Professional Documents
Culture Documents
Impulse Generation and Conduction
Uploaded by
Zacharia muraciaOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Impulse Generation and Conduction
Uploaded by
Zacharia muraciaCopyright:
Available Formats
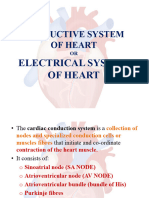
Impulse Generation
• The heart is composed of three
types of muscles
SANode
• Atria & ventricles
AVNode
• Form the working myocardium
• They do the mechanical work of
Bundle
of His pumping
Purkinje
fibers
13-Jun-23 Physiology of the heart 2
Impulse Generation
• The specialized tissues
• Excitatory & conducting tissues
SANode
• Sino atrial node
• Atrio-ventricular node
AVNode • Bundle of his
Bundle
• Purkinje fibers
of His
Purkinje
fibers
13-Jun-23 Physiology of the heart 3
Depolarization and Impulse Conduction
• Heart is autorhythmic
• Depolarization begins in sinoatrial (SA) node
• Spread through atrial myocardium
• Delay in atrioventricular (AV) node
13-Jun-23 Physiology of the heart 4
13-Jun-23 Physiology of the heart 6
SINO ATRIAL NODE
• Small ,flattened , ellipsoid strip of specialized cardiac muscle
• Located in the superior posterolateral wall of the right atrium
immediately below the opening of the vena cava
• Automatic electrical rhythmicity of sinus fibers is caused by self-
excitation
13-Jun-23 Physiology of the heart 7
Sinoatrial node(SA node)
• It is located in the right atrium, near the
entrance of the superior vena cava.
• It acts as the heart’s natural pacemaker, i.e.
initiates heart beat and the heart rate with
help from autonomic NS.
• The SA node is a muscle in itself consisting
of cells which are involved in contraction of
the heart muscle.
• For a muscle to contract, its cells have to
first depolarize, that is, move from being
negatively charged to being positively
charged. The same has to happen for the SA
node.
• The SA node is able to depolarize on its
own without the help of other cells, which is
referred to as automaticity.
• The SA node is connected to the
neighboring heart muscle cells through gap
junctions, which allow for transmission of
signals from the SA node to the muscle
cells.
• When the SA node depolarizes, it spreads a
wave of depolarization throughout the atrial
muscle cells.
MECHANISM OF SINUS NODAL RHYTHMICITY
• Resting membrane potential of sinus nodal fiber is between -55 to -60
millivolts
• The cause of this less negativity is due to the leakiness of cell
membranes of sinus fibres to sodium and calcium ions .This therefore
neutralizes some of the intracellular negativity
13-Jun-23 Physiology of the heart 11
THE HEART
13-Jun-23 Physiology of the heart 12
INTERNODAL AND INTERATRIAL PATHWAYS
The end of sinus fibers connects to atrial muscle fibers
Therefore, action potential originating in the sinus
node travels into atrial muscle fibers
Action potential therefore spreads through the entire
muscle and eventually to the atrial-ventricular node
There are four bands for conduction;
i. Anterior interatrial band; passes through the
anterior walls of the right atrium to the left atrium
ii. Anterior ,middle , posterior bands; passes
respectively through the atrial wall and terminates to
atrial-ventricular nodes
13-Jun-23 Physiology of the heart 13
13-Jun-23 Physiology of the heart 14
The AV Node
• Its located in the interatrial septum near the atrioventricular valve.
• It serves as an electrical gateway to the ventricles.
• It receives signals from the SA node, and delays their transmission to
the bundle of His for about 0.1 seconds.
• This ensures that the atria have ample time to completely contract and
empty all their contents into the ventricles, before the ventricles start
contracting.
13-Jun-23 Physiology of the heart 15
DELAYED IMPULSE CONDUCTION FROM THE ATRIA TO THE VENTRICLES
AT THE ATRIO-VENTRICULAR NODE
The delay is to allow time for the atria to empty their blood into the
ventricles before ventricular contraction begins
This delay is caused by Atrial-ventricular node and its adjacent conductive
fibers
The Atrial-ventricular node is located in the posterior wall of the right
atrium below the tricuspid valve
From the sinus through the inter-nodal pathways ,the impulse reaches the
Atrial-ventricular node after about 0.03 second
There is a delay of 0.09 second in the atrial-ventricular node itself before
the impulse enters the atrial-ventricular bundle where it passes into the
ventricles
13-Jun-23 Physiology of the heart 16
13-Jun-23 Physiology of the heart 17
The Bundle of His
• It is found spread out in the interventricular septum, down to the
apex of the heart.
• It is divided into the right and left branches which conduct impulses
from the AV node to the apex of the heart.
• These impulses are then transmitted to the Purkinje fibers.
13-Jun-23 Physiology of the heart 18
• Another delay of about 0.04 second occurs in this penetrating Atrial-
ventricular bundle
• Thus the total delay in the Atrial-ventricular nodal and Atrial-
ventricular bundle system is about 0.13 second
• This delay in addition to initial conduction of 0.03 second from the
sinus node makes 0.16 second before impulses reaches the ventricles
13-Jun-23 Physiology of the heart 19
• Cause of slow conduction; caused by diminished numbers of gap
junctions between successive cells in the conducting pathways
• So there is a great resistance to conduction of excitatory ions from
one conducting fiber to the next
13-Jun-23 Physiology of the heart 20
Rapid Transmission In The Ventricular Purkinje Fibers
• Purkinje fibers lead from A-V node to the A-V bundle into the ventricles
• They have functional characteristics opposite to those of A-V Nodal fibers;-they
are very large fibers
-they transmit A.P at a velocity of about 6 times that of ventricular
muscles and 150 times than in some of A-V Nodal fibers
• This velocity allows almost instantaneous transmission throughout the remainder
part of ventricular muscles
• The rapid transmission by Purkinje fibers is believed to be due to:
Very high level of permeability of the gap junctions at the intercalated discs
between successive cells that make up Purkinje fibers
Purkinje fibers have very few myofibrils which means that they contract little or
not at all during the course of impulse transmission
13-Jun-23 Physiology of the heart 21
One-Conduction through the A-V Bundle
• Special characteristic of A-V Bundle-inability of action potentials to
travel backwards from ventricles to the atria
• Presence of a continuous fibrous barriers acts as an insulator to
prevent passage of the cardiac impulse backwards
• Everywhere except the A-V Bundle , the atrial muscle is separated
from the ventricular muscle by this continuous fibrous barrier
13-Jun-23 Physiology of the heart 22
Distribution of the Purkinje Fibers In The Ventricles
• After penetrating the fibrous tissue between atrial and ventricular
muscle , the distal portion of the A-V bundle passes downwards in the
ventricular septum towards the apex of the heart
• The bundles divides into left and right bundle branches that lie
beneath the endocardium on the two respective sides of ventricular
septum
• Each branch spreads downwards towards the apex of ventricles
dividing into smaller branches
13-Jun-23 Physiology of the heart 23
• These branches in turn course sideways around each ventricular
chamber and back towards the base of the heart
• The total elapsed time averages only 0.03 seconds from the time the
cardiac impulse enters the bundle branches in the ventricular septum
until it reaches the termination of Purkinje fibers
13-Jun-23 Physiology of the heart 24
Transmission of cardiac impulse in the ventricular
muscle
• Once the impulse reaches end of Purkinje fibers it is transmitted
through the ventricular muscle mass by the ventricular muscle fibers
• The velocity is about 0.3-0.5m/sec
• The cardiac muscle wraps around the heart in a double spiral with
fibrous septum between spiraling layers
13-Jun-23 Physiology of the heart 25
• Cardiac impulse therefore angulates towards the surface along the
direction of the spirals
• This transmission requires about 0.003secs almost equal to time
required for transmission through the entire ventricular portion of
Purkinje system
13-Jun-23 Physiology of the heart 26
Control of excitation and conduction in the heart
• SAN is the normal pacemaker of the heart because it has a high
impulse velocity
• Some parts of the heart can also exhibit intrinsic rhythmical excitation
in the same way as the sinus e.g A-V Nodal and Purkinje fibers
• When not stimulated from outside source the A-V Node discharge at
40-60 times per minute and the Purkinje fibers discharge at 15-40
times per minute
• Since the sinus discharge rate is higher than both the A-V Node and
Purkinje fibers , its impulses are discharged to both before the self
excitation of either A-V Node or Purkinje fibers
13-Jun-23 Physiology of the heart 27
Abnormal or Ectopic pacemakers
• This is a pacemaker elsewhere than the SAN
• A-V Node or Purkinje fibers may abnormally have a higher discharge
than sinus node hence become the pacemaker. This causes;
• Abnormal sequence of contraction of different part of the heart
• Debility of the heart pumping
• Blockage of transmission of the cardiac impulse from SAN to other parts of
the heart
13-Jun-23 Physiology of the heart 28
• When A-V Bundles blocks Purkinje fibers continues as pacemaker
• After sudden A-V bundle block the Purkinje system does not begin to
emit its intrinsic rhythmical impulses until 5-20 secs later because
before blockage Purkinje fibers had been overdriven by the rapid SAN
impulses and consequently are in a suppressed state.
• During these secs the ventricles fail to pump blood and the person
faints after the first 4-5 secs because of lack of blood flow to the brain
• This delayed pick up of heartbeat is called STOKES-ADAMS
SYNDROME
13-Jun-23 Physiology of the heart 29
Role of the Purkinje system in causing synchronous
contractions of ventricular muscle
• The rapid conduction of Purkinje fibers permits the cardiac impulse
to all ventricles and arrives after 0.03sec and contracts for about
another 0.3sec
• Effective pumping by the ventricular chambers requires this
synchronous type of contraction
13-Jun-23 Physiology of the heart 30
Mechanism of sinus node rhythmicity
• Resting membrane potential of sinus nodal fiber is between -55 to -60
millivolts unlike that of ventricular and atrial muscle cells which is -
90millivolts.
• The cause of this less negativity is due to the leakiness of cell
membranes of sinus fibers to sodium and calcium ions .
• This therefore neutralizes some of the intracellular negativity (-90 in
other excitable tissues).
13-Jun-23 Physiology of the heart 31
• The cells in SAN cell membrane are naturally leaky to Na+.
• Na+ tend to leak into the cell and this is responsible for the initial
phase of pace maker potential.
• Transient (T) Ca++ channels open and there is entry of Ca++ which
completes the pre-potential phase.
• The long lasting (L) Ca++ channels then open with resultant influx of
more Ca++ resulting in rapid depolarization.
13-Jun-23 Physiology of the heart 32
• At the peak of each impulse, K+ ion channels open, there is rapid
efflux of K+ ions which brings about repolarization.
• The K+ channels then close and Na+ ions leak into the cell causing the
initial phase of pre-potential, then the transient Ca++ channels with
the process repeating itself.
13-Jun-23 Physiology of the heart 33
13-Jun-23 Physiology of the heart 34
Control of heart rhythmicity and impulse conduction by
cardiac nerves
Parasympathetic Simulation
• Stimulation of parasympathetic nerves to the heart causes
Acetylcholine release
• Hormone has two major effects;
• Decreases rate of rhythm of SAN
• Decreases excitability of A-V junctional fibers between atrial musculature and
A-V Node thereby slowing transmission of cardiac impulse into ventricles
13-Jun-23 Physiology of the heart 35
Ventricular Escape
• Strong stimulation of Vagi can stop completely excitation of sinus
node or block transmission of impulse from atria to ventricles through
A-V Node
• Ventricles may stop beating for 5-20 secs but the ventricular septal
portion of the A-V bundle develops a rhythm of its own and causes
ventricular contraction at a rate of 15-40 beats per minute
13-Jun-23 Physiology of the heart 36
Mechanism of vagal effect
• The acetylcholine release at the vagal nerve ending increases the
permeability of potassium out of the conductive fibers
• Causes hyperpolarization making tissue much less excitable
• At SAN it causes more negativity than the normal -65 to -75
13-Jun-23 Physiology of the heart 37
• Initial rise of sinus nodal membrane potential requires much longer
to reach threshold potential for excitation;
• Slows rate of rhythmicity of nodal fibers
NOTE : If Vagal stimulation is strong enough it can stop entirely
rhythmical excitation of this node
13-Jun-23 Physiology of the heart 38
CONT’D
• In A-V node hyperpolarization makes it difficult for small atrial fibers
to generate enough electricity to excite nodal fibers
• Hence decrease of safety factor for transmission of cardiac impulse
through the transitional fibers into A-V Nodal fibers
• Moderate decrease simply delays conduction of the impulse
• A large decrease blocks the conduction entirely
13-Jun-23 Physiology of the heart 39
Control of Excitation in Heart
• The pacemaker cells
• SANode, AVNode, Purkinje cell
• All exhibit rhythmicity
• Why does the SAN
• Become the dominant pacemaker
• Why not
• The AVNode or Purkinje fibers dominate
13-Jun-23 Physiology of the heart 40
Control of Excitation
• The normal rate of discharge from these cells
• SAN = 70 to 80 per minute
• AVN = 40 to 60 per minute
• Purkinje fibers = 15 to 40 per minute
13-Jun-23 Physiology of the heart 41
Control of Excitation
• The rate of diastolic depolarization
• SAN = 15 to 60 mv/sec
• Purkinje fibers = 5 to 40 mv/sec
• In all these cells
• To change from “resting” to threshold potential
• Require a change of 20 to 25 mv
• Thus threshold is reached much faster
• In SAN than in Purkinje fibers
13-Jun-23 Physiology of the heart 42
Cardiotonic Agents
• Chronotropic agents
• Alter the excitability of
• Pacemaker
• Conducting system- Dromotropic effect
• Positive chronotropic agents
• Lead to increase in heart rate
• Negative chronotropic agents
• Lead to decrease in the heart rate
13-Jun-23 Physiology of the heart 43
Effects of Autonomic Nervous System
• Sympathetic stimulation increases
• Rate of sinus node discharge
• Rate of conduction
• Level of excitability of myocardium
• Force of contraction of myocardium
13-Jun-23 Physiology of the heart 44
Noradrenalin
• Noradrenalin increases
• The rate of SAN cells depolarization
• The rate of spontaneous discharge
• Heart rate
13-Jun-23 Physiology of the heart 45
Parasympathetic
• Parasympathetic stimulation
• Causes release of acetylcholine
• This causes a decrease
• Heart rate
• Excitability of AVN
• Slows transmission of impulses to ventricles
13-Jun-23 Physiology of the heart 46
Parasympathetic
• Very strong stimulation
• Can stop SAN discharge
• Block AVN transmission
• Ventricle can stop contraction
• Vagal escape
• Ectopic pacemaker from Purkinje fibers take over
13-Jun-23 Physiology of the heart 47
Parasympathetic
• Acetylcholine
• Activate M2 (muscarinic) receptors
• Through G-protein
• Open special K+ channels
• Efflux of K+
• Hyperpolarization
13-Jun-23 Physiology of the heart 48
Parasympathetic
• Activation of M2 receptors also
• Decrease cAMP concentration in cell
• Slows opening of Ca++ channels
• Rate of diastolic depolarization is retarded
• It takes longer to reach threshold
• Heart rate is slowed
13-Jun-23 Physiology of the heart 49
Depolarization and Impulse Conduction
• Spread from
atrioventricular (AV)
node
• AV bundle
• Bundle branches
• Purkinje fibers
13-Jun-23 Physiology of the heart 50
Depolarization and Impulse Conduction
• Depolarization in SA
node precedes
depolarization in atria,
AV node, ventricles
13-Jun-23 Physiology of the heart 51
13-Jun-23 Physiology of the heart 52
Cardiotonic Agents
• Inotropic agents
• Affect the contractility of the cardiac muscles
• Positive inotropic agents
• Lead to increase in contraction
• Negative inotropic agents
• Lead to decrease in contraction
13-Jun-23 Physiology of the heart 53
You might also like
- EKG Flash Cards PDFDocument9 pagesEKG Flash Cards PDFdiani arisandhi100% (1)
- Conduction System of The HeartDocument24 pagesConduction System of The HeartnirilibNo ratings yet
- The 12-Lead Electrocardiogram for Nurses and Allied ProfessionalsFrom EverandThe 12-Lead Electrocardiogram for Nurses and Allied ProfessionalsNo ratings yet
- A Simple Guide to the Heart beats, Related Diseases And Use in Disease DiagnosisFrom EverandA Simple Guide to the Heart beats, Related Diseases And Use in Disease DiagnosisRating: 5 out of 5 stars5/5 (1)
- Cardiac NursingDocument26 pagesCardiac Nursingjgcriste95% (20)
- The Medical Book of Lists A Primer of Differential Diagnosis in PDFDocument260 pagesThe Medical Book of Lists A Primer of Differential Diagnosis in PDFshoko100% (1)
- EKG | ECG: An Ultimate Step-By-Step Guide to 12-Lead EKG | ECG Interpretation, Rhythms & Arrhythmias Including Basic Cardiac DysrhythmiasFrom EverandEKG | ECG: An Ultimate Step-By-Step Guide to 12-Lead EKG | ECG Interpretation, Rhythms & Arrhythmias Including Basic Cardiac DysrhythmiasRating: 3 out of 5 stars3/5 (5)
- Heart Muscle: The Heart As A Pump and FunctionDocument4 pagesHeart Muscle: The Heart As A Pump and Functionmcwnotes100% (1)
- Coronary Artery Disease PathophysiologyDocument3 pagesCoronary Artery Disease Pathophysiologynursing concept maps50% (4)
- Rhythmical Excitation of The HeartDocument4 pagesRhythmical Excitation of The Heart22194No ratings yet
- Assessment of The Peripheral Vascular SystemDocument91 pagesAssessment of The Peripheral Vascular SystemKeid Reuma100% (1)
- 1.cardiac Muscle The Heart As A Pump and Function of The Heart Valves 2022Document73 pages1.cardiac Muscle The Heart As A Pump and Function of The Heart Valves 2022Sezanur Taalaibek kyzyNo ratings yet
- Lecture - 3 Properties of Cardiac MuscleDocument35 pagesLecture - 3 Properties of Cardiac MuscleMRM7MDNo ratings yet
- Surgical Intensive CareDocument95 pagesSurgical Intensive Carelizzy596No ratings yet
- Basic Life Support: Cardiopulmonary Resuscitation Prepared By: BSN - 3Document20 pagesBasic Life Support: Cardiopulmonary Resuscitation Prepared By: BSN - 3sheryline100% (1)
- BLS Training - Question PaperDocument3 pagesBLS Training - Question PaperNav J Kar100% (1)
- Anaesthesia Management of Patient of PacemakerDocument92 pagesAnaesthesia Management of Patient of PacemakerSiva KrishnaNo ratings yet
- Cardiac surgery 5th year 2017-محلولDocument11 pagesCardiac surgery 5th year 2017-محلولIbrahim BarhamNo ratings yet
- Cadiac Cycle, Heart Sound, ECG, HypertensionDocument110 pagesCadiac Cycle, Heart Sound, ECG, HypertensionNilesh100% (1)
- Interventional RadiologyDocument53 pagesInterventional Radiologypri_29275% (4)
- NCM 118 RLE (Week 7-8)Document7 pagesNCM 118 RLE (Week 7-8)kNo ratings yet
- Acsm Health Fitness Facility Standards Guidelines Download PDFDocument9 pagesAcsm Health Fitness Facility Standards Guidelines Download PDFAleksandar MihajlovićNo ratings yet
- 2 - Cardiac Electrical ActivityyytyyDocument31 pages2 - Cardiac Electrical ActivityyytyyTausif ChNo ratings yet
- Conductive System of HeartDocument7 pagesConductive System of HeartnidhiNo ratings yet
- Special Conductive System of Heart: By: Azher SyedDocument14 pagesSpecial Conductive System of Heart: By: Azher SyedAzhersyedNo ratings yet
- Origin & Conduction of Cardiac Impulse: Dr.S.Brinda MD Associate Professor PhysiologyDocument36 pagesOrigin & Conduction of Cardiac Impulse: Dr.S.Brinda MD Associate Professor PhysiologyAtchaya ThillainatarajanNo ratings yet
- Conducting System of The HeartDocument27 pagesConducting System of The HeartMuhammadNo ratings yet
- Conducting System of HeartDocument14 pagesConducting System of HeartAbdul Samee AslamNo ratings yet
- Heart ActionDocument14 pagesHeart ActionNqaba SisoNo ratings yet
- Physiology of Heart in DetailDocument101 pagesPhysiology of Heart in Detailakanksha sharmaNo ratings yet
- Conducting System of HeartDocument34 pagesConducting System of HeartWijesiri D WNo ratings yet
- Read 1 CVS OrgDocument34 pagesRead 1 CVS OrgEzeudu SomtoNo ratings yet
- Initiation and Propagation of Cardiac ImpulseDocument110 pagesInitiation and Propagation of Cardiac Impulsedavid mullingsNo ratings yet
- Cardiac PacemakersDocument49 pagesCardiac PacemakersMohammad AliNo ratings yet
- Cardiovascular Physiology 1Document44 pagesCardiovascular Physiology 1maxmus4No ratings yet
- Cardiovascular and Circulatory FunctionDocument271 pagesCardiovascular and Circulatory FunctionARAGON GEMMA LYNNo ratings yet
- 2-Cardiac Electical ActivityDocument26 pages2-Cardiac Electical ActivityhalayehiahNo ratings yet
- 106 FinalsDocument27 pages106 FinalsCreciabullecerNo ratings yet
- Cardiac Ana & DxticsDocument3 pagesCardiac Ana & Dxticsjames garciaNo ratings yet
- Physiology of Excitatory and Conducting System of Heart by Dr. Mudassar Ali RoomiDocument17 pagesPhysiology of Excitatory and Conducting System of Heart by Dr. Mudassar Ali RoomiMudassar Roomi100% (3)
- Chapter 10-Rhythmical Excitation of The HeartDocument13 pagesChapter 10-Rhythmical Excitation of The Heartmuna s100% (1)
- Physiology of Excitation and Conduction System of Heart by Dr. Mudassar Ali RoomiDocument17 pagesPhysiology of Excitation and Conduction System of Heart by Dr. Mudassar Ali RoomiMudassar Roomi100% (1)
- Rhythmical Excitation of The HeartDocument6 pagesRhythmical Excitation of The HeartTONY GO AWAYNo ratings yet
- Cardiac Muscles and Conducting System of HeartDocument37 pagesCardiac Muscles and Conducting System of HeartwalterNo ratings yet
- Histology of Heart Conducting SystemDocument9 pagesHistology of Heart Conducting SystemTasya AuliaNo ratings yet
- Cardiac Cycle and Myogenic Control of HeartbeatDocument25 pagesCardiac Cycle and Myogenic Control of HeartbeatFiona HennahNo ratings yet
- Lecture - HeartDocument102 pagesLecture - HeartohmedicalstudyNo ratings yet
- Conducting System of The HeartDocument13 pagesConducting System of The HeartKiran DeviNo ratings yet
- Cardiovascular System ATU (Autosaved)Document58 pagesCardiovascular System ATU (Autosaved)maxwell amponsahNo ratings yet
- As 1 2 2 Control of The Cardiac CycleDocument19 pagesAs 1 2 2 Control of The Cardiac Cyclepoikl098No ratings yet
- Cardiovascular System: Prepared by Samjhana GautamDocument71 pagesCardiovascular System: Prepared by Samjhana GautamSamjhana GautamNo ratings yet
- Unit - Ii Cardiovascular InstrumentationDocument125 pagesUnit - Ii Cardiovascular InstrumentationYashaswiniNo ratings yet
- Cardiac Muscle: Dr. Kanimozhi Sadasivam, MD Associate Professor SRM Medical College & RC, ChennaiDocument57 pagesCardiac Muscle: Dr. Kanimozhi Sadasivam, MD Associate Professor SRM Medical College & RC, ChennaiShampa SenNo ratings yet
- WEEK 1 MEDSURG AsynchDocument12 pagesWEEK 1 MEDSURG AsynchLeigh Angelika Dela CruzNo ratings yet
- The Cardiovascular SystemDocument4 pagesThe Cardiovascular SystemSharie Mae MataumNo ratings yet
- Cardiac Cycle: PacemakerDocument3 pagesCardiac Cycle: Pacemakerapi-296833859No ratings yet
- Conduction of The HeartDocument1 pageConduction of The HeartPearlyn John BrittoNo ratings yet
- 4 - PHYSIOLOGY - Electrical Activity of The Heart LectureDocument78 pages4 - PHYSIOLOGY - Electrical Activity of The Heart Lecturefznfbw8qqcNo ratings yet
- Anatomi Fisiologi Sistem Kardiovaskuler 1Document52 pagesAnatomi Fisiologi Sistem Kardiovaskuler 1Vaweli Putri Spelman DpNo ratings yet
- Anatomy & Function of Conducting SystemDocument22 pagesAnatomy & Function of Conducting SystemhalayehiahNo ratings yet
- HEART SimplifiedDocument94 pagesHEART Simplifiedcloud kumoishNo ratings yet
- Structure and Function of The Cardiovascular System PDFDocument9 pagesStructure and Function of The Cardiovascular System PDFteuuuuNo ratings yet
- 11 The Cardiovascular SystemDocument27 pages11 The Cardiovascular SystemHarshika KDGNo ratings yet
- Lecture5 - Electrocardiogram Electromyogram - 1Document33 pagesLecture5 - Electrocardiogram Electromyogram - 1AbdullahNo ratings yet
- Components of The Cardiovascular SystemDocument23 pagesComponents of The Cardiovascular SystemMr. DummyNo ratings yet
- Summary CH 10 Guton and HallDocument5 pagesSummary CH 10 Guton and HallDina AlsohaibiNo ratings yet
- Immediate Life Support for healthcare Practitioners: A Step-By-Step GuideFrom EverandImmediate Life Support for healthcare Practitioners: A Step-By-Step GuideNo ratings yet
- Veteriner Anatomi Dolaşım Sistemi by VETSDocument54 pagesVeteriner Anatomi Dolaşım Sistemi by VETSalparslanhocaoglu60No ratings yet
- Mitral Stenosis Mitral StenosisDocument68 pagesMitral Stenosis Mitral StenosisnijasNo ratings yet
- Point of Care Cardiac MarkersDocument14 pagesPoint of Care Cardiac MarkersLien TranNo ratings yet
- Jama Andersen 2021 Oi 210108 1632503925.26159Document9 pagesJama Andersen 2021 Oi 210108 1632503925.26159AlizaPinkyNo ratings yet
- Grade7 Bio Chapter10 Transportation - CW&HWDocument6 pagesGrade7 Bio Chapter10 Transportation - CW&HWTanushree RNo ratings yet
- Adaptive Aortic Pressure Observer For The Penn State Electric Ventricular Assist DeviceDocument10 pagesAdaptive Aortic Pressure Observer For The Penn State Electric Ventricular Assist DevicemaryamNo ratings yet
- 1.6, 1.7 Circulatory System Structure and Function Exam QuestionsDocument6 pages1.6, 1.7 Circulatory System Structure and Function Exam QuestionsAhmad LuqmanNo ratings yet
- Jurnal Mutiple StentDocument9 pagesJurnal Mutiple StentPrima Anggreini ArinNo ratings yet
- Acute Stroke CaseDocument19 pagesAcute Stroke CaseAsep BageurNo ratings yet
- Seminar On Rheumatic Heart Disease: by Zerihun GetachewDocument37 pagesSeminar On Rheumatic Heart Disease: by Zerihun GetachewZerihun Getachew ShiferawNo ratings yet
- Right Left: Abdominal Aorta and BranchesDocument1 pageRight Left: Abdominal Aorta and Branchesjesus Porras ColonNo ratings yet
- Cardiac Cycle and Myogenic Control of HeartbeatDocument25 pagesCardiac Cycle and Myogenic Control of HeartbeatFiona HennahNo ratings yet
- Nejmoa 003289Document7 pagesNejmoa 003289Mirela CiobanescuNo ratings yet
- 6 Ab 2Document3 pages6 Ab 2Erko100% (1)
- Guideline: Physical Therapist Clinical Practice Guideline For The Management of Individuals With Heart FailureDocument30 pagesGuideline: Physical Therapist Clinical Practice Guideline For The Management of Individuals With Heart FailureNindy Yantika MciNo ratings yet
- Unit 1 Introduction of BiomedicalDocument78 pagesUnit 1 Introduction of Biomedicalashu singhNo ratings yet
- Omron M3 Intellisense (HEM-7051-E) Manual PDFDocument38 pagesOmron M3 Intellisense (HEM-7051-E) Manual PDFZee Eagle100% (1)
- TurkJEmergMed22275 5543957 - 013223 2Document8 pagesTurkJEmergMed22275 5543957 - 013223 2Ria Junita AyuNo ratings yet