Professional Documents
Culture Documents
IVF Sepsis Review - JAMA2023
IVF Sepsis Review - JAMA2023
Uploaded by
Ahida VelazquezOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
IVF Sepsis Review - JAMA2023
IVF Sepsis Review - JAMA2023
Uploaded by
Ahida VelazquezCopyright:
Available Formats
Clinical Review & Education
JAMA | Review
Fluid Therapy for Critically Ill Adults With Sepsis
A Review
Fernando G. Zampieri, MD, PhD; Sean M. Bagshaw, MD, MSc; Matthew W. Semler, MD, MSc
Multimedia
IMPORTANCE Approximately 20% to 30% of patients admitted to an intensive care CME at jamacmelookup.com
unit have sepsis. While fluid therapy typically begins in the emergency department,
intravenous fluids in the intensive care unit are an essential component of
therapy for sepsis.
OBSERVATIONS For patients with sepsis, intravenous fluid can increase cardiac output
and blood pressure, maintain or increase intravascular fluid volume, and deliver
medications. Fluid therapy can be conceptualized as 4 overlapping phases from early
illness through resolution of sepsis: resuscitation (rapid fluid administered to restore
perfusion); optimization (the risks and benefits of additional fluids to treat shock
and ensure organ perfusion are evaluated); stabilization (fluid therapy is used only
when there is a signal of fluid responsiveness); and evacuation (excess fluid
accumulated during treatment of critical illness is eliminated). Among 3723 patients
with sepsis who received 1 to 2 L of fluid, 3 randomized clinical trials (RCTs)
reported that goal-directed therapy administering fluid boluses to attain a central
venous pressure of 8 to 12 mm Hg, vasopressors to attain a mean arterial blood pressure
of 65 to 90 mm Hg, and red blood cell transfusions or inotropes to attain a central
venous oxygen saturation of at least 70% did not decrease mortality compared
with unstructured clinical care (24.9% vs 25.4%; P = .68). Among 1563 patients with
sepsis and hypotension who received 1 L of fluid, an RCT reported that favoring
vasopressor treatment did not improve mortality compared with further fluid Author Affiliations: Department of
administration (14.0% vs 14.9%; P = .61). Another RCT reported that among 1554 Critical Care Medicine, Faculty of
patients in the intensive care unit with septic shock treated with at least 1 L of fluid Medicine and Dentistry, University of
Alberta and Alberta Health Services,
compared with more liberal fluid administration, restricting fluid administration Edmonton, Alberta, Canada
in the absence of severe hypoperfusion did not reduce mortality (42.3% vs 42.1%; (Zampieri, Bagshaw); Department of
P = .96). An RCT of 1000 patients with acute respiratory distress during the evacuation Medicine, Division of Allergy,
Pulmonary, and Critical Care
phase reported that limiting fluid administration and administering diuretics improved
Medicine, Vanderbilt University
the number of days alive without mechanical ventilation compared with fluid treatment Medical Center, Nashville, Tennessee
to attain higher intracardiac pressure (14.6 vs 12.1 days; P < .001), and it reported that (Semler); Center for Learning
hydroxyethyl starch significantly increased the incidence of kidney replacement therapy Healthcare, Vanderbilt Institute for
Clinical and Translational Research,
compared with saline (7.0% vs 5.8%; P = .04), Ringer lactate, or Ringer acetate. Vanderbilt University Medical Center,
Nashville, Tennessee (Semler).
CONCLUSIONS AND RELEVANCE Fluids are an important component of treating patients
Corresponding Author: Fernando G.
who are critically ill with sepsis. Although optimal fluid management in patients with
Zampieri, MD, PhD, Department of
sepsis remains uncertain, clinicians should consider the risks and benefits of fluid Critical Care Medicine, Faculty of
administration in each phase of critical illness, avoid use of hydroxyethyl starch, Medicine and Dentistry, University of
and facilitate fluid removal for patients recovering from acute respiratory Alberta and Alberta Health Services,
8440-112 St NW, 2-124, Edmonton,
distress syndrome.
AB T6G 2B7, Canada (fzampier@
ualberta.ca).
JAMA. 2023;329(22):1967-1980. doi:10.1001/jama.2023.7560 Section Editor: Mary McGrae
McDermott, MD, Deputy Editor.
A
pproximately 20% to 30% of patients admitted to an
intensive care unit (ICU) have sepsis.1 Of these, approxi- Methods
mately 25% to 40% die prior to hospital discharge.2,3
Fluid therapy is an important component of treatment for patients We searched PubMed for the terms early goal-directed therapy
with sepsis.4,5 Fluid therapy may be administered during any phase [and] sepsis, fluid resuscitation [and] sepsis, fluid therapy [and] sep-
of critical illness with sepsis, including before, during, and after ICU sis [and] critical illness, fluid responsiveness [and] sepsis, and
admission. This review summarizes fluid therapy in the ICU for POCUS (point-of-care ultrasonography) [and] critical care for rel-
patients critically ill with sepsis. evant references. Of 5585 manuscripts identified, 76 articles were
jama.com (Reprinted) JAMA June 13, 2023 Volume 329, Number 22 1967
© 2023 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a University of Toronto Libraries User on 06/17/2023
Clinical Review & Education Review Fluid Therapy for Critically Ill Adults With Sepsis: A Review
Figure 1. Fluid Infusion in Sepsis
A Fluid infusion and the 3-compartment model of fluid distribution B Effect of fluid infusion on volume of venous return,
right atrial pressure, and cardiac output
Intravenous
fluid infusion
Inflammation causes damage to endothelium 1 Increased right atrial pressure may increase cardiac output.
and endothelial glycocalyx, leading to increased
fluid extravasation, interstitial edema, and Fluid infusion increases venous return volume and right
decreased volume of venous return. 2 atrial pressure and may lead to increased cardiac output.
I N T R AVA S C U L A R
C O M PA RT M E N T Further infusion will not increase cardiac output despite
3 increased right atrial pressure and may lead to tissue edema.
n
Movement of fluid between compartments
tur
s re
f ve nou 3
o
Volume
Volume of venous return
INTERSTITIAL
C O M PA RT M E N T
2
Factors affecting fluid distribution
Interstitial fluid is
ut
Sepsis and anesthesia: primarily reabsorbed ou t p
• Decreased diuresis into the circulation via d iac
• Increased fluid extravasation the lymphatic system. 1 C ar
Low endothelial integrity:
• Increased fluid extravasation
Low infusion volume: INTERSTITIAL
C O M PA RT M E N T
• Decreased fluid extravasation
High infusion rate:
• Decreased fluid reabsorption Right atrial pressure
into circulation
Fluid is removed from
Low serum osmotic pressure: the circulation through
• Increased fluid extravasation diuresis or dialysis. As cardiac output increases,
Low capillary hydrostatic pressure:
• Decreased fluid extravasation
blood pressure (pulse pressure) will increase
if arterial elastance is high but may not increase
if arterial elastance is low.
INTRACELLULAR
C O M PA RT M E N T
A, In the classic 3-compartment model, fluid administered intravenously administration increases intravascular volume, the volume of blood in the right
distributes from the plasma to the interstitium and from the interstitium to ventricle increases. If the heart is in the ascending part of the curve, the
cells. Filtered fluid returns to the plasma mostly through the lymph system and increased ventricular filling increases cardiac output. If the heart is further to
is eliminated by urine.8,9 The composition of the fluid (ie, colloid vs crystalloid) the right on the curve, further fluid administration may not increase cardiac
and the characteristics of its administration (eg, volume and rate) influence its output. Whether an increase in cardiac output increases arterial blood pressure
movement from the plasma into the interstitium and cells.8 B, In the classic depends on cardiac elastance.
Frank-Starling model of cardiac physiology, when intravenous fluid
included, consisting of 28 randomized clinical trials (RCTs), 7 sec- when the arteries are stiff and noncompliant (high elastance) com-
ondary analyses of RCTs, 20 observational studies, 5 systematic pared with when the arteries are flexible and compliant.11 There-
reviews/meta-analyses, 1 scoping review, and 1 practice guideline. fore, fluid administration may increase a patient’s cardiac output
The remaining 14 references were added from reference review. without increasing blood pressure.
RCTs, including relevant secondary analyses of clinical trial data,
were prioritized for inclusion. Fluid Distribution
Administered fluid distributes initially to the intravascular compart-
ment and then distributes to the interstitial and intracellular
compartments.8 Fluid influx into the interstitial compartment is pri-
Pathophysiology of Fluid Therapy
marily reabsorbed into the circulation through the lymphatic
Multiple physiological pathways responsible for maintaining intra- system.9 Serum oncotic pressure, endothelial integrity, capillary
vascular volume, venous return, cardiac output, and tissue perfu- hydrostatic pressure, fluid infusion rate and volume, and other fac-
sion are disrupted by sepsis. Fluid losses, combined with increased tors affect fluid distribution.8 While hemodynamic improvements
venous capacitance and decreased venous resistance, reduce the (eg, augmented cardiac output, increased arterial blood pressure,
effective intravascular volume in sepsis, which may decrease ve- and improved tissue perfusion) can occur during initial fluid
nous return, cardiac output, and tissue perfusion.6,7 Intravenous (IV) therapy, excessive fluid administration can cause fluid extravasa-
fluid therapy can increase blood volume in the vasculature, the vol- tion and interstitial edema, especially in sepsis. Damage to the vas-
ume of venous blood returning to the heart, the cardiac output, and cular endothelium and the endothelial glycocalyx in sepsis may in-
the volume of oxygen delivered to tissues (Figure 1).8,10 Changes in crease fluid extravasation (Figure 1). Tissue edema due to increased
arterial pressure after fluid administration depend on arterial elas- venous pressure has been associated with organ dysfunction and
tance. A fluid bolus increases blood pressure by a greater amount potential complications12 such as intra-abdominal hypertension
1968 JAMA June 13, 2023 Volume 329, Number 22 (Reprinted) jama.com
© 2023 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a University of Toronto Libraries User on 06/17/2023
Fluid Therapy for Critically Ill Adults With Sepsis: A Review Review Clinical Review & Education
and compartment syndrome.13 Fluid therapy should be tailored to put with passive leg raising identified patients whose cardiac output
maximize early benefits while minimizing adverse effects. would increase with a fluid bolus (positive likelihood ratio, 11 [95% CI,
7.6-17]; specificity, 92%).28 Lack of increase in cardiac output with pas-
Four Forms of Fluid Use sive leg raising identified patients whose cardiac output would not in-
Critically ill patients primarily receive IV fluids in 4 forms: fluid chal- crease with a fluid bolus (negative likelihood ratio, 0.13 [95% CI, 0.07-
lenge, fluid bolus, maintenance or replacement fluid or as part of par- 0.22]; sensitivity of 88%).28
enteral nutrition, and medication diluent or carrier. A fluid chal- For each measure of fluid responsiveness, there are circum-
lenge is the administration of a small volume of IV fluid (eg, 250 mL) stances in which the measure is not valid or reliable (Table 1). Tech-
over a short period (eg, 10 minutes) with the goal of assessing a pa- nical and operator-dependent factors may also affect accuracy and
tient’s physiological response to the fluid such as changes in car- interpretation. Clinicians may select the most suitable method to
diac output, heart rate, arterial blood pressure, or urinary output.14 evaluate fluid responsiveness according to patient characteristics
A fluid bolus is the administration of a larger volume of IV fluid (eg, and resource availability. Although withholding fluid therapy from
500 mL or 1000 mL) over a relatively short period (eg, 15 min- patients expected to be fluid nonresponsive and administering fluid
utes), with the goal of increasing intravascular volume. Mainte- to patients who are expected to be fluid responsive is logical,28 few
nance or replacement fluid is the administration of IV fluid at lower data are available to inform whether this approach improves pa-
rates over longer durations (eg, hours to days) with the aim of pro- tient outcomes. Fluid responsiveness is not, when considered as an
viding daily needs for water, electrolytes, nutrition, and replace- independent factor, a marker of need for fluid therapy in the ab-
ment of measured losses (eg, urine, gastrointestinal, drains). Criti- sence of hypoperfusion.30
cally ill patients also receive substantial volumes of IV fluid as
medication diluent or carrier, for which the goal is to facilitate the Role of Point-of-Care Ultrasonography
administration of medication. Accumulation of fluid administered Point-of-care ultrasound refers to a directed ultrasound examina-
is often an unintended adverse effect.15 tion by the bedside clinician to evaluate for specific life-
threatening abnormalities or diagnostic information. Point-of-care
ultrasound can evaluate the etiology of shock and predict fluid re-
sponsiveness; it facilitates iterative assessment of cardiac func-
Assessment for Fluid Therapy
tion, characterizes preload responsiveness (eg, assessment of stroke
Overview volume changes during passive leg raising), and evaluates patients
Assessing whether IV fluid administration is indicated requires as- for complications of fluid accumulation (eg, assessing for lung
sessment of the patient’s medical history, physical examination, labo- edema31 before administering fluid).
ratory evaluation, and diagnostic imaging (ie, chest radiograph to as- Evaluating inferior vena cava diameter combined with pat-
sess pulmonary edema or point-of-care ultrasound to assess the terns of venous flow in liver and kidneys may identify tissue edema
etiology of shock. Assessment of intravascular volume status and and inform the decision to continue or to withhold fluid therapy.26
the expected response to IV fluid administration can be challenging.4 Abnormalities in flow pattern may differentiate simple fluid accu-
Because markers of hypoperfusion (eg, altered mental status, low mulation from organ dysfunction induced by increased systemic ve-
arterial pressure, cutaneous mottling, slow capillary refill time, low nous pressure. Point-of-care ultrasound may be limited by interop-
urine output, increased lactate) are not specific to hypovolemia, they erator experience and variability, changes in assessment between
must be considered in the clinical context of the patient and not as spontaneous breathing and positive pressure ventilation, and other
stand-alone indications for fluid therapy. technical limitations.26
Assessment of Fluid Responsiveness Fluid Therapy Goals
Scientific investigation has developed and validated objective mea- In addition to fluid therapy directed by fluid responsiveness, other
sures to anticipate a patient’s physiological response to an IV fluid bo- end points for fluid therapy over the course of critical illness have
lus prior to fluid administration.16-28 Each measure assesses cardiac been proposed such as lactate, capillary refill time, and central
preload to distinguish between patients for whom an IV fluid bolus venous saturation (Table 2).32-43 Despite significant research,
would be anticipated to increase stroke volume (and cardiac output optimal outcomes in response to fluid therapy for critically ill
[termed fluid responsive]) from patients for whom an IV fluid bolus patients remain uncertain. Normalizing blood pressure is no longer
would not be anticipated to increase stroke volume (and cardiac out- considered a sufficient goal for resuscitation. Clinicians should
put [termed fluid nonresponsive]) before fluid is administered to be select multiple therapeutic goals for each patient such as normal-
patient. Approximately 57% of patients with sepsis are fluid respon- ization of capillary refill time, lactate clearance, and normalization
sive at presentation.29 Patients with low variation in pulse pressure of urinary output.27
or stroke volume while receiving controlled mechanical ventilation or
those who do not increase cardiac output after a passive leg raising
maneuver (Table 1)16-26 may be considered as fluid nonresponsive.
Administration of Fluid Therapy
These patients would not be expected to increase cardiac output in
response to a fluid bolus. Dynamic measurements such as passive leg Timing of Fluid Administration and Removal
raising or pulse pressure variation, may identify patients who are fluid Fluid therapy for sepsis occurs in 4 phases of critical illness: resus-
responsive more accurately than static measurements, such as mea- citation, optimization, stabilization, and evacuation.10 Each phase
surement of central venous pressure.27 An increase in cardiac out- of therapy is associated with a separate clinical state of the patient,
jama.com (Reprinted) JAMA June 13, 2023 Volume 329, Number 22 1969
© 2023 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a University of Toronto Libraries User on 06/17/2023
Clinical Review & Education Review Fluid Therapy for Critically Ill Adults With Sepsis: A Review
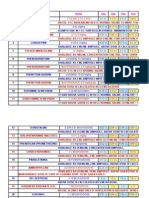
Table 1. Measures and Tests for Identifying Whether a Fluid Challenge Is Likely to Increase Cardiac Output
Normal
Marker Definition range Rationale Comments and application Application
Central venous Estimates the right 5-10 cm H2O Enables measuring vascular system An isolated or static measure of Measures should be
pressure16 atrial pressure and pressure using centrally placed central venous pressure alone may integrated with additional
cardiac preload venous catheters to estimate not reflect whether a patient will be clinical information and the
stressed volume, defined as the responsive to fluid therapy broader context to inform the
volume in the vasculature that value of fluid therapy
exerts stretch on vessel walls
Low values imply patients may
increase cardiac output and other
hemodynamic parameters (eg,
blood pressure) with fluid therapy
Pulmonary Estimates left 4-12 cm H2O Enables measuring vascular system An isolated or static measure of Measures should be
artery occlusion ventricular pressure using centrally placed pulmonary artery occlusion pressure integrated with additional
pressure16 end-diastolic venous catheters to estimate alone may not reflect whether a clinical information and the
pressure or left atrial stressed volume, defined as the patient will be responsive to broader context to inform the
pressure volume in the vasculature that fluid therapy value of fluid therapy
exerts stretch on vessel walls
Low values imply patients may
increase cardiac output and other
hemodynamic parameters (eg,
blood pressure) with fluid therapy
Pulse pressure Indicates the change 10%-15% Pulse pressure (systolic pressure Conditions with which pulse Pulse pressure variation
variation17-20a in pulse pressure minus diastolic pressure)a varies pressure variation may be a less >10%-12% has a sensitivity
that occurs during normally during the respiratory reliable predictor of fluid of 88% and a specificity of
respiration with cycle in patients receiving responsiveness: 89% for predicting fluid
mechanical mechanical (positive pressure) Spontaneous breathing responsiveness
ventilation ventilation due to dynamic changes (false positive) Pulse pressure variation
in intrathoracic pressure >10%-12% threshold would
Cardiac arrhythmias
During positive pressure (false positive) discriminate a greater
ventilation, a larger difference in likelihood of fluid
pulse pressure between inspiration Increased intra-abdominal responsiveness; however,
and expiration are associated with pressure (false positive) different thresholds may be
the following events: Right ventricular dysfunction used in different conditions
A decrease in right ventricular (false positive)
venous return leading to a Low tidal volume or low
decrease in left ventricular filling compliance (false negative)
after a lag of 2-4 heartbeats
An increase in cardiac preload
and output with large pulse
pressure variation in response to
a fluid challenge
Stroke volume Indicates the 10%-13% Large decreases in stroke volume Similar to pulse pressure variation, A value of stroke volume
variation20,21b dynamic change in between expiration and inspiration there are conditions in which stroke variation >12% threshold
left ventricular (>25%) among patients receiving volume variation may be a less may be used to predict fluid
stroke volume positive pressure ventilation reliable predictor of fluid responsiveness
occurring during indicates decreased right ventricular responsiveness: Performance is similar to that
respiration with preload and venous return and Spontaneous breathing of pulse pressure variation
mechanical identifies patients who are more (false positive)
ventilation likely to experience increased
cardiac preload and output in Cardiac arrhythmias
response to a fluid challenge (false positive)
Increased intra-abdominal
pressure (false positive)
Right ventricular dysfunction
(false positive)
Low tidal volume or low
compliance (false negative)
End-expiratory Indicates an Variable Large increases in pulse pressure Like other dynamic maneuvers to A change in pulse pressure
occlusion test22 approximate 15-s (>15%) and cardiac output (>12%) predict fluid responsiveness, the >5% during the
occlusion of the following the end-expiratory end-expiratory occlusion test end-expiratory occlusion test
endotracheal tube in occlusion test predict greater requires patients to receive invasive is associated with an increase
a patient receiving likelihood of responsiveness to a mechanical ventilation in cardiac output with a fluid
mechanical fluid challenge Conditions in which the challenge with a sensitivity
ventilation at end Temporarily augments venous end-expiratory occlusion test may of 87% and a specificity
expiration return, cardiac preload, and stroke be limited or a less reliable of 100%
volume in responsive patients, predictor of fluid responsiveness:
mimicking as a fluid challenge Inability to perform a 15-s
end-expiratory occlusion test in
patients with spontaneous high
work of breather
Low tidal volume or low
compliance (false negative)
(continued)
goals of fluid therapy, assessments performed, and the interven- phases highlight that the approach to fluid therapy changes during
tions delivered (Figure 2 and Table 3). 32,38,39,42,44-49 These a patient’s critical illness and recovery. This conceptual framework
1970 JAMA June 13, 2023 Volume 329, Number 22 (Reprinted) jama.com
© 2023 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a University of Toronto Libraries User on 06/17/2023
Fluid Therapy for Critically Ill Adults With Sepsis: A Review Review Clinical Review & Education
Table 1. Measures and Tests for Identifying Whether a Fluid Challenge Is Likely to Increase Cardiac Output (continued)
Normal
Marker Definition range Rationale Comments and application Application
Passive leg Indicates a dynamic Variable Large increases in pulse pressure or Unlike other dynamic maneuvers to A change in stroke volume
raising20,23 maneuver to assess stroke volume (>10%-15%) predict fluid responsiveness, the >9% and pulse pressure >10%
for changes in following a passive leg raising test passive leg raising test does not during passive leg raising is
cardiac preload and predict greater likelihood of fluid require a patient to receive invasive associated with an increase in
output in response to responsiveness mechanical ventilation cardiac output with a fluid
rapid repositioning Passive leg raising can temporarily Conditions in which passive leg challenge with pooled
of a semirecumbent augment venous return, cardiac raising may not be feasible or is sensitivity of 85% and a
patient to supine preload, and stroke volume in limited to predict fluid specificity of 91%
with both legs raised responsive patients, mimicking as responsiveness:
to 30°-45° a fluid challenge (≈300 mL of Severe hypovolemia
autotransfusion) (false negative)
Raised intra-abdominal pressure
(false negative)
Inability to mobilize or to rapidly
change position in bed
(eg, spinal trauma)
Diminished response with
concomitant use of compression
stockings
May be influenced by operator,
including correct passive leg
raising technique, and cardiac
output assessment
Mini fluid Indicates a dynamic Variable Large increases (>10%) in velocity Unlike other dynamic maneuvers to A change in velocity time
challenge20,24 maneuver in which a time index (an estimate of stroke predict fluid responsiveness, the index >10% in response to a
small volume of fluid volume) following a rapid 100-mL mini does not require a patient to be 100-mL fluid challenge is
( ≈ 100 mL) is given fluid bolus (followed by 400 mL over mechanically ventilated or to associated with an increase in
rapidly over ≈ 1 min 14 min) is predictive of fluid initially receive a large volume cardiac output with a fluid
to predict fluid responsiveness of fluid challenge with a sensitivity of
responsiveness Added considerations in which the 95% and a specificity of 78%
mini may be limited:
Not well validated
Requires administration of
fluid bolus
Requires point-of-care
ultrasound to measure real-time
change in velocity time index
Point-of-care Indicates a directed Variable Estimates the following Advantages: Point-of-care ultrasound is a
ultrasound25,26 ultrasound for parameters: Noninvasive versatile tool that can inform
several parameters Subaortic velocity time index as both fluid responsiveness and
to predict fluid Enables serial assessment fluid intolerance
an estimate of stroke volume
responsiveness and Enables assessment for changes
assess for Assesses left ventricular in response to interventions
complications of end-diastolic volume as an
fluid therapy estimate of preload Contexts in which point-of-care
ultrasound may be limited or less
Assesses the inferior vena cava reliable:
diameter and variation in
inspiratory collapse to predict Operator training for image
fluid responsiveness acquisition and interpretation
(or intolerance) Dynamic measures such as
Assesses lung parenchyma for respiratory variation in inferior
pulmonary edema (eg, B-lines) to vena cava diameter is less reliable
predict fluid intolerance in patients receiving mechanical
ventilation
a
Abbreviations: PPmax, maximum observed difference between systolic and The formula for pulse pressure variation: (PPmax – PPmin)/(PPmax + PPmin)/2.
diastolic pressure; PPmin, minimal difference between systolic and diastolic b
The formula for stroke volume variation (SVmax – SVmin)/(SVmean).
pressure during ventilatory cycle; SVmax, maximum observed difference
between systolic and diastolic stroke volume; SVmin, minimal stroke volume
observed during ventilatory cycle; SVmean, average stroke volume over the
ventilatory cycle.
begins with rapid initial resuscitation, proceeds through optimiza- to fluid resuscitation, sepsis diagnosis and evidence of hypoper-
tion of organ and tissue perfusion, is followed by a phase of physi- fusion should be established. Evidence of hypoperfusion in-
ologic stabilization, and ends with a phase of recovery of organ dys- cludes altered level of consciousness, low arterial blood pres-
function, often characterized by facilitated fluid evacuation.10 sure (typically defined as a mean arterial pressure < 65 mm Hg),
decreased urinary output (< 0.5 mL/kg/h), livedo reticularis, pro-
Resuscitation longed capillary refill time (ⱖ 3 seconds), and elevated serum
In the resuscitation phase, the therapeutic goal is to rapidly re- lactate (> 2 mmol/L) (Table 2).
verse hypoperfusion, with or without hypotension, administering Assessments of fluid responsiveness and diagnostic eval-
fluid boluses (and frequently administering vasopressors). Prior uation of the cause of the hemodynamic abnormality occur in the
jama.com (Reprinted) JAMA June 13, 2023 Volume 329, Number 22 1971
© 2023 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a University of Toronto Libraries User on 06/17/2023
Clinical Review & Education Review Fluid Therapy for Critically Ill Adults With Sepsis: A Review
Table 2. Summary of Measures to Guide Fluid Therapy in Patients With Sepsis
Normal
range
Measure Definition at rest Rationale Comments
Heart rate32 The number of heart 60-100 When blood pressure is low, heart rate Tachycardia may result from factors other than
beats/min beats/min increases to increase cardiac output and hypovolemia (eg, fever) or may not occur when
delivery of oxygen hypovolemia is present (eg, after β-blocker receipt)
Heart rate may return to normal when Heart rate is not a sufficient measure to guide fluid
hypovolemia is corrected therapy for most patients
Mean arterial Average arterial pressure 70-100 Mean arterial pressure is an assessment of Maintaining a mean arterial blood pressure ≥65 mm
blood throughout 1 cardiac mm Hg perfusion of vital organs Hg is recommended for most critically ill adults with
pressure33-35 cycle Perfusion of vital organs decreases with mean sepsis
arterial pressures <60-65 mm Hg A low mean arterial pressure does not accurately
identify patients whose cardiac output will increase
with fluid administration
Cardiac output36 Volume of blood pumped 5-6 L/min Cardiac output determines, in part, the The balance of oxygen supply and demand is more
by the heart/min volume of oxygen delivered to organs and important than absolute values for cardiac output
tissues Even with sufficient cardiac output, disordered
If cardiac output is insufficient to deliver microcirculation in sepsis may impair perfusion
adequate oxygen to tissues, ischemia and RCTs have not found that increasing cardiac output
anaerobic metabolism occur improves outcomes in sepsis
ScvO232,37-39 Hemoglobin saturation of 70%-80% ScvO2 reflects the balance between global RCTs did find using ScvO2 to guide treatment to
blood in the superior oxygen delivery and global oxygen improve outcomes in sepsis
vena cava consumption Measuring ScvO2 requires a central venous catheter
Low values suggest that increasing the Low values of ScvO2 may identify patients with
delivery of oxygen to tissues may be inadequate oxygen delivery, and high values may
beneficial identify patients with impaired oxygen extraction
Central venous Blood pressure in the 5-10 cm Central venous pressure has been used as a Central venous pressure does not accurately identify
pressure32,37-39 vena cava near the right H20 surrogate measure for right atrial pressure, patients who will experience an increase in cardiac
atrium right-ventricular end-diastolic pressure, and output with fluid administration
cardiac preload RCTs did not find using central venous pressure to
guide fluid therapy to improve outcomes in sepsis
40
Urine output Volume of urine 0.5-1.5 Urine output may be a surrogate measure of Urine output is influenced by factors other than
produced over a time mL/kg/h the perfusion of the kidney perfusion of the kidney, including microvascular
interval changes and the development of acute tubular
necrosis
Fluid administration that increases cardiac output
and organ perfusion may not increase urine output
Blood lactate Concentration of lactate 1 to 2 Increased lactate levels may indicate Elevated lactate levels in sepsis frequently occur
levels41,42 in the blood mmol/L inadequate oxygen delivery from insufficient despite adequate oxygen delivery to tissues
cardiac output or blood oxygen content Although decreasing lactate identifies patients likely
to experience better outcomes, RCTs did not find
using lactate clearance to guide resuscitation
improved outcomes in sepsis
Cutaneous Time required for return ≤3 s Capillary refill time measures peripheral Capillary refill time is an inexpensive and universally
capillary refill of color after application perfusion, reflects coupling between the available test of peripheral perfusion
time42,43 of pressure to a capillary macrocirculation and microcirculation, and An RCT found outcomes of sepsis to be at least as
bed responds rapidly to fluid resuscitation good with use of capillary refill time compared with
lactate clearance to guide fluid therapy
Abbreviations: RCT, randomized clinical trial; ScvO2, central venous oxygen saturation.
resuscitation phase. In the resuscitation phase, fluid therapy is associated with lower mortality (among 49 331 patients, the longer
typically continued until the patient’s mean arterial pressure no the time to complete the 3-hour bundle, the higher the in-hospital
longer increases with IV fluid administration, goals of resuscita- mortality; odds ratio, 1.04 per hour [95% CI, 1.02-1.05]; P < .001);
tion are attained, the patient’s condition is no longer immediately however, time completion of initial fluid bolus was not associated
life threatening, or complications of fluid therapy arise (eg, wors- with lower mortality (odds ratio, 1.01 per hour [95% CI, 0.99-1.02];
ening hypoxemia). P = .21).50
Optimal fluid therapy in the resuscitation phase has been in-
Early Fluid Therapy and Early Goal-Directed Therapy formed by RCTs to define early goal-directed therapy (EGDT). EGDT
Evidence for early fluid therapy immediately after sepsis diagnosis is defined by a specific approach to managing sepsis-induced hy-
is limited. An RCT of 3141 children (median age, 2 years) presenting poperfusion, which includes administering IV fluid boluses to achieve
with acute infection reported that, compared with no IV fluid bo- a central venous pressure of 8 to 12 mm Hg, vasopressors to achieve
lus, the mortality was higher among patients randomized to re- a mean arterial blood pressure of 65 to 90 mm Hg, and red blood
ceive IV fluid boluses of either 0.9% saline or albumin. Mortality rates cell transfusions and/or inotropes to achieve a central venous oxy-
were 12.0% with albumin, 12.2% with 0.9% saline, and 8.7% for gen saturation of at least 70%.32,37-39
those who received no IV fluid (P = .004).44 An administrative data In an RCT of 263 patients with sepsis-induced hypoperfusion
analysis reported that adherence to a 3-hour bundle of sepsis man- in an urban emergency department,26 compared with a control
agement (blood cultures, antibiotics, and lactate measurement) was group, EGDT reduced hospital mortality (30.5% vs 46.5%; P = .009).
1972 JAMA June 13, 2023 Volume 329, Number 22 (Reprinted) jama.com
© 2023 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a University of Toronto Libraries User on 06/17/2023
Fluid Therapy for Critically Ill Adults With Sepsis: A Review Review Clinical Review & Education
However, in an individual patient-level meta-analysis that com-
Figure 2. Timing of Fluid Administration and Removal
bined results from 3 subsequent international RCTs (3723 patients
in 138 hospitals) of patients who already received initial fluids, EGDT
Critically ill with sepsis
was not associated with improved 90-day mortality compared with
usual care (EGDT, 24.9% vs usual care, 25.4%; P = .68).51 It remains
unclear whether care bundles that include fluid therapy and other 1 Resuscitation - Administer fluids to reverse hypoperfusion
sepsis interventions improve outcomes.33,50,52,53 Establish diagnosis of sepsis and hypoperfusion.
POTENTIAL REGRESSION THROUGH PHASES
An open-label RCT compared restrictive vs liberal fluid therapy Administer initial fluid boluses.
among 1563 patients with sepsis-induced hypotension who had re- Administer vasopressors if necessary (eg, norepinephrine, vasopressin).
Assess responsivenss to fluids and treat infection.
ceived an average of 2 L of fluid prior to enrollment.47 In the restric-
tive group, hypotension was treated with vasopressors, and addi-
tional fluid was administered only for select indications. In the liberal 2 Optimization - Establish perfusion to organs and tissues
group, hypotension was treated with fluid administration, and va- Consider risks and benefits of additional fluid administration based on
sopressors were administered only for select indications. The me- responsiveness to fluids and signs of hypoperfusion.
dian volume of IV fluid received in the first 24 hours was 1.2 L in the Titrate vasopressors and inotropes for specific hemodynamic targets
(eg, lactate, capillary refill time).
restrictive group and 3.4 L in the liberal group. All-cause mortality
before discharge home by day 90 did not significantly differ be-
tween the restrictive fluid group (14.0%) and the liberal fluid group 3 Stabilization - Maintain perfusion
(14.9%) (P = .61).47 Monitor for fluid overload and associated organ dysfunction.
RCTs in low- and middle-income countries compared adminis- Assess and treat any organ dysfunction.
tration of IV fluid vs no fluid for acutely ill children and adults pre- Consider a restrictive approach that limits additional fluids.
Monitor capillary refill time, lactate, and other perfusion markers.
senting with hypoperfusion from infection. An RCT of 209 adults
with sepsis in Zambia reported significantly higher mortality in
patients randomized to receive IV fluid vs vasopressors as part of 4 Evacuation - Facilitate recovery and removal of excess fluid
an EGDT protocol compared with usual care (48.1% vs 33.0%)
Consider removal of excess fluid accumulated during critical illness
(P = .03).45 An RCT of 424 patients with early septic shock in 5 using diuresis or kidney replacement therapy if indicated.
countries (Argentina, Chile, Colombia, Ecuador, and Uruguay) that Initiate early rehabilitation, mobilization, and nutrition plans.
compared use of lactate levels vs capillary refill time to guide fluid
therapy found no statistically significant difference in mortality by
day 28 between the 2 groups (34.9% in the capillary refill time Discharge from hospital
group vs 43.4% in the lactate clearance group (P = .06).42 How-
Steps indicate fluid therapy across the conceptual phases of critical illness.
ever, a secondary bayesian analysis suggested probable benefit for
Patients may progress linearly through the 4 phases or may move back and
capillary refill time–guided resuscitation (odds ratio for 28-day mor- forth between phases.
tality, 0.65 [95% credible interval, 0.43-0.96]; 98% probability of
benefit).43 fluid was administered as long as patients experienced hemody-
Together, these results suggest that, for patients with sepsis who namic improvement. At 90-day follow-up, mortality did not differ
have received 1 to 3 L of fluid, early goal-directed therapy targeting between groups (restrictive [42.3%] vs standard [42.1%]; P = .96).
central venous pressure, mean arterial pressure, and central venous Secondary outcomes, including kidney injury; cerebral, myocardial,
oxygen saturation may not improve outcomes and that outcomes may intestinal, or limb ischemia; and number of days alive and out of the
be similar between an approach that prioritizes additional fluid ad- hospital were similar between groups. Variability between the trials
ministration and one that prioritizes use of vasopressors. in the definitions of restrictive or liberal fluid management, markers
of hypoperfusion, and the indications for fluid therapy made it diffi-
Optimization and Stabilization Phases cult to develop a single best approach to fluid therapy among
The optimization phase has the goal of attaining perfusion to patients with critical illness. A reasonable approach is to limit fluid
organs and tissues, and the stabilization phase has the goal of administration to patients’ objective markers of hypoperfusion and
maintaining homeostasis and facilitating organ dysfunction resolu- fluid responsiveness.27
tion. Few RCTs have studied fluid therapy during these phases. The
CLASSIC trial46 compared restrictive vs standard fluid management Evacuation
following initial resuscitation in 1554 critically ill adults. Investiga- Evacuation is the last phase of fluid therapy. Critically ill adults with
tors hypothesized that a more restrictive approach, with fluid sepsis may experience edema and organ failure due to excess accu-
boluses limited to patients with markers of severe hypoperfusion, mulation of fluids administered during critical illness15 and reduced
would improve 90-day mortality by avoiding unnecessary fluid capacity for fluid elimination (eg, due to acute kidney injury). Daily
accumulation. The restrictive strategy, in which fluid boluses were documentation of fluid intake, output, balance, and weights, and set-
allowed only for lactate level above 4 mmol/L, mean arterial pres- ting specific goals for fluid management may help clinicians prevent
sure below 50 mm Hg, mottling beyond the edge of the kneecap, adverse outcomes due to fluid accumulation such as acute kidney in-
or diuresis of less than 0.1 mL/kg/hour during first 2 hours after ran- jury, abdominal compartment syndrome, and mortality.12,13 During re-
domization, resulted in 1627 mL less IV fluid administration through covery from critical illness, patients may spontaneously excrete ex-
day 5 of ICU admission compared with the liberal group, in which cess accumulated fluid. For some patients, facilitating fluid removal
jama.com (Reprinted) JAMA June 13, 2023 Volume 329, Number 22 1973
© 2023 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a University of Toronto Libraries User on 06/17/2023
Clinical Review & Education Review Fluid Therapy for Critically Ill Adults With Sepsis: A Review
Table 3. Summary of Randomized Clinical Trials of Fluid Therapy in Critical Illness According to Resuscitation Phases
and Their Implications for Practice
Trial source by
phase of therapy Population
considered and location Setting Hypothesis Fluid management Results Implications
Resuscitation phase
FEAST 3141 Children 6 Centers: Kenya Fluid bolus Intervention 1 Higher 48-h mortality In a specific population,
Maitland et al,44 with severe (1), Tanzania (1), would improve Administering with any fluid bolus fluid bolus increased short
2011 febrile illness Uganda (4) 48-h mortality 20 mL/kg of 0.9% (relative risk, 1.45 term mortality
saline in 1 h [95% CI, 1.13-1.86];
P = .003)
Intervention 2
Cardiovascular collapse
Administering was the most common
20 mL/kg of 5% mortality cause
albumin in 1 h
Control
No bolus
Additional bolus allowed
in intervention groups
ProCESS 1351 Patients 31 Hospitals in EGDT would Intervention 1 Median fluid use of 2.8 L This trial did not support
Yealy et al,32 with sepsis and the United States improve Traditional EGDT (as in in EGDT group, 3.3 L in EGDT or a modified EGDT
2014 hypotension in-hospital Bentzer et al28); fluid modified (protocol-based) approach in sepsis patients
refractory to mortality given in 500-mL bolus group, and 2.3 L in control and could not confirm
≥1000 mL of truncated at 60 d until central venous group in the first 6 h previous results
initial bolus pressure is >8 mm Hg Mortality was similar in
Intervention 2 protocolized groups when
compared with standard
500- to 1000- mL fluid of care (relative risk, 1.04
bolus until systolic [95% CI, 0.82-1.31];
blood pressure is P = .83)
>100 mm Hg, or shock
index is <0.8 or signs of Patients in the EGDT
fluid overload group were more
frequently admitted to
Control the ICU
Fluid therapy as per
clinician’s discretion
until signs of fluid
overload
ProMISe 1260 Patients 56 Hospitals in EGDT would Intervention Median fluid use of 1750 This trial could not find a
Mouncey et al,38 with sepsis, signs England reduce 90-d Traditional EGDT (as in mL in EGDT group, 1500 benefit of EGDT therapy
2015 of systemic mortality Bentzer et al28); fluid mL in control group in the
inflammatory given in 500 mL over first 6 h
response 20-min bolus until No found differences in
syndrome, and central venous pressure outcome with EGDT
refractory is >8 mm Hg (relative risk, 1.01
hypotension to [95% CI, 0.85-1.20];
initial 1000-mL Control
P = .90)
fluid boluses Fluid therapy as per
clinician’s discretion
until signs of fluid
overload
ARISE 1600 Patients 51 Hospitals: EGDT would Intervention Mean fluid use in the first 6 This trial did not find a clear
Peake et al,39 with sepsis Australia (42), reduce 90-d Traditional EGDT (as in h was slightly higher in benefit of EGDT, but all
2014 defined as Finland (2), mortality Bentzer et al28); fluid EGDT than control groups patients used fluids before
ProCESS Hong Kong (3), given in 500-mL bolus (1964 vs 1713 mL) enrollment
Ireland (1), until central venous
New Zealand (3) pressure is >8 mm Hg or
>12 mm Hg if patient is
on noninvasive or
invasive ventilation
Control
Fluid therapy as per
clinician’s discretion
(continued)
through pharmacologic (eg, diuretics) or mechanical (eg, kidney re- more days alive (mean [SD] 14.6 [0.5] days vs 12.1 [0.5] days for the
placement therapy) approaches may be necessary. liberal group; P < .001) and were free of mechanical ventilation at
A clinical trial of 1000 mechanically ventilated patients with 60 days, and they had more days not spent in the ICU at 60 days
acute lung injury following initial resuscitation48 reported that when (13.4 [0.4] days vs 11.2 [0.4] days for the liberal group; P < .001). The
compared with conservative fluid management, liberal fluid man- GODIF trial compared furosemide titration to attain a net negative
agement increased fluid accumulation by approximately 7 L over 7 fluid balance with standard of care.49 The clinical trial was stopped
days (P < .001), but there was no significant difference in mortality early due to imprecise fluid balance assessment, underscoring chal-
between the 2 groups (conservative [25.5%] vs liberal [28.4%]; lenges in testing this scientific question. The protocol was altered,
P = .30). Patients in the conservative fluid management group had and a second phase of the trial was continued.
1974 JAMA June 13, 2023 Volume 329, Number 22 (Reprinted) jama.com
© 2023 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a University of Toronto Libraries User on 06/17/2023
Fluid Therapy for Critically Ill Adults With Sepsis: A Review Review Clinical Review & Education
Table 3. Summary of Randomized Clinical Trials of Fluid Therapy in Critical Illness According to Resuscitation Phases
and Their Implications for Practice (continued)
Trial source by
phase of therapy Population
considered and location Setting Hypothesis Fluid management Results Implications
Simplified 209 Adult 1 Center in An EGDT in a Intervention Intervention group A more aggressive fluid
Severe Sepsis patients with Zambia resource- 2.0 L Bolus in 1 h received 3.5 L resuscitation strategy with
Protocol 2 sepsis and constrained followed by additional (IQR, 2.7-4.0 L) vs 2.0 L blunt limits for fluid loading
Andrews et al,45 hypotension scenario would ≤2.0 L over 4 h; fluids (IQR, 1.0-2.5 L) in the results in worse outcomes
2017 improve withheld if arterial control group in this population
outcomes oxygen saturation Hospital mortality was
decreased by 3% or higher in intervention
respiratory rate group (relative risk, 1.46
increased by 5 or [95% CI, 1.04-2.05];
jugular venous pressure P = .03)
reached 3 cm or above
the sternal angle
Control
Usual care
Resuscitation + optimization phases
ANDROMEDA- 424 Patients 26 ICUs in Capillary refill For both groups, fluid The capillary refill-guided Capillary refill time–guided
SHOCK with early septic Argentina, Chile, time–guided boluses were only used if group received 2359 mL therapy might be superior to
Hernández shock Colombia, therapy would signs of preload vs 2767 mL in the control lactate-guided therapy and
et al,42 2019 Septic shock was Ecuador, improve responsiveness using (lactate clearance) group may result in lower amounts
defined as Uruguay outcomes in dynamic parameters Survival at day 28 was of fluid being used
suspected or patients with suggested patients were similar between groups
confirmed septic shock fluid responsive (hazard ratio, 0.75
infection, plus (28-d mortality) At least 57% of all [95% CI, 0.55-1.02];
hyperlactatemia patients were fluid P = .06), although a
(≥2.0 mmol/L) responsive at enrollment; bayesian reanalysis
and the protocol also included suggested a high
requirements of vasopressor and inodilator probability of overall
vasopressors to test use for some benefit43
maintain a mean scenarios31
arterial pressure
of 65 mm Hg
after an
intravenous
fluid load of
≥20 mL/kg over
60 min
Resuscitation + optimization + stabilization phases
CLASSIC 1554 Patients 31 ICUs in A restrictive Restrictive group Both groups received A restrictive strategy was
Meyhoff et al,46 with septic shock Belgium, the fluid therapy Fluid given only if approximately 3 L of not superior to a standard
2022 (sepsis, lactate Czech Republic, approach would severe hypoperfusion fluids before enrollment fluid regimen in this large
>2 mmol/L, need Denmark, Italy, be associated (lactate >4 mmol/L, Median intravenous fluid multicenter trial
for vasopressors Norway, Sweden, with 7% lower mean arterial pressure use at day 5 after
with ≥1 L of Switzerland, 90-d mortality <50 mm Hg, mottling enrollment was 1450 mL
fluid use) United Kingdom compared with beyond the edge of the in the restrictive vs 3077
standard care kneecap, diuresis of mL in the standard group
< 0.1 mL/kg/h during The trial had neutral
first 2 h after results for 90-d mortality
randomization was (relative risk, 1.00
present (recommended [95% CI 0.89-1.13])
bolus of 250-500 mL);
fluids to replenish
losses were allowed
Standard group
Fluid prescribed while
patients improved with
fluid challenges
Fluid strategies were
applied for ≤90 d after
enrollment
(continued)
Results of RCTs have been conflicting regarding kidney replace- tiating therapy only when urinary output was less than 0.3 mL/kg/
ment therapy for removing excess fluid. In a 231-patient single- hour for at least 24 hours and/or a greater than 3-fold increase in se-
center RCT, mortality was lower with early kidney replacement rum creatinine level compared with baseline or a serum creatinine
therapy (39.3%) vs with late kidney replacement therapy (54.7%) level of greater than or equal to 4 mg/dL and/or with an acute in-
at 90-day follow-up (P = .03).54 In this trial, early kidney replace- crease of at least 0.5 mg/dL within 48 hours or urgency for kidney
ment therapy was defined as kidney replacement therapy initiated replacement therapy such as refractory hypervolemia or hyperka-
if urinary output was less than 0.5 mL/kg/hour for at least 12 hours lemia among others (54.7%; P = .03 at 90-day follow-up).54
or if there was a 2-fold increase in serum creatinine level compared However, these results were not confirmed in 3 larger multi-
with baseline. Late kidney replacement therapy was defined as ini- center trials.55-58 In the AKIKI trial (620 patients including 484
jama.com (Reprinted) JAMA June 13, 2023 Volume 329, Number 22 1975
© 2023 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a University of Toronto Libraries User on 06/17/2023
Clinical Review & Education Review Fluid Therapy for Critically Ill Adults With Sepsis: A Review
Table 3. Summary of Randomized Clinical Trials of Fluid Therapy in Critical Illness According to Resuscitation Phases
and Their Implications for Practice (continued)
Trial source by
phase of therapy Population
considered and location Setting Hypothesis Fluid management Results Implications
CLOVERS 1563 Patients 60 Centers in the A restrictive fluid Restrictive group Median volume of fluid in For patients with sepsis and
Shapiro et al,47 with United States therapy would be Maintenance fluids the 24 h after enrollment continued hypotension after
2023 sepsis-induced associated with discontinued, no was 1.2 L in the 1-2 L of intravenous fluid,
hypotension lower 90-d further fluid boluses conservative group and an approach that limits fluid
despite receiving mortality administered except for 3.4 L in the liberal group and prioritizes vasopressors
1-3 L of select indications, (difference, −2.1 L) and an approach that
intravenous fluid vasopressors Trial was halted for futility prioritizes additional fluid
administered for administration produced
Death by day 90 did not similar patient outcomes
hypotension differ between the
Liberal group restrictive (14.0%) and
2 L of additional liberal (14.9%) groups
boluses were No secondary outcomes
administered with use differed between groups
of vasopressors only if
select were criteria met
Evacuation phase
FACTT 1000 patients 20 Centers in the A conservative Liberal Patients in the This was the first trial to
Wiedemann receiving United States fluid strategy Static preload conservative group had a show an improvement in
et al,48 2006 mechanical and Canada would improve measurements (central neutral fluid balance at respiratory organ
ventilation with 60-d mortality venous pressure or day 7, while patients in dysfunction with a clinically
acute lung injury pulmonary artery the liberal group were on relevant end point
occlusion pressure) average approximately 7 L A neutral fluid balance was
were kept at higher positive achieved without an
values Mortality at day 60 was increase in other organ
Conservative not significantly different dysfunctions including
between fluid shock or receipt of kidney
Lower values of static management strategies replacement therapy
preload measurements
were triggers for The conservative strategy
furosemide use was associated with an
increase in the mean (SD)
For both groups, number of ventilator-free
furosemide was titrated to days (14.6 [0.5] vs 12.1
achieve intravascular [0.5]; P < .001) and
pressure goals ICU-free days (13.4 [0.4]
Furosemide was not used vs 11.2 [0.4]; P < .001)
if patients were being There was no increase in
treated with vasopressors receipt of kidney
or had poor tissue replacement therapy
perfusion
GODIF Recruitment First protocol Furosemide will Placebo vs furosemide First version halted at 41 The second protocol version
Wichmann follows on a version was increase days infusion to obtain patients due to protocol is ongoing
et al,49 2023 second protocol halted after 41 alive and days negative fluid balance violations due to
version; includes patients of 1000 outside the toward neutralization of perceived imprecision in
Second patients with planned at 3 ICUs hospital at 90 d positive fluid balance recording of fluid balances
version fluid in Denmark
ongoing Updated trial is enrolling
accumulation patients
assessed by net
fluid balance
according to
weight at the
time of
enrollment
Abbreviations: EGDT, early goal-directed therapy; ICU, intensive care unit.
patients with sepsis), 60-day mortality was not different be- (net ultrafiltration <1 mL/kg/hour) and rapid (net ultrafiltration
tween early vs delayed kidney replacement treatment (48.5% vs >1.75 mL/kg/hour) fluid removal with kidney replacement therapy,
49.7%; P = .79).55 In the IDEAL-ICU trial (488 patients with sep- compared with moderate-rate fluid removal (1.01-1.75 mL/kg/
sis) mortality was 58% in the early-strategy group vs 54% in the hour), may be associated with higher mortality and longer duration
delayed-strategy group at 90 days (P = .38).56 In the STARRT-AKI of kidney replacement therapy.59 The optimal rate and duration of
international RCT (3019 patients with acute kidney injury of fluid removal by kidney replacement therapy during the later phases
whom 57.7% had sepsis), 90-day mortality was 43.9% in the of critical illness remains unclear.
early (accelerated-strategy) group and 43.7% in the standard-
strategy group (P = .92).57 Kidney replacement therapy among Selecting Fluid Type
survivors was higher in the accelerated-strategy group (10.4% IV fluid solutions may be classified as crystalloid solutions (which con-
vs 6.0%). tain water and electrolytes) or colloid solutions (which contain wa-
In summary, among patients without acute respiratory dis- ter, electrolytes, and a larger compound). The most common crys-
tress syndrome, RCTs did not support early (or accelerated) kid- talloid solutions are 0.9% sodium chloride (saline) and balanced or
ney replacement therapy to remove fluid. Furthermore, both slow buffered crystalloid solutions, such as Ringer lactate.
1976 JAMA June 13, 2023 Volume 329, Number 22 (Reprinted) jama.com
© 2023 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a University of Toronto Libraries User on 06/17/2023
Fluid Therapy for Critically Ill Adults With Sepsis: A Review Review Clinical Review & Education
Crystalloid Solutions
Two classes of isotonic crystalloid solutions exist: 0.9% sodium chlo- Box. Common Questions Regarding Fluid Therapy
ride (saline) and balanced crystalloid solutions, in which chloride is for Critically Ill Patients With Sepsis
replaced with a buffer such as lactate, gluconate, or acetate to pre-
vent hyperchloremic metabolic acidosis. Multiple large, interna- When Should Fluid Therapy Be Considered for Patients With Sepsis?
Fluid therapy should be initiated for patients with evidence of
tional RCTs have compared balanced solutions vs saline for fluid re-
sepsis-induced hypoperfusion (altered mental status, low arterial
suscitation in critically ill patients.60-63 Among 2278 ICU patients in blood pressure, reduced urinary output, abnormal capillary refill
the SPLIT trial (of whom only 77 had sepsis), acute kidney injury oc- time) who are likely to have increased cardiac output with fluid
curred in 9.6% of patients in the balanced crystalloid group and 9.2% administration. Fluid administration should be discontinued when
of patients in the 0.9% saline group (P = .77).60 Among 15 802 criti- evidence of hypoperfusion resolves, the patient no longer
cally ill adults at a single academic institution in the SMART trial,61 responds to fluid, or the patient shows evidence of fluid overload.
rates of death, kidney replacement therapy, or persistent kidney dys- What Type of Fluid Should Be Used?
function was 14.3% in the balanced crystalloid group vs 15.4% in the Balanced solutions (eg, Ringer lactate, Ringer acetate, Plasma
0.9% saline group (P = .04). In a secondary analysis of the SMART Lyte) should be selected over 0.9% saline for fluid therapy in
trial among the 1641 patients with sepsis,64 30-day in-hospital mor- patients with sepsis. Hydroxyethyl starches should not be used for
patients with sepsis.
tality was 26.3% in the balanced crystalloids group and 31.2% in the
0.9% saline group (P = .01).64 Among 10 520 critically ill adults in When Should Fluid Removal Be Considered, and How Should Fluid
the BaSICS trial, there was no difference in 90-day mortality be- Be Removed?
tween patients randomized to receive balanced crystalloid solu- Fluid removal should be considered after the resuscitation and
tion (26.4%) and patients randomized to receive 0.9% saline (27.2%) optimization phases and when a patient has stabilized
(eg, decreasing vasopressor doses, adequate peripheral
(adjusted hazard ratio, 0.97 [95% CI, 0.90-1.05]), and 90-day mor-
perfusion). Diuretics are first-line therapy to facilitate elimination
tality among patients with sepsis was 46.7% in the balanced crys- of fluid. Kidney replacement therapy may be considered for
talloids group and 49% in the saline group.62 Among 5037 criti- patients with severe acute kidney injury who have complications
cally ill adults in the PLUS trial, there was no difference in 90-day from fluid overload are unresponsive to diuretic therapy.
mortality between patients in the balanced crystalloids group and
patients in the 0.9% saline group (21.8% vs 22.0%; difference, −0.2
percentage points [95% CI, −3.6 to 3.3]).63 Among patients with sep-
sis, mortality at 90 days was not significantly different between the sepsis.69-71 In an RCT of 537 patients with sepsis, compared with crys-
balanced crystalloid and saline groups. talloid therapy (lactated Ringer), hydroxyethyl starch increased the
A meta-analysis of 34 450 patients in 6 low-risk of bias RCTs re- incidence of acute kidney injury (22.8% vs 34.9%; P = .002).69 In
ported in a frequentist analysis that the relative risk for 90-day mor- an RCT of 804 patients with sepsis or septic shock, compared with
tality was 0.96 (95% CI, 0.91-1.01) for balanced solutions com- Ringer acetate, hydroxyethyl starch increased mortality at 90 days
pared with saline.65 In bayesian analysis, the probability that balanced (51% vs 43%; P = .03).70 In an RCT of 7000 ICU patients, com-
crystalloids decreased mortality compared with saline was 89.5%. pared with saline, hydroxyethyl starch significantly increased need
Among 6754 patients with sepsis from 5 RCTs, there was no differ- for kidney replacement therapy (7.0% vs 5.8%; P = .04)71; in the sub-
ence in mortality between a balanced crystalloid group and a saline group of 1921 patients with sepsis in this trial, compared with sa-
group (31.3% vs 33.9%; relative risk, 0.93 [95% CI, 0.86-1.01]).65 In line, hydroxyethyl starch did not increase mortality (25.4% mortal-
a preplanned subgroup analysis (BASICS trial), balanced crystal- ity for hydroxyethyl starch and 23.7% for saline; risk ratio, 1.07
loids increased mortality in 483 patients with traumatic brain in- [95% CI, 0.92-1.25]; P = .38).71 In summary, hydroxyethyl starch
jury (odds ratio, 1.48; 95% credible interval, 1.04-2.09).66 It is con- should not be administered to patients with sepsis.
ceivable that balanced crystalloid solutions attain outcomes that are
at least as good as for saline in patients with sepsis. Infusion Rate
A systematic review that included 3601 patients in 85 studies re-
Colloid Solutions ported that a rapid infusion rate (<30 minutes) was associated with
Human albumin is the most frequently used colloid in ICU settings. higher probability of increasing stroke volume or cardiac output in re-
An RCT of 6997 critically ill patients that included 1218 patients with sponse to fluid administration, likely by more effectively increasing
sepsis reported that compared with saline, albumin did not reduce venous return and preload.72 The volume of fluid use was less than
mortality (20.7% for albumin vs 20.8% for saline; P = .87).67 Re- 500 mL in 12.7% of the trials, 500 mL in 79.4% of the studies, and
sults for mortality were similar in the subgroup of patients with sep- more than 500 mL in 7.9% of the reports. An RCT involving 10 520
sis (30.7% for albumin vs 35.3% for saline; P = .09). An RCT of 1818 critically ill patients requiring IV fluid therapy compared infusion at a
ICU patients with sepsis found that mortality at 28-day follow-up was slower rate (333 mL/hour) vs a faster rate (999 mL/hour).73 Mortal-
not significantly different between patients who received albumin ity rates were 26.6% in the group that received a slower infusion and
(31.8%) compared with patients who received crystalloid solutions 27.0% in the faster infusion group (P = .46). In a post hoc analysis,
(32.0%) (P = .94).68 The role of albumin in sepsis treatment, if any, faster infusion rates were associated with benefit in a subgroup that
is presently unclear. included patients with sepsis (odds ratio for mortality, 0.72 [95% cred-
In multiple RCTs, semisynthetic colloid solutions such as hy- ible interval, 0.54-0.91]; probability of benefit >0.99).74 The effects
droxyethyl starch were associated with increased rates of acute kid- of different infusion rates on outcomes in critically ill patients with sep-
ney injury, kidney replacement therapy, and death in patients with sis remain unclear.75
jama.com (Reprinted) JAMA June 13, 2023 Volume 329, Number 22 1977
© 2023 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a University of Toronto Libraries User on 06/17/2023
Clinical Review & Education Review Fluid Therapy for Critically Ill Adults With Sepsis: A Review
sion),toharm(eg,abdominalcompartmentsyndrome).Balancedcrys-
Applying Evidence, Uncertainties, talloids are a reasonable initial IV fluid for patients with sepsis, but bal-
and Future Directions anced crystalloids should be avoided in patients with traumatic brain
injury. Hydroxyethyl starch, a semisynthetic colloid solution, should
When treating a patient with sepsis, clinicians must evaluate ben- be avoided in patients with sepsis.
efits and risks of fluid therapy in each phase of critical illness (Box).
Decisions regarding fluid management require consideration of the
patient’s acute conditions and chronic comorbidities that may in- Limitations
fluence measures of fluid responsiveness (eg, right ventricular fail- This review has several limitations. First, the literature search may
ure) or the patient’s ability to receive fluid without developing com- have missed some relevant research articles. Second, quality of in-
plications from fluid therapy (eg, end-stage kidney disease)76 cluded articles was not formally evaluated. Third, the trials re-
(Table 1). Information about the patient’s condition should be inte- viewed were heterogeneous and several definitions such as restric-
grated with evidence that informs which fluid therapies improve pa- tive, liberal, and early may impair interpretation of the results.
tient outcomes.
Based on current evidence, critically ill patients with sepsis should
typically receive fluid as therapy for expansion, maintenance, or medi- Conclusion
cation administration. Administration of additional IV fluid and the
amount of fluid to administer should be based on medical history, Fluid therapy is an important component of treating patients who
physical examination, laboratory studies, and imaging along with the are critically ill with sepsis. Although optimal fluid management in
patient’s phase of illness and measures of fluid responsiveness. Effects patients with sepsis remains uncertain, clinicians should consider the
of fluid restriction have ranged from benefit (eg, shorter duration risks and benefits of fluid administration in each phase of critical ill-
of ventilation in acute respiratory distress syndrome), to no effect ness, avoid use of hydroxyethyl starch, and facilitate fluid removal
(eg, no evidence of effect on mortality in sepsis-induced hypoten- for patients recovering from acute respiratory distress syndrome.
ARTICLE INFORMATION PREvalence Assessment Database, SPREAD): an Med. 2015;41(7):1247-1255. doi:10.1007/s00134-
Accepted for Publication: May 7, 2023. observational study. Lancet Infect Dis. 2017;17(11): 015-3898-7
1180-1189. doi:10.1016/S1473-3099(17)30322-5 12. Finfer S, Myburgh J, Bellomo R. Intravenous fluid
Conflict of Interest Disclosures: Dr Zampieri
reported other from Baxter Hospitalar (provision of 3. Vincent JL, Sakr Y, Singer M, et al; EPIC III therapy in critically ill adults. Nat Rev Nephrol. 2018;14
fluids and logistics for the BaSICS trial) during the Investigators. Prevalence and outcomes of (9):541-557. doi:10.1038/s41581-018-0044-0
conduct of the study; personal fees from infection among patients in intensive care units in 13. Jacobs R, Wise RD, Myatchin I, et al. Fluid
Bactiguard (statistical consulting) and Baxter 2017. JAMA. 2020;323(15):1478-1487. doi:10.1001/ management, intra-abdominal hypertension and
(advisory board); grants from Ionis Pharmaceuticals jama.2020.2717 the abdominal compartment syndrome: a narrative
(to his institution for investigator initiated trials) 4. Myburgh JA, Mythen MG. Resuscitation fluids. review. Life (Basel). 2022;12(9):1390. doi:10.3390/
outside the submitted work; and serving as lead N Engl J Med. 2013;369(13):1243-1251. doi:10.1056/ life12091390
investigator of the BaSICS trial. Dr Bagshaw NEJMra1208627 14. Cecconi M, Parsons AK, Rhodes A. What is a
reported personal fees (advisory board) from 5. Malbrain MLNG, Langer T, Annane D, et al. fluid challenge? Curr Opin Crit Care. 2011;17(3):290-
Baxter during the conduct of the study; personal Intravenous fluid therapy in the perioperative and 295. doi:10.1097/MCC.0b013e32834699cd
fees from BioPorto (funding for clinical critical care setting: executive summary of the
adjudication) and Novartis (advisory board) outside 15. Van Regenmortel N, Verbrugghe W, Roelant E,
International Fluid Academy (IFA). Ann Intensive Care. Van den Wyngaert T, Jorens PG. Maintenance fluid
the submitted work; and serving as lead 2020;10(1):64. doi:10.1186/s13613-020-00679-3
investigator of the STARRT-AKI trial. Dr Semler therapy and fluid creep impose more significant
reported grants from the National Heart Lung and 6. Russell JA, Rush B, Boyd J. Pathophysiology of fluid, sodium, and chloride burdens than
Blood Institute (K23HL143053) and personal fees septic shock. Crit Care Clin. 2018;34(1):43-61. doi: resuscitation fluids in critically ill patients:
from Baxter International (advisory board) during 10.1016/j.ccc.2017.08.005 a retrospective study in a tertiary mixed ICU
the conduct of the study; personal fees from Aerpio 7. Hochman JS. Cardiogenic shock complicating population. Intensive Care Med. 2018;44(4):409-417.
Pharmaceuticals (data safety monitoring board acute myocardial infarction: expanding the doi:10.1007/s00134-018-5147-3
member) outside the submitted work; and serving paradigm. Circulation. 2003;107(24):2998-3002. 16. Marik PE, Cavallazzi R. Does the central venous
as lead investigator of the SMART trial and as doi:10.1161/01.CIR.0000075927.67673.F2 pressure predict fluid responsiveness? an updated
co-investigator of the CLOVERS trial. 8. Hahn RG. Understanding volume kinetics. Acta meta-analysis and a plea for some common sense.
Submissions: We encourage authors to submit Anaesthesiol Scand. 2020;64(5):570-578. doi:10. Crit Care Med. 2013;41(7):1774-1781. doi:10.1097/
papers for consideration as a Review. Please 1111/aas.13533 CCM.0b013e31828a25fd
contact Mary McGrae McDermott, MD, at 9. Woodcock TE, Woodcock TM. Revised Starling 17. Teboul JL, Monnet X, Chemla D, Michard F.
mdm608@northwestern.edu. equation and the glycocalyx model of transvascular Arterial pulse pressure variation with mechanical
fluid exchange: an improved paradigm for ventilation. Am J Respir Crit Care Med. 2019;199(1):
REFERENCES prescribing intravenous fluid therapy. Br J Anaesth. 22-31. doi:10.1164/rccm.201801-0088CI
1. Vincent JL, Marshall JC, Namendys-Silva SA, 2012;108(3):384-394. doi:10.1093/bja/aer515 18. Biais M, Ehrmann S, Mari A, et al; AzuRea
et al; ICON Investigators. Assessment of the 10. Malbrain MLNG, Van Regenmortel N, Group. Clinical relevance of pulse pressure
worldwide burden of critical illness: the intensive Saugel B, et al. Principles of fluid management and variations for predicting fluid responsiveness in
care over nations (ICON) audit. Lancet Respir Med. stewardship in septic shock: it is time to consider mechanically ventilated intensive care unit
2014;2(5):380-386. doi:10.1016/S2213-2600(14) the four D’s and the four phases of fluid therapy. patients: the grey zone approach. Crit Care. 2014;18
70061-X Ann Intensive Care. 2018;8(1):66. doi:10.1186/ (6):587. doi:10.1186/s13054-014-0587-9
2. Machado FR, Cavalcanti AB, Bozza FA, et al; s13613-018-0402-x 19. Michard F, Boussat S, Chemla D, et al. Relation
SPREAD Investigators; Latin American Sepsis 11. Monge García MI, Guijo González P, Gracia between respiratory changes in arterial pulse
Institute Network. The epidemiology of sepsis in Romero M, et al. Effects of fluid administration on pressure and fluid responsiveness in septic patients
Brazilian intensive care units (the Sepsis arterial load in septic shock patients. Intensive Care with acute circulatory failure. Am J Respir Crit Care
1978 JAMA June 13, 2023 Volume 329, Number 22 (Reprinted) jama.com
© 2023 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a University of Toronto Libraries User on 06/17/2023
Fluid Therapy for Critically Ill Adults With Sepsis: A Review Review Clinical Review & Education
Med. 2000;162(1):134-138. doi:10.1164/ajrccm.162.1. 34. Cecconi M, Hofer C, Teboul JL, et al; FENICE 2022;386(26):2459-2470. doi:10.1056/
9903035 Investigators; ESICM Trial Group. Fluid challenges in NEJMoa2202707
20. Monnet X, Marik PE, Teboul JL. Prediction of intensive care: the FENICE study: a global inception 47. Shapiro NI, Douglas IS, Brower RG, et al; The
fluid responsiveness: an update. Ann Intensive Care. cohort study. Intensive Care Med. 2015;41(9):1529- National Heart, Lung, and Blood Institute
2016;6(1):111. doi:10.1186/s13613-016-0216-7 1537. doi:10.1007/s00134-015-3850-x Prevention and Early Treatment of Acute Lung
21. García MI, Romero MG, Cano AG, et al. Dynamic 35. Asfar P, Meziani F, Hamel JF, et al; SEPSISPAM Injury Clinical Trials Network. Early restrictive or
arterial elastance as a predictor of arterial pressure Investigators. High versus low blood-pressure liberal fluid management for sepsis-induced
response to fluid administration: a validation study. target in patients with septic shock. N Engl J Med. hypotension. N Engl J Med. 2023;388:499-510. doi:
Crit Care. 2014;18(6):626. doi:10.1186/s13054- 2014;370(17):1583-1593. doi:10.1056/NEJMoa1312173 10.1056/NEJMoa2212663
014-0626-6 36. Gattinoni L, Brazzi L, Pelosi P, et al. A trial of 48. Wiedemann HP, Wheeler AP, Bernard GR, et al;
22. Monnet X, Osman D, Ridel C, Lamia B, Richard goal-oriented hemodynamic therapy in critically ill National Heart, Lung, and Blood Institute Acute
C, Teboul JL. Predicting volume responsiveness by patients: SvO2 Collaborative Group. N Engl J Med. Respiratory Distress Syndrome (ARDS) Clinical
using the end-expiratory occlusion in mechanically 1995;333(16):1025-1032. doi:10.1056/ Trials Network. Comparison of two
ventilated intensive care unit patients. Crit Care Med. NEJM199510193331601 fluid-management strategies in acute lung injury.
2009;37(3):951-956. doi:10.1097/CCM. 37. Rivers E, Nguyen B, Havstad S, et al; Early N Engl J Med. 2006;354(24):2564-2575. doi:10.
0b013e3181968fe1 Goal-Directed Therapy Collaborative Group. Early 1056/NEJMoa062200
23. Monnet X, Rienzo M, Osman D, et al. Passive goal-directed therapy in the treatment of severe 49. Wichmann S, Schønemann-Lund M, Perner A,
leg raising predicts fluid responsiveness in the sepsis and septic shock. N Engl J Med. 2001;345 et al. Goal-directed fluid removal with furosemide
critically ill. Crit Care Med. 2006;34(5):1402-1407. (19):1368-1377. doi:10.1056/NEJMoa010307 versus placebo in intensive care patients with fluid
doi:10.1097/01.CCM.0000215453.11735.06 38. Mouncey PR, Osborn TM, Power GS, et al; overload: a randomised, blinded trial (GODIF
ProMISe Trial Investigators. Trial of early, trial-first version). Acta Anaesthesiol Scand. 2023;
24. Muller L, Toumi M, Bousquet PJ, et al; AzuRéa 67(4):470-478. doi:10.1111/aas.14196
Group. An increase in aortic blood flow after an goal-directed resuscitation for septic shock. N Engl
infusion of 100 mL colloid over 1 minute can predict J Med. 2015;372(14):1301-1311. doi:10.1056/ 50. Seymour CW, Gesten F, Prescott HC, et al. Time
fluid responsiveness: the mini-fluid challenge study. NEJMoa1500896 to treatment and mortality during mandated
Anesthesiology. 2011;115(3):541-547. doi:10.1097/ALN. 39. Peake SL, Delaney A, Bailey M, et al; ARISE emergency care for sepsis. N Engl J Med. 2017;376
0b013e318229a500 Investigators; ANZICS Clinical Trials Group. (23):2235-2244. doi:10.1056/NEJMoa1703058
25. Mayo P, Arntfield R, Balik M, et al. The ICM Goal-directed resuscitation for patients with early 51. Rowan KM, Angus DC, Bailey M, et al; PRISM
research agenda on critical care ultrasonography. septic shock. N Engl J Med. 2014;371(16):1496-1506. Investigators. Early, goal-directed therapy for septic
Intensive Care Med. 2017;43(9):1257-1269. doi:10. doi:10.1056/NEJMoa1404380 shock—a patient-level meta-analysis. N Engl J Med.
1007/s00134-017-4734-z 40. Lammi MR, Aiello B, Burg GT, et al; National 2017;376(23):2223-2234. doi:10.1056/
Institutes of Health, National Heart, Lung, and NEJMoa1701380
26. Rola P, Miralles-Aguiar F, Argaiz E, et al. Clinical
applications of the venous excess ultrasound Blood Institute ARDS Network Investigators. 52. Barbash IJ, Rak KJ, Kuza CC, Kahn JM. Hospital
(VExUS) score: conceptual review and case series. Response to fluid boluses in the fluid and catheter perceptions of Medicare’s sepsis quality reporting
Ultrasound J. 2021;13(1):32. doi:10.1186/s13089- treatment trial. Chest. 2015;148(4):919-926. doi:10. initiative. J Hosp Med. 2017;12(12):963-968. doi:10.
021-00232-8 1378/chest.15-0445 12788/jhm.2929
27. Bakker J, Kattan E, Annane D, et al. Current 41. Jansen TC, van Bommel J, Schoonderbeek FJ, 53. Barbash IJ, Davis B, Kahn JM. National
practice and evolving concepts in septic shock et al; LACTATE study group. Early lactate-guided performance on the Medicare SEP-1 sepsis quality
resuscitation. Intensive Care Med. 2022;48(2):148- therapy in intensive care unit patients: measure. Crit Care Med. 2019;47(8):1026-1032. doi:
163. doi:10.1007/s00134-021-06595-9 a multicenter, open-label, randomized controlled 10.1097/CCM.0000000000003613
trial. Am J Respir Crit Care Med. 2010;182(6):752-761. 54. Zarbock A, Kellum JA, Schmidt C, et al. Effect of
28. Bentzer P, Griesdale DE, Boyd J, MacLean K, doi:10.1164/rccm.200912-1918OC
Sirounis D, Ayas NT. Will this hemodynamically early vs delayed initiation of renal replacement
unstable patient respond to a bolus of intravenous 42. Hernández G, Ospina-Tascón GA, Damiani LP, therapy on mortality in critically ill patients with
fluids?. JAMA. 2016;316(12):1298-1309. doi:10. et al; The ANDROMEDA SHOCK Investigators and acute kidney injury: the ELAIN randomized clinical
1001/jama.2016.12310 the Latin America Intensive Care Network (LIVEN). trial. JAMA. 2016;315(20):2190-2199. doi:10.
Effect of a resuscitation strategy targeting 1001/jama.2016.5828
29. Kattan E, Ospina-Tascón GA, Teboul JL, et al; peripheral perfusion status vs serum lactate levels
ANDROMEDA-SHOCK Investigators. Systematic 55. Gaudry S, Hajage D, Schortgen F, et al;
on 28-day mortality among patients with septic AKIKI Study Group. Initiation strategies for
assessment of fluid responsiveness during early shock: the ANDROMEDA-SHOCK randomized
septic shock resuscitation: secondary analysis of renal-replacement therapy in the intensive care
clinical trial. JAMA. 2019;321(7):654-664. doi:10. unit. N Engl J Med. 2016;375(2):122-133. doi:10.
the ANDROMEDA-SHOCK trial. Crit Care. 2020;24 1001/jama.2019.0071
(1):23. doi:10.1186/s13054-020-2732-y 1056/NEJMoa1603017
43. Zampieri FG, Damiani LP, Bakker J, et al. Effects 56. Barbar SD, Clere-Jehl R, Bourredjem A, et al;
30. Elwan MH, Roshdy A, Reynolds JA, Elsharkawy of a resuscitation strategy targeting peripheral
EM, Eltahan SM, Coats TJ. What is the normal IDEAL-ICU Trial Investigators and the CRICS
perfusion status versus serum lactate levels among TRIGGERSEP Network. Timing of
haemodynamic response to passive leg raise? a patients with septic shock. a bayesian reanalysis of
study of healthy volunteers. Emerg Med J. 2018;35 renal-replacement therapy in patients with acute
the ANDROMEDA-SHOCK trial. Am J Respir Crit kidney injury and sepsis. N Engl J Med. 2018;379
(9):544-549. doi:10.1136/emermed-2017-206836 Care Med. 2020;201(4):423-429. doi:10.1164/rccm. (15):1431-1442. doi:10.1056/NEJMoa1803213
31. Lichtenstein DA. BLUE-protocol and 201905-0968OC
FALLS-protocol: two applications of lung 57. Bagshaw SM, Wald R, Adhikari NKJ, et al;
44. Maitland K, Kiguli S, Opoka RO, et al; FEAST STARRT-AKI Investigators; Canadian Critical Care
ultrasound in the critically ill. Chest. 2015;147(6): Trial Group. Mortality after fluid bolus in African
1659-1670. doi:10.1378/chest.14-1313 Trials Group; Australian and New Zealand Intensive
children with severe infection. N Engl J Med. 2011; Care Society Clinical Trials Group; United Kingdom
32. Yealy DM, Kellum JA, Huang DT, et al; ProCESS 364(26):2483-2495. doi:10.1056/NEJMoa1101549 Critical Care Research Group; Canadian Nephrology
Investigators. A randomized trial of protocol-based 45. Andrews B, Semler MW, Muchemwa L, et al. Trials Network; Irish Critical Care Trials Group.
care for early septic shock. N Engl J Med. 2014;370 Effect of an early resuscitation protocol on Timing of initiation of renal-replacement therapy in
(18):1683-1693. doi:10.1056/NEJMoa1401602 in-hospital mortality among adults with sepsis and acute kidney injury. N Engl J Med. 2020;383(3):
33. Evans L, Rhodes A, Alhazzani W, et al. Surviving hypotension: a randomized clinical trial. JAMA. 240-251. doi:10.1056/NEJMoa2000741
sepsis campaign: international guidelines for 2017;318(13):1233-1240. doi:10.1001/jama.2017.10913 58. Wald R, Kirkham B, daCosta BR, et al. Fluid
management of sepsis and septic shock 2021. 46. Meyhoff TS, Hjortrup PB, Wetterslev J, et al; balance and renal replacement therapy initiation
Intensive Care Med. 2021;47(11):1181-1247. doi:10. CLASSIC Trial Group. Restriction of intravenous fluid strategy: a secondary analysis of the STARRT-AKI
1007/s00134-021-06506-y in ICU patients with septic shock. N Engl J Med.
jama.com (Reprinted) JAMA June 13, 2023 Volume 329, Number 22 1979
© 2023 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a University of Toronto Libraries User on 06/17/2023
Clinical Review & Education Review Fluid Therapy for Critically Ill Adults With Sepsis: A Review
trial. Crit Care. 2022;26(1):360. doi:10.1186/s13054- 65. Hammond NE, Zampieri FG, Di Tanna GL, et al. starch or saline for fluid resuscitation in intensive
022-04229-0 Balanced crystalloids versus saline in critically ill care. N Engl J Med. 2012;367(20):1901-1911. doi:10.
59. Murugan R, Bellomo R, Palevsky PM, adults: a systematic review with meta-analysis. 1056/NEJMoa1209759
Kellum JA. Ultrafiltration in critically ill patients NEJM Evid. Published online January 18, 2022. doi: 72. Toscani L, Aya HD, Antonakaki D, et al. What is
treated with kidney replacement therapy. Nat Rev 10.1056/EVIDoa2100010 the impact of the fluid challenge technique on
Nephrol. 2021;17(4):262-276. doi:10.1038/s41581- 66. Zampieri FG, Damiani LP, Biondi RS, et al; diagnosis of fluid responsiveness? a systematic
020-00358-3 BRICNet. Effects of balanced solution on short-term review and meta-analysis. Crit Care. 2017;21(1):207.
60. Young P, Bailey M, Beasley R, et al; SPLIT outcomes in traumatic brain injury patients: doi:10.1186/s13054-017-1796-9
Investigators; ANZICS CTG. Effect of a buffered a secondary analysis of the BaSICS randomized trial. 73. Zampieri FG, Machado FR, Biondi RS, et al;
crystalloid solution vs saline on acute kidney injury Rev Bras Ter Intensiva. 2022;34(4):410-417. doi:10. BaSICS Investigators and the BRICNet members.
among patients in the intensive care unit: the SPLIT 5935/0103-507X.20220261-en Effect of slower vs faster intravenous fluid bolus
randomized clinical trial. JAMA. 2015;314(16):1701- 67. Finfer S, Bellomo R, Boyce N, French J, rates on mortality in critically ill patients: the BaSICS
1710. doi:10.1001/jama.2015.12334 Myburgh J, Norton R; SAFE Study Investigators. randomized clinical trial. JAMA. 2021;326(9):830-
61. Semler MW, Self WH, Wanderer JP, et al; A comparison of albumin and saline for fluid 838. doi:10.1001/jama.2021.11444
SMART Investigators and the Pragmatic Critical resuscitation in the intensive care unit. N Engl J Med. 74. Zampieri FG, Damiani LP, Bagshaw SM, et al;
Care Research Group. Balanced crystalloids versus 2004;350(22):2247-2256. doi:10.1056/ BRICNet. Conditional treatment effect analysis of
saline in critically ill adults. N Engl J Med. 2018; NEJMoa040232 two infusion rates for fluid challenges in critically ill
378(9):829-839. doi:10.1056/NEJMoa1711584 68. Caironi P, Tognoni G, Masson S, et al; ALBIOS patients: a secondary analysis of Balanced Solution
62. Zampieri FG, Machado FR, Biondi RS, et al; Study Investigators. Albumin replacement in versus Saline in Intensive Care Study (BaSICS) trial.
BaSICS Investigators and the BRICNet members. patients with severe sepsis or septic shock. N Engl J Ann Am Thorac Soc. Published online February 3,
Effect of intravenous fluid treatment with a Med. 2014;370(15):1412-1421. doi:10.1056/ 2023. doi:10.1513/AnnalsATS.202211-946OC
balanced solution vs 0.9% saline solution on NEJMoa1305727 75. Alves JAM, Magalhães MR, Zampieri FG, Veiga
mortality in critically ill patients: the BaSICS 69. Brunkhorst FM, Engel C, Bloos F, et al; German VC, Maia IS, Cavalcanti AB. Physiological and clinical
randomized clinical trial. JAMA. 2021;326(9):1-12. Competence Network Sepsis (SepNet). Intensive effects of different infusion rates of intravenous
doi:10.1001/jama.2021.11684 insulin therapy and pentastarch resuscitation in fluids for volume expansion: a scoping review. J Crit
63. Finfer S, Micallef S, Hammond N, et al; PLUS severe sepsis. N Engl J Med. 2008;358(2):125-139. Care. Published online March 29, 2023. doi:10.1016/
Study Investigators and the Australian New Zealand doi:10.1056/NEJMoa070716 j.jcrc.2023.154295
Intensive Care Society Clinical Trials Group. 70. Perner A, Haase N, Guttormsen AB, et al; 76. Pecanha Antonio AC, Basso Gazzana M, Souza
Balanced multielectrolyte solution versus saline in 6S Trial Group; Scandinavian Critical Care Trials Castro P, Knorst M. Fluid balance predicts weaning
critically ill adults. N Engl J Med. 2022;386(9): Group. Hydroxyethyl starch 130/0.42 versus failure in chronic obstructive pulmonary disease
815-826. doi:10.1056/NEJMoa2114464 Ringer’s acetate in severe sepsis. N Engl J Med. patients. Crit Care. Published online March 17, 2014.
64. Brown RM, Wang L, Coston TD, et al. Balanced 2012;367(2):124-134. doi:10.1056/NEJMoa1204242 doi:10.1186/cc13489
crystalloids versus saline in sepsis: a secondary 71. Myburgh JA, Finfer S, Bellomo R, et al; CHEST
analysis of the SMART clinical trial. Am J Respir Crit Investigators; Australian and New Zealand Intensive
Care Med. 2019;200(12):1487-1495. doi:10.1164/ Care Society Clinical Trials Group. Hydroxyethyl
rccm.201903-0557OC
1980 JAMA June 13, 2023 Volume 329, Number 22 (Reprinted) jama.com
© 2023 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a University of Toronto Libraries User on 06/17/2023
You might also like
- Fluido Therapy - Sepsis Jama Zampieri 2023 RV 230010 1686240954.61353Document14 pagesFluido Therapy - Sepsis Jama Zampieri 2023 RV 230010 1686240954.61353VictorMéndezNo ratings yet
- Infective Endocarditis: A Multidisciplinary ApproachFrom EverandInfective Endocarditis: A Multidisciplinary ApproachArman KilicNo ratings yet
- Clinical Assessment and Diagnosis of Hypovolemia (Dehydration) in Children - UpToDateDocument12 pagesClinical Assessment and Diagnosis of Hypovolemia (Dehydration) in Children - UpToDateNedelcu MirunaNo ratings yet
- 29744226: Cerebral Pathophysiology in Extracorporeal Membrane Oxygenation Pitfalls in Daily Clinical ManagementDocument11 pages29744226: Cerebral Pathophysiology in Extracorporeal Membrane Oxygenation Pitfalls in Daily Clinical ManagementEward Rod SalNo ratings yet
- Inhalational AgentsDocument17 pagesInhalational Agentsanaeshkl100% (1)
- Picu Drug Dosage Chart AmitDocument9 pagesPicu Drug Dosage Chart AmitIze C VijiNo ratings yet
- Νευρολογία σύνολο απαντήσεωνDocument38 pagesΝευρολογία σύνολο απαντήσεωνCheng Kuao HengNo ratings yet
- Blindness Power PointDocument128 pagesBlindness Power PointmanognaaaaNo ratings yet
- Surviving Sepsis Campaign 2016 Guidelines Presentation Final RevisiedDocument32 pagesSurviving Sepsis Campaign 2016 Guidelines Presentation Final RevisiedAdli Wafi Jabbar100% (1)
- Critical Care Admission OrdersDocument6 pagesCritical Care Admission OrdersTariq Niaz Ahmad, MDNo ratings yet
- CNS - Clinical Evaluation of HemiplegiaDocument36 pagesCNS - Clinical Evaluation of HemiplegiaDipin ManiNo ratings yet
- Renal PharmacologyDocument52 pagesRenal Pharmacologyashraf0% (1)
- Sleep Apnoea - Prof - DR K.K.PDocument44 pagesSleep Apnoea - Prof - DR K.K.PjialeongNo ratings yet
- Medical Management of GlaucomaDocument43 pagesMedical Management of Glaucomahemnath rajendran100% (1)
- Resp Medicine NotesDocument95 pagesResp Medicine Noteshugolucas182100% (1)
- Surgical Implications of Low Cardiac Output Syndrome After Myocardial InfarctionDocument5 pagesSurgical Implications of Low Cardiac Output Syndrome After Myocardial Infarctionrandomized1234No ratings yet
- Captopril Renography: Physiologic Principle - Loss of Preferential Vasoconstriction of The EfferentDocument3 pagesCaptopril Renography: Physiologic Principle - Loss of Preferential Vasoconstriction of The EfferentSri HariNo ratings yet
- NoradrenalineDocument1 pageNoradrenalineMohammad IslamNo ratings yet
- Hypoglycemia PresentationDocument45 pagesHypoglycemia Presentationask1400100% (1)
- Low Back Pain New-31!12!14Document61 pagesLow Back Pain New-31!12!14Vishv Rathore DHANSIANo ratings yet
- 17 The Brigham Board Review in Critical Care Medicine 2017Document1,355 pages17 The Brigham Board Review in Critical Care Medicine 2017Thanh NguyenNo ratings yet
- AntibioticsDocument30 pagesAntibioticsRoza RahbeniNo ratings yet
- Valvular Heart Disease To TW FinalDocument13 pagesValvular Heart Disease To TW FinalMohammed ElSayedNo ratings yet
- Aspirin To Prevent Future CVDDocument10 pagesAspirin To Prevent Future CVDAngelo DestaNo ratings yet
- Management of Diabetes MellitusDocument42 pagesManagement of Diabetes Mellitusayu ersa lestari100% (1)
- Hepa-Merz: (L-Ornithine L-Aspartate)Document2 pagesHepa-Merz: (L-Ornithine L-Aspartate)Sami UfoNo ratings yet
- Procedure For Balloon Aortic Valvuloplasty (BAV)Document17 pagesProcedure For Balloon Aortic Valvuloplasty (BAV)jaganjaggi100% (1)
- 2010-2011 Antibiotic GuidelinesDocument78 pages2010-2011 Antibiotic GuidelinesMuhammad Rizki BachtiarNo ratings yet
- Pacing Week PresentationsDocument54 pagesPacing Week PresentationsjoejenningsNo ratings yet
- DO /VO Relationships: J. L. VincentDocument8 pagesDO /VO Relationships: J. L. VincentLucas Cárcamo SaavedraNo ratings yet
- Pericardial EffusionDocument3 pagesPericardial EffusionNita Hurek100% (1)
- SB Intern Survival Guide 0Document12 pagesSB Intern Survival Guide 0nevmerkaNo ratings yet
- ArdsDocument2 pagesArdsKakaa KakaNo ratings yet
- Wallenberg Syndrome: Publication DetailsDocument9 pagesWallenberg Syndrome: Publication DetailsHuang Jen Liang100% (1)
- I.V Fluid: PathologyDocument7 pagesI.V Fluid: PathologyruchikaNo ratings yet
- ICP Head InjuryDocument57 pagesICP Head InjuryWengel RedkissNo ratings yet
- Non-Steroidal Anti-Inflammatory Drugs (Nsaids) : Analgesic, Anti-Pyretic and Anti-Inflammatory AgentsDocument45 pagesNon-Steroidal Anti-Inflammatory Drugs (Nsaids) : Analgesic, Anti-Pyretic and Anti-Inflammatory AgentsArvi KhanNo ratings yet
- Hemodynamic MonitoringDocument41 pagesHemodynamic MonitoringSuresh KumarNo ratings yet
- Cardiopulmonary BypassDocument62 pagesCardiopulmonary BypassNidya Putri100% (1)
- Toujeo Speaker Slide Deck TW - Tjo.16.04.03 FINALDocument55 pagesToujeo Speaker Slide Deck TW - Tjo.16.04.03 FINAL陳品汎100% (1)
- Hemorrhagic StrokeDocument57 pagesHemorrhagic StrokeAnonymous oEbVOENo ratings yet
- AION Anterior Ischemic Optic Neuropathy AIONDocument22 pagesAION Anterior Ischemic Optic Neuropathy AIONNyak Rahmat100% (1)
- Congenital Heart DiseaseDocument74 pagesCongenital Heart DiseaseKeith LajotNo ratings yet
- GERIATRIC MEDICINE (Basic)Document41 pagesGERIATRIC MEDICINE (Basic)Medical AdvicesNo ratings yet
- Infective Endocarditis: Hariprasad KDocument28 pagesInfective Endocarditis: Hariprasad KHari Prasad K100% (1)
- Anaesthesia and Me Whatsapp Group: Anaesthetic ManagementDocument14 pagesAnaesthesia and Me Whatsapp Group: Anaesthetic Managementelika dwi67% (3)
- The Red Eye The Swollen Eye and Acute Vision Loss Handling Non Traumatic Eye Disorders in The EDDocument28 pagesThe Red Eye The Swollen Eye and Acute Vision Loss Handling Non Traumatic Eye Disorders in The EDBimantoro SaputroNo ratings yet
- Physical Assessment Iv Neurological Exam: Jessica Mendoza-Guno, MSN, RN Clinical InstructorDocument52 pagesPhysical Assessment Iv Neurological Exam: Jessica Mendoza-Guno, MSN, RN Clinical InstructorQueen Klein SamaritaNo ratings yet
- Regional AnesthesiaDocument54 pagesRegional AnesthesiaIdza Fariha AfriNo ratings yet
- Cardiac ValveDocument12 pagesCardiac ValveHellen WestgroveNo ratings yet
- PG BookDocument5 pagesPG BookUnnithan Rendezvous100% (2)
- Standard Management of Various Medical ConditionsDocument47 pagesStandard Management of Various Medical ConditionsManik bhushan ShrivastavNo ratings yet
- Quick Uveitis PDFDocument59 pagesQuick Uveitis PDFirinaNo ratings yet
- Para PhimosisDocument9 pagesPara PhimosisNazurah Azmira100% (1)
- Superior Oblik PalsyDocument13 pagesSuperior Oblik PalsyYunita ManurungNo ratings yet
- Textbook Reference-Unit VI (p449) : Part 1 of 3Document53 pagesTextbook Reference-Unit VI (p449) : Part 1 of 3glenn johnstonNo ratings yet
- On Admission:: STROKE MANAGEMENT (Beaumont Hospital)Document3 pagesOn Admission:: STROKE MANAGEMENT (Beaumont Hospital)Nadia SalwaniNo ratings yet
- Permanent Pacemaker TechniqueDocument7 pagesPermanent Pacemaker TechniqueMonica TrifitrianaNo ratings yet
- Prosthetic Heart Valves - Part 1 - SelectionDocument13 pagesProsthetic Heart Valves - Part 1 - SelectionwalltercesarNo ratings yet
- Gastrointestinal Diseases and Disorders Sourcebook, Fifth EditionFrom EverandGastrointestinal Diseases and Disorders Sourcebook, Fifth EditionNo ratings yet
- Functional Hemodynamic Monitoring PDFDocument10 pagesFunctional Hemodynamic Monitoring PDFPGI AnaesthesiaNo ratings yet
- Parameters of Fluid Responsiveness Curr Op Crit Care Shi2020Document8 pagesParameters of Fluid Responsiveness Curr Op Crit Care Shi2020Tadeo PradoNo ratings yet
- PDF Passive Leg Raise PLR Test Stroke Volume Index SviDocument3 pagesPDF Passive Leg Raise PLR Test Stroke Volume Index SviNama ManaNo ratings yet