Professional Documents
Culture Documents
Ensa
Uploaded by
075. Hortensa MukudjeyOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ensa
Uploaded by
075. Hortensa MukudjeyCopyright:
Available Formats
28 absorption of topically applied nicotine.
50 Regional dif-
ferences in the percutaneous absorption of piroxicam,
For example, whereas the skin of aged people exhib-
its normal barrier function, the recovery of barrier
a nonsteroidal antiinflammatory drug, depend on the activity after perturbation is markedly reduced.63 This
local vasculature rather than on skin barrier function.57 kinetic basis for reduced barrier function may also
An additional consideration is that the rate of account for interindividual variation in barrier func-
resorption may indirectly influence the diffusion of tion or the apparently increased susceptibility of cer-
compounds to the underlying musculature, tissues, tain individuals to contact dermatitis.64
and joints.58 The principle of locally enhanced deliv-
ery to underlying musculature has been demon-
strated for piroxicam as well as several local anesthetic OTHER FACTORS THAT
preparations.59
AFFECT ABSORPTION
INFLUENCE OF STRATUM CORNEUM
Part 28
PATHOLOGIC PROCESSES Stratum corneum, the rate-limiting barrier to percuta-
ON SKIN BARRIER neous drug delivery, is composed of ceramides, free
fatty acids, and cholesterol in a 1:1:1 molar ratio. By
::
FUNCTION weight, the stratum corneum consists of 50% cerami-
Topical and Systemic Treatments
des (acylceramides being the most abundant), 35%
Reduced skin barrier function has been observed in cholesterol, and 15% free fatty acids. Stratum corneum
pathologic conditions, including the ichthyoses,60 thickness and thus drug penetration vary depending
psoriasis,27 atopic dermatitis,61 and contact dermatitis.61 on body site (Fig. 183-2).65
It is generally accepted that this is attributable to struc- There are two main routes for permeation through
tural alterations in the stratum corneum. These struc- the stratum corneum: the (1) transepidermal and (2)
tural deficiencies may arise from an absence of an transappendageal pathways (Fig. 183-3). The transap-
enzyme or structural protein in the underlying viable pendageal, or shunt, route involves the flow of mol-
tissues or may be related to the improper formation ecules through eccrine glands and hair follicles via the
of the stratum corneum resulting from an increase in associated sebaceous glands.66 In the transepidermal
keratinocyte proliferation. Thus, in individuals pre- route, molecules pass between the corneocytes via the
disposed to a defective barrier, a minor perturbation intercellular micropathway or through the cytoplasm
may become amplified as the skin “attempts to com- of dead keratinocytes and intercellular lipids, defined
pensate” by increasing keratinocyte proliferation.62 A as the transcellular micropathway.66,67 The intercellular
further consideration is that the homeostatic mecha- pathway is considered the most important route for
nisms responsible for recovery of barrier activity after cutaneous drug delivery.
perturbation may be altered in some diseases or physi- An important consideration in topical therapy is
ologic states. that diseased skin may have an altered (increased,
Relative percutaneous absorption of hydrocortisone
Foot arch
Ankle
Palm
Ventral forearm
Dorsal forearm
Back
Scalp
Axilla
Forehead
Jaw angle
Scrotum
0 5 10 15 20 25 30 35 40 45
Figure 183-2 Relative percutaneous absorption of hydrocortisone. Regional variation was measured in males using
carbon14-labeled hydrocortisone dissolved in acetone solvent. Values depicted are relative to the percutaneous absorp-
3370 tion of topical applied to the ventral forearm. (Adapted from Feldman RJ, Maibach HI. Regional variation in percutaneous
penetration of 14C cortisol in man. J Invest Dermatol. 1967;48(2):181-83.)
Kang_CH183_p3363-3381.indd 3370 08/12/18 1:46 pm
Penetration pathways
lidocaine and prilocaine, occlusion hastens absorp-
tion into both the skin and the bloodstream, which has
28
Intracellular led in rare cases to cardiac complications from lido-
Transappendegeal
absorption absorption caine toxicity or methemoglobinemia from prilocaine
toxicity.
Stratum
corneum
APPLICATION FREQUENCY
The frequency of topical application for some drugs,
such as corticosteroids, appear to saturate the stratum
corneum so that multiple daily application yields min-
imum penetration increases compared with once-daily
Chapter 183 :: Principles of Topical Therapy
application.71,72 Clinical studies support the same con-
clusion, so many topical package inserts are labeled for
Hair Sweat/
once-daily use.
follicle eccrine
gland
QUANTITY OF APPLICATION
Figure 183-3 Penetration pathways. The quantity of the drug applied likely has a negligible
effect on drug absorption. Obviously, enough drug
must be dispensed and spread to cover the affected
areas. Furthermore, the quantity of drug applied might
decreased, or absent) stratum corneum, thus changing affect patient adherence to the prescribed regimen. For
the body site’s barrier function.68 Abraded or eczema- example, too much applied drug might negatively
tized skin presents less of a barrier. Solvents, surfac- alter the subjective experience of having a medication
tants, and alcohols can denature the cornified layer and on the skin, that is, the drug may feel “wrong” (greasy,
increase penetration; as a result, topical medications caked, chalky, and so on) or is cosmetically unattractive
with these components may enhance absorption.69 (shiny, white color). Regardless, the amount prescribed
Importantly, simple hydration of the stratum corneum must be adequate to treat the affected body surface
enhances the absorption of topically applied steroids area (BSA) for the necessary length of time. In this
by four to five times.10 Abnormal epidermal prolifera- regard, patient education is critical to prevent wasteful
tion disrupts the skin barrier architecture, enhancing overuse or ineffective underuse of the medication. The
percutaneous absorption. amounts of topical medications to dispense is based
on the estimated BSA, frequency of application, and
duration of therapy. For topical medications such as
sunscreens that are used over large areas, underap-
OCCLUSION plication is a problem for most patients. However, for
smaller areas, patients may apply a large amount of an
Occlusion via closed, airtight dressings or greasy oint- ointment, for example, leading to complaints of greasi-
ment bases increases stratum corneum hydration; ness or rubbing off on clothing, which can be mini-
limits rub-off and wash-off of the drug; and, conse- mized by using an appropriate amount. The finger-tip
quently, enhances penetration. Occlusion techniques unit (FTU) is a measurement that allows health care
range from application under an airtight dressing such providers and patients to easily communicate about
as vinyl gloves, plastic wrap, and hydrocolloid dress- treatment application. An FTU is the amount of topical
ings to occlusion at night for treatment of hands and dispensed from a 5-mm-diameter nozzle onto the tip of
feet, to application of a medication already impreg- the palmar aspect of the index finger to the distal inter-
nated into an airtight dressing, as seen in flurandre- phalangeal joint skin crease. One FTU is equivalent to
nolide tape. With many drugs, occlusion increases approximately 500 mg of the topical agent, which can
drug delivery by 10 times the amount of drug deliv- cover about 2% of the BSA.
ered when not occluded.70 This approach can lead to
more rapid onset times and increased efficacy when
compared with topical application alone. On the other
hand, occlusion may also lead to a more rapid appear- MISCELLANEOUS FACTORS
ance of the drug’s adverse effects, such as the ability of
topical corticosteroids to induce local skin atrophy or Vigorous rubbing or massaging of the drug into the
suppression of the hypothalamus–pituitary–adrenal skin not only increases the surface area of skin cov-
axis. Occlusion may promote infection, folliculitis, ered but also increases blood supply to the area locally, 3371
or miliaria. In the case of topical anesthetics such as augmenting systemic absorption. It may cause a local
Kang_CH183_p3363-3381.indd 3371 08/12/18 1:46 pm
28 exfoliative effect that also enhances penetration. The
presence of hair follicles on a particular body site also TABLE 183-3
enhances drug delivery, with the scalp and beard areas Vehicle Ingredients Commonly Used In Topical
presenting less of a barrier compared with the rela- Preparations
tively hairless body sites.
Emulsifying Agents
Reducing the particle size of the active ingredi-
■ Cholesterol
ent increases its surface area–volume ratio, allowing
■ Disodium mono-oleamidosulfosuccinate
for a greater solubility of the drug in its vehicle. This
■ Emulsifying wax
forms the basis for the increased absorption of certain ■ Polyoxyl 40 stearate
micronized drugs.73 ■ Polysorbates
■ Sodium laureth sulfate
■ Sodium lauryl sulfate
CLASSIFICATION AND Auxiliary Emulsifying Agents or Emulsion Stabilizers
■ Carbomer
CLINICAL APPLICATION OF ■ Catearyl alcohol
Part 28
■ Cetyl alcohol
TOPICAL FORMULATIONS ■ Glyceryl monostearate
■ Lanolin and lanolin derivatives
■ Polyethylene glycol
::
The vehicle is the inactive part of a topical preparation
that brings a drug into contact with the skin. Before ■ Stearyl alcohol
Topical and Systemic Treatments
the mid-1970s, pharmaceutical companies performed Stabilizers
limited testing of the impact of vehicle on the potency ■ Benzyl alcohol
of a given formulation. Lack of a scientific analysis ■ Butylated hydroxyanisole
of the vehicle led to the marketing of topical drugs ■ Butylated hydroxytoluene
that, although having different concentrations of the ■ Chlorocresol
■ Citric acid
same active ingredient, nevertheless exhibited simi-
■ Edetate disodium
lar bioavailability and potency. For example, older
■ Glycerin
preparations of triamcinolone acetonide showed no ■ Parabens
real differences in potency among the 0.025%, 0.1%, ■ Propyl gallate
and 0.5% concentrations. By contrast, modern drug ■ Propylene glycol
development attempts to maximize drug bioavail- ■ Sodium bisulfite
ability by optimizing vehicle formulation. Addition- ■ Sorbic acid or potassium sorbate
ally, during the current drug development process, Solvents
dose–response studies determine the maximal effec- ■ Alcohol
tive concentration within a given vehicle, above ■ Diisopropyl adipate
which any further increase in concentration serves no ■ Glycerin
therapeutic benefit. ■ 1,2,6-Hexanetriol
Vehicle of a topical formulation often has beneficial ■ Isopropyl myristate
■ Propylene carbonate
nonspecific effects by possessing cooling, protective,
■ Propylene glycol
emollient, occlusive, or astringent properties. Ratio-
■ Water
nal topical therapy matches an appropriate vehicle
that contains an effective concentration of the drug. Thickening Agents
■ Beeswax
The vehicle functions optimally when it is stable both
■ Carbomer
chemically and physically and does not inactivate the
■ Petrolatum
drug. The vehicle also should be nonirritating, non- ■ Polyethylene
allergenic, cosmetically acceptable, and easy to use. ■ Xanthan gum
Additionally, the vehicle must release the drug into
Emollients
the pharmacologically important compartment of the
■ Caprylic or capric triglycerides
skin. Finally, the patient must accept using the vehicle ■ Cetyl alcohol
or else compliance will be poor. For example, although ■ Glycerin
ointments are often pharmacodynamically more effec- ■ Isopropyl myristate
tive than creams, patients generally prefer creams to ■ Isopropyl palmitate
ointments, and thus, more prescriptions are written for ■ Lanolin and lanolin derivatives
cream-based formulations. Table 183-3 lists many com- ■ Mineral oil
monly used ingredients in topical preparations. Many ■ Petrolatum
of these compounds serve more than one function in a ■ Squalene
■ Stearic acid
particular formulation.
■ Stearyl alcohol
Humectants
■ Glycerin
TOPICAL FORMULATIONS ■ Propylene glycol
3372 ■ Sorbitol solution
See Table 183-4.
Kang_CH183_p3363-3381.indd 3372 08/12/18 1:46 pm
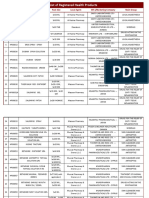
TABLE 183-4
28
Summary of Topical Formulations
FORMULATION COMMON COMPONENTS DESCRIPTION
Powders Zinc oxide, talc (magnesium silicate) Cosmetic, hygienic purposes; ideal for intertriginous areas
and feet
Poultice Dextranomer beads Wound cleansers, absorptive agents; applied on decubiti
or leg ulcers
Ointments
Hydrocarbon base Petrolatum most commonly used Prevent evaporation of moisture from the skin; contain no
(ointments; Silicon ointments preservatives; not for water-soluble drug use; ideal for
oleaginous bases; diaper rash, incontinence, bedsores, colostomy sites
emollients)
Chapter 183 :: Principles of Topical Therapy
Absorption base Lanolin and lanolin derivatives Lubricating and hydrophilic substances; can form
Cholesterol and cholesterol derivatives emulsions; emollients and protectants; easier to
Sorbitan monostearate remove than hydrocarbon bases
Emulsions (water in oil; Sodium lauryl sulfate, quaternary ammonium compounds, Less greasy; easy to spread on film; provide a protective
<25% water) (creams) spans, tweens film of oil as an emollient with a cooling effect
Emulsions (oil in water; Glycerin, propylene glycol, PEG, paraffin alcohols Most commonly used to deliver a drug; easily spread,
>31% water) (creams) water washable and less greasy; easily removed from
the skin; preservative containing (parabens)
Water-soluble bases PEGs (liquid or solid) No preservatives or additives; less occlusive, nonstaining,
greaseless, easily washed off from the skin; poor
absorption into the skin but maintains a high surface
concentration; ideal for topical antifungals and topical
antibiotics
Gels Water, propylene glycol, PEGS with a cellulose derivative or Organic molecules uniformly distributed in a lattice
Carbopol throughout the liquid; deposits drug in concentrated
form; ideal for use in facial or hair bearing areas; lack
protective or emollient effects; may cause drying or
stinging
Pastes (up to 50% Zinc oxide, starch, calcium carbonate, talc Less greasy than ointments; more drying and less
powder in ointment occlusive; used as protectants, sunblocks, or for
base) localizing a drug that may be staining or irritating
Liquids
Solutions Liquid vehicle may be aqueous, hydroalcoholic, or nonaqueous Function as astringents, counterirritants, antipruritics,
■ Tincture: hydroalcoholic solution with 50% alcohol; collodion: emollients
nonaqueous solution of pyroxylin with ether and ethanol
■ Liniments: nonaqueous solutions or drugs in oil or alco-
holic soap solutions
Suspensions Biphasic solution: insoluble drug in up to 20% concentration Cooling effect; easier to apply and allows for uniform
dispersed in liquid coating of larger affected areas; more drying than
ointments
Shake lotions Solutions with added powder; zinc oxide, talc, calamine, Used to dry and cool wet and weeping skin
glycerol, alcohol, and water
Foams Triphasic solution with oil, organic solvents, and water, Deliver a greater amount of drug at an increased rate;
formulated with a hydrocarbon propellant especially useful for scalp application
Aerosols Drug in a solution mixed with a pure propellant Deliver drugs formulated as solutions, suspensions,
(nonpolar hydrocarbons) emulsions, powders, and semisolids; ease of application
to hair-bearing areas
PEG, polyethylene glycol.
the feet. Adverse effects of powders include caking
POWDERS (especially if used on weeping skin), crusting, irrita-
tion, and granuloma formation. Furthermore, powders
Powders absorb moisture and decrease friction. may be inhaled by the user. Most powders contain zinc
Because they adhere poorly to skin, their use is mainly oxide for antiseptic and covering properties, talc (pri-
limited to cosmetic and hygienic purposes. Generally, marily composed of magnesium silicate) for lubricat- 3373
powders are used in the intertriginous areas and on ing and drying properties, and a stearate for improved
Kang_CH183_p3363-3381.indd 3373 08/12/18 1:46 pm
28 adherence to the skin. Calamine is a popular skin-
colored powder composed of 98% zinc oxide and
and its derivatives, cholesterol and its derivatives, and
partial esters of polyhydric alcohols such as sorbitan
1% ferric oxide and acts as an astringent to relieve monostearate. These ointments are lubricating and
pruritus. Other drugs formulated as powders include hydrophilic, and they can form emulsions. They func-
some over-the-counter antifungals.73 tion well as emollients and protectants. They are greasy
to apply but are easier to remove than hydrocarbon
bases. They do not contain water. Examples include
anhydrous lanolin and hydrophilic petrolatum.73
POULTICES
A poultice, also referred to as a cataplasm, is a wet solid WATER-IN-OIL EMULSIONS (CREAMS)
mass of particles, sometimes heated, that is applied to
diseased skin. Historically, poultices contained meal, Emulsions are two-phase systems involving one or
herbs, plants, and seeds. The modern poultice often more immiscible liquids dispersed in another, with the
consists of porous beads of dextranomer. Poultices are assistance of one or more emulsifying agents. A water-
Part 28
used as wound cleansers and absorptive agents in exu- in-oil emulsion, by definition, contains less than 25%
dative lesions such as decubiti and leg ulcers.73 water, with oil being the dispersion medium. The two
phases may separate unless shaken. The emulsifier (or
::
surfactant) is soluble in both phases and surrounds the
dispersed drops to prevent their coalescence. Examples
Topical and Systemic Treatments
OINTMENTS of surfactants used include sodium lauryl sulfate, qua-
ternary ammonium compounds, Spans (sorbitan fatty
Ointments, semisolid preparations that spread easily, acid esters), and Tweens (polyoxyethylene sorbitan
are petrolatum-based vehicles capable of providing fatty acid esters). Preservatives are frequently added
occlusion, hydration, and lubrication. Drug potency to increase emulsion’s shelf life. Water-in-oil emulsions
often is increased by an ointment vehicle because of its are less greasy, spread easily on the skin, and provide
ability to enhance permeability.5 Ointment bases used a protective film of oil that remains on the skin as an
in dermatology can be classified into five categories: emollient, and the slow evaporation of the water phase
(1) hydrocarbon bases, (2) absorption bases, (3) emul- provides a cooling effect.5
sions of water-in-oil, (4) emulsions of oil-in-water, and
(5) water-soluble bases. Dermatologists commonly
refer to the hydrocarbon bases and absorption bases as OIL-IN-WATER EMULSIONS
ointments and the water-in-oil and oil-in-water emul-
An oil-in-water emulsion contains greater than 31%
sion bases as creams. In pharmaceutical terms, all of
water. In fact, the aqueous phase may constitute up
these preparations are ointments and are specifically
to 80% of the formulation. This type of formulation is
indicated for conditions affecting the glabrous skin
most commonly chosen to deliver a dermatologic drug.
(palms and soles) and lichenified areas.10
Clinically, oil-in-water emulsions spread easily, are
water washable and less greasy, and are easily removed
HYDROCARBON BASES from the skin and clothing. Invariably, they contain
preservatives, such as the parabens, to inhibit mold
Also called oleaginous bases, hydrocarbon bases are growth. Additionally, oil-in-water emulsions contain a
often referred to as emollients because they prevent humectant (an agent that draws moisture into the skin),
the evaporation of moisture from skin, are composed such as glycerin, propylene glycol, or polyethylene gly-
of a mixture of hydrocarbons of varying molecular col (PEG), to prevent the cream from drying out. The oil
weights, with petrolatum being the most commonly phase may contain either cetyl or stearyl alcohol (paraf-
used (white petrolatum, except for being bleached, is fin alcohols) to impart a stability and velvety smooth
identical to yellow petrolatum). They are greasy and feel upon application to the skin. After application,
can stain clothing. Silicon ointments are composed of the aqueous phase evaporates, leaving behind a small
alternating oxygen and silicon atoms bonded to organic hydrating oil layer and a concentrated drug deposit.73
groups, such as phenyl or methyl, and are excellent
skin protectants. They can be used for diaper rash,
incontinence, bedsores, and colostomy sites. Hydro- WATER-SOLUBLE BASES
carbon bases are generally stable and do not contain
preservatives. They cannot absorb aqueous solutions Water-soluble bases consist either primarily or com-
and thus are not used for water-soluble drugs.73 pletely of various PEGs. Depending on their molecu-
lar weight, PEGs are either liquid (PEG 400) or solid
(PEG 4000). These formulations are water soluble, do
ABSORPTION BASES not decompose, and do not support mold growth and
therefore require no preservative additives. They are
Absorption bases contain hydrophilic substances that much less occlusive than water-in-oil emulsions and
3374 allow for the absorption of water-soluble drugs. The are nonstaining, greaseless, and easily washed off of
hydrophilic (polar) compounds may include lanolin the skin. Without water, the ointment poorly delivers
Kang_CH183_p3363-3381.indd 3374 08/12/18 1:46 pm
its coformulated drug. Therefore, it is useful in scenar-
ios when the practitioner desires a high surface con-
(alcohol, oils, or propylene glycol). An example of an
aqueous solution is aluminum acetate or Burow solu-
28
centration and low percutaneous absorption of drug. tion. A hydroalcoholic solution with a concentration
For example, topical antifungal drugs and topical anti- of alcohol of approximately 50% is called a tincture. A
biotics (eg, mupirocin) are formulated in this base. collodion is a nonaqueous solution of pyroxylin in a
Gels are made from water-soluble bases by formulat- mixture with ether and ethanol and is applied to the
ing water, propylene glycol, and/or PEGs with a cel- skin with a soft brush. Flexible collodions have added
lulose derivative or Carbopol. A gel consists of organic castor oil and camphor and are used, for example, to
macromolecules uniformly distributed in a lattice deliver 10% salicylic acid as a keratolytic agent. Lini-
throughout the liquid. After application, the aqueous ments are nonaqueous solutions of drugs in oil or
or alcoholic component evaporates, and the drug is alcoholic solutions of soap. The base of oil or soap
deposited in a concentrated form. This provides a faster facilitates application to the skin with rubbing or mas-
release of the drug independent of its water solubility. sage. Liniments can be used as counterirritants, astrin-
Gels are popular because of their clarity and ease of both gents, antipruritics, emollients, and analgesics.73
Chapter 183 :: Principles of Topical Therapy
application and removal. They are suitable for facial
or hairy areas because after application, little residue
remains.10 Nevertheless, they lack protective or emol- SUSPENSIONS (LOTIONS)
lient properties. If they contain high concentrations of
alcohol or propylene glycol, they tend to be drying or A suspension, or lotion, is a two-phase system consist-
cause stinging. Gels require preservatives.12 Newer gel ing of a finely divided, insoluble drug dispersed into
formulations may contain the humectant glycerin, the a liquid in a concentration of up to 20%. Nonuniform
emollient dimethicone, or the viscoelastic polysaccha- dosing can result if the suspended particles coalesce and
ride hyaluronic acid, which can mitigate some of the separate out of a homogeneous mixture, therefore shak-
associated irritation. Nonaqueous gels, with bases such ing of the lotion before application may be required.
as glycerol, may be used for poorly solubilized thera- Examples include calamine lotion, steroid lotions, and
peutics such as 5-aminolevulonic acid.74 emollients containing urea or lactic acid. The applied
Microspheres, or microsponges, are formulated in lotion leaves skin feeling cooler via evaporation of
an aqueous gel. Medication, in this case tretinoin, is the aqueous component. Lotions are easier to apply
combined into porous beads 10 to 25 µm in diameter. and allow for uniform coating of the affected area and
The beads are made up of methyl methacrylate and are often the favorite preparation in treating children.
glycol dimethacrylate. Lotions are more drying than ointments, and prepara-
tions with alcohol tend to sting eczematized or abraded
skin. Lotions are suitable for application to large surface
areas because of their ability to spread easily.73
PASTES
Pastes are simply the incorporation of high concentra-
SHAKE LOTIONS
tions of powders (up to 50%) into an ointment such Shake lotions are lotions to which a powder is added
as a hydrocarbon base or a water-in-oil emulsion. The to increase the surface area of evaporation. As a result
powder must be insoluble in the ointment. Invariably, of increased evaporation, application of shake lotions
they are “stiffer” than the original ointment. Powders effectively dries and cools wet and weeping skin.
commonly used are zinc oxide, starch, calcium carbon- Generally, shake lotions consist of zinc oxide, talc,
ate, and talc. Pastes function to localize the effect of a calamine, glycerol, alcohol, and water, to which spe-
drug that may be staining or irritating (ie, anthralin). cific drugs and stabilizers may be added. Shake lotions
They also function as impermeable barriers that serve tend to sediment and derive their name from the need
as protectants or sunblocks. Pastes are less greasy than to shake the preparation before each use to obtain a
ointments, more drying, and less occlusive.73 homogeneous suspension. In addition, after water has
evaporated from the lotion, the powder component
may clump together and become abrasive. Therefore,
patients should be instructed to remove the residual
LIQUIDS particles before the reapplication of shake lotions.73
Liquids can be subdivided into solutions, suspensions,
emulsions (discussed in section “Ointments”), and FOAMS
foams.
Foams are triphasic liquids composed of oil, organic
solvents, and water, kept under pressure in aluminum
SOLUTIONS cans. Foams are formulated with a hydrocarbon pro-
pellant, either butane or propane.75 The foam lattice is
A solution involves the dissolution of two or more formed when the valve is activated. When in contact
substances into homogenous clarity. The liquid vehi- with skin, the lattice breaks down, the alcohol evapo- 3375
cle may be aqueous, hydroalcoholic, or nonaqueous rates within 30 seconds and leaves minimal residue
Kang_CH183_p3363-3381.indd 3375 08/12/18 1:46 pm
28 in the skin. The alcohol component of the foam is
thought to act as a penetration enhancer, momentarily
by observations in animal models: liposome formu-
lations were believed to enhance the penetration of
altering the barrier properties of the stratum corneum compounds across the skin or to optimize the reten-
and increasing drug delivery through the intercellular tion of bioactive compounds in target tissues.32 How-
route.75 Foam vehicles are highly effective in delivering ever, these early studies, which relied largely on animal
greater amount of active drug at an increased rate com- models, were followed by relatively few in vivo studies
pared with other vehicles that traditionally depend on for humans conducted under standard conditions.69
hydration of the intercellular spaces within the stra- Action mechanism of liposomes is based on a partly
tum corneum. Foams have not been associated with an damaged liquid layer of the stratum corneum, so that
increase in the adverse events, and compliance seems the liposomes can penetrate efficiently into the skin
to be better with this formulation, especially for local- barrier. Deep in the stratum corneum, the liposomes
ized conditions affecting the scalp.75 get damaged and release their drug, which has to pass
through the last cell layers of the stratum corneum by
itself to reach the living cells.
Part 28
There is no clear evidence that liposomes can pass
AEROSOLS the skin barrier as intact structures, but intact lipo-
somes can penetrate along the hair shaft, and this
Topical aerosols may be used to deliver drugs formu- route may be appropriate for delivery of bioactive
::
lated as solutions, suspensions, emulsions, powders, and compounds into sebaceous glands or hair follicles.16,66
Topical and Systemic Treatments
semisolids. Aerosols involve formulating the drug in a Rigid liposomes penetrate better into the hair follicles
solution within a pure propellant. Usually, the propel- than flexible liposomes, which supports the assump-
lant is a blend of nonpolar hydrocarbons. When applied tion that the moving hairs act as a geared pump.52,66
to abraded or eczematized skin, aerosols lack the irrita-
tion of other formulations, especially when the quality
of the skin makes direct application painful or difficult.
Furthermore, aerosols dispense a drug as a thin layer
PENETRATION ENHANCERS
with minimal waste, and the unused portion cannot be
contaminated. Aerosol foams, a relatively new vehicle CHEMICAL ENHANCERS
for drug delivery, are commonly used to deliver cortico-
A penetration enhancer is a compound that is able to pro-
steroids such as betamethasone valerate and clobetasol
mote drug transport through skin. Skin hydration and
propionate. The foam contains the drug within an emul-
interaction with the polar head group of the lipids are
sion formulated with a foaming agent (a surfactant), a
mechanisms for increasing penetration. Water, alcohols
solvent system (eg, water and ethanol), and a propellant.
(mainly ethanol), sulphoxides (dimethylsulphoxide),
On application, a foam lattice forms transiently until it
decylmethylsulphoxide, azones (laurocapram), and
is broken by both the heat of the skin and the heat of
urea are some commonly used compounds.67 Urea is
rubbing the foam onto skin. Foams that are alcohol
thought to act as a penetration enhancer because of
based leave little residue within seconds of application.
its keratolytic properties and by increasing the water
Furthermore, a given corticosteroid formulated in a
content in the stratum corneum. Other substances that
foam vehicle demonstrates comparable potency com-
may also act as enhancers include propylene glycol,
pared with the same corticosteroid in other vehicles.11,76
surfactants, fatty acids, and esters.69
Although aerosols allow for the ease of application (espe-
Vesicular systems are widely used in dermatologic
cially to hair-bearing areas) and high patient satisfaction,
and cosmetic fields to enhance drug transport into the
they suffer from the disadvantages of being expensive
skin through the transcellular and follicular pathways.
and potentially ecologically damaging.73
Examples of vesicular systems include liposomes
(phospholipid-based vesicles), niosomes (nonionic
surfactant vesicles), proliposomes, and proniosomes,
which, respectively, are converted to liposomes and
LIPOSOMES AS niosomes upon hydration.77
TRANSDERMAL DELIVERY
SYSTEMS PHYSICAL ENHANCERS
Physical methods such as the application of a small
Liposomes are microscopic spheres consisting of a electric current (iontophoresis), ultrasound energy
bilayer that encloses an inner aqueous core. A wide (phono- or sonophoresis), and the use of microneedles
variety of cosmetics contain liposomes. Liposome- increase cutaneous drug penetration.67 Microder-
based formulations are safe, cosmetically attractive, moabrasion is the application of crystals (generally
and well accepted. There is considerable evidence that, aluminum oxide) on the skin and the collection of such
at least for some preparations, application of liposomes crystals and skin debris under vacuum suction. This
is mildly occlusive and improves stratum corneum technique enhances drug permeation and facilitates
3376 hydration. Interest in the use of liposomes to enhance drug absorption by altering the architecture of the stra-
the delivery of drugs across the skin has been spurred tum corneum.78
Kang_CH183_p3363-3381.indd 3376 08/12/18 1:47 pm
STABILIZERS
active ingredient mask or immediately treat the toxic
effects of the formulation so that acutely toxic effects
28
are transient.79 For example, allergic contact dermatitis
Stabilizers are nontherapeutic ingredients and include to a preservative in a topical steroid may be masked by
the preservatives, antioxidants, and chelating agents. the effects of the glucocorticoid itself.
Preservatives protect the formulation from microbial
growth. The ideal preservative is effective at a low
concentration against a broad spectrum of organisms, IRRITANT CONTACT DERMATITIS
nonsensitizing, odor free, color free, stable, and inex- Irritation is driven less by drug penetration and more
pensive. Unfortunately, the ideal preservative does by drug concentration. Thus, lowering the concen-
not exist. The parabens are the most frequently added tration of an irritating drug may lower the risk of
preservatives and are active against molds, fungi, and side effects. However, a change in formulation may
yeasts but less effective against bacteria. Alternative reduce the preparation’s efficacy. Nevertheless, often
agents include the halogenated phenols, benzoic acid, using a less concentrated preparation over a greater
Chapter 183 :: Principles of Topical Therapy
sodium benzoate, formaldehyde-releasing agents, and period of time is as therapeutically efficacious while
previously, thimerosal. Most commonly used preser- minimizing adverse effects (eg, the use of benzoyl
vatives may act as contact sensitizers. peroxide 2% to 5% preparations in contrast to 10%
Antioxidants or preservatives prevent the drug preparations).79 In some instances, though, skin irri-
or vehicle from degrading via oxidation. Examples tancy might be central to drug efficacy. For exam-
include butylated hydroxyanisole and butylated ple, although not conclusively shown, the power of
hydroxytoluene, used in oils and fats. Ascorbic acid, immunomodulating agents such as imiquimod might
sulfites, and sulfur-containing amino acids are used rely on an increased innate (inflammatory or irritant)
in water-soluble phases. Chelating agents, such as immune response.
sodium EDTA (ethylenediaminetetraacetic acid) and
citric acid, work synergistically with antioxidants by
complexing heavy metals in aqueous phases. SUBJECTIVE OR SENSORY IRRITANT
CONTACT DERMATITIS
Patients may detect burning or stinging sensations
THICKENING AGENTS without any signs of cutaneous irritation after apply-
ing a topical medication. Several compounds, such
Thickening agents increase the viscosity of products as tacrolimus, sorbic acid, propylene glycol, benzoyl
or suspend ingredients in a formulation. Examples peroxide hydroxy acids, mequinol, ethanol, lactic acid,
include beeswax and carbomers. In addition to func- azelaic acid, benzoic acid, and tretinoin, may induce
tioning as an ointment vehicle, petrolatum may be sensory irritant contact dermatitis in predisposed
added to an emulsion to increase its viscosity. As in individuals.80,81
this example, an ingredient may have a therapeutic
effect as well as acting as part of a vehicle.
ALLERGIC CONTACT DERMATITIS
Contact allergy development depends on local pen-
SIDE EFFECTS AND etration. Allergy is driven by antigen recognition and
presentation, so percutaneous absorption of the drug
PRECAUTIONS must be at a level that guarantees interaction with
the immune effector cells of the skin. Therefore, the
LOCAL EFFECTS contact allergenicity of a drug relates significantly to
percutaneous absorption. In some instances, cutane-
Either the vehicle or its active ingredients may cause ous allergy may be therapeutic, for example, the treat-
local toxicity to the applied site. Local adverse effects ment of patients with cutaneous T-cell lymphoma with
are usually minor and reversible. Major cutaneous side topical nitrogen mustard. The shift in malignant T cells
effects include irritation, allergenicity, atrophy, come- from T helper (Th) 2 to Th1-type cytokine expression is
dogenicity, formation of telangiectases, pruritus, sting- believed to lead to apoptosis of the malignant T cells
ing, and pain. The mechanism of toxicity may be as and tumor regression.82
simple as the desiccation of the stratum corneum (eg,
the removal of sebum and oils by the preparation’s MALIGNANCIES
emulsifiers) or involve a more complex effect on either
the cells of the epidermis or dermis and the struc- Rarely, topical therapy may result in neoplasia. For
tures these cells comprise (ie, epidermis, adnexae). example, the risk of secondary malignancies, such as
Local damage may occur either directly at or within keratoacanthomas, basal and squamous cell carcino-
close proximity to the treated site. Furthermore, irri- mas, lentigo maligna, and primary melanoma, have
tation and damage may appear even after a drug has been reported with the long-term use of nitrogen 3377
been discontinued. Often the therapeutic effects of the mustard.82
Kang_CH183_p3363-3381.indd 3377 08/12/18 1:47 pm
28 OTHERS or infusable biologics, or ultraviolet radiotherapy) to
patients whose disease involves an extensive BSA.
The application of topical corticosteroids to the perior- Nonimmunologic acute toxicity results from substances
bital skin has been suggested to induce cataracts and such as pesticides and chemical warfare agents that rap-
increase intraocular pressure.10 idly diffuse through the skin and reach target organs.
IMMUNOLOGIC CONTACT
SYSTEMIC EFFECTS URTICARIA
One should be aware of the potential systemic toxici- In rare instances, anaphylactic shock can be precipi-
ties of topical drugs. Although generally safer than the tated by topical drug application. For example, when
other administration routes, topical application can applied to diseased or abraded skin, bacitracin oint-
result in systemic toxicities ranging from end-organ tox- ment can induce an immediate-type (Type I) hyper-
sensitivity reaction in susceptible individuals. Such
Part 28
icity (central nervous system, cardiac, renal, and so on),
teratogenicity, and carcinogenicity to drug interactions. reactions might be represented by a local and then
These outcomes may relate to the drug itself, its metabo- subsequently generalized pruritus, leading to cardio-
lites, or even a component of the vehicle. pulmonary arrest.73
::
The kinetics of topically applied drugs differ sig-
Topical and Systemic Treatments
nificantly from those administered by other routes. An
important consideration is the lack of hepatic first-pass
MALIGNANCIES
metabolism of a topical drug. This is especially rele- Systemic calcineurin inhibitors have been associated
vant to drugs such as salicylic acid that are relatively with increased risk of lymphoma and nonmelanoma
innocuous when given enterally but may manifest cen- skin cancer. But the topical use of such drugs does not
tral nervous system toxicity when applied topically. yet appear to induce cancer.83 In fact, the risk for lym-
Additionally, acting as a reservoir, the stratum cor- phoma with the use of topical calcineurin inhibitors
neum may store large amounts of a topical drug, and a was assessed in animal studies that demonstrated an
subsequently long diffusion period of many days may increased risk only when blood levels were 30 times
ensue, delivering a steady supply of drug to the sys- higher than those measured after topical application
temic circulation. in human subjects.83 More than 50 cases of lymphoma
Percutaneous toxicity directly relates to percutaneous have been reported, although the topical calcineurin
absorption. Therefore, factors that modulate absorp- inhibitor use may be coincidental. Nevertheless, there
tion also influence toxicity: concentration of drug, its is a need for additional follow-up information to estab-
vehicle, use of occlusion, body site and area treated, lish the long-term safety profile of these drugs.83
frequency of use, duration of therapy, and nature of
the diseased skin. For example, 6% salicylic acid in
Eucerin used for 11 days in the treatment of psoriasis ENDOCRINE SYSTEM
has been associated with epistaxis and deafness, and
the same concentration of salicylic acid in hydrophilic Topical corticosteroids can rarely cause hypothalamic–
cream under occlusion for 4 days for the treatment of pituitary–adrenal axis suppression, growth retarda-
dermatitis (involving the same amount of BSA) may tion, hyperglycemia, iatrogenic Cushing syndrome,
result in hallucination.79 Similar to their effect on sys- and femoral head osteonecrosis.10 Factors that enhance
temically administered drugs, renal and hepatic dis- drug absorption are directly related to an increase in
eases, by influencing drug clearance, also contribute to these side effects; therefore, careful monitoring must
an increased potential for drug toxicity. be ensured when prescribing usage in large surfaces
Infants and young children have a greater surface areas, prolonged use of potent corticosteroids, usage
area–volume ratio and thus are at greater risk of percu- under occlusion, high-potency corticosteroids, or use
taneous toxicity than adults. This phenomenon neces- for the pediatric age group (because of their increased
sitates alternative drugs, formulations, and dosing surface–body mass ratio).
schedules for children with widespread cutaneous dis-
ease. Patients with acute flares of cutaneous illness (eg, TRANSDERMAL DRUGS
psoriasis or atopic dermatitis) may require treatment of
a larger BSA in a relatively abbreviated period. These Transdermal drug delivery, in contrast to topical drug
patients may also increase their dose and frequency of delivery, uses topical application of therapeutic drug
application during such flares. Coupled with the likely as a delivery system for systemic therapy. Transdermal
increased percutaneous absorption of the diseased skin, patches have been approved by the FDA since 1981 (sco-
these scenarios exponentially increase the possibility of polamine being the first) for the delivery of numerous
systemic toxicity, and patient education is vital to pre- medications, with more seeking approval. Advantages
vent adverse outcomes.73 To reduce the risk of toxicity of this approach include controlled release, a steady
from topical drugs and to increase treatment efficacy, blood-level profile with zero-order kinetics, lack of a
3378 many practitioners will rationally advocate systemic plasma peak, and, in some cases, improved patient
approaches (ie, methotrexate, cyclosporine, injectable compliance. These patches remain on the skin for
Kang_CH183_p3363-3381.indd 3378 08/12/18 1:47 pm
12 hours to 1 week. A patch consists of a plastic backing,
a reservoir of medication, and either a rate-controlling
9. Feldman SR. Tachyphylaxis to topical corticosteroids:
the more you use them, the less they work? Clin
28
membrane or a polymer matrix system for controlled Dermatol. 2006;24(3):229-230; discussion 230.
diffusion followed by an adhesive facing the skin. The 10. Tadicherla S, Ross K, Shenefelt PD, et al. Topical cor-
most common adhesives used are acrylates, silicones, ticosteroids in dermatology. J Drugs Dermatol. 2009;
8(12):1093-1105.
and polyisobutylenes. These patches have been tested
11. Franz TJ. Kinetics of cutaneous drug penetration. Int J
and are approved for use on the thighs, buttocks, lower Dermatol. 1983;22(9):499-505.
abdomen, upper arms, and chest; application to other 12. Bronaugh RL, Maibach HI, eds. Percutaneous Absorp-
sites can lead to either sub- or supratherapeutic blood tion: Drugs, Cosmetics, Mechanisms, Methodology
levels. Adverse effects of patches include local irritation (Drugs and the Pharmaceutical Sciences). 4th ed.
and allergic contact dermatitis to either an adhesive or Abingdon, UK: Taylor & Francis; 2005.
to the drug itself and may necessitate discontinuation. 13. Flynn G. General introduction and conceptual
differentiation of topical and transdermal drug deliv-
ery systems. In: Shah VP, Maibach HI, eds. Topical
CONCLUSIONS Drug Bioavailability: Bioequivalence and Penetration.
Chapter 183 :: Principles of Topical Therapy
New York: Plenum: Springer; 1993:369.
Topical therapies are a mainstay of treatment for the 14. Vickers CF. Existence of reservoir in the stratum cor-
dermatologist. An understanding of the interactions neum. Experimental proof. Arch Dermatol. 1963;
between a drug’s concentration, penetration, availabil- 88:20-23.
15. Lademann J, Lange-Asschenfeldt S, Ulrich M, et al.
ity, and treatment of diseased skin allows physicians
Application of laser scanning microscopy in derma-
to maximize both efficacy and tolerability of topical tology and cutaneous physiology. In: Non Invasive
therapy. An understanding of local and systemic tox- Diagnostic Techniques in Clinical Dermatology. Berlin:
icities allows selection of appropriate, safe therapy for Springer Berlin Heidelberg; 2014:101-113.
patients and minimizes unwanted effects. Appropriate 16. Otberg N, Richter H, Schaefer H, et al. Visualization
selection of topical agents and patient education on of topically applied fluorescent dyes in hair follicles
proper use can optimize therapeutic outcomes. by laser scanning microscopy. Laser Phys. 2003;13(5):
761-764.
17. Rolland A. Particulate carriers in dermal and trans-
ACKNOWLEDGMENTS dermal drug delivery: myth or reality. In: Walters K,
Hadgraft J, eds. Pharmaceutical Particulate Carriers:
Therapeutic Applications. New York: Marcel Dekker;
Previous authors were Aieska De Souza, Bruce E.
1993:367.
Strober, Hans Schaefer, Thomas E. Redelmeier, Gerhard J. 18. Lademann J, Otberg N, Richter H, et al. Investigation of
Nohynek, and Jürgen Lademann. follicular penetration of topically applied substances.
Skin Pharmacol Appl Skin Physiol. 2001;14(suppl 1):
17-22.
19. Schaefer H, Lademann J. The role of follicular pen-
REFERENCES etration. A differential view. Skin Pharmacol Appl Skin
Physiol. 2001;14(suppl 1):23-27.
1. Feldman SR, Vrijens B, Gieler U, et al. Treatment adher- 20. Toll R, Jacobi U, Richter H, et al. Penetration profile of
ence intervention studies in dermatology and guid- microspheres in follicular targeting of terminal hair
ance on how to support adherence. Am J Clin Dermatol. follicles. J Invest Dermatol. 2004;123(1):168-176.
2017;18(2):253-271. 21. Lademann J, Richter H, Schaefer UF, et al. Hair
2. Foley P, Stockfleth E, Peris K, et al. Adherence to topi- follicles—a long-term reservoir for drug delivery. Skin
cal therapies in actinic keratosis: a literature review. Pharmacol Physiol. 2006;19(4):232-236.
J Dermatolog Treat. 2016;27(6):538-545. 22. Higuchi T. Physical chemical analysis of percutaneous
3. Lee IA, Maibach HI. Pharmionics in dermatology: a absorption process from creams and ointments. J Soc
review of topical medication adherence. Am J Clin Cosmet Chem. 1960;11(85).
Dermatol. 2006;7(4):231-236. 23. Guy R, Hadgraft J, Maibach H. A pharmacokinetic model
4. Anderson KL, Dothard EH, Huang KE, et al. Frequency for percutaneous absorption. Int J Pharm. 1982;11(119).
of primary nonadherence to acne treatment. JAMA 24. Gupta SK, Bashaw E, Hwang S. Pharmacokinetic and
Dermatol. 2015;151(6):623. pharmacodynamic modeling of transdermal prod-
5. Zaghloul SS, Goodfield MJD. Objective assessment of ucts: in vivo methods, problems, and pitfalls. In:
compliance with psoriasis treatment. Arch Dermatol. Shah V, Maibach H, eds. Topical Drug Bioavailability:
2004;140(4):408-414. Bioequivalence and Penetration. New York, Plenum; 1993.
6. Kulkarni AS, Balkrishnan R, Camacho FT, et al. Medi- 25. Kubota K, Sznitowska M, Maibach HI. Percutaneous
cation and health care service utilization related to absorption: a single-layer model. J Pharm Sci. 1993;
depressive symptoms in older adults with psoriasis. 82(5):450-456.
J Drugs Dermatol. 3(6):661-666. 26. Williams PL, Riviere JE. A biophysically based dermato-
7. Molassiotis A, Morris K, Trueman I. The importance pharmacokinetic compartment model for quantifying
of the patient–clinician relationship in adherence to percutaneous penetration and absorption of topi-
antiretroviral medication. Int J Nurs Pract. 2007;13(6): cally applied agents. I. Theory. J Pharm Sci. 1995;84(5):
370-376. 599-608.
8. Snyder A, Farhangian M, Feldman SR. A review of 27. Schaefer H (Hans), Redelmeier TE. Skin Barrier: Prin-
patient adherence to topical therapies for treatment ciples of Percutaneous Absorption. Basel, Switzerland: 3379
of atopic dermatitis. Cutis. 2015;96(6):397-401. Karger; 1996.
Kang_CH183_p3363-3381.indd 3379 08/12/18 1:47 pm
28 28. Elias PM, Menon GK. Structural and lipid biochemical
correlates of the epidermal permeability barrier. Adv
genotype in human subjects treated with a para-
phenylenediamine-containing oxidative hair dye.
Lipid Res. 1991;24:1-26. Food Chem Toxicol. 2004;42(11):1885-1891.
29. Elias PM, Feingold KR. Coordinate regulation of epi- 49. Dressler WE, Appelqvist T. Plasma/blood pharmacoki-
dermal differentiation and barrier homeostasis. Skin netics and metabolism after dermal exposure to para-
Pharmacol Appl Skin Physiol. 2001;14(suppl 1):28-34. aminophenol or para-phenylenediamine. Food Chem
30. Otberg N, Richter H, Schaefer H, et al. Variations of hair Toxicol. 2006;44(3):371-379.
follicle size and distribution in different body sites. 50. Nohynek GJ, Duche D, Garrigues A, et al. Under the
J Invest Dermatol. 2004;122(1):14-19. skin: biotransformation of para-aminophenol and
31. Mangelsdorf S, Otberg N, Maibach HI, et al. Ethnic para-phenylenediamine in reconstructed human epi-
variation in vellus hair follicle size and distribution. dermis and human hepatocytes. Toxicol Lett. 2005;
Skin Pharmacol Physiol. 2006;19(3):159-167. 158(3):196-212.
32. Egbaria K, Weiner N. Liposomes as a drug delivery 51. Guzek DB, Kennedy AH, McNeill SC, et al. Transdermal
system. Adv Drug Deliv Rev. 1990;(5):287-300. drug transport and metabolism. I. Comparison of in
33. Rolland A, Wagner N, Chatelus A, et al. Site-specific drug vitro and in vivo results. Pharm Res. 1989;6(1):33-39.
delivery to pilosebaceous structures using polymeric 52. Novotný J, Kovaríková P, Novotný M, et al. Dimethyl-
Part 28
microspheres. Pharm Res. 1993;10(12):1738-1744. amino acid esters as biodegradable and reversible trans-
34. Nemanic MK, Elias PM. In situ precipitation: a novel dermal permeation enhancers: effects of linking chain
cytochemical technique for visualization of perme- length, chirality and polyfluorination. Pharm Res. 2009;
ability pathways in mammalian stratum corneum. 26(4):811-821.
::
J Histochem Cytochem. 1980;28(6):573-578. 53. Mukhtar H, Khan WA. Cutaneous cytochrome P-450.
Topical and Systemic Treatments
35. Squier CA, Lesch CA. Penetration pathways of differ- Drug Metab Rev. 1989;20(2-4):657-673.
ent compounds through epidermis and oral epithelia. 54. Higo N, Hinz RS, Lau DT, et al. Cutaneous metabo-
J Oral Pathol. 1988;17(9-10):512-516. lism of nitroglycerin in vitro. II. Effects of skin con-
36. Teichmann A, Jacobi U, Ossadnik M, et al. Differential dition and penetration enhancement. Pharm Res.
stripping: determination of the amount of topically 1992;9(3):303-306.
applied substances penetrated into the hair follicles. 55. Riviere JE, Sage B, Williams PL. Effects of vasoactive
J Invest Dermatol. 2005;125(2):264-269. drugs on transdermal lidocaine iontophoresis. J Pharm
37. Maibach HI, Feldman RJ, Milby TH, et al. Regional varia- Sci. 1991;80(7):615-620.
tion in percutaneous penetration in man. Pesticides. 56. Danon A, Ben-Shimon S, Ben-Zvi Z. Effect of exer-
Arch Environ Health. 1971;23(3):208-211. cise and heat exposure on percutaneous absorp-
38. Hueber F, Besnard M, Schaefer H, et al. Percutaneous tion of methyl salicylate. Eur J Clin Pharmacol. 1986;
absorption of estradiol and progesterone in normal 31(1):49-52.
and appendage-free skin of the hairless rat: lack of 57. Monteiro-Riviere NA, Inman AO, Riviere JE, et al.
importance of nutritional blood flow. Skin Pharmacol. Topical penetration of piroxicam is dependent on the
1994;7(5):245-256. distribution of the local cutaneous vasculature. Pharm
39. Hueber F, Schaefer H, Wepierre J. Role of transepider- Res. 1993;10(9):1326-1331.
mal and transfollicular routes in percutaneous absorp- 58. Singh P, Roberts MS. Blood flow measurements in skin
tion of steroids: in vitro studies on human skin. Skin and underlying tissues by microsphere method: appli-
Pharmacol. 1994;7(5):237-244. cation to dermal pharmacokinetics of polar nonelec-
40. Teichmann A, Otberg N, Jacobi U, et al. Follicular pene- trolytes. J Pharm Sci. 1993;82(9):873-879.
tration: development of a method to block the follicles 59. Kushla GP, Zatz JL, Mills OH, et al. Noninvasive assess-
selectively against the penetration of topically applied ment of anesthetic activity of topical lidocaine formu-
substances. Skin Pharmacol Physiol. 2006;19(4):216-223. lations. J Pharm Sci. 1993;82(11):1118-1122.
41. Otberg N, Teichmann A, Rasuljev U, et al. Follicular pen- 60. Williams ML. Ichthyosis: mechanisms of disease.
etration of topically applied caffeine via a shampoo for- Pediatr Dermatol. 1992;9(4):365-368.
mulation. Skin Pharmacol Physiol. 2007;20(4):195-198. 61. Werner Y, Lindberg M. Transepidermal water loss in
42. Pinnagoda J, Tupker RA, Agner T, et al. Guidelines for dry and clinically normal skin in patients with atopic
transepidermal water loss (TEWL) measurement. A dermatitis. Acta Derm Venereol. 1985;65(2):102-105.
report from the Standardization Group of the European 62. Ghadially R, Brown BE, Sequeira-Martin SM, et al.
Society of Contact Dermatitis. Contact Dermatitis. 1990; The aged epidermal permeability barrier. Structural,
22(3):164-178. functional, and lipid biochemical abnormalities in
43. Scheuplein RJ. Mechanism of percutaneous absorp- humans and a senescent murine model. J Clin Invest.
tion. II. Transient diffusion and the relative importance 1995;95(5):2281-2290.
of various routes of skin penetration. J Invest Dermatol. 63. Lavrijsen AP, Bouwstra JA, Gooris GS, et al. Reduced
1967;48(1):79-88. skin barrier function parallels abnormal stratum cor-
44. Rutter N. Clinical consequences of an immature neum lipid organization in patients with lamellar
barrier. Semin Neonatol. 2000;5(4):281-287. ichthyosis. J Invest Dermatol. 1995;105(4):619-624.
45. Kao J, Carver MP. Cutaneous metabolism of 64. Wilhelm KP, Surber C, Maibach HI. Effect of sodium
xenobiotics. Drug Metab Rev. 1990;22(4):363-410. lauryl sulfate-induced skin irritation on in vivo percu-
46. Rolsted K, Benfeldt E, Kissmeyer A-M, et al. Cutaneous taneous penetration of four drugs. J Invest Dermatol.
in vivo metabolism of topical lidocaine formulation in 1991;97(5):927-932.
human skin. Skin Pharmacol Physiol. 2009;22(3):124-127. 65. Feldman RJ, Maibach HI. Regional variation in percu-
47. Jacobi U, Toll R, Sterry W, et al. Do follicles play a role taneous penetration of 14C cortisol in man. J Invest
as penetration pathways in in vitro studies on porcine Dermatol. 1967;48(2):181-183.
skin? An optical study. Las Phys. 2005;15:1594. 66. El Maghraby GM, Barry BW, Williams AC. Liposomes
3380 48. Nohynek GJ, Skare JA, Meuling WJA, et al. Urinary and skin: from drug delivery to model membranes. Eur
acetylated metabolites and N-acetyltransferase-2 J Pharm Sci. 2008;34(4-5):203-222.
Kang_CH183_p3363-3381.indd 3380 08/12/18 1:47 pm
67. Trommer H, Neubert RHH. Overcoming the stratum
corneum: the modulation of skin penetration. A
75. Huang X, Tanojo H, Lenn J, et al. A novel foam vehicle for
delivery of topical corticosteroids. J Am Acad Dermatol.
28
review. Skin Pharmacol Physiol. 2006;19(2):106-121. 2005;53(1 suppl 1):S26-S38.
68. Chiang A, Tudela E, Maibach HI. Percutaneous absorp- 76. Franz TJ, Parsell DA, Halualani RM, et al. Betametha-
tion in diseased skin: an overview. J Appl Toxicol. sone valerate foam 0.12%: a novel vehicle with
2012;32(8):537-563. enhanced delivery and efficacy. Int J Dermatol. 1999;
69. Dragicevic N, Maibach HI, eds. Percutaneous Penetration 38(8):628-632.
Enhancers Chemical Methods in Penetration Enhance- 77. Choi MJ, Maibach HI. Liposomes and niosomes as
ment: Modification of the Stratum Corneum. Springer- topical drug delivery systems. Skin Pharmacol Physiol.
Verlag: Berlin Heidelberg; 2016. 2005;18(5):209-219.
70. Ryan T, ed. Beyond occlusion: dermatology proceed- 78. Karimipour DJ, Karimipour G, Orringer JS. Microderm-
ings. In: No. 137 of International Congress Symposium abrasion: an evidence-based review. Plast Reconstr
Series. London: Royal Society of Medicine Services; Surg. 2010;125(1):372-377.
1988. 79. Zesch A. Short and long-term risks of topical drugs.
71. Wester RC, Noonan PK, Maibach HI. Frequency of Br J Dermatol. 1986;115 suppl:63-70.
application on percutaneous absorption of hydrocor- 80. Farage MA, Katsarou A, Maibach HI. Sensory, clinical
Chapter 183 :: Principles of Topical Therapy
tisone. Arch Dermatol. 1977;113(5):620-622. and physiological factors in sensitive skin: a review.
72. Eaglstein WH, Farzad A, Capland L. Editorial: topical Contact Dermatitis. 2006;55(1):1-14.
corticosteroid therapy: efficacy of frequent applica- 81. Kligman AM, Sadiq I, Zhen Y, et al. Experimental stud-
tion. Arch Dermatol. 1974;110(6):955-956. ies on the nature of sensitive skin. Skin Res Technol.
73. Ricciatti-Sibbald D, Sibbald RG. Dermatologic vehicles. 2006;12(4):217-222.
Clin Dermatol. 7(3):11-24. 82. Kim YH. Management with topical nitrogen mustard in
74. McCarron PA, Donnelly RF, Andrews GP, et al. Stability mycosis fungoides. Dermatol Ther. 2003;16(4):288-298.
of 5-aminolevulinic acid in novel non-aqueous gel and 83. Thaçi D, Salgo R. Malignancy concerns of topical
patch-type systems intended for topical application. calcineurin inhibitors for atopic dermatitis: facts and
J Pharm Sci. 2005;94(8):1756-1771. controversies. Clin Dermatol. 28(1):52-56.
3381
Kang_CH183_p3363-3381.indd 3381 08/12/18 1:47 pm
You might also like
- Pharmaceutics-II LCPS-1 PDFDocument28 pagesPharmaceutics-II LCPS-1 PDFShahzaib Shoukat100% (3)
- Manufacturing Pharmacy Answer Key - RED PACOPDocument29 pagesManufacturing Pharmacy Answer Key - RED PACOPMelbhon Fabro RamosNo ratings yet
- Principle of Topical Agent-FzpDocument16 pagesPrinciple of Topical Agent-FzpMurwani LatifahNo ratings yet
- Water Balance in The SCDocument12 pagesWater Balance in The SCCosNo ratings yet
- Prausnitz Derm Book Chapter 2012Document10 pagesPrausnitz Derm Book Chapter 2012Valentina AdindaNo ratings yet
- Discusion IIIDocument10 pagesDiscusion IIIBelisario riverosNo ratings yet
- 39 Adrenocorticosteroids and Andrenocortical AntagonistsDocument5 pages39 Adrenocorticosteroids and Andrenocortical AntagonistsJENICCA GONo ratings yet
- Anti Age Properties of PhytoglycogenDocument2 pagesAnti Age Properties of PhytoglycogenSevres ParisNo ratings yet
- Ultrasound-Assisted Drug Delivery in Fractional Cutaneous ApplicationsDocument16 pagesUltrasound-Assisted Drug Delivery in Fractional Cutaneous ApplicationsErik BrooksNo ratings yet
- Simon Hill 1989 Rotator Cuff Injuries An UpdateDocument5 pagesSimon Hill 1989 Rotator Cuff Injuries An Updatearaujoaoh07No ratings yet
- Topical AnaesthesiaDocument7 pagesTopical Anaesthesiapaul WongNo ratings yet
- Pharma - SkinDocument8 pagesPharma - Skinreference books100% (1)
- Nephrotic Syndrome: Components, Connections, and Angiopoietin-Like 4 - Related TherapeuticsDocument6 pagesNephrotic Syndrome: Components, Connections, and Angiopoietin-Like 4 - Related TherapeuticsDiego Kaleth BastidasNo ratings yet
- Novel Mechanisms and Devices To Enable Successful Trans Dermal Drug DeliveryDocument14 pagesNovel Mechanisms and Devices To Enable Successful Trans Dermal Drug Deliveryapi-3750955100% (1)
- Cosmetics 06 00052Document11 pagesCosmetics 06 00052Ali HadjinNo ratings yet
- Transdermal BioavalibilityDocument13 pagesTransdermal BioavalibilityRizqon MukhaddamNo ratings yet
- 295 PDFDocument6 pages295 PDFHaola andaniNo ratings yet
- Gastrointestinal Mucus: R AN EDocument24 pagesGastrointestinal Mucus: R AN EFlorsie MirandaNo ratings yet
- Transdermal Drug DeliveryDocument38 pagesTransdermal Drug DeliveryJhansi SattiNo ratings yet
- Kinetics of Skin Optical Clearing at Topical Application of 40%-GlucoseDocument8 pagesKinetics of Skin Optical Clearing at Topical Application of 40%-GlucoseMindaugas TNo ratings yet
- Symmetrical Intertriginous and Flexural Exanthema Due To Bortezomib (A Proteasome Inhibitor) Given For MyelomaDocument3 pagesSymmetrical Intertriginous and Flexural Exanthema Due To Bortezomib (A Proteasome Inhibitor) Given For MyelomaLucin HuseinNo ratings yet
- Dermofat Grafts The: Extraconal OrbitalDocument4 pagesDermofat Grafts The: Extraconal OrbitalJeane SuyantoNo ratings yet
- Experimental Dermatology - 2008 - Proksch - The Skin An Indispensable BarrierDocument10 pagesExperimental Dermatology - 2008 - Proksch - The Skin An Indispensable BarrierDanna Valentina MartinezNo ratings yet
- Update On Systemic Glucocorticosteroids in Dermatology: C. MD, T. MDDocument15 pagesUpdate On Systemic Glucocorticosteroids in Dermatology: C. MD, T. MDAsiatiNo ratings yet
- ANA213 - Urinary System - AY2020-2021 PDFDocument42 pagesANA213 - Urinary System - AY2020-2021 PDFSairelle Sordilla ObangNo ratings yet
- Art:10.1007/s00266 013 0134 0Document10 pagesArt:10.1007/s00266 013 0134 0FabianaNisanNo ratings yet
- Transdermal Drug Delivery System - PendahuluanDocument18 pagesTransdermal Drug Delivery System - PendahuluanRizqon MukhaddamNo ratings yet
- The Use of Botulinum Toxin Type A in Aesthetic Mandibular ContouringDocument12 pagesThe Use of Botulinum Toxin Type A in Aesthetic Mandibular ContouringP.No ratings yet
- Anatomy of The SkinDocument15 pagesAnatomy of The SkinTrustia RizqandaruNo ratings yet
- Rugas de Acordeon 2012Document10 pagesRugas de Acordeon 2012Dr. Frederico NevesNo ratings yet
- Creatine Face-CareDocument9 pagesCreatine Face-Careemiliana.wirawanNo ratings yet
- 2011 Article 9715Document8 pages2011 Article 9715Junior LopesNo ratings yet
- Systemic Absorption of Topically Administered DrugsDocument8 pagesSystemic Absorption of Topically Administered Drugstaner_soysuren100% (2)
- Part 1: The Role of Filaggrin in The Stratum Corneum Barrier and Atopic SkinDocument7 pagesPart 1: The Role of Filaggrin in The Stratum Corneum Barrier and Atopic SkincuribepNo ratings yet
- Bouchez Natali 2001Document7 pagesBouchez Natali 2001Horacio SilvaNo ratings yet
- Overcoming The Stratum Corneum: The Modulation of Skin PenetrationDocument17 pagesOvercoming The Stratum Corneum: The Modulation of Skin Penetrationmaulana faridNo ratings yet
- Trommer 2006Document17 pagesTrommer 2006maulana faridNo ratings yet
- Thyl-2-P YrrolidoneDocument11 pagesThyl-2-P Yrrolidonetakron.chantadeeNo ratings yet
- The Tape-Stripping Technique As A Method For Drug Quantification in SkinDocument27 pagesThe Tape-Stripping Technique As A Method For Drug Quantification in SkinfelinsiamelvanNo ratings yet
- 07 Dermatological Formulation and Transdermal SystemsDocument81 pages07 Dermatological Formulation and Transdermal SystemsAlberto JacobusNo ratings yet
- Formulation and Invitro Characterisation of Mucoadhesive Microspheres of Oseltamivir by Ionic Gelation MethodDocument12 pagesFormulation and Invitro Characterisation of Mucoadhesive Microspheres of Oseltamivir by Ionic Gelation MethodSriram NagarajanNo ratings yet
- Drug StudyDocument11 pagesDrug StudySean DadulaNo ratings yet
- v4 A7 Tudor-Costinel Serban IchtyosisDocument3 pagesv4 A7 Tudor-Costinel Serban IchtyosisMinnossNo ratings yet
- Bir 1987 24606Document7 pagesBir 1987 24606Constanza Martinez ArancibiaNo ratings yet
- Transdermal Drug Delivery System: Shirode Rahul ADocument37 pagesTransdermal Drug Delivery System: Shirode Rahul AFrancisco MarcanoNo ratings yet
- Skin: Unique Anatomy: The IowerDocument3 pagesSkin: Unique Anatomy: The IowerAnonymous kdBDppigENo ratings yet
- Topical Drug DeliveryDocument21 pagesTopical Drug Deliveryeva damamainNo ratings yet
- Schwartz Cpap 16 Skin and Subcutaneous TissueDocument16 pagesSchwartz Cpap 16 Skin and Subcutaneous TissueRem AlfelorNo ratings yet
- Actinic Cheratosis - A ReviewDocument4 pagesActinic Cheratosis - A ReviewMARIUS-MIRCEA POPESCU-MICLOSANUNo ratings yet
- Mucoadhesive Drug Delivery System PDFDocument42 pagesMucoadhesive Drug Delivery System PDFdrgdswNo ratings yet
- RETINOL (Improvement of Naturally Age Skin)Document7 pagesRETINOL (Improvement of Naturally Age Skin)produksi roiNo ratings yet
- Pentravan Scientific BrochureDocument38 pagesPentravan Scientific BrochureГабриела ГеоргиеваNo ratings yet
- Ultrastructure of Rat Adenohypophysis: Correlation with FunctionFrom EverandUltrastructure of Rat Adenohypophysis: Correlation with FunctionNo ratings yet
- Extra-Oral Nerve: BlocksDocument4 pagesExtra-Oral Nerve: Blocksleslie kalathilNo ratings yet
- Expert Opinion On Drug Delivery Volume 3 Issue 6 2006 (Doi 10.1517/17425247.3.6.727) Benson, Heather AE - Transfersomes For Transdermal Drug DeliveryDocument11 pagesExpert Opinion On Drug Delivery Volume 3 Issue 6 2006 (Doi 10.1517/17425247.3.6.727) Benson, Heather AE - Transfersomes For Transdermal Drug DeliveryprinceamitNo ratings yet
- Specialized Techniques in DermatopathologyDocument23 pagesSpecialized Techniques in Dermatopathologyadriana PeraltaNo ratings yet
- ACS Parotidectomy PDFDocument10 pagesACS Parotidectomy PDFadel santosNo ratings yet
- Cutaneous Microdialysis Is It Worth The 2006 Journal of Investigative DermaDocument3 pagesCutaneous Microdialysis Is It Worth The 2006 Journal of Investigative DermaMedina PabloNo ratings yet
- Sdarticle 32Document8 pagesSdarticle 32api-19973331No ratings yet
- 42 PDF PDFDocument6 pages42 PDF PDFSelvi Silvia EmalianyNo ratings yet
- HTMLE SEMINAR NOTES DOC. ORTEGA - CompressedDocument35 pagesHTMLE SEMINAR NOTES DOC. ORTEGA - CompressedNISSI JUNE T. UNGABNo ratings yet
- The Photobiology of LED PhototherapyDocument2 pagesThe Photobiology of LED Phototherapysanjay6969No ratings yet
- Midterm Unit 5Document5 pagesMidterm Unit 5Catherine SsiNo ratings yet
- Surface Tension Impact On Pharma ProductsDocument4 pagesSurface Tension Impact On Pharma ProductsOmar Alta'amerehNo ratings yet
- Clay Minerals in Skin Drug DeliveryDocument14 pagesClay Minerals in Skin Drug Deliverynourisana85No ratings yet
- جرعات الاطفالDocument50 pagesجرعات الاطفالWael Hamdy100% (1)
- Liquid FormsDocument29 pagesLiquid FormsFranchesca LugoNo ratings yet
- Intertrigo and Common Secondary Skin InfectionsDocument6 pagesIntertrigo and Common Secondary Skin InfectionsSkonbull Kennel100% (1)
- How To Extract Lemongrass OilDocument4 pagesHow To Extract Lemongrass OilSam GamezNo ratings yet
- Alopecia Areata Symptoms TreatmentsDocument4 pagesAlopecia Areata Symptoms TreatmentsBudac ViorelNo ratings yet
- A Systematic Review of Contact Dermatitis Treatment and PreventionDocument24 pagesA Systematic Review of Contact Dermatitis Treatment and PreventionMuhammad Riza FahlawiNo ratings yet
- DDS-lab Midterm ReviewerDocument13 pagesDDS-lab Midterm Reviewerchincaluscusin4No ratings yet
- Diaper Rash OverviewDocument6 pagesDiaper Rash OverviewJonas Marvin AnaqueNo ratings yet
- Pharmacy Technician Certification 8172019 ExamDocument115 pagesPharmacy Technician Certification 8172019 Examfatdaddys100% (2)
- KATINKO PAIN AND ITCH RELIEVING-camphor (S Ynthetic), Menthol, Methyl S Alicylate Ointment Greens Tone Pharmaceutical H.K. IncDocument4 pagesKATINKO PAIN AND ITCH RELIEVING-camphor (S Ynthetic), Menthol, Methyl S Alicylate Ointment Greens Tone Pharmaceutical H.K. IncMarvin VerdadNo ratings yet
- Clean Treat: Caring For Eczema - Easy As 1, 2, 3Document1 pageClean Treat: Caring For Eczema - Easy As 1, 2, 3Ferdinand EnebradNo ratings yet
- Aromatherapy EO Reference Chart PDFDocument10 pagesAromatherapy EO Reference Chart PDFJanice Ng100% (2)
- Testing of Ointment Quality & Challenges in Ointment Formulation.Document10 pagesTesting of Ointment Quality & Challenges in Ointment Formulation.Muhammad Abu HurairaNo ratings yet
- Product BatchDocument44 pagesProduct BatchKarthik SunnyNo ratings yet
- Brenner and Stevens Pharmacology e Book 5th Edition Ebook PDFDocument62 pagesBrenner and Stevens Pharmacology e Book 5th Edition Ebook PDFjanice.mosley139100% (43)
- BAMU B.pharmacy First Year SyllabusDocument31 pagesBAMU B.pharmacy First Year SyllabusGajanan Vaishnav0% (1)
- NSTP Blue TeamDocument38 pagesNSTP Blue TeamRienz Garren MarianoNo ratings yet
- Ippp-Ii (SSDF)Document139 pagesIppp-Ii (SSDF)Tinsaye HayileNo ratings yet
- Formulation and Evaluation of Antifungal Micro Emulsion-Based Gel For Topical Drug Delivery Using MilletiapinnataDocument15 pagesFormulation and Evaluation of Antifungal Micro Emulsion-Based Gel For Topical Drug Delivery Using MilletiapinnataIJAR JOURNALNo ratings yet
- 02.ophthalmic Solutions and SuspensionsDocument7 pages02.ophthalmic Solutions and SuspensionskhalidNo ratings yet
- 5 6116307916568921949Document15 pages5 6116307916568921949jhafar dlexoNo ratings yet
- Reporter: Date: Group No.: 2 Rating: Experiment No. 10 Ointments Questions: 1. State The Uses Of: A. OintmentsDocument6 pagesReporter: Date: Group No.: 2 Rating: Experiment No. 10 Ointments Questions: 1. State The Uses Of: A. Ointmentsjanicedeguia1394No ratings yet
- DRUG StudyDocument4 pagesDRUG StudyMaica LectanaNo ratings yet
- 11health - EnglishDocument42 pages11health - Englishkolipaka rajeshNo ratings yet
- Appendix C Uniform Terms: Dosage FormsDocument3 pagesAppendix C Uniform Terms: Dosage FormslichenresearchNo ratings yet