100% found this document useful (3 votes)
1K views6 pagesAdvanced Trauma Life Support Protocols
The document outlines the Advanced Trauma Life Support (ATLS) protocol for managing a trauma patient brought by ambulance following a motor vehicle accident, including assessing the patient's airway, breathing, circulation, and identifying any life-threatening conditions like tension pneumothorax that require immediate intervention to stabilize the patient. The primary and secondary surveys are described to systematically evaluate the patient and identify injuries, with a focus on the ATOM FC conditions that could lead to rapid deterioration and require emergency procedures.
Uploaded by
syasyaCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PDF, TXT or read online on Scribd
100% found this document useful (3 votes)
1K views6 pagesAdvanced Trauma Life Support Protocols
The document outlines the Advanced Trauma Life Support (ATLS) protocol for managing a trauma patient brought by ambulance following a motor vehicle accident, including assessing the patient's airway, breathing, circulation, and identifying any life-threatening conditions like tension pneumothorax that require immediate intervention to stabilize the patient. The primary and secondary surveys are described to systematically evaluate the patient and identify injuries, with a focus on the ATOM FC conditions that could lead to rapid deterioration and require emergency procedures.
Uploaded by
syasyaCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PDF, TXT or read online on Scribd
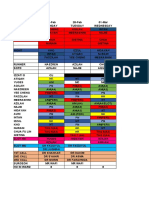
- Assessment and Management of ATLS: Covers the initial assessment of a trauma patient using personal protective equipment and airway management techniques.
- Chest Trauma - Management: Details the procedure for managing chest trauma, including needle thoracocentesis and chest tube insertion.
- Emergency Procedures and Management: Explores procedures involving thoracotomy indications and fluid management.
- ATOM FC Circulation and Disability: Details circulation and disability management according to the ATOM FC approach, including evaluation of vital signs.