Professional Documents
Culture Documents
Case 126:: Extramedullary Hematopoiesis
Uploaded by
Vo VũOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Case 126:: Extramedullary Hematopoiesis
Uploaded by
Vo VũCopyright:
Available Formats
Note: This copy is for your personal non-commercial use only.
To order presentation-ready
copies for distribution to your colleagues or clients, contact us at www.rsna.org/rsnarights.
DIAGNOSIS PLEASE
Case 126: Extramedullary
Hematopoiesis1
䡲 CASE 126
Yahya M. Berkmen, MD†
History A 63-year-old man was admitted with a history of gradually
Benjamin A. Zalta, MD
increasing abdominal pain of 3 days duration. At admis-
sion, the pain was mostly localized to the right upper
quadrant. The patient had a slightly elevated white blood
cell count (10 ⫻ 109/L). The clinical impression of acute
cholecystitis was confirmed with ultrasonography and
computed tomography (CT). Several gallstones were also
depicted, and cholecystectomy was performed. Chest CT
studies were obtained postoperatively to evaluate an ab-
normality seen on the admission chest radiograph.
biliary tree on a lower section obtained
Imaging Findings
through the midportion of the liver.
The posteroanterior chest radiograph There were surgical clips in the left up-
obtained at admission (Fig 1) showed a per quadrant of the abdomen and the
smoothly outlined mass posterior to the spleen was absent, indicating previous
heart on the left side of the body. There splenectomy.
was also the hint of a retrocardiac opac-
ity on the right side. The heart was mod-
Discussion
erately enlarged. Contrast material–en-
hanced CT of the chest was performed Extramedullary hematopoiesis (EMH) is
after cholecystectomy and revealed the proliferation of hematopoietic cells
inhomogeneously enhancing bilateral outside of the bone marrow in response
paraspinal masses in the lower half of to production of too few blood cells to
the thorax (Fig 2). Air was visible in the satisfy the body’s demand. This insuffi-
cient production is caused by either
bone marrow replacement disease (my-
Figure 1 elofibrosis or chronic myelogenous leu-
kemia) or hemolytic anemia (thalasse-
mia, sickle cell anemia, or hereditary
spherocytosis).
The findings of experimental studies
Part one of this case appeared 4 months previously and may indicate that the organs develop from
contain larger images. specialized cells differentiated from one
Published online
totipotent cell but retain their ability to
10.1148/radiol.2453040715 dedifferentiate and proliferate into yet
another cell group. This explains how
Radiology 2007; 245:905–908
neural cells can be generated from bone
1
From the Department of Radiology, Columbia University marrow cells (1) and how muscle can be
Medical Center, 177 Fort Washington Ave, Milstein Hospi- regenerated by bone marrow– derived
tal Bldg, MC 3, New York, NY 10032. Received April 22, myogenic progenitors (2). Conversely,
2004; revision requested June 29; revision received July
muscles and neural tissues can be in-
9; final version accepted July 28. Address correspon- Figure 1: Posteroanterior chest radiograph
dence to B.A.Z. (e-mail: baz2101@columbia.edu).
duced to produce hematopoietic cells
obtained at admission. There is a smoothly out- under certain experimental conditions
Authors stated no financial relationship to disclose. lined mass (arrow) posterior to the heart on the left (3). It appears that “subpopulations of
†
side of the body. There is also suggestion of a cells within specific tissues may remain
Deceased.
retrocardiac opacity on the right side of the body.
unrestricted and possess pluripotent
姝 RSNA, 2007
The heart is moderately enlarged.
potential that is reminiscent of embry-
Radiology: Volume 245: Number 3—December 2007 905
DIAGNOSIS PLEASE: Extramedullary Hematopoiesis Berkmen and Zalta
onic stem cells” (3). Extrusion of bone gland (10), middle ear (11), spine (12), nodes can be found in patients with
marrow through a defect of severely paratracheal region (13), abdomen Castleman disease (24). Typically, they
thinned and attenuated cortex of the (14), and pelvis (15). enhance homogeneously and intensely
vertebrae or ribs in individuals with he- Intrathoracic EMH may manifest as and frequently have calcifications (24),
molytic anemias may be another mech- a paraosseous mass, interstitial pulmo- although inhomogeneous or ringlike en-
anism for development of EMH (4,5). nary abnormality, pleural mass, or he- hancement has been reported in rare in-
The liver, spleen, kidney, lymph mothorax, either alone or in combina- stances (24,25). Calcification in patients
nodes, and posterior mediastinum are tion. Paraosseous EMH is the most com- with EMH is demonstrated extremely
the most common sites of EMH, with mon manifestation of intrathoracic EMH. rarely (18,21). In tuberculosis, the lymph
EMH often occurring in more than one It appears as a small or large mass adja- nodes commonly enhance peripherally
site, although instances of isolated he- cent to the vertebrae (frequently bilater- (26); in lymphomas, enhancement is
patic (6) and renal (7) EMH have been ally), ribs (commonly multiple ribs), or usually faint and homogeneous. Neuro-
reported. EMH also may occur in un- both. These masses are usually asymp- genic tumors of the posterior mediasti-
common locations, such as the skin (8), tomatic and may be discovered inciden- num commonly have erosions or defects
central nervous system (9), adrenal tally (16,17). If specific clinical features of the vertebrae, ribs, or both and may
and radiologic evidence of myelofibrosis show moderate homogeneous contrast
or hemolytic anemia are present, this enhancement.
Figure 2 disease is easy to diagnose. In the ab- Involvement of the pulmonary inter-
sence of specific bone changes associ- stitium with hematopoietic cells causes
ated with the underlying disease (my- severe and often fatal respiratory failure
elofibrosis or anemia), the diagnosis can and rarely occurs (19,27). Chest radio-
be established with percutaneous fine- graphic findings are described as “inter-
needle aspiration (16,18), open biopsy stitial lung infiltrates” (27). EMH masses
(14,19), or thoracoscopic biopsy (20) may form in the pleura and may be com-
in uncertain cases. EMH usually re- plicated by hemothorax (28).
gresses or disappears after treatment Hereditary spherocytosis is one of
with blood transfusion and hydroxyurea several forms of congenital hemolytic
(14), splenectomy in cases of spherocy- anemia. The erythrocytes acquire a spher-
tosis (21), or radiation therapy (13,19). ical shape because of a molecular defect
Chest radiography reveals a sharply in one of the proteins of the red cell
outlined, smooth, or lobulated (17) membrane. Clinical findings are ane-
paraspinal or rib mass(es). Paraspinal mia, jaundice, and splenomegaly. Gall-
EMH may be an isolated (16,17) or ex- stones occur frequently. Splenectomy is
tensive mediastinal mass (5), or it may the treatment of choice. With improve-
be contiguous with abdominal paraspi- ment of the anemia, EMH regresses or
nal masses of EMH (14). These lesions disappears. However, occasional per-
homogeneously enhance on CT scans sistence of EMH after splenectomy, as
obtained with intravenous contrast ma- occurred in this patient, has been re-
terial because of their high vascularity ported (21). In conclusion, the combi-
(22). Iron deposition and fat infiltration nation of inhomogeneously enhancing
may occur in long-standing lesions (22), bilateral paraspinal masses at CT in a
and CT reveals an inhomogeneous con- patient with gallstones and previous
trast-enhanced mass, as in this case. splenectomy makes EMH the most
Inhomogeneity of the mass may be evi- likely diagnosis.
dent even without contrast enhacement
(21). Magnetic resonance imaging (22,23) References
and technetium 99m sulfur colloid scan- 1. Bjornson CR, Rietze RL, Reynolds BA, Magli
ning (18) are often useful diagnostic im- MC, Vescovi AL. Turning brain into blood: a
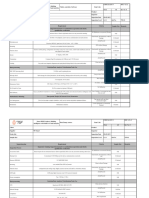
Figure 2: Transverse contrast-enhanced CT aging modalities. haematopoietic fate adopted by adult neural
images of the chest obtained after cholecystec- Inhomogeneously enhancing bilat- stem cells in vivo. Science 1999;283:534 –
tomy. (a) Inhomogeneously enhancing bilateral eral paravertebral masses in patients 537.
paraspinal masses (M) at the lower end of the with myelofibrosis or hemolytic anemia 2. Ferrari G, Cusella-De Angelius G, Coletta M,
thorax. (b) Lower section obtained through the are highly indicative of EMH. These et al. Muscle regeneration by bone-marrow-
middle of the liver. Surgical clips in the left upper masses have to be differentiated from derived myogenic progenitors. Science
quadrant (arrowhead) and absence of the spleen 1998;279:1528 –1530.
lymphadenopathy and neurogenic tu-
are evident. mors. Large posterior mediastinal lymph 3. Jay KE, Gallacher L, Bhatia M. Emergence of
906 Radiology: Volume 245: Number 3—December 2007
DIAGNOSIS PLEASE: Extramedullary Hematopoiesis Berkmen and Zalta
muscle and neural hematopoiesis in humans. a paraspinal chest mass. Chest 2003;124: Individual responses
Blood 2002;100:3193–3202. 732–734.
Jaleel P. Abdul, MD, Dammam, Saudi Arabia
4. Case records of the Massachusetts General Amr M. Ajlan, MBBS, Montreal, Quebec, Can-
18. Bolaman Z, Polatli M, Çilda ð O, Kadýköylü
Hospital. Weekly clinicopathological exer- ada
G, Çulhac ý N. Intrathoracic extramedullary
cises, case 3-1968. N Engl J Med 1968;278: Oguz Akin, MD, New York, NY
hematopoiesis resembling posterior medias-
782–791. tinal tumor. Am J Med 2002;112:739 –740. Erhan Akpinar, Ankara, Turkey
Roger L. Antonelli, MD, Dayton, Ohio
5. Hanford RB, Schneider GF, McCarthy JD. 19. Weinschenker P, Kutner JM, Salvajoli JV, Fahad Azzumeea, MBBS, Montreal, Quebec,
Massive thoracic extramedullary hematopoi- et al. Whole-pulmonary low-dose radiation Canada
esis. N Engl J Med 1960;263:120 –123. therapy in agnogenic myeloid metaplasia Asim K. Bag, MD, Birmingham, Ala
with diffuse lung involvement. Am J Hematol Ronald L. Becker, MD, Rolling Hills, Calif
6. Gupta P, Naran A, Auh YH, Chung JS. Focal
2002;69:277–280. Bryan D. Berkey, MD, Tripler AMC, Hawaii
intrahepatic extramedullary hematopoiesis
J. Scott Bolton, MD, Dothan, Ala
presenting as fatty lesions. AJR Am J Roent-
20. Ng CS, Wan S, Lee TW, et al. Video-assisted Ronald N. Boyle, MD, La Plata, Md
genol 2004;182:1031–1032.
thoracic surgery for mediastinal extramedul- Eric L. Bressler, MD, Minnetonka, Minn
7. Choi H, David CL, Katz RL, Podoloff DA. lary haematopoiesis. Ann R Coll Surg Engl Douglas C. Brown, MD, Virginia Beach, Va
Case 69: extramedullary hematopoiesis. Ra- 2002;84:161–163. Marcelo Cabrini, Lomas de Zamora, Argentina
diology 2004;231:52–56. Chris E. Chernesky, MD, Springfield, Mo
21. Xiros N, Economopoulos T, Papageorgiou E, Michael H. Childress, MD, Silver Spring, Md
8. Rogalski C, Paasch U, Friedrich T, Haustein Mantzios G, Raptis S. Massive hemothorax Alex T. Chuang, MD, Dallas, Tex
UF, Sticherling M. Cutaneous extramedul- due to intrathoracic extramedullary hemato- Ming-Tsung Chuang, MD, Kaohsiung, Taiwan
lary hematopoiesis in idiopathic myelofibro- poiesis in a patient with hereditary spherocy- Neal R. Conti, MD, Seattle, Wash
sis. Int J Dermatol 2002;41:883– 884. tosis. Ann Hematol 2001;80:38 – 40. Gonzalo L. Cortes, MD, Bilbao, Vizcaya, Spain
9. Ayyildiz O, Isikdogan A, Celik M, Muftuoglu Marco A. Cura, MD, San Antonio, Tex
22. Georgiades CS, Neyman EG, Francis IR,
E. Intracranial meningeal extramedullary he- Paxton H. Daniel, MD, Fort Worth, Tex
Sneider MB, Fishman EK. Typical and atypi-
matopoiesis inducing serious headache in a Marc G. De Baets, MD, Collina d’Oro, Switzer-
cal presentations of extramedullary hemato-
patient with idiopathic myelofibrosis. J Pedi- land
poiesis. AJR Am J Roentgenol 2002;179:
atr Hematol Oncol 2004;26:28 –29. Peter De Baets, Damme, Belgium
1239 –1243.
Johannes F. De Villiers, MBChB, MMed, Gis-
10. Calhoun SK, Murphy RC, Shariati N, Jacir borne, New Zealand
23. Tunaci M, Tunaci A, Engin G, et al. Imaging
N, Bergman K. Extramedullary hematopoie- Thaworn Dendumrongsup, MD, Songkla, Thai-
features of thalassemia. Eur Radiol 1999;9:
sis in a child with hereditary spherocytosis: land
1804 –1809.
an uncommon cause of an adrenal mass. Pe- Bart D’herde, Hasselt, Belgium
diatr Radiol 2001;31:879 – 881. 24. McAdams HP, Rosado-de-Christenson M, Seyed A. Emamian, MD, PhD, Rockville, Md
Fishback NF, Templeton NF. Castleman’s Juliet H. Fallah, MD, Clarendon Hills, Ill
11. Aronsohn MS, Antonelli PJ, Mancuso A. Ex-
disease of the thorax: radiologic features Susan M. Fanapour, DO, Lombard, Ill
tramedullary hematopoiesis presenting as a
with clinical and histopathologic correlation. Virginia Fattal Jaef, MD, Rosario, Argentina
middle ear mass. Otol Neurotol 2003;24:
Radiology 1998;209:221–228. Mario Fava, MD, Miami, Fla
963–964.
Luis G. Ferrer, MD, Valencia, Spain
12. de Haas KP, van de Loosdrecht AA, Daenen 25. Chaloupka JC, Castillo M, Hudgins P. Castle- Angeles Franco Lopez, Madrid, Spain
SM. Intraspinal extramedulary haemato- man disease in the neck: atypical appearance Akira Fujikawa, MD, Setagaya, Tokyo, Japan
poiesis in a patient with myelofibrosis. Neth on CT. AJR Am J Roentgenol 1990;154(5): Ann S. Fulcher, MD, Midlothian, Va
J Med 2002;60:256 –259. 1051–1052. Marcelo B. Funari, MD, São Paulo, Brazil
Rajneesh Galwa, Jaipur, India
13. Kurtman C, Ozbilgin MK, Andrieu MN, 26. Im JG, Song KS, Kang HS, et al. Mediastinal
Ram P. Galwa, MD, Chandigarh, India
Celebioglu B. Paratracheal extramedullary tuberculous lymphadenitis: CT manifesta-
Gilles Genin, Annecy, France
hematopoiesis. Int J Hematol 2001;73:492– tions. Radiology 1987;164:115–119.
Carlos R. Gimenez, MD, New Orleans, La
495. Ferris Ginsberg, DO, Ocean, NJ
27. Yusen RD, Kollef MH. Acute respiratory fail-
14. Horwood E, Dowson H, Gupta R, Kaczmarski R, ure due to extramedullary hematopoiesis. Francisco Jose Gonzalez, Santander, Spain
Williamson M. Myelofibrosis presenting as spi- Chest 1995;108:1170 –1172. Bruno Miguel Graca, MD, Coimbra, Portugal
nal cord compression. J Clin Pathol 2003;56: Aleksandar Grgic, MD, Zweibruecken, Germany
154–156. 28. Kupferschmid JP, Shahian DM, Villanueva Dan G. Gridley, MD, Phoenix, Ariz
AG. Massive hemothorax associated with in- Flavius F. Guglielmo, MD, Basking Ridge, NJ
15. Miyake H, Matsuda M, Iyomasa S, Mizuno trathoracic extramedullary hematopoiesis Pramod K. Gupta, MD, Plano, Tex
K. Presacral extramedullary hematopoiesis. involving the pleura. Chest 1993;103:974 – Adam R. Guttentag, MD, Philadelphia, Pa
Surgery 2004;135:112–113. 975. Ehsan A. Haider, MBBCh, Montreal, Quebec,
Canada
16. Al-Marzooq YM, Al-Bahrani AT, Chopra R,
Al-Momatten MI. Fine-needle aspiration bi-
Congratulations to the 150 individuals Ferris M. Hall, MD, Brookline, Mass
and nine resident groups that submitted Clare M. Hartigan, MBBCh, London, United
opsy diagnosis of intrathoracic extramedul-
Kingdom
lary hematopoiesis presenting as a posterior the most likely diagnosis (extramedul-
John J. Hines, Jr, MD, Huntington, NY
mediastinal tumor in a patient with sickle- lary hematopoiesis) for Diagnosis Please, Hideki Hyodoh, MD, Sapporo, Hokkaido, Japan
cell disease: case report. Diagn Cytopathol Case 126. The names and locations of the Alberto C. Iaia, MD, Wilmington, Del
2004;30:119 –121.
individuals and resident groups, as sub- Teeranan Intharapat, MD, Hat-Yai, Songkhla,
17. Lall C, Payne DK. A patient with anemia and mitted, are as follows: Thailand
Radiology: Volume 245: Number 3—December 2007 907
DIAGNOSIS PLEASE: Extramedullary Hematopoiesis Berkmen and Zalta
Rathachai Kaewlai, MD, Boston, Mass Hiroshi Nobusawa, MD, PhD, Ota, Tokyo, Japan Osman Temizoz, Edirne, Turkey
Kiriakos Kalampoukas, MD, Halandri, Greece Anietie E. Okon, MD, North Liberty, Iowa Eugene Tong, MD, Austin, Tex
Andrew J. Kapustin, MD, Charlotte, NC Laura Oleaga, Philadelphia, Pa Vaiman S. Tsang, MD, Holtsville, NY
Ashok Katti, MD, Warrington, Cheshire, United Cinthia D. Ortega, MD, São Paulo, Brazil Baris I. Turkbey, MD, Baltimore, Md
Kingdom Klaus Orth, Aachen, Germany Unni K. Udayasankar, MD, FRCR, Atlanta, Ga
Takuji Kiryu, MD, PhD, Gifu, Japan Marc G. Ossip, MD, Toronto, Ontario, Canada Eleni Vafeiadou, Thessaloniki, Greece
Steven A. Klein, MD, Shrewsbury, Mass Neeraj J. Panchal, MD, San Diego, Calif Piet K. Vanhoenacker, MD, Moorsel, Belgium
Arlene M. Klink, MD, MS, Irvine, Calif David M. Panicek, MD, New York, NY Elida Vazquez, MD, Barcelona, Spain
Stefanos Lachanis, Athens, Greece Matteo Passamonti, MD, Lodi, Italy Nanda Venkatanarasimha, MBBS, MRCP, Ply-
Alexis Lacout, MD, Paris, France Narendrakumar P. Patel, MD, Newburgh, NY mouth, United Kingdom
James F. Lally, MD, Wallingford, Pa Suresh K. Patel, MD, Chicago, Ill Ricardo Luis Videla, Córdoba, Argentina
Martin Lecompte, MD, Manotick, Ontario, Yeliz Pekcevik, Izmir, Turkey Christopher P. Vittore, MD, Belvidere, Ill
Canada Nicola Pelosi, Palmanova, Italy Ivan Vollmer, MD, Barcelona, Spain
Karl J. Lehmann, MD, Karlsruhe, Germany Ivan Pilate, Brussels, Belgium Michael Weber, MD, Berlin, Germany
Myron M. Levitt, MD, Scotch Plains, NJ Rubem Pochaczevsky, MD, Bronx, NY Jeffrey H. West, MD, Jacksonville, Fla
Donald R. Lewis, Jr, MD, Huntington, WVa Ilias Primetis, MD, Athens, Greece Satoru Yoshida, Muroran, Hokkaido, Japan
John T. Lim, MD, Newport Coast, Calif Daniel C. Rappaport, MD, Toronto, Ontario, Kaneko You, Gifu, Japan
Eric D. Lindgren, MD, Grand Rapids, Mich Canada Stanko Yovichevich, MD, Sydney, Australia
David A. Lisle, MBBS, Brisbane, Australia Matthew C. Rheinboldt, MD, Nashville, Tenn Joe Yut, Olathe, Kan
Jaime Llauger, MD, Barcelona, Spain Carla F. Ribeiro, MD, Viseu, Portugal
Edward Lubat, MD, Englewood, NJ Walter S. Rose, MD, Oakhurst, NJ
Michael B. Martin, MD, Austin, Tex Arnold J. Rotter, MD, Los Angeles, Calif
Resident group responses
Daniel L. Martins, MD, São Paulo, Brazil Tsutomu Sakamoto, MD, Tokyo, Japan
Andrew C. Mason, MBBCh, Vancouver, British Roberto Q. Santos, MD, Rio de Janeiro, Brazil Baylor University Medical Center Radiology Res-
Columbia, Canada Debra M. Sarasohn, MD, New York, NY idents, Dallas, Tex
Satoshi Matsushima, MD, Tokyo, Japan Anthony J. Scuderi, MD, Johnstown, Pa Fukushima University Radiology Residents, Fuku-
Waldir H. Maymone, MD, Rio de Janeiro, Brazil Hidekazu Seo, MD, Hamamatsu, Shizuoka, shima, Japan
Frank J. McKowne, MD, Vancouver, Wash Japan Fundacion Jimenez Diaz Radiology Residents,
Sunil L. Mehta, MD, Mississauga, Ontario, Matthew P. Shapiro, MD, Charlottesville, Va Madrid, Spain
Canada Hideki Shima, MD, Tokyo, Japan Hospital Italiano Cordoba Radiology Residents,
Jose M. Mellado Santos, Tudela, Navarra, Spain Grady V. Shue, Jr, MD, Hickory, NC Cordoba, Argentina
Flavia Mendez, MD, Porto Alegre, Brazil Ana C. Silva, MD, Porto, Portugal Hospital das Clinicas da Faculdade de Medicina
Michael P. Meyers, MD, Winnipeg, Manitoba, Annamaria Skacelova, MD, Veazie, Me da Universidade de São Paulo Radiology
Canada Darrin S. Smith, MD, Visalia, Calif Residents, São Paulo, Brazil
Nikolaos Michailidis, Thessaloniki, Greece Annemie Snoeckx, MD, Zandhoven, Belgium Kaohsiung Medical University Radiology Resi-
Manabu Minami, MD, PhD, Yokohama, Japan Luis A. Sosa, Jr, MD, Mexico City, Mexico dents, Kaohsiung, Taiwan
Mansour Mirfakhraee, MD, Shreveport, La James D. Sprinkle, Jr, MD, Spotsylvania, Va Prince of Songkla University Radiology Resi-
Tammam N. Nehme, MD, East Wenatchee, Paul Stark, La Jolla, Calif dents, Songkla, Thailand
Wash Evan Stein, MD, PhD, New York, NY University of Pennsylvania Radiology Residents,
Christopher C. Ng, MD, Nashville, Tenn Subramanian Subramanian, MD, New Delhi, India Philadelphia, Pa
Soheil Niku, MD, San Diego, Calif Norio Takahashi, MD, Fukui, Japan Virginia Commonwealth University Radiology
Mizuki Nishino, MD, Boston, Mass Douglas L. Teich, MD, Brookline, Mass Residents, Richmond, Va
908 Radiology: Volume 245: Number 3—December 2007
You might also like
- Treatment Cysts: Thoracoscopic PleuropericardialDocument8 pagesTreatment Cysts: Thoracoscopic PleuropericardialJuhi SahajwaniNo ratings yet
- A Giant Spinal Arterial Aneurysm in A Child Presenting As Quadriparesis (Case Reports, Vol. 2013, Issue Aug20 1) (2013)Document4 pagesA Giant Spinal Arterial Aneurysm in A Child Presenting As Quadriparesis (Case Reports, Vol. 2013, Issue Aug20 1) (2013)negin.safari8227No ratings yet
- 1958 CantrellDocument13 pages1958 CantrellAmro Al PeckNo ratings yet
- Teratoma of The Mediastinum: A Case Report: Casereport Open AccessDocument3 pagesTeratoma of The Mediastinum: A Case Report: Casereport Open AccessAndry Wahyudi AgusNo ratings yet
- Metanephric Adenoma in An 8-Year-Old Child: Case Report and Review of The LiteratureDocument4 pagesMetanephric Adenoma in An 8-Year-Old Child: Case Report and Review of The LiteratureNGUYEN QUYNHNo ratings yet
- Canine InsulinomaDocument5 pagesCanine Insulinomasoff4ikaNo ratings yet
- Laparoscopic Excision of A Renal Subcapsular Abscess Presenting As A Subcapsular HaematomaDocument3 pagesLaparoscopic Excision of A Renal Subcapsular Abscess Presenting As A Subcapsular HaematomaDavid MorgNo ratings yet
- Granulocytic SarcomaDocument6 pagesGranulocytic Sarcomafriiday.qNo ratings yet
- Strangulated Small Bowel Obstruction Related To Chronic Torsion of An Epiploic Appendix: CT FindingsDocument3 pagesStrangulated Small Bowel Obstruction Related To Chronic Torsion of An Epiploic Appendix: CT FindingsKomang Adhi AmertajayaNo ratings yet
- Arrhythmogenic Right Ventricular Cardiomyopathy in A WeimaranerDocument5 pagesArrhythmogenic Right Ventricular Cardiomyopathy in A WeimaranerEmilia AmmariNo ratings yet
- Noncompaction of The Left Ventricle in A Patient With DextroversionDocument4 pagesNoncompaction of The Left Ventricle in A Patient With DextroversionDinda Wanodya SNo ratings yet
- Short Reports: R J Kennedy, J L Scoyeld, W I H GarstinDocument2 pagesShort Reports: R J Kennedy, J L Scoyeld, W I H Garstinezzat anasNo ratings yet
- Solitary Right Ventricular Metastasis of Endometrial AdenocarcinomaDocument3 pagesSolitary Right Ventricular Metastasis of Endometrial AdenocarcinomaAbdullah Khaerul AzzamNo ratings yet
- Beyond The Boundaries: Enigma of Distinguishing Exophytic Upper Pole Renal Cell Carcinoma From An Adrenal MassDocument4 pagesBeyond The Boundaries: Enigma of Distinguishing Exophytic Upper Pole Renal Cell Carcinoma From An Adrenal MassAyush JainNo ratings yet
- Linician Pdate: Management of Deep Vein Thrombosis of The Upper ExtremityDocument7 pagesLinician Pdate: Management of Deep Vein Thrombosis of The Upper ExtremityhestyNo ratings yet
- 1812 FullDocument6 pages1812 FullWinston FontesNo ratings yet
- Ginek3 PDFDocument3 pagesGinek3 PDFberlinaNo ratings yet
- Shoulder Pain in Smokers Could Be A Life ChangerDocument2 pagesShoulder Pain in Smokers Could Be A Life Changerمجاهد إسماعيل حسن حسينNo ratings yet
- Emphysematous Prostatitis in A Patient With DiabetesDocument3 pagesEmphysematous Prostatitis in A Patient With DiabetesChandrashekhar SohoniNo ratings yet
- Potential Applications of Three-Dimensional Bioprinting in Regenerative MedicineDocument3 pagesPotential Applications of Three-Dimensional Bioprinting in Regenerative Medicinefreeway1313No ratings yet
- Infective EndocarditisDocument21 pagesInfective EndocarditisMohamad HamzaNo ratings yet
- 804 FullDocument3 pages804 FullRaluca IuliaNo ratings yet
- 1.2 Ohkuchi2001Document4 pages1.2 Ohkuchi2001Lina BorreroNo ratings yet
- Letters To The Editor: Pulmonary Atresia With Intact Ventricular SeptumDocument2 pagesLetters To The Editor: Pulmonary Atresia With Intact Ventricular SeptumanindiawNo ratings yet
- Usingtriphasic Helical CT To Detect Focal Hepatic Lesions in Patients With NeoplasmsDocument7 pagesUsingtriphasic Helical CT To Detect Focal Hepatic Lesions in Patients With NeoplasmsCalstore IdNo ratings yet
- Omar 2014Document5 pagesOmar 2014Fede WeckesserNo ratings yet
- Ijpd 24 221Document2 pagesIjpd 24 221intan yunni aztiNo ratings yet
- Bilateral Abdominal Cryptorchidism With Large Left Testicular Seminoma and Failed Right Urogenital UnionDocument4 pagesBilateral Abdominal Cryptorchidism With Large Left Testicular Seminoma and Failed Right Urogenital UnionMagdi HassanNo ratings yet
- Nascimento Et Al. - 2013 - Asymptomatic Anomalous Left Anterior Descending Artery Arising From The Right Coronary Artery With A Rare AntDocument3 pagesNascimento Et Al. - 2013 - Asymptomatic Anomalous Left Anterior Descending Artery Arising From The Right Coronary Artery With A Rare AntflashjetNo ratings yet
- Primary Haemangioma of The Skull: Case ReviewDocument3 pagesPrimary Haemangioma of The Skull: Case ReviewSoemantri Doank100% (1)
- Caudal Duplication SyndromeDocument3 pagesCaudal Duplication Syndromekhumaira1982No ratings yet
- Clinical Imaging: Yang Jiang, Frank Chen, Jordan Legout, Lauren Alexander, John Stauffer, Allie MetcalfeDocument4 pagesClinical Imaging: Yang Jiang, Frank Chen, Jordan Legout, Lauren Alexander, John Stauffer, Allie MetcalfeEdwin PradanaNo ratings yet
- Ajcr 2010 1 2Document3 pagesAjcr 2010 1 2Muhammad Bilal MirzaNo ratings yet
- Linician Pdate: Catheter Ablation of Ventricular TachycardiaDocument6 pagesLinician Pdate: Catheter Ablation of Ventricular TachycardiaSonia Rahma ANo ratings yet
- Clinical Imaging: Jay Tank, Abraham Knoll, Anthony Gilet, Susanne KimDocument4 pagesClinical Imaging: Jay Tank, Abraham Knoll, Anthony Gilet, Susanne Kimjansen siahaanNo ratings yet
- McConnell SignDocument6 pagesMcConnell SignAsdiana NurNo ratings yet
- Kim 2008Document3 pagesKim 2008HendrawanDianAgungWicaksanaNo ratings yet
- Atypical Extralobar Sequestration - JCTDocument4 pagesAtypical Extralobar Sequestration - JCTRafaella AranhaNo ratings yet
- Primary Review: Psoas Abscess: Case of The LiteratureDocument3 pagesPrimary Review: Psoas Abscess: Case of The LiteratureDung Tran HoangNo ratings yet
- Congenital Ewing's Sarcoma/Peripheral Primitive Neuroectodermal Tumor: A Case Report and Review of The LiteratureDocument4 pagesCongenital Ewing's Sarcoma/Peripheral Primitive Neuroectodermal Tumor: A Case Report and Review of The LiteratureMadalina GeorgianaNo ratings yet
- Combined Subcutaneous, Intrathoracic and Abdominal SplenosisDocument4 pagesCombined Subcutaneous, Intrathoracic and Abdominal Splenosis'Emilya'No ratings yet
- 660 FullDocument5 pages660 FullBatgirl xoxoNo ratings yet
- STUDY OF ILLNESS CONDITION FormatDocument2 pagesSTUDY OF ILLNESS CONDITION FormatChryst Louise SaavedraNo ratings yet
- Gastroent 09 06665Document3 pagesGastroent 09 06665HandayaniNo ratings yet
- DISCAPACIDAD ESPAÑA317.fullDocument5 pagesDISCAPACIDAD ESPAÑA317.fullAnonymous zLoi5mINo ratings yet
- Epithelioid Hemangioendothelioma of The Infundibular-Hypothalamic Region: Case Report and Literature ReviewDocument6 pagesEpithelioid Hemangioendothelioma of The Infundibular-Hypothalamic Region: Case Report and Literature ReviewcarlosNo ratings yet
- Reading Abdominal X-Rays and Head CTs - Presentation PDFDocument33 pagesReading Abdominal X-Rays and Head CTs - Presentation PDFRushi PatelNo ratings yet
- Bladder Pecoma Dynamic CT and MRI Presentation of 2 Cases With 2yr Follow Up and Review of The LiteratureDocument7 pagesBladder Pecoma Dynamic CT and MRI Presentation of 2 Cases With 2yr Follow Up and Review of The LiteratureJanetNo ratings yet
- Splenomegaly PDFDocument1 pageSplenomegaly PDFlakshminivas PingaliNo ratings yet
- Utd 13 1 74 77Document4 pagesUtd 13 1 74 77Abhishek Soham SatpathyNo ratings yet
- Management of Gastrointestinal Bleeding With.654Document1 pageManagement of Gastrointestinal Bleeding With.654Rizki AmeliaNo ratings yet
- Pinealoblastoma With Shunt Metastasis: A Case Report: e Ea e yDocument4 pagesPinealoblastoma With Shunt Metastasis: A Case Report: e Ea e yMuhammad Azhary LazuardyNo ratings yet
- Lin 2019Document3 pagesLin 2019Mahmoud AbouelsoudNo ratings yet
- Case Report: Giant Abdomino Scrotal Hydrocele: A Case Report With Literature ReviewDocument6 pagesCase Report: Giant Abdomino Scrotal Hydrocele: A Case Report With Literature ReviewMella IntaniabellaNo ratings yet
- CIRCULATIONDocument2 pagesCIRCULATIONRVDNo ratings yet
- PROCEEDINGS OF THE PAEDlATRlC NEURO-ONCOLOGY TUMOUR BOARDDocument9 pagesPROCEEDINGS OF THE PAEDlATRlC NEURO-ONCOLOGY TUMOUR BOARDfriiday.qNo ratings yet
- 81-Texto Del Artículo-1437-1-10-20210903Document3 pages81-Texto Del Artículo-1437-1-10-20210903suelly-majorNo ratings yet
- Carotid Body Tumor As A Cause of Stroke2016Document4 pagesCarotid Body Tumor As A Cause of Stroke2016Nicolas RodriguezNo ratings yet
- Endometriosis of The Vastus Lateralis Muscle: CasereportDocument4 pagesEndometriosis of The Vastus Lateralis Muscle: CasereporttabareeNo ratings yet
- J Seminoncol 2018 01 004Document4 pagesJ Seminoncol 2018 01 004Vo VũNo ratings yet
- Clinical Manifestations and Diagnosis of Primary MyelofibrosisDocument2 pagesClinical Manifestations and Diagnosis of Primary MyelofibrosisVo VũNo ratings yet
- Stem Cells, Cancer, and Cancer Stem Cells: InsightDocument7 pagesStem Cells, Cancer, and Cancer Stem Cells: InsightMekki Lazir IlhdafNo ratings yet
- Pictorial Essay: Typical and Atypical Presentations of Extramedullary HemopoiesisDocument5 pagesPictorial Essay: Typical and Atypical Presentations of Extramedullary HemopoiesisVo VũNo ratings yet
- Mass-Like Extramedullary Hematopoiesis: Imaging Features: Scientific ArticleDocument6 pagesMass-Like Extramedullary Hematopoiesis: Imaging Features: Scientific ArticleVo VũNo ratings yet
- Tushnet - An Essay On RightsDocument43 pagesTushnet - An Essay On RightslarisamannNo ratings yet
- Self-Efficacy and Academic Stressors in University StudentsDocument9 pagesSelf-Efficacy and Academic Stressors in University StudentskskkakleirNo ratings yet
- SST Vs BBTDocument7 pagesSST Vs BBTFlaxkikare100% (1)
- CA Level 2Document50 pagesCA Level 2Cikya ComelNo ratings yet
- Paper:Introduction To Economics and Finance: Functions of Economic SystemDocument10 pagesPaper:Introduction To Economics and Finance: Functions of Economic SystemQadirNo ratings yet
- Introduction To Human MovementDocument5 pagesIntroduction To Human MovementNiema Tejano FloroNo ratings yet
- Al-Farabi Fusul Al MadaniDocument107 pagesAl-Farabi Fusul Al MadaniDaniel G.G.100% (1)
- Malaybalay CityDocument28 pagesMalaybalay CityCalvin Wong, Jr.No ratings yet
- New KitDocument195 pagesNew KitRamu BhandariNo ratings yet
- Matrix CPP CombineDocument14 pagesMatrix CPP CombineAbhinav PipalNo ratings yet
- EQUIP9-Operations-Use Case ChallengeDocument6 pagesEQUIP9-Operations-Use Case ChallengeTushar ChaudhariNo ratings yet
- -4618918اسئلة مدني فحص التخطيط مع الأجوبة من د. طارق الشامي & م. أحمد هنداويDocument35 pages-4618918اسئلة مدني فحص التخطيط مع الأجوبة من د. طارق الشامي & م. أحمد هنداويAboalmaail Alamin100% (1)
- B1 Editable End-of-Year TestDocument6 pagesB1 Editable End-of-Year TestSyahira Mayadi50% (2)
- Quality Assurance Plan-75FDocument3 pagesQuality Assurance Plan-75Fmohamad chaudhariNo ratings yet
- Unit 7 - Evolution and Classification: Regents BiologyDocument24 pagesUnit 7 - Evolution and Classification: Regents BiologyTalijah JamesNo ratings yet
- Basics of Petroleum GeologyDocument23 pagesBasics of Petroleum GeologyShahnawaz MustafaNo ratings yet
- A Mini-Review On New Developments in Nanocarriers and Polymers For Ophthalmic Drug Delivery StrategiesDocument21 pagesA Mini-Review On New Developments in Nanocarriers and Polymers For Ophthalmic Drug Delivery StrategiestrongndNo ratings yet
- 0n9) O6..,w48j-GDocument14 pages0n9) O6..,w48j-GMocha FurrerNo ratings yet
- Theory of Construction of The Giza Plateau Pyramids (Original Title Hypothesis of Construction of The Pyramids of The Valley of Gizeh (Giza)Document15 pagesTheory of Construction of The Giza Plateau Pyramids (Original Title Hypothesis of Construction of The Pyramids of The Valley of Gizeh (Giza)International Journal of Innovative Science and Research TechnologyNo ratings yet
- Evaluating Websites A Checklist - JOHN CARLO G. GAERLANDocument3 pagesEvaluating Websites A Checklist - JOHN CARLO G. GAERLANMarvin CincoNo ratings yet
- Award Presentation Speech PDFDocument3 pagesAward Presentation Speech PDFNehal RaiNo ratings yet
- Creativity Triggers 2017Document43 pagesCreativity Triggers 2017Seth Sulman77% (13)
- Nugent 2010 Chapter 3Document13 pagesNugent 2010 Chapter 3Ingrid BobosNo ratings yet
- Project Report On HeritageDocument39 pagesProject Report On HeritageBALA YOGESH YANDAMURINo ratings yet
- List of Practicals Class Xii 2022 23Document1 pageList of Practicals Class Xii 2022 23Night FuryNo ratings yet
- Protected PCM USB Memory Sticks For Pa3X.Document1 pageProtected PCM USB Memory Sticks For Pa3X.mariuspantera100% (2)
- New Client QuestionnaireDocument13 pagesNew Client QuestionnairesundharNo ratings yet
- Jail Versus Substance Abuse TreatmentDocument5 pagesJail Versus Substance Abuse Treatmentapi-240257564No ratings yet
- First Aid Transportation of The InjuredDocument30 pagesFirst Aid Transportation of The InjuredMuhammad Naveed Akhtar100% (1)
- Bsa2105 FS2021 Vat Da22412Document7 pagesBsa2105 FS2021 Vat Da22412ela kikayNo ratings yet