Professional Documents
Culture Documents
Bengin SGT 2023
Uploaded by
Hazem MouradCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Bengin SGT 2023
Uploaded by
Hazem MouradCopyright:
Available Formats
Oral Pathology Made Easy ….!!!
Salivary Gland Neoplasm
Salivary Gland
Neoplasm
Dr. Ahmed ElNashar
2023
• Incidence: 2% of head and neck neoplasm & 2nd most common tumors affecting oral cavity (after SCC).
• Etiology: Unknown, but radiotherapy to head and neck considered as an etiological factor.
• Differentiated cells of all cell types of salivary gland tissue are capable of
Multicellular theory producing a neoplasm.
• De-differntiatted theory ) not accepted)
• Stem cell present in (intercalated ducts ) or ( excxretory duct)
• These cell will be differentiated into …….
Bicellular theory (1) epithelial cell that forming the tumor
OR .. (2) myoepithelial cell w is multipotent can differentiate into
multiple & variable cell
Dr Ahmed ElNashar 2023
Oral Pathology Made Easy ….!!! Salivary Gland Neoplasm
CLASSIFICATION
Epithelial Salivary Gland Neoplasm
• Plemorphic adenoma • Mucoepidermoid carcinoma
• Papillary cystic adenoma lymphatosum • Acinic cell carcinoma.
= warthin's tumor • Adenoid cystic carcinoma.
• Oncocytoma = oxyphilic adenoma • Polymorphous adenocarcinoma.
• basal cell adenoma. • Carcinoma Ex pleomorphic adenoma
• Myo-epithelioma • Carcinosarcoma
Malignant
Benign • Canalicular adenoma • metastasizing mixed tumor.
=
= • sebaceous lymphadenoma • Basal cell adenocarcinoma.
Adeno-
adenoma • cystadenoma.
carcinoma • Epithelial Myopepithelial Carcinoma
• Sialadenoma. • Clear cell adenocarcinoma
• Ductal papillomas • Sebaceous adenocarcinoma.
• Sialadeno papilliferum • Lympghoadenocarcinoma.
• Inverted ductal papilloma • Polymorphusadenocarcinoma
• Lymphoadenoma • Squamous cell carcinoma.
• Intraductal papilloma • Adenosquamous cell carcinoma
Other MESENCHYMAL TUMORS
Hemangioma , lipoma , hematolymphoid tumors , lymphoma , metastatic tumors.
DISTRIBUTION
Major (Extra-Oral )(91%)
Minor SG (10%)
Parotid Sub-mand. Sub-lingual Benign Malignant
(70-80%) (12%) (0.3%) 55% 45%
Benign Benign Benign Malignant Malignant
75% 70% 70% 30% 90%
(THE SMALLER THE GLAND. THE GREATER THE LIKELIHOOD OF MALIGNANCY)
-most common S.G.T Pleomorphic adenoma
- most common benign S.G.T. Pleomorphic adenoma
- most common malignant S.G.T. mucoepidermoid carcinoma
- most common malignant S.G.T.in childern mucoepidermoid carcinoma
- most common malignant S.G.T in sublingual SG or minor SG adenoid cystic carcinoma.
- most common tumor of parotid gland in infancy hemangioma (no epithelial SGT).
General Clinical features of SGT
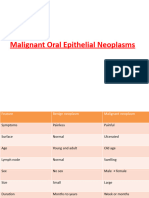
Benign salivary gland tumor Malignant Salivary Gland tumor
Site • 75%of parotid tumors are benign • 45%of minor gland tumors are malignant
• outer surface is smooth (=not ulcerated) • ulcerated, especially intra oral lesions.
• Slowly growing • Rapidly growing or slow e sudden rapid growth.
• Painless =- asymptomatic • painful.
S&S • No facial nerve involvement • Facial nerve paralysis is common
• No enlarged L.N. • Enlarged L.N.
• Soft or rubbery consistency • Sometimes hard consistency
• No-local bone destruction • Bone destruction is usually present
• Capsulated. • Not capsulated.
Metastasis
• No distant metastasis • Metastasize.
Prognosis • Prognosis is good • according to the condition.
Dr Ahmed ElNashar 2023
Oral Pathology Made Easy ….!!! Salivary Gland Neoplasm
Benign Salivary Gland Neoplasm
1.Pleomorphic Adenoma
= Benign Mixed tumor
Introduction
• Most common SGT.
80 % of parotid tumor rte begin
• Role of 80 80% of parotid tumor are pleomorphic adenoma
80% of parotid pleomorphic are in superficial lobe
80 % of untreated pleomorphic adenoma remain bengin.
Histogenesis (origin) :
• Pure epithelial tumor arises from intercalated duct stem cell.
• Stem cell can differentiated giving epiuthelial and myoepithelial cells forming the tumors.
Terminology
• Means arises from more than one germ layer, Not completely accurate??? Pure epithelial tumor
Mixed
• Used here bcoz tumor show variable histological changes ( epith.& stromal component)
Clinical features
Age • 30 - 60.
Sex • Slight ♀> ♂.
• common site extraoral is parotid gland(80%)(superficial lobe & tail) 1st site
Site
• common site intraoral, palate. 2nd site
• Long standing parotid lesions may reach giant size (=grotesque).
size
. ف الترم االولameloblastoma • تسند على كتف العيان زي ال
• الكالم العامpainless. slowly growing, mobile, soft or slightly firm mass.
• overlying skin is intact.
• On palpation: nodular or globular mass.
S&S • Occur . in post lateral part of palate & junction bn hard and soft.
• Non-mobile ???!! bcoz mucosa is tightly bounded to bone.
palate
• Ulcerated ???!! palate has thin stretched over bone so any swelling may
cause mucosal ulceration.
Gross Pathology تستطيع ان تالحظ مزي ج من االنسجة السوفت و الهارد
• typically lobulated and show various consistencies and structure.
• Incomplete capsule.
Histopathology
- tumor characterized by : (1) multimodal nature. (2) morphologic diversity. (3) partially capsulated
- tumor is capsulated & composed of epithelial element + mesenchyme –like background
Dr Ahmed ElNashar 2023
Oral Pathology Made Easy ….!!! Salivary Gland Neoplasm
• Tumor composed of………. EPITHELIAL COMPONENT + CT COMPONENT
From Myoepithelial cells or Ductal epithelium
• Epithelial component form (DUCTS, TUBULES) , or (NESTS, SHEET)
Epithelial ▪ Duct structure and tubules from ductal epithelium
▪ Squamous metaplasia of ductal epithelium with keratin formation. lar
▪ Sheets of myoepithelial cells (angular cells
• Myxamtous like (=mucoid like), chondroid like , bone or osteoid tissue.
Stroma • believed to be produced by myoepithelial cells?!!! ازاي
=
▪ CHONDROID ??! MUCOID ??!
Intercellular
material ▪ oid mean resemble cartilage tissue…………(not a real cartilage)
• Some cases show bone or osteoid giving calcification.
• capsule may be INCOMPLETE or INFILTRATED WITH tumor cells.
Capsule
• Bcoz of this fact tumor ch. ch. by high rate of recurrence & treated by wide surgical excision.
Tumors composed of myoepith. cells e no ductal elements are called "myoepitheliomas"
- Melting Phenomena myoepithelial cell melt in sea of stroma they produce.
TTT & prognosis
• prognosis is excellent with wide surgical excision. ( i.e with safety margin)
• Best treated by surgical excision e preservation of facial nerve.
• Malignant transformation (5%-10%) to carcinoma EX pleomorphic adenoma.
Lecture notes
• Causes of high rate of recurrence (20%) in pleomorphic??!!
1. incomplete CT capsule. 2. Multi-nodal nature. 3. chondromyxoid material.
2. Warthin’s Tumor
= Papillary cystadenoma lymphomatosum
Introduction
• the 2nd most common benign SGT.
• Heterotropic SGT composed of both epithelial and lymphoid elements.
Histogenesis: ductal cells.
pathogenesis
1st • tumor arise from embryonic Entrapment of SG tissue ein parotid (para or intra parotid) L.N.
(accepted) • ectopic (heterotopic = choristoma)
• reactive lymphoid hyperplasia secondery to chronic irritation.
2nd
• عكس اللي فاتتProliferation of lymphocytes around salivary gland duct.
• there is a strong association e cigarette smoking.
• EBV implicated in pathogenies.
Dr Ahmed ElNashar 2023
Oral Pathology Made Easy ….!!! Salivary Gland Neoplasm
Clinical features
Age • 5th to 8th decade of live
• Early studies ………. ♂ =♀.(5:1)
Sex
• Recent studies…….. ♀= ♂.e slight male predilection
Race • white > black.
• Extraoral : parotid (mostly) , subman d. (occasionally)
Site
• Intraoral : Rare.
• الكالم العام
S&S • Tend to occur bilaterally (2-6%( →mostly metachronous ?!
occurring at different times
Gross Pathology تستطيع ان تالحظ مزي ج من االنسجة السوفت و الهارد
(1) smooth or lobulated. (2)encapsulated (well-demarcated).
(3) solid, with white nodule. (4)cystic spaces with viscous fluid and papillary projection.
Histopathological Features
• Composed of … Mix of epithelium + lymphoid stroma.
• cystic spaces lined e 2raws of epith. Cells
▪ lumina = Inner Layer: eosinophilic columnar cells (oncocyte)
Esinophilc granules are mitochondria detected by EM
Epithelial ▪ basal = outer Layer: cuboidal e central & vesicular nuclei.
• Mucous secreting cells (goblet cells ) scattered bn e[pith lining cells.
• multiple papillary in folding protrude into cystic spaces.
• Focal areas of sq. metaplasia.
Lymphoid • Normal lymphoid stroma shows germinal center (B-lymphocytes) + sinusoidal spaces
Treatment & prognosis
• Conservative surgical removal (= enucleation). Very good prognosis.
• In case of parotid : preservation of facial nerve is recommended.
• (6% - 12%) recurrence rate has been reported, mostly pseudo-recurrence. Bcoz , tumor is multicentric.
3. Oncocytoma
= Oxyphilic adenoma
Introduction
• Rare benign SGT (2.3%). ●common in parotid gland. ●Common in elder.
Origin : Acinic cell (= oncocytes).
Clinical features
Age • 6th decade
Sex • ♀= ♂.
• parotid gland (majority) then submandibular.
Site
• Intraoral : upper lip
• unilateral or bilateral
S&S
• Typical clinical features of benign salivary gland tumor.
Histological features
• oncocytoma is usually a well-circumscribed tumor
• composed of sheets of oncocytes , Sometimes these cells form an alveolar or glandular pattern .
Oncocytes
▪ large polyhedral cells + granular eosinophilic cytoplasm + Central small hyperchromatic or large and vesicular nuclei.
▪ granularity of cytoplasm created by large no of mitochondria, demonstrated by E/M & L/M (PTAH) stain.
▪ My contain glycogen, evidenced by +ve (PAS).
• thin fibrovascular septa + lymphocytic infiltrate may be noted + may contain variable no. of clear cell.
TTT: surgical excision.
Dr Ahmed ElNashar 2023
Oral Pathology Made Easy ….!!! Salivary Gland Neoplasm
4. Basal Cell Adenoma
Introduction
• Rare benign SGT (1-2%).
Origin: ductal cells.
Clinical features
Age • 60 years old.
Sex • ♀>♂.
• extraoral 70 % parotid gland then submandibular SG
Site
• intraoral in upper lip then buccal mucosa then lower lip.
Size • < 3 cm
• Typical clinical features of benign salivary gland tumor.
S&S
• May be mulinodular.
Histological features
• well-defined connective tissue capsule.
• proliferating epithelial cells arranged in 1 of the following manner…..
(1) Solid, sheets of cells resembles bsasal cell carcinoma.
(2) Trabecular- Tubular.
(3) Membranous, thick double membrane (+ve PAS)
TTT: surgical excision.
N.B. Canalicular adenoma (clinically resembles basal cell adenoma) ( upper lip then buccal)
5. Canalicular adenoma
Clinical features
Age • 50 years old (30-60)
Sex • ♀>♂.
Site • 81% of lesion intraoral in upper lip
S&S • Typical clinical features of benign salivary gland tumor.
Histological features
• May be not totally capsulated
• Formed of cords of basaloid cells rembles solid or cystic types of basal cell adenoma.
TTT: surgical excision.
5. Myoepithelioma
Introduction : benign SGT (15%).
Origin : Myoepithelial cells
Clinical features
Age • Adults (53)
Sex • ♀=♂.
• Extraoral parotid gland.
Site
• Intraoral palate.
S&S • Typical clinical features of benign salivary gland tumor.
Histological features
• sheets of myoepithelial cells ( spindle or plasmacytoid or epithelioid or clear cell).
• IHC : P63 , S100, SMA , calponin, CD10, smooth ms. actin.
TTT: surgical excision.
Dr Ahmed ElNashar 2023
Oral Pathology Made Easy ….!!! Salivary Gland Neoplasm
2. Malignant epithelial salivary gland Tumor
Risk Factors
radiation • risk for (pleomorphic adenoma) ( mucoepidermoid carcinoma)
Smoking • risk for (Warthin’s tumor)
Wood, asbestos, rubber, shoes • risk for (Adenocarcinoma)
How to differentiate malignant from benign tumors
1. neural manifestation. 2. Warmer ( d.t. angiogenesis)
3. pigmentation. 4. Fixation ( to overlying skin & underlying CT)
5. rough polypoid surface. 6. Highly vascularized.
7. perineural invasion. 8. Early invasion to bone. Important criteria of palatal SGT
Parameters highly suspect malignancy (suggestive features of malignancy)
1. induration of margins and floor. 2. fixation to underlying CT and overlying skin.
3. ulceration (not respond to TTT). 4. rapid growth.
5. discoloration. 6. pain & neural manifestation.
7. fixed regional lymphadenopathy.
1.Muco-epidermoid carcinoma
Epithelial and mucin producing tumors = Mix of mucous-producing cells and epidermoid
Introduction
• Most common malignant SGT extraoral and in childhood.
• accounting for only (10%) of malignant SGT in major SG. & (15-23) % of malignant SGT in minor SG.
N.B. most common unilateral parotid swelling in children While most common bilateral is mumps.
Histogenesis : reserve cell in ductal syst. (intra or inter lobular)
Clinical features
Age • 5th decade of life.
Sex • ♀>♂.
• extraoral: parotid gland (1st common site)
Site • intraoral : palate (2nd common site)
• it is the most common malignant SGT in submandibular SG.
• CF of benign → Slowly growing, fluctuant painless mass , covered e intact mucosa.
low grade
• In lip : Similar to mucocele. In palate : similar to periapical abscess or cysts.
S&S
• CF of malignant → Rapidly growing mass ±pain, covered e ulcerated mucosa.
High grade
• Similar to sq cell carcinoma.
Gross Pathology
Low grade • Lesion with multiple cystic spaces
High grade • Solid mass with few or no cystic spaces.
Histopathological features
• Composed of a mixture of mucus-producing cells and squamous (epidermoid) cells.
Mucous • Round cells , contain foamy cytoplasm → +ve to mucin stains PAS & (mucicarmine)
• resembles epidermis cells. Reserve cell in origin.
Epidermoid
• squamous or polygonal cell with intercellular bridges & rarely keratinization.
Intermediate • stem cell or reserve cell . ممكن تدي اي واحدة من الخليتين
Clear cell • -------------------------------------------
Dr Ahmed ElNashar 2023
Oral Pathology Made Easy ….!!! Salivary Gland Neoplasm
• Tumor classified into 3 Histopathological grades based on ……
1. Amount of cyst formation. 2. Degree of cytologic atypia
3. No. of mucous, epidermoid& intermediate cells
Low grade Intermediate grade High grade
• cystic spaces • Fewer and smaller cysts. • cystic spaces
• mucous cells • Intermediate & epidermoid = mucous • mucous cells
• epidermoid cell cells • epidermoid cell
• intermediate cells • intermediate cells
• Well differentiated • ------------------------ • poorly differentiated
• atypia. • pleomorphism &mitotic figures • atypia.
More mucous cell , more well differentiated, and more low grade
• Ch.ch by perineural invasion.
Treatment: wide surgical excision + radiation therapy.
Prognosis: Submandibular poorer than parotid + Minor SGT generally good prognosis .
Central muco-epidermoid carcinoma
Most common intrabony SGT
Pathogenesis
• embryonic entrapment of salivary gland tissue entrapped within jaw. (stafen defect= latent bone cyst)
mandible
• mucous cells in wall of dentigerous cysts (95% of cases)
maxilla • mucous cells in lining of maxillary sinus.
Clinical features
• mand.> max. (3:1). most often seen in molar ramus area.
Radiographic features:
• well defined multilocular radiolucency related to unerupted tooth
• DDX : ameloblastoma , Odont.myxoma, OKC , centeral mucoepidermoid carcinoma ركز اربعة بس
Histopathological Features: similar to that of its soft tissue counterpart (mainly low grade)
TTT : Surgical excision is the treatment of choice, followed by radiation therapy.
2. Adenoid cystic carcinoma = cylindroma
Introduction
• Most common malignant SGT of minor SG (any site intraoral) حضات
ركزوا يا ر
• Most common malignant SGT of sublingual SG.
Histogenesis: Ductal & myoepithelial cells.
Clinical features
Age • Middle age.
Sex • ♀=♂.
• major SG (extra-oral) → parotid.
Site
• major SG (intra-oral)→ minor SG & sublingual SG (60%) & sinonasal glands.
• 1st sign → neural manifestation.
• Pain is a common finding??!! Bcoz of perineural invasion.
S&S • Pain starts as a constant dull pain & gradually increase.
• slowly growing but aggressive?!! bcoz it is a hidden lesion so mass present for years prior patient seeking for TTT.
• May present as an ulceration و متعالجش قرحة اكتر من اسبوعين، فخلى بالك، قرحة او الم، اول حاجة ممكن تظهر كلينيكال
Histological features
Cells are small cuboidal,+ large hyper chromtic nuclei + little cytoplasm
Dr Ahmed ElNashar 2023
Oral Pathology Made Easy ….!!! Salivary Gland Neoplasm
• composed of mix of myoepithelial cells & ductal cells , arranged in one of 3 major patterns …..
• Consist of islands of epith. cells that contain multiple cyst like spaces.
cribriform pattern
• Cysts contain basophilic or eosinophilic product or combination.
=
Swiss cheese • most common patterns (classic form) & best to be recognized.
• Cells: well defined with hyperchromatic neucli
Tubular pattern • consists of multiple small ducts or tubules of epith. Cells.
• Consists of larger islands or sheets of tumor cells.
Solid pattern
• Most aggressive pattern e poorest prognosis.
Usually a combination of these 3 patterns is seen, and the tumor is classified based on the predominant pattern .
Ch. ch. by: (1) perineural invasion. (2) early metastasis. (3) bone invasion.
Prognosis
• poor prognosis…..why??
(1) local recurrence :42%. (2) Metastatic spread : lungs and bones.
(3) perinerural invasion. (4) inrabony invasion.
• Solid pattern poorest prognosis (present in max sinus, palate , sublingual & submandibular SG)
TTT :
• Radical surgical excision + radiation therapy.
• d.t. perineural invasion we usually sacrifices by facial nerve.
3. POLYMORPHUS LOW GRADE ADENOCARCINOMA
Introduction
• 1st described in 1983 by
• WHO classification 2017: polymorphous adenocarcinoma (low grade removed).
Histogenesis: Ductal cells.
Clinical features
Age • 6th-8th decade
Sex • ♀>♂.
• major SG (extra-oral) → parotid.
Site
• major SG (intra-oral)→ palate >buccal > upper lip
• slowly growing painless lesion.
S&S • Associated with bleeding & ulceration.
• Invade bone.
Gross pathology:
• uncapsulated , Firm, well circumscribed, lobulated nodule.
Histopathological features :
Cells are small cuboidal,+ large hyper chromtic nuclei + little cytoplasm
• CHARACTERIZED BY
1. morphologic diversity.
2. malignant cells has ovoid vesicular nuclei & lightly eosinophilic cytoplasm
3. cells has indefinite out line.
4. cells arranges in single file pattern (Indian file)
5. perineural invasion ( targetoid lesion) cells invade neurovascular bundles.
DDX : adenoid cystic ?!
TTT : wide surgical excision.
Prognosis: better prognosis than adenoid cystic carcinoma & less metastatic spread.
Dr Ahmed ElNashar 2023
Oral Pathology Made Easy ….!!! Salivary Gland Neoplasm
4. ACINIC CELL CARCINOMA
Incidence
• 6% of all salivary gland & 17% of malignant salivary gland.
• 2nd most common parotid malignancy
Histogenesis: (1) intercalated duct reserve cells. (2) terminal acinar intercalated duct unit.
Clinical features
Age • 5th- 6thdecade
Sex • ♀>♂.
• major SG (extra-oral) → parotid (bilateral).
Site
• major SG (intra-oral)→ palate >buccal.
S&S • 50% resembles benign/ SG.
Gross pathology:
• well circumscribed, homogenous , firm to soft, Solid Or Cystic, Grayish or reddish mass.
Histopathological features:
• well circumscribed tumor
• CHARACTERIZED by proliferation of serous acinar cell in 4 different pattern
1) CELLs : plyhydral cells with abundant basophilic cytoplasm & round darkly stained eccentric nuclei
2) PATTERNs : solid OR microcystic OR papillary cystic OR follicular pattern
solid & mictocystic pattern most commn
Prognosis: better prognosis than adenoid cystic carcinoma.
5. malignancy In Mixed tumors
= Malignancy in pleomorphic adenoma
• malignant transformation of epithelial component of a preexist benign
pleomorphic adenoma.
• Incidence:
▪ 2-4 % of all salivary gland.
▪ Parotid > submandibular > palate.
▪ (1.5 % in 1st 5 year) (9.5 % after 15 years).
Carcinoma ex
pleomorphic adenoma • C/F:
▪ 6th – 8th decade
▪ Longstanding painless mass undergoes ….
▪ sudden enlargement + neural manifestation + changes in color + fixation + ulceration
• H/P:
▪ Pleomorphic adenoma that is show….
▪ Infiltration + cancer malignant cells + hemorrhage + necrosis
• Malignant transformation of epithelial (carcinomatous) & mesenchymal
component (sarcomatous) of gland.
• Incidence:
▪ Rare (>0.5 of all salivary gland)
▪ Parotid > submandibular > palate.
▪ (1.5 % in 1st 5 year) (9.5 % after 15 years).
• C/F:
Carcino-sarcoma ▪ 6thdecade. ♀=♂.
▪ History of : recurrence or previous excision of pleomorphic adenoma
▪ Longstanding painless mass undergoes ….
▪ sudden enlargement + neural manifestation + changes in color + fixation + ulceration
• H/P:
▪ Pleomorphic adenoma that is show, biphasic apperance….
▪ Carcinomatous component (moderate or poorly diffrentiatted ductal epith)
▪ Sarcomatous component (chondrosarcoma)
• Histologically tumor are identical to benign pleomorphic (mixed) tumor.
Metastasizing mixed
• Although this benign appearance , lesion metastasize to 2ry sites.
tumors
• Tumor in 2ry site (metastatic tumor) also has the benign microscopic appearance.
Dr Ahmed ElNashar 2023
Oral Pathology Made Easy ….!!! Salivary Gland Neoplasm
6. BASAL CELL ADENO-CARCINOMA
7.EPITHELIAL-MYOEPITHELAIL CARCINOMA
Def يا دوب ال، كده يعين انت مش مهم بالنسبة ليك قوي اخر اتنني دول: قالت ف اخر الفيديو، استاذتنا دكتورة اميان الشامي
Dr Ahmed ElNashar 2023
You might also like
- Oral Neoplasma IDocument31 pagesOral Neoplasma INandika 'ndek' DewaraNo ratings yet
- Sebaceous Cyst, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandSebaceous Cyst, A Simple Guide To The Condition, Treatment And Related ConditionsRating: 5 out of 5 stars5/5 (1)
- Salivary Gland TumorDocument67 pagesSalivary Gland TumorMeri NovitaNo ratings yet
- Lecture, 9Document38 pagesLecture, 9محمد ربيعيNo ratings yet
- Oral Cavity & OesophagousDocument44 pagesOral Cavity & OesophagousrashmiNo ratings yet
- Benign Salivary Gland Tumors - Dr. Nermine El Bahey (2019-2020)Document13 pagesBenign Salivary Gland Tumors - Dr. Nermine El Bahey (2019-2020)MOHAMED AMINNo ratings yet
- Head and Neck LesionsDocument131 pagesHead and Neck Lesionslunaghilvin2026No ratings yet
- Skull Base Tumors NBNDocument30 pagesSkull Base Tumors NBNAbdullah Yeamin PeyalNo ratings yet
- Spindle Cell TumorsDocument138 pagesSpindle Cell TumorsMadhura ShekatkarNo ratings yet
- ORALDocument97 pagesORALMuhammadWathoniIkhlasNo ratings yet
- Malignant Tumors of Oral CavityDocument144 pagesMalignant Tumors of Oral CavitySivakumar LakshminarayananNo ratings yet
- k5 Patologi PencernaanDocument80 pagesk5 Patologi PencernaanKresna Denta ElygioNo ratings yet
- Nasal TumorDocument20 pagesNasal TumorMahmoud ElsherbenyNo ratings yet
- Epithelial Tumours - SreejaDocument184 pagesEpithelial Tumours - SreejaaakiNo ratings yet
- Cervical CaDocument43 pagesCervical Caraul sinatoNo ratings yet
- Submitted TO: Shivani Ma'am: Submitted By: Deeksha Thakur BSC 2 YearDocument20 pagesSubmitted TO: Shivani Ma'am: Submitted By: Deeksha Thakur BSC 2 YearPrajjwal PalNo ratings yet
- Morning case: CH. Nguyễn Xuân PhongDocument47 pagesMorning case: CH. Nguyễn Xuân PhongQuynh TranNo ratings yet
- Chapter 16 - Head and NeckDocument8 pagesChapter 16 - Head and NeckAgnieszka WisniewskaNo ratings yet
- Surgical OncologyDocument33 pagesSurgical Oncology4s6gw4xvntNo ratings yet
- Salivary Glands TumoursDocument102 pagesSalivary Glands TumoursSokna SyNo ratings yet
- Ovarian TumoursDocument24 pagesOvarian TumoursBinta BaptisteNo ratings yet
- Lecture 3 Ovarian PathologiesDocument5 pagesLecture 3 Ovarian Pathologiesslmsmn101No ratings yet
- Dermoid CystDocument18 pagesDermoid CystNaila0% (1)
- Skin Tumors: .Benign Tumors .Precancerous TumorsDocument38 pagesSkin Tumors: .Benign Tumors .Precancerous TumorsanandafirstyNo ratings yet
- LECTURE 22 Ovarian LesionsDocument57 pagesLECTURE 22 Ovarian LesionsLogadarshini VeerasamyNo ratings yet
- Salivary NeoplasmDocument29 pagesSalivary Neoplasm李丞永No ratings yet
- Malignant Tumors FESSHDocument40 pagesMalignant Tumors FESSHProfesseur Christian DumontierNo ratings yet
- NMIBC DX and Management PDFDocument104 pagesNMIBC DX and Management PDFOlteanu Dragos-NicolaeNo ratings yet
- Kuliah Kelainan KulitDocument47 pagesKuliah Kelainan KulitdinahzrNo ratings yet
- Colonic Polyps and Polyposis SyndromesDocument30 pagesColonic Polyps and Polyposis SyndromesIndhumathiNo ratings yet
- Patologi Anatomi Kelainan MuskuloskeletalDocument38 pagesPatologi Anatomi Kelainan Muskuloskeletalmuthia saniNo ratings yet
- Salivary Gland TumoursDocument131 pagesSalivary Gland TumoursSushmithaNo ratings yet
- Benign Non-Odontogenic Tumors of Oral CavityDocument64 pagesBenign Non-Odontogenic Tumors of Oral CavityvannaputriwNo ratings yet
- Neoplasia Patho - 1Document53 pagesNeoplasia Patho - 1Alishba MushtaqNo ratings yet
- Tumor Ganas Mata: Alfa SylvestrisDocument53 pagesTumor Ganas Mata: Alfa SylvestrisAzilu FalaNo ratings yet
- 19 Soft Tissue Tumors by DR NazishDocument55 pages19 Soft Tissue Tumors by DR NazishAhmed YTNo ratings yet
- 3 - Imaging Hand Tumours FESSHDocument37 pages3 - Imaging Hand Tumours FESSHProfesseur Christian DumontierNo ratings yet
- Oral TumorsDocument69 pagesOral TumorsOlga SolomonNo ratings yet
- YeeerDocument91 pagesYeeerbilljohn.bueno.crsNo ratings yet
- Examination of Lumps and BumpsDocument47 pagesExamination of Lumps and Bumpszoya shaikhNo ratings yet
- Patho PracticalsDocument27 pagesPatho Practicalsroyce charlieNo ratings yet
- Learning Unit 8 - Neoplasia of The Female Genital Tract - Part2Document36 pagesLearning Unit 8 - Neoplasia of The Female Genital Tract - Part2Marelize ErasmusNo ratings yet
- SECTION 6: Spleen: and OverviewDocument38 pagesSECTION 6: Spleen: and Overviewtudoranluciana1No ratings yet
- (Basic Surg A) Oncology-Dr. Acuna (Sleepy Crammers)Document3 pages(Basic Surg A) Oncology-Dr. Acuna (Sleepy Crammers)Mildred DagaleaNo ratings yet
- Oculars TumorDocument109 pagesOculars TumorNovita EmyNo ratings yet
- Blok Spesial Sense NewDocument34 pagesBlok Spesial Sense NewYola SurbaktiNo ratings yet
- Tumors of Salivary GlandDocument28 pagesTumors of Salivary Glandrameshparajuli14100% (1)
- Soft Tissue Tumor SeminarDocument39 pagesSoft Tissue Tumor SeminarAhmad SyahmiNo ratings yet
- Non Odontogenic Tumors: Dental ScienceDocument68 pagesNon Odontogenic Tumors: Dental ScienceRealdy PangestuNo ratings yet
- Breast CarcinomasDocument19 pagesBreast CarcinomasGirkati ShivaniNo ratings yet
- Lumps and Ulcer, Sebaceous Cyst, Lipoma, Dermoid CystDocument88 pagesLumps and Ulcer, Sebaceous Cyst, Lipoma, Dermoid CystAbdulsalam DostNo ratings yet
- Thediagnosisand Managementof Scrotalmasses: Jeffrey S. Montgomery,, David A. BloomDocument10 pagesThediagnosisand Managementof Scrotalmasses: Jeffrey S. Montgomery,, David A. BloomLyka MahrNo ratings yet
- Soft Tissue Tumors New Plan 1445Document32 pagesSoft Tissue Tumors New Plan 1445Asem AlhazmiNo ratings yet
- NeoplasiaDocument78 pagesNeoplasiageetikaNo ratings yet
- Silent But Deadly - How To Spot A Sarcoma: Craig Gerrand Consultant Orthopaedic Surgeon Freeman Hospital, NewcastleDocument31 pagesSilent But Deadly - How To Spot A Sarcoma: Craig Gerrand Consultant Orthopaedic Surgeon Freeman Hospital, NewcastleAfriade yolandaNo ratings yet
- Cancer 1 - 2022 - LectureDocument42 pagesCancer 1 - 2022 - LectureJoshua KaoNo ratings yet
- Lecture 7 NeolasiaI 16 416Document72 pagesLecture 7 NeolasiaI 16 416srishti soniNo ratings yet
- Ped Solid TumorDocument52 pagesPed Solid TumorIndranil GhoshNo ratings yet
- Bronchogenic CarcinomaDocument86 pagesBronchogenic CarcinomaAkshita Amit AgarwalNo ratings yet
- Reviewer in Health 6 PDFDocument2 pagesReviewer in Health 6 PDFmanilynNo ratings yet
- Integ 4 Answer PDFDocument12 pagesInteg 4 Answer PDFRhasdie MandiNo ratings yet
- Open Food RevolutionDocument71 pagesOpen Food RevolutionCarlos Chávez100% (1)
- Guide Olympus2009Document36 pagesGuide Olympus2009Carlos RamirezNo ratings yet
- New Client Intake FormDocument1 pageNew Client Intake FormTori BaileyNo ratings yet
- MycetomaDocument16 pagesMycetomapedrixon123No ratings yet
- PranayamDocument24 pagesPranayamkprabhublr100% (3)
- Colposcopy CourseDocument50 pagesColposcopy CourseNam Le100% (1)
- Evidence Table WorksheetDocument16 pagesEvidence Table Worksheetapi-282223043No ratings yet
- The Pros and Cons of Spaying A SheltieDocument15 pagesThe Pros and Cons of Spaying A SheltiepsykosomatikNo ratings yet
- Anorectal DiseaseDocument122 pagesAnorectal DiseasejolagusuNo ratings yet
- Antibacterial Activity of Passion Fruit (Passiflora SP.) Leaf ExtractsDocument23 pagesAntibacterial Activity of Passion Fruit (Passiflora SP.) Leaf ExtractsJaslynn PintoNo ratings yet
- Bleeding Disorder ApproachDocument9 pagesBleeding Disorder Approachmalik003No ratings yet
- Baile Bab 28Document45 pagesBaile Bab 28suciNo ratings yet
- MnemonicsDocument31 pagesMnemonicspickach100% (3)
- Trichomoniasis in Gram StainDocument3 pagesTrichomoniasis in Gram StainCliff Clarence HalimanNo ratings yet
- OD4141 Medical - Recreational Marijuana Growing Industry ReportDocument31 pagesOD4141 Medical - Recreational Marijuana Growing Industry ReportOozax OozaxNo ratings yet
- The Pioneering Work of William J. McCormick, M.D.Document4 pagesThe Pioneering Work of William J. McCormick, M.D.Βόρειο ΣέλαςNo ratings yet
- Aquifer Case 16Document4 pagesAquifer Case 16Dina KristevaNo ratings yet
- Diagnostic Tests For Low Back Disorders-Apr-2019Document14 pagesDiagnostic Tests For Low Back Disorders-Apr-2019cjlevanoNo ratings yet
- Male HypogonadismDocument11 pagesMale HypogonadismRendhy Wisnugroho SantosoNo ratings yet
- Inflammatory Bowel Disease (Ibd)Document28 pagesInflammatory Bowel Disease (Ibd)suhaNo ratings yet
- Case Report - CholesystitisDocument4 pagesCase Report - CholesystitisBenzoyl BeingNo ratings yet
- Undescended Testicles, Retractile Testicles, and Testicular TorsionDocument7 pagesUndescended Testicles, Retractile Testicles, and Testicular TorsionYudhistira SuryamanggalaNo ratings yet
- Sequence: Respiratory-Triggered Inversion Recovery-HASTE (IRHASTE) (31) Sequence With 4Document6 pagesSequence: Respiratory-Triggered Inversion Recovery-HASTE (IRHASTE) (31) Sequence With 4kingpintamNo ratings yet
- Grammer PDFDocument54 pagesGrammer PDFKhansa Rubab100% (1)
- Malignant Vs Traumatic Tongue Ulcer A Clinical AppDocument6 pagesMalignant Vs Traumatic Tongue Ulcer A Clinical Appvivi hutabaratNo ratings yet
- Excerpt: "Fat Chance" by Robert LustigDocument3 pagesExcerpt: "Fat Chance" by Robert Lustigwamu885067% (3)
- Introduction To Indoor Air QualityDocument23 pagesIntroduction To Indoor Air QualityRoshan Nanjundaiah100% (2)
- Material Safety Data Sheet: Effective Date 18.10.2010 According To EC Directive 2001/58/ECDocument7 pagesMaterial Safety Data Sheet: Effective Date 18.10.2010 According To EC Directive 2001/58/ECRey Regaspi TuyayNo ratings yet
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (403)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo ratings yet
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (80)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (23)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Gut: the new and revised Sunday Times bestsellerFrom EverandGut: the new and revised Sunday Times bestsellerRating: 4 out of 5 stars4/5 (392)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (5)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (3)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- 12 Rules for Life by Jordan B. Peterson - Book Summary: An Antidote to ChaosFrom Everand12 Rules for Life by Jordan B. Peterson - Book Summary: An Antidote to ChaosRating: 4.5 out of 5 stars4.5/5 (207)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- Algorithms to Live By: The Computer Science of Human DecisionsFrom EverandAlgorithms to Live By: The Computer Science of Human DecisionsRating: 4.5 out of 5 stars4.5/5 (722)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningFrom EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningRating: 4 out of 5 stars4/5 (3)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (1)
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsFrom EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsNo ratings yet
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)