Professional Documents
Culture Documents
2023-04-05 12-58
2023-04-05 12-58
Uploaded by
api-6620264730 ratings0% found this document useful (0 votes)
44 views6 pagesCopyright
© © All Rights Reserved
Available Formats
PDF or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
0 ratings0% found this document useful (0 votes)
44 views6 pages2023-04-05 12-58
2023-04-05 12-58
Uploaded by
api-662026473Copyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
You are on page 1of 6
Assessment and Concept Map Care Plan
for
Critical Care Patient
Created by
KayLynn Rounds
Nursing Student
‘Youngstown State University
P. Schuster, Concept Mapping: A Critical Thinking Approach, Davis, 2002.
ey Problet
Impaired Gas Exchange
sip:
Raise HOB
Chest physiotherapy
AIC vent
Hypoxemia
PEEP 10
ABG’S
Propofol 35mg,
Excessive thick white secretions
‘Trach 8mm.
Reason for Needing Health Care
Key Problem
i Dw/Surgery)
Risk for Impaired Skin
Integrity
a found unconscious inthe field. Due Impaired Physical
‘to gun shots in the cranium. Patient
Intubated while in field. Craniotomy upon,
admission to SICU. a
24 yo female, Full Code, NKA Ineffective tissue perfusion
[Impaired skin integrity
Loc
Bed Rest
A 4 + 1 sided cranial wound
See eae Le
Risk for Infection
Key Problem
Risk for Aspiration
Ineffective tissue perfusion
Sedation
Poor nutrition
Key Problem
Risk for Ineffective Breathing Pattern
SD:
Urine analysis /cuture & -—J}
sensitivity
Ineffective tissue perfusion
SD:
Ventilator rate 14
‘Thick white secretions
7} Patent is sedated
oor nutrition |
Inactive Decreased LOC | Prepoft
L sided cranial wound Trach
Pain ‘Increased ICP
Sedated Patient Respiratory Rate 14
GCS 10
Nonsterile intubation
P. Schuster, Concept Mapping: A Critical Thinking Approach, Davis, 2002.
: Ineffective Airway Clearance
General Goal: Effective Airway Clearance
Re
Predicted Behavioral Outcome Objective (s): The patient will...
ventilator settings without having any issues...on the day of care
‘Nursing Interventions Patient Responses
1. Suction PRN 1. Coughing, no gag
2. Q2 tums 2. Patient occasionally moved on her
3. Assess breath sounds ‘own but maintained position most of
4. Assess mouth and nose the time.
5. Maintain HOB elevated 30 3. Diminished clear breath sounds
degrees 4. No signs of occlusion
6. Monitor oxygenation status 5. HOB elevated, tolerated well
6. SpO2 maintained in normal limits.
Evaluation of outcome objectives: Outcome met. Patient maintained ventilator settings
and was stable during my shift.
Problem #2 _; Impaired gas exchange
General Goal: Improved gas exchange
Predicted Behavioral Outcome Objective (s): The patient will... maintain an SpO2
greater than 95% and ABG’s within or close to normal limits...on day of care
‘Nursing Interventions Patient Responses
1. Continuous monitor of SpO2 1, Sp02 maintained >95%
2. Monitor ABG’s 2. ABG’s improving since admission
3. Keep HOB elevated 30-45 degrees 3. HOB elevated
4, Assess for diaphragmatic breathing 4. Pt. wasn’t using accessory muscles
Evaluation of outcome objectives: Outcome met. Patient maintained SpO2 > 95% and
ABG’s are near normal more than before.
P. Schuster, Concept Mapping: A Critical Thinking Approach, Davis, 2002.
Problem # 3 ___: Risk for Aspiration
General Goal: Free of aspiration
Predicted Behavioral Outcome Objective (s): The patient will... be able to avoid
aspiration and pneumonia... on the day of care.
‘Nursing Interventions Patient Responses
1. Assess trach placement 1. Trach midline
2. Suction PRN 2. Cough, no gag
3. HOB elevated 30-45 degrees 3. HOB elevated
4. Assess cough and gag reflex 4, Cough present, no gag
5. Medication 5. Patient receiving UNASYN
Evaluation of outcome objectives: Outcome met. Patient didn’t aspirate during my shift.
Problem #_4__; Risk for Ineffective Breathing Pattern
General Goal: Allow the patient to have slow and controlled breaths
Predicted Behavioral Outcome Objective (s): ‘The patient will... Maintain a slow and
controlled breathing pattern...on day of care.
‘Nursing Interventions Patient Responses
1. Co
nuous monitor of SpO2 1. SpO2 maintained >95%
2. Monitor ABG’s 2. ABG’s improving since admission
3. Keep HOB elevated 30-45 degrees 3. HOB elevated
4. Assess for diaphragmatic breathing 4. Pt. wasn’t using accessory muscles
5. Assess pain/anxiety 5. Patient on pain/anxiety meds
Evaluation of outcome objectives: Outcome met. Patient maintained normal breaths while
on the ventilator with minimal signs of anxiety.
P. Schuster, Concept Mapping: A Critical Thinking Approach, Davis, 2002.
Problem # _5__: Risk for Infection
General Goal: Keep pt. free from infection.
Predicted Behavioral Outcome Objective (8): The patient will... remain free of signs and
symptoms of infection on the day of care.
Nursing interventions
1. Assess trach 1. Trach clean and in place
2. Suction PRN 2. Cough, no gag
3. HOB clevated 30-45 degrees 3. Dec. lung secretions
4, PIN 4, Nutrition through PEG
5. Medication 5. Tolerating medication
6. Chest physiotherapy 6. Pt’s lungs remain clear
Evaluation of outcome objectives: Outcome met patient remained free of bacteria and
infection during my shift
Problem #6: Risk for Impaired Skin Integrity
General Goal: Keep my patient free from skin breakdown.
Predicted Behavioral Outcome Objective (s): ‘The patient will... remain free of skin
breakdowns...on day of care.
‘Nursing Interventions Patient Responses
1. 2QH tums 1, No redness or breakdowns
2. Skin Assessment 2. Pt. shows no signs of breakdown or
redness
3. assess nutritional status 3. Pt. receiving continuous tube feed
4. 1V fluids 4. Hydration being maintained
Evaluation of outcome objectives: Outcome met. Patients skin remained intact and free
from redness / breakdown during my day of care.
P. Schuster, Concept Mapping: A Critical Thinking Approach, Davis, 2002.
Problem #_7__: Impaired Physical Mobility
General Goal: Improve physical mobility
Predicted Behavioral Outcome Objective (5): The patient will...do ROM exercises with
the me to decrease atrophy on the day of care.
‘Nursing Interventions Patient Responses
1. Pain Assessment 1. CPOT scaled = not aggravated or
anxious
2. IV fluids 2. Hydration being maintained
3. HOB elevated 30-45 degrees 3. easy respirations
4. Nasal cannula 4, ine. oxygenation so pt. isn’t out of
5. Anxiety medication breath.
5. Pt. tolerated
Evaluation of outcome objectives: Outcome not met. Tried getting patient to help with
ROM exercises. Pt. too sedated and worn out to help. Student nurses picked up extremities
and did as much as possible until resistance was met on day of care.
P. Schuster, Concept Mapping: A Critical Thinking Approach, Davis, 2002.
You might also like
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5813)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (844)
- In Vitro FertilizationDocument13 pagesIn Vitro Fertilizationapi-662026473No ratings yet
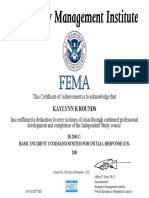
- Fema 200 CertDocument1 pageFema 200 Certapi-662026473No ratings yet
- Certificate 2Document1 pageCertificate 2api-662026473No ratings yet
- Windshield SurveyDocument6 pagesWindshield Surveyapi-662026473No ratings yet
- Resume KRDocument1 pageResume KRapi-662026473No ratings yet