Professional Documents
Culture Documents
Biochem Tables Ver 2
Biochem Tables Ver 2
Uploaded by
Sugar DC0 ratings0% found this document useful (0 votes)
4 views6 pagesBiochemistry Tables
Original Title
Biochem-Tables-Ver-2
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentBiochemistry Tables
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
4 views6 pagesBiochem Tables Ver 2
Biochem Tables Ver 2
Uploaded by
Sugar DCBiochemistry Tables
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 6
SUMMARY OF PATHWAYS INHIBITORS/POISONS OF THE ETC
PATHWAY LOCATION RATE-LIMITING C NAME OF COMPLEX INHIBITORS
ENZYME I NADH Dehydrogenase Rotenone, Amobarbital
Glycolysis Cytosol PFK-1 II Succinate
Malonate (competitive)
Cytosol Dehydrogenase
Gluconeo- Fructose-1,6-
(90% Liver, III Cytochrome
genesis Bisphosphatase Antimycin A, BAL
10% Kidneys) Reductase (btc1)
Cytosol Glycogen IV Cytochrome Oxidase Cyanide (CN),
Glycogenesis
(liver & muscle) Synthase (ata3) Carbon monoxide (CO)
Cytosol Glycogen V ATP Synthase Oligomycin (direct)
Glycogenolysis
(liver & muscle) Phosphorylase ➢ NOTE: If Complex IV is inhibited, it stops the
PPP/HMPS Cytosol G6PD upstream and stops the whole ETC
Mitochondria Isocitrate ➢ UNCOUPLING AGENTS/UNCOUPLERS
Kreb’s Cycle
(matrix) Dehydrogenase - Increase permeability of inner membranes to
Mitochondria protons → Proton gradient is lost → ATP synthesis
ETC
(membrane) stops but ETC continues and substrates are still
Cytosol oxidized → ↑↑ Heat production →
[Liver (major),
Hyperthermia/Hyperpyrexia
Lactating Acetyl-CoA
FA Synthesis - Examples:
mammary Carboxylase
gland, Adipose • Aspirin
(minor)] • 2,4-Dinitrophenol
Carnitine • Thermogenin – natural uncoupling proteins
Mitochondria
FA Oxidation Acyltransferase (found in brown fat)
(matrix)
(CAT I) - Previously used for weight loss
Cytosol HMG-CoA
Mevalonate
(smooth ER) Reductase
HMG-CoA GLYCOGEN STORAGE DISEASES (GSD)
Ketogenesis Mitochondria
Lyase
T DISEASE DEFICIENCY FINDINGS
Carbamoyl
Glycogen
Phosphate 0 Hypoglycemia
Urea Cycle Liver synthase
Synthetase I
Von Glucose-6-
(CPS I) 1 Hypoglycemia
Gierke’s Phosphatase
Lysosomal
Cardiomegaly,
2 Pompe’s α-glucosidase
METABOLIC EFFECTS OF INSULIN AND GLUCAGON Heart failure
(Acid maltase)
INSULIN GLUCAGON Debranching Hypoglycemia,
3 Cori’s
Timing Fed state Fasting state enzyme Hepatomegaly
Effect ↓ Blood sugar ↑ Blood sugar Branching Hypoglycemia,
4 Andersen’s
Energy is Stored Used enzyme Hepatomegaly
Glycolysis ↑ ↓ Muscle glycogen Muscle
5 McArdle’s
Gluconeogenesis ↓ ↑ phosphorylase weakness
Glycogenesis ↑ ↓ Hepatic glycogen
6 Her’s Hypoglycemia
Glycogenolysis ↓ ↑ phosphorylase
FA Synthesis ↑ ↓ Muscle
7 Tarui’s Muscle PFK-1
FA Oxidation ↓ ↑ weakness
➢ With GLUCAGON-Like Effects:
• Epinephrine
• Cortisol
• Somatotropin
APFZ / L-NU / BIOCHEM REVIEW NOTES / PLE 2021
VITAMINS AND DEFICIENCY STATES LYSOSOMAL STORAGE DISORDERS (LSD)
V OTHER NAMES DEFICIENCY STATES DISORDER STATE NOTES
Night Blindness Most
Gaucher
Retinoids, (nyctalopia), β-glucosidase common
A Disease
Anti-infective Vitamin Dry eyes LSD
(xerophthalmia) Fabry
α-galactosidase
Beri-beri, Disease
Thiamine, Wernicke-Korsakoff Krabbe
B1 β-galactosidase
Aneurine (observed in alcohol Disease
intoxication) Tay Sach’s
Hexosaminidase A
Cheilosis, Disease
B2 Riboflavin
Ariboflavinosis Sandhoff’s
Hexosaminidase A & B
Niacin, Disease
Niacinamide, Farber
Pellagra (PP means Ceramidase
B3 Nicotinic Acid, Disease
pellagra-preventing)
Nicotinamide, Niemann-Pick
PP Vitamin Sphingomyelinase
Disease
Burning Foot Accumu-
B5 Pantothenic Acid Metachromatic
Syndrome Arylsulfatase A lation of
Leukodystrophy
B6 Pyridoxine Peripheral neuropathy sulfatides
Biotin, ➢ Mucopolysaccharidoses (MPS) are also LSDs
B7 Vitamin H,
Coenzyme R
Folic Acid,
Spina bifida (neural
B9 Folacin,
tube defect)
Vitamin M
B12 Cyanocobalamin Megaloblastic anemia
Ascorbic Acid,
C Scurvy
Cevitamic Acid
Cholecalciferol, Rickets,
D
Antirachitic vitamin Osteomalacia
E Tocopherols
Essential FAs
F (Linoleic acid &
Linolenic acid)
Impaired blood
Phytonadione, clotting (bleeding),
K
Phylloquinone Hemorrhagic disease
of the newborn
Permeability Factors
P
(Rutin & Hesperidin)
Ubiquinone 10,
Q10 Ubidecanenone,
Coenzyme Q10
APFZ / L-NU / BIOCHEM REVIEW NOTES / PLE 2021
MUCOPOLYSACCHARIDOSES (MPS)
T DISEASE ENZYMES DEFICIENT NOTES
Hurler Syndrome Most severe MPS;
(1-H) Accumulation of dermatan and heparan sulfates
Scheie Syndrome Mildest MPS;
1 α-L-iduronidase
(1-S) Accumulation of dermatan sulfate
Hurler-Scheie Intermediate in severity between 1-H & 1-S;
Syndrome (1-H/S) Accumulation of dermatan sulfate
Only type of MPS inherited as an X-linked trait;
Accumulation of heparin sulfate may occur
2 Hunter Syndrome Iduronate 2-sulfatase
2A: Neuronopathic form (severe; early progressive)
2B: Non-neuronopathic form (mild; slowly progressive)
Accumulation of heparan sulfate may occur
3-A: Heparan N-sulfatase
Sanfilippo
3 (multiple, see notes) 3-B: α-N-acetylglucosaminidase
Syndrome
3-C: Heparan-α-glucosaminide N-acetyltransferase
3-D: N-acetylglucosamine 6-sulfatase
N-acetylgalactosamine 6-sulfatase
Accumulation of keratan and chondroitin sulfates
Morquio (4-A)
4
Syndrome Accumulation of keratan sulfate;
β-galactosidase (4-B)
Milder and fewer clinical features
5 Former designation for Scheie Syndrome (1-S)
Maroteaux-Lamy
6 N-acetylgalactosamine 4-sulfatase Accumulation of dermatan sulfate
Syndrome
Accumulation of dermatan, heparan and chondroitin
7 Sly Syndrome β-glucuronidase
sulfates
With clinical and biochemical features of Morquio and
DiFerrante Sanfilippo syndromes BUT NOT A VALID MEDICAL
8 Glucosamine 6-sulfate sulfatase
Syndrome DISORDER (enzyme was normal in a patient who was
misdiagnosed)
Natowicz
9 Hyaluronidase Extremely rare
Syndrome
CONNECTIVE TISSUE DISORDERS
DISORDER STATE NOTES
Joint or skin abnormalities (due to impaired integrity);
Ehlers-Danlos Syndrome ↓ Lysyl Hydroxylase Also involves something about α-collagen-1, pro-
collagen N-peptidase (not sure if synonym?)
Excessive spinal curvature
Kyphoscoliosis ↓ Lysyl Hydroxylase*
*NOTE: Not the only cause of kyphoscoliosis
Menkes Syndrome / Kinky hair; Growth retardation;
↓ Lysyl Oxidase
Kinky Hair Syndrome Lysyl oxidase requires Cu
Kindler’s Syndrome ↓ Anchoring Fibrils Severe blistering or scarring of skin
Damage of basement
Alport’s Syndrome Hematuria
membrane of glomerulus
Marfan Syndrome Gene mutation for Fibrillin-1 Long arms, CVS risk
Genetic Emphysema /
Alpha-1 Antitrypsin ↓ α-1 Antitrypsin Causes emphysema, lung disease, and panniculitis
Deficiency (AATD)
APFZ / L-NU / BIOCHEM REVIEW NOTES / PLE 2021
LIPOPROTEIN METABOLISM DISORDERS
T DISORDER SYNONYMS SUB-TYPES / EXAMPLES NOTES
/ STATE
HYPOLIPOPROTEINEMIAS
Usually, mutations in
Malabsorption; Hepatic
Familial Hypo- the APOB gene (apob31,
steatosis (fatty liver) which may
β-Lipoproteinemia apob39, apob40,
progress to cirrhosis in severe
(FHBL) apob46, apob87,
cases
apob89, or apob90)
Mutations in the MTTP
“Bassen-Kornzweig
gene
Syndrome”
Growth delay; Malabsorption;
A-β-Lipoproteinemia Permanently low levels Hepatomegaly; Neurological
“Microsomal
(ABL) (below the 5th and neuromuscular
Triglyceride Transfer
percentile) of manifestations
Protein (MTTP)
apolipoprotein B and
Deficiency”
LDL- cholesterol
“Anderson Syndrome” Severe fat malabsorption
Chylomicron Retention associated with failure to thrive;
Mutations in the SAR1B
Disease (CMRD) “Lipid Transport Defect Slow growth; Weight gain;
of Intestine” Chronic diarrhea; Steatorrhea
Hepatosplenomegaly;
Hyperplastic yellow-orange
tonsils; Lymph node
enlargement; Peripheral
neuropathy; Deposition of
“Tangier Disease (TGD)”
cholesteryl and retinyl esters
Mutations in the ABCA1 and carotenoids in nonadipose
“Cholesterol
Familial α-Lipoprotein (9q31) gene tissues
thesaurismosis”
Deficiency /
Familial HDL Deficiency Almost complete ATP-binding cassette
“Defective ATP-binding
absence of plasma HDL transporter (ABC1) – a
Cassette Transporter A1
cholesterol efflux regulatory
(ABCA1)”
protein that is able to orient
cellular cholesterol towards the
cell surface and to facilitate its
transfer towards the core of
HDL
HYPERLIPOPROTEINEMIAS
Mutations in the LPL
and apolipoprotein
“Familial Lipoprotein
(apo) C-II genes
Lipase (LPL) Deficiency” Abdominal pain; Pancreatitis;
Familial Hyper-
1 Eruptive xanthomas;
chylomicronemia Criteria:
“Burger-Grutz Hepatosplenomegaly
Chylomicrons present,
Syndrome”
Normal or slightly ↑
VLDL (pre-β)
APFZ / L-NU / BIOCHEM REVIEW NOTES / PLE 2021
One of the most common
genetic diseases (affects approx.
1 in 250 individuals);
Presence of pathogenic Xanthomas (tendon xanthomas
variant in any of the usually indicate this type;
LDLR, APOB, and PCSK9 tuberous xanthoma; planar
genes (other related xanthoma in homozygotes);
genes include APOA2, Xanthelasma (more frequent in
Familial Hyper- GHR, EPHX2) this type);
“Low-density
β-Lipoproteinemia / Arcus corneae (arcus senilis)
2 Lipoprotein Receptor
Familial Hyper- General Criteria: before the age of 40 yrs. usually
(LDLR) Disorder”
cholesterolemia ↑ LDL (β) implies this type
2 Types: Heterozygous
Type IIa: (common) and Homozygous
Normal VLDL (pre-β) (rare);
Type IIb: Tx: Statins
↑ VLDL (pre-β) Non-statin Tx: Ezetimibe,
Bempedoic acid, PCSK9
inhibitors (e.g. Alirocumab,
Evolocumab)
“Floating β or Broad β
Disease” Mutations in the APOE
Xanthomas [xanthoma striata
gene
palmaris (planar xanthoma in
“Remnant Removal
the palms of the hands) is
Disease” Criterion: Presence of
Familial Dys- specific to this disease; tuberous
3 VLDL having abnormally
β-Lipoproteinemia xanthoma; tuberoeruptive
“Apolipoprotein E high cholesterol content
xanthoma];
(APOE) Deficiency” and abnormal
Xanthelasma (sometimes)
electrophoretic mobility
“Carbohydrate-induced (floating β or β-VLDL)
hyperlipemia”
Mutations in the APOA5
“Endogenous gene
Familial Hyper-
hyperlipemia”
pre-β-Lipoproteinemia /
4 Criteria: Tuberoeruptive xanthoma
Familial Hyper-
“Carbohydrate-inducible ↑ VLDL (pre-β),
triglyceridemia
hyperlipemia” No ↑ in LDL (β),
Chylomicrons absent
“Late-onset hyper- Mutations in the APOA5
Combined
chylomicronemia” gene
Hyperlipidemias /
Abdominal pain; Pancreatitis;
5 Hyperpre-β-
“Combined fat and Criteria: Eruptive xanthomas
Lipoproteinemia &
carbohydrate-induced Chylomicrons present,
Chylomicronemia
hyperlipemia” ↑ VLDL
➢ Bempedoic Acid (ETC-1002)
- Prodrug; Requires activation to its active metabolite, ESP15228, by Very Long-chain Acyl-CoA Synthetase I
(ACSLV1), an enzyme present in the liver and not in the skeletal muscle (thus, ↓ muscle-related A/E)
- MOA: Inhibits ATP-Citrate Lyase (ACL) → ↓ Conversion of mitochondrial-derived citrate to cytosolic ACL → Less
substrate for cholesterol and FA synthesis
APFZ / L-NU / BIOCHEM REVIEW NOTES / PLE 2021
AMINO ACID METABOLISM DISORDERS
DISORDER ENZYME DEFICIENT NOTES
Maple Syrup Urine Branched Chain Keto-acid Viscous, burnt sugar odor of urine; Mental retardation; Death
Disease (MSUD) Dehydrogenase Tx: Diet free of BCAAs (Val, Ile, Leu)
Musty odor of urine; Fair-skinned; Mental retardation
Phenylketonuria
Phenylalanine Hydroxylase Tx: Diet free of Phe, rich in Tyr
(PKU)
C/I: Aspartame
Alkaptonuria Homogentisic Acid Oxidase Dark urine coloration
Albinism Melanocyte Tyrosinase
Cystathionine Synthase or Cystathionine synthase requires B6
Homocystinuria
Methionine Synthase Methionine synthase requires B9 & B12
Any enzyme in the
Hyperammonemia ↑ NH3 = Nausea, vomiting, confusion, coma, death
Urea Cycle
NUCLEIC ACID METABOLISM DISORDERS
DISORDER STATE NOTES
Self-mutilation; Cognitive defects; HYPERuricemia
↓ Hypoxanthine Guanine
HGPRT converts Hypoxanthine to Inosine monophosphate
Lesch-Nyhan Syndrome Phosphoribosyl Transferase
(when deficient, hypoxanthine is instead converted to uric
(HGPRT)
acid by xanthine oxidase)
Severe Combined
↓ Adenosine Deaminase Immune dysfunctions
Immunodeficiency
Folates play an important role in the synthesis of DNA
Neural Tube Defects ↓ Folate derivatives
precursors in early pregnancy
Gout ↑ Urates
OTHER METABOLIC DISORDERS
DISORDER STATE NOTES
Refsum’s Disease /
↓ Phytanoyl-CoA Retinitis pigmentosa; Cerebellar ataxia; Anosmia;
Classic or Adult Refsum’s Disease /
Hydroxylase (PHYH) Ichthyosis; Deafness
Phytanic Acid Oxidase Deficiency
SOURCES: Manor Notes, MedlinePlus, NORD, Trease & Evans (16th ed.), NIH, AHA
APFZ / L-NU / BIOCHEM REVIEW NOTES / PLE 2021
You might also like
- Biochem SuperTableDocument2 pagesBiochem SuperTablePrincess MarielleNo ratings yet
- Internal Medicine Ple ReviewerDocument7 pagesInternal Medicine Ple ReviewerReinhard Ivan MansibangNo ratings yet
- Biochem SuperTable PDFDocument2 pagesBiochem SuperTable PDFPrincess MarielleNo ratings yet
- Hi-Yield Notes in Im & PediaDocument20 pagesHi-Yield Notes in Im & PediaJohn Christopher LucesNo ratings yet
- Anatomy Supertable PDFDocument14 pagesAnatomy Supertable PDFAlex Ondevilla100% (1)
- Rate Limiting Step PDFDocument1 pageRate Limiting Step PDFCoy NuñezNo ratings yet
- Pharmacology Table - GonzalesDocument14 pagesPharmacology Table - GonzalesMark Angelo PonferradoNo ratings yet
- Pathology PRC FinaleditDocument11 pagesPathology PRC FinaleditVince Cabahug100% (1)
- TOPNOTCH DIGITAL HANDOUT - BIOCHEMISTRY Juan Dela CruzDocument2 pagesTOPNOTCH DIGITAL HANDOUT - BIOCHEMISTRY Juan Dela CruzJoy Fucanan100% (1)
- #ROADTOPLE An Almost Complete Guide To The... - Chloramphenicole - MD - Facebook PDFDocument10 pages#ROADTOPLE An Almost Complete Guide To The... - Chloramphenicole - MD - Facebook PDFJoy FucananNo ratings yet
- 4 Physiology Supplement Handout Based On Ganong For TOPNOTCH 21 by Jaffar PinedaDocument46 pages4 Physiology Supplement Handout Based On Ganong For TOPNOTCH 21 by Jaffar PinedaAthena Borja100% (3)
- 4 - Physiology Main Handout Oct 2023Document99 pages4 - Physiology Main Handout Oct 2023Trisha Anne WacasNo ratings yet
- Anatomy Supertable With Pics PDFDocument39 pagesAnatomy Supertable With Pics PDFCla NuvalNo ratings yet
- September 2021 PleDocument20 pagesSeptember 2021 PleGian PagadduNo ratings yet
- 1 Topnotch Biochemistry SuperExam1 PDFDocument92 pages1 Topnotch Biochemistry SuperExam1 PDFSheinna BarcelonaNo ratings yet
- Junior Intern Review - Oral Revalida 2016Document170 pagesJunior Intern Review - Oral Revalida 2016Cyrus ZalameaNo ratings yet
- MetabolismDocument1 pageMetabolismClaudius AlexiusNo ratings yet
- Final Coaching - Obgyne 2022Document7 pagesFinal Coaching - Obgyne 2022Jhon PauloNo ratings yet
- Final Coaching - Biochem 2022Document6 pagesFinal Coaching - Biochem 2022Jhon Paulo100% (1)
- Clerkship EssentialsDocument14 pagesClerkship EssentialsKirstie de Luna100% (2)
- Surgery Ple ReviewerDocument5 pagesSurgery Ple ReviewerReinhard Ivan MansibangNo ratings yet
- (Fold/Cover If You Don'T Wanna See The Answers Yet) BDocument43 pages(Fold/Cover If You Don'T Wanna See The Answers Yet) BManila Med100% (2)
- 12 Health Healing FoodsDocument10 pages12 Health Healing FoodsBahukhandiNo ratings yet
- 03 Biochemistry PLE 2019 RatioDocument72 pages03 Biochemistry PLE 2019 RatioMae SimborioNo ratings yet
- Tips Sa Boards TextsDocument3 pagesTips Sa Boards Textshallegail100% (1)
- Final Coaching - Patho 2022Document6 pagesFinal Coaching - Patho 2022Jhon PauloNo ratings yet
- Cebu Doctors BiochemistryDocument9 pagesCebu Doctors BiochemistryVince Cabahug100% (1)
- Final Coaching - Im 2022Document9 pagesFinal Coaching - Im 2022Jhon PauloNo ratings yet
- Compilation Day 1 BIOCHEM - Topnotch Handout + USMLEDocument9 pagesCompilation Day 1 BIOCHEM - Topnotch Handout + USMLEClyde Yuchengco Cu-unjieng100% (2)
- Suggested Review MaterialsDocument1 pageSuggested Review MaterialsJoher MendezNo ratings yet
- Board Exam Review Pearls (Physician)Document6 pagesBoard Exam Review Pearls (Physician)Jo Anne100% (2)
- Blueprint For Questions Pharmacology and Therapeutics Subject Matter Question No. Recall Applica Tion Compre HensionDocument12 pagesBlueprint For Questions Pharmacology and Therapeutics Subject Matter Question No. Recall Applica Tion Compre HensionJohn Christopher LucesNo ratings yet
- Topnotch Mnemonics - September 2018Document8 pagesTopnotch Mnemonics - September 2018Nicole BaysaNo ratings yet
- Topnotch Microbiology Supertable - by DR - Cocoy Calderon, Jaffar Pineda, Troy SoberanoDocument3 pagesTopnotch Microbiology Supertable - by DR - Cocoy Calderon, Jaffar Pineda, Troy SoberanoJohn Christopher Luces100% (1)
- Board Recall Must ReadDocument8 pagesBoard Recall Must ReadSarahSalvanNo ratings yet
- Physician Licensure Exam March 2019 Recall: MicrobiologyDocument4 pagesPhysician Licensure Exam March 2019 Recall: MicrobiologyNica Lopez FernandezNo ratings yet
- Mcu-Fdt Medical Foundation College of Medicine Department of BiochemistryDocument12 pagesMcu-Fdt Medical Foundation College of Medicine Department of BiochemistryKaye bagasin100% (1)
- September 2019 Boards TipsDocument3 pagesSeptember 2019 Boards TipspaoloobiasNo ratings yet
- USMLE - BRS Pathology - Flash CardsDocument37 pagesUSMLE - BRS Pathology - Flash CardsJake ChuengNo ratings yet
- MBR 2019 - Physiology Handouts PDFDocument121 pagesMBR 2019 - Physiology Handouts PDFKenneth T. NuñezNo ratings yet
- Philippine Pediatric Society, IncDocument19 pagesPhilippine Pediatric Society, IncAsmphLibrary OrtigasNo ratings yet
- Boards TipsDocument2 pagesBoards TipsElaine June FielNo ratings yet
- Most CommonsDocument6 pagesMost CommonsBobet ReñaNo ratings yet
- Biokem PRC QuestionsDocument13 pagesBiokem PRC Questionsyanafk33% (3)
- NUTR LS1020 Fall Comprehensive Case Study-LeoJuneDocument8 pagesNUTR LS1020 Fall Comprehensive Case Study-LeoJuneCollin Hiett0% (8)
- PresentationDocument69 pagesPresentationsyamsulmaarifNo ratings yet
- Pre-Board Examination in Clinical Chemistry (Part 2)Document4 pagesPre-Board Examination in Clinical Chemistry (Part 2)Godofredo Hermosura100% (1)
- AnaPLEDocument20 pagesAnaPLEMc EstanislaoNo ratings yet
- For The Boards Summary of Metabolic Pathways BiochemDocument4 pagesFor The Boards Summary of Metabolic Pathways BiochemJaybee SarmientoNo ratings yet
- Therapeutic ExerciseDocument47 pagesTherapeutic ExercisedicksonNo ratings yet
- Feb 2015 Physician Licensure ExamDocument1 pageFeb 2015 Physician Licensure ExamyanafkNo ratings yet
- Republic of The Philippines Professional Regulation Commission ManilaDocument3 pagesRepublic of The Philippines Professional Regulation Commission ManilaTheSummitExpressNo ratings yet
- 6 - Topnotch Pharma Supertable UPDATED APRIL 2017 by Yns PereyraDocument170 pages6 - Topnotch Pharma Supertable UPDATED APRIL 2017 by Yns PereyraVien CervantesNo ratings yet
- Notes For Pedia HandoutDocument2 pagesNotes For Pedia HandoutAiszel Angeli Pepito Ligo100% (2)
- Pocket-Pedia PDFDocument9 pagesPocket-Pedia PDFKatrin Miñas MendozaNo ratings yet
- March 2022 Hybrid Full Course OFFICIAL Lecture Schedule - NOV-DEC UPLOADDocument3 pagesMarch 2022 Hybrid Full Course OFFICIAL Lecture Schedule - NOV-DEC UPLOADJhon PauloNo ratings yet
- Philippine Physician Licensure Examination (Ple) : A Primer For Serviam by Exequiel Dimaano, MD WVSU COM Class 2013Document43 pagesPhilippine Physician Licensure Examination (Ple) : A Primer For Serviam by Exequiel Dimaano, MD WVSU COM Class 2013Choi SpeaksNo ratings yet
- Biochemistry - 230204 - 191022Document41 pagesBiochemistry - 230204 - 191022DRJS 74No ratings yet
- Biochemistry RR PROMO.Document68 pagesBiochemistry RR PROMO.KUTLUHAN YILMAZ Prof DrNo ratings yet
- Physio Correl - Insulin and GlucagonDocument33 pagesPhysio Correl - Insulin and GlucagonDan Tristam MicabaloNo ratings yet
- A 59-Year-Old Man With A History of Diabetes and Alcohol Abuse Is Brought To The Emergency Room in A Semiconscious and Minimally Responsive StateDocument43 pagesA 59-Year-Old Man With A History of Diabetes and Alcohol Abuse Is Brought To The Emergency Room in A Semiconscious and Minimally Responsive StateAnonymous eDD0YqzPMNo ratings yet
- Curs 1 2015 DZDocument44 pagesCurs 1 2015 DZIoana DiaconuNo ratings yet
- DM Type 2 Pa Tho PhysiologyDocument4 pagesDM Type 2 Pa Tho PhysiologyEllen Grace Cañarejo BaroyNo ratings yet
- Inborn Errors of Carbohydrate Metabolism and KetonesDocument11 pagesInborn Errors of Carbohydrate Metabolism and Ketoneslianefheldelrosario20No ratings yet
- GluconeogenesisDocument21 pagesGluconeogenesisNoor Al Huda MohammedNo ratings yet
- Pharmacological and Therapeutic Effects of Jasminum Sambac - A ReviewDocument13 pagesPharmacological and Therapeutic Effects of Jasminum Sambac - A ReviewBaru Chandrasekhar RaoNo ratings yet
- The Heart of The MatterDocument3 pagesThe Heart of The Mattercklcat1437No ratings yet
- A Bornstein, MD, FACC Assistant Professor of Public Health Weill Cornell Medical CollegeDocument50 pagesA Bornstein, MD, FACC Assistant Professor of Public Health Weill Cornell Medical CollegeSyed ImranNo ratings yet
- Phytochemical and Pharmacological Review of Gymnema SylvestreDocument8 pagesPhytochemical and Pharmacological Review of Gymnema SylvestreInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Lehninger Principles of Biochemistry, Fourth Edition - David L. Nelson, Michael M. Cox (0354-0377) (13-24)Document12 pagesLehninger Principles of Biochemistry, Fourth Edition - David L. Nelson, Michael M. Cox (0354-0377) (13-24)Nur AuliaNo ratings yet
- FEM 3202-3 LipidDocument15 pagesFEM 3202-3 LipidRon ChongNo ratings yet
- What Are The Benefits of GarlicDocument7 pagesWhat Are The Benefits of GarlicBellia AyudiaNo ratings yet
- Assignment 3.1 - LipidsDocument4 pagesAssignment 3.1 - LipidsJameseu KimNo ratings yet
- Lipid Metabolism: Hirowati AliDocument39 pagesLipid Metabolism: Hirowati Alinajdah fakhirahNo ratings yet
- Anredera Cordifolia Leaves Extract As Antihyperlipidemia and Endothelial Fat Content Reducer in Male Wistar RatDocument5 pagesAnredera Cordifolia Leaves Extract As Antihyperlipidemia and Endothelial Fat Content Reducer in Male Wistar RatRigotti BrNo ratings yet
- 18.4 Chemical Properties of Fats and Oils: 1. HydrolysisDocument14 pages18.4 Chemical Properties of Fats and Oils: 1. HydrolysisHanif KadekarNo ratings yet
- Toc PDFDocument12 pagesToc PDFSOURAV DAS100% (1)
- 13 Ways To Treat Hypothyroidism NaturallyDocument14 pages13 Ways To Treat Hypothyroidism NaturallyZelina KesavathparambilNo ratings yet
- Mi41021 - Chol - Liq - 2017Document4 pagesMi41021 - Chol - Liq - 2017Dafne Manrique JerezNo ratings yet
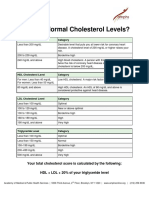
- Cholesterol Handout - ENGLDocument2 pagesCholesterol Handout - ENGLOladipupo Adejumobi LawalNo ratings yet
- Himanshu Healthians.Document7 pagesHimanshu Healthians.Himanshu GarkhelNo ratings yet
- Lipoprotein DisordersDocument9 pagesLipoprotein DisordersSourav MondalNo ratings yet
- BylawsDocument136 pagesBylawsdannyfiguracion45No ratings yet
- Crestor®: Rosuvastatin 5 MG, 10 MG, 20 MG or 40 MG TabletsDocument6 pagesCrestor®: Rosuvastatin 5 MG, 10 MG, 20 MG or 40 MG Tabletsnasir uddinNo ratings yet
- NSG 210 Study GuideDocument25 pagesNSG 210 Study GuideyasserNo ratings yet
- LIPIDS QUIZ - Google FormsDocument25 pagesLIPIDS QUIZ - Google FormsJOHN MIKE RAMIREZNo ratings yet
- T33 - Long Term Complications of Diabetes - PTPDocument7 pagesT33 - Long Term Complications of Diabetes - PTPangela adelantarNo ratings yet
- Colostrum-LD AntiAging BenefitsDocument6 pagesColostrum-LD AntiAging BenefitsAntonio CarneiroNo ratings yet
- Randomized Controlled Trial of Early Versus Delayed Statin Therapy in Patients With Acute Ischemic StrokeDocument7 pagesRandomized Controlled Trial of Early Versus Delayed Statin Therapy in Patients With Acute Ischemic StrokeShelin ClarissaNo ratings yet
- Health Impacts of Yoga and PranayamaDocument15 pagesHealth Impacts of Yoga and PranayamaCraig Van HeerdenNo ratings yet