Professional Documents
Culture Documents
Early Events in Coccidioidomycosis
Uploaded by
MIGUELCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Early Events in Coccidioidomycosis
Uploaded by
MIGUELCopyright:
Available Formats
REVIEW
crossm
Early Events in Coccidioidomycosis
Fariba M. Donovan,a,b Lisa Shubitz,a Daniel Powell,a Marc Orbach,a,c Jeffrey Frelinger,a,d John N. Galgiania,b
a Valley Fever Center for Excellence, University of Arizona College of Medicine—Tucson, Tucson, Arizona, USA
b Department of Medicine, University of Arizona College of Medicine—Tucson, Tucson, Arizona, USA
c
School of Plant Sciences, College of Agriculture and Life Sciences, University of Arizona, Tucson, Arizona, USA
d Department of Immunobiology, University of Arizona, Tucson, Arizona, USA
SUMMARY . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 1
INTRODUCTION . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 1
LIFE CYCLE: EARLY EVENTS SURROUNDING THE TRANSITION FROM SAPROBIC TO
INVASIVE GROWTH . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3
RESPIRATORY TRACT COMPONENTS . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5
HISTOPATHOLOGY OF EARLY COCCIDIOIDES INFECTION . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 6
PATHOGEN-RELATED COMPONENTS . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 8
HOST-RELATED RESPONSE . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10
IMMUNE RESPONSE . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 11
Innate Immunity . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 11
Adaptive Immunity . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 13
CLINICAL ASPECTS OF COCCIDIOIDOMYCOSIS . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 14
CONCLUDING REMARKS . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 16
Downloaded from https://journals.asm.org/journal/cmr on 04 February 2023 by 2806:290:a80b:cc8:c419:e160:befc:f9a8.
ACKNOWLEDGMENTS . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 17
REFERENCES . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 17
AUTHOR BIOS . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 21
SUMMARY Since its description nearly 130 years ago, hundreds of studies have
deepened our understanding of coccidioidomycosis, also known as valley fever (VF),
and provided useful diagnostic tests and treatments for the disease caused by the
dimorphic fungi Coccidioides spp. In general, most of the literature has addressed
well-established infections and has described patients who have experienced major
complications. In contrast, little attention has been given to the earliest conse-
quences of the pathogen-host interaction and its implications for disease manifesta-
tion, progression, and resolution. The purpose of this review is to highlight published
studies on early coccidioidomycosis, identify gaps in our knowledge, and suggest new
or former research areas that might be or remain fertile ground for insight into the early
stages of this invasive fungal disease.
KEYWORDS early coccidioidomycosis, early events in valley fever, Coccidioides
research, coccidioidomycosis
INTRODUCTION
C occidioides spp. are dimorphic fungi that cause coccidioidomycosis, a disease that
was first described by Alejandro Posadas in 1892 (1). Their life cycle progresses from
a mycelial (saprobic/soil) phase to a spherule/endospore (parasitic/host) phase (2, 3).
Citation Donovan FM, Shubitz L, Powell D,
Orbach M, Frelinger J, Galgiani JN. 2019. Early
events in coccidioidomycosis. Clin Microbiol
The two known species are Coccidioides immitis and Coccidioides posadasii. C. immitis is Rev 33:e00112-19. https://doi.org/10.1128/CMR
found predominantly in California, and its range extends to Baja California, Arizona, and .00112-19.
parts of Utah and eastern Washington state. C. posadasii is found predominantly in Copyright © 2019 American Society for
Microbiology. All Rights Reserved.
Arizona, and its range extends to Utah, New Mexico, Texas, Mexico, and parts of Central
Address correspondence to Fariba M. Donovan,
and South America (4, 5). It has long been known that dry, dusty environmental conditions faribadonovan@deptofmed.arizona.edu.
and soil disruption promote the release of arthroconidia into the air, so nearly all Published 16 October 2019
infections begin in the lungs (6, 7). Extrapolating from in vitro studies, by 24 h after
January 2020 Volume 33 Issue 1 e00112-19 Clinical Microbiology Reviews cmr.asm.org 1
Donovan et al. Clinical Microbiology Reviews
inhalation, arthroconidia have already begun to transform into large spherules (8, 9).
From approximately 24 until 120 to 132 h after inhalation of arthroconidia, spherules
continue to grow, septate, develop endospores, rupture, and release the endospores,
which can repeat the process (10–12).
When first inhaled, arthroconidia encounter ciliated, goblet, and club cells in the
conducting zone (oronasopharynx to the terminal bronchioles) and type I and II
alveolar cells (pneumocytes) in the respiratory zone (respiratory bronchioles and
alveolar ducts/sacs), along with myeloid-derived cells, such as alveolar macro-
phages. Arthroconidia are met with mechanical and physical barriers, such as the
beating action of cilia, mucus, and tight junctions between cells (13). Humoral
factors, such as complement, could be part of the initial host interactions. Histo-
pathological changes are well documented in the murine model, but early histo-
logical changes in the human lung are not well understood (14). Pathogen-related
factors that aid in inhalation, adhesion, invasion, and survival in the host have been
studied, but there are many areas still to be investigated (15). The host response to
the pathogen is equally complex and merits further investigation. The innate
immune system includes cell types such as polymorphonuclear neutrophils (PMNs),
macrophages, dendritic cells (DCs), eosinophils, natural killer (NK) cells, innate
lymphoid cells (ILCs), invariant natural killer T (iNKT) cells, ␥␦ T cells, and epithelial
cells. Noncellular substances include antimicrobial peptides/molecules, such as
lysozyme, lactoferrin, protease inhibitors, human -defensins, and cathelicidins, and
oxidants, such as nitric oxide (NO) and hydrogen peroxide (H2O2) (13, 16, 17). In
other infections, innate responses are important in early pathogen recognition,
pathogen clearance and/or inhibition, and cooperation with the adaptive immune
system to further host defense. However, the exact role of each cell type and
Downloaded from https://journals.asm.org/journal/cmr on 04 February 2023 by 2806:290:a80b:cc8:c419:e160:befc:f9a8.
noncellular substance in coccidioidomycosis has yet to be determined.
Approximately 60% of persons who inhale Coccidioides arthroconidia develop in-
fections that are subclinical, with either mild symptoms or none at all (18). Most of
the remainder experience a respiratory syndrome of community-acquired pneumonia
(CAP), including a nonproductive cough, chest pain, and dyspnea (19, 20). Global signs
and symptoms of fever, night sweats, fatigue, and weight loss are frequent (21). Smith
summarized other symptoms, such as an influenza-like illness followed by skin lesions
associated with arthralgia and conjunctivitis, with the synonymous terms San Joaquin
valley fever (VF), desert fever, and desert rheumatism and suggested these symptoms
predict a more benign course (22). Eventually, despite often protracted morbidity, most
patients resolve their illnesses regardless of whether they are treated with antifungal
drugs, occasionally with a residual asymptomatic pulmonary nodule or thin-walled
cavity evident on chest imaging (23). A few develop either fibrocavitary pulmonary
lesions or hematogenous spread beyond the chest, and these complications usually
need long-term medical management. Those with self-limited courses of their first
infection, and possibly even those with complicated courses, rarely if ever develop
illness from a second exposure to Coccidioides (22, 24).
This wide variety of disease manifestations might be due to differences among
strains of Coccidioides, but to date there is no or very little evidence in support of this
possibility. Perhaps other coexisting conditions, such as concurrent infections, the
enteric microbiome, or nutritional factors, are involved, but again, there is very little (if
any) evidence directly linking these variables to the spectrum of coccidioidal illness. A
2013 study demonstrated that vitamin D does not play a significant role in host
susceptibility to coccidioidomycosis, but investigation of other nutritional factors may
be of value (25). It is clear that profound cellular immunosuppression and some gene
mutations may predispose patients to disseminated infection (26, 27). Although im-
munogenetic variations might explain the spectrum of disease manifestation, differ-
ences in early innate responses could also be a contributing factor in both disease
presentation and course.
January 2020 Volume 33 Issue 1 e00112-19 cmr.asm.org 2
Early Events in Coccidioidomycosis Clinical Microbiology Reviews
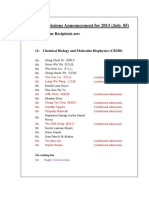
FIG 1 Life cycle of Coccidioides. Coccidioides spp. alternate between saprobic (mycelia) (left) and parasitic (spher-
ules) (right). The saprobic cycle is found in the environment and produces infectious arthroconidia. They may
become airborne and be inhaled by the host or may return to the environment to continue the saprobic life cycle.
(Adapted from reference 11, published under a Creative Commons license.)
LIFE CYCLE: EARLY EVENTS SURROUNDING THE TRANSITION FROM SAPROBIC
TO INVASIVE GROWTH
Downloaded from https://journals.asm.org/journal/cmr on 04 February 2023 by 2806:290:a80b:cc8:c419:e160:befc:f9a8.
As a dimorphic fungus, Coccidioides alternates between saprobic (mycelium) and
infectious (spherule) phases. Under environmental conditions, the fungus can cycle
through the mycelial phase without infecting a mammalian host (11, 28) (Fig. 1). As
Mead and others wrote in 2018, “the molecular mechanisms that initiate the morpho-
logical switch from a saprobic to a parasitic phase are not understood” (29). The obstacles
to understanding these mechanisms include (i) applying in vitro models to in vivo
processes, (ii) limitations of applying animal models (primarily murine) to the human
disease process (14), (iii) difficulties in studying the early infective process in humans
(30), and (iv) the risk of attempting to ascribe biological processes studied in other fungi
to Coccidioides.
Recent studies on the structure, morphogenesis, and immunogenicity of arthro-
conidia are lacking. Once inhaled, the morphogenesis from small barrel-shaped cells to
larger immature spherules begins in just 8 to 24 h (28). Pioneering work by Converse
and others (31–35) has advanced in vitro studies of the parasitic phase of Coccidioides
by utilizing temperature (approximately 37°C), CO2 tension (10 to 20%), and surfactant-
like agents (e.g., Tamol SN [Rohm and Haas, Philadelphia, PA]) to model conditions in
the host lung. In vitro modeling has been essential, as the rapid arthroconidial changes
and inability to visualize arthroconidia in murine tissue samples after intranasal inoc-
ulation limit the assessment of this critical period. Early studies of Coccidioides structure
focused on the lipid, carbohydrate, and protein compositions of the various fungal
forms. The mechanisms that regulate these changes in chemical composition and their
biological significance from one form to another remain undefined. In 1977, Wheat and
colleagues described fungal structure by analyzing and comparing the cell wall com-
positions of arthrospores, mycelia, and spherule walls, noting that arthrospores retain
1.5 times more protein than mycelium walls and 3 times more protein than spherule
walls. They also measured the lipid and carbohydrate composition of the cell walls.
Differences in lipid content and composition were observed between arthrospores,
mycelia, and spherules. The smallest amount of lipid was found in mycelia (36). Taking
this work further in 1985, Cole and Sun summarized their efforts to analyze the
arthroconidial outer and inner cell walls and suggested there are antigenic differences
January 2020 Volume 33 Issue 1 e00112-19 cmr.asm.org 3
Donovan et al. Clinical Microbiology Reviews
between arthroconidia and spherules based on their different chemical compositions.
Their chapter in Fungal Dimorphism (10) remains the definitive description of “conid-
iogenesis” (development of arthroconidia from mycelia, illustrating the alternating
production of viable arthroconidia between degenerating cells in the branching my-
celium). Interestingly, arthroconidia do not cleanly break off from the hyphae but retain
a portion of the degenerate hyphal cell wall through inhalation of the arthroconidia by
the host (10). In 1983, Drutz and Huppert suggested this retained hyphal outer wall
layer (HOWL) served some level of antiphagocytic action (15). Subsequent research has
not investigated this idea. In 1987, Cole et al. and Bayley et al. further demonstrated
that arthroconidia have a hydrophobic outer layer, similar to the hydrophobins de-
scribed for many aerially dispersed fungal spores, that contains immunosuppressive
compounds that are easily stripped away, revealing a water-soluble fraction with T
cell-stimulating antigens (37, 38). As a side note, this soluble wall fraction antigen was
demonstrated in the mycelial phase by Ward et al. in 1975 (39) and in the spherule
phase by Cox et al. in 1984 (40). It is now known as antigen 2/proline-rich antigen
(Ag2/PRA) and has been extensively studied in immune responses and as a vaccine
candidate (41–43). The initiation of parasitic-cell differentiation involves two unique
events, formation of uninucleate cells and the coalescence of multiple cytoplastic
vacuoles into a large central vacuole as arthroconidia grow isotropically into round cells
and young spherules (44).
Unlike the study of arthroconidia, interest in spherule composition did not seem to
wane as much in the 1990s and 2000s. A great deal of knowledge about spherule outer
and inner wall structure is derived from early electron microscopy studies (10, 15, 28,
45). The spherule phase can vary temporally and is generally considered to be from 24
through 120 h after inhalation of arthroconidia. Inhaled arthroconidia are multinucleate
(dikaryons are the most common) but within 8 h are uninucleate, and at 24 h, the
Downloaded from https://journals.asm.org/journal/cmr on 04 February 2023 by 2806:290:a80b:cc8:c419:e160:befc:f9a8.
developing round cells (early spherules) are multinucleate again. The question, pro-
posed by Huppert et al. in 1982, of whether the transition of multinucleate to uninu-
cleate cells is the result of nuclear fusion or degeneration remains unanswered today
(28). However, it is clear that during the first 48 h, the spherules undergo repeated
mitosis with little cellular enlargement (46). It is thought that mitosis ceases at 48 h,
right before spherule septation begins (10). At about 48 h, the immature spherules are
about 5 m in diameter, contain multiple nuclei, and have already begun the segmen-
tation process (28). Septation continues for the next 48 to 72 h and produces a mature
spherule with as many as 200 to 300 endospores by approximately 96 to 120 h
postinhalation (10, 12, 28). Mature Coccidioides spherules may vary from 60 to more
than 100 m in diameter (12). Spherules have higher lipid and glucosamine concen-
trations than arthroconidia and mycelia (36). The importance of this difference in
composition is not known. Hector and Pappagianis utilized different enzymes to
degrade the spherule cell wall and suggested the outer half of the cell wall is largely
␣-(1-3)-glucan and the inner half is a matrix of chitin and -(1-3)-glucan. Interspersed
between the two halves is a mannan-protein complex that they proposed holds the
halves together and anchors the wall to the membrane (47). In 1986, Frey and Drutz
described an extracellular glycoprotein matrix that surrounds young and mature spherules,
but not arthroconidia and endospores (48). They proposed that the matrix helps
spherules resist attacks by PMNs. These proposals have not been further investigated.
At that time, it was believed PMNs did not attack spherules, but a study by Lee et al.
suggests otherwise (49). Resolving these differences could be an interesting avenue of
research. In a similar vein, the spherule outer wall glycoprotein (SOWgp), which is
expressed only in the parasitic phase, is thought to act as an adhesin to mammalian
extracellular matrix proteins, such as laminin, fibronectin, and collagen type IV, and
thereby aids attachment of arthroconidia and spherules to host endothelial tissue (50).
Interestingly, a metalloproteinase (Mep1) secreted during endosporulation digests the
immunodominant SOWgp and limits host recognition of endospores during the phase
of development when these fungal cells are most vulnerable to phagocytosis by the
host (51). In the early 2000s, fungal wall components, such as -glucans, took on new
January 2020 Volume 33 Issue 1 e00112-19 cmr.asm.org 4
Early Events in Coccidioidomycosis Clinical Microbiology Reviews
interest as the concept of pathogen-associated molecular patterns (PAMPs) and their
interactions with host pattern recognition receptors (PRRs) became more widespread.
In 2005, Viriyakosol et al. published a prescient article introducing Charles Janeway’s
theory recognizing nonself and self in coccidioidomycosis research (52). The examina-
tion of pathogen “pattern” and host “receptor” remains a mainstay of Coccidioides
research to this day. PAMPs and PRRs are discussed further below.
The next morphological stage in the Coccidioides life cycle is the endospore, on
which there has been scant research since the 1980s. Segmentation of a spherule into
primary, then secondary, and finally tertiary segmentation planes is the cue for devel-
opment of endospores (about 72 h) (10). Measuring about 2 to 4 m in diameter,
endospores are released from a ruptured spherule at approximately 120 to 132 h and
during this process are held in clusters by fibrils that eventually give way and release
the endospores as round, uninucleate cells (10, 12, 28). The fibrils are derived from the
spherule inner wall and released in large 10-m packets, which are thought to make
the endospores less “digestible” for phagocytes. As mentioned in the article, there are
no direct studies of this interaction (15). The endospores, as shown for arthroconidia,
were eventually phagocytized by either alveolar macrophages (obtained from rhesus
macaques) or murine peritoneal macrophages, but in either case were not killed, as
demonstrated by Beaman et al. The inability of macrophages to kill endospores was
suggested to be partly due to inhibition of fusion between phagosomes containing
fungal spores and the lysosomes within the macrophages (9, 53). Other than Hector’s
speculation that endospores maintain ␣-(1-3)-glucan from septating spherules, there
are no summaries of the chemical composition of endospores, as there are for mycelia,
arthroconidia, and spherules (10, 36, 47). A 2014 article briefly mentions that the
endospore cell wall contains chitin, -(1-3)-glucan, 3-0-methyl mannan, and mannans
(54). Garcia-Sherman et al. detected fungal surface amyloids on endospores and spherules
Downloaded from https://journals.asm.org/journal/cmr on 04 February 2023 by 2806:290:a80b:cc8:c419:e160:befc:f9a8.
that bind to the host serum amyloid protein (SAP) component. This process aids in fungal
attachment and forms a biofilm that may diminish the host inflammatory response by
protease inhibition (55).
RESPIRATORY TRACT COMPONENTS
The primary route of Coccidioides infection is through inhalation of arthroconidia.
Wiesner and Klein provide a succinct overview of the role lung epithelial cells play in
fungal immunity. They highlight three pathways for Pneumocystis, Aspergillus, and
Cryptococcus. In their concluding remarks, they outline the concept of fungal attach-
ment, penetration, and avoidance (56). This is the essence of the challenge associated
with learning more about early events in coccidioidomycosis.
The airway tract consists of two zones: the conducting zone (oronasopharynx
through the terminal bronchioles) and the respiratory zone (respiratory bronchioles and
alveoli). Far from being a static, passive tube, the conducting airway consists of a variety
of cells; the most prominent are ciliated, goblet, basal, and club cells (formerly known
as Clara cells), which, besides sweeping out pathogens or producing mucus, initiate
early innate immune responses (13). The importance of mucociliary function, apicolat-
eral junctional complexes, and antimicrobial products released by the conducting
airway cells is further illustrated and elucidated by Whitsett and Alenghat (57). The role
of ciliary cells in coccidioidomycosis has not been examined. There is increasing
evidence that secreted mucins, such as MUC5AC and MUC53, besides helping form the
mucus protective barriers and rafts, are involved in pulmonary innate immunity (57).
There are no studies on the roles of these mucus products in coccidioidomycosis. Club
cells become more numerous as the airway transitions to the terminal bronchioles.
Aside from a brief mention of club cells’ role in innate defense by Awasthi et al., there
are no further studies of their role in coccidioidomycosis (58). The respiratory zone and
innate immune system cells were illustrated by Hussell and Bell, especially in relation to
alveolar macrophages (30). In the alveoli, the goblet and club cells seen in the respiratory
bronchioles give way to type I and II alveolar cells. The elongate type I alveolar cells are
primarily responsible for gas exchange, and the more cuboidal type II alveolar cells
January 2020 Volume 33 Issue 1 e00112-19 cmr.asm.org 5
Donovan et al. Clinical Microbiology Reviews
serve as immune responders (16, 57). Type II alveolar cells express many PRRs, and
among them are collectins, which are soluble secreted PRRs, such as the pulmonary
surfactant protein A (SP-A) and SP-D (59). Researchers seem split on the question of
whether inhaled arthroconidia are able to reach the alveoli or only reach the terminal
bronchioles. The barrel-shaped arthroconidia are generally considered to be 3 to 5 m
in width and length. At these dimensions, it could be assumed that arthroconidia are
most impactful at the terminal and respiratory bronchioles (60).
HISTOPATHOLOGY OF EARLY COCCIDIOIDES INFECTION
The fate of Coccidioides immediately following inhalation of arthroconidia is poorly
understood because of the current inability to study early postinfection events in
humans. Researchers have relied on information gathered from both in vitro studies
and animal infection models for insight into inhaled arthroconidium, spherule, and
endospore morphogenesis and early host immune response. In spite of potential limita-
tions, in vitro studies, such as those using peripheral blood mononuclear cells (PBMCs)
and bronchoalveolar lavage fluid (BALF), have provided valuable information about the
early events in coccidioidomycosis. For example, an early study by Deresinski et al.
using PBMCs demonstrated that PBMCs from both immune and nonimmune subjects
could avidly phagocytize killed endospores (61). In a more recent study, Nesbit et al.
utilized both cells from BALF and PBMCs of patients with pulmonary coccidioidomy-
cosis and demonstrated specific cellular immune responses, including interleukin 17
(IL-17) expression (62).
While there have been studies utilizing monkeys and rabbits, mice are the best
developed and most easily used laboratory model of coccidioidomycosis (63–65). The
advantages of the murine model include their small size and ease of handling at animal
biosafety level 3 (ABSL3). Another advantage is that, although they vary in their
Downloaded from https://journals.asm.org/journal/cmr on 04 February 2023 by 2806:290:a80b:cc8:c419:e160:befc:f9a8.
susceptibility to Coccidioides spp. based upon strain genetics, all mice are susceptible
and can be infected intranasally to a level at which they develop progressive pneu-
monia, dissemination, and death within a few weeks. Because the entire lung weighs
⬃0.25 g in a normal mouse, the total lung is conducive to extensive study of early
events by histopathology. A disadvantage of using a mouse model to mimic human
response is their rapid progression to death in 14 to 28 days postchallenge. This may
interfere with the assessment of early immune system responses that lead to disease
control in humans. In addition, unlike humans, a low inoculum intranasally leads to
rapid death (14). There are no studies correlating the inoculum size with disease
severity in humans. From epidemiological studies of point source outbreaks, such as
archeological excavations, where high inoculum exposures occur, there are much
higher rates of symptomatic pulmonary infections. Radiographic findings for such
patients often exhibit infiltrate in multiple lobes of both lungs. Although disseminated
infections have resulted from such exposures, the frequency is low, and it does not
appear that high-inoculum infections are more likely to develop chronic complications.
On the other hand, most coccidioidal infections do not occur in clusters, suggesting
that point source infections are the exception (66). When pneumonia is present, it is
usually unilateral (67, 68). Also, it is surprisingly common that patients with dissemi-
nated coccidioidomycosis (DCM) have minor or no evident pulmonary disease (69). This
suggests that most, if not nearly all, ambient coccidioidal infections are the result of
very small inocula.
Insight into the early pathogen-host interaction and response have been made via
sequential assessment of murine lung histopathology by Shubitz and colleagues (70,
71). In a 2011 study, different mouse strains were challenged intranasally with varying
numbers of C. posadasii (strain Silveira), arthroconidia. At 24 to 48 h, no spherules were
detected, even utilizing a Coccidioides-specific immunohistochemical stain (71). This
stain is a polyclonal goat antibody to the ubiquitous Coccidioides wall antigen Ag2/PRA,
which was discussed previously (70). The lack of in situ information on the early events
in the first 48 h may be due to arthroconidia being small, few in number, and intracellular
(72).
January 2020 Volume 33 Issue 1 e00112-19 cmr.asm.org 6
Early Events in Coccidioidomycosis Clinical Microbiology Reviews
Downloaded from https://journals.asm.org/journal/cmr on 04 February 2023 by 2806:290:a80b:cc8:c419:e160:befc:f9a8.
FIG 2 Histopathology of early murine lung infection. The panels span 72 to 144 h postinfection with C.
posadasii strain Silveira. Tissues were immunohistochemically stained with a polyclonal goat antibody
against the Coccidioides cell wall antigen, Ag2/PRA, with hematoxylin counterstain. Note that spherules
and endospores appear dark red to brown. (A and B) Unruptured first-generation spherules with very few
surrounding immune cells at approximately 72 h (A) and approximately 96 h (B). Virtually all are
macrophages. (Magnification, ⫻200 [A] and ⫻400 [B].) (C and D) There is an enormous influx of PMNs,
and also macrophages, once the endospores are released (approximately 120 h). Note the lack of
inflammatory cells around the unruptured spherule in panel C. (Magnification, ⫻200 [C] and ⫻400 [D].)
(E and F) Ongoing recruitment of inflammatory cells to the area and dispersal of endospores, now
enlarging back into early spherules (approximately 144 h). In panel F, the top two arrows point to a
damaged airway filled with inflammatory cells; the third arrow points to endospores within the damaged
airway. (Magnification, ⫻40 [E and F].)
By approximately 72 h, immature spherules can be visualized with the Coccidioides-
specific immunohistochemical stain (Fig. 2A). Around 72 to 96 h, the spherules, though
visible, have provoked only a minimal inflammatory response. The response consists
primarily of a few monocytes and an occasional PMN. PMNs are notably absent even
when a layer or two of macrophages and occasional lymphocytes is seen (Fig. 2A and
B). While the first-generation spherules remain unruptured, the Coccidioides infection
appears to be relatively invisible to the host immune system. Data to confirm this
conclusion are lacking, as is information about the potential signaling between patho-
gen and host. These histopathological observations are supported by a 2018 vaccine
study that measured cytokines in the lungs (73). Cytokines were measured in lung cell
supernatants from vaccinated and unvaccinated mice on days 1, 2, 4, and 6 following
infection with virulent arthroconidia. A mouse Illumina 31-plex panel measured cyto-
kines on 24-h supernatants from the lung cell cultures. In this assay, unvaccinated mice
exhibited no increases in IL-4, gamma interferon (IFN-␥), macrophage inflammatory
January 2020 Volume 33 Issue 1 e00112-19 cmr.asm.org 7
Donovan et al. Clinical Microbiology Reviews
protein 1a (MIP1a), MIP1b, macrophage colony-stimulating factor (MCSF), monokine-
induced by IFN-␥ (MIG), or tumor necrosis factor alpha (TNF-␣) prior to day 4, while the
vaccinated mice had early increases in these cytokines, as previously described (73).
Causally or coincidentally, spherule rupture starts around 96 h and is nearly completed
by 120 h, with dispersing endospores and a dramatic influx of inflammatory cells,
primarily PMNs and some macrophages (Fig. 2C and D). Once the spherules rupture,
releasing endospores, PMNs and macrophages rapidly and robustly infiltrate the tissue
and surround the endospores, so much so that the lesions become visible to the naked
eye (⬃1 to 2 mm in diameter). It has been reported that endospores are chemotactic
for PMNs, and the histopathology is consistent (49, 71). However, PMNs have a limited
ability to kill endospores (15). By 144 h (day 6), dense islands of pyogranulomatous
inflammation are present, and the first generation of endospores begins to enlarge into
spherules (Fig. 2E). PMNs (as well as rare eosinophils and basophils) pack terminal
airways adjacent to the original spherules and fill the alveolar spaces where the
growing endospores have dispersed (70). Suppurative infiltrates are seen in both the
tissue and terminal bronchioles (Fig. 2F).
PATHOGEN-RELATED COMPONENTS
Since the year 2000, Coccidioides research has involved examination of PAMPs,
signal transduction pathways, gene expression, and gene expression products that aid
in fungal production of transcription factors, adhesion, and immune system evasion.
The production of cell wall components, adhesins, reactive oxygen species (ROS), and
biofilms and the expression of virulence factors are areas of interest.
An overview of PAMPs in Coccidioides has been published (74). Noting that the
fungal cell wall is a complex structure comprised of mannan, glucans, and chitin, the
author illustrates the interaction of mannan with the PRR and mannose receptor (MR)
Downloaded from https://journals.asm.org/journal/cmr on 04 February 2023 by 2806:290:a80b:cc8:c419:e160:befc:f9a8.
on macrophages or dendritic cells, as well as that of -glucan with the Dectin-1
receptor. The article further notes that fungal PAMPs that interact with Toll-like receptor
2 (TLR2) and TLR4, as well as SP-A and SP-D, are not known (74). Erwig and Gow noted
that fungal ␣-mannans interact with the host Dectin-2 receptor, but Viryakosol et al.
suggested Dectin-2 and MR are not essential for murine resistance to Coccidioides
(54, 75).
In 2000, Lengeler et al. published an article describing signaling pathways in various
fungi with an emphasis on Saccharomyces cerevisiae as a paradigm for signaling in
other organisms, with additional insights provided by Runyanga et al. in 2017 (76, 77).
Cyclic AMP-protein kinase A (cAMP-PKA) and mitogen-activated protein kinase (MAPK)
are thought to be major signaling pathways and are postulated to be involved in
regulation of phase transition in endemic dimorphic fungi. Studies of these pathways
have been done in S. cerevisiae and Neurospora crassa and in fungal pathogens, such
as Candida albicans and Cryptococcus neoformans (78). There are no specific studies of
signal transduction pathways in Coccidioides, and this might be an area of future
research.
Early genetic studies in Coccidioides cloned the chitinase genes (cts1 and cts2) that
were surmised to be responsible for the cell wall hydrolase chitinase. These genes are
involved in spherule growth and endospore release by remodeling chitin (44, 79). A tool
for Coccidioides genetic transformation is Agrobacterium tumefaciens, a Gram-negative
bacterium that had previously been utilized in plants and filamentous fungi to transfer
hygromycin resistance via a transfer DNA (T-DNA) vector plasmid to arthroconidia (80).
This is a simple and effective method widely used in fungal-gene manipulations. The
availability of a nearly complete genome sequence has furthered the understanding of
Coccidioides (https://www.broadinstitute.org/scientific-community/science/projects/fungal-
genome-initiative/coccidioides-genomes). Additional chitinase and -1,3-glucan synthase
genes have been described (12, 81, 82). In 2006, Johannesson et al. greatly expanded
the understanding of Coccidioides phase-specific gene expression by combining gene
expression data with predicted protein localization and gene binding sites, thus
identifying a list of putative C. posadasii antigens (83). In addition to primary sequence
January 2020 Volume 33 Issue 1 e00112-19 cmr.asm.org 8
Early Events in Coccidioidomycosis Clinical Microbiology Reviews
differences between C. posadasii and C. immitis, Delgado et al. in their transcriptome-
sequencing (RNA-seq) analysis showed differential gene expression in the two C.
posadasii isolates examined, C735 and Silveira (84). In 2006, Rappleye and Goldman
reviewed virulence genes in four dimorphic fungi, Histoplasma, Blastomyces, Paracoc-
cidioides, and Coccidioides. They reviewed the six virulence factors then known and
proposed potential candidate virulence factors. They also reviewed pulmonary de-
fenses, such as complement, immunoglobulins, defensins, and collectins. When the
article was published, the authors anticipated the completion of genomic sequencing
for pathogenic fungi, such as Coccidioides, would provide additional candidate viru-
lence factors (85). With the completion of the genomic sequences of Coccidioides, the
identification of additional virulence factors is a potential area for future research.
A 2012 study using next-generation sequencing (NGS) assessed gene expression
and identified genes differentially expressed between the saprobic and parasitic
growth phases of both C. immitis and C. posadasii. The authors suggest there are genes
with unknown functions that may contribute to fungal growth and virulence (86).
Viriyakosol and colleagues complemented this study in 2013, investigating differential
gene expression in day 2 mycelia and day 8 spherules. By examining a number of gene
products and comparing their functions with those of homologous genes in other
fungi, they were able to speculate about the functions of either up- or downregulated
genes in the various coccidioidal growth phases (87). Similar studies would be valuable
in understanding early events in Coccidioides infection. An intriguing prospect for
Coccidioides gene expression was suggested by Lewis et al. when they noted that the
last common ancestor of both C. immitis and C. posadasii underwent gene expansion
for proteases, keratinases, membrane biology, and toxin production (11). Perhaps these
gene products could be targets for further studies. Gene disruption remains an impor-
Downloaded from https://journals.asm.org/journal/cmr on 04 February 2023 by 2806:290:a80b:cc8:c419:e160:befc:f9a8.
tant strategy in vaccine development. Narra and colleagues’ recent development of a
protective, avirulent strain of Coccidioides by deletion of the chloroplast protein syn-
thesis gene (cps1) is an example of how a virulence factor in one pathogen, Cochliobolus
heterostrophus (a maize pathogen), can lead to discovery of analogous genes in other
pathogenic fungi. Interestingly, the exact function of the CPS1 gene product in Coc-
cidioides is unknown in spite of extensive study of the mutant strain as a vaccine
candidate (88). This underscores the necessity of understanding other fungal patho-
genic determinants, as they may be applicable to Coccidioides.
The increasing sophistication of proteomic techniques has enhanced rather than
diminished the work of earlier researchers in coccidioidomycosis. In 2016, Grys et al.
generated a proteome of nearly 1,400 proteins found in spherulin (a lysate of spherule
cells). They hypothesized that fungal proteins and their glycosylation patterns could be
different from those of mammals and could be used as bases for identification of fungal
elements in the host tissue. They focused on two lectins, Griffonia simplificonia lectin II
(GSL-II) and succinylated wheat germ agglutinin (sWGA), that bind to chitin, which is
composed of repeating units of N-acetylglucosamine (GlcNAc) (89). The more recent
study recalls investigations performed in the 1980s and 1990s demonstrating inhibition
of fungal GlcNAc incorporation by PMNs and PBMCs (90–92). Similarly, a general review
of urease, a virulence factor in fungal pathogens, published in 2014 might prompt
further study of the enzyme (93). Initial studies of urease in Coccidioides were reported
in the early 2000s (94, 95). These studies reported host tissue damage by the release of
ammonia from spherules via enzymatically active urease. In 2013, the findings of the
earlier urease studies were reaffirmed, as disruption of the urease (URE) and uredogly-
colate hydrolase (Ugh) genes in the fungus demonstrated less virulence (96). The role
of urease and Ugh in early coccidioidomycosis may merit further investigation. Many
studies and articles since the 1980s give glimpses into early Coccidioides dimorphism
from arthroconidia through spherules to endospores. These individual studies detail a
wide range of subjects, including enzymes associated with fungal cell wall remodeling,
host conditions that trigger arthroconidium transformation, and various cell wall
components that show potential as virulence factors or vaccine candidates. A challenge
January 2020 Volume 33 Issue 1 e00112-19 cmr.asm.org 9
Donovan et al. Clinical Microbiology Reviews
moving forward will be to tie these individual studies into a comprehensive under-
standing of early Coccidioides-host interaction.
HOST-RELATED RESPONSE
Schenten and Medzhitov published a comprehensive overview of the control of the
adaptive immune response by the innate immune system. They concluded, “however
it is becoming increasingly clear that additional layers of control may exist that
determine the choice of effector class, the magnitude and duration of the immune
response. How these regulatory mechanisms operate in the context of infections is an
exciting area for future investigations” (97). This is specifically applicable to understand-
ing the host response in coccidioidomycosis. When reviewing individual components,
such as PRRs, signaling transduction pathways, etc., it is important to be mindful of the
complex interactions between them.
In many fungal infections, early recognition and control of the pathogen is depen-
dent on its recognition by host PRRs (98). PRRs can be secreted or bound to the cell
wall. Secreted PRRs can act as opsonins and activate complement. Bound receptors are
involved in both pathogen uptake and processing, as well as T cell stimulation, such as
the MR on phagocytes. They can act as inducers of antimicrobial peptides, cytokines,
and proinflammatory chemokines (97).
In coccidioidomycosis, the most studied cell wall-bound PRRs are the TLRs and the
C-type lectin receptors (CLRs) (54, 87, 99–101). In 2004, Awasthi and Magee demon-
strated significant arthroconidium-induced upregulation of TLR2 and TLR4 gene ex-
pression, along with IL-12, in bone-marrow-derived DCs in a resistant mouse strain
(DBA/2) compared to a susceptible strain (BALB/c). They suggested the DC activation
status could be responsible for the differences in C. posadasii susceptibility (102).
Viriyakosol et al. in 2005 studied the roles of TLR2 and TLR4 in Coccidioides infections.
Downloaded from https://journals.asm.org/journal/cmr on 04 February 2023 by 2806:290:a80b:cc8:c419:e160:befc:f9a8.
Stimulation of mouse peritoneal macrophages with either live Coccidioides or formalin-
killed spherules (FKS) produced the proinflammatory cytokines TNF-␣, MIP-2, IL-6, and
IL-12. TLR2⫺/⫺ macrophages failed to produce these cytokines in response to either live
Coccidioides or FKS (52). TLR4⫺/⫺ macrophages and macrophages from TLR4-deficient
C3H/HeJ mice produced levels of cytokines similar to those in wild-type (WT) controls.
In vivo, following infection, TLR2⫺/⫺ mice showed susceptibility to Coccidioides similar
to that of WT controls. Interestingly, Awasthi demonstrated that TLR4-deficient C3H/
HeJ mice had pulmonary burdens similar to those of functional C3H/HeJ controls but
found a 10-fold reduction in spleen dissemination, indicating a role for TLR4 responses
in increased Coccidioides dissemination (103). The authors’ concluding suggestions that
multiple PRRs determine the final outcome of Coccidioides infection and that more
studies need to be done remain valid.
Of the CLRs, Dectin-1 expression has the most importance in Coccidioides infection
(52). Mice deficient in Dectin-1, which recognizes the -1,3-glucan on fungal cell walls,
produced lower levels of T helper 17 (Th17) cytokines and had increased lung fungal
burdens compared to WT mice (100, 104). Dectin-2 binds fungal ␣-mannan (105).
Dectin-2-deficient macrophages produce fewer cytokines than their WT controls but
show no differences in fungal burden. Macrophage-inducible C-type lectin (Mincle),
which binds mannose-like structure, is able to bind to Coccidioides spherules, but
reporter assays using a lacZ reporter in Mincle-expressing cells showed no activation,
indicating the Mincle receptor is not involved in Coccidioides infection (54, 100).
There are extensive studies focusing on Aspergillus and Candida suggesting several
common pathways with Coccidioides, but there are many unexplored areas. For exam-
ple, the role of IL-17 is well established in Aspergillus infection but remains poorly
understood in Coccidioides infection (106, 107). The best understood Coccidioides signal
transduction pathways are the Card 9 and MyD88 pathways in antigen-presenting cells
(APCs), such as macrophages and DCs (54, 75, 108–110). The pathway involved in the
signal transduction and activator of transcription 1 (STAT-1) gene mutation that leads
to impairment of the IFN-␥/IL-12 receptor and increases susceptibility to DCM is not
well known (111). Similarly, while not essential to Coccidioides immunity, the signal
January 2020 Volume 33 Issue 1 e00112-19 cmr.asm.org 10
Early Events in Coccidioidomycosis Clinical Microbiology Reviews
transduction pathways involved in the PRRs Dectin-2, MR, and SP-A/SP-D are not known
(54, 74).
The study of host genes and their expression in response to Coccidioides infection
has its roots in a 1999 study by Fierer et al. that was the first to map coccidioidomycosis
susceptibility to loci on murine chromosomes 4 and 6 (112). ROS and NO are produced
by mammalian cells (particularly phagocytes) against several microbial pathogens (113,
114). Studies have also examined the roles of ROS and NO in host defense against
Coccidioides. These studies suggested they have limited roles in protective immunity
against coccidioidomycosis but may contribute to immune modulation (110, 115–117).
Future research into the early pathogen-host interaction of coccidioidomycosis may
shed light on this subject. Gonzalez reviewed previous studies on the role of arginase
in Coccidioides and succinctly described how arginase upregulation may decrease the
level of NO production, allowing fungal survival (74). Lewis et al. found two proteins
differentially expressed in BALF from mice on day 5 postinfection. Two other gene
expression products are the proteins aminopeptidase N and annexin A5, which reduce
inflammation and degranulation/apoptosis, respectively (118). A 2017 article by Van
Dyken et al. demonstrated that the absence of one of two mammalian chitinases, acidic
mammalian chitinase (AMCase), secreted from lung epithelial cells, such as club and
type II alveolar cells, can lead to an accumulation of chitin. The AMCase-deficient mice
in the study were more prone to develop interstitial lung diseases, such as spontaneous
pulmonary fibrosis (119). Deficiency of this enzyme or chitotriosidase, the other hydro-
lase mentioned in the article, has not been investigated in pulmonary coccidioidomy-
cosis.
Perhaps no subject in the study of Coccidioides has been of more interest over the
last 30 years than the signaling cytokines between immune cells. Slagle, Cox, and
Kuruganti were the first to demonstrate that C. immitis activates TNF-␣, a cytokine that
Downloaded from https://journals.asm.org/journal/cmr on 04 February 2023 by 2806:290:a80b:cc8:c419:e160:befc:f9a8.
can activate PMNs, augment NK cells, promote T cell and B cell proliferation, and
modulate endothelial cell surface antigens, thus ushering in studies of the interaction
between innate and adaptive immune responses to Coccidioides infection. They sug-
gested the idea of cytokine production being “rapidly upregulated and downregu-
lated,” which appears to promote a protective response to Coccidioides infection (120).
A 1995 study by Magee and Cox elucidated early cytokine interaction with Th1 and Th2
cells in C. immitis infection (121). Published well before the appreciation of multiple Th
cell subsets, their work in coccidioidomycosis tied the “protective effects” of the Th1
pathway and the “nonprotective effects” of the Th2 pathways. Studies and review
articles by Ampel et al. and Lewis et al. in 2015 provide an overview of the current
known main aspects of murine and human cytokine production (11, 122).
IMMUNE RESPONSE
It is becoming clear that the immune response is not easily divided temporally or
into distinct processes of an early innate response and later adaptive response. Under-
standing the complex interaction between the innate and adaptive immune systems
remains a formidable task in Coccidioides research.
Innate Immunity
Muñoz-Hernández and colleagues have reported that innate immunity protects
healthy individuals from Coccidioides infection in 70% of cases (123). This percentage is
an intriguing contention; however, the exact derivation has not been elucidated and
may merit further investigation. To deepen the complexity, recent studies expanded
the cells generally considered part of the innate response in the lungs, such as PMNs,
macrophages, DCs, eosinophils, and NK cells, to include ILCs, iNKT cells, ␥␦ T cells, and
epithelial cells (16, 17). Soluble components of the innate immune system include
complement, collectins, and antimicrobial peptides, such as defensins.
PMNs are among the first cell responders and are the most studied component of
the innate immune system’s response to Coccidioides. A previous study of early PMN
migration and the importance of complement (124) was reinforced by Lee et al. in 2015
January 2020 Volume 33 Issue 1 e00112-19 cmr.asm.org 11
Donovan et al. Clinical Microbiology Reviews
(49). PMNs phagocytize arthroconidia and endospores but kill less than 20 to 30% (15).
They are even less efficient at killing spherules (125). This paradox has not yet been
resolved. An intriguing concept is that PMNs can promote the conversion of arthro-
conidia into spherules; however, the histopathology in the early days of a mouse
infection showed few to no PMNs immediately surrounding the developing spherule
(71, 91). In 2007, Rubin-Bejerano et al. reported that the minor fungal cell wall
component -1,6-glucan is more stimulating to PMNs than the abundant -1,3-glucan
(126). This has not been studied in Coccidioides, and in fact, only one study mentions
-1,6-glucan as a component of the Coccidioides cell wall (54). Any relevance of this cell
wall component to Coccidioides infection is unknown. A 2015 study reported that
depletion of neutrophils (PMNs) did not increase mortality in mice infected with
Coccidioides, but they appeared to be required for vaccine immunity to develop (99).
The study points to the potential inflammatory and anti-inflammatory abilities of
neutrophils (PMNs) in Coccidioides infection and underscores the need to better
understand the intricacy of the relationship between the innate and adaptive immune
systems.
Monocytes are precursors to tissue macrophages and DCs; however, in many
Coccidioides studies, PBMCs are the focus and include macrophage and DC precursors,
as well as B cells, T cells, and NK cells. Studies in the 1990s in which PBMCs were
separated showed that fractions that were predominantly monocytes were capable of
killing arthroconidia (92, 127). Beaman and associates isolated macrophages and
demonstrated that unstimulated macrophages were not able to kill arthroconidia and
endospores but that the addition of previously activated T lymphocytes improved
macrophage killing (9, 128). These studies were another step forward in understanding
innate and adaptive immune system cooperation in Coccidioides clearance. The above-
Downloaded from https://journals.asm.org/journal/cmr on 04 February 2023 by 2806:290:a80b:cc8:c419:e160:befc:f9a8.
mentioned 1991 study hypothesized that “at the time of infection and before the
development of specific immunity, peripheral blood monocytes, polymorphonuclear
leukocytes, and perhaps natural killer cells limit the survival of C. immitis. Subsequently,
specific cellular immunity develops against those fungi which have survived. Severe
coccidioidomycosis would then occur when both the nonspecific defenses and the
specific cellular immune responses are overcome” (92). In the respiratory tract, macro-
phages are found in the interstitial space and in the alveoli, where they are “tethered”
to type II alveolar cells (30). The exact mechanism of their interaction with arthroconidia
or spherules remains unknown.
In 2012, Roy and Klein extensively explored and summarized the role of DCs in
antifungal immunity. They described DCs’ pivotal position between the innate and
adaptive immune systems by driving and fine-tuning the Th response to clear the
fungus with minimal host damage (129). In Coccidioides, it has been shown that DCs can
ingest killed spherules and stimulate T lymphocytes via CLR and TLR receptors (102,
108, 130). DCs have been proposed as adjuvants for a Coccidioides vaccine or for
therapeutic use in patients with DCM to reset an effective cell-mediated immune
response, but these proposals require further study, as preliminary results in mice were
ambiguous (131, 132).
Dickson and Gifford long ago noted that patients’ eosinophil counts were highest
when erythema nodosum (EN) first appeared (6). Later articles suggested that eosino-
philia and eosinophilic microabscesses correlate with progressive disease and poor
prognosis (133, 134). Beyond their role as a clinical marker, eosinophils’ function in
Coccidioides infection is unknown.
NK cells are lymphocytes that are considered components of the innate immune
system and that induce apoptosis and are essential to early responses to viruses and
tumor cells, and their role in fungal infections has generated renewed interest (135).
Recent studies suggest NK cells, long considered innate immune cells, can demonstrate
qualities of acquired immunity, such as memory (136). Petkus and Baum suggested NK
cells are involved in the early resolution of coccidioidal lung infection (137). It was later
speculated that NK cell production of IFN-␥ indirectly reduces the Coccidioides fungal
January 2020 Volume 33 Issue 1 e00112-19 cmr.asm.org 12
Early Events in Coccidioidomycosis Clinical Microbiology Reviews
burden (138). There are no recent studies of NK cell significance in combating early
Coccidioides infection.
More recently identified innate immune cells include ILCs, iNKT cells, and ␥␦ T cells.
Now categorized into individual groups of cells, ILCs are believed to be involved in
immunity and tissue repair (139, 140). Little is known about ILCs’ role in antifungal
immunity in the lung, and there are no studies of ILCs, iNKT cells, or ␥␦ T cells in the
host response to Coccidioides infection (17, 141).
Complement is considered a key feature of the innate immune system that has
variable pathways leading to recruitment of inflammatory cells, opsonization, and cell
membrane perforation. The role of complement has long been suggested in early
Coccidioides infection with respect to PMN response (90, 124, 142). Lower CH50 (the
CH50 measures the total hemolytic activity of a test sample and is the reciprocal of the
dilution of serum complement needed to lyse 50% of a standardized suspension of
sheep erythrocytes coated with antierythrocyte antibody) levels have been associated
with DCM (142). A more recent study emphasizes the importance of complement in the
short-range redirection of recruited immune cells from host to pathogen (49). In spite
of this, complement involvement in the control of early Coccidioides infection remains
largely unknown.
Other soluble innate immune system components include the collectins, defensins,
and antimicrobial peptides (59, 143, 144). Only one study has investigated the role of
the collectins SP-A and SP-D in coccidioidomycosis. The authors speculated that SP-A
and SP-D reduction could lead to disease progression and fungal dissemination (58).
The “target” for SP-A, and SP-D has not been defined (145). Mannose-binding lectin
(MBL), a soluble collectin that is synthesized in the liver and activates complement, was
found to be low in patients with active coccidioidomycosis (146). Other defensins
include neutrophil peptide 1 (NP-1) and NP-2, which were demonstrated by Segal et al.
Downloaded from https://journals.asm.org/journal/cmr on 04 February 2023 by 2806:290:a80b:cc8:c419:e160:befc:f9a8.
in rabbit granulocytes and have antimicrobial action against arthroconidia. They antic-
ipated a search for peptides analogous to NP-1 and NP-2 in humans with and without
coccidioidal infection (147). This search remains to be completed. The study was
included in De Lucca and Walsh’s 1999 review of various hosts’ antimicrobial peptide
production in defense against pathogenic fungi. The authors noted that antifungal
peptides are classified by their modes of action as either acting to lyse fungal cells or
interfering with cell wall synthesis or biosynthesis of essential cellular components,
such as glucan or chitin. In the mammalian host, they reviewed a number of defensins,
including NP-1 to NP-5 and human neutrophil peptide 1 (HNP-1) to HNP-3, along with
other antifungal peptides (143). Ordonez et al. recently expanded this review with an
update on the current knowledge of soluble innate effector molecules in lung defense
against fungi (144). In 1974, Collins and Pappagianis demonstrated the antimicrobial
peptide lysozyme’s role in spherule development inhibition (148). There are no recent
studies of collectins, defensins, or antimicrobial products in Coccidioides infection.
Adaptive Immunity
Successful host immune response to Coccidioides infection is cell mediated, and
increased susceptibility is due to a defective cell-mediated immune (CMI) response
(149). The genesis of this understanding has its roots in Smith’s standardization of the
mycelium-derived coccidioidin skin test in the 1930s (150, 151). The test and its
successor, which is spherule derived, detect delayed-type hypersensitivity (DTH) reac-
tion and demonstrate T cell activation (152). Zweiman and colleagues reported that
coccidioidin-induced lymphocytes from Coccidioides-immune subjects proliferated at a
higher rate than those from nonimmune subjects (153). Since that time, there have
been numerous studies involving the T cell response to Coccidioides. The question
posed by Stevens in 1995, when he asked whether coccidioidomycosis progression was
the result of deficient CMI response secondary to antigen overload, suppressor (regu-
latory) cells, immune complexes (ICs), or fungal immune-suppressive substances, re-
mains relevant (154). The discovery of PRRs in ciliated, club, goblet, and type I/II alveolar
cells, along with those on alveolar macrophages and DCs, begs the question of just how
January 2020 Volume 33 Issue 1 e00112-19 cmr.asm.org 13
Donovan et al. Clinical Microbiology Reviews
early the adaptive immune system is engaged in response to Coccidioides infection and
underscores how much there is to learn about its interaction with the innate immune
system.
Studies of the adaptive immune system in Coccidioides infection have focused
mainly on T cells. Catanzaro et al. asked an important question in 1975, inquiring
whether T cell dysregulation in Coccidioides infection is a matter of an intrinsic lymphocyte
defect or is induced by the fungus itself (155). More recent studies have focused on
gene mutation in patients susceptible to DCM, suggesting the first part of this question,
but the latter part may merit further investigation (26, 27, 111, 156). The importance of
T cells became clear by the 1970s (53, 157, 158). Studies over the last 40 years have
demonstrated the importance of Th cells in the host response to fungal infections while
expanding the known Th subsets to include Th1, Th2, Th17, regulatory T (Treg), T
follicular helper (Tfh), Th9, Th22, and Th25 cells (108, 109). The response of the first
three subsets to APC presentation of Coccidioides antigen is well documented and was
reviewed by Teixeira and Barker (5). Nonetheless, the roles of other Th subsets in the
host response to coccidioidomycosis and the complex interplay of all known (and
unknown) subsets require further study.
While the critical importance of T cells in successful host response to Coccidioides is
well documented, the role of B cells in a successful host response is much less
established. Casadevall reviewed this question in a number of fungal infections with the
premise that antibody (B cell) immunity in fungal infections is a controversial subject
(159). This controversy still remains in coccidioidal research. An early study of B cells in
Coccidioides documented an unsuccessful attempt to transfer passive immunity be-
tween immune and nonimmune mice (160). A recent unpublished study by Shubitz and
Frelinger showed similar results. Ibrahim and Pappagianis demonstrated a correlation
between high serum antibody titers and more severe disease, which is evidence of the
Downloaded from https://journals.asm.org/journal/cmr on 04 February 2023 by 2806:290:a80b:cc8:c419:e160:befc:f9a8.
lack of a protective role for antibodies (161). There is conjecture in a 2004 article that
monoclonal antibodies with protective effects might be found by utilizing monoclonal
antibody technology, as was done for C. neoformans (42). Despite previous evidence to
the contrary, investigators have reported that B cells are required for a protective
vaccine response in mice (162, 163). A recent study abrogating B cells with anti-CD20
antibody during immunization was not able to corroborate these findings. In the study,
mice treated with anti-CD20 developed the same immunity as normal C57BL/6 mice
(L. F. Shubitz and J. A. Frelinger, unpublished data). There is some evidence that B cells
may play a role in host control of coccidioidomycosis, but the bulk of current knowl-
edge does not support this, and therefore further research is warranted.
There are conflicting data on the role of ICs (soluble Coccidioides antigen bound to
antibody). Yoshinoya and colleagues found ICs in a significant number of patients with
active coccidioidomycosis and proposed that they depressed T cell-mediated DTH
responses, inhibited antibody-dependent cell-mediated cytotoxicity, and suppressed
the chemotactic response of PMNs (164). These findings were later challenged in a 1987
study demonstrating that ICs did not suppress lymphocyte transformation. They ad-
vocated further investigations, but none have been pursued (165).
CLINICAL ASPECTS OF COCCIDIOIDOMYCOSIS
Brown and colleagues in 2013 summarized the history, ecology, geographic range,
and risk factors of coccidioidomycosis and concluded that early diagnosis and treat-
ment could lead to improved outcomes, reduced (patient) anxiety, and fewer proce-
dures/treatments (166). Their article and others have identified the “traditional” at-risk
populations for progressive coccidioidomycosis, including people with African ethnic-
ity, Filipinos, pregnant women, and the immunocompromised (24, 166, 167). For the
foreseeable future, awareness of these broader groups will remain important and will
likely be a touchstone as researchers discover specific gene mutations and their
products that could identify at-risk individuals for more serious forms of progressive
disease (27). Efforts and success in this regard could lead to earlier interventions,
targeted treatments, and fewer disease complications.
January 2020 Volume 33 Issue 1 e00112-19 cmr.asm.org 14
Early Events in Coccidioidomycosis Clinical Microbiology Reviews
Symptoms of pulmonary coccidioidomycosis are thought to appear from 1 to
3 weeks (average, 2 weeks) after exposure (22). Researchers at California military bases
during World War II meticulously compiled a comprehensive list of early coccidioido-
mycosis symptoms from the large influx of young, generally healthy, and previously
unexposed males. They noted, in descending order, the percentages with fever, chest
pain, cough, malaise, anorexia, headache, pharyngitis, chills, joint manifestations, EN,
conjunctivitis, erythema multiforme (EM), urticaria, and hemoptysis as presenting
symptoms (168). Later studies, each with a smaller but more diverse population,
reported similar symptoms and percentages, which supports the continued relevance
of the 1945 study (169, 170). The 1996 study, which focused on the symptoms chest
pain, EN, fever, cough, and rash, along with chest X-ray findings, skin test results, and
laboratory values, highlighted the “crossover” of coccidioidomycosis with other respi-
ratory illnesses and, more importantly, estimated that one- to two-thirds of standard
coccidioidal serologic tests may miss the diagnosis (169). It should be noted that this
study utilized unconcentrated sera, but current protocols generally use concentrated
sera in immunodiffusion tests to improve the diagnostic yield (171, 172).
Historically, as with other diseases, a proper coccidioidomycosis diagnosis has relied
upon patient history; symptoms; basic laboratory tests, such as complete blood count
(CBC); erythrocyte sedimentation rate (ESR); eosinophil count; and chest X-ray, but
these all lack specificity. Obtaining a diagnosis with fungal culture or histopathology,
while definitive, can be labor-intensive, invasive, and expensive. A recent article has
advocated for the return of skin testing (a positive test for the cell-mediated DTH
response proves patient immunity) with the second-generation spherule extract
Spherusol. The authors suggested wider use could aid in clinical response to treatment;
be of value in prevalence studies; and identify high-risk occupational exposures, as well
as those who would not need vaccination (152). A recent study reported potential
Downloaded from https://journals.asm.org/journal/cmr on 04 February 2023 by 2806:290:a80b:cc8:c419:e160:befc:f9a8.
limitations of skin testing, including the possibility that it might not always identify past
controlled infections and has lower positive rates than previously reported (173, 174).
Nonetheless, a 2018 study demonstrated the successful use of large-scale skin testing
to stratify inmate risk in a coccidioidomycosis prevention program within the California
prison system (175).
Serologic testing remains the mainstay of coccidioidomycosis diagnosis. Pappa-
gianis and Zimmer authored a comprehensive overview of the history and utility of
serological testing that remains a reference (176). The need to improve the availability,
ease of use, rapidity, reliability, and cost of coccidioidomycosis testing has sparked
development of lateral-flow assays (LFAs), which show promise as easy to use point-
of-care tests that will speed diagnosis and lessen antibiotic overuse in coccidioidomy-
cosis (177). The contrary view could argue that earlier confirmation of VF may not
appreciably change clinician antibiotic-prescribing habits or might lead to increased
and unnecessary use of antifungals. At such time as these tests become available,
studies of this may be valuable. Resolving such questions is facilitated by utilizing the
expanding ability of electronic medical records (EMRs) to mine data and perform
analytics to ascertain if new tests, such as the LFA, or clinical interventions actually have
the desired effects of improved antibiotic stewardship, providing better patient out-
comes, or lowering health care costs (178–180).
Another relatively new coccidioidomycosis diagnostic test is real-time PCR (RT-PCR),
which has the advantage of a 4-h turnaround time and high sensitivity and specificity
for specimens obtained from BALF or bronchial wash (BW) fluid. The most notable
disadvantage for use of PCR is lower sensitivity and specificity in tissue specimens other
than BALF and BW fluid (181–183).
Treatment decisions for coccidioidomycosis can be challenging due to variable
presentations and prognoses. Noting that 60% of those who acquire Coccidioides
infection are asymptomatic and the other 40% may have a pulmonary syndrome,
recent treatment recommendations advise observation in otherwise healthy or recov-
ering patients and reserve potential antifungal treatment for those with severe disease
or persistent symptoms or the immunocompromised (20). The Infectious Diseases
January 2020 Volume 33 Issue 1 e00112-19 cmr.asm.org 15
Donovan et al. Clinical Microbiology Reviews
Society of America (IDSA) guidelines and recent summary guide are excellent resources
for treatment options (184, 185). Ironically, in an effort to diagnose coccidioidomycosis
earlier, and in spite of diagnostic advancements, experts have returned to an earlier era,
placing renewed emphasis on patient history, symptoms, and examination. They are
asking clinicians to remember the mnemonic C-O-C-C-I and consider the diagnosis,
order the appropriate tests, check for risk factors, check for complications, and initiate
management (21).
Another important consideration for treatment decisions is the recognition of
potential resistant Coccidioides isolates, which could alter the clinician’s choice of the
triazole medication class. This class of antifungal medications includes the most com-
monly used, fluconazole, along with itraconazole, posaconazole, and voriconazole
(186). This concern, coupled with the protracted treatment course usually utilized for
those with progressive coccidioidomycosis, highlights the need to develop improved
treatments, such as that offered by a chitin synthase inhibitor, nikkomycin Z, or a new
class of medications, the Gwt1 inhibitors, such as APX001 (fosmanogepix) and its active
compound, APX001A (manogepix) (187, 188). Other agents under investigation include
olorofim, an orotomide analog investigated for central nervous system coccidioidomy-
cosis, and fungal CYP51 inhibitors, such as oteseconazole, studied in canine respiratory
coccidioidomycosis (189, 190). In spite of the substantial financial hurdle to developing
treatment for an “orphan disease” such as coccidioidomycosis, the coupling of ad-
vancements recognizing at-risk individuals with development of a potentially shorter-
course curative medication could more than compensate for the medication’s devel-
opment costs (27).
CONCLUDING REMARKS
There are challenges to making advancements in understanding early pathogen-
Downloaded from https://journals.asm.org/journal/cmr on 04 February 2023 by 2806:290:a80b:cc8:c419:e160:befc:f9a8.
host events in coccidioidomycosis. Fortunately, there are strategies and solutions to
overcome these obstacles. As mentioned above, understanding of early events in
coccidioidomycosis is limited by the inability to study the early pathogen-host inter-
action. This is complicated by the hazardous nature of the fungus, requiring an ABSL3
facility for handling fungal cultures. A strategy to meet this challenge would include
ongoing development or discovery of less virulent Coccidioides strains and the devel-
opment of new technologies or computer modeling that could provide insight into
early pathogen-host interaction in a safe and efficient manner. Another challenge in
understanding early coccidioidomycosis is how and why nearly 60% of those exposed
have few symptoms and develop lifelong immunity. This requires further means to
investigate the innate and adaptive immune systems and their complex interaction in
response to the fungus. Greater collaborative efforts among clinicians, research groups,
and industry would be a way forward.
The lack of coccidioidomycosis awareness, even among health care providers in
areas of endemicity, is an ongoing issue leading to unnecessary health care utilization
and cost. An example of a simple solution to this problem is the subject of a recent
study utilizing EMR that demonstrates potential cost savings and improved antibiotic
stewardship with earlier coccidioidomycosis diagnosis (178). As is the case with other
diseases, coccidioidomycosis is considered an “orphan disease” and, as such, oftentimes
faces funding challenges. One solution is the development of simpler and cost-effective
studies, such as an ongoing project examining efforts to raise VF awareness among
primary health care providers in an area where Coccidioides is endemic that will assess
if such interventions improve patient outcomes and lower costs (F. M. Donovan and
J. N. Galgiani, unpublished data). Another challenge shared by pharmaceutical compa-
nies and research groups is the use and success of biologics, immune-suppressive
agents, and chemotherapy medications. In areas where coccidioidomycosis is endemic,
there is justified concern about and evidence of increased susceptibility of previously
healthy patients treated with these medications, along with potential reactivation of
dormant disease or waning immunity in an aging population. A solution would be the
development of tests that are simpler and more consistent than the current skin test
January 2020 Volume 33 Issue 1 e00112-19 cmr.asm.org 16
Early Events in Coccidioidomycosis Clinical Microbiology Reviews
that could identify or monitor Coccidioides immunity and thereby help guide therapy
and lessen complications from these valuable medications. Probably the most signifi-
cant research challenge going forward is recognizing Coccidioides as a unique fungal
entity that is on the top of the invasive fungal pyramid. Its complex life cycle, structure,
and early interaction with the host pose a formidable research problem. Strategies to
improve understanding will require integration of bioinformatics, genetics, and pro-
teomics, along with the training of a new generation of research scientists who are well
versed in these disciplines and inspired by the previous generation’s experience and
enthusiasm.
ACKNOWLEDGMENTS
We report no conflict of interest.
This work received no specific grant from any funding agency in the public,
commercial, or not-for-profit sector.
REFERENCES
1. Posadas A. 1892. Un nuevo caso de micosis fungoidea con psorosper- 19. Valdivia L, Nix D, Wright M, Lindberg E, Fagan T, Lieberman D, Stoffer
mias. An Circ Med Argent 15:585–597. T, Ampel NM, Galgiani JN. 2006. Coccidioidomycosis as a common
2. Ophuls W, Moffitt HC. 1900. A new pathogenic mould. (Formerly cause of community-acquired pneumonia. Emerg Infect Dis 12:
described as a protozoon: Coccidioides immitis pyogenes.) Preliminary 958 –962. https://doi.org/10.3201/eid1206.060028.
report. Philadelphia Med J 5:1471–1472. 20. Ampel NM. 2015. The treatment of coccidioidomycosis. Rev Inst Med
3. Ophuls W. 1905. Further observations on a pathogenic mold formerly Trop Sao Paulo 57(Suppl 19):51–56. https://doi.org/10.1590/S0036
described as a protozoan (Coccidioides immitis, Coccidioides pyo- -46652015000700010.
genes). J Exp Med 6:443– 486. https://doi.org/10.1084/jem.6.4-6.443. 21. Galgiani JN, Thompson GR, III, Board of Valley Fever Alliance of Arizona
4. Teixeira MM, Barker BM. 2016. Use of population genetics to assess the Clinicians. 2016. Valley Fever (coccidioidomycosis) tutorial for primary care
ecology, evolution, and population structure of Coccidioides. Emerg professionals. Valley Fever Center for Excellence, The University of Arizona,
Infect Dis 22:1022–1030. https://doi.org/10.3201/eid2206.151565. Tucson, AZ. http://www.vfce.arizona.edu/sites/vfce/files/tutorial_
5. Teixeria MM, Barker B. 2017. Coccidioides and coccidioidomycosis, p for_primary_care_professionals.pdf.
Downloaded from https://journals.asm.org/journal/cmr on 04 February 2023 by 2806:290:a80b:cc8:c419:e160:befc:f9a8.
255–280. In Mora-Montes H, Lopes-Bezerra L (ed), Current progress in 22. Smith CE. 1940. Epidemiology of acute coccidioidomycosis with ery-
medical mycology. Springer, Cham, Switzerland. https://doi.org/10 thema nodosum. Am J Public Health Nations Health 30:600 – 611.
.1007/978-3-319-64113-3_8. https://doi.org/10.2105/ajph.30.6.600.
6. Dickson EC, Gifford MA. 1938. Coccidioides infection (coccidioidomy- 23. Fiese MJ, Cheu S, Sorensen RH. 1955. Mycelial forms of Coccidioides
cosis). II. The primary type of infection. Arch Intern Med 62:853– 871. immitis in sputum and tissues of the human host. Ann Intern Med
https://doi.org/10.1001/archinte.1938.00180160132011. 43:255–270.
7. Smith CE, Beard RR. 1946. Effect of season and dust control on coccid- 24. Drutz DJ, Catanzaro A. 1978. Coccidioidomycosis. Part II. Am Rev Respir
ioidomycosis. JAMA 132:833– 838. https://doi.org/10.1001/jama.1946 Dis 117:727–771. https://doi.org/10.1164/arrd.1978.117.4.727.
.02870490011003. 25. Thompson GR, III, Bays D, Taylor SL, Cohen SH, Pappagianis D. 2013.
8. Baker O, Braude AI. 1956. A study of stimuli leading to the prodution of Association between serum 25-hydroxyvitamin D level and type of
spherules in coccidioidomycosis. J Lab Clin Med 47:169 –181. coccidioidal infection. Med Mycol 51:319 –323. https://doi.org/10.3109/
9. Beaman L, Holmberg CA. 1980. In vitro response of alveolar macro- 13693786.2012.690536.
phages to infection with Coccidioides immitis. Infect Immun 28: 26. Vinh DC, Masannat F, Dzioba RB, Galgiani JN, Holland SM. 2009. Re-
594 – 600. fractory disseminated coccidioidomycosis and mycobacteriosis in
10. Cole GT, Sun SH. 1985. Arthroconidium-spherule-endospore transfor- interferon-gamma receptor 1 deficiency. Clin Infect Dis 49:e62– e65.
mation in Coccidioides immitis, p 281–333. In Szaniszlo PJ (ed), Fungal https://doi.org/10.1086/605532.
dimorphism. Plenum Publishing Corp., New York, NY. 27. Odio CD, Marciano BE, Galgiani JN, Holland SM. 2017. Risk factors for
11. Lewis ER, Bowers JR, Barker BM. 2015. Dust devil: the life and times of disseminated coccidioidomycosis, United States. Emerg Infect Dis 23:4.
the fungus that causes valley fever. PLoS Pathog 11:e1004762. https:// https://doi.org/10.3201/eid2302.160505.
doi.org/10.1371/journal.ppat.1004762. 28. Huppert M, Sun SH, Harrison JL. 1982. Morphogenesis throughout
12. Cole GT, Hung CY. 2001. The parasitic cell wall of Coccidioides immitis. saprobic and parasitic cycles of Coccidioides immitis. Mycopathologia
Med Mycol 39:31– 40. https://doi.org/10.1080/744118874. 78:107–122. https://doi.org/10.1007/bf00442634.
13. Ganesan S, Comstock AT, Sajjan US. 2013. Barrier function of airway 29. Mead HL, Teixeira MM, Galgiani JN, Barker BM. 2018. Characterizing in
tract epithelium. Tissue Barriers 1:e24997. https://doi.org/10.4161/tisb vitro spherule morphogenesis of multiple strains of both species of
.24997. Coccidioides. Med Mycol 57:478 – 488. https://doi.org/10.1093/mmy/
14. Ampel NM, Hoover SE. 2015. Pathogenesis of coccidioidomycosis. Curr myy049.
Fungal Infect Rep 9:253–258. https://doi.org/10.1007/s12281-015-0242-1. 30. Hussell T, Bell TJ. 2014. Alveolar macrophages: plasticity in a tissue-
15. Drutz DJ, Huppert M. 1983. Coccidioidomycosis: factors affecting the specific context. Nat Rev Immunol 14:81–93. https://doi.org/10.1038/
host-parasite interaction. J Infect Dis 147:372–390. https://doi.org/10 nri3600.
.1093/infdis/147.3.372. 31. Converse JL. 1955. Growth of spherules of Coccidioides immitis in a
16. Werner JL, Steele C. 2014. Innate receptors and cellular defense against chemically defined liquid medium (22144). Proc Soc Exp Biol Med
pulmonary infections. J Immunol 193:3842–3850. https://doi.org/10 90:709 –711. https://doi.org/10.3181/00379727-90-22144.
.4049/jimmunol.1400978. 32. Converse JL. 1957. Effect of surface active agents on endosporulation
17. Chen K, Kolls JK. 2013. T cell-mediated host immune defenses in the of Coccidioides immitis in a chemically defined medium. J Bacteriol
lung. Annu Rev Immunol 31:605– 633. https://doi.org/10.1146/annurev 74:106 –107.
-immunol-032712-100019. 33. Lones GW, Peacock CL. 1960. Studies of the growth and metabolism of
18. Smith CE, Beard RR, Whiting EG, Rosenberger HG. 1946. Varieties of Coccidioides immitis. Ann N Y Acad Sci 89:102–108. https://doi.org/10
coccidioidal infection in relation to the epidemiology and control of .1111/j.1749-6632.1960.tb20134.x.
the disease. Am J Public Health Nations Health 36:1394 –1402. https:// 34. Lones GW, Peacock CL. 1960. Role of carbon dioxide in the dimorphism
doi.org/10.2105/ajph.36.12.1394. of Coccidioides immitis. J Bacteriol 79:308 –309.
January 2020 Volume 33 Issue 1 e00112-19 cmr.asm.org 17
Donovan et al. Clinical Microbiology Reviews
35. Breslau AM, Kubota MY. 1964. Continuous in vitro cultivation of spher- pulmonary innate immunity. Nat Immunol 16:27–35. https://doi.org/10
ules of Coccidioides immitis. J Bacteriol 87:468 – 472. .1038/ni.3045.
36. Wheat RW, Tritschler C, Conant NF, Lowe EP. 1977. Comparison of 58. Awasthi S, Magee DM, Coalson JJ. 2004. Coccidioides posadasii infec-
Coccidioides immitis arthrospore, mycelium, and spherule cell walls, tion alters the expression of pulmonary surfactant proteins (SP)-A and
and influence of growth medium on mycelial cell wall composition. SP-D. Respir Res 5:28. https://doi.org/10.1186/1465-9921-5-28.
Infect Immun 17:91–97. 59. Leiva-Juarez MM, Kolls JK, Evans SE. 2018. Lung epithelial cells: thera-
37. Cole GT, Kirkland TN, Sun SH. 1987. An immunoreactive, water-soluble peutically inducible effectors of antimicrobial defense. Mucosal Immu-
conidial wall fraction of Coccidioides immitis. Infect Immun 55:657–667. nol 11:21–34. https://doi.org/10.1038/mi.2017.71.
38. Bayry J, Aimanianda V, Guijarro JI, Sunde M, Latge JP. 2012. Hydropho- 60. Austwick PKC. 1980. The pathogenic aspects of the use of fungi: the
bins— unique fungal proteins. PLoS Pathog 8:e1002700. https://doi need for risk analysis and registration of fungi. Ecol Bull 31:91–102.
.org/10.1371/journal.ppat.1002700. 61. Deresinski SC, Levine HB, Stevens DA. 1978. Coccidioides immitis
39. Ward ER, Jr, Cox RA, Schmitt JA, Jr, Huppert M, Sun SH. 1975. Delayed- endospores: phagocytosis by human cells. Mycopathologia 64:
type hypersensitivity responses to a cell wall fraction of the mycelial 179 –181. https://doi.org/10.1007/bf00576371.
phase of Coccidioides immitis. Infect Immun 12:1093–1097. 62. Nesbit LA, Knox KS, Nguyen CT, Roesch J, Wheat LJ, Johnson SM,
40. Cox RA, Huppert M, Starr P, Britt LA. 1984. Reactivity of alkali-soluble, Pappagianis D, Chavez S, Ampel NM. 2013. Immunological character-
water-soluble cell wall antigen of Coccidioides immitis with anti- ization of bronchoalveolar lavage fluid in patients with acute pulmo-
Coccidioides immunoglobulin M precipitin antibody. Infect Immun 43: nary coccidioidomycosis. J Infect Dis 208:857– 863. https://doi.org/10
502–507. .1093/infdis/jit246.
41. Kirkland TN, Zhu S, Kruse D, Hsu L, Seshan KR, Cole GT. 1991. Coccid- 63. Levine HB, Miller RL, Smith CE. 1962. Influence of vaccination on
ioides immitis fractions which are antigenic for immune T lymphocytes. respiratory coccidioidal disease in cynomolgus monkeys. J Immunol
Infect Immun 59:3952–3961. 89:242–251.
42. Cox RA, Magee DM. 2004. Coccidioidomycosis: host response and vaccine 64. Williams PL, Sobel RA, Sorensen KN, Clemons KV, Shuer LM, Royaltey SS,
development. Clin Microbiol Rev 17:804–839. https://doi.org/10.1128/ Yao Y, Pappagianis D, Lutz JE, Reed C, River ME, Lee BC, Bhatti SU,
CMR.17.4.804-839.2004. Stevens DA. 1998. A model of coccidioidal meningoencephalitis and
43. Awasthi S, Vilekar P, Conkleton A, Rahman N. 2019. Dendritic cell-based cerebrospinal vasculitis in the rabbit. J Infect Dis 178:1217–1221.
immunization induces Coccidioides Ag2/PRA-specific immune re- https://doi.org/10.1086/515689.
sponse. Vaccine 37:1685–1691. https://doi.org/10.1016/j.vaccine.2019 65. Clemons KV, Capilla J, Stevens DA. 2007. Experimental animal models
.01.034. of coccidioidomycosis. Ann N Y Acad Sci 1111:208 –224. https://doi.org/
44. Cole GT, Pshko EJ, Seshan KR. 1995. Possible roles of wall hydrolases in 10.1196/annals.1406.029.
the morphogenesis of Coccidioides immitis. Can J Bot 73:132–S1141. 66. Werner SB, Pappagianis D, Heindl I, Mickel A. 1972. An epidemic of
https://doi.org/10.1139/b95-369. coccidioidomycosis among archeology students in northern California. N
45. Breslau AM, Hensley TJ, Erickson JO. 1961. Electron microscopy of
Engl J Med 286:507–512. https://doi.org/10.1056/NEJM197203092861003.
cultured spherules of Coccidioides immitis. J Biophys Biochem Cytol
67. Jamison HW, Carter RA. 1947. The roentgen findings in early coccid-
9:627– 637. https://doi.org/10.1083/jcb.9.3.627.
Downloaded from https://journals.asm.org/journal/cmr on 04 February 2023 by 2806:290:a80b:cc8:c419:e160:befc:f9a8.
ioidomycosis. Radiology 48:323–332. https://doi.org/10.1148/48.4.323.
46. Li L, Schmelz M, Kellner EM, Galgiani JN, Orbach MJ. 2007. Nuclear
68. Jude CM, Nayak NB, Patel MK, Deshmukh M, Batra P. 2014. Pulmonary
labeling of Coccidioides posadasii with green fluorescent protein. Ann
coccidioidomycosis: pictorial review of chest radiographic and CT find-
N Y Acad Sci 1111:198 –207. https://doi.org/10.1196/annals.1406.014.
ings. Radiographics 34:912–925. https://doi.org/10.1148/rg.344130134.
47. Hector RF, Pappagianis D. 1982. Enzymatic degradation of the walls of
69. Crum NF, Lederman ER, Stafford CM, Parrish JS, Wallace MR. 2004.
spherules of Coccidioides immitis. Exp Mycol 6:136 –152. https://doi.org/
Coccidioidomycosis: a descriptive survey of a reemerging disease. Clin-
10.1016/0147-5975(82)90088-3.
ical characteristics and current controversies. Medicine 83:149 –175.
48. Frey CL, Drutz DJ. 1986. Influence of fungal surface components on the
https://doi.org/10.1097/01.md.0000126762.91040.fd.
interaction of Coccidioides immitis with polymorphonuclear neutro-
70. Shubitz LF, Dial SM, Perrill R, Casement R, Galgiani JN. 2008. Vaccine-
phils. J Infect Dis 153:933–943. https://doi.org/10.1093/infdis/153.5.933.
induced cellular immune responses differ from innate responses in
49. Lee CY, Thompson GR, Hastey CJ, Hodge GC, Lunetta JM, Pappagianis
D, Heinrich V. 2015. Coccidioides endospores and spherules draw susceptible and resistant strains of mice infected with Coccidioides
strong chemotactic, adhesive, and phagocytic responses by individual posadasii. Infect Immun 76:5553–5564. https://doi.org/10.1128/IAI
human neutrophils. PLoS One 10:e0129522. https://doi.org/10.1371/ .00885-08.
journal.pone.0129522. 71. Shubitz LP, Lewis ML, Dial SM, Galgiani J. 2011. Early post-infection
50. Hung CY, Yu JJ, Seshan KR, Reichard U, Cole GT. 2002. A parasitic detection of Coccidioides in intranasally infected mice, p 40. In Pro-
phase-specific adhesin of Coccidioides immitis contributes to the vir- ceedings of the 55th Annual Coccidioidomycosis Study Group Meeting.
ulence of this respiratory fungal pathogen. Infect Immun 70: 72. Sun SH, Cole GT, Drutz DJ, Harrison JL. 1986. Electron-microscopic
3443–3456. https://doi.org/10.1128/iai.70.7.3443-3456.2002. observations of the Coccidioides immitis parasitic cycle in vivo. J Med
51. Hung CY, Seshan KR, Yu JJ, Schaller R, Xue J, Basrur V, Gardner MJ, Cole Vet Mycol 24:183–192. https://doi.org/10.1080/02681218680000281.
GT. 2005. A metalloproteinase of Coccidioides posadasii contributes to 73. Shubitz LF, Powell DA, Trinh HT, Lewis ML, Orbach MJ, Frelinger JA,
evasion of host detection. Infect Immun 73:6689 – 6703. https://doi.org/ Galgiani JN. 2018. Viable spores of Coccidioides posadasii Deltacps1 are
10.1128/IAI.73.10.6689-6703.2005. required for vaccination and provide long lasting immunity. Vaccine
52. Viriyakosol S, Fierer J, Brown GD, Kirkland TN. 2005. Innate immunity to 36:3375–3380. https://doi.org/10.1016/j.vaccine.2018.04.026.
the pathogenic fungus Coccidioides posadasii is dependent on Toll-like 74. Gonzalez A. 2013. Innate immune response to the dimorphic fungal
receptor 2 and Dectin-1. Infect Immun 73:1553–1560. https://doi.org/ pathogen Coccidioides: molecular and cellular mechanisms. J Clin Cell
10.1128/IAI.73.3.1553-1560.2005. Immunol S13:1– 6. https://doi.org/10.4172/2155-9899.S13-001.
53. Beaman L, Benjamini E, Pappagianis D. 1983. Activation of macro- 75. Erwig LP, Gow NA. 2016. Interactions of fungal pathogens with phago-
phages by lymphokines: enhancement of phagosome-lysosome fusion cytes. Nat Rev Microbiol 14:163–176. https://doi.org/10.1038/nrmicro
and killing of Coccidioides immitis. Infect Immun 39:1201–1207. .2015.21.
54. Viriyakosol S, Jimenez MDP, Saijo S, Fierer J. 2014. Neither dectin-2 nor the 76. Lengeler KB, Davidson RC, D’Souza C, Harashima T, Shen W-C, Wang P,
mannose receptor is required for resistance to Coccidioides immitis in Pan X, Waugh M, Heitman J. 2000. Signal transduction cascades regu-
mice. Infect Immun 82:1147–1156. https://doi.org/10.1128/IAI.01355-13. lating fungal development and virulence. Microbiol Mol Biol Rev 64:
55. Garcia-Sherman MC, Lundberg T, Sobonya RE, Lipke PN, Klotz SA. 2015. 746 –785. https://doi.org/10.1128/MMBR.64.4.746-785.2000.
A unique biofilm in human deep mycoses: fungal amyloid is bound by 77. Runyanga TJ, Chen Y, Sun F. 2017. Cell communication and fungal
host serum amyloid P component. NPJ Biofilms Microbiomes 1:15009. virulence: a review. Res Rev Res J Biol 5:8 –16.
https://doi.org/10.1038/npjbiofilms.2015.9. 78. Gauthier G, Klein BS. 2008. Insights into fungal morphogenesis and
56. Wiesner DL, Klein BS. 2017. Lung epithelium: barrier immunity to immune evasion: fungal conidia, when situated in mammalian lungs,
inhaled fungi and driver of fungal-associated allergic asthma. Curr Opin may switch from mold to pathogenic yeasts or spore-forming spher-
Microbiol 40:8 –13. https://doi.org/10.1016/j.mib.2017.10.007. ules. Microbe Wash DC 3:416 – 423.
57. Whitsett JA, Alenghat T. 2015. Respiratory epithelial cells orchestrate 79. Pishko EJ, Kirkland TN, Cole GT. 1995. Isolation and characterization of two
January 2020 Volume 33 Issue 1 e00112-19 cmr.asm.org 18
Early Events in Coccidioidomycosis Clinical Microbiology Reviews
chitinase-encoding genes (cts1, cts2) from the fungus Coccidioides immitis. for MyD88-dependent Th17 immunity to Coccidioides infection. Infect
Gene 167:173–177. https://doi.org/10.1016/0378-1119(95)00654-0. Immun 82:2106 –2114. https://doi.org/10.1128/IAI.01579-13.
80. Abuodeh RO, Orbach MJ, Mandel MA, Das A, Galgiani JN. 2000. Genetic 100. Wang H, LeBert V, Hung CY, Galles K, Saijo S, Lin X, Cole GT, Klein BS,
transformation of Coccidioides immitis facilitated by Agrobacterium tu- Wuthrich M. 2014. C-type lectin receptors differentially induce th17
mefaciens. J Infect Dis 181:2106 –2110. https://doi.org/10.1086/315525. cells and vaccine immunity to the endemic mycosis of North America.
81. Mandel MA, Galgiani JN, Kroken S, Orbach MJ. 2006. Coccidioides J Immunol 192:1107–1119. https://doi.org/10.4049/jimmunol.1302314.
posadasii contains single chitin synthase genes corresponding to 101. del Pilar Jimenez AM, Viriyakosol S, Walls L, Datta SK, Kirkland T,
classes I to VII. Fungal Genet Biol 43:775–788. https://doi.org/10.1016/ Heinsbroek SE, Brown G, Fierer J. 2008. Susceptibility to Coccidioides
j.fgb.2006.05.005. species in C57BL/6 mice is associated with expression of a truncated
82. Kellner EM, Orsborn KI, Siegel EM, Mandel MA, Orbach MJ, Galgiani JN. splice variant of Dectin-1 (Clec7a). Genes Immun 9:338 –348. https://
2005. Coccidioides posadasii contains a single 1,3-{beta}-glucan syn- doi.org/10.1038/gene.2008.23.
thase gene that appears to be essential for growth. Eukaryot Cell 102. Awasthi S, Magee DM. 2004. Differences in expression of cell surface
4:111–120. https://doi.org/10.1128/EC.4.1.111-120.2005. co-stimulatory molecules, Toll-like receptor genes and secretion of
83. Johannesson H, Kasuga T, Schaller RA, Good B, Gardner MJ, Townsend IL-12 by bone marrow-derived dendritic cells from susceptible and
JP, Cole GT, Taylor JW. 2006. Phase-specific gene expression underlying resistant mouse strains in response to Coccidioides posadasii. Cell
morphological adaptations of the dimorphic human pathogenic fun- Immunol 231:49 –55. https://doi.org/10.1016/j.cellimm.2004.11.006.
gus, Coccidioides posadasii. Fungal Genet Biol 43:545–559. https://doi 103. Awasthi S. 2010. Susceptibility of TLR4-defective C3H/HeJ mice to
.org/10.1016/j.fgb.2006.02.003. Coccidioides posadasii infection. Med Mycol 48:470 – 475. https://doi
84. Delgado N, Hung CY, Tarcha E, Gardner MJ, Cole GT. 2004. Profiling .org/10.3109/13693780903226019.
gene expression in Coccidioides posadasii. Med Mycol 42:59 –71. 104. Viriyakosol S, Jimenez MDP, Gurney MA, Ashbaugh ME, Fierer J. 2013.
https://doi.org/10.1080/1369378031000156890. Dectin-1 is required for resistance to coccidioidomycosis in mice. mBio
85. Rappleye CA, Goldman WE. 2006. Defining virulence genes in the 4:e00597. https://doi.org/10.1128/mBio.00597-12.
dimorphic fungi. Annu Rev Microbiol 60:281–303. https://doi.org/10 105. Kerscher B, Willment JA, Brown GD. 2013. The Dectin-2 family of C-type
.1146/annurev.micro.59.030804.121055. lectin-like receptors: an update. Int Immunol 25:271–277. https://doi
86. Whiston E, Zhang Wise H, Sharpton TJ, Jui G, Cole GT, Taylor JW. 2012. .org/10.1093/intimm/dxt006.
Comparative transcriptomics of the saprobic and parasitic growth 106. Murdock BJ, Falkowski NR, Shreiner AB, Sadighi Akha AA, McDonald RA,
phases in Coccidioides spp. PLoS One 7:e41034. https://doi.org/10 White ES, Toews GB, Huffnagle GB. 2012. Interleukin-17 drives pulmo-
.1371/journal.pone.0041034. nary eosinophilia following repeated exposure to Aspergillus fumiga-
87. Viriyakosol S, Singhania A, Fierer J, Goldberg J, Kirkland TN, Woelk CH. tus conidia. Infect Immun 80:1424 –1436. https://doi.org/10.1128/IAI
2013. Gene expression in human fungal pathogen Coccidioides immitis .05529-11.
changes as arthroconidia differentiate into spherules and mature. BMC 107. Malacco N, Rachid MA, Gurgel I, Moura TR, Sucupira PHF, de Sousa LP,
de Souza DDG, Russo RC, Teixeira MM, Soriani FM. 2018. Eosinophil-
Microbiol 13:121. https://doi.org/10.1186/1471-2180-13-121.
associated innate IL-17 response promotes Aspergillus fumigatus lung
88. Narra HP, Shubitz LF, Mandel MA, Trinh HT, Griffin K, Buntzman AS,
pathology. Front Cell Infect Microbiol 8:453. https://doi.org/10.3389/
Downloaded from https://journals.asm.org/journal/cmr on 04 February 2023 by 2806:290:a80b:cc8:c419:e160:befc:f9a8.
Frelinger JA, Galgiani JN, Orbach MJ. 2016. A Coccidioides posadasii
fcimb.2018.00453.
CPS1 deletion mutant is avirulent and protects mice from lethal infec-
108. Castro-Lopez N, Hung CY. 2017. Immune response to coccidioidomy-
tion. Infect Immun 84:3007–3016. https://doi.org/10.1128/IAI.00633-16.
cosis and the development of a vaccine. Microorganisms 5:13. https://
89. Grys TE, Kaushal S, Chowdhury Y, Dasari S, Mitchell NM, Magee DM,
doi.org/10.3390/microorganisms5010013.
Blair JE, Colby TV, Lake DF. 2016. Total and lectin-binding proteome of
109. Geijtenbeek TB, Gringhuis SI. 2009. Signalling through C-type lectin
spherulin from Coccidioides posadasii. J Proteome Res 15:3463–3472.
receptors: shaping immune responses. Nat Rev Immunol 9:465– 479.
https://doi.org/10.1021/acs.jproteome.5b01054.
https://doi.org/10.1038/nri2569.
90. Galgiani JN, Payne CM, Jones JF. 1984. Human polymorphonuclear-
110. Hung CY, Castro-Lopez N, Cole GT. 2016. Card9- and MyD88-mediated
leukocyte inhibition of incorporation of chitin precursors into mycelia
gamma interferon and nitric oxide production is essential for resistance
of Coccidioides immitis. J Infect Dis 149:404 – 412. https://doi.org/10
to subcutaneous Coccidioides posadasii infection. Infect Immun 84:
.1093/infdis/149.3.404. 1166 –1175. https://doi.org/10.1128/IAI.01066-15.
91. Galgiani JN. 1986. Inhibition of different phases of Coccidioides immitis 111. Sampaio EP, Hsu AP, Pechacek J, Bax HI, Dias DL, Paulson ML, Chan-
by human neutrophils or hydrogen peroxide. J Infect Dis 153:217–222. drasekaran P, Rosen LB, Carvalho DS, Ding L, Vinh DC, Browne SK, Datta
https://doi.org/10.1093/infdis/153.2.217. S, Milner JD, Kuhns DB, Long Priel DA, Sadat MA, Shiloh M, De Marco
92. Ampel NM, Galgiani JN. 1991. Interaction of human peripheral blood B, Alvares M, Gillman JW, Ramarathnam V, de la Morena M, Bezrodnik
mononuclear cells with Coccidioides immitis arthroconidia. Cell Immu- L, Moreira I, Uzel G, Johnson D, Spalding C, Zerbe CS, Wiley H, Green-
nol 133:253–262. https://doi.org/10.1016/0008-8749(91)90195-h. berg DE, Hoover SE, Rosenzweig SD, Galgiani JN, Holland SM. 2013.
93. Rutherford JC. 2014. The emerging role of urease as a general microbial Signal transducer and activator of transcription 1 (STAT1) gain-of-
virulence factor. PLoS Pathog 10:e1004062. https://doi.org/10.1371/ function mutations and disseminated coccidioidomycosis and histo-
journal.ppat.1004062. plasmosis. J Allergy Clin Immunol 131:1624 –1634. https://doi.org/10
94. Li K, Yu JJ, Hung CY, Lehmann PF, Cole GT. 2001. Recombinant urease .1016/j.jaci.2013.01.052.
and urease DNA of Coccidioides immitis elicit an immunoprotective 112. Fierer J, Walls L, Wright F, Kirkland TN. 1999. Genes influencing resis-
response against coccidioidomycosis in mice. Infect Immun 69: tance to Coccidioides immitis and the interleukin-10 response map to
2878 –2887. https://doi.org/10.1128/IAI.69.5.2878-2887.2001. chromosomes 4 and 6 in mice. Infect Immun 67:2916 –2919.
95. Mirbod-Donovan F, Schaller R, Hung CY, Xue J, Reichard U, Cole GT. 113. Nathan C, Shiloh MU. 2000. Reactive oxygen and nitrogen intermedi-
2006. Urease produced by Coccidioides posadasii contributes to the ates in the relationship between mammalian hosts and microbial
virulence of this respiratory pathogen. Infect Immun 74:504 –515. pathogens. Proc Natl Acad Sci U S A 97:8841– 8848. https://doi.org/10
https://doi.org/10.1128/IAI.74.1.504-515.2006. .1073/pnas.97.16.8841.
96. Wise HZ, Hung CY, Whiston E, Taylor JW, Cole GT. 2013. Extracellular 114. Bogdan C. 2001. Nitric oxide and the immune response. Nat Immunol
ammonia at sites of pulmonary infection with Coccidioides posadasii 2:907–916. https://doi.org/10.1038/ni1001-907.
contributes to severity of the respiratory disease. Microb Pathog 59- 115. Margolis DA, Viriyakosol S, Fierer J, Kirkland TN. 2011. The role of
60:19 –28. https://doi.org/10.1016/j.micpath.2013.04.003. reactive oxygen intermediates in experimental coccidioidomycois in
97. Schenten D, Medzhitov R. 2011. The control of adaptive immune mice. BMC Microbiol 11:71. https://doi.org/10.1186/1471-2180-11-71.
responses by the innate immune system. Adv Immunol 109:87–124. 116. Gonzalez A, Hung CY, Cole GT. 2011. Coccidioides releases a soluble factor
https://doi.org/10.1016/B978-0-12-387664-5.00003-0. that suppresses nitric oxide production by murine primary macrophages.
98. Plato A, Hardison SE, Brown GD. 2015. Pattern recognition receptors in Microb Pathog 50:100–108. https://doi.org/10.1016/j.micpath.2010.11.006.
antifungal immunity. Semin Immunopathol 37:97–106. https://doi.org/ 117. Gonzalez A, Hung CY, Cole GT. 2011. Nitric oxide synthase activity has
10.1007/s00281-014-0462-4. limited influence on the control of Coccidioides infection in mice.
99. Hung C-Y, Jiménez-Alzate MDP, Gonzalez A, Wüthrich M, Klein BS, Cole Microb Pathog 51:161–168. https://doi.org/10.1016/j.micpath.2011.03
GT. 2014. Interleukin-1 receptor but not Toll-like receptor 2 is essential .013.
January 2020 Volume 33 Issue 1 e00112-19 cmr.asm.org 19
Donovan et al. Clinical Microbiology Reviews
118. Lewis ER, David VR, Doyle AL, Rajabi K, Kiefer JA, Pirrotte P, Barker BM. 140. Vivier E, Artis D, Colonna M, Diefenbach A, Di Santo JP, Eberl G, Koyasu
2015. Differences in host innate responses among Coccidioides isolates S, Locksley RM, McKenzie ANJ, Mebius RE, Powrie F, Spits H. 2018.
in a murine model of pulmonary coccidioidomycosis. Eukaryot Cell Innate lymphoid cells: 10 years on. Cell 174:1054 –1066. https://doi.org/
14:1043–1053. https://doi.org/10.1128/EC.00122-15. 10.1016/j.cell.2018.07.017.
119. Van Dyken SJ, Liang HE, Naikawadi RP, Woodruff PG, Wolters PJ, Erle DJ, 141. Mindt BC, Fritz JH, Duerr CU. 2018. Group 2 innate lymphoid cells in
Locksley RM. 2017. Spontaneous chitin accumulation in airways and pulmonary immunity and tissue homeostasis. Front Immunol 9:840.
age-related fibrotic lung disease. Cell 169:497–509.e13. https://doi.org/ https://doi.org/10.3389/fimmu.2018.00840.
10.1016/j.cell.2017.03.044. 142. Galgiani JN, Yam P, Petz LD, Williams PL, Stevens DA. 1980. Comple-
120. Slagle DC, Cox RA, Kuruganti U. 1989. Induction of tumor necrosis ment activation by Coccidioides immitis: in vitro and clinical studies.
factor alpha by spherules of Coccidioides immitis. Infect Immun 57: Infect Immun 28:944 –949.
1916 –1921. 143. De Lucca AJ, Walsh TJ. 1999. Antifungal peptides: novel therapeutic
121. Magee DM, Cox RA. 1995. Roles of gamma interferon and interleukin-4 compounds against emerging pathogens. Antimicrob Agents Che-
in genetically determined resistance to Coccidioides immitis. Infect mother 43:1–11. https://doi.org/10.1128/AAC.43.1.1.
Immun 63:3514 –3519. 144. Ordonez SR, Veldhuizen EJA, van Eijk M, Haagsman HP. 2017. Role of
122. Ampel NM, Nesbit LA, Nguyen CT, Chavez S, Knox KS, Johnson SM, soluble innate effector molecules in pulmonary defense against fungal
Pappagianis D. 2015. Cytokine profiles from antigen-stimulated whole- pathogens. Front Microbiol 8:2098. https://doi.org/10.3389/fmicb.2017
blood samples among patients with pulmonary or nonmeningeal dis- .02098.
seminated coccidioidomycosis. Clin Vaccine Immunol 22:917–922. 145. Nayak A, Dodagatta-Marri E, Tsolaki AG, Kishore U. 2012. An insight into
https://doi.org/10.1128/CVI.00280-15. the diverse roles of surfactant proteins, SP-A and SP-D in innate and
123. Muñoz-Hernández B, Palma-Cortés G, Manjarrez ME. 2012. Innovation of adaptive immunity. Front Immunol 3:131. https://doi.org/10.3389/
the parasitic cycle of Coccidioides spp.,p 29–52. In Shah MM (ed), Parasi- fimmu.2012.00131.
tology. IntechOpen, London, United Kingdom. http://www.intechopen 146. Ampel NM, Dionne SO, Giblin A, Podany AB, Galgiani J. 2009. Mannose-
.com/books/parasitology/innovation-of-the-parasitic-cycle-of-coccidioides binding lectin serum levels are low in persons with clinically active
-spp-. coccidioidomycosis. Mycopathologia 167:173–180. https://doi.org/10
124. Galgiani JN, Isenberg RA, Stevens DA. 1978. Chemotaxigenic activity of .1007/s11046-008-9172-6.
extracts from the mycelial and spherule phases of Coccidioides immitis 147. Segal GP, Lehrer RI, Selsted ME. 1985. In vitro effect of phagocyte
for human polymorphonuclear leukocytes. Infect Immun 21:862– 865. cationic peptides on Coccidioides immitis. J Infect Dis 151:890 – 894.
125. Galgiani JN. 1995. Differences in oxidant release by human polymor- https://doi.org/10.1093/infdis/151.5.890.
phonuclear leukocytes produced by stimulation with different phases 148. Collins MS, Pappagianis D. 1974. Inhibition by lysozyme of growth of
of Coccidioides immitis. J Infect Dis 172:199 –203. https://doi.org/10 the spherule phase of Coccidioides immitis in vitro. Infect Immun
.1093/infdis/172.1.199. 10:616 – 623.
126. Rubin-Bejerano I, Abeijon C, Magnelli P, Grisafi P, Fink GR. 2007. Phago-
149. Cox RA, Baker BS, Stevens DA. 1982. Specificity of immunoglobulin E in
cytosis by human neutrophils is stimulated by a unique fungal cell wall
coccidioidomycosis and correlation with disease involvement. Infect
component. Cell Host Microbe 2:55– 67. https://doi.org/10.1016/j.chom
Downloaded from https://journals.asm.org/journal/cmr on 04 February 2023 by 2806:290:a80b:cc8:c419:e160:befc:f9a8.
Immun 37:609 – 616.
.2007.06.002.
150. Smith CE, Whiting EG, Baker EE, Rosenberger HG, Beard RR, Saito MT.
127. Ampel NM, Bejarano GC, Galgiani JN. 1992. Killing of Coccidioides
1948. The use of coccidioidin. Am Rev Tuberc 57:330 –360.
immitis by human peripheral blood mononuclear cells. Infect Immun
151. Drutz DJ, Catanzaro A. 1978. Coccidioidomycosis. Part I. Am Rev Respir
60:4200 – 4204.
Dis 117:559 –585.
128. Beaman L, Benjamini E, Pappagianis D. 1981. Role of lymphocytes in
152. Wack EE, Ampel NM, Sunenshine RH, Galgiani JN. 2015. The return of
macrophage-induced killing of Coccidioides immitis in vitro. Infect Im-
delayed-type hypersensitivity skin testing for coccidioidomycosis. Clin
mun 34:347–353.
Infect Dis 61:787–791. https://doi.org/10.1093/cid/civ388.
129. Roy RM, Klein BS. 2012. Dendritic cells in antifungal immunity and
153. Zweiman BD, Pappagianis D, Maibach H, Hildreth E. 1969. Coccidioidin
vaccine design. Cell Host Microbe 11:436 – 446. https://doi.org/10.1016/
delayed hypersensitivity: skin test and in vitro lymphocyte reactivities.
j.chom.2012.04.005.
130. Dionne SO, Podany AB, Ruiz YW, Ampel NM, Galgiani JN, Lake DF. 2006. J Immunol 102:1284 –1289.
Spherules derived from Coccidioides posadasii promote human den- 154. Stevens DA. 1995. Current concepts: coccidioidomycosis. N Engl J Med
dritic cell maturation and activation. Infect Immun 74:2415–2422. 332:1077–1082. https://doi.org/10.1056/NEJM199504203321607.
https://doi.org/10.1128/IAI.74.4.2415-2422.2006. 155. Catanzaro A, Spitler LE, Moser KM. 1975. Cellular immune response in
131. Awasthi S. 2007. Dendritic cell-based vaccine against coccidioides in- coccidioidomycosis. Cell Immunol 15:360 –371. https://doi.org/10.1016/
fection. Ann N Y Acad Sci 1111:269 –274. https://doi.org/10.1196/annals 0008-8749(75)90014-3.
.1406.013. 156. Vinh DC, Schwartz B, Hsu AP, Miranda DJ, Valdez PA, Fink D, Lau KP,
132. Ampel NM. 2007. The complex immunology of human coccidioidomy- Long-Priel D, Kuhns DB, Uzel G, Pittaluga S, Hoover S, Galgiani JN,
cosis. Ann N Y Acad Sci 1111:245–258. https://doi.org/10.1196/annals Holland SM. 2011. Interleukin-12 receptor beta1 deficiency predispos-
.1406.032. ing to disseminated coccidioidomycosis. Clin Infect Dis 52:e99 – e102.
133. Echols RM, Palmer DL, Long GW. 1982. Tissue eosinophilia in human https://doi.org/10.1093/cid/ciq215.
coccidioidomycosis. Rev Infect Dis 4:656 – 664. https://doi.org/10.1093/ 157. Beaman L, Pappagianis D, Benjamini E. 1977. Significance of T cells in
clinids/4.3.656. resistance to experimental murine coccidioidomycosis. Infect Immun
134. Simons CM, Stratton CW, Kim AS. 2011. Peripheral blood eosinophilia as 17:580 –585.
a clue to the diagnosis of an occult Coccidioides infection. Hum Pathol 158. Beaman L, Pappagianis D, Benjamini E. 1979. Mechanisms of resistance
42:449 – 453. https://doi.org/10.1016/j.humpath.2010.09.005. to infection with Coccidioides immitis in mice. Infect Immun 23:
135. Schmidt S, Zimmermann SY, Tramsen L, Koehl U, Lehrnbecher T. 2013. 681– 685.
Natural killer cells and antifungal host response. Clin Vaccine Immunol 159. Casadevall A. 1995. Antibody immunity and invasive fungal infections.
20:452– 458. https://doi.org/10.1128/CVI.00606-12. Infect Immun 63:4211– 4218.
136. Schmidt S, Tramsen L, Lehrnbecher T. 2017. Natural killer cells in 160. Kong Y-C, Savage DC, Levine HB. 1966. Enhancement of immune
antifungal immunity. Front Immunol 8:1623. https://doi.org/10.3389/ responses in mice by a booster injection of Coccidioides spherules. J
fimmu.2017.01623. Immunol 95:1048 –1056.
137. Petkus AF, Baum LL. 1987. Natural killer cell inhibition of young spher- 161. Ibrahim AB, Pappagianis D. 1973. Experimental induction of anergy to
ules and endospores of Coccidioides immitis. J Immunol 139:3107–3111. coccidioidin by antigens of Coccidioides immites. Infect Immun 7:786–794.
138. Magee DM, Cox RA. 1996. Interleukin-12 regulation of host defenses 162. Magee DM, Friedberg RL, Woitaske MD, Johnston SA, Cox RA. 2005.
against Coccidioides immitis. Infect Immun 64:3609 –3613. Role of B cells in vaccine-induced immunity against coccidioidomyco-
139. Spits H, Artis D, Colonna M, Diefenbach A, Di Santo JP, Eberl G, Koyasu sis. Infect Immun 73:7011–7013. https://doi.org/10.1128/IAI.73.10.7011
S, Locksley RM, McKenzie AN, Mebius RE, Powrie F, Vivier E. 2013. Innate -7013.2005.
lymphoid cells—a proposal for uniform nomenclature. Nat Rev Immu- 163. Hung CY, Gonzalez A, Wuthrich M, Klein BS, Cole GT. 2011. Vaccine
nol 13:145–149. https://doi.org/10.1038/nri3365. immunity to coccidioidomycosis occurs by early activation of three
January 2020 Volume 33 Issue 1 e00112-19 cmr.asm.org 20
Early Events in Coccidioidomycosis Clinical Microbiology Reviews
signal pathways of T helper cell response (Th1, Th2, and Th17). Infect 179. Ginn RMR, Bollmann K, Goodsell J, Mendez G, Bradley B, Galgiani JN.
Immun 79:4511– 4522. https://doi.org/10.1128/IAI.05726-11. 2019. Delays in the diagnosis of coccidioidomycosis and their relation-
164. Yoshinoya S, Cox RA, Pope RM. 1980. Circulating immune complexes in ship to healthcare utilization. Emerg Infect Dis. https://doi.org/10.3201/
coccidioidomycosis. Detection and characterization. J Clin Invest 66: eid2509.190019.
655– 663. https://doi.org/10.1172/JCI109901. 180. Pu J, Donovan F, Galgiani JN. 2019. Informatic profile of primary care
165. Cox RA, Pope RM. 1987. Serum-mediated suppression of lymphocyte practioners’ testing and managing patients with coccidioidomycosis
transformation responses in coccidioidomycosis. Infect Immun 55: (cm), p 33. In Proceedings of the 63rd Annual Cocci Study Group
1058 –1062. meeting, April 5– 6, Sacramento, California.
166. Brown J, Benedict K, Park BJ, Thompson GR, III. 2013. Coccidioidomycosis: 181. Mitchell M, Dizon D, Libke R, Peterson M, Slater D, Dhillon A. 2015.
epidemiology. Clin Epidemiol 5:185–197. Development of a real-time PCR assay for identification of Coccidioides
167. Stockamp NW, Thompson GR, III. 2016. Coccidioidomycosis. Infect Dis immitis by use of the BD Max system. J Clin Microbiol 53:926 –929.
Clin North Am 30:229 –246. https://doi.org/10.1016/j.idc.2015.10.008. https://doi.org/10.1128/JCM.02731-14.
168. Willett FM, Weiss A. 1945. Coccidioidomycosis in southern California: 182. Saubolle MA, Wojack BR, Wertheimer AM, Fuayagem AZ, Young S,
report of a new endemic area with a review of 100 cases. Ann Intern Koeneman BA. 2018. Multicenter clinical validation of a cartridge-based
Med 23:349 –375. real-time PCR system for detection of Coccidioides spp. in lower respi-
169. Wieden MA, Lundergan LL, Blum J, Delgado KL, Coolbaugh R, Howard ratory specimens. J Clin Microbiol 56:e01277-17. https://doi.org/10
R, Peng T, Pugh E, Reis N, Theis J, Galgiani JN. 1996. Detection of .1128/JCM.01277-17.
coccidioidal antibodies by 33-kDa spherule antigen, Coccidioides EIA, 183. Thompson GR, III, Sharma S, Bays DJ, Pruitt R, Engelthaler DM, Bowers
and standard serologic tests in sera from patients evaluated for coc- J, Driebe EM, Davis M, Libke R, Cohen SH, Pappagianis D. 2013.
cidioidomycosis. J Infect Dis 173:1273–1277. https://doi.org/10.1093/ Coccidioidomycosis: adenosine deaminase levels, serologic parame-
infdis/173.5.1273. ters, culture results, and polymerase chain reaction testing in pleural
170. Blair JE, Chang YH, Cheng MR, Vaszar LT, Vikram HR, Orenstein R, Kusne
fluid. Chest 143:776 –781. https://doi.org/10.1378/chest.12-1312.
S, Ho S, Seville MT, Parish JM. 2014. Characteristics of patients with mild
184. Galgiani JN, Ampel NM, Blair JE, Catanzaro A, Geertsma F, Hoover SE,
to moderate primary pulmonary coccidioidomycosis. Emerg Infect Dis
Johnson RH, Kusne S, Lisse J, MacDonald JD, Meyerson SL, Raksin PB,
20:983–990. https://doi.org/10.3201/eid2006.131842.
Siever J, Stevens DA, Sunenshine R, Theodore N. 2016. 2016 Infectious
171. Pappagianis D. 2001. Serologic studies in coccidioidomycosis. Semin
Diseases Society of America (IDSA) clinical practice guideline for the
Respir Infect 16:242–250. https://doi.org/10.1053/srin.2001.29315.
treatment of coccidioidomycosis. Clin Infect Dis 63:e112-46. https://doi
172. Blair JE, Coakley B, Santelli AC, Hentz JG, Wengenack NL. 2006. Sero-
.org/10.1093/cid/ciw360.
logic testing for symptomatic coccidioidomycosis in immunocompe-
185. Donovan FM, Zangeneh TT, Malo J, Galgiani JN. 2017. Top questions in
tent and immunosuppressed hosts. Mycopathologia 162:317–324.
the diagnosis and treatment of coccidioidomycosis. Open Forum Infect
https://doi.org/10.1007/s11046-006-0062-5.
173. Mafi NG, Blair J. 2019. A retrospective evaluation of coccidioidomycosis Dis 4:ofx197. https://doi.org/10.1093/ofid/ofx197.
skin testing in patients with pulmonary coccidioidomycosi in an en- 186. Thompson GR, III, Barker BM, Wiederhold NP. 2017. Large-scale evalu-
demic region, poster 14. In Proceedings of the 63rd Annual Coccidioid- ation of in vitro amphotericin B, triazole, and echinocandin activity
Downloaded from https://journals.asm.org/journal/cmr on 04 February 2023 by 2806:290:a80b:cc8:c419:e160:befc:f9a8.
omycosis Study Group Meeting. against Coccidioides species from U.S. institutions. Antimicrob Agents
174. Johnson R, Kernerman SM, Sawtelle BG, Rastogi SC, Nielsen HS, Ampel Chemother 61:e02634-16. https://doi.org/10.1128/AAC.02634-16.
NM. 2012. A reformulated spherule-derived coccidioidin (Spherusol) to 187. Ostrosky-Zeichner L, Casadevall A, Galgiani JN, Odds FC, Rex JH. 2010.
detect delayed-type hypersensitivity in coccidioidomycosis. Myco- An insight into the antifungal pipeline: selected new molecules and
pathologia 174:353–358. https://doi.org/10.1007/s11046-012-9555-6. beyond. Nat Rev Drug Discov 9:719 –727. https://doi.org/10.1038/
175. Wheeler C, Lucas KD, Derado G, McCotter O, Tharratt RS, Chiller T, nrd3074.
Mohle-Boetani JC. 2018. Risk stratification with coccidioidal skin test to 188. Viriyakosol S, Kapoor M, Okamoto S, Covel J, Soltow QA, Trzoss M, Shaw KJ,
prevent valley fever among inmates, California, 2015. J Correct Health Fierer J. 2019. APX001 and other Gwt1 inhibitor prodrugs are effective in
Care 24:342–351. https://doi.org/10.1177/1078345818792679. experimental Coccidioides immitis pneumonia. Antimicrob Agents Che-
176. Pappagianis D, Zimmer BL. 1990. Serology of coccidioidomycosis. Clin mother 63:e01715-18. https://doi.org/10.1128/AAC.01715-18.
Microbiol Rev 3:247–268. https://doi.org/10.1128/cmr.3.3.247. 189. Wiederhold NP, Najvar LK, Jaramillo R, Olivo M, Birch M, Law D, Rex JH,
177. Maddox SE. 2017. Rapid detection of anti-Coccidioides antibodies us- Catano G, Patterson TF. 2018. The orotomide olorofim is efficacious in
ing the sonaTM Coccidioides Ab lateral flow assay, p 36. In Proceedings an experimental model of central nervous system coccidioidomycosis.
of the Sixty-First Annual Meeting of the Coccidioidomycosis Study Antimicrob Agents Chemother 62:e00999-18. https://doi.org/10.1128/
Group. Coccidioidomycosis Study Group, Stanford, CA. AAC.00999-18.
178. Donovan FM, Wightman P, Zong Y, Gabe L, Majeed A, Ynosencio T, 190. Shubitz LF, Roy ME, Trinh HT, Hoekstra WJ, Schotzinger RJ, Garvey EP.
Bedrick EJ, Galgiani JN. 2019. Delays in coccidioidomycosis diagnosis 2017. Efficacy of the investigational antifungal VT-1161 in treating
and associated healthcare utilization in Tucson, Arizona. Emerg Infect naturally occurring coccidioidomycosis in dogs. Antimicrob Agents
Dis 25:1745. https://doi.org/10.3201/eid2508.190023. Chemother 61:e00111-17. https://doi.org/10.1128/AAC.00111-17.
Fariba M. Donovan, M.D., Ph.D., as both a Lisa Shubitz, D.V.M., is a research scientist at
practicing physician and a research scientist, the Valley Fever Center for Excellence. Her
has long cultivated a particular interest in research focus includes developing a vaccine
medical mycology. Her research focuses on for valley fever and studying the epidemiol-
the identification of virulence factors and the ogy of the disease in canines, the ecological
interaction of several fungi with the human distribution of the fungus in southern Arizona,
host. She has conducted studies in Coccid- and interactions between the host (both ani-
ioides with the goal of helping in the earlier mal and human) and the fungus that causes
diagnosis of valley fever to improve patient valley fever, using animal models.
outcomes, lower costs, and heighten antibi-
otic stewardship. Additionally, she is devel-
oping strategies to study the host innate immune response to Coccid-
Continued next page
ioides with a focus on the early events in coccidioidomycosis.
January 2020 Volume 33 Issue 1 e00112-19 cmr.asm.org 21
Donovan et al. Clinical Microbiology Reviews
Daniel Powell, Ph.D., received his Ph.D. from Jeffrey Frelinger, Ph.D., and the members
the University of Baltimore, Baltimore, MD, in of his laboratory have been interested for
2011 working on immune responses to lipo- some years in immune responses to the lung
polysaccharide mutants. Since then, he has pathogens influenza virus and Francisella tu-
conducted research at the University of Ari- larensis. They have begun collaborations on
zona. He is a cellular immunologist with inter- the role of T cell responses in Coccidioides
ests in vaccine development, as well as early infections and the development of an effective
host responses in lung infections. vaccine.
Marc Orbach, Ph.D., is a professor of plant John N. Galgiani, M.D., has been working
pathology in the College of Agriculture and with valley fever (coccidioidomycosis) for the
Life Sciences. His focus is based on studying last four decades. As director of the Valley
the ecological niche of the fungus that Fever Center for Excellence, his passion is
causes valley fever and the analysis of global research in the treatment of valley fever. This
gene expression in Coccidioides posadasii involves studies to improve the detection of
during both saprobic and parasitic growth. the fungus in the environment, to increase
In his analysis, he has been working with the the sensitivity of diagnostic tests for pa-
Serial Analysis of Gene Expression (SAGE). tients, and to develop a vaccine to prevent
His research interests also include the mo- the disease in both humans and animals.
lecular genetics of fungal pathogenicity in
animals and plants.
Downloaded from https://journals.asm.org/journal/cmr on 04 February 2023 by 2806:290:a80b:cc8:c419:e160:befc:f9a8.
January 2020 Volume 33 Issue 1 e00112-19 cmr.asm.org 22
You might also like
- Clinical Microbiology Reviews 2017 Jeffery Smith E00029 17.fullDocument18 pagesClinical Microbiology Reviews 2017 Jeffery Smith E00029 17.fullKatherine FlemingNo ratings yet
- Ansari 2020Document13 pagesAnsari 2020Prasanna BakshiNo ratings yet
- Host-Pathogen Interactions in Gram-Positive Bacterial PneumoniaDocument22 pagesHost-Pathogen Interactions in Gram-Positive Bacterial PneumoniapaulinasilvatoledoNo ratings yet
- Chemosphere: Sindy Sanjuan-Reyes, Leobardo Manuel G Omez-Olivan, Hariz Islas-FloresDocument11 pagesChemosphere: Sindy Sanjuan-Reyes, Leobardo Manuel G Omez-Olivan, Hariz Islas-FloresabeldiceNo ratings yet
- Artigo 1 Toxoplasma GondiiDocument18 pagesArtigo 1 Toxoplasma GondiiDan AlmeidaNo ratings yet
- What We Have Learnt From The SARS Epdemics in Mainland ChinaDocument5 pagesWhat We Have Learnt From The SARS Epdemics in Mainland ChinaLorena Galindo GuerreroNo ratings yet
- Corona Virus DiseaseDocument34 pagesCorona Virus DiseaseJoseph CruzNo ratings yet
- Clinical Microbiology Reviews-2018-Franco-Paredes-e00069-18.fullDocument25 pagesClinical Microbiology Reviews-2018-Franco-Paredes-e00069-18.fullluck2livNo ratings yet
- Cordyceps For HealthDocument11 pagesCordyceps For HealthFerry WijayaNo ratings yet
- Covid-19 Pandemic: a Comprehensive UnderstandingFrom EverandCovid-19 Pandemic: a Comprehensive UnderstandingNo ratings yet
- Cutanoeus BacteriumDocument25 pagesCutanoeus BacteriumDwi Puja SetiawanNo ratings yet
- Clinical, Molecular, and Epidemiological Characterization of TheDocument31 pagesClinical, Molecular, and Epidemiological Characterization of TheQueijer SalasNo ratings yet
- PandemicH1N1 2009virusEvolutiionaryRetrospective 11Document9 pagesPandemicH1N1 2009virusEvolutiionaryRetrospective 11Homer967No ratings yet
- 1 s2.0 S0045653521000710 MainextDocument22 pages1 s2.0 S0045653521000710 MainextAbdul ZahirNo ratings yet
- Caracterizacion Clinica, Molecular y Epidemiologica COVID19Document47 pagesCaracterizacion Clinica, Molecular y Epidemiologica COVID19Joe2805No ratings yet
- Bacterial Associations With LegumesDocument27 pagesBacterial Associations With LegumesJorge CorderoNo ratings yet
- Real Ebo PeterDocument36 pagesReal Ebo PeterOlabintan OlabodeNo ratings yet
- 10 1128@CMR 00036-20Document19 pages10 1128@CMR 00036-20Luis AlbertoNo ratings yet
- Advances in Parasitology PDFDocument321 pagesAdvances in Parasitology PDFalmiraerickaiNo ratings yet
- Muriuki - The Role of Brucellosis As A Cause of Human Illness in The Pastoral Narok, District, KenyaDocument129 pagesMuriuki - The Role of Brucellosis As A Cause of Human Illness in The Pastoral Narok, District, KenyadestaNo ratings yet
- Advances in Parasit OlogyDocument321 pagesAdvances in Parasit Ologyintanhardianti7No ratings yet
- Pharmacological Basis For The Potential Role of Azithromycin and Doxycycline in Management of COVID-19 Production and Hosting by ElsevierDocument11 pagesPharmacological Basis For The Potential Role of Azithromycin and Doxycycline in Management of COVID-19 Production and Hosting by Elsevierاحمد علىNo ratings yet
- HS1557Document518 pagesHS1557Abhishek Singh0% (1)
- African Swine Fever Virus: W.R.HessDocument2 pagesAfrican Swine Fever Virus: W.R.HessArtemio Jr A LonzagaNo ratings yet
- Journal of Infection and Public HealthDocument5 pagesJournal of Infection and Public HealthIndiraNo ratings yet
- Inventarisasi Hama Dan Penyakit Pada Berbagai Varietas Tanaman Kentang Di Ketinggian 700 MDPL Dengan Dan Tanpa NaunganDocument119 pagesInventarisasi Hama Dan Penyakit Pada Berbagai Varietas Tanaman Kentang Di Ketinggian 700 MDPL Dengan Dan Tanpa NaunganDwita saputriNo ratings yet
- FUNGICASDocument46 pagesFUNGICASMARCELO DONIZETTI CHAVESNo ratings yet
- Aetiology of Canine Infectious Respiratory Disease Complex and Prevalence of Its Pathogens in EuropeDocument23 pagesAetiology of Canine Infectious Respiratory Disease Complex and Prevalence of Its Pathogens in EuropeNadia AbarcaNo ratings yet
- Microbiology and Molecular Biology Reviews 2020 Kaldalu E00070 20.fullDocument24 pagesMicrobiology and Molecular Biology Reviews 2020 Kaldalu E00070 20.fullNiilo KaldaluNo ratings yet
- Project ResearchDocument35 pagesProject ResearchEnoch BoafoNo ratings yet
- The Botanical Review (Inglês)Document98 pagesThe Botanical Review (Inglês)arlinda rodriguesNo ratings yet
- Doern Et Al 2019 Practical Guidance For Clinical Microbiology Laboratories A Comprehensive Update On The Problem ofDocument21 pagesDoern Et Al 2019 Practical Guidance For Clinical Microbiology Laboratories A Comprehensive Update On The Problem ofrehanaNo ratings yet
- Environmental Exposure To MicroplasticsDocument9 pagesEnvironmental Exposure To MicroplasticsZainie Aboo BakkarNo ratings yet
- 1 s2.0 S0160412013002870 MainDocument16 pages1 s2.0 S0160412013002870 MainRilly Yane PutryNo ratings yet
- Lab DX of UurtDocument45 pagesLab DX of UurtKrishna Rathod100% (1)
- Distribucion de LoxocelesDocument10 pagesDistribucion de LoxocelesDaniel Cristóbal Sepúlveda CaroNo ratings yet
- BaylucideDocument208 pagesBaylucidelaboratorioentomologiacevaoNo ratings yet
- Livro AjudaDocument22 pagesLivro AjudaAndressa OliveiraNo ratings yet
- Clinical Microbiology Reviews-2018-Hamilton-e00085-17.full PDFDocument19 pagesClinical Microbiology Reviews-2018-Hamilton-e00085-17.full PDFDillaNo ratings yet
- Revised File 2Document46 pagesRevised File 2April Mae ManipolNo ratings yet
- Brucellosis - A Re-Emerging ZoonosisDocument7 pagesBrucellosis - A Re-Emerging ZoonosisAndika Budi KurniantoNo ratings yet
- The Emergence of Arthropod-Borne Viral DiseaseDocument9 pagesThe Emergence of Arthropod-Borne Viral DiseasedianamfgNo ratings yet
- Consequences of Chemical Impact of Disinfectants Safe Preventive Measures Against COVID 19Document9 pagesConsequences of Chemical Impact of Disinfectants Safe Preventive Measures Against COVID 19michellelyt1993No ratings yet
- KGDocument505 pagesKGJade BreukinkNo ratings yet
- Clinical Microbiology Reviews 2018 Hamilton E00085 17.fullDocument19 pagesClinical Microbiology Reviews 2018 Hamilton E00085 17.fullMero ElbazeNo ratings yet
- Current Affairs Strategist Program: Target Prelims 2020: Booklet-28 Science and Technology Booklet-10 Corona UpdatesDocument24 pagesCurrent Affairs Strategist Program: Target Prelims 2020: Booklet-28 Science and Technology Booklet-10 Corona UpdatesRohit KumarNo ratings yet
- Measuring The Impact of COVID 19 Vaccines To The Grade 11 Students in Universidad de Manila1Document40 pagesMeasuring The Impact of COVID 19 Vaccines To The Grade 11 Students in Universidad de Manila1MoyeonNo ratings yet
- Corrected Version of TBDocument34 pagesCorrected Version of TBBarnabas KipngetichNo ratings yet
- Forensic Mycology ReviewDocument11 pagesForensic Mycology ReviewDaniel MontealegreNo ratings yet
- Makalah Corona B. InggrisDocument14 pagesMakalah Corona B. InggrisyasagobrasnetNo ratings yet
- Group 5 BSN 4 2 Case Study Dengue FinalDocument63 pagesGroup 5 BSN 4 2 Case Study Dengue FinalCindy vicenteNo ratings yet
- Lumber Mold - WPPA - Mold-Housing-Wood-Tg2Document12 pagesLumber Mold - WPPA - Mold-Housing-Wood-Tg2Jeff HNo ratings yet
- The Securitization of The Coronavirus CRDocument85 pagesThe Securitization of The Coronavirus CRgygyNo ratings yet
- Peng Et Al. 2019. Pasteurella Multocida Genotypes and GenomicsDocument37 pagesPeng Et Al. 2019. Pasteurella Multocida Genotypes and GenomicsFREDY GUTIERREZNo ratings yet
- Fake Test Lacc2 1st TermDocument4 pagesFake Test Lacc2 1st TermByron PacaizaNo ratings yet
- Research Proposal FinalDocument35 pagesResearch Proposal FinalBienne Zyrus Earl CarpioNo ratings yet
- Main PDFDocument9 pagesMain PDFMelissaNo ratings yet
- COT LESSON PLAN IN SCIENCE V OfficialDocument4 pagesCOT LESSON PLAN IN SCIENCE V OfficialLovely CalagdayNo ratings yet
- Study of Cancer Investigatory ProjectDocument15 pagesStudy of Cancer Investigatory ProjectRavi KNo ratings yet
- Etextbook PDF For Invertebrates 3rd Edition by Richard C BruscaDocument61 pagesEtextbook PDF For Invertebrates 3rd Edition by Richard C Bruscabeverly.bustos487100% (43)
- Advanced Technology. Simplified.: How It WorksDocument2 pagesAdvanced Technology. Simplified.: How It Worksleopardus pardalisNo ratings yet
- Exchange With The Environment Ch4.1 7th PDF (Information Obtained From Holt Science and Technology: Life Science. Austin: Holt Rinehart & Winston, 2007. Print.)Document18 pagesExchange With The Environment Ch4.1 7th PDF (Information Obtained From Holt Science and Technology: Life Science. Austin: Holt Rinehart & Winston, 2007. Print.)thegedusNo ratings yet
- How Genes Influence Behaviour 2nd Edition 2020 OxfDocument2 pagesHow Genes Influence Behaviour 2nd Edition 2020 OxfPatrícia VieiraNo ratings yet
- Antibacterial Protection of Polyphenols From Curry Leaves (Murraya Koenigii) A Research StudyDocument3 pagesAntibacterial Protection of Polyphenols From Curry Leaves (Murraya Koenigii) A Research StudyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Lymphoid NeoplasmsDocument52 pagesLymphoid NeoplasmsAmalia Riska GNo ratings yet
- Dopamine D3 Receptor - A Neglected Participant in Parkinson Disease Pathogenesis and Treatment?Document45 pagesDopamine D3 Receptor - A Neglected Participant in Parkinson Disease Pathogenesis and Treatment?Daniel TorresNo ratings yet
- Abstract: Rice Field Ecosystem Provides A Favourable Environment I.E. Light, WaterDocument10 pagesAbstract: Rice Field Ecosystem Provides A Favourable Environment I.E. Light, Watersangita sharmaNo ratings yet
- TIGP Admissions Announcement For 2013Document6 pagesTIGP Admissions Announcement For 2013WinataWahyuFajarNo ratings yet
- Bryophytes and PteridophytesDocument3 pagesBryophytes and PteridophytesStarnley TemboNo ratings yet
- Intermittent Fasting & Calorie RestrictionDocument19 pagesIntermittent Fasting & Calorie Restrictiontemp222100% (2)
- Multiple Choice Questions On MycorrhizaDocument10 pagesMultiple Choice Questions On Mycorrhizaamandajwarner58No ratings yet
- University of Gondar College of Medicine and Health Sciences Department of Medical PhysiologyDocument202 pagesUniversity of Gondar College of Medicine and Health Sciences Department of Medical PhysiologyGifti DemisseNo ratings yet
- Literature Review Hepatitis B VirusDocument4 pagesLiterature Review Hepatitis B Virusafmztwoalwbteq100% (1)
- Agarose Gels IMBB 2013Document31 pagesAgarose Gels IMBB 2013Andrés Suazo SánchezNo ratings yet
- Lab Report 1 - Aseptic TechniqueDocument20 pagesLab Report 1 - Aseptic TechniqueAlyaa AthiraNo ratings yet
- Mutation: - From The Latin Word "Mutare" MeansDocument38 pagesMutation: - From The Latin Word "Mutare" MeansJan Andrea BendijoNo ratings yet
- Massively Parallel Sequencing Solutions For Human Identity: Sample To InsightDocument12 pagesMassively Parallel Sequencing Solutions For Human Identity: Sample To InsightVicontNo ratings yet
- Cell Biology Lecture 1 & 2 Sem I 2011-2012 Introduction To Cell Biology, Cell As The Basic Unit of Life SPINDocument121 pagesCell Biology Lecture 1 & 2 Sem I 2011-2012 Introduction To Cell Biology, Cell As The Basic Unit of Life SPINPrimo Arc100% (1)
- Exercise 3 - TRANSFER AND COLONY SELECTION TECHNIQUESDocument13 pagesExercise 3 - TRANSFER AND COLONY SELECTION TECHNIQUESArslan AmeenNo ratings yet
- VirologyDocument129 pagesVirologyAmoako KingsleyNo ratings yet
- Convergent Evolution Limited Forms Most Beautiful Ebook3000 PDFDocument335 pagesConvergent Evolution Limited Forms Most Beautiful Ebook3000 PDFgavinf1100% (1)
- Stefan Lanka 20 Juillet 2020 ANG FR-1Document10 pagesStefan Lanka 20 Juillet 2020 ANG FR-1K Mehmet ŞensoyNo ratings yet
- Complete Blood Count: Result Test Reference RangeDocument1 pageComplete Blood Count: Result Test Reference RangeRajaNo ratings yet
- Patho A 1. 11 Infectious Diseases Tagayuna 2015Document10 pagesPatho A 1. 11 Infectious Diseases Tagayuna 2015Ala'a Emerald AguamNo ratings yet
- Bright Field MicroscopeDocument3 pagesBright Field MicroscopeAgyei Kwaku SamuelNo ratings yet
- Cell DifferentiationDocument26 pagesCell DifferentiationQusai Haimone100% (1)
- Molecular Genetics: Test Yourself 20.1 (Page 389) 1Document2 pagesMolecular Genetics: Test Yourself 20.1 (Page 389) 1leeNo ratings yet