Professional Documents
Culture Documents
Sevsere Hypophosphatimia
Sevsere Hypophosphatimia
Uploaded by
VCOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Sevsere Hypophosphatimia
Sevsere Hypophosphatimia
Uploaded by
VCCopyright:
Available Formats
Advertisement
PDF $ Split View % Cite & Permissions ' Share " Clinical Chemistry (
Journals Books
Volume 69, Issue 5
May 2023 More Content
Issues " Submit " Purchase Alerts About " Clinical Chemistry (
Advanced
Search
Article Contents Advertisement
Case Description JOURNAL ARTICLE
Discussion Severe Hypophosphatemia: The Hidden Truth !
Farzahna Mohamed # , Frederick J Raal Author Notes
Case Resolution
Clinical Chemistry, Volume 69, Issue 5, May 2023, Pages 450–453,
Nonstandard Abbreviations
https://doi.org/10.1093/clinchem/hvad028
Human Genes Published: 28 April 2023 Article history "
Author Contributions
PDF $ Split View % Cite & Permissions ' Share "
Authors’ Disclosures or
Potential Conflicts of Interest Advertisement
Employment or Leadership Issue Section: Clinical Case Study
Consultant or Advisory Role
VIEWS ALTMETRIC
Stock Ownership
Honoraria
Case Description 331
Research Funding
A 52-year-old woman presented with a 14-year history of progressive proximal More metrics information
Expert Testimony muscle weakness and myalgia. She had been wheelchair-bound for the previous 10
Patents years, with a significant loss of height since the onset of symptoms. She was
previously healthy, with no family history of metabolic bone disease. Clinical
Other Remuneration examination revealed a proximal myopathy, short stature with marked Email alerts
References kyphoscoliosis and pectus carinatum. Her admission laboratory investigations
Article activity alert
showed severe hypophosphatemia, with a serum phosphate of 0.87 mg/dL (0.28
Author notes Advance article alerts
mmol/L [reference interval 2.5–4.5 mg/dL; 0.8–1.4 mmol/L]). 25-Hydroxy
vitamin D (25-OHD) was reduced with a normal 1,25-dihydroxy vitamin D (1,25- New issue alert
< Previous Next > OHD). Laboratory results are summarized in Table 1. Of note, the tubular
maximum reabsorption of phosphate for glomerular filtration rate (TmP/GFR) Receive exclusive offers and updates
was 0.8 mg/dL (0.22 mmol/L [reference interval 2.0–3.4 mg/dL; 0.80–1.35 from Oxford Academic
mmol/L]), suggestive of renal phosphate wasting. Fibroblast growth factor 23
(FGF-23) was elevated at 9207 pg/mL (reference interval 12–49 pg/mL). Despite
phosphate and vitamin D replacement, the hypophosphatemia persisted.
See also
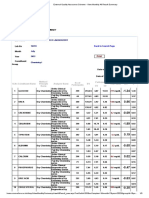
Table 1. Biochemical results at the time of admission (all serum unless specified otherwise). COMMENTARY
Commentary on Severe Hypophosphatemia:
Analyte Reference interval Result The Hidden Truth
Adjusted calcium 8.8–10 mg/dL 8.8 Commentary on Severe Hypophosphatemia:
The Hidden Truth
Phosphate 2.5–4.5 mg/dL 0.87
Magnesium 1.5–2.6 mg/dL 1.97
Citing articles via
Albumin 3.5–5.2 g/dL 4.4
Google Scholar
Parathyroid hormone 14–72 pg/mL 622
25-hydroxy vitamin D <20 ng/mL—deficient; >30 ng/mL—sufficient 13 Latest Most Read Most Cited
1,25-dihydroxy vitamin D 17–65 pg/mL 53 A Single Reference Interval for Interpreting
Serum Free Light Chains across Patients with
Alkaline phosphatase 42–98 IU/L 460
Varying Renal Function
Bone-specific alkaline phosphatase 14–42 IU/L 305 Analytical and Non-Analytical Variation May
Lead to Inappropriate Antimicrobial Dosing in
Creatinine 0.55–1.02 mg/dL 0.43
Neonates: An In Silico Study
2
Estimated glomerular filtration rate 90–120 mL/min/1.73m 117 A Case of Yellow Airway Secretions and Oral
Fluid
TmP/GFR 2.0–3.4 mg/dL 0.8
Severe Hypophosphatemia: The Hidden Truth
Fibroblast growth factor 23 12–49 pg/mL 9207
Commentary on Severe Hypophosphatemia:
Open in new tab The Hidden Truth
More from Oxford Academic
Questions to Consider Biochemistry Biological Sciences
1. What are the causes of urine phosphate wasting? Medical Skills Medicine and Health
2. What is the most likely cause of persistent hypophosphatemia in the Pathology
setting of a normal or low plasma calcitriol level (1,25-OHD)?
Research Methods in Life Sciences
3. What is the most common phosphatonin responsible for diseases
Science and Mathematics Books
characterized by urine phosphate wasting?
Journals
4. What is the diagnostic localization image of choice in this case?
Discussion
A diagnosis of tumor-induced osteomalacia (TIO) was considered and localization
of the tumor was pursued. Localization images included a Gallium 68 DOTATATE
68
positron emission tomography/ computed tomography ( Ga DOTATATE PET/CT),
which showed a 2 cm soft tissue density inferior to the right 2nd and 3rd
metatarsophalangeal joint (Fig. 1 A). MRI of the right foot revealed a
corresponding soft tissue mass (Fig. 1 B). A bone densitometry scan showed
severely reduced bone mineral density with a T-score of -4.4 and -6.4 at the
lumbar spine and left neck of femur respectively. This was in keeping with
osteomalacia. The whole body bone scan showed typical findings of TIO, such as
the ‘tie sign,’ ‘rachitic rosary sign,’ and ‘pseudo-reactivation’ of growth plates (1)
(Fig. 1 C).
Fig. 1.
Open in new tab Download slide
68
(A), Gallium 68 DOTATATE positron emission tomography/ computed tomography ( Ga DOTATATE
PET CT): soft tissue density (1.8 cm×1.8 cm), inferior to the right metatarsophalangeal joint of the
2nd and 3rd digit, with avid uptake of tracer (white arrow); (B), MRI right foot: soft tissue mass
plantar to the 2nd and 3rd metatarsal heads (open arrow). (C) Bone scan: ‘tie sign’ (black arrow),
‘rachitic rosary sign’ (black open arrow), ‘pseudo-reactivation’ of growth plates (black curved
arrow).
Hypophosphatemia is defined as a plasma phosphate less than 2.5 mg/dL (0.8
mmol/L). Phosphate is important for optimal cellular function and serum
phosphorous concentration is predominantly determined by proximal renal
tubular reabsorption via parathyroid hormone regulation (2, 3). Intestinal
phosphorous absorption contributes to a lesser extent to phosphate homeostasis,
with a low phosphate diet and low 1,25-OHD being the 2 most important
regulators for intestinal phosphate absorption (2, 3). Hence, phosphate deficiency
can occur secondary to reduced input, either from insufficient intake or
absorption, or due to increased renal losses and abnormalities in vitamin D
homeostasis. Clinical manifestations of hypophosphatemia depend on the severity
and chronicity of phosphate deficiency, with severe hypophosphatemia (≤1.0
mg/dL [0.3 mmol/L]) being associated with rhabdomyolysis, respiratory failure,
hemolysis, and left ventricular dysfunction (3).
Chronic severe hypophosphatemia is typically caused by rare disorders, including
X-linked hypophosphatemic rickets, autosomal-dominant hypophosphatemic
rickets, and TIO (3). TIO, also known as oncogenic osteomalacia, is a rare
paraneoplastic syndrome of unknown prevalence, with 1000 cases reported
worldwide to date (4, 5). It is usually caused by a phophaturic mesenchymal tumor
(PMT), which is generally a slow-growing and typically benign mesenchymal or
mixed connective tissue neoplasm that affects bone or soft tissue (2, 4). The most
common phosphatonin secreted by these tumors is FGF-23; however, rarely, other
phosphatonins can be secreted. These include frizzled-related protein-4, FGF-7,
and matrix extracellular phosphoglycoprotein (MEPE), none of which is routinely
measured (4, 6).
FGF-23 acts predominantly at the renal tubule, impairing phosphate reabsorption
and 1-alpha hydroxylation of 25-OHD. Thus, the biochemical hallmarks of TIO are
severe hypophosphatemia secondary to phosphaturia and inappropriately normal
or low 1,25-OHD, with normal serum levels of calcium, parathyroid hormone, and
25-OHD. This biochemical phenotype should direct FGF-23 testing to support the
diagnosis of TIO. The renal phosphate leak is defined by a TmP/GFR result below
the lower reference interval, with the reference range being age and sex dependent
(2, 4, 7, 8). TmP/GFR measures maximum renal tubular phosphate reabsorption in
mass per unit volume of glomerular filtrate, with an increase in TmP/GFR when
plasma phosphate is low and vice versa (8). In a non-disease state, the TmP/GFR
will be high when there is hypophosphatemia, but in TIO, it is abnormally low,
confirming phosphaturia (2).
Due to the lack of awareness of this condition, there is often a prolonged lag time
between the onset of symptoms and diagnosis. Oncogenic osteomalacia, like X-
linked hypophosphatemia, exhibits decreased mineralization of newly formed
bone, and a useful clinical discriminator between the 2 diseases is the age of onset,
whereby X-linked hypophosphatemia typically manifests in the second year of life
(7). The predominant clinical presentation of TIO includes muscle weakness and
severe bone pain that is an unusual symptom for X-linked hypophosphatemia (7).
TIO may also present with or without bone deformities and pathological fractures
or pseudo-fractures.
These tumors are usually small and hence challenging to localize, with successful
localization achieved in only 61% of subjects utilizing a combination of functional
111
imaging including In-pentetreotide single-photon emission computer
tomography (Octreoscan-SPECT), fluorodeoxyglucose-positron emission
18 68
tomography ( F FDG-PET/CT), and anatomical imaging (9). Ga-DOTATATE
PET/CT showed greater sensitivity and specificity in TIO localization when
18
compared to Octreoscan-SPECT/CT and F FDG-PET/CT (9).
The therapeutic modality of choice for TIO is surgical resection of the neoplasm. A
resection with wide margins is recommended to avoid persistent disease, local or
multifocal relapse, and/or distant metastasis when small amounts of residual
tissue remain (4). Therapeutic options for irresectable tumors include primary or
adjuvant radiotherapy and chemotherapy (4). Targeted therapy is based on the
expression of somatostatin receptors on PMTs. Octreotide and peptide receptor
177
radionuclide therapy (PRRT) with Lu DOTATATE has been proposed, with a
variable but modest response (4). Alternative medical therapies utilized in FGF-
23–mediated renal phosphaturia include burosamab or cinacalcet (4). Burosumab
is a fully human monoclonal antibody that inhibits FGF-23 (10). Data from an open
label phase 2 study, in patients with TIO, showed a significant increase in serum
phosphate from baseline, as well as an improvement in all measures of
osteomalacia at 48 weeks (10). Cinacalcet reduces renal phosphate wasting by
inducing a functional hypophosphatemia (4). Furthermore, vitamin D metabolites,
preferably calcitriol, and oral phosphate salts are recommended in those where the
tumor is not identified or irresectable (7).
A recent systematic review of 1725 TIO cases showed a male predominance, with
male patients also showing a higher incidence of fractures compared to women
(4). Almost 80% of TIOs were benign and a neoplasm was identified in 87% of
cases, with somatostatin receptor-based imaging modalities having the highest
sensitivity (4). The neoplasm is most frequently located in the lower limbs (53%
[femur, acetabulum, or feet]) and the head (30% [paranasal sinuses, maxilla, or
oral cavity]), with a preferential localization in the lower limbs seen in men,
compared to women predominantly localizing in the head (4, 9). The reason for
these site preferences is unknown, but sexual differentiation may be linked to
variations of expression of the FN1-FGFR1 fusion gene (4). Malignant TIO was
observed in 3.8% of patients and was associated with a higher risk of pseudo-
fractures, lower TmP/GFR, and higher calcium levels compared to non-malignant
TIO (4). Multifocal TIO occurred in only 6 patients and showed no biochemical or
clinical difference in presentation to unifocal TIO, except for a higher risk of
pseudo-fractures (4). Surgery was the therapeutic modality of choice (98.7%) in
patients with an identifiable tumor (4).
Case Resolution
Our patient proceeded to surgery, and a well-circumscribed mass measuring 12 ×
10 × 9 mm was excised, with a 1 mm clear margin of resection. Histology was
compatible with a benign PMT, specifically the non-ossifying fibroma-like variant
whereby trabeculae of woven bone, spindle cells with nuclear pleomorphisms, and
osteoclast-like giant cells were noted. Phosphate and vitamin D replacement was
discontinued and the phosphate level normalized 1 week postoperatively, with a
68% reduction in FGF-23 levels. The patient no longer required phosphate and
vitamin D replacement and showed an overall improvement in muscle strength.
TIO is a paraneoplastic syndrome caused by over-secretion of FGF-23 from a PMT.
The clinical and biochemical presentation of TIO is important to recognize as it is
an endocrine neoplasm which may have debilitating consequences, yet can have a
very gratifying outcome if cured.
Points to Remember
Severe hypophosphatemia requires prompt evaluation for renal phosphate
wasting, allowing early diagnosis and treatment.
Tumor-induced osteomalacia is a paraneoplastic syndrome caused by
over-secretion of FGF-23 from a phosphaturic mesenchymal tumor.
These tumors are usually benign and are typically small, thus proving a
diagnostic challenge.
Treatment of choice is surgical excision of the tumor.
Nonstandard Abbreviations
OHD, hydroxy vitamin D; TmP/GFR, tubular maximum reabsorption of phosphate
for glomerular filtration rate; FGF-23,fibroblast growth factor 23; TIO, tumor-
induced osteomalacia; PET/CT, positron emission tomography/ computed
tomography; PMT, phophaturic mesenchymal tumor.
Human Genes
FN1-FGFR1
Author Contributions
All authors confirmed they have contributed to the intellectual content of this paper and
have met the following 4 requirements: (a) significant contributions to the conception
and design, acquisition of data, or analysis and interpretation of data; (b) drafting or
revising the article for intellectual content; (c) final approval of the published article;
and (d) agreement to be accountable for all aspects of the article thus ensuring that
questions related to the accuracy or integrity of any part of the article are appropriately
investigated and resolved.
Farzahna Mohamed (Conceptualization, Writing—original draft, Writing—review
& editing), Frederick J. Raal (Supervision, Funding acquisition)
Authors’ Disclosures or Potential Conflicts of Interest
Upon manuscript submission, all authors completed the author disclosure form.
Disclosures and/or potential conflicts of interest:
Employment or Leadership
None declared.
Consultant or Advisory Role
F.J. Raal, fees for advisory board presentations on lipid-lowering therapy and
honoraria from Amgen, Sanofi-Aventis, Regeneron, Novartis, and LIB
Therapeutics. No conflict of interest for the publication above.
Stock Ownership
None declared.
Honoraria
F.J. Raal, fees for lectures on lipid-lowering therapy and honoraria from Amgen,
Sanofi-Aventis, Regeneron, Novartis, and LIB Therapeutics. No conflict of interest
for the publication above.
Research Funding
None declared.
Expert Testimony
None declared.
Patents
None declared.
Other Remuneration
F.J. Raal, support for attending meetings and/or travel from Amgen, Sanofi-
Aventis, Regeneron, Novartis, and LIB Therapeutics.
References
1 Chakraborty PP, Bhattacharjee R, Mukhopadhyay S, Chowdhury S. ‘Rachitic rosary sign’ and ‘tie
sign’ of the sternum in tumour-induced osteomalacia. BMJ Case Rep 2016;2016:bcr2016214766.
Google Scholar WorldCat
2 Chong WH, Molinolo AA, Chen CC, Collins MT. Tumor-induced osteomalacia. Endocr Relat Cancer
2011;18:53–77.
Google Scholar Crossref WorldCat
3 Amanzadeh J, Reilly RF Jr. Hypophosphatemia: an evidence-based approach to its clinical
consequences and management. Nat Clin Pract Nephrol 2006;2:136–48.
Google Scholar Crossref PubMed WorldCat
4 Rendina D, Abate V, Cacace G, D'Elia L, De Filippo G, Del Vecchio S, et al. Tumor-induced
osteomalacia: a systematic review and individual patient's data analysis. J Clin Endocrinol
Metab 2022;107:3428–3436.
Google Scholar Crossref PubMed WorldCat
5 Dahir K, Zanchetta MB, Stanciu I, Robinson C, Lee JY, Dhaliwal R, et al. Diagnosis and
management of tumour-induced osteomalacia: perspectives from clinical experience. J Endocr
Soc 2021;5:bvab099.
Google Scholar Crossref PubMed WorldCat
6 Jonsson KB, Zahradnik R, Larsson T, White KE, Sugimoto T, Imanishi Y, et al. Fibroblast growth
factor 23 in oncogenic osteomalacia and X-linked hypophosphatemia. N Engl J Med
2003;348:1656–63.
Google Scholar Crossref PubMed WorldCat
7 Carpenter TO. Oncogenic osteomalacia—a complex dance of factors. N Engl J Med
2003;348:1705–8.
Google Scholar Crossref PubMed WorldCat
8 Payne RB. Renal tubular reabsorption of phosphate (TmP/GFR): indications and interpretation.
Ann Clin Biochem 1998;35:201–6.
Google Scholar Crossref PubMed WorldCat
68
9 El-Maouche D, Sadowski SM, Papadakis GZ, Guthrie L, Cottle-Delisle C, Merkel R, et al. Ga-
DOTATATE for tumor localization in tumor-induced osteomalacia. J Clin Endocrinol Metab
2016;101:3575–81.
Google Scholar Crossref PubMed WorldCat
10 Jan de Beur SM, Miller PD, Weber TJ, Peacock M, Insogna K, Kumar R, et al. Burosumab for the
treatment of tumor-induced osteomalacia. J Bone Miner Res 2021;36:627–635.
Google Scholar Crossref PubMed WorldCat
Author notes
Previous Presentation: Portions of this manuscript were presented as a poster at the 52nd Society
of Endocrinology, Metabolism and Diabetes of South Africa (SEMDSA) Congress, May 2017, in
Johannesburg, South Africa.
© American Association for Clinical Chemistry 2023. All rights reserved. For permissions, please e-
mail: journals.permissions@oup.com
This article is published and distributed under the terms of the Oxford University Press, Standard
Journals Publication Model (https://academic.oup.com/pages/standard-publication-reuse-rights)
Advertisement
About Clinical Chemistry Facebook
About AACC Recommend to Your Librarian
Editorial Board Advertising and Corporate
Services
Author Guidelines
Journals Career Network
Online ISSN 1530-8561 Print ISSN 0009-9147 Copyright © 2023 American Association of Clinical Chemistry
About Oxford Academic Authoring Get help with access Oxford University Press Oxford University Press is a department
of the University of Oxford. It furthers
Publish journals with us Open access Accessibility News
the University's objective of excellence
University press partners Purchasing Contact us Oxford Languages in research, scholarship, and education
by publishing worldwide
What we publish Institutional account management Advertising University of Oxford
Oxford University Press uses cookies to
New features enhance
Rights your experience on our website. ByMedia
and permissions selecting ‘accept all’ you are agreeing to our use of cookies. You can change your cookie settings
enquiries
at any time. More information can be found in our Cookie Policy.
Accept all Deny all Cookie settings
Copyright © 2023 Oxford University Press Cookie settings Cookie policy Privacy policy Legal notice
You might also like
- Autism Test-1Document4 pagesAutism Test-1Salbia RiasatNo ratings yet
- Physical Examination Report: 23/FEMALE Dalig, Balayan, Batangas 7/11/1997 8:50 AM Waltermart Balayan 6/4/2021 SingleDocument3 pagesPhysical Examination Report: 23/FEMALE Dalig, Balayan, Batangas 7/11/1997 8:50 AM Waltermart Balayan 6/4/2021 SingleIan De LeonNo ratings yet
- Asepsis and Infection Control Nursing SchoolDocument20 pagesAsepsis and Infection Control Nursing Schoolleonardo orozco100% (1)
- Cattle and Sheep Medicine, 2nd Edition, Self-Assessment Color Review PDFDocument336 pagesCattle and Sheep Medicine, 2nd Edition, Self-Assessment Color Review PDFViktorija VasilkovaNo ratings yet
- Clinical Psychiatry - Emil KraepelinDocument628 pagesClinical Psychiatry - Emil KraepelinSandra LanguréNo ratings yet
- Midterm Quiz - NCM 106.2016Document4 pagesMidterm Quiz - NCM 106.2016Andrea BroccoliNo ratings yet
- BPSA 2020 Extractables & Leachables Considerations For Cell & Gene Therapy DP DevelopementDocument19 pagesBPSA 2020 Extractables & Leachables Considerations For Cell & Gene Therapy DP DevelopementbioNo ratings yet
- Identification of Staphylococcus Species Micrococcus PDFDocument32 pagesIdentification of Staphylococcus Species Micrococcus PDFputri hidayasyahNo ratings yet
- Udan's Neuro, Musculoskel, EentDocument2 pagesUdan's Neuro, Musculoskel, EentReygie Marsada100% (4)
- RADIONIC ASSOC - Base 10 Patologie ConditionsDocument44 pagesRADIONIC ASSOC - Base 10 Patologie Conditionscorrado9freddiNo ratings yet
- Group 7 - Medical Technology Laws and BioethicsDocument10 pagesGroup 7 - Medical Technology Laws and Bioethicsjulo_0550% (4)
- Experimental Protein-Calorie Deficiency - ScienceDirectDocument1 pageExperimental Protein-Calorie Deficiency - ScienceDirectPablo AndrésNo ratings yet
- Nanotechnology and Medicine - Expert Opinion On Biological Therapy - Vol 3, No 4Document3 pagesNanotechnology and Medicine - Expert Opinion On Biological Therapy - Vol 3, No 4Ana JuliaNo ratings yet
- Clinical Pharmacology & BiopharmaceuticsDocument7 pagesClinical Pharmacology & BiopharmaceuticsTrivedi EffectNo ratings yet
- SOME ACTIVE PRINCIPLES of PEPTONE - Journal of Pharmacology and Experimental TherapeuticsDocument4 pagesSOME ACTIVE PRINCIPLES of PEPTONE - Journal of Pharmacology and Experimental TherapeuticssajimarsNo ratings yet
- Syllabus of M. Pharm: Session: 2007-2008 Examination: 2008Document10 pagesSyllabus of M. Pharm: Session: 2007-2008 Examination: 2008afsanakhatunNo ratings yet
- Anti-Tubercular Evaluation of Rivea Hypocrateriformis (Der.) Choisy Against Mycobacterium Tuberculosis H37Rv StrainDocument3 pagesAnti-Tubercular Evaluation of Rivea Hypocrateriformis (Der.) Choisy Against Mycobacterium Tuberculosis H37Rv Strainwadhah albaadaniNo ratings yet
- RLE Alterations in Fluid and Electrolyte BalanceDocument6 pagesRLE Alterations in Fluid and Electrolyte BalanceVince BalisiNo ratings yet
- ESR-eBook-for Endocrine-SystemDocument80 pagesESR-eBook-for Endocrine-SystemkarolynaNo ratings yet
- Modulus - and Surface Energy-Tunable Ultraviolet-Curable Polyurethane Acrylate Properties and Applications - Journal of MaterialDocument1 pageModulus - and Surface Energy-Tunable Ultraviolet-Curable Polyurethane Acrylate Properties and Applications - Journal of Materialacong acongNo ratings yet
- Pharmacological Effects and Potential TherapeuticDocument3 pagesPharmacological Effects and Potential TherapeuticMohsin RizwanNo ratings yet
- Validation of An Experimental Setup To Reliably Simulate Flow Through Nonvalved Glaucoma Drainage DevicesDocument3 pagesValidation of An Experimental Setup To Reliably Simulate Flow Through Nonvalved Glaucoma Drainage Devicesemreka82No ratings yet
- OMX Organic Metabolomics Urine Plasma Sample ReportDocument14 pagesOMX Organic Metabolomics Urine Plasma Sample ReportLudmilaMerlinNo ratings yet
- ID - 13i3 Identification of Pasteurella Species and Morphologically Similar OrganismsDocument28 pagesID - 13i3 Identification of Pasteurella Species and Morphologically Similar OrganismsQworldNo ratings yet
- Petechiae - StatPearls - NCBI BookshelfDocument1 pagePetechiae - StatPearls - NCBI Bookshelfmdrnh6shbmNo ratings yet
- Oximetry-Guided Normoxic Resuscitation Following Canine Cardiac Arrest Reduces Cerebellar Purkinje Neuronal Damage - ResuscitationDocument2 pagesOximetry-Guided Normoxic Resuscitation Following Canine Cardiac Arrest Reduces Cerebellar Purkinje Neuronal Damage - ResuscitationCarlos GomesNo ratings yet
- Lecture 1 Importance of Pharmacoeconomics v2Document18 pagesLecture 1 Importance of Pharmacoeconomics v2dhimas11No ratings yet
- 1 M840-GalleyProofDocument8 pages1 M840-GalleyProofAna GNo ratings yet
- Microbiology and Industrial Biotechnology of FoodDocument12 pagesMicrobiology and Industrial Biotechnology of FoodMartin CastañoNo ratings yet
- Biology An Open Access Journal From MDPIDocument1 pageBiology An Open Access Journal From MDPIDiamant MusicNo ratings yet
- ID - 12i3 Identification of Haemophilus Species and The HACEK Group of OrganismsDocument35 pagesID - 12i3 Identification of Haemophilus Species and The HACEK Group of OrganismsQworldNo ratings yet
- Temperature Variations and The Histological Impact of Diode Laser Irradiation On Oral Soft Tissue at Two Different AppliDocument5 pagesTemperature Variations and The Histological Impact of Diode Laser Irradiation On Oral Soft Tissue at Two Different Applisupiah spdNo ratings yet
- Plus Min HPLCDocument30 pagesPlus Min HPLClusianaNo ratings yet
- Apple Academic PressDocument3 pagesApple Academic PressshrikantmsdNo ratings yet
- 7 - Proteus Syndrome - A Case Report and Review of The LiteratureDocument5 pages7 - Proteus Syndrome - A Case Report and Review of The LiteratureJosé Paulo Ribeiro JúniorNo ratings yet
- Cataract Phcog MagDocument8 pagesCataract Phcog MagKumaranNo ratings yet
- Seite1943 1947140312 MolinarioDocument6 pagesSeite1943 1947140312 MolinarioSm Bikash Kumar MohonNo ratings yet
- Chromatography TheessenceofbioanalysisDocument13 pagesChromatography TheessenceofbioanalysisRivani RahmawatiNo ratings yet
- Toxic Effect of Paracetamol On Mitotic Index of Onion Root TipDocument2 pagesToxic Effect of Paracetamol On Mitotic Index of Onion Root TipEditor IJTSRDNo ratings yet
- Proteomic Analysis of Human Plasma During Intermittent FastingDocument13 pagesProteomic Analysis of Human Plasma During Intermittent FastingioanalupumNo ratings yet
- AcaciacatechuDocument23 pagesAcaciacatechu하은No ratings yet
- Clinical PK PD Etoricoxib - TakemotoDocument19 pagesClinical PK PD Etoricoxib - Takemotoervano1969No ratings yet
- AALL0331DOC Standard RiskDocument208 pagesAALL0331DOC Standard RiskKim66No ratings yet
- Martignago Et Al-2019-Lasers in Medical ScienceDocument9 pagesMartignago Et Al-2019-Lasers in Medical Sciencedevrajsinhchauhan8055No ratings yet
- New Opportunities For Biocatalysis: Making Pharmaceutical Processes GreenerDocument7 pagesNew Opportunities For Biocatalysis: Making Pharmaceutical Processes GreenermnjagaNo ratings yet
- 18 6 Ebook Biosimilars RaderDocument11 pages18 6 Ebook Biosimilars RaderBalaNo ratings yet
- A Dietary Supplement Improves Facial Photoaging AnDocument40 pagesA Dietary Supplement Improves Facial Photoaging AnTatta CamposNo ratings yet
- Formulation Development Characterization of Microemulsiondrug Delivery Systems Containing Antiulcer DrugDocument9 pagesFormulation Development Characterization of Microemulsiondrug Delivery Systems Containing Antiulcer DrugRenan PioliNo ratings yet
- Craik2012 Konformasi THDP AktivitasDocument12 pagesCraik2012 Konformasi THDP AktivitasHasna NoerNo ratings yet
- ESR Ebook For Undergraduate Education in Radiology - 08b Bile Ducts - 0 PDFDocument81 pagesESR Ebook For Undergraduate Education in Radiology - 08b Bile Ducts - 0 PDFANAS ALINo ratings yet
- Rejuvenecimiento PeriocularDocument9 pagesRejuvenecimiento PeriocularDaniela GonzalezNo ratings yet
- Hydroxyurea Toxicity - StatPearls - NCBI BookshelfDocument1 pageHydroxyurea Toxicity - StatPearls - NCBI BookshelfJatin AnandNo ratings yet
- Lab - Development - Booklet Survey Nilai KritisDocument37 pagesLab - Development - Booklet Survey Nilai KritisRidwan Adi PratamaNo ratings yet
- Thiametal 2008Document19 pagesThiametal 2008omar lee mohammadNo ratings yet
- ESR Ebook For Undergraduate Education in Radiology - 07b Small Bowel - 0 PDFDocument80 pagesESR Ebook For Undergraduate Education in Radiology - 07b Small Bowel - 0 PDFANAS ALINo ratings yet
- Eqas July ChemistryDocument3 pagesEqas July ChemistryHitesh GolakiyaNo ratings yet
- PosterfinalDocument1 pagePosterfinalapi-332658607No ratings yet
- Safari - Feb 5, 2023 at 916 AM PDFDocument1 pageSafari - Feb 5, 2023 at 916 AM PDFغاز الشمالNo ratings yet
- Rheology Filler JurnalDocument6 pagesRheology Filler JurnalRobertoNo ratings yet
- Tata Memorial Hospital: Units InvestigationDocument2 pagesTata Memorial Hospital: Units InvestigationSATISH KUMARNo ratings yet
- 2006 Mesotherapy and Phosphatidylcholine Injections - Historical Clarification and ReviewDocument16 pages2006 Mesotherapy and Phosphatidylcholine Injections - Historical Clarification and ReviewDra. Tatiane FariaNo ratings yet
- TaskchemDocument17 pagesTaskchemShahid mailsiNo ratings yet
- Clinical Ocular Pharmacology 5th Ed .18Document2 pagesClinical Ocular Pharmacology 5th Ed .18Jéssica RabeloNo ratings yet
- Pmfnews 13 10 0710Document12 pagesPmfnews 13 10 0710linhNo ratings yet
- B4.1.1 APP The Protocol of Scientific Literatures EvaluationDocument50 pagesB4.1.1 APP The Protocol of Scientific Literatures EvaluationЕвгений ГольдманNo ratings yet
- Comprehensive Overview and Treatment Update On Hair LossDocument9 pagesComprehensive Overview and Treatment Update On Hair LossZuldan KaramiNo ratings yet
- Low-Abundance Proteome Discovery: State of the Art and ProtocolsFrom EverandLow-Abundance Proteome Discovery: State of the Art and ProtocolsNo ratings yet
- Ovarian CancerDocument71 pagesOvarian CancerAyuni SallehNo ratings yet
- Sampoorna Arogya - Group_brochure (1)Document10 pagesSampoorna Arogya - Group_brochure (1)gvcalifornia989No ratings yet
- Gastritis Englis 2018Document115 pagesGastritis Englis 2018irinaNo ratings yet
- Hepatic Hemangioma: CausesDocument2 pagesHepatic Hemangioma: CausesEliza StanescuNo ratings yet
- PTSD Informative SpeechDocument3 pagesPTSD Informative SpeechMorgan GoadNo ratings yet
- Unit 6Document5 pagesUnit 6Bình HồNo ratings yet
- Mulat B.: Gastro Esophageal Reflux Disease (Gerd)Document44 pagesMulat B.: Gastro Esophageal Reflux Disease (Gerd)NehimyaNo ratings yet
- Tube Insertion - NGT, Ogt (RM2021)Document2 pagesTube Insertion - NGT, Ogt (RM2021)Ray Emmanuel Enriquez DomingoNo ratings yet
- Pulmonary Consolidation SyndromesDocument141 pagesPulmonary Consolidation SyndromesGiorgos Doukas KaranasiosNo ratings yet
- Chapter 3 - WoundDocument37 pagesChapter 3 - Woundwp6mq5bb25No ratings yet
- SleepDocument3 pagesSleepBSN 2-2 Espiritu Melody Mae DNo ratings yet
- Kaviyarasan Visitor PassDocument7 pagesKaviyarasan Visitor PassTRISTAR TEKZONENo ratings yet
- KYLE OLOR RLE REQS - Docx 1Document14 pagesKYLE OLOR RLE REQS - Docx 1Bernadeth Barrientos ZamoraNo ratings yet
- Pharmacology of Antiviral DrugsDocument1 pagePharmacology of Antiviral Drugssarah90222100% (1)
- Radiology Mission NEETDocument203 pagesRadiology Mission NEETakramalikhan601No ratings yet
- Kalyanaka Ghrita ConstituentsDocument8 pagesKalyanaka Ghrita ConstituentsQadiir AlamNo ratings yet
- 1 - Perception and CoordinationDocument37 pages1 - Perception and CoordinationJek Dela CruzNo ratings yet
- Greasy Pig DiseaseDocument3 pagesGreasy Pig DiseaseAbhijith S. P100% (1)
- 1 Public Materials Book - IC Com MTG 8.26.2020Document304 pages1 Public Materials Book - IC Com MTG 8.26.2020unidadqualityNo ratings yet
- 6 S's of Common Summer Diseases (Article and Infographics)Document4 pages6 S's of Common Summer Diseases (Article and Infographics)Dimitri MangubatNo ratings yet
- Disaster Nursing Cfu 084740Document9 pagesDisaster Nursing Cfu 084740Leone HeathensNo ratings yet
- Geriatric Medicine Certification Examination Blueprint - ABIMDocument7 pagesGeriatric Medicine Certification Examination Blueprint - ABIMabimorgNo ratings yet
- Pelvic Abscess Concept MapDocument1 pagePelvic Abscess Concept Mapaijiel talisikNo ratings yet