Professional Documents
Culture Documents
Articles: Background
Uploaded by
DayannaPintoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Articles: Background
Uploaded by
DayannaPintoCopyright:
Available Formats
Articles
Antepartum dalteparin versus no antepartum dalteparin for
the prevention of pregnancy complications in pregnant
women with thrombophilia (TIPPS): a multinational
open-label randomised trial
Marc A Rodger, William M Hague, John Kingdom, Susan R Kahn, Alan Karovitch, Mathew Sermer, Anne Marie Clement, Suzette Coat,
Wee Shian Chan, Joanne Said, Evelyne Rey, Sue Robinson, Rshmi Khurana, Christine Demers, Michael J Kovacs, Susan Solymoss, Kim Hinshaw,
James Dwyer, Graeme Smith, Sarah McDonald, Jill Newstead-Angel, Anne McLeod, Meena Khandelwal, Robert M Silver, Gregoire Le Gal,
Ian A Greer, Erin Keely, Karen Rosene-Montella, Mark Walker, Philip S Wells, for the TIPPS Investigators
Summary
Background Thrombophilias are common disorders that increase the risk of pregnancy-associated venous Published Online
thromboembolism and pregnancy loss and can also increase the risk of placenta-mediated pregnancy complications July 25, 2014
http://dx.doi.org/10.1016/
(severe pre-eclampsia, small-for-gestational-age infants, and placental abruption). We postulated that antepartum S0140-6736(14)60793-5
dalteparin would reduce these complications in pregnant women with thrombophilia.
See Online/Comment http://
dx.doi.org/10.1016/S0140-
Methods In this open-label randomised trial undertaken in 36 tertiary care centres in five countries, we enrolled 6736(14)60850-3
consenting pregnant women with thrombophilia at increased risk of venous thromboembolism or with previous Thrombosis Program, Division
placenta-mediated pregnancy complications. Eligible participants were randomly allocated in a 1:1 ratio to either of Hematology, Department of
Medicine, University of
antepartum prophylactic dose dalteparin (5000 international units once daily up to 20 weeks’ gestation, and twice daily
Ottawa, Ottawa, ON, Canada
thereafter until at least 37 weeks’ gestation) or to no antepartum dalteparin (control group). Randomisation was done (Prof M A Rodger MD); Ottawa
by a web-based randomisation system, and was stratified by country and gestational age at randomisation day with a Hospital Research Institute,
permuted block design (block sizes 4 and 8). At randomisation, site pharmacists (or delegates) received a randomisation Ottawa, ON, Canada
(Prof M A Rodger,
number and treatment allocation (by fax and/or e-mail) from the central web randomisation system and then dispensed
A M Clement RN,
study drug to the local coordinator. Patients and study personnel were not masked to treatment assignment, but the Prof G Le Gal MD,
outcome adjudicators were masked. The primary composite outcome was independently adjudicated severe or early- Prof E Keely MD, M Walker MD,
onset pre-eclampsia, small-for-gestational-age infant (birthweight <10th percentile), pregnancy loss, or venous Prof P S Wells MD); Obstetric
Medicine, Robinson Institute,
thromboembolism. We did intention-to-treat and on-treatment analyses. This trial is registered with ClinicalTrials.gov,
University of Adelaide,
number NCT00967382, and with Current Controlled Trials, number ISRCTN87441504. Women’s and Children’s
Hospital, Adelaide, South
Findings Between Feb 28, 2000, and Sept 14, 2012, 292 women consented to participate and were randomly assigned Australia, Australia
(Prof W M Hague MD); Division
to the two groups. Three women were excluded after randomisation because of ineligibility (two in the antepartum
of Maternal-Fetal Medicine,
dalteparin group and one in the control group), leaving 146 women assigned to antepartum dalteparin and 143 assigned Department of Obstetrics and
to no antepartum dalteparin. Some patients crossed over to the other group during treatment, and therefore for on- Gynecology, Mount Sinai
treatment and safety analysis there were 143 patients in the dalteparin group and 141 in the no dalteparin group. Hospital, University of Toronto,
Toronto, ON, Canada
Dalteparin did not reduce the incidence of the primary composite outcome in both intention-to-treat analysis (Prof J Kingdom MD,
(dalteparin 25/146 [17·1%; 95% CI 11·4–24·2%] vs no dalteparin 27/143 [18·9%; 95% CI 12·8–26·3%]; risk difference Prof M Sermer MD); Centre for
−1·8% [95% CI –10·6% to 7·1%)) and on-treatment analysis (dalteparin 28/143 [19·6%] vs no dalteparin 24/141 Clinical Epidemiology, Jewish
[17·0%]; risk difference +2·6% [95% CI –6·4 to 11·6%]). In safety analysis, the occurrence of major bleeding did not General Hospital, Montreal, QC,
Canada (Prof S R Kahn MD);
differ between the two groups. However, minor bleeding was more common in the dalteparin group (28/143 [19·6%]) Department of Medicine,
than in the no dalteparin group (13/141 [9·2%]; risk difference 10·4%, 95% CI 2·3–18·4; p=0·01). University of Ottawa/Ottawa
Hospital, Ottawa, ON, Canada
Interpretation Antepartum prophylactic dalteparin does not reduce the occurrence of venous thromboembolism, (A Karovitch MD, Prof G Le Gal,
Prof E Keely, Prof P S Wells);
pregnancy loss, or placenta-mediated pregnancy complications in pregnant women with thrombophilia at high risk Robinson Institute, University
of these complications and is associated with an increased risk of minor bleeding. of Adelaide, Adelaide, South
Australia, Australia
Funding Canadian Institutes of Health Research, Heart and Stroke Foundation of Canada, and Pharmacia and UpJohn. (S Coat PhD); Department of
Medicine, University of British
Columbia, Vancouver, BC,
Introduction women.2 Thrombophilia acts synergistically with Canada (W S Chan MD);
Thrombophilias are common acquired or genetic pregnancy to increase further the risk of venous Maternal Fetal Medicine,
NorthWest Academic Center,
predispositions to develop venous thromboembolism.1 thromboembolism during pregnancy.3
University of Melbourne,
Venous thromboembolism, which comprises deep vein Placenta-mediated pregnancy complications, comprising Melbourne, Australia
thrombosis and pulmonary embolism, is more frequent pre-eclampsia, birth of a small-for-gestational-age infant, (J Said MBBS); Departments of
in pregnant women than in non-pregnant age-matched placental abruption, or pregnancy loss, are also common4,5 Medicine and Obstetrics and
www.thelancet.com Published online July 25, 2014 http://dx.doi.org/10.1016/S0140-6736(14)60793-5 1
Articles
Gynecology, University of and lead to substantial maternal and fetal or neonatal the Therapeutic Goods Administration (Australia), or the
Montreal, and CHU Sainte- morbidity and mortality.4 Placental microvascular and Medicines and Healthcare Product Regulatory Agency
Justine Research Center,
Montreal, QC, Canada
macrovascular thrombosis is a frequent, overlapping, (UK), and local research ethics board approvals before we
(E Rey MD); Department of pathophysiological link in many affected pregnancies.5 began the study. All women participating in the study
Medicine, Dalhousie University, Patients with previous placenta-mediated pregnancy provided written informed consent.
Halifax, NS, Canada complications have a raised risk of both recurrent We screened 3022 women with previous pregnancy
(Prof S Robinson MD);
Departments of Medicine and
placenta-mediated pregnancy complications6 and venous complications, venous thromboembolism risk factors, or
Obstetrics and Gynecology, thromboembolism during subsequent pregnancies.7,8 thrombophilia for eligibility. Women were eligible for
University of Alberta, Royal Similarly, evidence suggests that women with previous inclusion if they had a confirmed thrombophilia (panel 1),
Alexandra Hospital, Edmonton,
venous thromboembolism have a raised risk of placenta- were at raised risk of placenta-mediated pregnancy
AB, Canada (R Khurana MD);
Department of Medicine, mediated pregnancy complications in subsequent complications or venous thromboembolism (panel 1),
Université de Laval, Quebec, QC, pregnancies.9 were pregnant, and had provided written informed
Canada (C Demers MD); Thrombophilias are consistently associated with early consent. Women were excluded if they were 21 weeks or
Department of Medicine,
and late pregnancy loss10,11 and can also be related to more gestational age at the time of randomisation, had a
London Health Sciences Centre,
University of Western Ontario, severe pre-eclampsia, birth of a small-for-gestational-age contraindication to heparin treatment (panel 1), were
London, ON, Canada infant below the third percentile of birthweight, and geographically inaccessible, needed anticoagulant therapy
(Prof M J Kovacs MD); placental abruption.10 Since the initial discovery of an as judged by the local investigator (panel 1), had already
Department of Medicine, McGill
association between thrombophilia and placenta- previously participated in the study, or were younger than
University, St Mary’s Hospital
Center, Montreal, QC, Canada mediated pregnancy complications more than 15 years the legal lower age limit to provide consent according to
(S Solymoss MD); Department of ago,12 clinicians, patients, guideline developers, and policy country-specific regulations. We maintained screening
Obstetrics, Sunderland Royal makers have struggled to address the question of whether records to detail any reason for ineligibility in all patients
Hospital, Sunderland, Tyne and
pregnant women with thrombophilia should receive approached for the study.
Wear, UK (K Hinshaw MBBS);
Department of Obstetrics and antepartum thromboprophylaxis.13
Gynaecology, York Hospital, Low-molecular-weight heparin is the thrombo- Randomisation and masking
York, UK (J Dwyer MBBS); prophylactic drug of choice in pregnancy because, unlike After confirming eligibility and obtaining consent, research
Department of Obstetrics and
Gynecology, Queen’s University,
oral anticoagulants, it does not cross the placenta and has a coordinators at each centre randomly assigned eligible
Kingston, ON, Canada favourable maternal safety profile with a low risk of major patients in a 1:1 ratio to antepartum dalteparin or no
(Prof G Smith MD); Division of bleeding, heparin-induced thrombocytopenia, and antepartum dalteparin by a web-based randomisation
Maternal-Fetal Medicine, heparin-induced osteoporosis.14 Nonetheless, the drug system. The computer-generated randomisation schedule
Department of Obstetrics and
Gynecology, Department of
needs to be administered by burdensome daily or twice was stratified by country and gestational age at
Radiology, and Department of daily subcutaneous injections, is expensive, and can randomisation day (<8 weeks, 8–12 weeks, and 12–20 weeks)
Clinical Epidemiology and complicate regional anaesthetic options if not discontinued and had a permuted block design (block sizes 4 and 8). At
Biostatistics, McMaster within 12–24 h of labour onset. the time of randomisation, site pharmacists (or delegates)
University, Hamilton, ON,
Canada (S McDonald MD);
In the Thrombophilia in Pregnancy Prophylaxis Study received a randomisation number and treatment allocation
Department of Medicine, (TIPPS) we aimed to establish whether antepartum (by fax and/or e-mail) from the central web randomisation
University of Saskatchewan, prophylactic dalteparin, a low-molecular-weight heparin, system. The site pharmacist (or delegate) then dispensed
Saskatoon, SK, Canada would reduce the risk of venous thromboembolism and study drug to the local coordinator who taught the study
(J Newstead-Angel MD);
Department of Medicine,
placenta-mediated pregnancy complications in pregnant participants how to self-administer the study drug and
Sunnybrook Health Sciences women with thrombophilia at high risk of pregnancy explained the trial procedures. Patients and study personnel
Centre, Toronto, ON, Canada complications. were not masked but outcome adjudicators were masked to
(A McLeod MD); Department of treatment assignment.
Obstetrics and Gynecology,
Cooper Medical School of Methods
Rowan University/Cooper Study design and participants Procedures
Hospital, Camden, NJ, USA We enrolled pregnant women with thrombophilia who We randomly assigned 292 women to receive either
(Prof M Khandelwal MD);
were at increased risk of placenta-mediated pregnancy antepartum dalteparin 5000 international units (IU)
Department of Obstetrics and
Gynecology, University of Utah complications, venous thromboembolism, or both in a once daily by subcutaneous self-injection from the day
Health Sciences Center, Salt Lake randomised trial to compare prophylactic dose antepartum of randomisation until 20 weeks of gestation followed
City, UT, USA dalteparin with no antepartum dalteparin. Between by 5000 IU twice daily from 20 weeks until at least
(Prof R M Silver MD); Faculty of
Feb 28, 2000, and Sept 14, 2012, the study was initiated in 37 weeks gestational age, or no antepartum dalteparin.
Health and Life Sciences,
University of Liverpool, 36 tertiary care centres in Canada, Australia, the USA, the The dose of dalteparin was doubled at 20 weeks’
Liverpool, UK (Prof I A Greer MD); UK, and France. 26 of these 36 centres screened patients gestation on the basis of pharmacokinetic studies
and Department of Medicine, for eligibility (the other ten did not because they were suggesting that the dose requirement increases in most
The Warren Alpert Medical
either unable to implement local trial operations or get women after this point.15 During the initial 26 months
School of Brown University,
Women’s Medicine referrals to screen potentially eligible patients) and of the study, the control group received matching,
Collaborative, Providence, RI, 21 centres recruited at least one patient. We obtained identically supplied and formulated placebo in prefilled
USA (Prof K Rosene-Montella MD) appropriate regulatory approvals from Health Canada syringes. Owing to poor recruitment (only 19 participants
(Canada), the US Food and Drug Administration (USA), were recruited in 26 months), on June 25, 2002, the trial
2 www.thelancet.com Published online July 25, 2014 http://dx.doi.org/10.1016/S0140-6736(14)60793-5
Articles
Correspondence to:
Panel 1: Specific inclusion and exclusion criteria Prof Marc A Rodger, Ottawa
Hospital, General Campus,
Inclusion criteria (1, 2, 3, and 4 must have been met for 3 Pregnancy confirmed by a positive serum, or urine 501 Smyth Road, Box 201A,
inclusion): βhCG, or by ultrasound Ottawa, ON, K1H 8L6, Canada
4 Signed informed consent mrodger@ohri.ca
1 Thrombophilia confirmed by one or more of the following:
1·1 Factor V Leiden: one positive DNA based assay for factor V Exclusion criteria (any one criterion met led to exclusion):
Leiden (homozygous or heterozygous), or documented
1 21 weeks or more gestational age at time of randomisation
activated protein C resistance and a first-degree relative
testing positive once for factor V Leiden in a DNA-based assay 2 Contraindication to heparin therapy, including:
1·2 Prothrombin gene mutation (homozygous or heterozygous) in 2·1 History of heparin-induced thrombocytopenia
a DNA-based assay 2·2 Platelet count lower than 100 000 × 106/L
or 2·3 History of osteoporosis or steroid use (potential
Two abnormal tests, and no normal tests, for one or more of increased risk of osteoporosis and osteoporotic
the following: fracture with heparin therapy)
1·3 Protein C deficiency 2·4 Actively bleeding
1·4 Protein S deficiency: at least one test done outside 2·5 Documented peptic ulcer within 6 weeks
pregnancy or the 6 week post-partum period, or, in addition (contraindication to anticoagulation)
to two abnormal tests in pregnancy, one abnormal test 2·6 Heparin, bisulphite, or fish allergy
obtained in a first-degree relative 2·7 Severe hypertension (systolic blood pressure
1·5 Antithrombin deficiency >200 mm Hg and/or diastolic blood pressure
or >120 mm Hg: contraindication to anticoagulation)
1·6 Anti-phospholipid antibody confirmed by two positive tests 2·8 Severe hepatic failure (international normalised ratio
for one or more of the following: anticardiolipin IgG >1·8): increased likelihood of bleeding
(>30 U/ml), anticardiolipin IgM (>30 U/ml), anti-β2 2·9 Women with serum creatinine level greater than
glycoprotein IgG (>20 U/ml), anti-β2 glycoprotein IgM 80 μmol/L (1·3 mg/dL) and 24-h creatinine clearance
(>20 U/ml), or positive Lupus anticoagulant less than 30 mL/min. However, women with serum
creatinine clearance of 80 μmol/L (1·3 mg/dL) or less
2 One or more of the following high-risk criteria for
did not require a normal 24-h creatinine clearance to
pregnancy complications (venous thromboembolism,
be eligible.
pregnancy loss, or placenta-mediated complications):
2·1 Previous history of pre-eclampsia (including late-onset and 3 Geographical inaccessibility (less likely to comply with
non-severe pre-eclampsia) necessary follow-up visits and care)
2·2 Previous unexplained birth of a small-for-gestational-age
4 Need for anticoagulants as judged by the local
infant (birthweight <10th percentile, corrected for sex and
investigator, including (but not limited to):
gestational age)
4·1 Women with recurrent pregnancy loss with
2·3 Previous major placental abruption, defined as an abruption
antiphospholipid antibody syndrome
associated with: vaginal bleeding or concealed
4·2 Women with previous unprovoked§ proximal¶
haemorrhage, and uterine tenderness, and fetal distress,
venous thromboembolism, whose pulmonary
maternal shock, or maternal coagulopathy
embolism or deep vein thrombosis was treated with
2·4 Previous pregnancy loss* defined as:
anticoagulants (more than 1 month of heparin or
2·4·1 Three or more unexplained pregnancy losses at
warfarin) or inferior vena cava interruption
less than 10 weeks’ gestation, or
4·3 Women with mechanical heart valves
2·4·2 Two or more unexplained pregnancy losses between
4·4 Women on long-term anticoagulants before
10 and 16 weeks’ gestation, or
pregnancy
2·4·3 One or more unexplained pregnancy losses at or more
than 16 weeks’ gestation 5 Previous participation in the TIPPS trial
2·5 Women with a history of one or more of the following
6 Below the legal age limit to provide informed consent
thromboembolic events/risk factors:
according to country-specific regulations
2·5·1 Previous documented provoked proximal† venous
thromboembolism *Examples of explained miscarriage or fetal loss include loss associated with severe congenital
2·5·2 Previous documented calf vein‡ thrombosis malformations, chromosomal abnormalities, neonatal alloimmune haemolytic anaemia,
recent cytomegalovirus infection, positive fetal or placental listeria cultures, and women with
2·5·3 Previous superficial phlebitis known abnormal uterine anatomy. †Proximal venous thromboembolism includes pulmonary
2·5·4 A first-degree relative with a history of pulmonary embolism or deep vein thrombosis occurring at or above the trifurcation of the popliteal vein.
‡Calf vein thrombosis is a deep vein thrombosis that occurs below the trifurcation of the
embolism or deep vein thrombosis treated with
popliteal vein. §Unprovoked refers to a venous thromboembolism that occurs outside all of
anticoagulants (more than 1 month of heparin or the following periods: surgery, immobilisation, cast, and/or malignancy. ¶Proximal refers to a
warfarin) venous thromboembolism that occurs above the trifurcation of the popliteal vein.
www.thelancet.com Published online July 25, 2014 http://dx.doi.org/10.1016/S0140-6736(14)60793-5 3
Articles
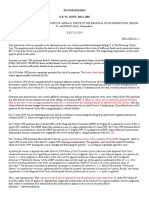
3022 women assessed for eligibility
2730 excluded
2378 did not meet eligibility criteria
175 had ≥1 exclusion criteria
177 refused to participate
292 randomised
148 initially allocated to antepartum dalteparin 144 initially allocated to no antepartum dalteparin
2 excluded for ineligibility 1 excluded for ineligibility
146 allocated to antepartum dalteparin 143 allocated to no antepartum dalteparin
12 crossed over to the control group 14 crossed over to the antepartum
dalteparin group
14 patients crossed over from other group 12 patients crossed over from other group
148 received antepartum dalteparin 141 received no antepartum dalteparin
0 lost to follow-up (note: 3 patients did not 0 lost to follow-up (note: 6 patients did not
have a 6-week post-partum visit) have a 6-week post-partum visit)
15 non-compliant with dalteparin 14 non-compliant with post-partum
1 had <80% antepartum doses dalteparin (<80% post-partum doses)
10 had <80% post-partum doses
4 had <80% doses in both periods
146 women in intention-to-treat analysis 143 women in intention-to-treat analysis
143 women in on-treatment and safety analyses* 141 women in on-treatment and safety analyses
Figure 1: Trial profile
*The five patients who were non-compliant with antepartum dalteparin were excluded from the on-treatment and safety analyses.
steering committee changed the study design to an assessment for protein and blood, complete blood
open-label trial comparing antepartum open-label count, and serum creatinine and liver function tests.
dalteparin with no antepartum dalteparin control. Post Bone mineral density was measured at the 6-week post-
partum, all participants were prescribed dalteparin at a partum visit. Additionally, follow-up visits, either in
dose of 5000 IU once daily by subcutaneous self- person or on the telephone, were done at 8, 16, 24, 30,
injection from day 1 (administered 6–28 h after delivery) 34, 35, 37, 38, 39, and 40 weeks’ gestation. We assessed
until day 42. All participants received otherwise similar outcomes and adverse events at the time of labour and
obstetrical care (according to local practices) and study delivery by review of participants’ medical records and
follow-up. any gaps were resolved at the 6 weeks post-partum
We defined crossovers as participants who switched follow-up visit.
study groups within 10 days of randomisation.
Participants who discontinued dalteparin after 10 days Outcomes
were labelled as non-compliant. Throughout study The primary endpoint was a composite outcome that
follow-up, we recorded cointerventions (eg, aspirin) and included any of the following events: objectively
concomitant use of other medications. documented symptomatic major venous thrombo-
Patients attended clinic follow-up visits within embolism (deep vein thrombosis proximal to the calf
7–9 days of randomisation and then at 12, 20, 28, 32, trifurcation, pulmonary embolism, or sudden maternal
36 weeks’ gestation and at 6 weeks post partum. These death); severe or early-onset (<32 weeks) pre-eclampsia
visits included assessments of outcome and adverse (defined as severe if accompanied by blood pressure
events, measurement of weight and blood pressure, ≥160/110 mm Hg or liver function tests three-times
study drug compliance diary review, urine dipstick above normal limits, platelet count <100 000 × 10⁶/L,
4 www.thelancet.com Published online July 25, 2014 http://dx.doi.org/10.1016/S0140-6736(14)60793-5
Articles
oliguria [<30 mL/h urine output in a 24 h period], Hemostasis17) and minor bleeding (non-major bleeding),
pulmonary oedema [on chest x-ray], coagulopathy bone mineral density measured at 6 weeks post partum,
[partial thromboplastin time >1·5 ×baseline, preterm delivery, placental abruption, heparin-induced
international normalised ratio >1·5 ×baseline, or thrombocytopenia, and symptomatic fracture.
fibrinogen <1·0 g/dL], proteinuria >5 g/24 h, or All suspected primary and secondary outcome events
seizures); birth of a small-for-gestational-age infant were adjudicated independently and blindly by at least
(birthweight <10th percentile);16 or pregnancy loss. two physicians in a panel that included experts in
Placental abruption was not included in the composite obstetrics and thrombosis.
primary outcome because of the hypothetical possibility
that dalteparin might increase the frequency of this
Antepartum No
bleeding complication. dalteparin antepartum
Secondary outcomes included major bleeding (as group dalteparin
defined by the International Society of Thrombosis and (n=146) group (n=143)
(Continued from previous column)
Antepartum No High-risk inclusion criteria
dalteparin antepartum
Previous pregnancy complications 92 (63%) 84 (59%)
group dalteparin
(any of those listed below)
(n=146) group (n=143)
Pre-eclampsia 20 (14%) 25 (18%)
Age (years) 31·9 (4·7) 31·6 (5·1)
Eclampsia 3 (2%) 3 (2%)
Gestational age at randomisation 12·0 (4·5) 11·7 (4·7)
(weeks) SGA infant (<10th percentile) 26 (18%) 19 (13%)
Ethnic origin Major placental abruption 16 (11%) 10 (7%)
White 133 (91%) 129 (90%) Three or more miscarriages at 24 (16%) 20 (14%)
<10 weeks’ gestation
Black 3 (2%) 3 (2%)
Two or more fetal losses at 11 (8%) 14 (10%)
Asian 8 (6%) 4 (3%) 10–16 weeks’ gestation
Native Canadian 0 3 (2%) One or more fetal losses at 27 (19%) 33 (23%)
Other 2 (1%) 4 (3%) ≥16 weeks’ gestation
Smoking status VTE risk factors/events (any of the 67 (46%) 61 (43%)
Ever smoker 56 (38%) 51 (36%) following)
Current smoker 5 (3%) 4 (3%) Family history of VTE in first- 45 (31%) 46 (32%)
degree relatives
BMI (kg/m²)
Mean number of first-degree 1·1 1·1
Pre-pregnancy 26·3 (6·6) 27·0 (6·8) relatives with VTE, per participant
At time of randomisation 27·7 (6·8) 27·8 (6·5) Previous secondary VTE 11 (8%) 9 (6%)
Baseline blood pressure (mm Hg) Previous calf deep vein thrombosis 10 (7%) 6 (4%)
Systolic 112·3 (12·0) 114·4 (12·6) Previous superficial phlebitis 7 (5%) 5 (4%)
Diastolic 67·9 (8·9) 69·6 (9·5) Concurrent medications during study
Obstetrical history pregnancy
Gravidity 3·1 (1·8) 3·3 (1·9) Aspirin (all participants) 43 (30%) 57 (40%)
Parity 1·0 (1·2) 1·0 (1·0) Aspirin (participants with previous 15/37 (41%) 19/28 (68%)
Preterm deliveries 0·33 (0·54) 0·32 (0·53) pre-eclampsia or SGA infants)
Spontaneous abortions 1·1 (1·48) 1·2 (1·5) Vitamins including folic acid 136 (93%) 142 (99%)
Therapeutic abortions 0·2 (0·58) 0·2 (0·45) Analgesic use in pregnancy 67 (46%) 49 (34%)
Living children 0·7 (1·0) 0·6 (0·75) Antibiotic use in pregnancy 45 (31%) 40 (28%)
Multiple pregnancies (ie, twins, 0·01 (0·1) 0·03 (0·18) Labour and delivery of study pregnancy
triplets) Induced 64 (44%) 55 (39%)
Outcomes after previous livebirths Epidural use 80 (55%) 82 (57%)
Neonatal death 13 (9%) 14 (10%) Caesarean section 61 (42%) 53 (37%)
Infant death 5 (3%) 4 (3%) Emergency caesarean section 25 (17%) 19 (13%)
Thrombophilia inclusion criteria Peri-partum haemorrhage 6 (4%) 9 (6%)
Factor V Leiden* 94 (64%) 82 (57%) Major 2 (1%) 2 (1%)
Prothrombin gene mutation 30 (21%) 33 (23%) Minor 4 (3%) 7 (5%)
Protein S deficiency 11 (8%) 13 (9%) Estimated blood loss at delivery (mL) 467·4 (201·0) 470·4 (237·1)
Protein C deficiency 6 (4%) 11 (8%)
Data are mean (SD) or n (%), unless otherwise indicated. SGA=small for
Antithrombin deficiency 2 (1%) 1 (1%) gestational age. VTE=venous thromboembolism. *Four patients with
Antiphospholipid antibody 12 (8%) 10 (7%) homozygous Factor V Leiden.
(Table continues in next column)
Table 1: Baseline characteristics
www.thelancet.com Published online July 25, 2014 http://dx.doi.org/10.1016/S0140-6736(14)60793-5 5
Articles
expected minimal clinically important difference of 16%
Antepartum No antepartum Difference (95% CI) p
dalteparin dalteparin value (ie, 33% relative risk reduction), we aimed for a sample size
(n=146) (n=143) of 284 to achieve 80% power with a two-tailed α of 0·05.
Primary analysis The data safety monitoring board reviewed study
Patients with one or more of major 25 (17·1%) 27 (18·9%) −1·8% (−10·6 to 7·1) 0·70 performance and safety outcomes regularly. The board
VTE, severe or early onset also did a single planned formal blinded interim analysis
pre-eclampsia, SGA (<10%), or after 50% of study participants completed follow-up.
pregnancy loss
All data analyses were done according to a pre-
Stratified by gestational age at
randomisation
established analysis plan, with an intention-to-treat
approach. Intention-to-treat analysis was supplemented
<8 weeks 9/33 (27·3%) 12/32 (37·5%) −10·2% (−32·9 to 12·4) 0·38
by an on-treatment sensitivity analysis to assess the
8–12 weeks 9/33 (27·3%) 3/32 (9·4%) 17·9% (−0·3 to 36·1) 0·06
robustness of our findings.
12–20 weeks 7/80 (8·8%) 12/79 (15·2%) −6·4% (−16·5 to 3·6) 0·21
For the primary analysis, we compared the proportion
Stratified by location
of patients experiencing one or more of the composite
Australia 8/38 (21·0%) 8/36 (22·2%) −1·2% (−19·9 to 17·6) 0·90
outcome events between the dalteparin group and the
Canada 17/102 (16·7%) 19/104 (18·3%) −1·6% (−12·0 to 8·8) 0·76
control group using an unadjusted χ² test of proportions.
Europe 0/3 0/1 NA NA
We did prespecified subgroup analyses, in which we
USA 0/3 0/1 NA NA
analysed treatment effects in subgroups based on
Secondary analysis: efficacy outcomes
stratification variables (country and gestational age at
Symptomatic major VTE 1 (0·7%) 2 (1·4%) −0·7 (−3·1 to 1·6) 0·62
recruitment), thrombophilia, previous history of specific
Pre-eclampsia 8 (5·5%) 5 (3·5%) 2·0 (−2·8 to 6·8) 0·42 placenta-mediated pregnancy complications, and history
Severe or early onset pre- 7 (4·8%) 4 (2·8%) 2·0 (−2·4 to 6·4) 0·38 of venous thromboembolism events or risk factors.
eclampsia
In secondary analyses, for each of the binary outcomes
Small-for-gestational-age infant 9 (6·2%) 12 (8·4%) −2·2 (−8·2 to 3·8) 0·47
(<10%) (major bleeding, minor bleeding, preterm delivery,
SGA (<5%) 2 (1·4%) 3 (2·1%) −0·7 (−3·7 to 2·3) 0·68 heparin-induced thrombocytopenia, and fractures), we
SGA (<3%) 3 (2·0%) 0 2·0 (−0·2 to 4·4) 0·25
used an unadjusted χ² test of proportions to compare the
Pregnancy loss (any) 12 (8·2%) 10 (7·0%) 1·2 (−4·9 to 7·3) 0·69
proportion of patients with these outcomes between the
Early (≥3 at <10 weeks) 4 (2·7%) 5 (3·5%) 0·8 (−4·8 to 3·2) 0·75
dalteparin group and the control group. We compared
mean bone mineral density, gestational age at delivery,
Late (≥2 at >10 weeks or ≥1 at 6 (4·1%) 2 (1·4%) 2·7 (−1·0 to 6·5) 0·28
>16 weeks) and birthweight in the dalteparin and control groups with
Any pre-eclampsia, SGA, or loss 27 (18·5%) 28 (19·6%) −1·1 (−10·1 to 8·0) 0·81 independent t tests. We also did on-treatment sensitivity
or abruption analyses for the primary and secondary analyses.
Placental abruption 4 (2·7%) 3 (2·1%) 0·6 (−2·9 to 4·2) 0·72 Descriptive data are presented as percentages or means
Preterm delivery (<37 weeks) 23 (15·8%) 17 (11·9%) 3·9 (−4·1 to 11·8) 0·34 (SDs). All statistical tests were two-sided and significance
Birthweight of livebirths (g) 3186·2 (758) 3241·4 (764) −55·2 (−238·6 to 0·55 was set at p<0·05. SAS version 9.3 was used for all
128·1) analyses. This trial is registered with ClinicalTrials.gov,
Gestational age at delivery (weeks) number NCT00967382, and with Current Controlled
Of livebirths 38·1 (2·84) 38·2 (3·1) −0·13 (−0·86 to 0·59) 0·72 Trials, number ISRCTN87441504.
Of pregnancy loss 16·8 (8·2) 10·8 (5·3) 6·0 (−0·09 to 12·11) 0·06
Secondary analysis: safety outcomes (on-treatment analysis) (n=143 in dalteparin group, n=141 in Role of the funding source
control group) The funders of the study had no role in the design or
Major bleeding 3 (2·1%) 2 (1·4%) 0·7 (−2·4 to 3·7) 1·0 conduct of the study; in the collection, analysis, and
Minor bleeding (non-major) 28 (19·6%) 13 (9·2%) 10·4 (2·3 to 18·4) 0·01 interpretation of the data; or in the preparation, review, or
Heparin-induced 0 0 ·· ·· approval of the report. MAR, TR, RM, DF, and AMC had
thrombocytopenia
complete access to all the data in the study, and MAR,
Osteoporotic fracture 0 0 ·· ··
PSW, AK, JK, MS, WMH, SRK, WSC, and AMC had final
Bone mineral density measured at 2·16 (0·35) 2·23 (0·42) −0·07 (−0·19 to 0·04) 0·21
6 weeks post partum (g/cm³)
responsibility for the decision to submit for publication.
Data are n (%) or mean (SD), unless otherwise indicated. VTE=venous thromboembolism. SGA=small for gestational Results
age. NA=not applicable.
Between Feb 28, 2000, and Sept 14, 2012, we approached
Table 2: Primary and secondary analysis 469 eligible women to participate in the study, of whom
292 consented and were randomly allocated to either
Statistical analysis antepartum dalteparin (n=148) or no antepartum
A priori, based on the prediction that venous dalteparin (n=144; figure 1). Three women were excluded
thromboembolism, severe or early onset pre-eclampsia, post-randomisation because of ineligibility (two in the
small-for-gestational-age infants, or pregnancy loss would antepartum dalteparin group [who received the drug but
occur in 49% of the control participants12,18–20 and an were not eligible to participate] and one in the control
6 www.thelancet.com Published online July 25, 2014 http://dx.doi.org/10.1016/S0140-6736(14)60793-5
Articles
Events/total (n/N) Risk ratio (95% CI) p value
Dalteparin Control
Subgroup
Maternal age <35 years 14/109 17/98 0·70 (0·4–1·4) 0·37
Maternal age <40 years 22/135 26/136 0·90 (0·5–1·4) 0·54
Previous pregnancy loss 14/69 17/74 0·90 (0·5–1·6) 0·70
Previous early loss 7/24 4/20 1·50 (0·5–4·3) 0·49
Previous late loss 9/37 12/44 0·90 (0·4–1·9) 0·76
Previous pre-eclampsia 7/20 6/25 1·50 (0·6–3·6) 0·42
Previous severe/early pre-eclampsia 6/13 2/9 2·10 (0·5–8·1) 0·29
Previous SGA <10% 7/26 5/19 1·02 (0·4–2·7) 0·96
Previous SGA <5% 1/3 0/1 1·50 (0·1–22·6) 0·77
Previous SGA <3% 3/13 3/11 0·80 (0·2–3·4) 0·81
Previous abruption 0/16 4/10 0·10 (0·004–1·2) 0·07
Previous secondary VTE 2/11 0/9 4·20 (0·2–77·1) 0·34
Previous calf deep vein thrombosis 0/10 3/6 0·10 (0·01–1·5) 0·09
Family history of VTE 5/45 6/46 0·80 (0·3–2·6) 0·78
Factor V Leiden 17/94 13/82 1·10 (0·6–2·2) 0·70
Prothrombin gene mutation 3/30 4/33 0·80 (0·2–3·4) 0·79
APLA 4/12 3/10 1·10 (0·3–3·8) 0·87
Protein C/protein S/antithrombin 1/19 7/25 0·20 (0·03–1·4) 0·10
Aspirin users 3/43 12/57 0·30 (0·1–1·1) 0·07
Aspirin non-users 22/103 15/86 1·20 (0·7–2·2) 0·50
0·01 0·1 1 10 100
Favours dalteparin Favours control
Figure 2: Subgroup analysis forest plot with risk ratio (95% CI) for the primary composite outcome
The primary composite outcome was major VTE or severe/early-onset pre-eclampsia, SGA infant (<10th percentile), or pregnancy loss. SGA=small for gestational age.
VTE=venous thromboembolism. APLA=anti-phospholipid antibodies.
group), leaving 146 patients assigned to antepartum >40 g/L decrease in haemoglobin at 24 h post-partum)
dalteparin and 143 to no antepartum dalteparin. were similar between groups, as was estimated blood loss
Therefore, for the intention-to-treat analyses, there were at delivery (table 1).
146 women in the antepartum dalteparin group and No participants were lost to follow-up during the
143 in the control group. However, 26 women crossed antepartum period or at labour and delivery. Five of
over within 10 days of randomisation (12 from dalteparin 146 women (3·4%) in the antepartum dalteparin group
to no dalteparin, and 14 from no dalteparin to dalteparin), were non-compliant with antepartum dalteparin (ie, they
and an additional five patients in the treatment group took <80% of the prescribed doses). In the post-partum
were non-compliant with antepartum dalteparin and period, non-compliance with post-partum dalteparin was
were excluded from on-treatment and safety analyses. similar between the groups (9·6% [14/146] in the
Therefore, there were 143 women on antepartum antepartum dalteparin group vs 9·8% [14/143] in the
dalteparin and 141 women on no antepartum dalteparin control group).
for the on-treatment and safety analyses (figure 1). Overall, 52 of 289 randomised women experienced one
The baseline characteristics of the two groups were or more components of the primary composite outcome
similar (table 1). Overall, the mean age of the women was measure (symptomatic major venous thromboembolism,
31·8 years (SD 4·9), mean gestational age at randomisation severe or early onset pre-eclampsia, birth of a small-for-
was 11·9 weeks (4·6), and most participants were white gestational-age infant [<10th percentile], or pregnancy
(91% [262/289]). Most women had either the factor V loss). 25 of 146 (17·1% [95% CI 11·4–24·2%]) had the
Leiden (60% [176/289]) or prothrombin gene mutation primary composite outcome in the antepartum dalteparin
(22% [63/289]). During a mean of 2·2 previous pregnancies group compared with 27 of 143 (18·9% [12·8–26·3]) in the
(SD 1·8) and a mean of 1·0 (1·0) previous deliveries, 61% no antepartum dalteparin group (p=0·70), with a difference
(176/289) of the study population had experienced of −1·8% in favour of dalteparin (95% CI of difference
pregnancy complications. 44% (128/289) of participants –10·6% to 7·1%) (table 2). None of the component
had a risk factor for venous thromboembolism, most of outcomes of the primary composite outcome measure
whom (79% [101/128]) had a first-degree relative with the differed between the two groups (table 2). There were also
disorder. During the study pregnancy, aspirin use was no between-group differences with alternate severity
slightly more common in the control group (difference definitions for these component outcomes (table 2). Three
+10·4% [95% CI −0·5% to 21·3%]) whereas analgesic use patients had symptomatic major venous thromboembolism
was slightly more frequent in the antepartum dalteparin while on dalteparin (two with previous calf deep vein
group (difference +11·6% [−0·4% to 22·8%]). thrombosis had venous thromboembolism during the
The proportions of patients undergoing a caesarean post-partum period and one patient with previous
section or experiencing peri-partum haemorrhage (a provoked proximal deep vein thrombosis and anti-
www.thelancet.com Published online July 25, 2014 http://dx.doi.org/10.1016/S0140-6736(14)60793-5 7
Articles
phospholipid antibodies had venous thromboembolism at mid-1990s led to widespread off-label use of low-molecular-
11 weeks’ gestation while on antepartum dalteparin). Mean weight heparin in pregnant women—both with and
birthweight and gestational age at delivery of livebirths without thrombophilia—who had previous pregnancy
were similar between the groups. complications. This off-label use has been fuelled by the
Our prespecified subgroup analyses showed no emotional consequences of these complications21
significant differences between groups in terms of combined with expert opinion,22,23 consensus panels,24,25
thrombophilia, previous pregnancy complications, and small non-randomised studies suggesting benefit.26–28
previous venous thromboembolism events or risk Antepartum low-molecular-weight herparin is not a
factors, aspirin use, gestational age at enrolment or benign intervention; it can be complicated by heparin-
country, in both intention–to-treat and on-treatment induced thrombocytopenia29,30 (albeit rarely), withholding
See Online for appendix analyses (table 2, figure 2, and appendix). of epidural analgesia, and, as shown in our trial, increased
Although we recorded no differences in major bleeding minor bleeding,14 allergic reactions,14 skin reactions,14 raised
events, more minor bleeding events occurred in the ante- liver transaminase concentrations, and the risk of
partum dalteparin group (19·6% [28/143]) than in the no induction of labour. Additionally, up to 400 subcutaneous
antepartum dalteparin group (9·2% [13/141]; p=0·01) injections of the drug per term of pregnancy is both a
(table 2). No patients had heparin-induced thrombo- personal and financial burden. Clinicians and patients can
cytopenia, changes in bone mineral density, or clinical be reassured that dalteparin use throughout the
fracture. antepartum period does not lead to significant changes in
One patient who received antepartum dalteparin had a bone mineral density. Finally, the continued belief in
left parieto-occipital transient ischaemic attack (expressive ineffective therapy hampers further research for efficacious
aphasia and right visual field loss for 1 h) at 27 weeks’ treatments for women at risk of venous thromboembolism
gestation with no thrombocytopenia. One participant in and pregnancy complications.
the control group had a severe allergic reaction (lip/ We designed the trial to detect a minimal clinically
tongue swelling) after a first dose of post-partum important difference of 16% in the composite primary
dalteparin. Allergic-type skin reactions were noted in outcome (severe or early-onset pre-eclampsia, small-for-
15 participants on dalteparin (nine antepartum and six gestational-age infants <10th percentile, pregnancy loss, or
post partum) and in four participants not on dalteparin major venous thromboembolism). This 16% absolute
(three antepartum and one post partum in a non- difference translates into a number needed to treat of six—
compliant participant). Raised levels of liver enzymes ie, six women would need to inject up to 400 needles per
(aspartate aminotransferase or alanine transaminase)— pregnancy at a drug cost of more than US$8000 per
defined as two-times normal values—were recorded in pregnancy to prevent one outcome. The lower bound of
11 participants on dalteparin (ten antepartum and one the 95% CI of the difference in composite event rates
post partum) and in none of the control participants. between groups in our intention-to-treat analysis (−1·8%
Three neonatal deaths occurred in infants born favouring dalteparin [95% CI of difference –10·6% to
prematurely. One of these deaths occurred in the 7·1%) and in our on-treatment analysis (+2·6% favouring
antepartum dalteparin group (preterm rupture of control [95% CI –6·4 to 11·6%]), excludes a 16% difference
membranes at 24 weeks’ gestation) and two were in the favouring dalteparin; therefore, we can conclude that
control group (preterm rupture of membranes at 24 weeks’ important treatment effects have been excluded. Although
gestation and pre-eclampsia at 30 weeks). Six children in our trial was not designed to detect important differences
pregnancies exposed to antepartum dalteparin had in each individual component of our composite outcome,
congenital anomalies (ankyloglossia [n=2], ectopic kidney, our secondary analyses do not support important treatment
trisomy, strawberry haemangioma, and cataract). Two effects in these outcomes. We noted that in the relevant
children in the control group had congenital anomalies subgroups of women with thrombophilia, such as those
(hemi-vertebrae/scoliosis and duplex renal collecting with previous pregnancy loss, previous pre-eclampsia,
system). previous birth of a small-for-gestational-age infant, and a
family history of venous thromboembolism, antepartum
Discussion dalteparin did not seem to reduce the risk of pregnancy
In our trial, antepartum dalteparin did not reduce the loss, placenta-mediated pregnancy complications, or
risk of either pregnancy loss, venous thromboembolism, venous thromboembolism. Although these secondary and
or placenta-mediated pregnancy complications in subgroup analyses should be interpreted with caution,
pregnant women with thrombophilia at high risk of they suggest that women with thrombophilia should not
pregnancy loss, venous thromboembolism, or placenta- be prescribed low-molecular-weight heparin to prevent
mediated pregnancy complications. these complications unless further research suggests
This trial addresses a key therapeutic question in a large benefit in these subgroups or individual outcomes.
and vulnerable patient group. The absence of benefit is an The strengths of our trial include its generalisability
important finding. The discovery of an association between provided by the multinational design, the strategies used
thrombophilia and pregnancy complications in the to protect against bias (including allocation concealment
8 www.thelancet.com Published online July 25, 2014 http://dx.doi.org/10.1016/S0140-6736(14)60793-5
Articles
from central web randomisation, masked independent
adjudication of all outcome events, and no loss of patients Panel 2: Research in context
to follow-up), and a dosing regimen that ensured Systematic review
prophylactic dose anti-factor Xa activity throughout We did a systematic review and meta-analysis following a systematic review protocol
pregnancy in most women.15 Our primary composite previously published39 and updated in January, 2014, to explore the benefit of
outcome measure included events that are all clinically low-molecular-weight heparin in preventing placenta-mediated pregnancy complications
important, and equal weighting of these events was judged and pregnancy loss. We also added the search terms “venous thrombosis”, “deep vein
appropriate by the investigators and grant reviewers a thrombosis”, and “pulmonary embolism” to explore the benefit of antepartum low-
priori. In view of the fact that women with thrombophilia molecular-weight heparin to prevent venous thromboembolism in thrombophilic women.
who have had previous complications seem to be at higher The latter search identified no trials. We assessed the quality of the evidence with the
risk of all of these complications in subsequent Cochrane Handbook’s risk of bias assessment tool.
pregnancies, and that these complications often overlap, to
study a composite outcome measure in this therapeutic Interpretation
area also seemed to be a sensible and pragmatic approach. Our findings are consistent with previously published high-quality evidence that suggests
Our trial has some limitations. Crossover and non- no benefit of antepartum low-molecular-weight heparin in women with previous
compliance might have led to a reduction in detectable pregnancy loss, women with previous non-severe or late-onset pre-eclampsia, or women
treatment effect. However, crossover was balanced, non- with previous small-for-gestational-age birth between the 5th and 10th percentile. Our
compliance was negligible (3·4% of participants randomised trial is the first to show that thrombophilic women without previous venous
administered <80% of antepartum dalteparin doses), and thrombosis do not benefit from antepartum low-molecular-weight-heparin. Our meta-
our on-treatment sensitivity analysis did not change the analysis shows that lower quality evidence suggests that low-molecular-weight heparin
conclusions of the study. Recruitment challenges led to might prevent recurrent severe placenta-mediated pregnancy complications (severe or
the trial being completed after more than 12 years of early-onset pre-eclampsia, small-for–gestational-age birth <5th percentile, and placental
enrolment and introduce the possibility of time trend or abruption) but we did not record this benefit in the subgroup analyses of our trial.
cohort effects. The characteristics of participants, co-
interventions, or both, might have varied over time and thromboembolism in our trial had a history of calf deep
led to changes in participants’ risk for outcomes. A vein thrombosis or provoked venous thromboembolism.
plausible notion is that the combination of dalteparin with All three women had venous thromboembolism while on
aspirin is effective whereas dalteparin alone is not prophylactic dalteparin (one antepartum and two post-
effective. Indeed, in our subgroup analysis in aspirin partum), and the overall event rate was 3 of 36 (8·3%;
users, antepartum dalteparin trended toward a treatment 95% CI 1·7–22·5%) in the subgroup with previous calf
effect but did not reach significance. Ideally, all patients deep vein thrombosis or previous provoked venous
would have been randomised in early pregnancy to thromboembolism. This finding suggests that these
maximise the possibility that dalteparin could positively patients might need more aggressive prophylaxis.13
affect placental development. Our subgroup analysis of Our subgroup analysis in women with thrombophilia
treatment effect by gestational age at enrolment did not and previous pregnancy loss suggesting no improvement
suggest differential effect but had low power to explore in livebirth rate with low-molecular-weight heparin is
this hypothesis. Future research into higher doses of low- consistent with other multicentre trials that have shown no
molecular-weight heparin with and without aspirin, or increase in livebirth rate with this treatment in unselected
trials that start treatment with low-molecular-weight patients,31–34 women without thrombophilia,34 and in
heparin earlier in pregnancy, might be warranted. women with thrombophilia.35 This finding contrasts with
Our findings need to be considered in the context of the results of three single-centre trials, with a higher risk of
previous trials exploring the benefit of low-molecular- bias, suggesting benefit in women with thrombophilia36
weight heparin to prevent pregnancy-associated venous and without thrombophilia.37,38 Overall, the existing
thromboembolism, recurrent pregnancy loss, and late evidence does not support the use of low-molecular-weight
placenta-mediated pregnancy complications. Our study is heparin to prevent recurrent pregnancy loss.
the first randomised trial to assess the risks and benefits of To analyse the cumulative evidence assessing the use of
low-molecular-weight heparin to prevent pregnancy- low-molecular-weight heparin to prevent recurrent late
associated venous thromboembolism in women with placenta-mediated pregnancy complications (late
thrombophilia (panel 2). None of the pregnant women pregnancy loss, pre-eclampsia, abruption, or small-for-
with thrombophilia without previous distal or provoked gestational-age infants <10th percentile), we updated our
venous thromboembolism had symptomatic major recently published meta-analysis39 with our present
antepartum venous thromboembolism in the control findings (figure 3). This updated meta-analysis suggests a
group (0%, 95% CI 0–2·8%). This result affirms consensus benefit in reducing recurrent late placenta-mediated
guidelines that suggest that women with thrombophilia complications (RR 0·57, 95% CI 0·36–0·91) but showed
without previous venous thromboembolism can have substantial heterogeneity (I²=68%). We did subgroup
antepartum anticoagulant prophylaxis withheld.13 analyses to assess the causes of this heterogeneity. When
However, all three women who had venous we explored the summary effects and heterogeneity in
www.thelancet.com Published online July 25, 2014 http://dx.doi.org/10.1016/S0140-6736(14)60793-5 9
Articles
multicentre trials,40–42 including TIPPS (RR 0·86 [95% CI complications, or venous thrombosis does not reduce the
0·53–1·41]; I²=47%) compared with single-centre trials43–45 occurrence of these complications. Further research is
(0·36 [0·24–0·52]; I²=0%), we noted a reduction in overall needed to establish whether low-molecular-weight heparin
heterogeneity and no clear treatment effect from the reduces the risk of recurrent severe pre-eclampsia,
results of multicentre trials. When we explored trials severely small-for-gestational-age infants (birthweight
registered in a clinical trials registry before completion,40,42 <5th percentile), or placental abruption.
including TIPPS (RR 1·08 [95% CI 0·74–1·60]; I²=0%) Contributors
compared with trials not registered before completion41,43–45 MAR and PSW participated in study design, data collection and
(0·35 [0·25–0·50]; I²=0%), we also noted an important interpretation, writing and critical review of the report, and approval of
the final version. WMH, JK, SRK, AK, EK, and MW participated in study
reduction in heterogeneity and no clear treatment effect design, data collection, critical review of the report, and approval of the
in registered trials. Conversely, when we analysed trials final version. DF* and TR* contributed to study design, data analysis, data
that included only women with previous severe late interpretation, critical review of the report, and approval of the final
placenta-mediated pregnancy complications, at a study version. AMC and GLG participated in data collection, data analysis, data
interpretation, writing and critical review of the report, and approval of
level41,44,45 (RR 0·37 [95% CI 0·25–0·55]; I²=0%) compared the final version. RM participated in data analysis and interpretation,
with trials that included women with previous non-severe critical review of the report, and approval of the final version. MS, SC,
late placenta-mediated pregnancy complications, at a WSC, JS, ER, SR, RK, CD, MJK, SS, KH, JD, GS, SM, JN-A, AM, MK,
study level,40,42,43 including TIPPS (RR 0·80 [95% CI RMS, IAG, KR-M, BM*, NT*, JM*, LO*, MB*, WF*, LM*, PvD*, MP*,
MC*, HC*, PC*, AT*, CC*, and SM* participated in data collection,
0·44–1·46]; I²=68%), we also noted a reduction in critical review of the report, and approval of the final version. CN*
heterogeneity and no clear treatment effect in trials (deceased), PG* (deceased), and RL* (deceased) participated in study
including women with non-severe late placenta-mediated design and data collection. *Denotes members of the TIPPS investigators
pregnancy complications. In summary, higher quality not listed in main author list.
evidence suggests that low-molecular-weight heparin The TIPPS investigators
does not prevent recurrent non-severe placenta-mediated M A Rodger, W M Hague, J Kingdom, S R Kahn, A Karovitch, M Sermer,
A M Clement, S Coat, W S Chan, J Said, E Rey, S Robinson, R Khurana,
pregnancy complications, whereas lower quality evidence C Demers, M J Kovacs, S Solymoss, K Hinshaw, J Dwyer, G Smith,
suggests that low-molecular-weight heparin might S McDonald, J Newstead-Angel, A McLeod, M Khandelwal, R Silver,
prevent recurrent severe placenta-mediated pregnancy G Le Gal, I A Greer, E Keely, K Rosene-Montella, M Walker, P S Wells,
B McCarron, N Thomas, J Martel, C Nimrod (deceased), L Opatrny,
complications. However, given that the latter evidence is
M Blostein, L Magee, P von Dadelszen, M Carrier, R Mallick, T Ramsay,
mainly driven by single-centre unregistered trials, the E Pasquier, D Fergusson, and M Paidas. Data Safety Monitoring Board:
quality of evidence dictates that further research is needed M Cushman (Chair 2007–12), H Clark (Chair 2003–06), P Garner
to explore this hypothesis. Meanwhile, women with and (deceased) (Chair 2000–02), R Lee (deceased), P Callas, A Tinmouth,
C Code, and S McFaul.
without thrombophilia, with previous late-onset and non-
severe pre-eclampsia and previous mildly small-for- Declaration of interests
AM has received honoraria for educational activities from Leo Pharma,
gestational-age infants (birthweight between 5th and 10th
Sanofi, and Bayer. The other authors declare no competing interests.
percentile) should not be offered low-molecular-weight
Acknowledgments
heparin to prevent recurrent pregnancy complications. This study was funded by the Canadian Institutes of Health Research
In conclusion, antepartum prophylactic dose (MCT 82205) and the Heart and Stroke Foundation of Canada (NA 4849).
dalteparin in women with thrombophilia at increased risk Partial start-up funding (US$150 000) and initial study drug were provided
of pregnancy loss, placenta-mediated pregnancy by Pharmacia and UpJohn (2000–02). MR was supported by a Heart and
Stroke Foundation of Ontario Career Investigator Award (CI6225 and
CI7441) and a University of Ottawa Faculty of Medicine Clinical Research
Relative risk Chair in Venous Thrombosis and Thrombophilia. SRK is supported by a
(95% CI)
National Research Scientist award from the Fonds de la Recherche en Santé
Rey et al (2009) 0·35 (0·15–0·79) du Québec. SM is supported by a Canadian Institutes of Health Research
Gris et al (2010) 0·39 (0·21–0·68) New Investigator Award. JK was supported by the Rose Torno Chair.
Gris et al (2011) 0·36 (0·18–0·69) References
Mello et al (2005) 0·30 (0·14–0·60) 1 Rodeghiero F, Tosetto A. The epidemiology of inherited
Martinelli et al (2012) 1·10 (0·55–2·21) thrombophilia: the VITA Project. Vicenza Thrombophilia and
Atherosclerosis Project. Thromb Haemost 1997; 78: 636–40.
de Vries et al (2012) 1·10 (0·63–1·93)
2 Heit JA, Kobbervig CE, James AH, Petterson TM, Bailey KR,
Rodger et al (2014) 1·05 (0·50–2·25) Melton LJ 3rd. Trends in the incidence of venous thromboembolism
Combined (random effects) 0·57 (0·36–0·91) during pregnancy or postpartum: a 30-year population-based study.
Ann Intern Med 2005; 143: 697–706.
0·1 0·2 0·5 1 2 5 3 Gerhardt A, Scharf RE, Beckmann MW, et al. Prothrombin and
Relative risk (95% CI) factor V mutations in women with a history of thrombosis during
pregnancy and the puerperium. N Engl J Med 2000; 342: 374–80.
Figure 3: Meta-analysis of published randomised trials assessing the relative risk reduction (random effects) 4 Berg CJ, Atrash HK, Koonin LM, Tucker M. Pregnancy-related
of recurrent placenta-mediated pregnancy complications with low-molecular-weight heparin in women mortality in the United States, 1987–1990. Obstet Gynecol 1996;
with previous placenta-mediated pregnancy complications 88: 161–67.
Recurrent placenta-mediated complications were defined as any pre-eclampsia, placental abruption, birth of a 5 Stillbirth Collaborative Research Network Writing Group. Causes of
small-for-gestational-age infant (birthweight <10th percentile), or pregnancy loss at more than 20 weeks. death among stillbirths. JAMA 2011; 306: 2459–68.
Previous placenta-mediated complications were pre-eclampsia, birth of a small-for-gestational-age infant 6 van Rijn BB, Hoeks LB, Bots ML, Franx A, Bruinse HW. Outcomes
(birthweight <10th percentile), late pregnancy loss (>12 weeks), or placental abruption. of subsequent pregnancy after first pregnancy with early-onset
preeclampsia. Am J Obstet Gynecol 2006; 195: 723–28.
10 www.thelancet.com Published online July 25, 2014 http://dx.doi.org/10.1016/S0140-6736(14)60793-5
Articles
7 van Walraven C, Mamdani M, Cohn A, Katib Y, Walker M, 27 Grandone E, Brancaccio V, Colaizzo D, et al. Preventing adverse
Rodger MA. Risk of subsequent thromboembolism for patients obstetric outcomes in women with genetic thrombophilia.
with pre-eclampsia. BMJ 2003; 326: 791–92. Fertil Steril 2002; 78: 371–75.
8 Jacobsen AF, Skjeldestad FE, Sandset PM. Ante- and postnatal risk 28 Kupferminc MJ, Fait G, Many A, et al. Low-molecular-weight
factors of venous thrombosis: a hospital-based case-control study. heparin for the prevention of obstetric complications in women
J Thromb Haemost 2008; 6: 905–12. with thrombophilias. Hypertens Pregnancy 2001; 20: 35–44.
9 Pabinger I, Grafenhofer H, Kaider A, et al. Preeclampsia and fetal 29 Huhle G, Geberth M, Hoffmann U, Heene DL, Harenberg J.
loss in women with a history of venous thromboembolism. Management of heparin-associated thrombocytopenia in pregnancy
Arterioscler Thromb Vasc Biol 2001; 21: 874–79. with subcutaneous r-hirudin. Gynecol Obstet Invest 2000; 49: 67–69.
10 Rodger MA, Betancourt MT, Clark P, et al. The association of factor 30 Lepercq J, Conard J, Borel-Derlon A, et al. Venous
V leiden and prothrombin gene mutation and placenta-mediated thromboembolism during pregnancy: a retrospective study of
pregnancy complications: a systematic review and meta-analysis of enoxaparin safety in 624 pregnancies. BJOG 2001; 108: 1134–40.
prospective cohort studies. PLoS Med 2010; 7: e1000292. 31 Visser J, Ulander VM, Helmerhorst FM, et al. Thromboprophylaxis
11 Rey E, Kahn SR, David M, Shrier I. Thrombophilic disorders and for recurrent miscarriage in women with or without thrombophilia.
fetal loss: a meta-analysis. Lancet 2003; 361: 901–08. HABENOX: a randomised multicentre trial. Thromb Haemost 2011;
12 Kupferminc MJ, Eldor A, Steinman N, et al. Increased frequency of 105: 295–301.
genetic thrombophilia in women with complications of pregnancy. 32 Kaandorp SP, Goddijn M, van der Post JA, et al. Aspirin plus
N Engl J Med 1999; 340: 9–13. heparin or aspirin alone in women with recurrent miscarriage.
13 Bates SM, Greer IA, Middeldorp S, Veenstra DL, Prabulos AM, N Engl J Med 2010; 362: 1586–96.
Vandvik PO. VTE, thrombophilia, antithrombotic therapy, and 33 Clark P, Walker ID, Langhorne P, et al, and the Scottish Pregnancy
pregnancy: Antithrombotic Therapy and Prevention of Thrombosis, Intervention Study (SPIN) collaborators. SPIN (Scottish Pregnancy
9th ed: American College of Chest Physicians Evidence-Based Intervention) study: a multicenter, randomized controlled trial of
Clinical Practice Guidelines. Chest 2012; 141 (2 suppl): e691S–736S. low-molecular-weight heparin and low-dose aspirin in women with
14 Greer IA, Nelson-Piercy C. Low-molecular-weight heparins for recurrent miscarriage. Blood 2010; 115: 4162–67.
thromboprophylaxis and treatment of venous thromboembolism in 34 Dolitzky M, Inbal A, Segal Y, Weiss A, Brenner B, Carp H.
pregnancy: a systematic review of safety and efficacy. Blood 2005; A randomized study of thromboprophylaxis in women with
106: 401–07. unexplained consecutive recurrent miscarriages. Fertil Steril 2006;
15 Hunt BJ, Doughty HA, Majumdar G, et al. Thromboprophylaxis 86: 362–66.
with low molecular weight heparin (Fragmin) in high risk 35 Laskin CA, Spitzer KA, Clark CA, et al. Low molecular weight
pregnancies. Thromb Haemost 1997; 77: 39–43. heparin and aspirin for recurrent pregnancy loss: results from the
16 Kramer MS, Platt RW, Wen SW, et al, and the Fetal/Infant Health randomized, controlled HepASA Trial. J Rheumatol 2009; 36: 279–87.
Study Group of the Canadian Perinatal Surveillance System. A new 36 Gris J-C, Mercier E, Quéré I, et al. Low-molecular-weight heparin
and improved population-based Canadian reference for birth weight versus low-dose aspirin in women with one fetal loss and a
for gestational age. Pediatrics 2001; 108: E35. constitutional thrombophilic disorder. Blood 2004; 103: 3695–99.
17 Schulman S, Kearon C, and the Subcommittee on Control of 37 Fawzy M, Shokeir T, El-Tatongy M, Warda O, El-Refaiey AA,
Anticoagulation of the Scientific and Standardization Committee of Mosbah A. Treatment options and pregnancy outcome in women
the International Society on Thrombosis and Haemostasis. with idiopathic recurrent miscarriage: a randomized placebo-
Definition of major bleeding in clinical investigations of controlled study. Arch Gynecol Obstet 2008; 278: 33–38.
antihemostatic medicinal products in non-surgical patients. 38 Badawy AM, Khiary M, Sherif LS, Hassan M, Ragab A, Abdelall I.
J Thromb Haemost 2005; 3: 692–94. Low-molecular weight heparin in patients with recurrent early
18 Friederich PW, Sanson BJ, Simioni P, et al. Frequency of miscarriages of unknown aetiology. J Obstet Gynaecol 2008; 28: 280–84.
pregnancy-related venous thromboembolism in anticoagulant 39 Rodger MA, Carrier M, Le Gal G, et al, and the Low-Molecular-
factor-deficient women: implications for prophylaxis. Weight Heparin for Placenta-Mediated Pregnancy Complications
Ann Intern Med 1996; 125: 955–60. Study Group. Meta-analysis of low-molecular-weight heparin to
19 Lie RT, Rasmussen S, Brunborg H, Gjessing HK, Lie-Nielsen E, prevent recurrent placenta-mediated pregnancy complications.
Irgens LM. Fetal and maternal contributions to risk of pre- Blood 2014; 123: 822–28.
eclampsia: population based study. BMJ 1998; 316: 1343–47. 40 de Vries JIP, van Pampus MG, Hague WM, Bezemer PD,
20 Sibai BM, Ewell M, Levine RJ, et al, and the The Calcium for Joosten JH, and the FRUIT Investigators. Low-molecular-weight
Preeclampsia Prevention (CPEP) Study Group. Risk factors heparin added to aspirin in the prevention of recurrent early-onset
associated with preeclampsia in healthy nulliparous women. pre-eclampsia in women with inheritable thrombophilia: the
Am J Obstet Gynecol 1997; 177: 1003–10. FRUIT-RCT. J Thromb Haemost 2012; 10: 64–72.
21 Rodger MA, Makropoulos D, Walker M, Keely E, Karovitch A, 41 Rey E, Garneau P, David M, et al. Dalteparin for the prevention of
Wells PS. Participation of pregnant women in clinical trials: will recurrence of placental-mediated complications of pregnancy in
they participate and why? Am J Perinatol 2003; 20: 69–76. women without thrombophilia: a pilot randomized controlled trial.
22 Brenner B. Antithrombotic prophylaxis for women with J Thromb Haemost 2009; 7: 58–64.
thrombophilia and pregnancy complications—Yes. 42 Martinelli I, Ruggenenti P, Cetin I, et al, and the HAPPY Study
J Thromb Haemost 2003; 1: 2070–72. Group. Heparin in pregnant women with previous placenta-
23 Lockwood CJ. Inherited thrombophilias in pregnant patients: mediated pregnancy complications: a prospective, randomized,
detection and treatment paradigm. Obstet Gynecol 2002; 99: 333–41. multicenter, controlled clinical trial. Blood 2012; 119: 3269–75.
24 Duhl AJ, Paidas MJ, Ural SH, et al. Antithrombotic therapy and 43 Mello G, Parretti E, Fatini C, et al. Low-molecular-weight heparin
pregnancy: consensus report and recommendations for prevention lowers the recurrence rate of preeclampsia and restores the
and treatment of venous thromboembolism and adverse pregnancy physiological vascular changes in angiotensin-converting enzyme
outcomes. Am J Obstet Gynecol 2007; 197: 457.e1–.e21. DD women. Hypertension 2005; 45: 86–91.
25 Lussana F, Dentali F, Abbate R, et al, and the Italian Society for 44 Gris JC, Chauleur C, Molinari N, et al. Addition of enoxaparin to
Haemostasis and Thrombosis. Screening for thrombophilia and aspirin for the secondary prevention of placental vascular
antithrombotic prophylaxis in pregnancy: Guidelines of the Italian complications in women with severe pre-eclampsia. The pilot
Society for Haemostasis and Thrombosis (SISET). Thromb Res 2009; randomised controlled NOH-PE trial. Thromb Haemost 2011;
124: e19–25. 106: 1053–61.
26 Brenner B, Hoffman R, Carp H, Dulitsky M, Younis J, and the 45 Gris JC, Chauleur C, Faillie JL, et al. Enoxaparin for the secondary
LIVE-ENOX Investigators. Efficacy and safety of two doses of prevention of placental vascular complications in women with
enoxaparin in women with thrombophilia and recurrent pregnancy abruptio placentae. The pilot randomised controlled NOH-AP trial.
loss: the LIVE-ENOX study. J Thromb Haemost 2005; 3: 227–29. Thromb Haemost 2010; 104: 771–79.
www.thelancet.com Published online July 25, 2014 http://dx.doi.org/10.1016/S0140-6736(14)60793-5 11
Comment
TIPPing practice away from anticoagulation in pregnancy
Clinical management of women with a history of adverse comprised the composite primary outcome (severe or
pregnancy outcomes (ie, recurrent early pregnancy early-onset pre-eclampsia, small-for-gestational-age
loss, severe pre-eclampsia, placental abruption, and infants [<10th percentile], pregnancy loss, or venous
unexplained fetal growth restriction or stillbirth) is a thromboembolism); in both intention-to-treat and on-
challenging area in obstetrics because of the paucity treatment analyses; and across pre-planned subgroup
of evidence-based preventive therapies. In the face analyses. From a patient safety perspective, although
Science Photo Library
of emotionally charged requests for preventive treat- no differences in major bleeding or bone mineral density
ment by women with adverse pregnancy outcomes, were recorded, dalteparin was associated with an
clinicians are often tempted to provide non-evidence- increase in minor bleeding, abnormal liver enzymes, and
based therapies that might seem to be both biologically local skin reactions. Published Online
July 25, 2014
plausible and of minimum harm. The TIPPS study design was methodologically http://dx.doi.org/10.1016/
In the 1990s, epidemiological data emerged showing an rigorous. The investigators used pragmatic eligibility S0140-6736(14)60850-3
association between genetic thrombophilias and adverse criteria (which make the results broadly generalisable See Articles
http://dx.doi.org/10.1016/
pregnancy outcomes.1,2 The proposed pathophysiological to pregnant women with thrombophilias), event S0140-6736(14)60793-5
mechanism linking maternal prothrombotic tendencies adjudication was masked, there was no loss to follow-
with adverse pregnancy outcomes is through placental up for the primary outcome, participant adherence to
insufficiency caused by microvascular or macrovascular dalteparin was high, and crossover rates were similar
thrombosis of this crucial maternal–fetal interface. This in the two study groups. The study limitations include
concept led researchers to investigate low-molecular- the low event rates (18·9% events observed vs 49%
weight heparin as a potential treatment to reduce anticipated in the control group), differential use of
placental thrombosis and thereby reduce adverse aspirin between the study groups, slow recruitment
pregnancy outcomes. Early studies showed promising rate, and the small subgroup sizes. However, several
results3,4 and, despite the absence of high-quality important points should be noted. First, the lower than
evidence, clinicians and guideline committees5 quickly anticipated event rate of adverse pregnancy outcomes
adopted use of these drugs. However, subsequent higher is consistent with recent prospective observational data
quality randomised clinical trials6,7 were unable to replicate showing lower (and often non-significant) associations
the success of earlier research. between thrombophilias and adverse pregnancy
The Thrombophilia in Pregnancy Prophylaxis Study outcomes.9 The difference in event rates in TIPPS still
(TIPPS),8 undertaken by Marc Rodger and colleagues reliably excludes the trial’s prespecified minimally
and reported in The Lancet, is the first large international clinically significant difference of 16% (ie, resulting in a
randomised controlled trial designed to resolve the number needed to treat of six).
clinical equipoise of the effect of antepartum low- Second, the rate of aspirin use was higher in the
molecular-weight heparin (dalteparin) on adverse non-dalteparin group (40%) than in the dalteparin
pregnancy outcomes in women at the highest risk of group (30%), especially in women with previous pre-
these outcomes (ie, women with both thrombophilia eclampsia or small-for-gestational-age infants (68%
and a history of either adverse pregnancy outcomes or control vs 41% dalteparin). This finding probably
venous thromboembolism). The results of this study represents the clinicians’ perceived need to intervene
are convincingly negative: following randomisation (because the study was unmasked), but aspirin use is
of 292 women, antepartum dalteparin did not unlikely to have significantly biased the trial results,
significantly reduce the incidence of adverse pregnancy since other large studies have not shown a benefit of
outcomes, the trial’s primary outcome, recorded in aspirin in reducing adverse pregnancy outcomes10,11
25 of 146 women (17·1%) in the dalteparin group versus apart from a minor reduction in pre-eclampsia.12
27 of 143 (18·9%) in the control group (risk difference Third, although the 12-year recruitment period was
–1·8%, 95% CI –10·6 to 7·1). The results were consistent extremely long, treatments for prevention of adverse
across the wide range of clinically important events that pregnancy outcomes did not change substantially
www.thelancet.com Published online July 25, 2014 http://dx.doi.org/10.1016/S0140-6736(14)60850-3 1
Comment
during this period. Fourth, despite the small subgroup *Paul S Gibson, Kara A Nerenberg
sizes, TIPPS showed no statistically significant benefit Departments of Medicine and Obstetrics and Gynecology,
University of Calgary, Calgary, AB, T3L 2Y3, Canada (PSG); and
across any of these subgroups, which is consistent
The Ottawa Hospital Research Institute, University of Ottawa,
with the investigators’ updated systematic review Ottawa, ON, Canada (KAN)
and meta-analysis.8 Finally, caution should be used in gibsonp@ucalgary.ca
interpretation of the subgroup analysis that showed PSG receives an unrestricted educational grant from Sanofi. KN declares no
an apparent non-significant benefit of low-molecular- competing interests.
1 Kupferminc MJ, Eldor A, Steinman N, et al. Increased frequency of genetic
weight heparin in patients who used aspirin, in view of thrombophilia in women with complications of pregnancy. N Engl J Med
the high number of subgroups compared and the small 1999; 340: 9–13.
2 Rey E, Kahn SR, David M, Shrier I. Thrombophilic disorders and fetal loss:
subgroup size. Nonetheless, this latter finding might a meta-analysis. Lancet 2003; 361: 901–08.
merit further research. 3 Gris JC, Mercier E, Quéré I, et al. Low-molecular-weight heparin versus
low-dose aspirin in women with one fetal loss and a constitutional
TIPPS emphasises other important messages for thrombophilic disorder. Blood 2004; 103: 3695–99.
clinicians and researchers. Despite vigorous recruitment 4 Brenner B, Hoffman R, Carp H, Dulitsky M, Younis J. Efficacy and safety of
two doses of enoxaparin in women with thrombophilia and recurrent
efforts, it took more than 12 years to recruit 292 women pregnancy loss: the LIVE-ENOX study. J Thromb Haemost 2005; 3: 227–29.
at 36 centres in five countries. 15 centres did not recruit 5 Bates SM, Greer IA, Hirsh J, Ginsberg JS. Use of antithrombotic agents
during pregnancy: the Seventh ACCP Conference on Antithrombotic and
any participants at all, mainly because the use of low- Thrombolytic Therapy. Chest 2004; 126: 627S–44S.
6 de Vries JIP, van Pampus MG, Hague WM, Bezemer PD, Joosten JH. Low-
molecular-weight heparin had already become local molecular-weight heparin added to aspirin in the prevention of recurrent
standard practice. This situation draws attention to the early-onset pre-eclampsia in women with inheritable thrombophilia: the
FRUIT-RCT. J Thromb Haemost 2012; 10: 64–72.
fact that clinicians’ altruistic intentions to treat these 7 Martinelli I, Ruggenenti P, Cetin I, et al. Heparin in pregnant women with
high-risk women might have inadvertently caused them previous placenta-mediated pregnancy complications: a prospective,
randomized, multicenter, controlled clinical trial. Blood 2012;
minor harm, potentially increased the rates of labour 119: 3269–75.
induction, reduced access to regional anaesthetics, 8 Rodger MA, Hague WM, Kingdom J, et al. Antepartum dalteparin versus no
antepartum dalteparin for the prevention of pregnancy complications in
increased health-care costs (because of the high cost of pregnant women with thrombophilia (TIPPS): a multinational open-label
randomised trial. Lancet 2014; published online July 25. http://dx.doi.
low-molecular-weight heparin), and slowed the research org/10.1016/S0140-6736(14)60793-5.
momentum in this area. Importantly, TIPPS also shows 9 Rodger MA, Betancourt MT, Clark P, et al. The association of factor V Leiden
and prothrombin gene mutation and placenta-mediated pregnancy
that withholding of antepartum low-molecular- complications: a systematic review and meta-analysis of prospective
cohort studies. PLoS Med 2010; 7: e1000292.
weight heparin in women with thrombophilias
10 Kaandorp SP, Goddijn M, van der Post JA, et al. Aspirin plus heparin or
did not significantly increase rates of venous aspirin alone in women with recurrent miscarriage. N Engl J Med 2010;
362: 1586–96.
thromboembolism, which supports recent guidelines 11 Clark P, Walker ID, Langhorne P, et al, on behalf of the Scottish Pregnancy
that advise only post-partum thromboprophylaxis for Intervention Study (SPIN) collaborators. SPIN (Scottish Pregnancy
Intervention) study: a multicenter, randomized controlled trial of
women with anything but the most serious cases of low-molecular-weight heparin and low-dose aspirin in women with
recurrent miscarriage. Blood 2010; 115: 4162–67.
thrombophilia.13
12 Askie LM, Duley L, Henderson-Smart DJ, Stewart LA. Antiplatelet agents for
The TIPPS investigators should be congratulated for prevention of preeclampsia: a meta-analysis of individual patient data.
Lancet 2007; 369: 1791–98.
completing this much needed, rigorous trial, which, along 13 Bates SM, Greer IA, Middeldorp S, Veenstra DL, Prabulos AM, Vandvik PO.
with their updated systematic review and meta-analysis, VTE, thrombophilia, antithrombotic therapy, and pregnancy.
Antithrombotic Therapy and Prevention of Thrombosis, 9th edn: American
clearly shows that low-molecular-weight heparin is College of Chest Physicians Evidence-Based Clinical Practice Guidelines.
ineffective in preventing a wide range of clinically Chest 2012; 141 (2 suppl): e691S–736S.
important adverse pregnancy outcomes in women with
thrombophilia. Hopefully, these results will finally tip
clinicians away from using the drug in this setting and
motivate researchers to pursue other potentially effective
preventive interventions.
2 www.thelancet.com Published online July 25, 2014 http://dx.doi.org/10.1016/S0140-6736(14)60850-3
You might also like
- New England Journal Medicine: The ofDocument10 pagesNew England Journal Medicine: The ofTiffany Rachma PutriNo ratings yet
- Enoxaparin and AspirinDocument11 pagesEnoxaparin and AspirinFemtom PriyoNo ratings yet
- Management of Hereditary Colorectal Cancer: A Multidisciplinary ApproachFrom EverandManagement of Hereditary Colorectal Cancer: A Multidisciplinary ApproachJose G. GuillemNo ratings yet
- Adnexal Masses in Pregnancy: Surgery Compared With ObservationDocument6 pagesAdnexal Masses in Pregnancy: Surgery Compared With ObservationAgustinus FatollaNo ratings yet
- Articles: BackgroundDocument13 pagesArticles: BackgroundDita Putri DamayantiNo ratings yet
- Treatment of Mild Chronic Hypertension During PregnancyDocument12 pagesTreatment of Mild Chronic Hypertension During PregnancyChioma AnowaiNo ratings yet
- Enoxa en Obesas Post-CesareaDocument5 pagesEnoxa en Obesas Post-CesareaKrmnCruzJiménezNo ratings yet
- A Pragmatic, Randomized Clinical Trial of Gestational Diabetes ScreeningDocument10 pagesA Pragmatic, Randomized Clinical Trial of Gestational Diabetes ScreeningWillians ReyesNo ratings yet
- Progestogen TreatmentDocument6 pagesProgestogen TreatmentIndah HaneNo ratings yet
- Good18.Prenatally Diagnosed Vasa Previa A.30Document9 pagesGood18.Prenatally Diagnosed Vasa Previa A.30wije0% (1)
- Association of Biochemical Markers With The Severity of Pre EclampsiaDocument7 pagesAssociation of Biochemical Markers With The Severity of Pre EclampsiaFer OrnelasNo ratings yet
- Aust NZ J Obst Gynaeco - 2022 - Silveira - Placenta Accreta Spectrum We Can Do BetterDocument7 pagesAust NZ J Obst Gynaeco - 2022 - Silveira - Placenta Accreta Spectrum We Can Do BetterDrFeelgood WolfslandNo ratings yet
- Biomarker 2Document8 pagesBiomarker 2Devianti TandialloNo ratings yet
- Medical Record Validation of Maternally Reported History of PreeclampsiDocument7 pagesMedical Record Validation of Maternally Reported History of PreeclampsiezaNo ratings yet
- Faysal Bas It,+86-89-MinDocument4 pagesFaysal Bas It,+86-89-MinIT RSMPNo ratings yet
- Original ArticleDocument4 pagesOriginal ArticlefeyzarezarNo ratings yet
- Placenta PreviaDocument5 pagesPlacenta PreviaKuro HanabusaNo ratings yet
- PIIS2210778916303701Document2 pagesPIIS2210778916303701Fatimah AssagafNo ratings yet
- PIIS0002937821019992Document2 pagesPIIS0002937821019992made dharmaNo ratings yet
- 2021 Article 1541Document6 pages2021 Article 1541bintangNo ratings yet
- VHRM 5 085Document4 pagesVHRM 5 085Agus WijayaNo ratings yet
- Prediction of Recurrent Preeclampsia Using First-Trimester Uterine Artery DopplerDocument6 pagesPrediction of Recurrent Preeclampsia Using First-Trimester Uterine Artery Dopplerganesh reddyNo ratings yet
- Mon 2018Document7 pagesMon 2018Nadieda Ayu MarthalitasariNo ratings yet
- Predictors For Single Agent Resistance in FIGO Score 5 or 6 Gestational Trophoblastic NeoplasiaDocument11 pagesPredictors For Single Agent Resistance in FIGO Score 5 or 6 Gestational Trophoblastic NeoplasiaKim RamirezNo ratings yet
- MJCU Volume 86 Issue December Pages 4259-4265Document7 pagesMJCU Volume 86 Issue December Pages 4259-4265SamarNo ratings yet
- NuevoDocument11 pagesNuevoTatiana AlvarezNo ratings yet
- Avaliação Da Gestação em DownDocument11 pagesAvaliação Da Gestação em DownLene2002No ratings yet
- Mclintock 2011Document9 pagesMclintock 2011rodolfo riosNo ratings yet
- Refluks VuDocument10 pagesRefluks Vuwilliam sitnerNo ratings yet
- Screening For Fetal Chromosomal AbdnormalitiesDocument22 pagesScreening For Fetal Chromosomal AbdnormalitiesAlejandra MurilloNo ratings yet
- Nejme2032499 PDFDocument2 pagesNejme2032499 PDFBladimir CentenoNo ratings yet
- Malaria in Pregnancy 3: SeriesDocument14 pagesMalaria in Pregnancy 3: SeriesLIRYS YULEXI FEIJOO ROJASNo ratings yet
- Atlas TrialDocument12 pagesAtlas Trialgan choon huiNo ratings yet
- A Retrospective Study On Ectopic Pregnancy: A Two Year StudyDocument4 pagesA Retrospective Study On Ectopic Pregnancy: A Two Year StudyGung GiscaNo ratings yet
- Maternal and Perinatal Complications of Severe Preeclampsia in Three Referral Hospitals in Yaoundé, CameroonDocument8 pagesMaternal and Perinatal Complications of Severe Preeclampsia in Three Referral Hospitals in Yaoundé, CameroonIke Istofani KNo ratings yet
- Turner BJOG 2008Document9 pagesTurner BJOG 2008linggaNo ratings yet
- Meijers Heijboer2001Document6 pagesMeijers Heijboer2001Market PlusNo ratings yet
- D-Diamer To Diagnose DVT in PregnancyDocument8 pagesD-Diamer To Diagnose DVT in Pregnancymago1961No ratings yet
- Saudi Pharmaceutical Journal: Original ArticleDocument5 pagesSaudi Pharmaceutical Journal: Original ArticleDicky CaritoNo ratings yet
- Management of Fungal Infections in MCS and Cardiothoracic Organ Transplant Recipients: ISHLT Monograph Series (Volume 12)From EverandManagement of Fungal Infections in MCS and Cardiothoracic Organ Transplant Recipients: ISHLT Monograph Series (Volume 12)No ratings yet
- Frequency of Morbidly Adherent Placenta in Previous Scar: Fakhar Un Nissa, Saira Dars, Shazia Awan, Firdous MumtazDocument5 pagesFrequency of Morbidly Adherent Placenta in Previous Scar: Fakhar Un Nissa, Saira Dars, Shazia Awan, Firdous MumtazprobouNo ratings yet
- Chemotherapy and Immunotherapy in Urologic Oncology: A Guide for the Advanced Practice ProviderFrom EverandChemotherapy and Immunotherapy in Urologic Oncology: A Guide for the Advanced Practice ProviderEdouard J. TrabulsiNo ratings yet
- Hemorragia y EmbrazoDocument6 pagesHemorragia y Embrazoana catalinaNo ratings yet
- Aspirin in The Prevention of Preeclampsia in High Risk WomenDocument11 pagesAspirin in The Prevention of Preeclampsia in High Risk WomenSemir MehovićNo ratings yet
- Stochino Loi2017Document10 pagesStochino Loi2017Maria MogosNo ratings yet
- CTP6 Biosimilar Trastuzumab Lancet Oncol 2017Document12 pagesCTP6 Biosimilar Trastuzumab Lancet Oncol 2017AS Ngọc ÁnhNo ratings yet
- Nej Mo A 1414838Document10 pagesNej Mo A 1414838anggiNo ratings yet
- Lancet Oncol 2013 VermorkenDocument14 pagesLancet Oncol 2013 Vermorkens007972No ratings yet
- Ijgo 12692Document10 pagesIjgo 12692Putri Sari DewiNo ratings yet
- Blood Pressure Evaluation in Children Treated With Laser Surgery For Twin-Twin Transfusion Syndrome at 2-Year Follow UpDocument7 pagesBlood Pressure Evaluation in Children Treated With Laser Surgery For Twin-Twin Transfusion Syndrome at 2-Year Follow UpSelene JuarezNo ratings yet
- Breast Cancer in Young WomenFrom EverandBreast Cancer in Young WomenOreste GentiliniNo ratings yet
- Aogs 12933Document11 pagesAogs 12933Warawiri 11No ratings yet
- 8699 36053 1 PBDocument7 pages8699 36053 1 PBPatrick RamosNo ratings yet
- Association Between Pregnancy and Perinatal Outcomes Among Women With EpilepsyDocument9 pagesAssociation Between Pregnancy and Perinatal Outcomes Among Women With EpilepsyQinthara MuftiNo ratings yet
- Nej Mo A 1113216Document11 pagesNej Mo A 1113216daypranitaNo ratings yet
- Ner Enberg 2017Document7 pagesNer Enberg 2017Ruben Dario Choque CutipaNo ratings yet
- Ecografia para Variedad PresentacionDocument9 pagesEcografia para Variedad PresentacionMagic_OverNo ratings yet
- Fetal Aneuploidy - Screening and Diagnostic TestingDocument8 pagesFetal Aneuploidy - Screening and Diagnostic TestingAngela FernandezNo ratings yet
- Journal Atonia Uteri YuyunDocument6 pagesJournal Atonia Uteri YuyunMoh RamliNo ratings yet
- Ultrasound in Obstet Gyne - 2021 - Fernlund - Reproductive Outcome After Early Miscarriage Comparing Vaginal MisoprostolDocument7 pagesUltrasound in Obstet Gyne - 2021 - Fernlund - Reproductive Outcome After Early Miscarriage Comparing Vaginal MisoprostolPutu Gede WidyatamaNo ratings yet
- ACOBA BiblioDocument2 pagesACOBA BiblioOliver Cortes AcobaNo ratings yet
- NSD Case FormatDocument4 pagesNSD Case FormatIkea BalhonNo ratings yet
- Prenatal Diagnosis and Management of Bronchopulmonary SequestrationDocument16 pagesPrenatal Diagnosis and Management of Bronchopulmonary SequestrationTung PhamNo ratings yet
- Breech Birth NZ Group GuidelinesDocument2 pagesBreech Birth NZ Group Guidelinesapi-223713414No ratings yet
- Appellate 10-09Document93 pagesAppellate 10-09Susannie AcainNo ratings yet
- Postnatal Assessment Lesson PlanDocument12 pagesPostnatal Assessment Lesson PlanDelphy Varghese100% (8)
- No. 373-Cervical Insuf Ficiency and Cervical Cerclage: Sogc Clinical Practice GuidelineDocument15 pagesNo. 373-Cervical Insuf Ficiency and Cervical Cerclage: Sogc Clinical Practice GuidelineGusti Paramartha100% (1)
- Number of Ohio Abortion Drug Complications by AbortionistDocument2 pagesNumber of Ohio Abortion Drug Complications by AbortionistCheryl SullengerNo ratings yet
- Postpartum Haemorrhage: Reference For Questions 1-4: SBA Questions in Obstetrics, Chapter 2, Page 26. (Answer To Q. 1&2)Document23 pagesPostpartum Haemorrhage: Reference For Questions 1-4: SBA Questions in Obstetrics, Chapter 2, Page 26. (Answer To Q. 1&2)Choden JamyangNo ratings yet
- Competency Assessment Module - Obstetric CareDocument17 pagesCompetency Assessment Module - Obstetric CareJeremy HamptonNo ratings yet
- Lesson Plan On Eclampsia: Submitted To Mrs. Cimil Babu Assistant Professor Holi Family College of NursingDocument13 pagesLesson Plan On Eclampsia: Submitted To Mrs. Cimil Babu Assistant Professor Holi Family College of Nursingvarshasharma0580% (5)
- Skenario A Blok 17 L3 FixDocument35 pagesSkenario A Blok 17 L3 FixSelli Novita BelindaNo ratings yet
- OF Jigjiga UniversityDocument22 pagesOF Jigjiga UniversityMatusal ErdachewNo ratings yet
- Edward Syndrome: Submitted byDocument11 pagesEdward Syndrome: Submitted byFrancine RoxasNo ratings yet
- The Endocrine SystemDocument7 pagesThe Endocrine SystemRODGIELYN MAE GEJONNo ratings yet
- Module For Grade 8 - Health (1 Quarter)Document51 pagesModule For Grade 8 - Health (1 Quarter)Alicia FelicianoNo ratings yet
- Physiologic Changes in Pregnancy: 1. UterusDocument14 pagesPhysiologic Changes in Pregnancy: 1. UterusNiña Ricci MtflcoNo ratings yet
- Usapan PDFDocument51 pagesUsapan PDFPerry Bear100% (1)
- Role of Maternal Serum Lactate Dehydrogenase As A Biochemical Marker in Pre-EclampsiaDocument8 pagesRole of Maternal Serum Lactate Dehydrogenase As A Biochemical Marker in Pre-EclampsiaIOSRjournalNo ratings yet
- Module 1 - Framework of Maternal and Child Health Nursing 2023Document12 pagesModule 1 - Framework of Maternal and Child Health Nursing 2023AinaB ManaloNo ratings yet
- Hematologic Disorders in PregnancyDocument34 pagesHematologic Disorders in PregnancyMara Medina - BorleoNo ratings yet
- Cayao-Lasam V Sps RamoleteDocument3 pagesCayao-Lasam V Sps RamoleteGabby GuecoNo ratings yet
- Fcps Guideline Vol.1: Perfect Time For PreparationDocument6 pagesFcps Guideline Vol.1: Perfect Time For PreparationFatima SagguNo ratings yet
- IVF TRAINING For EMBRYOLOGIST & GYNAECOLOGISTDocument3 pagesIVF TRAINING For EMBRYOLOGIST & GYNAECOLOGIST24x7emarketingNo ratings yet
- EArl Case StudyDocument35 pagesEArl Case StudyAna LuisaNo ratings yet
- Textbook of Obstetrics and Gynaecology: A Life Course ApproachDocument51 pagesTextbook of Obstetrics and Gynaecology: A Life Course ApproachAhmad Fitriawan0% (1)
- A Short History of The Real-Time Ultrasound ScannerDocument14 pagesA Short History of The Real-Time Ultrasound ScannerBmet ConnectNo ratings yet
- 19 Nursing Care of A Child With Life Threatening ConditionsDocument31 pages19 Nursing Care of A Child With Life Threatening ConditionsBea Bianca CruzNo ratings yet
- Lesson Plan: Female Hormonal CyclesDocument9 pagesLesson Plan: Female Hormonal CyclesGunaNo ratings yet
- Instructional Planning on Puberty ChangesDocument12 pagesInstructional Planning on Puberty ChangesMerce Tojino ManigosNo ratings yet