more than 1 significant findings
APGHN | www.agphn.com Vol 1| August 2022 | Page 11
The laboratory findings of each participant were then interpreted to determine the
etiology of diarrhea. The most common interpretation indicated that most patients
suffered from diarrhea caused by bacterial infection (48%).
Table 4. Interpretation of stool analysis profile in patients aged 0-18 years
Diagnosis* n (%)
Bacterial infection 503 (48.8)
Fungal infection 80 (7.8)
Carbohydrate maldigestion 130 (12.6)
Food maldigestion 187 (18.1)
Protein maldigestion 29 (2.8)
Fat malabsorption 214 (20.8)
Lactose malabsorption 76 (7.4)
Suspected cow’s milk allergy 45 (4.4)
Dysentery/Infective colitis 143 (13.4)
*One participant might have more than 1 interpretation
Table 5. Interpretation of stool analysis profile in patients aged 0-59 months
Diagnosis* n (%)
Bacterial infection 269 (35.2)
Fungal infection 49 (6.5)
Carbohydrate maldigestion 72 (9.5)
Food maldigestion 81 (10.7)
Protein maldigestion 9 (1.2)
Fat malabsorption 228 (30.2)
Lactose malabsorption 76 (10.1)
Suspected cow’s milk allergy 42 (5.6)
Dysentery/Infective colitis 94 (12.4)
*One participant might have more than 1 interpretation
Discussion
The relationship between diarrhea and nutrition has been discussed widely. Many
factors contributed in the effect of diarrhea towards nutritional status. Increased
APGHN | www.agphn.com Vol 1| August 2022 | Page 12
nutrients loss, malabsorption, maldigestion, and the impact of inflammatory responses
are some of the factors involved in diarrhea with malnutrition. In this study, diarrhea
mainly occurred in children aged 0-24 months (55.6%). This result was similar to other
research in Indonesia, which stated that diarrhea mainly occurred in children aged less
than 24 months with the prevalence of 56.68%.8
This study demonstrated that the prevalence of diarrhea in children, especially boys,
was higher than in girls. It is similar to a study done in a hospital located in Yogyakarta,
Indonesia.9 Another study in Munimbili National hospital also revealed that 60% of
diarrhea patients were boys aged 7-12 months old.10
The characteristics of stool analysis varied among patients. The most prevalent
consistency among the samples in our study was liquid / watery stool (67%). Diarrhea
can cause malabsorption when the fluid volume in the colon is higher than the
absorption capacity. Damage in the intestine due to diarrhea decreases absorption and
increases secretion, generating the liquid consistency of the stool.1
Leukocytes in stools are produced as a response to the inflammatory process in the
mucosa of the colon. The presence of leukocytes in the feces indicates the existence
of invasive bacteria or bacteria-produced cytotoxin, which may cause tissue damage.
Furthermore, higher numbers of leukocytes increase the likelihood of invasive
pathogens infection. Fecal leukocyte stain was considered to have better accuracy and
diagnostic value in determining the etiology of diarrhea.11, 12 In our study, the number
of samples with leukocyte counts of +2 was higher than patients with leukocytes count
of +3, which accounted for 38.3% and 19.2% respectively.
The erythrocyte counts in our study were accounted for 19.4% (+2) and 8% (+3),
respectively. Although there was still no consensus in interpreting the erythrocytes
count in stool analysis, a study in Bangladesh had reported the benefit of direct
microscopical stool examination to quantify the leukocytes and erythrocytes in making
an early diagnosis of Shigella infection.13
Diarrhea is commonly related to motility dysfunction. Changes in motility can affect
absorption and lead to diarrhea. The reduction in motility promotes faster growth of
bacteria, as the pathogen can invade the intestine and disrupt the immunity of the
mucosal intestine, leading to the disruption of nutrient absorption.14
Based on the interpretation of stool analysis, bacterial infections were the most
frequently identified etiology of diarrhea in our study. It contradicts other findings,
which stated that viral infection was more likely to cause diarrhea in children. 15
However, our study did not perform any viral examination and stool culture.
APGHN | www.agphn.com Vol 1| August 2022 | Page 13
Therefore, the presence of viral infection and the type of bacteria causing diarrhea
could not be determined.
Diarrhea can cause maldigestion and malabsorption, which decreases nutrient
absorption. The main types of maldigestion and malabsorption that frequently
occurred in this study were fat malabsorption (20.8%), food maldigestion (18.1%), and
carbohydrate maldigestion (12.6%). Despite the lack of information on the prevalence
of food maldigestion, a study by Hendrawati et al. stated that the prevalence of fat
malabsorption and carbohydrate maldigestion were 51% and 19%, respectively. These
findings were higher compared to our study.3 The lower prevalence in our study could
be caused by the absence of data in some medical records. In addition, Hendrawati et
al. found that the peak incidence of carbohydrate maldigestion occurred at the age of
12-59 months.3 Carbohydrate is a component of diet with the highest percentage of
consumption in children at this particular age (12-59 months old). Furthermore,
diarrhea caused by Enterotoxigenic E.coli (ETEC) was found to occur more
frequently in children aged 12-59 months old. Diarrhea caused by ETEC is classified
as secretory diarrhea, in which the increase in intestinal motility and decrease in transit
time were observed. This will cause rapid contact between digestive enzymes and
carbohydrates, leading to inadequate digestion of carbohydrates, which results in the
occurrence of carbohydrate maldigestion.16
Conclusion
Diarrhea in children mainly occurs before two years old, particularly in boys than girls.
Watery diarrhea was the most frequent type of diarrhea, and bacterial was found to be
the primary etiology.
Conflict of Interest
None declared.
Funding
This research was a self-funded study.
Acknowledgement
The authors would like to thank the medical record and laboratories staffs in Cipto
Mangunkusumo Hospital for their support and help during the study.
APGHN | www.agphn.com Vol 1| August 2022 | Page 14
References
1. Juffrie M, Soenarto, Sri SY, Oswari H, Arief S, Rosalina I. 10. John S, Nuru P. Admission patterns and outcomes of
Buku ajar gastroenterologi-hepatologi. Jakarta: Badan paediatric patients admitted at the diarrhea unit of
Penerbit IDAI; 2012. Muhimbili National Hospital (MNH). Dar Es Salaam
2. Badan Penelitian dan Pengembangan Kesehatan. Riset Medical Students' Journal. 2008;15(1):9-12.
kesehatan dasar Jakarta [Internet]. 2013 [cited 2022 11. Savola KL, Baron EJ, Tompkins LS, Passaro DJ. Fecal
August 6]. Available from: www.litbang.depkes.go.id. leukocyte stain has diagnostic value for outpatients but not
3. Hendrawati LD, Firmansyah A, Darwis D. Macronutrient inpatients. J Clin Microbiol. 2001;39(1):266-9.
malabsorption in acute diarrhea: Prevalence and affecting 12. Manalip D, Warouw SM, Manoppo JIC. Hubungan antara
factors. Paediatr Indones. 2005;45(5):207-10. patogen usus dengan kadar laktoferin tinja pada anak
4. Marzuki N, Akib A, Boediman I. Cow's milk allergy in dengan diare akut. Sari Pediatri. 2016;17(2):124-8.
patients with diarrhea. Paediatr Indones. 2016;44(6):239- 13. Khan AI, Huq S, Malek MA, Hossain MI, Talukder KA,
42. Faruque A, et al. Analysis of fecal leukocytes and
5. Mundt LA, Shanahan K. Graff's textbook of urinalysis erythrocytes in Shigella infections in urban Bangladesh.
and body fluids. 2nd Edition. Philadelphia: Lippincott Southeast Asian J Trop Med Public Health.
Williams & Wilkins; 2011. 2006;37(4):747.
6. Davidson AGF, Mullinger M. Reducing substances in 14. Subagyo B, NB S. Diare akut. Buku ajar gastroenterologi-
neonatal stools detected by clinitest. Pediatrics. hepatologi. 1st Edition. Jakarta: Badan Penerbit IDAI.
1970;46(4):632-5. 2010.
7. Joneja JV. Lactose intolerance. Dealing with food allergies 15. Widowati T, Mulyani NS, Nirwati H, Soenarto Y. Diare
in babies and children. Boulder, Colorado: Bull Publishing Rotavirus pada anak usia balita. Sari Pediatri.
Company; 2007. 2016;13(5):340-5.
8. Yusuf S. Profil diare di ruang rawat inap anak. Sari 16. Bouchier IAD. Gastroenterology: Clinical science and
Pediatri. 2016;13(4):265-70. practice: Saunders; 1993.
9. Palupi A, Hadi H, Soenarto SS. Status gizi dan
hubungannya dengan kejadian diare pada anak diare akut
di ruang rawat inap RSUP Dr. Sardjito Yogyakarta. Jurnal
Gizi Klinik Indonesia. 2009;6(1):1-7.
APGHN | www.agphn.com Vol 1| August 2022 | Page 15
You might also like
- Vitamin Water - Arnel Ricafranca PDFDocument32 pagesVitamin Water - Arnel Ricafranca PDFAlaa EssamNo ratings yet
- BlsDocument62 pagesBlspaediatrica89% (19)
- Insurance Fraud PPT (Final)Document30 pagesInsurance Fraud PPT (Final)Gaurav Savlani83% (6)
- Acute Complications of Diabetes MellitusDocument1 pageAcute Complications of Diabetes MellitusGerardLum100% (1)
- Small-Sided Games and Integrating Physical PreparationDocument196 pagesSmall-Sided Games and Integrating Physical Preparationbolebs1475% (4)
- Lactose Intolerance Among Severely Malnourished Children With Diarrhoea Admitted To The Nutrition Unit, Mulago Hospital, UgandaDocument10 pagesLactose Intolerance Among Severely Malnourished Children With Diarrhoea Admitted To The Nutrition Unit, Mulago Hospital, UgandaSuci Joe ArmstrongNo ratings yet
- Hse Risk Assessment - 006 Ra - Hdpe Duct LayingDocument7 pagesHse Risk Assessment - 006 Ra - Hdpe Duct Layingbinunalukandam83% (12)
- Change Your Life in 7 Days With NLP - Paul Mckenna BrochureDocument2 pagesChange Your Life in 7 Days With NLP - Paul Mckenna Brochureapi-385316675% (4)
- Question and AnswerDocument4 pagesQuestion and AnswerShaf AbubakarNo ratings yet
- CPG AID - Pocket Guide.v7 PDFDocument31 pagesCPG AID - Pocket Guide.v7 PDFR ParkNo ratings yet
- SpitzDocument30 pagesSpitzprabhatNo ratings yet
- Toddler's Diarrhea: Is It An Under-Recognized Entity in Developing Countries?Document6 pagesToddler's Diarrhea: Is It An Under-Recognized Entity in Developing Countries?deonardNo ratings yet
- Efficacy of Probiotics in Acute Diarrhoea in Children: Original Research ArticleDocument5 pagesEfficacy of Probiotics in Acute Diarrhoea in Children: Original Research ArticledwimellyndaNo ratings yet
- Paediatrica Indonesiana: Teny Tjitrasari, MD Agus Firmansyah, MD, PHD Imral Chair, MDDocument7 pagesPaediatrica Indonesiana: Teny Tjitrasari, MD Agus Firmansyah, MD, PHD Imral Chair, MDakreditasi rsunhNo ratings yet
- Prolonged Acute Diarrhea in Adults: Decades of Observation From Epidemiological Perspective in Urban BangladeshDocument7 pagesProlonged Acute Diarrhea in Adults: Decades of Observation From Epidemiological Perspective in Urban BangladeshDefi MerisaNo ratings yet
- Saccharomyces boulardii May Shorten Diarrhea in ChildrenDocument5 pagesSaccharomyces boulardii May Shorten Diarrhea in ChildrenShankar YadavNo ratings yet
- Efficacy of Zinc Therapy in Acute Diarrhea in ChilDocument4 pagesEfficacy of Zinc Therapy in Acute Diarrhea in ChilKusuma IntanNo ratings yet
- Journal Reading Diare - Dea DickytaDocument7 pagesJournal Reading Diare - Dea DickytaDea DickytaNo ratings yet
- Clinical Profile of Functional Constipation in ChildrenDocument4 pagesClinical Profile of Functional Constipation in ChildrenIJAR JOURNALNo ratings yet
- The Clinical Spectrum of Chronic Diarrhea in ChildrenDocument15 pagesThe Clinical Spectrum of Chronic Diarrhea in ChildrenInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Askep KomplementerDocument14 pagesAskep KomplementernatiyaNo ratings yet
- 1 s2.0 S168719792100040X MainDocument4 pages1 s2.0 S168719792100040X MainfelipetheNo ratings yet
- Pattern of Acute Parasitic Diarrhea in Children Under Five Years of Age in Kathmandu, NepalDocument6 pagesPattern of Acute Parasitic Diarrhea in Children Under Five Years of Age in Kathmandu, NepalDaniel EvansNo ratings yet
- Diare Rotavirus Pada Anak Dibawah Usia 3 Tahun Yang Dirawat Di Rsu Dr. Saiful Anwar Malang Tahun 2005 (Preliminary Study)Document3 pagesDiare Rotavirus Pada Anak Dibawah Usia 3 Tahun Yang Dirawat Di Rsu Dr. Saiful Anwar Malang Tahun 2005 (Preliminary Study)Lala SyahaabNo ratings yet
- As URO Disfunção InfantilDocument5 pagesAs URO Disfunção InfantilKelvin CelliNo ratings yet
- Cochrane BVS: Oral Zinc For Treating Diarrhoea in ChildrenDocument25 pagesCochrane BVS: Oral Zinc For Treating Diarrhoea in ChildrenLaura AnguloNo ratings yet
- Lactose Intolerance Among Severely Malnourished Children With Diarrhoea Admitted To The Nutrition Unit, Mulago Hospital, UgandaDocument9 pagesLactose Intolerance Among Severely Malnourished Children With Diarrhoea Admitted To The Nutrition Unit, Mulago Hospital, UgandaArsy Mira PertiwiNo ratings yet
- Hubungan Diare Dengan Status Gizi Pada Balita Di Rumah Sakit Umum Daerah Dr. H. Chasan BoesoirieDocument6 pagesHubungan Diare Dengan Status Gizi Pada Balita Di Rumah Sakit Umum Daerah Dr. H. Chasan BoesoirieRippie RifdahNo ratings yet
- Jurnal AnakDocument7 pagesJurnal AnakNurul SahanaNo ratings yet
- Dokumen Tanpa JudulDocument10 pagesDokumen Tanpa JudulZakia AmeliaNo ratings yet
- Hubungan Pengetahuan Ibu Tentang Hygiene Makanan dan Diare pada BalitaDocument6 pagesHubungan Pengetahuan Ibu Tentang Hygiene Makanan dan Diare pada BalitaKoco Totok SugiartoNo ratings yet
- Natural evolution of regurgitation in children aged 12-24 monthsDocument6 pagesNatural evolution of regurgitation in children aged 12-24 monthsTianKaunangNo ratings yet
- HUBUNGAN SANITASI LINGKUNGAN DAN PERILAKU HIDUP BERSIH SEHAT DENGAN KEJADIAN DIARE PADA BALITADocument19 pagesHUBUNGAN SANITASI LINGKUNGAN DAN PERILAKU HIDUP BERSIH SEHAT DENGAN KEJADIAN DIARE PADA BALITAjumowoNo ratings yet
- Spectrum of Dysentery in Children Presenting To A Tertiary Level Teaching Hospital in New DelhiDocument5 pagesSpectrum of Dysentery in Children Presenting To A Tertiary Level Teaching Hospital in New DelhiNasNo ratings yet
- Influence of Nutritional Status On Clinical Outcomes in Critically Ill ChildrenDocument5 pagesInfluence of Nutritional Status On Clinical Outcomes in Critically Ill ChildrenAnonymous h0DxuJTNo ratings yet
- Influence of Nutritional Status On Clinical Outcomes in Critically Ill ChildrenDocument5 pagesInfluence of Nutritional Status On Clinical Outcomes in Critically Ill ChildrenIvana YunitaNo ratings yet
- 12933-Article Text-16095-1-10-20191208Document11 pages12933-Article Text-16095-1-10-20191208jaskiran kaurNo ratings yet
- Prevalence of Diarrhea and Malnutrition in Bangladeshi ChildrenDocument6 pagesPrevalence of Diarrhea and Malnutrition in Bangladeshi ChildrenSukmaNo ratings yet
- Analisis Jurnal Pico GeaDocument3 pagesAnalisis Jurnal Pico GeaMuhammad Robi Al BanjariNo ratings yet
- Submit Ijbs EditedDocument10 pagesSubmit Ijbs Editedpuannita santosoNo ratings yet
- Bacillus Clausii As An Adjuvant Therapy in Acute Childhood DiarrhoeaDocument3 pagesBacillus Clausii As An Adjuvant Therapy in Acute Childhood DiarrhoeaIOSRjournalNo ratings yet
- Nutritional Assessment of Children Admitted at The Children'S Ward of The Volta Regional HospitalDocument10 pagesNutritional Assessment of Children Admitted at The Children'S Ward of The Volta Regional HospitalClifford AfuNo ratings yet
- PrognosisDocument7 pagesPrognosispenyimpanankoas8No ratings yet
- PBL 2 KedkelDocument7 pagesPBL 2 KedkelDanindNo ratings yet
- Investigating Key Determinants of Childhood Diarrheal Incidence Among Patients at Hoima Regional Referral Hospital, Western UgandaDocument14 pagesInvestigating Key Determinants of Childhood Diarrheal Incidence Among Patients at Hoima Regional Referral Hospital, Western UgandaKIU PUBLICATION AND EXTENSIONNo ratings yet
- Synopsis Edited 3 - 073650 PDFDocument7 pagesSynopsis Edited 3 - 073650 PDFMohammad ShafiqNo ratings yet
- Comparison of Body Mass Index On Children With Functional Constipation and Healthy ControlsDocument5 pagesComparison of Body Mass Index On Children With Functional Constipation and Healthy ControlsGita TrisnawatiNo ratings yet
- 404 398 1 SMDocument4 pages404 398 1 SMfak youNo ratings yet
- Probiotics in Adolescent Prediabetes: A Pilot RCT On Glycemic Control and Intestinal BacteriomeDocument14 pagesProbiotics in Adolescent Prediabetes: A Pilot RCT On Glycemic Control and Intestinal BacteriomeKarina EkawidyaniNo ratings yet
- Jtstikesmuhgo GDL Wiwinpujia 1337 2 Hal.151 8Document8 pagesJtstikesmuhgo GDL Wiwinpujia 1337 2 Hal.151 8Bayou Fore YouNo ratings yet
- Electronic Physician (ISSN: 2008-5842)Document5 pagesElectronic Physician (ISSN: 2008-5842)Aldian DianNo ratings yet
- Acute Pyelonephritis in PregnancyDocument7 pagesAcute Pyelonephritis in PregnancyKvmLlyNo ratings yet
- Journal GastroenteritisDocument4 pagesJournal GastroenteritisRian KurniawanNo ratings yet
- Nutritional Assessment of Children With CHD CompareDocument9 pagesNutritional Assessment of Children With CHD CompareIntan Robi'ahNo ratings yet
- RCT Finds Gelatine Tannate Ineffective for Childhood GastroenteritisDocument39 pagesRCT Finds Gelatine Tannate Ineffective for Childhood Gastroenteritiszaky ariandyNo ratings yet
- 2305Document3 pages2305HelenCandyNo ratings yet
- 5 PBDocument5 pages5 PBluciaNo ratings yet
- Etiology of Acute Diarrhea in ChildrenDocument5 pagesEtiology of Acute Diarrhea in ChildrenZazaNo ratings yet
- Protective Effect of Breast Milk On Urinary Tract Infection in Children Aged 0-3 YearsDocument5 pagesProtective Effect of Breast Milk On Urinary Tract Infection in Children Aged 0-3 YearsChika FebrianiNo ratings yet
- Paediatric Appendicitis Scoring: A Useful Guide To Diagnose Acute Appendicitis in ChildrenDocument6 pagesPaediatric Appendicitis Scoring: A Useful Guide To Diagnose Acute Appendicitis in ChildrenFebrian Naranggi Aradia PutraNo ratings yet
- Knowledge Level and Determinants of Neonatal Jaundice A Cross-Sectional Study in The Effutu Municipality of GhanaDocument10 pagesKnowledge Level and Determinants of Neonatal Jaundice A Cross-Sectional Study in The Effutu Municipality of GhananicloverNo ratings yet
- E377 FullDocument6 pagesE377 FullBerliana SitanggangNo ratings yet
- Risk Correlates of Diarrhea in Children Under 5 Years of Age in Slums of Bankura, West BengalDocument8 pagesRisk Correlates of Diarrhea in Children Under 5 Years of Age in Slums of Bankura, West BengalSanaNo ratings yet
- Effect of diarrhea management at home on parents' knowledge and skillsDocument7 pagesEffect of diarrhea management at home on parents' knowledge and skillsCut Qurrata A'yunNo ratings yet
- Gastrointestinal Flora and Gastrointestinal Status in Children With Autism - Comparisons To Typical Children and Correlation With Autism SeverityDocument14 pagesGastrointestinal Flora and Gastrointestinal Status in Children With Autism - Comparisons To Typical Children and Correlation With Autism SeverityapriliaNo ratings yet
- Scholl Hammer 2015Document7 pagesScholl Hammer 2015jesslynNo ratings yet
- Estreñimiento y TeaDocument9 pagesEstreñimiento y TeaElena Martin LopezNo ratings yet
- Tannuri 2016Document5 pagesTannuri 2016sytaNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 5: GastrointestinalFrom EverandComplementary and Alternative Medical Lab Testing Part 5: GastrointestinalNo ratings yet
- BPN Datangi MalaysiaDocument62 pagesBPN Datangi MalaysiaafandianddonkeyNo ratings yet
- Otto Chemie PVT LTD: Material Safety Data SheetDocument4 pagesOtto Chemie PVT LTD: Material Safety Data Sheetenes duhanNo ratings yet
- SIP Physical SCiDocument8 pagesSIP Physical SCiShane Catherine BesaresNo ratings yet
- UG MaharashtraNationalLawUniversityMNLUMumbaiDocument5 pagesUG MaharashtraNationalLawUniversityMNLUMumbaiArpan KushwahaNo ratings yet
- Unilag MSC Environmenatl Toxicology SampleDocument4 pagesUnilag MSC Environmenatl Toxicology SamplebdianNo ratings yet
- City of Peterborough 2023 Draft Capital BudgetDocument535 pagesCity of Peterborough 2023 Draft Capital BudgetPeterborough ExaminerNo ratings yet
- IELTS-Style Speaking Test Questions and Answers SportDocument4 pagesIELTS-Style Speaking Test Questions and Answers SportĐại Học Ôn ThiNo ratings yet
- MSDSDocument3 pagesMSDSSiti Nurjanah SeptianiNo ratings yet
- Theory Critique of Boundaries in MarriageDocument8 pagesTheory Critique of Boundaries in MarriagepatrickakingNo ratings yet
- Grain Legumes/Pulses Introduction and ImportanceDocument5 pagesGrain Legumes/Pulses Introduction and ImportancesumandhakalNo ratings yet
- Types of Solder FluxDocument6 pagesTypes of Solder Fluxpeter paulNo ratings yet
- Strain Index Scoring Sheet: Date: Task: Company: Supervisor: Dept: EvaluatorDocument1 pageStrain Index Scoring Sheet: Date: Task: Company: Supervisor: Dept: EvaluatorUdaydeep SinghNo ratings yet
- Empowering Women Key to Ending PovertyDocument25 pagesEmpowering Women Key to Ending PovertydassmbaNo ratings yet
- Chapt01 The Sudy of ChangeDocument34 pagesChapt01 The Sudy of ChangeIkhsan Abdul HanifNo ratings yet
- A Comparative Study of The Efficacy of Cedarwood Oil, Coconut Oil and Dish Wash Liquid As Alternatives To Xylene As Deparaffinizing AgentsDocument98 pagesA Comparative Study of The Efficacy of Cedarwood Oil, Coconut Oil and Dish Wash Liquid As Alternatives To Xylene As Deparaffinizing AgentszzzzNo ratings yet
- KPJ Pasir Gudang Covid Test ReportDocument1 pageKPJ Pasir Gudang Covid Test ReportNooh DinNo ratings yet
- Product SelectionDocument5 pagesProduct Selectionemmanuelgk100No ratings yet
- Cricket Academy Head Coach RoleDocument4 pagesCricket Academy Head Coach Roletauseef1716No ratings yet
- Autoimmune HepatitisDocument3 pagesAutoimmune HepatitisMohammed FaragNo ratings yet
- Maynilad Valenzuela Sewerage Project Environmental ReportDocument297 pagesMaynilad Valenzuela Sewerage Project Environmental ReportmarvilouNo ratings yet
- Apply teacher short leaveDocument1 pageApply teacher short leaveJean Claudine MandayNo ratings yet