Professional Documents
Culture Documents
Assessment and Diagnostic Exams
Uploaded by
Jan Mark Soto0 ratings0% found this document useful (0 votes)
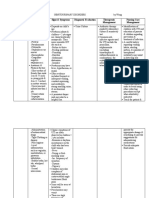
5 views10 pagesThis document provides information on nursing assessments and diagnostic exams for infectious, inflammatory, and immunologic diseases. It discusses subjective and objective data to collect during assessments, including symptoms, risk factors, and physical exam findings. It also summarizes several common non-invasive and invasive diagnostic tests and exams including urinalysis, chest x-rays, complete blood counts, strep titers, and biopsies. Nursing responsibilities are outlined for each test to ensure proper informed consent, preparation, monitoring, and follow up care for patients.
Original Description:
Original Title
ASSESSMENT AND DIAGNOSTIC EXAMS
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document provides information on nursing assessments and diagnostic exams for infectious, inflammatory, and immunologic diseases. It discusses subjective and objective data to collect during assessments, including symptoms, risk factors, and physical exam findings. It also summarizes several common non-invasive and invasive diagnostic tests and exams including urinalysis, chest x-rays, complete blood counts, strep titers, and biopsies. Nursing responsibilities are outlined for each test to ensure proper informed consent, preparation, monitoring, and follow up care for patients.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
5 views10 pagesAssessment and Diagnostic Exams
Uploaded by
Jan Mark SotoThis document provides information on nursing assessments and diagnostic exams for infectious, inflammatory, and immunologic diseases. It discusses subjective and objective data to collect during assessments, including symptoms, risk factors, and physical exam findings. It also summarizes several common non-invasive and invasive diagnostic tests and exams including urinalysis, chest x-rays, complete blood counts, strep titers, and biopsies. Nursing responsibilities are outlined for each test to ensure proper informed consent, preparation, monitoring, and follow up care for patients.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 10
ASSESSMENT AND DIAGNOSTIC may produce
EXAMS, AND DEPENDENT AND phlegm
INDEPENDENT NURSING CARE Shortness of
FOR INFECTIOUS, breath
INFLAMMATORY, AND Vulvar and
IMMUNOLOGIC DISEASES vaginal burning
and itching
Part 1: Nursing Assessment Pain on coitus
RISK FACTORS or on tampon
Gender insertion
Age Intense pain on
Race contact with
Past medical history clothing or
Family history/Genetics acidic urine
Current treatment Flu-like
Lifestyle/High risk behaviors symptoms
Travel history/Geography
Occupation OBJECTIVE DATA
Observe for pallor, cyanosis,
SUBJECTIVE DATA jaundice, and erythema
Infectious Immunologic Evaluate skin integrity
Headache, Increased thirst Check for rash and note is distribution
nausea, Frequent Observe hair texture and distribution
vomiting, urination Inspect nails
abdominal pain Extreme Inspect the oral mucous membranes
Nuchal rigidity, hunger Inspect the male and female genitalia
more severe Pink or cola- Palpate the peripheral pulses
headache, colored urine Palpate superficial lymph nodes
back, and Foamy urine Palpate for masses or lesions
lower Sneezing Percuss the anterior, lateral, and
extremity pain Itching of the posterior thorax
Spasms and nose, eyes, or Auscultate over the lungs
stiffness in jaw roof of the
muscles mouth Part 2: Non-Invasive Diagnostic
Stiffness of Itching or hives Examinations
your neck all over the
muscles body A. Urinalysis (UA) and Urine Culture
Difficulty Fatigue and Sensitivity (Urine CS)
swallowing Joint pain - A group of manual and/or automated
Excessive (usually worse qualitative and semi-quantitative tests
salivation in mornings performed on a urine sample.
Hydrophobia and after - A routine UA usually includes:
Hallucinations activity), Color
Loss of stiffness Transparency
appetite Headaches, Specific gravity
Nausea and confusion and pH
vomiting memory loss Protein
Weakness and Tender, warm, Glucose
fatigue and swollen Ketones Blood
Fever joints Bilirubin
Night sweats Nitrite
Chills Urobilinogen
Chest pain Leukocyte esterase
when you - To perform this, first urinate a small
breathe or amount into the toilet bowl to clear the
cough urethra of any contaminants.
Cough, which
- Then, collect a sample in a clean or No preparation is required
sterile container. About 1-2 oz is needed. Ensure the pt is not pregnant or
- Remove the container from the urine suspected to be
stream w/out stopping the flow. Assess the pt’s ability to hold his
- You may finish urinating into the bowl breath
- Take the sample to the lab Provide appropriate clothing
- For infants, the genital area is cleaned Instruct pt to cooperate during the
and dried, and then a collection device is procedure
attached.
- If you are asked to collect, be sure the Part 3: Invasive Diagnostic
collection device is attached securely to Examination
prevent leakage. A. Complete Blood Count (CBC)
- After baby has urinated, the urine (at - one of the most commonly ordered
least 20 cc) is place in a sterile container. blood tests which include the calculation
Nursing Considerations: of the cellular (formed elements) of blood
Instruct the patient to void directly - special machines analyze the different
into a clean, dry container. Sterile, components of blood in less than a minute
disposable containers are generally determine these calculations
recommended. Uses:
Cover all specimens tightly, label It may be a part of a routine check-up
properly and send immediately to the or screening, or as a follow-up test to
laboratory. monitor certain treatments
If a urine sample is obtained from an can be done as a part of an evaluation
indwelling catheter, it may be based on a pt’s symptoms
necessary to clamp the catheter for Screen for a wide range of conditions
about 15-30 minutes before obtaining and diseases
the sample. Help diagnose various conditionas,
Observe standard precautions when such as anemia, infection,
handling urine specimens. inflammation, bleeding disorder or
leukemia, etc.
B. Chest X-ray (Chest Radiography) monitor the condition and/or
- A painless, non-invasive test uses effectiveness of treatment after a
electromagnetic waves to produce visual diagnosis is established
images of the heart, lungs, bones, and Monitor treatment that is known to
blood vessels of the chest. affect blood cells, such as
Indications: chemotherapy or radiation therapy
Assist in the diagnosis of Nursing Responsibility:
diaphragmatic hernia, lung tumors, Explain procedure
and metastasis. Encourage to avoid stress if possible
Detect known or suspected because altered physiologic status
pulmonary, cardiovascular, and influences and changes normal
skeletal disorders. hematologic values
Identify the presence of chest trauma. Explain that fasting is not necessary
Confirm correct placement and Apply manual pressure and dressings
position of the endotracheal tube, over puncture site on removal of
tracheostomy tube, chest tubes, dinner
nasogastric feeding tube. Monitor the puncture site for oozing
Evaluate positive purified protein or hematoma formation
derivative (PDD) or Mantoux test for Instruct to resume normal activities
pulmonary tuberculosis. and diet
Monitor progressions, resolutions, or
maintenance of disease B. Anti-Streptolysin O titer (ASO titer)
Evaluate the patient’s response to a - looks for antibodies that the body makes
therapeutic regimen (antibiotic, while fighting group A Streptococcus
chemotherapy) bacteria
Nursing Considerations: - the antibodies work against a substance
Remove all metallic objects made by the bacteria called streptolysin O.
- group A stretococcus causes strep throat C. Biopsy
that may lead to rheumatic fever - to remove a piece of tissue or a sample
Purpose: of cells from the body so that it can be
To find out a current or recent strep analyzed in a laboratory
infection - imaging tests can’t differentiate
Antibodies from a strep infection cancerous cells for noncancerous cells
begin to increase about 1 week after Kinds:
infection Bone marrow biopsy
Get higher for several weeks before Endoscopic biopsy
decreasing Needle (thyroid)
As antibodies don’t increase righgt Procedures:
away, the better test to use to 1. Fine-needle aspiration
diagnose a strep infection is the rapid 2. Core needle biopsy
strep test. 3. Vacuum-assisted biopsy
Other tests maybe done 4. Image-guided biopsy
Throat culture for group A beta- Skin
hemolytic streptococci Shave
If a rheumatic fever may ensure, there Punch
is also a need for other antibody tests Incisional
(anti-DNase B, antihyaluronidase, Excisional
or anti-Streptozyme) Biopsy analysis and results:
Results of the test and its meaning Tissue sample sent to a laboratory for
The results may not mean the patient analysis
have a problem Sample may be chemically treated or
A negative result - no antobodies to frozen and sliced into very thin
the strep bacteria in the blood sections, stained to enhance contrast
A positive result - antibodies have and studied under a microscope
been found The grade is on a scale of 1 to 4
Reference Values Low-grade (grade 1) cancers are
<5 years: < or =70 IU/mL generally the least aggressive and
5-17 years: < or =640 IU/mL high-grade (grade 4) are the most.
> or =18 yrs: < or =530 IU/mL Nursing Responsibilities
Elevated values - infection by group Before the test
A streptococci Confirm pt’s identity
Risks Describe the procedure
Bleeding Needle biopsy - need to sit still during
Infection the procedure
Bruising W/ local anesthetic - no restriction of
Feeling lightheaded food, fluids, and medication
Slight sting or pain General anesthetic - fast from mn
Soreness before the procedure
Nursing Responsibilities Explain that pretest studies - blood,
Explain that slight discomfort may be urine, and chest x-rays, may be
felt when the skin is punctured required.
Encourage to avoid stress if possible Make sure the pt or surrogate a
because altered physiologic status consent form
influences and changes normal Check the pt’s history for
hematologic values hypersensitivity to anesthetics
Explain that fasting is not necessary During the test
Apply manual pressure and dressings Remind the pt undergoing a needle
over puncture site on removal of biopsy to sit still
dinner Assist w/ the collection of specimens
Monitor the puncture site for oozing into the appropriate containers, if
or hematoma formation indicated
Instruct to resume normal activities Send the specimens to the laboratory
and diet immediately, if appropriate
After the test
If pt received a general or local This test is done to confirm an infection
anesthetic - monitor VS regularly (pneumonia) and figure out the best way
General anesthetic - check VS q15 to treat it.
minutes for 1h, every 30m for 2h, Other tests
every hour for the 4h, and then every If HCP penumonia - a gram stain on
4h sputum (find out what causes
Administer analgesics for pain and infection)
provide ice bags for comfort Susceptibility testing - find out which
Instruct the pt to wear a support brace antibiotic is applicable for infection
at all times until healing is complete CBC either before or with the blood
Observe and report bleeding, culture - test level of WBC
tenderness, and redness at biopsy site Results
Provide emotional support while Test results may not mean a problem
waiting Dx. A positive result means bacteria or
yeast are present in your blood
D. Blood Culture & Sensitivity Test A negative result means that no signs
- blood is injected into bottles with culture of any bacteria or yeast were found in
media to determine whether the blood
microorganisms have invaded the pt’s Procedure
bloodstream Done with at least 2 blood samples
- a test to find germs (such as bacteria or a (multiple samples produces accurate
fungus) that can cause an infection results)
- checks to see what kind of medicine, Blood samples are placed in a dish
such as an antibiotic, will work best to with a substance that promotes
treat the illness or infection growth of bacteria or yeast - called
Nursing Responsibilities: culture
After the test Results after 24h, but it can take 48h
If pt received a general or local anes - to 72h to find out the specific bacteria
monitor VS regularly or yeast causing your infection
General anes - check VS q15m for 1h, Risks
every 30m for 2h, every h for the next Bleeding
4h, and then every 4h Infection
Administer analgesics for pain and Bruising
provide ice bags for comfort Feeling lightheaded
Instruct the pt to wear a support brace Slight sting or pain when needle is
at all times until healing is complete inserted
Observe and report bleeding, Soreness of the site
tenderness, and redness at biopsy site Antibiotic effect
Provide emotional support while Blood sample should be drawn just
awaiting Dx. before taking antibiotics
Blood Culture Antibiotic could slow the growth of
- to find out systemic infection the infecting bacteria
- infection that affects the whole body, not Nursing Responsibilities
just one part Before the test
- sample of blood is studied in a lab to Confirm the pt’s identity
check for bacteria or a type of fungus Explain to pt that procedure is used to
called yeast help identify the organism
Purpose: Inform pt NO restriction of food and
Symptoms of a systemic infection: fluids
Chills Advise pt slight discomfort from the
Fever tourniquet and needle punctures
Tiredness (fatigue) Perform a venipuncture: draw 1-
Confusion 20mL of blood for an adult
Nausea After the test
Rapid breathing or heart rate Apply direct pressure to the
Passing urine less often venipuncture site until bleeding stops
Assess the venipuncture site for Nerve damage
hematoma formation; if one develops, Uses
apply direct pressure. Identify cause of bacterial infection
Prepare to initiate antimicrobial Shape of bacteria and whether they
therapy, as ordered are Gram-positive or negative - to
prescribe an appropriate antibiotic
E. CSF Gram staining while waiting for more specific tests,
- lab proc used to detect the presence of such as a culture, to be completed
bacteria and sometimes funi in a sample For evaluation of a culture - to help
taken from the site of a suspected determine the type of bacteria and to
infection help determine what other tests may
- permits rapid identification of bacterial need to be performed
cause in 60-90% of pts w/ bacterial To detect fungi, including yeast
meningitis Viruses cannot be detected with a
- presence of bacteria is 100% specific, gram stain
but the sensitivity of this test for detection Nursing Responsibility for Lumbar
is variable Puncture
Gram Staining Before the procedure
Involves applying a sample from the Explain the procedure - the purpose
infected area onto a glass slide and of lumbar puncture
allowing it to dry - then treated w/ a Obtain a signed consent form
special stain and examined under a Reinforce diet
microscope Promote comfort
Any bacteria that may be present are Establish a baseline assessment data -
categorized by color and shape during VS and neurologic
the microscopic evaluation: Assist the client to assume a lateral
Color - “gram positive” purple or decubitus (fetal) position
“gram negative” pink Instruct to remain still
Shape - round (cocci) or rod- After the procedure
shaped (bacilli) Apply brief pressure to the puncture
Collection of sample site
Lumbar puncture or “spinal tap” Place the pt flat on bed
- used to sample spinal fluid or give Monitor VS, neurologic status, and
medication I/O - at least every 4h for 24h
Patient Safety Tips Prior to a Lumbar Monitor the puncture site for signs of
Puncture CSF leakage and drainage of blood
Know of any allergies or adverse Encourage increase fluid intake
reactions to medications Label and number the specimen tube
For pregnant or may be pregnant - correctly
doctor or technologist must be aware Administer analgesia as ordered
Leave valuables at home or in the
room F. ELISA Test
Interpreting services - an abbreviation for “enzyme-linked
List of current medications immunosorbent assay”
Stop taking Aspirin and other blood - substitute for certain radioimmunoassay
thinning medications tests, and eventually, it replaced the
For outpatients, must be accompanied Western blot test for HIV confirmation
by an adult - versatile and medical professionals can
Risks perform it easily
Discomfort or pain during the - uses components of the immune system
procedure (such as IgG or IgM antibodies) and
Bleeding into the spinal cord, chemicals for the detection of immune
particularly in ppl who take blood responses in the body (for example, to
thinners or have a low platelet count infectious microbes)
(thrombocytopenia) - involves an enzyme (a protein that
Headache as a result of CSF leakage catalyzes a biochemical reaction) or an
Infection antibody or antigen (immunologic
molecules) that may form an antigen- ELISA test for viral RNA can detect
antibody reaction to provide a positive it (a positive test), not detect it (a
result or, if they do not react, a negative negative test), or be indeterminate
result (borderline test)
Uses Rarely false negative or false positive
Primarily detect proteins (as opposed result
to small molecules and ions such as Nurse Responsibility
glucose and potassium) Explain test procedure - slight
As blood tests to detect antigens that discomfort may be felt when the skin
may be present in the blood. is punctured
The substances detected: Encourage to avoid stress
Hormones, an allergen, viral antigens Explain that fasting is not necessary
(dengue fever), bacterial antigens Apply manual pressure and dressings
(TB, for example), and antibodies that over puncture site on removal of
the body has made in response to dinner
infection (antibodies to hepatitis B, Monitor the puncture site for oozing
for example) or vaccination. or hematoma formation
Can also identify an infectious disease Instruct to resume normal activities
FOUR TYPES: and diet
1. Direct ELISA: attachment of an
antigen to a polystyrene plate followed by G. Western Blot
an enzyme-labeled antibody. - AKA immunoblotting
2. Indirect ELISA: attachment of an - a test for a specific protein within a
antigen to a polystyrene plate followed by protein mixture
an unlabeled or primary antibody Performed after gel-electrophoresis or an
followed by an enzyme-labeled antibody. enzyme-linked immunosorbent assay
3. Sandwich ELISA: a capture antibody (ELISA) test, and it uses antibodies to
is attached to the polystyrene plate, then identify specific proteins
antigen is added that specifically attaches - typically used to confirm a positive HIV
or captures the antigen. diagnosis
4. Competitive ELISA: like the sandwich Principle
ELISA but involves the addition of In this, gel electrophoresis is used to
competing antibodies or proteins when the separate proteins in a sample based on
second antibody is added. their molecular weight
Advantages The separated proteins are then
Generally good and accurate tests transferred to a solid support, which is
Considered highly sensitive and then exposed to antibodies that can
specific (accurate) and compare bind to the target protein
favorably with other methods used for This binding is detected using a
the detection of substances in the chemical or radioactive tag
body Large proteins molecules need to be
More straightforward and easier to denatured before electrophoresis to
perform than older laboratory facilitate their movement in the gel
techniques, which often required Procedure
radioactive materials. Denaturation of proteins
Preparation & Risks: Involves unfolding of the protein’s
P: no special preparation tertiary structure to a linear structure
P: blood is required - blood Detergents such as sodium dodecyl
collection. sulfate are commonly used to
R: rare and associated with blood denature proteins’
withdrawal (infection, vessel damage) Separation of proteins
Actual Results The denatured protein sample is
Hundreds of variations of ELISA loaded onto an electrophoretic gel and
tests an electrical charge is applied
Results and their meaning depend on Protein molecules are separated on
what is being tested the basis of their size and electrical
charge
Transfer to a support membrane Previously known agents whose role
The separated proteins is transferred in specific diseases has previously
to a sheet of blotting paper made of gone unrecognized
nitrocellulose Re-emergence of agents whose
Visualizing target protein incidence of disease had significantly
A primary or monoclonal antibody is declined in the past, but whose
added to the blot, which binds to the incidence of disease has reappeared
target protein (re-emerging infectious diseases)
A labeled secondary antibody which Emerging diseases
binds to the primary antibody is then Respiratory viruses such as influenza
added, allowing detection of the A viruses (IAV) or human respiratory
specific protein syncytial virus (RSV)
Application Avian influenza viruses (AIV) such as
Detection of circulating antibodies IAV H5N1, H7N7, or H9N2 crossed
specific to a single protein or several the species barrier to infect humans
proteins several times in the last years
In clinical diagnosis - HIV testing to (reviewed in Kim et al., 2016)
detect anti-HIV antibody or as Coronavirus disease (COVID-19)
confirmatory tests for diseases Commercially Available Test Systems
(epidermolysis bullosa acquiaita or Respiratory viruses such as IAV,
paraneoplastic pemphigus) influenza B virus (IBV), and RSV -
Analysis of biomarkers such as point-of-care tests (POCTs) and near-
hormones, growth factors, and POCTs
cytokines Three newer generation rapid
In gene expression studies multiplex polymerase chain reaction
Disadvantages systems (mPCRs) are highly accurate
Very delicate and time-consuming Diagnosis of emerging and novel
process viruses, including HboV, RV-C,
The secondary antibody can cause coronaviruses as well as specific
labeling of an incorrect protein subtypes of AIV and reassortant IAV
Insufficient transfer time can result in strains - Polymerase chain reaction
the larger proteins not transferring (PCR) remains the gold standard
properly technique for the diagnosis
Well trained technicians are a must Innovative Approaches for Future
for this technique POCTs
Semi-quantitative at best Biosensors
Primary antibody availability is A reliable and cost-effective way to
crucial detect sepcific pathogens in POCT
Nursing Responsibilities setting
Same as in blood testing New Techniques and Prototypes
Capillary convective PCR (CCPCR) -
Tests for emerging infection the reagents circulate across a
Emerging infectious diseases are those temperature gradient in a simple
whose incidence in humans has increased capillary tube, which allows run times
in the past 2 decades or threaten to shorter than 30m - used to test for
increase in the near future non-respiratory viruses like hepatitis
It can challenge efforts to protect C virus
workers as prevention and control Lab-Based nucleic acid amplification
recommendations may not be tests (NAATs) with potential use as
immediately available Point-of-Care Applications
Can be caused by: In comparison to PCRs, isothermal
Previously undetected or unknown NAATs do not require complex
infectious agents devices when working with extracted
Known agents that have spread to nucleic acids
new geographic locations or new Reverse transcription strand invasion-
populations based amplification (RT-SIBA) and
reverse transcription loop-mediated
isothermal amplification (RT-LAMP) Non-pharmacological comfort
- to detect Human metapneumovirus interventions
(HMPV), IAV and MERS-CoV
B. Psychosocial Care
COVID-19 - given to help meet the mental,
An infectious disease caused by a newly emotional, social, and spiritual needs of
discovered coronavirus patients and their families
At this time, no specific vaccines or Include:
treatments for COVID-19 Counseling: aim to assist pt identify goals
Most people infected will experience and potential solutions to problems which
mild to moderate respiratory illness cause emotional turmoil
and recover without requiring special Education: the process of influencing pt
treatment behavior and producing the changes in
Older people, and those with knowledge, attitudes, and skills.
underlying medical problems like Group support: a group of people
CVD, diabetes, chronic respiratory meeting either physically or online to
disease, and cancer are more likely to share information, experiences, problems
develop serious illness and solutions
CDC 2019-nCoV RT-PCR Diagnostic Spiritual support: the goal is to help the
Panel person feel peace and comfort
In early 2020, CDC developed its first
laboratory test kit - CDC 2019 Novel C. Spiritual Care
Coronavirus (2019-nCoV) Real-Time - aspect of health care that supports the
Reverse Transcriptase (RT)-PCR inner person (spirit/soul) to help deal with
Diagnostic Panel the health challenges that patient and their
During validation of the CDC SARS- loved ones is facing
CoV-2 test, some laboratories - spending time with the people important
discovered a problem - reagent to them; spending time in nature; spending
produced a positive result with the time on hobbies; following religious
negative control customs
On June 12, 2020, CDC add the
Promega Maxwell RSC 48 as an Dependent Nursing Care
authorized extraction instrument for A. Pharmacologic
use with the CDC 2019-nCoV rRT- 1. Antibiotics
PCR Diagnostic Panel a. It is used based on the premise that:
infection trigger an immune reaction like
autoimmunity through several
INFECTIOUS, INFLAMMATORY, mechanisms:
AND IMMUNOLOGIC: Molecular mimicry
INDEPENDENT AND DEPENDENT Epitope spreading
NURSING CARE Bystander activation
Independent Nursing Care b. Antibiotics are also utilized for their
A. Physiologic Care anti-inflammatory and
- ensures that any physical needs are being immunomodulatory properties
met and that the patient is in a healthy
condition 2. Antifungal agents
- promotes physical health and wellness - when there is immunosuppression, a
by providing care and comfort, reducing common therapeutic side-effect
and managing potential health alterations. predisposes pt to invasive fungal
This include: infections
Use of assistive devices There are four main types of antifungal
Elimination drugs:
Nutrition and oral hydration Polyenes (Nystatin, Amphotericin B)
Personal hygiene Azoles (Imidazole - Clotrimazole,
Mobility/immobility Ketoconazole, Miconazole) (Triazole
Rest and sleep - Fluconazole, Isavuconazole,
Itraconazole, Posaconazole, b. Deplete certain immune cells called T
Voriconazole) and B cells and eosinophils
Allylamines (Terbinafine) c. Make it more difficult for immune cells
Echinocandins (Andidulafungin, to travel to spots of infection or injury
Caspofungin, Micafungin) though the body
Types:
3. Keratolytic agents Systemic - can be administered through:
- designed to dissolve skin flakes, scales oral medications, intramuscular, and
and a ranger of skin conditions intravenous injection
- Ex: mild to moderate acne, dandruff, Localized - can be applied through: skin
psoriasis, warts, and hyperpigmentation. creams and ointments, eye drops, ear
Sources: drops, inhalers
> Salycylic Acid: breaks down connection Common Corticosteroids:
between dead cells on the surface of the Prednisone (Deltalone, Prednicot,
skin (exfoliant) Cotolone)
> Urea: soften and soothe the skin. Has Prednisolone (Orapred, Omnipred)
hydrating and anti-itching properties. Cortisone (Cortone)
Helps other medications to penetrate the Hydrocortisone (Cortef, Hydrocort)
skin. Triamcinolone (Aristocort)
> Lactic Acid: exfoliates the skin, while Dexamethasone (Decadron)
also helping to stimulate skin cell renewal Mometasone (Nasonex spray)
and keeping the skin hydrated
> Olive oil: may also be used to remove 6. Immunologic Agents
scales - drugs that can alter the immune
> Other sources: coal tar, pyrithione zine, response, either by enhancing or
glycolic acid, tretinoin, and acitretin. suppressing the immune system
- used to fight infections, prevent and treat
4. Anti-inflammatory agents certain diseases
- reduces inflammation (redness, swelling, Types of immunologic agents
and pain) in the body. Immune globulins
- block the production of a certain body Immunostimulants
chemicals caused by the activation of Bacterial vaccines
inflammatory cells that results to Colony stimulating factors
inflammation. Interferons
Example of commonly prescribed Interleukins
NSAID: Other immunostimulants
Celecoxib (Celebrex) Therapeutic vaccines
Diclofenac (Voltaren) Vaccine combinations
Fenoprofen (Nalfon) Viral vaccines
Indomethacin (Indocin) Immunosuppressive agents
Ketorolac tromethamine (Toradol) Calcineurin inhibitors
Meclofenamate sodium Interleukin inhibitors
Diflunisal Selective immunosuppressants
Tolmetin TNF alfa inhibitors
Ketoprofen
Flurbiprofen B. Surgical procedures
1. Debridement
5. Corticosteroids - removal of devitalized tissue such as
- are powerful anti-inflammatory necrotic tissue, slough, bioburden,
medications from a class of human-made biofilm, and apoptotic cells
or synthetic drugs Common indications for sharp surgical
- when the body’s immune system fails to debridement:
function correctly, and attack its own Removal of the source of sepsis,
body organs, bones, or tissues. mainly necrotic tissue
STEROIDS: “ of local infection to decrease
a. Stop the body from making cytokines bacterial burden, to reduce the
that cause inflammation probability of resistance from
antibiotic treatment, and to obtain - excisions that involve removing the
accurate cultures epidermis and part of the dermis or
Collection of deep cultures taken after epidermis and the entire dermal layers are
debridement from the tissue left generally termed partial- or full- thickness
behind to evaluate persistent infection surgical excisions
and requirements for systemic Possible Complications:
antibiotic treatment Excessive scarring
Stimulation of the wound bed to Signs of infection such as fever and
support healing and to prepare for a chills
skin graft or flap Drainage from the wound site
Complications include: Nerve damage
Irritation Bleeding
Bleeding Swelling
Damage to healthy tissue Pain and discomfort
Allergic reaction Incision reopening/dehiscence
Pain Post Excision Care:
Bacterial infection Keep the sterile bandage to prevent
Post debridement care the risk of infection
1. Regularly change the dressing Maintain the excision site dry
2. Keep the dressing dry Pt is on antibiotic therapy to promote
3. Keep the wound clean wound healing
4. Don’t apply pressure. Use special Avoid strenuous activity for at least 2
cushions to avoid placing weight on weeks after the surgery
wound. Pt is advised to refrain from smoking
for at least a week as it impairs would
2. Incision and Drainage (I&D) healing
- primary treatment for skin and soft tissue Pain medication is given as necessary
abscesses, w/ or w/o adjunctive antibiotic Follow-up w/ the doctor after 1-2
therapy weeks
Complications:
Normally I&D is well tolerated with
pain as the most common
complication
Becteremia and sepsis
Chronic draining sinuses and fistulas,
secondary to inadequate drainage of
deep or complicated abscesses
Post I&D Care:
Reevaluate and redress the wound in
24-48h except for some small
abscesses. Which do not need to be
monitored closely
Postoperative analgesics may be
required for pain
Instruct the pt to elevate the wound
and keep dressing and splint clean
and intact before the 1st follow-up
visit
Pts should be reevaluated if they have
worsening pain, increased drainage,
or spreading erythema
Antibiotic therapy at least 5-7 days
after the procedure
3. Excisional Surgery
- removal of growths on superficial
structures
You might also like
- Parasite Summary Table FinalDocument3 pagesParasite Summary Table FinalTamarah Yassin100% (1)
- Dictionary of Veterinary Terms: Vet-Speak Deciphered for the Non VeterinarianFrom EverandDictionary of Veterinary Terms: Vet-Speak Deciphered for the Non VeterinarianNo ratings yet
- IntussusceptionDocument24 pagesIntussusceptionOjambo Flavia100% (1)
- Cholecystitis Concept MapDocument4 pagesCholecystitis Concept Mapnursing concept maps100% (7)
- Microbiology and Parasitology Week 3. ABCDDocument21 pagesMicrobiology and Parasitology Week 3. ABCDohsehuns wifeuNo ratings yet
- URINARY TRACT INFECTION - FinalDocument86 pagesURINARY TRACT INFECTION - FinalShreyance Parakh100% (2)
- Report ViewerDocument2 pagesReport ViewerAsif Fareed QaisraniNo ratings yet
- Dysphagia, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandDysphagia, A Simple Guide To The Condition, Treatment And Related ConditionsRating: 5 out of 5 stars5/5 (1)
- AppendectomyDocument6 pagesAppendectomyapi-3797941100% (10)
- (Document Title) : Group 4: Ilarde, Judegarcia, Krllopez, Klim Casing, Rychele BSN4 2019Document8 pages(Document Title) : Group 4: Ilarde, Judegarcia, Krllopez, Klim Casing, Rychele BSN4 2019qwerty24No ratings yet
- Virus Explorer ActivityDocument4 pagesVirus Explorer ActivityDiane Princess SultanNo ratings yet
- Neonatal Acute Abdomen. 7th YrDocument54 pagesNeonatal Acute Abdomen. 7th YrFreeburn SimunchembuNo ratings yet
- Interstitial CystitisDocument9 pagesInterstitial CystitisKousik Amancharla100% (3)
- Activity 11 - Nursing Care Plan Septic ShockDocument2 pagesActivity 11 - Nursing Care Plan Septic ShockCloe CorpuzNo ratings yet
- Liver Biopsy - H. Takahashi (Intech, 2011) WWDocument414 pagesLiver Biopsy - H. Takahashi (Intech, 2011) WWmientweg100% (1)
- Thyroid Encyclopedia: Encyclopedia of Thyroid Disease, Thyroid Conditions and Thyroid CancerFrom EverandThyroid Encyclopedia: Encyclopedia of Thyroid Disease, Thyroid Conditions and Thyroid CancerNo ratings yet
- Assisting in EndosDocument6 pagesAssisting in EndosTheSweetpea501No ratings yet
- Approach To Abdominal Pain in The Emergency DepartmentDocument27 pagesApproach To Abdominal Pain in The Emergency Departmentdebra_euromNo ratings yet
- Expanded Program On Immunization ReportDocument38 pagesExpanded Program On Immunization ReportKimm Delos ReyesNo ratings yet
- Lymphatic-System-and-Body-Defense PDFDocument57 pagesLymphatic-System-and-Body-Defense PDFJulia Stefanel PerezNo ratings yet
- Pingen, Kathleen Joy R. BSN 3ADocument3 pagesPingen, Kathleen Joy R. BSN 3AKathleen Joy PingenNo ratings yet
- UntitledDocument40 pagesUntitleddNo ratings yet
- A Case Study: Nephrolit HiasisDocument19 pagesA Case Study: Nephrolit HiasisCarna BuenconsejoNo ratings yet
- Mass Casualty Incident MCIDocument20 pagesMass Casualty Incident MCIAiza Nicole BarelaNo ratings yet
- Lay Language GlossaryDocument16 pagesLay Language GlossaryqubiivanNo ratings yet
- Intestinal ObstructionDocument13 pagesIntestinal Obstructionsantosh kumarNo ratings yet
- Nursing Care For Children With Urinary DisordersDocument55 pagesNursing Care For Children With Urinary DisordersTania Febria AzizahNo ratings yet
- Elimination - Urinary and BowelDocument58 pagesElimination - Urinary and BowelAnn A.No ratings yet
- NCM 101 Health AssessmentDocument4 pagesNCM 101 Health AssessmentAinah Batua-anNo ratings yet
- Diagnostic TestDocument40 pagesDiagnostic TestLimYi100% (1)
- Acute Abdomen: DR Teamir Negussie Assistant Professor Dept of SurgeryDocument69 pagesAcute Abdomen: DR Teamir Negussie Assistant Professor Dept of SurgeryteamirNo ratings yet
- Pedsinreview 2021005196Document4 pagesPedsinreview 2021005196Claudio MontiNo ratings yet
- Decelos ColostomyDocument7 pagesDecelos ColostomyCharlene Sumba DecelosNo ratings yet
- Abdominal Examination DetailedDocument22 pagesAbdominal Examination Detailedsaveetha purushothamanNo ratings yet
- ABC MsDocument17 pagesABC MsdrewbieskieeNo ratings yet
- Abdominal PainDocument11 pagesAbdominal PainSNo ratings yet
- GenitoDocument12 pagesGenitofatima_antonioNo ratings yet
- Patients With Multiple DisordersDocument7 pagesPatients With Multiple DisordersKathleen Joy PingenNo ratings yet
- Male RSDocument7 pagesMale RSpravina praviNo ratings yet
- Acute Appendicitis: Patan Academy of Health SciencesDocument10 pagesAcute Appendicitis: Patan Academy of Health Sciencessuman subediNo ratings yet
- Articulo Abdomen AgudoDocument12 pagesArticulo Abdomen AgudoAlejandra VelezNo ratings yet
- Medical 9 Case Study and Medical TermDocument23 pagesMedical 9 Case Study and Medical TermJeremia SimbolonNo ratings yet
- Gynec ExamDocument45 pagesGynec ExamPutri Anggia BungaNo ratings yet
- Chapter 36 The Urinary System in GynaecologyDocument19 pagesChapter 36 The Urinary System in Gynaecologypmj050gpNo ratings yet
- Escherichia Coli Streptococcus Group B Haemophilus Influenzae Streptococcus Pneumoniae Neisseria Meningitides Staphylococcus AureusDocument4 pagesEscherichia Coli Streptococcus Group B Haemophilus Influenzae Streptococcus Pneumoniae Neisseria Meningitides Staphylococcus AureusBrent NicholsNo ratings yet
- The EMERGENCY SEVERITY INDEXDocument6 pagesThe EMERGENCY SEVERITY INDEXWindyNo ratings yet
- NCM 102: Gynecology Nursing ManagementDocument7 pagesNCM 102: Gynecology Nursing ManagementdubhieNo ratings yet
- Diagnostic and Laboratory ProceduresDocument6 pagesDiagnostic and Laboratory ProceduresDon Ray Aganon GalatNo ratings yet
- Kidney InfectionDocument12 pagesKidney InfectionShiangNo ratings yet
- 18 Manuscript For PeritonitisDocument8 pages18 Manuscript For Peritonitiskint manlangitNo ratings yet
- CASE STUDY PPT Group1 - Revised WithoutvideoDocument34 pagesCASE STUDY PPT Group1 - Revised WithoutvideoSamantha BolanteNo ratings yet
- 2 AppendicitisDocument9 pages2 AppendicitisPavi MuruganathanNo ratings yet
- Moleno April Mariebsn Ii F Case Scenario 1 Pediatric-Community Acquired Pneumonia Pcap-C IDocument11 pagesMoleno April Mariebsn Ii F Case Scenario 1 Pediatric-Community Acquired Pneumonia Pcap-C IyounggirldavidNo ratings yet
- Communicable DiseasesDocument162 pagesCommunicable DiseasesCarlo VigoNo ratings yet
- Appendicitis: San Roque Extension, Roxas City, Capiz 5800Document10 pagesAppendicitis: San Roque Extension, Roxas City, Capiz 5800GUEZIL JOY DELFINNo ratings yet
- Introduction To General Pathology VPM 152: Web ReviewDocument41 pagesIntroduction To General Pathology VPM 152: Web ReviewRenien Khim BahayaNo ratings yet
- Stress IncontinenceDocument35 pagesStress IncontinenceVeronica MendozaNo ratings yet
- Pelvis Perineum Cases 04Document5 pagesPelvis Perineum Cases 04Uloko ChristopherNo ratings yet
- Appendix ModuleDocument30 pagesAppendix ModuleNagulan ChanemougameNo ratings yet
- Paralytic IleusDocument5 pagesParalytic IleusKimoy MacabungaNo ratings yet
- Multiple Sclerosis (MS)Document15 pagesMultiple Sclerosis (MS)Arianna Jasmine MabungaNo ratings yet
- Description Incidence Causative AgentDocument7 pagesDescription Incidence Causative AgentJhasseryne Orias SanchezNo ratings yet
- Urinary Tract Infection: Notre Dame of Marbel UniversityDocument4 pagesUrinary Tract Infection: Notre Dame of Marbel Universityspain michaelisNo ratings yet
- History GynecologyDocument23 pagesHistory GynecologyE. Zeynep YilmazNo ratings yet
- Rules and Directions for the Employment of Injections in Various DiseasesFrom EverandRules and Directions for the Employment of Injections in Various DiseasesNo ratings yet
- Booklet-Health Centre Simple Guide For Reaching Every PurokDocument38 pagesBooklet-Health Centre Simple Guide For Reaching Every PurokchateNo ratings yet
- Report ViewerDocument4 pagesReport ViewerAsad PrinceNo ratings yet
- Intestinal Amoebiasis CSDocument34 pagesIntestinal Amoebiasis CSabigailxDNo ratings yet
- Herpes ZosterDocument3 pagesHerpes ZosterjotayuNo ratings yet
- AtsDocument3 pagesAtsIntanNirmalaNo ratings yet
- Bio InsecticideDocument26 pagesBio Insecticidevivek pattani93% (15)
- MicroDocument13 pagesMicroArsalan KhanNo ratings yet
- M. Omberg: Abstracts - 17th World Congress On Disaster and Emergency Medicine s133Document3 pagesM. Omberg: Abstracts - 17th World Congress On Disaster and Emergency Medicine s133Icha YulianiNo ratings yet
- Clinical & Diagnostic Tests For GpatDocument10 pagesClinical & Diagnostic Tests For GpatSHRIKANTNo ratings yet
- PharmacologyDocument116 pagesPharmacologyvargheseNo ratings yet
- PODS Health Global Catalogue - May 2022Document439 pagesPODS Health Global Catalogue - May 2022Malc BergeNo ratings yet
- A Brief Note On: Chicken PoxDocument29 pagesA Brief Note On: Chicken PoxRemesh ChandranNo ratings yet
- Safe Entry Contactless Symptom Detector For CovidDocument60 pagesSafe Entry Contactless Symptom Detector For CovidSujit GangurdeNo ratings yet
- Paeds McqsDocument4 pagesPaeds McqsSidra JavedNo ratings yet
- Tinea Pedis An Update 1Document6 pagesTinea Pedis An Update 1putrinurulapriliaNo ratings yet
- Anemia On Chronic Infection-Dr. Made Gede Dwilingga Utama, Sp.A (K) PDFDocument24 pagesAnemia On Chronic Infection-Dr. Made Gede Dwilingga Utama, Sp.A (K) PDFKukuh Prasetyo WibowoNo ratings yet
- Sarla Birala BrochureDocument18 pagesSarla Birala BrochurewithraviNo ratings yet
- Practice: Pneumomediastinum and Subcutaneous Emphysema Associated With Pandemic (H1N1) Influenza in Three ChildrenDocument3 pagesPractice: Pneumomediastinum and Subcutaneous Emphysema Associated With Pandemic (H1N1) Influenza in Three ChildrenYandiNo ratings yet
- Purwanchal Nagrik SamityDocument6 pagesPurwanchal Nagrik SamityMohit DasNo ratings yet
- Aasha Ram BapuDocument10 pagesAasha Ram BapussmaddiNo ratings yet
- Bakul-Patofisiologi TraumaDocument53 pagesBakul-Patofisiologi TraumaClarissa SuheryNo ratings yet
- Mouhamadou Lamine Sarr CPC 1B MR Brunson Peace 2 Semester English TestDocument3 pagesMouhamadou Lamine Sarr CPC 1B MR Brunson Peace 2 Semester English TestLamine SarrNo ratings yet
- HPV Immunisation - MalaysiaDocument13 pagesHPV Immunisation - MalaysiaMadeline TanNo ratings yet