Professional Documents
Culture Documents
Bioessays Article
Uploaded by
vasanthnatesanOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Bioessays Article
Uploaded by
vasanthnatesanCopyright:
Available Formats
HYPOTHESIS
Insights & Perspectives www.bioessays-journal.com
Beta-Adrenergic Blockers as a Potential Treatment
for COVID-19 Patients
Natesan Vasanthakumar
entry into the cell. SARS-CoV-2 invades
More than 15 million people have been affected by coronavirus disease 2019 host cells via a novel route: CD147-spike
(COVID-19) and it has caused 640 016 deaths as of July 26, 2020. Currently, protein.[4,5] In this paper, I develop a novel
no effective treatment option is available for COVID-19 patients. Though proposal for treatment of COVID-19 in-
many drugs have been proposed, none of them has shown particular efficacy fection based on the following compo-
nents: (i) Adrenergic system by its action
in clinical trials. In this article, the relationship between the Adrenergic system
on Renin-angiotensin-aldosterone system
and the renin-angiotensin-aldosterone system (RAAS) is focused in COVID-19 (RAAS), ACE2, and SARS-CoV-2 might play
and a vicious circle consisting of the Adrenergic system-RAAS-Angiotensin a crucial role in COVID-19. (ii) Hyperactiva-
converting enzyme 2 (ACE2)-severe acute respiratory syndrome coronavirus 2 tion of the vicious ARAS loop may be the
(SARS-CoV-2) (which is referred to as the “ARAS loop”) is proposed. mechanism behind COVID-19. (iii) Beta-
adrenergic blockers should be used as a po-
Hyperactivation of the ARAS loop may be the underlying pathophysiological
tential treatment option in COVID-19 pa-
mechanism in COVID-19, and beta-adrenergic blockers are proposed as a tients.
potential treatment option. Beta-adrenergic blockers may decrease the
SARS-CoV-2 cellular entry by decreasing ACE2 receptors expression and
cluster of differentiation 147 (CD147) in various cells in the body. 1.1. Pathophysiological Features in
Beta-adrenergic blockers may decrease the morbidity and mortality in COVID-19
COVID-19 patients by preventing or reducing acute respiratory distress
1.1.1. Clinical and Laboratory Features of
syndrome (ARDS) and other complications. Retrospective and prospective COVID-19
clinical trials should be conducted to check the validity of the hypothesis. Also
see the video abstract here https://youtu.be/uLoy7do5ROo. Clinical course of COVID-19 patients are
variable—ranging from being asymp-
tomatic to having mild symptoms like
fever, cough, sore throat, dyspnea, muscle pain, tiredness, loss
1. Introduction of taste or smell sensation, etc.[6] Around 15% of COVID-19 pa-
tients exhibit pneumonia and ≈5% progress to acute respira-
Coronavirus disease 2019 (COVID-19) has affected people’s lives tory distress syndrome (ARDS) wherein patients have tachyp-
across the world, and as of 26 July 2020, 15 785 641 people noea, decreased oxygen saturation, decreased partial pressure of
are affected globally and caused 640 016 deaths.[1] Severe acute oxygen in arterial blood, and lung infiltrates in the X-ray and
respiratory syndrome coronavirus 2 (SARS-COV-2), a positive- CT chest imaging.[7] Severe COVID-19 patients with complica-
sense single-stranded RNA virus, belongs to the beta coronavirus tions like ARDS, respiratory failure, and septic shock have a
genus. It is known that the SARS-CoV-2 spike protein binds to high mortality rate.[8] Laboratory investigations in moderately
human angiotensin-converting enzyme 2 (ACE2), which acts as or severely affected COVID-19 patients showed increased In-
a receptor, and binding to ACE2 is crucial for the cellular entry terleukin 6 (IL-6), D-dimer (a degradation product of fibrin),
of SARS-COV-2.[2,3] It has been proposed recently that cluster of C-reactive protein (CRP), and lactate dehydrogenase (LDH).[6]
differentiation 147 (CD147) also known as Basigin, maybe an- Severely affected COVID-19 patients had lymphopenia and in-
other receptor in the host cells that play a role in the SARS-CoV-2 creased IL-6, Interleukin-1𝛽 (IL-1𝛽), tumor necrosis factor alpha
(TNF𝛼) cytokines levels.[7]
Dr. N. Vasanthakumar[+]
School of Chemical and Biotechnology
SASTRA Deemed University 1.1.2. IL-6 Increase in COVID-19 Produce Complications
Thanjavur, Tamil Nadu 613401, India
E-mail: vasanth.dr@gmail.com Increased IL-6 is an indicator of poor outcome in patients with
ARDS and Tocilizumab can be used to block the action of IL-6.[7]
The ORCID identification number(s) for the author(s) of this article
can be found under https://doi.org/10.1002/bies.202000094
It has been shown that IL-6 is increased in COVID-19
nonsurvivors.[9] Increased mucus aggregation has been noticed
[+] Present address: Abel Clinic, Uthangarai, Tamil Nadu 635207, India in the distal airways and alveoli in the postmortem study of
DOI: 10.1002/bies.202000094 COVID-19 patients.[10] It is known that IL-6 plays a key role in
BioEssays 2020, 42, 2000094 2000094 (1 of 9) © 2020 Wiley Periodicals LLC
www.advancedsciencenews.com www.bioessays-journal.com
the activation of MUC5AC and MUC5B gene expression and has been suggested to be activated by SARS-CoV-2. It is known
increases the mucus secretion.[11] It has been suggested that that colchicine inhibits NLRP3 inflammasome, and clinical tri-
Tocilizumab by the inhibition of IL-6 receptor may help decrease als have already been registered to test whether colchicine treat-
the mucus secretion in COVID-19.[12] Postmortem study has ment in COVID-19 improves the clinical condition by inhibiting
shown the presence of hyperplasia of type II alveolar epithelial NLRP3.[25] It is known that the SARS-COV orf3a protein activates
cells, diffuse alveolar damage, macrophage and neutrophil in- the NLRP3.[26] SARS-CoV viroporin 3a has also been shown to ac-
filtration, fibrosis, hyaline membrane formation.[13] It is known tivate NLRP3.[27] SARS-CoV-2 may also activate NLRP3 by a simi-
that cytokine storm occurs in COVID-19, as the levels of IL-1𝛽, lar mechanism. The downstream effectors of NLRP3 are caspase
IL-6, TNF𝛼 are increased and this leads to multiple organ dys- 1, IL-1𝛽, and IL-18.[28] It is known that the decrease in surfac-
function and septic shock.[7] tant protein D in ARDS patients is associated with mortality[29]
and interestingly surfactant protein D has been shown to inhibit
1.1.3. Pulmonary Complications in COVID-19 Patients NLRP3.[30] Since the type 2 alveolar epithelial cells which secrete
the surfactant are one of the main cells affected by SARS-CoV-2,
Inflammatory responses like macrophage and neutrophil infiltra- surfactant secretion may likely be decreased. Reduction in surfac-
tion may lead to alveolar damage, pulmonary capillary endothe- tant D may result in loss of its inhibitory role on NLRP3 and the
lial dysfunction, and the pulmonary capillary leak that may lead resultant activation of the NLRP3 inflammasome pathway may
to pulmonary edema. Since type II pulmonary alveolar epithelial produce an inflammatory response in COVID-19.
cells are the main cells that express ACE2 receptors, their dam-
age might cause problems in surfactant secretion by these cells.
Decreased surfactant leads to increased surface tension in the 1.1.6. Hypercoagulation State in COVID-19 Patients
alveoli, which along with the damage in the alveolar epithelium
and pulmonary capillary endothelium, may lead to pulmonary As mentioned earlier, severely affected COVID-19 patients devel-
edema. Respiratory dysfunction as a result of this leads to de- oped pulmonary embolism, and D-dimer levels were shown to
creased partial pressure of oxygen in arterial blood (Pa O2 ), de- be high.[15–17] But so far, it is not known what causes pulmonary
creased oxygen saturation, and severe cases warrant mechanical embolism or deep vein thrombosis (DVT) in COVID-19. I hy-
ventilation. If refractory hypoxemia develops despite mechanical pothesize that the hypercoagulation state in COVID-19 may be
ventilation, then extracorporeal membrane oxygenation (ECMO) due to a sympathetic storm. Increased catecholamine levels may
can be tried as per World Health Organization’s (WHO) interim hyperactivate the vicious ARAS loop, which will be explained
guidance.[14] in a later section. It has been known that beta2-adrenergic ago-
nist nebulization increases the plasma catecholamine levels.[31]
Sympathetic hyperactivation has been shown to be related to
1.1.4. Severely Affected Patients Exhibit Complications Like ARDS, hypercoagulation state.[32] Inhalation of beta2-adrenergic ago-
Pulmonary Embolism, Septic Shock nists has been shown to increase coagulation factor VIII, von
Willebrand factor (VWF), D-dimer, and lead to hypercoagulation
Around 30% of the severely affected COVID-19 patients devel- state.[33] I hypothesize that use of catecholamines in COVID-19
oped pulmonary embolism and D-dimer level is found higher patients may lead to hypercoagulation state, and nebulization
in these patients.[15–17] Around 5% of them had severe com- with beta2-adrenergic agonists for respiratory symptoms and in-
plications like ARDS, septic shock.[18] Septic shock occurs in travenous administration of norepinephrine for treating septic
severely affected COVID-19 patients wherein the mean arterial shock should be avoided in COVID-19, as it may lead to hyper-
pressure is low (<65 mmHg) irrespective of fluid management coagulation state and may induce complications like deep vein
and plasma lactate concentration will be >2 × 10−3 m L−1 . Sep- thrombosis and pulmonary embolism.
tic shock state carries a high mortality rate and the primary drug Other organs damage in COVID-19 is not discussed in this
used in the treatment is norepinephrine.[19] article due to space constraints.
1.1.5. Cytokine Storm, Nucleotide-binding domain (NOD)-like
Receptor Protein 3 (NLRP3) Activation and Hyperinflammation 1.2. Current Treatment Recommendations are Largely Ineffective
Occurs in COVID-19 and Controversial
Cytokine storm and hyperinflammation occurs in COVID-19 ir- At present, there is no effective drug available against the COVID-
respective of lymphopenia.[20,21] Considering the cytokine storm 19 pandemic.[6,34] Many potential treatments are proposed and
and potential activation of the NLRP3 inflammasome, it is likely some are on clinical trials. Many are focusing on drugs that inter-
that immune hyperactivation occurs in COVID-19. Nucleocapsid rupt the binding of spike protein with the ACE2 receptor. Remde-
protein of SARS-CoV has been shown to increase IL-6 via the acti- sivir, hydroxychloroquine, azithromycin, tocilizumab are used in
vation of Nuclear factor kappa B (NF-𝜅B).[22] Since the nucleocap- COVID-19 condition all over the world, though there is no evi-
sid protein of SARS-CoV-2 shares 89.6% homology with SARS- dence so far, for their efficacy. Remdesivir is presumed to work, by
CoV nucleocapsid,[23] it is likely that the increase in IL-6 found in its inhibitory action on RNA dependent RNA polymerase restrict-
severely affected COVID-19 patients may also have a similar un- ing the viral replication but so far, its efficacy has not been shown
derlying mechanism. IL-6 level has been shown to positively cor- in clinical trials.[34] Hydroxychloroquine may restrict the SARS-
relate with the SARS-CoV-2 viral load.[24] NLRP3 inflammasome CoV-2 cellular entry but its efficacy has not been shown in clinical
BioEssays 2020, 42, 2000094 2000094 (2 of 9) © 2020 Wiley Periodicals LLC
www.advancedsciencenews.com www.bioessays-journal.com
trials. Tocilizumab by its action on the IL-6 receptor blocks the SARS-CoV-2 infection may also lead to increased catecholamine
inflammatory actions due to IL-6, but its efficacy has not been levels.[39] I speculate that in the severely affected COVID-19
proven in clinical trials. As mentioned earlier, Tocilizumab may patients with complications like ARDS and septic shock, it is
help decrease the mucus secretion in COVID-19.[12] Recently Na- likely that endogenous catecholamine levels may be high and
tional Institutes of Health (NIH) had recommended Remdesivir it may trigger the ARAS loop. Apart from the increased en-
for COVID-19 patients who are on supplemental oxygen but not dogenous catecholamine level in these complicated COVID-19
for those who are on mechanical ventilation. NIH has also rec- patients, giving exogenous catecholamines like beta-agonists in
ommended dexamethasone due to their immunomodulatory role the nebulizer solution for treating dyspnea or norepinephrine
for the COVID-19 patients who are on mechanical ventilation. given intravenously for the patients having septic shock, may
NIH has not recommended hydroxychloroquine, azithromycin, further increase the catecholamine level and hyperactivate the
tocilizumab treatment in COVID-19.[35] vicious ARAS loop and worsen the condition. I speculate that
Another treatment option on the trial is convalescent plasma any drug that augments the activation of the ARAS loop will
therapy. Supportive measures are used depending on the clinical worsen the COVID-19 condition and increase the mortality. The
condition such as the use of mechanical ventilation, ECMO, etc. potential dangers of using norepinephrine, beta2-agonists, and
As mentioned earlier, WHO suggests that if refractory hypoxemia angiotensin receptor-blockers (ARBs) in COVID-19 are discussed
persists despite mechanical ventilation, then ECMO can be opted in a later section.
for in selected cases. Many have raised concerns about the use
of ECMO in COVID-19, as some studies showed increased mor-
tality in patients who suffered from ARDS and were on ECMO 1.4. RAAS Inhibitors Role in COVID-19 Patients is not Clear
support.[9,36,37]
In summary, the underlying pathophysiology of the COVID-19 It is known that the RAAS plays a crucial role in the regulation
is not known and no effective treatment is available at present. of blood pressure, sodium level, extracellular fluid volume,
In this article, I speculate that the dangerous relationship be- etc. RAAS system has two opposing arms, the classic Renin-
tween the adrenergic system, RAAS, ACE2, and SARS-CoV-2 angiotensinI-angiotensin converting enzyme (ACE)–angiotensin
may be the underlying pathological mechanism in COVID-19. II(ATII)-aldosterone and Renin-ATII-angiotensin-converting-
I propose the existence of a vicious Adrenergic system-RAAS- enzyme2(ACE2)-angiotensin-(1-7)-Mas receptor (MasR). Along
ACE2-SARS-CoV-2 (ARAS) loop in COVID-19 condition. Any with the classic pathway which produces effects like vasocon-
drugs like norepinephrine, beta2 agonist that increase the activity striction and inflammation, one more pathway with opposing
of ARAS loop, may worsen the condition in COVID-19 patients. actions to classic pathway exist which produces effects like va-
Adrenergic blockers may inhibit this vicious ARAS loop and sorelaxation and is anti-inflammatory. Unlike the classic RAAS
provide beneficial effect in COVID-19 patients. I propose beta- pathway which uses ACE, the vasorelaxation arm uses ACE2.[40]
adrenergic blockers as a potential drug option for the treatment of Angiotensin II receptor-blockers (ARBs) and angiotensin-
COVID-19. converting-enzyme inhibitors (ACEIs) are common drugs used
in hypertension patients. They have inhibitory action on RAAS
pathway and produce the antihypertensive effect. Recently
1.3. The Adrenergic System-RAAS-ACE2-SARS-CoV-2 (ARAS) concerns were raised regarding the use of angiotensin receptor
Loop May be the Underlying Pathophysiological Mechanism in blocker (ARB) drugs as it may increase the ACE2 expression,
COVID-19 which in turn may increase the SARS-CoV-2 entry.[41,42] It has
been suggested that other antihypertensive drugs like beta-
It is important to study whether sympathetic storm, i.e., in- adrenergic blockers and calcium channel blockers can be used in
creased catecholamine level in the body occurs in COVID-19. COVID-19 cases with hypertension instead of ARBs.[41] On the
Considering all the above evidences and clinical features of contrary, many opined that in the absence of sufficient evidence
pulmonary edema, pulmonary embolism, deep vein thrombosis, there is no need to change the drugs like ARBs in the COVID-19
and septic shock it appears that the critical illness in COVID-19 patients who are already taking them.[43] Withdrawal of ARBs
may exhibit sympathetic storm in the body and maybe the and ACEIs in COVID-19 patients with hypertension was sug-
basis for all the complications. Increased catecholamine level gested not to be done without sufficient evidence.[44] I speculate
in the COVID-19 patients may trigger a hypothetical ARAS that beta-adrenergic blockers decrease the renin level by their
loop. Adrenergic system regulation of RAAS is crucial in the inhibitory action on the sympathetic system and decrease ATII.
COVID-19. Increased plasma catecholamine level will activate Unlike ARBs and ACEIs, beta-adrenergic blockers have an
the adrenergic system leading to the activation of RAAS and advantage by their action on upstream protein renin which may
increase in ACE2, as a result of which the entry of SARS-CoV-2 decrease the activity of both arms. Therefore, beta-adrenergic
increases, producing complications in COVID-19 patients; in blockers not only decrease ATII levels but also reduce the ACE2
response to the critical illness, endogenous catecholamines will receptors, which will be useful in regulating the blood pressure
be increased and the vicious cycle goes on. I would like to call this and at the same time decrease the SARS-CoV-2 cellular entry.
as adrenergic system-RAAS-ACE2-SARS-CoV-2 (ARAS) loop I suggest that beta-adrenergic blockers can be considered as
(Figure 1). an alternative to ARBs in the COVID-19 patients having hy-
It is known that critical illnesses will increase the plasma pertension and ARBs should be avoided in COVID-19 patients.
catecholamine level.[38] It is interesting to note that adenoviral Since ARBs, by blocking the angiotensin II receptor increase
respiratory illness causes increased plasma catecholamine level. the ATII level, they may trigger the ARAS loop and complicate
BioEssays 2020, 42, 2000094 2000094 (3 of 9) © 2020 Wiley Periodicals LLC
www.advancedsciencenews.com www.bioessays-journal.com
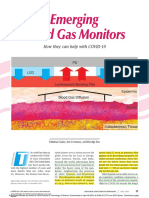
Figure 1. The adrenergic system-RAAS-ACE2-SARS-CoV-2 (ARAS) loop: A hypothetical vicious circle consisting of the adrenergic system-RAAS-ACE2-
SARS-CoV-2 (ARAS) is predicted to emerge in COVID-19 pathology. Severely affected COVID-19 patients may have “sympathetic storm” (increased
catecholamine levels in the body), which may hyperactivate this loop, and increase ACE2 which in turn may increase the viral entry into cells. Ad-
ministration of catecholamines exogenously via application of beta2-adrenergic agonists in a nebulizer solution, or by intravenous administration of
norepinephrine for treating the septic shock condition in COVID-19 patients, will serve as an agonist of the ARAS loop, and worsen the condition. Beta-
adrenergic blockers will inhibit this ARAS loop and may produce beneficial effects in COVID-19 patients by preventing or reducing complications such
as pulmonary embolism, ARDS and septic shock.
the COVID-19 condition. It has been already shown that ATII 1.6. Why Norepinephrine Given for Septic Shock Complication in
induces pulmonary edema in the animal model study,[45] which COVID-19 Patients May Worsen the Condition?
supports the view that increased ATII may be detrimental in
COVID-19. Adrenergic system hyperactivation occurs in critical conditions,
which increases the catecholamine level. Critically ill COVID-
19 patients may also have sympathetic storm, i.e., increased
catecholamine level in the body. So far whether increased cat-
1.5. Why Beta2-adrenergic Agonist in Nebulizer Form Likely echolamine level occurs in COVID-19 patients is not known.
Worsens Symptoms? As any critical condition may activate the adrenergic system, it
is likely that in severe COVID-19 patients catecholamine lev-
Clinicians treat dyspneic patients routinely with beta2-adrenergic els may increase. Increased catecholamine level will lead to
agonists like salbutamol, anticholinergics, and corticosteroids ei- increase renin release, which increases the activity of both its
ther alone or in combinations. Beta2-adrenergic agonists are one arms including an increase in ACE2 expression facilitating the
of the primary drugs used in nebulizers. Considering their role in SARS-Cov-2 cellular entry and worsening the condition. Some
sympathetic activation and renin release, beta2-adrenergic ago- of the severe COVID-19 patients may end up in septic shock.
nists may increase ACE2 expression in the alveolar epithelial cells The primary drug used in septic shock is norepinephrine.[19]
which may help the SARS-CoV-2 and worsen the condition. It has As mentioned earlier, in the critical COVID-19 patients, endoge-
been already suggested that beta-2 agonists should be avoided nous catecholamine levels may be increased, and giving nore-
in ARDS, as they worsen the condition.[46] As mentioned ear- pinephrine exogenously will further worsen the condition. Many
lier, beta2-adrenergic agonists like salbutamol used in the nebu- have raised concerns about the use of norepinephrine in sep-
lizer solutions, increase the plasma catecholamine level, and pro- tic shock, as norepinephrine may worsen the condition and in-
duce hypercoagulable state.[31–33] Considering the vicious ARAS crease the mortality rate in septic shock.[47–50] Not only increased
loop, I suggest beta2-adrenergic agonists should be avoided in catecholamine but also increased RAAS activation is detrimen-
the nebulizer solutions, as they may worsen the clinical condi- tal in sepsis patients. It has been shown that increased ATII and
tion in COVID-19 patients and may produce complications like plasma renin activity worsen the sepsis condition.[51] Recent stud-
pulmonary embolism. ies showed that beta-adrenergic blockers may be beneficial in
BioEssays 2020, 42, 2000094 2000094 (4 of 9) © 2020 Wiley Periodicals LLC
www.advancedsciencenews.com www.bioessays-journal.com
Figure 2. The effect of beta-adrenergic blockers on RAAS and COVID-19: A) Beta-adrenergic blockers by their inhibitory action on the sympathetic
nervous system decrease renin release by juxtaglomerular (JG) cells in the Kidney. A decrease in renin may reduce activity in both arms of the RAAS, and
may decrease ACE2 receptor expression on cells. B) Beta-adrenergic blockers decrease ACE2 receptor abundance, hence reducing the opportunities for
SARS-CoV-2 cellular entry and thereby reducing viral infectivity. Beta-adrenergic blockers reduce mortality in cases of ARDS, septic shock and respiratory
failure. Beta-adrenergic blockers may inhibit the NLRP3 inflammasome, reduce IL-6 level, decrease mucus secretion, reduce the pulmonary edema,
pulmonary embolism, and refractory hypoxemia complications.
septic shock.[52,53] I suggest that norepinephrine should not be receptor for SARS-CoV-2, beta-adrenergic blockers may decrease
used in the treatment of COVID-19 patients with septic shock, the cellular entry of SARS-CoV-2. It is already known that beta-
instead beta-adrenergic blockers should be used. adrenergic blocker propranolol down-regulates CD147.[54] There-
fore, beta-adrenergic blockers treatment in COVID-19 patients
may reduce the cellular entry of SARS-COV-2 via downregula-
2. Beta-Adrenergic Blocker Treatment in tion of the ACE2 receptor as well as CD147.
COVID-19: How They Work, and Why They Hold
Promise in Treating COVID-19?
2.2. Beta Adrenergic Blockers Reduce IL-6
The aforementioned considerations suggest that beta-adrenergic
blockers like Propranolol should be used in COVID-19 patients, It is known that activation of beta-adrenergic receptors plays a
as per the schematic reasoning presented in Figure 2. Here, I role in the IL-6 secretion.[55] It is also known that beta-adrenergic
focus mainly on the beta-adrenergic blocker’s role in COVID-19. blockers decrease IL-6 in cardiac disorder patients.[56,57] I suggest
Which subtype of beta-adrenergic receptor blocker plays a crucial beta-adrenergic blockers will reduce the IL-6 level in COVID-19
role in COVID-19 remains to be seen. It is possible that alpha1 patients and reduce the inflammatory complications associated
adrenergic blockers such as Prazosin or combination of beta- with it.
and alpha-adrenergic blockers may also be beneficial in COVID-
19. I discuss the advantages of using beta-adrenergic blockers in
COVID-19 in the following section. 2.3. Beta Adrenergic Blockers Decrease Proinflammatory
Cytokines and Inhibit Cytokine Storm
2.1. Beta-Adrenergic Blockers Reduce the SARS-COV-2 Beta-adrenergic blockers have been shown to decrease a variety
Host Cell Entry of proinflammatory cytokines expression including IL-1𝛽, IL-6,
TNF𝛼, IFN𝛾.[56–60] The use of beta-adrenergic blockers in COVID-
Beta-blockers by its negative regulation on the juxtaglomerular 19 patients may reduce the cytokine storm by decreasing the ex-
cells in the kidney reduce the activity of both arms of the RAAS pression of the proinflammatory cytokines and the inflammation
pathway, thereby it may decrease the ACE2 level. As ACE2 is the associated with it.
BioEssays 2020, 42, 2000094 2000094 (5 of 9) © 2020 Wiley Periodicals LLC
www.advancedsciencenews.com www.bioessays-journal.com
2.4. Beta-Adrenergic Blockers Might be Beneficial in ARDS 2.8. Improvement of Oxygenation level by Beta Adrenergic
and Respiratory Failure Condition Blockers
It is known that beta-adrenergic agonists counterintuitively Beta-adrenergic blockers have been shown to improve the oxy-
worsen the ARDS condition and beta-adrenergic blockers have genation level in the patients who were on ECMO.[66] This
been shown to reduce the mortality in ARDS.[46] Based on suggests the possibility that the use of beta-adrenergic block-
the BASEL II ICU study Noveanu et al had shown that ers in COVID-19 patients who are on ECMO may improve
beta-adrenergic blockers reduce mortality in respiratory failure the oxygenation level. It has been shown that beta-adrenergic
cases.[61] A recent study has shown that beta-adrenergic blockers blockers improved the oxygenation level in the hypoxic con-
reduce mortality in ARDS.[62] dition induced in an animal study.[67] It is known that beta-
adrenergic blockers improve the Pa O2 level in critically ill patients
and increase the oxygenation.[68,69] Considering the above evi-
dences, I hypothesize that beta-adrenergic blockers may improve
2.5. Beta-Adrenergic Blockers are Beneficial in Septic Shock the oxygenation level and reduce the hypoxemia in COVID-19
patients.
Recent trends suggest that beta-adrenergic blockers are benefi-
cial in septic shock and reduce the mortality rate.[52,53] As men-
tioned earlier, many have raised concerns about the use of nore- 2.9. Beta-Adrenergic Blockers May Reduce the Mucus
pinephrine in septic shock.[47–50] I suggest that norepinephrine Hypersecretion in COVID-19
for treating septic shock in the COVID-19 condition should be
avoided. Instead beta-adrenergic blockers should be used for Increased mucus aggregation has been noticed in the distal
treating septic shock in COVID-19 patients. airways and alveoli in the postmortem study of COVID-19
patients.[10] It is known that IL-6 plays a key role in the activa-
tion of MUC5AC and MUC5B gene expression and increases the
mucus secretion.[11] It has been suggested that Tocilizumab by
2.6. Beta-Adrenergic Blockers May Reduce the Pulmonary Edema the inhibition of IL-6 receptor may help decrease the mucus se-
cretion in COVID-19.[12] As mentioned earlier, beta-adrenergic
As mentioned earlier, increased catecholamine levels may trig- blockers decrease IL-6. It is interesting to note that chronic pro-
ger the ARAS loop and worsen the COVID-19. It is well known pranolol administration has been shown to decrease MUC5AC
that increased catecholamine induces pulmonary edema in the expression and mucus secretion.[70] I hypothesize that the use of
animal model studies. Studies have shown that both alpha- and beta-adrenergic blockers like propranolol may decrease the mu-
beta-adrenergic receptors may be involved in this. Both alpha1 cus secretion in COVID-19 patients.
and beta-adrenergic blockers have shown to relieve pulmonary
edema in many animal models studies. Due to adrenergic recep-
tor involvement in the etiology of pulmonary edema, it has been 2.10. Computational Studies Suggest the Potential use of
suggested that beta-2 agonists should not be used routinely in Beta-Adrenergic Blocker in COVID-19
the mechanically ventilated patients.[63] Increased catecholamine
level induced pulmonary edema can be prevented by adrenergic Wu et al. using the computational method has shown some po-
receptor blockers. I suggest that beta-adrenergic blockers like tential molecules that could be used for the treatment in COVID-
Propranolol or alpha1 adrenergic blockers like Prazosin should 19. In the article, beta-adrenergic blocker Oxprenolol has been
be used to reduce or prevent pulmonary edema in COVID-19 suggested to potentially inhibit SARS-CoV-2 papain-like protease
patients. (PLpro) and Carvedilol has been suggested to potentially inhibit
SARS-CoV-2 3-chymotrypsin like protease.[71] Using a network-
based approach Zhou et al shown 16 potential drugs that can be
used in the treatment of COVID-19 and one of the drugs men-
2.7. Beta Adrenergic Blockers May Reduce the Hypercoagulation tioned was beta-adrenergic blocker Carvedilol.[23] The above two
State and Prevent Pulmonary Embolism in COVID-19 Patients recent computational studies support the hypothesis that beta-
adrenergic blockers may be useful in the treatment of COVID-19
Severely affected COVID-19 patients developed pulmonary em- patients.
bolism in COVID-19 and D-dimer level was shown to be
high.[15–17] This indicates that the hypercoagulation state occurs
in COVID-19. Adrenergic hyperactivation is known to be asso- 2.11. Beta-Adrenergic Blockers Inhibit NLRP3 Inflammasome
ciated with the hypercoagulation state. Beta-adrenergic block-
ers have been shown to reduce the coagulation parameters and As mentioned earlier, NLRP3 has been suggested to be activated
prevent complications like venous thrombosis in both animal in COVID-19 and a clinical trial targeting the inhibition of NLRP3
models and patients.[64,65] I suggest that beta-adrenergic blockers using Colchicine is already registered.[25] It is interesting to note
should be used in COVID-19 patients to prevent or reduce the that beta-adrenergic blocker carvedilol has been shown to inhibit
hypercoagulation state complications like pulmonary embolism NLRP3 inflammasome.[72] Thus, one of the many uses of beta-
and deep vein thrombosis. adrenergic blockers in COVID-19 condition may be the inhibi-
BioEssays 2020, 42, 2000094 2000094 (6 of 9) © 2020 Wiley Periodicals LLC
www.advancedsciencenews.com www.bioessays-journal.com
tion of NLRP3 inflammasome and thereby reducing the inflam- COVID-19 patients in many ways ranging from decreasing the
mation by decreasing the NLRP3 downstream effectors IL-1 and SARS-CoV-2 virus entry, inhibiting NLRP3 inflammasome, re-
IL-8. duction of IL-6 to decreasing the complications such as pul-
monary embolism, ARDS, and septic shock. It is important now
to act quickly and do retrospective clinical studies on the COVID-
2.12. Use of Beta-Adrenergic Blockers are Safe in Respiratory 19 patients who were already on beta-adrenergic blockers for pre-
Illness Condition existing cardiovascular illness, and assess their effect on mortal-
ity. The proposed retrospective studies will test the validity of the
Traditionally clinicians are hesitant in using beta-blockers in pa- hypothesis that I develop in this paper. If the retrospective study
tients with respiratory illness. But recent studies are changing result transpires as expected, it would help millions of people all
this viewpoint, for example, beta-adrenergic blockers have been over the world, because beta-adrenergic blockers are well-known
shown beneficial effects in chronic obstructive pulmonary dis- drugs with longstanding safety profiles. Furthermore, they are
ease (COPD) patients.[73] I suggest that clinicians should not hes- relatively inexpensive, can be taken orally and intravenously, and
itate to use beta-adrenergic blockers in COVID-19 patients having are readily available in all parts of the world. It is imperative to
respiratory dysfunction. do the proposed retrospective and prospective clinical trial stud-
Considering the above evidence beta-adrenergic blockers like ies as soon as possible, with the aim of clarifying the role of beta-
Propranolol may be a good candidate for treating COVID-19 pa- adrenergic blockers in COVID-19 patients.
tients. As mentioned earlier which subtype of beta-adrenergic re-
ceptor blocker works better in COVID-19 needs to be clarified in
the future. It is possible that alpha1-adrenergic blockers like Pra- Acknowledgements
zosin or combination of beta and alpha-adrenergic blockers may
also be beneficial in COVID-19. The author would like to thank Dr. Raja for his help in editing the
manuscript.
3. Testing of the Hypothesis
Conflict of Interest
3.1. Testing the Existence of ARAS Loop and Sympathetic Storm
in COVID-19 Patients The authors declare no conflict of interest.
To check the presence of the hypothetical ARAS loop, I suggest Keywords
measuring the following in COVID-19 patients—plasma cate-
cholamine levels especially plasma norepinephrine levels, AT II, ACE2, ARDS, beta-adrenergic blockers, COVID-19, pulmonary embolism,
ACE, ACE2, Renin levels. These parameters need to be mea- SARS-CoV-2, septic shock
sured in all the COVID-19 patients along with the viral load mea-
Received: April 30, 2020
surement. If the plasma concentration of above said ARAS loop
Revised: July 28, 2020
molecules correlates with the viral load in the COVID-19, it would Published online: September 2, 2020
validate the existence of the ARAS loop in COVID-19. The plasma
catecholamine levels in COVID-19 patients have to be measured
in all the COVID-19 patients which would clarify whether a sym-
pathetic storm occurs in this condition. [1] https://www.who.int/docs/default-source/coronaviruse/situation-
reports/20200726-covid-19-sitrep-188.pdf?sfvrsn=f177c3fa_2
(accessed: July 2020).
3.2. Retrospective and Prospective Clinical Trials Would Test the
[2] M. Hoffmann, H. Kleine-Weber, S. Schroeder, N. Krüger, T. Herrler,
Effect of Beta-Adrenergic Blockers in COVID-19 Patients S. Erichsen, T. S. Schiergens, G. Herrler, N. H. Wu, A. Nitsche, M. A.
Müller, C. Drosten, S. Pöhlmann, Cell 2020, 181, 271.e8.
I suggest conducting retrospective and prospective clinical trials [3] H. Zhang, J. M. Penninger, Y. Li, N. Zhong, A. S. Slutsky, Intensive
to clarify the following questions; Care Med. 2020, 46, 586.
[4] H. Ulrich, M. M. Pillat, Stem Cell Rev. Rep. 2020, 16, 434.
i. Do beta-adrenergic blockers reduce the morbidity and mor- [5] K. Wang, W. Chen, Y. S. Zhou, J. Q. Lian, Z. Zhang, P. Du, L. Gong, Y.
tality in COVID-19 patients? Zhang, H. Y. Cui, J. J. Geng, B. Wang. SARS-CoV-2 invades host cells
ii. Do beta-adrenergic blockers reduce the SARS-CoV-2 host cell via a novel route: CD147-spike protein. BioRxiv. 2020 Jan 1 (accessed:
entry and viral load? July 2020).
[6] R. T. Gandhi, J. B. Lynch, C. Del Rio, N. Engl. J. Med. 2020.
[7] X. Cao, Nat. Rev. Immunol. 2020, 20, 269.
[8] F. Zhou, T. Yu, R. Du, G. Fan, Y. Liu, Z. Liu, J. Xiang, Y. Wang, B. Song,
4. Conclusion X. Gu, L. Guan, Y. Wei, H. Li, X. Wu, J. Xu, S. Tu, Y. Zhang, H. Chen,
B. Cao, Lancet 2020, 395, 1054.
The interrelationship between the adrenergic system, RAAS, [9] B. M. Henry, Lancet Respir. Med. 2020, 8, e24.
ACE2, and SARS-CoV-2 plays a crucial role in COVID-19 pathol- [10] C. Wang, J. Xie, L. Zhao, X. Fei, H. Zhang, Y. Tan, X. Nie, L. Zhou, Z.
ogy. I propose a hypothetical ARAS loop, hyperactivation of which Liu, Y. Ren, L. Yuan, Y.u Zhang, J. Zhang, L. Liang, X. Chen, X. Liu, P.
may be the pathophysiological mechanism behind COVID- Wang, X. Han, X. Weng, Y. Chen, T. Yu, X. Zhang, J. Cai, R. Chen, Z.-L.i
19. Beta-adrenergic blockers may produce beneficial effects in Shi, X.-W.u Bian, EBioMedicine 2020, 57, 102833.
BioEssays 2020, 42, 2000094 2000094 (7 of 9) © 2020 Wiley Periodicals LLC
www.advancedsciencenews.com www.bioessays-journal.com
[11] Y. Chen, P. Thai, Y.u-H. Zhao, Y.e-S. Ho, M. M. Desouza, R. Wu, J. Biol. [31] E. M. Snyder, E. C. Wong, W. T. Foxx-Lupo, C. M. Wheatley, N. A.
Chem. 2003, 278, 17036. Cassuto, A. E. Patanwala, Pharmacother.: J. Hum. Pharmacol. Drug
[12] Z. Zhu, T. Cai, L. Fan, K. Lou, X. Hua, Z. Huang, G. Gao, Int. J. Infect. Ther. 2011, 31, 748.
Dis. 2020, 95, 332. [32] R. Von Kanel, J. E. Dimsdale, Eur. J. Haematol. 2000, 65, 357.
[13] H. Zhang, P. Zhou, Y. Wei, H. Yue, Y.i Wang, M. Hu, S. Zhang, [33] M. Ali-Saleh, G. Sarig, J. N. Ablin, B. Brenner, G. Jacob, PLoS One
T. Cao, C. Yang, M. Li, G. Guo, X. Chen, Y. Chen, M. Lei, H. Liu, 2016, 11, e0158652.
J. Zhao, P. Peng, C.-Y.i Wang, R. Du, Ann. Intern. Med. 2020, 172, [34] J. M. Sanders, M. L. Monogue, T. Z. Jodlowski, J. B. Cutrell, JAMA
629. 2020, 323, 1824.
[14] https://www.who.int/publications/i/item/clinical-management-of- [35] https://www.covid19treatmentguidelines.nih.gov/whats-new/
severe-acute-respiratory-infection-when-novel-coronavirus-(ncov)- (accessed: July 2020).
infection-is-suspected (accessed: July 2020). [36] B. M. Henry, G. Lippi, J. Crit. Care 2020, 58, 27.
[15] I. Leonard-Lorant, X. Delabranche, F. Severac, J. Helms, C. Pauzet, [37] S. A. Ñamendys-Silva, Heart Lung J. Crit. Care 2020, 49, 348.
O. Collange, F. Schneider, A. Labani, P. Bilbault, S. Moliere, P. Leyen- [38] A. C. Groves, J. Griffiths, F. Leunc, R. N. Meek, Ann. Surg. 1973, 178,
decker, C. Roy, M. Ohana, Radiology 2020, 201561. 102.
[16] J. Poissy, J. Goutay, M. Caplan, E. Parmentier, T. Duburcq, F. Lassalle, [39] J. W. Mason, E. L. Buescher, M. L. Belfer, M. S. Artenstein, E. H.
E. Jeanpierre, A. Rauch, J. Labreuche, S. Susen, Circulation 2020, 142, Mougey, J. Hum. Stress 1979, 5, 18.
184. [40] L. A. Rabelo, N. Alenina, M. Bader, Hypertens. Res. Off. J. Jpn. Soc.
[17] F. Grillet, J. Behr, P. Calame, S. Aubry, E. Delabrousse, Radiology 2020, Hypertens. 2011, 34, 154.
201544, 296, E186. [41] M. Esler, D. Esler, J. Hypertens. 2020, 38, 781.
[18] Z. Wu, J. M. Mcgoogan, JAMA 2020, 323, 1239. [42] L. Fang, G. Karakiulakis, M. Roth, Lancet Respir. Med. 2020, 8,
[19] A. Rhodes, L. E. Evans, W. Alhazzani, M. M. Levy, M. Antonelli, R. e21.
Ferrer, A. Kumar, J. E. Sevransky, C. L. Sprung, M. E. Nunnally, B. [43] G. M. Kuster, O. Pfister, T. Burkard, Q. Zhou, R. Twerenbold, P. Haaf,
Rochwerg, G. D. Rubenfeld, D. C. Angus, D. Annane, R. J. Beale, G. A. F. Widmer, S. Osswald, Eur. Heart J. 2020, 41, 1801.
J. Bellinghan, G. R. Bernard, J. D. Chiche, C. Coopersmith, D. P. De [44] M. Vaduganathan, O. Vardeny, T. Michel, J. J. V. Mcmurray, M. A. Pf-
Backer, C. J. French, S. Fujishima, H. Gerlach, J. L. Hidalgo, S. M. effer, S. D. Solomon, N. Engl. J. Med. 2020, 382, 1653.
Hollenberg, A. E. Jones, D. R. Karnad, R. M. Kleinpell, Y. Koh, T. C. [45] T. Yamamoto, L.i-M. Wang, K. Shimakura, M. Sanaka, Y. Koike, S. Mi-
Lisboa, F. R. Machado, J. J. Marini, J. C. Marshall, J. E. Mazuski, L. neshita, Jpn. J. Pharmacol. 1997, 73, 33.
A. Mcintyre, A. S. Mclean, S. Mehta, R. P. Moreno, J. Myburgh, P. [46] R. M. Sweeney, D. F. McAuley, Lancet 2016, 388, 2416.
Navalesi, O. Nishida, T. M. Osborn, A. Perner, C. M. Plunkett, M. [47] R. F. Stolk, T. Van Der Poll, D. C. Angus, J. G. Van Der Hoeven, P.
Ranieri, C. A. Schorr, M. A. Seckel, C. W. Seymour, L. Shieh, K. A. Pickkers, M. Kox, Am J. Respir. Crit. Care Med. 2016, 194, 550.
Shukri, S. Q. Simpson, M. Singer, B. T. Thompson, S. R. Townsend, [48] C. Martin, S. Medam, F. Antonini, J. Alingrin, M. Haddam, E. Ham-
T. Van Der Poll, J. L. Vincent, W. J. Wiersinga, J. L. Zimmerman, R. P. mad, B. Meyssignac, C. Vigne, L. Zieleskiewicz, M. Leone, Shock
Dellinger, Intensive Care Med. 2017, 43, 304. 2015, 44, 305.
[20] S. F. Pedersen, Y. A. C. Ho, J. Clin. Invest. 2020, 130, 2202. [49] V. Natesan, Int. J. Clin. Exp. Physiol. 2018, 5, 3.
[21] P. Mehta, D. F. Mcauley, M. Brown, E. Sanchez, R. S. Tattersall, J. J. [50] M. Singer, Lancet 2007, 370, 636.
Manson, Lancet 2020, 395, 1033. [51] K. C. Doerschug, A. S. Delsing, G. A. Schmidt, A. Ashare, Crit. Care
[22] X. Zhang, K. Wu, D. I. Wang, X. Yue, D. Song, Y. Zhu, J. Wu, Virology 2010, 14, R24.
2007, 365, 324. [52] S. Coppola, S. Froio, D. Chiumello, Crit. Care 2015, 19, 119.
[23] Y. Zhou, Y. Hou, J. Shen, Y. Huang, W. Martin, F. Cheng, Cell Discov. [53] K. Tan, M. Harazim, B. Tang, A. Mclean, M. Nalos, Crit. Care. 2019,
2020, 6, 1. 23, 298.
[24] X. Chen, B. Zhao, Y. Qu, J. Xiong, Y. Feng, D. Men, Q. Huang, Y. Liu, [54] W. Xie, H. Xie, F. Liu, W. Li, J. Dan, L. Liu, L. Dan, X. Xiao, J. Li, X.
B. Yang, J. Ding, Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2020. Chen, Br. J. Dermatol. 2013, 168, 739.
[25] S. G. Deftereos, G. Siasos, G. Giannopoulos, D. A. Vrachatis, C. [55] C. Chen, J. Du, W. Feng, Y. Song, Z. Lu, M. Xu, Z. Li, Y. Zhang, Br. J.
Angelidis, S. G. Giotaki, P. Gargalianos, H. Giamarellou, C. Gogos, Pharmacol. 2012, 166, 676.
G. Daikos, M. Lazanas, P. Lagiou, G. Saroglou, N. Sipsas, S. Tsio- [56] Y. C. Doo, D. M. Kim, D. J. Oh, K. H. Ryu, C. Y. Rhim, Y. Lee, Am. J.
dras, D. Chatzigeorgiou, N. Moussas, A. Kotanidou, N. Koulouris, E. Cardiol. 2001, 88, 422.
Oikonomou, A. Kaoukis, C. Kossyvakis, K. Raisakis, K. Fountoulaki, [57] T. Matsumura, K. Tsushima, E. Ohtaki, K. Misu, T. Tohbaru, R. Asano,
M. Comis, D. Tsiachris, E. Sarri, A. Theodorakis, L. Martinez-Dolz, J. M. Nagayama, K. Kitahara, J. Umemura, T. Sumiyoshi, S. Hosoda, J.
Sanz-Sanchez, B. Reimers, G. G. Stefanini, M. Cleman, D. Filippou, C. Cardiol. 2002, 39, 253.
D. Olympios, V. N. Pyrgakis, J. Goudevenos, G. Hahalis, T. M. Kolet- [58] A. Deten, H. C. Volz, A. Hölzl, W. Briest, H. G. Zimmer, Mol. Cell.
tis, E. Iliodromitis, D. Tousoulis, C. Stefanadis, Hell. J. Cardiol. 2020, Biochem. 2003, 251, 127.
61, 42. [59] F. Hajighasemi, A. Mirshafiey, Int. J. Hematol.-Oncol. Stem Cell Res.
[26] K. L. Siu, K. S. Yuen, C. Castano-Rodriguez, Z. W. Ye, M. L. Yeung, S. 2016, 10, 99.
Y. Fung, S. Yuan, C. P. Chan, K. Y. Yuen, L. Enjuanes, D. Y. Jin, FASEB [60] C. Woiciechowsky, B. Schöning, G. Stoltenburg-Didinger, F. Stock-
J. 2019, 33, 8865. hammer, H. D. Stockhammer, Med. Sci. Monit. Int. Med. J. Exp. Clin.
[27] I. Y. Chen, M. Moriyama, M. F. Chang, T. Ichinohe, Front. Microbiol. Res. 2004, 10, BR325.
2019, 10. [61] M. Noveanu, T. Breidthardt, T. Reichlin, E. Gayat, M. Potocki, H.
[28] Y. Yang, H. Wang, M. Kouadir, H. Song, F. Shi, Cell Death Dis. 2019, Pargger, A. Heise, J. Meissner, R. Twerenbold, N. Muravitskaya, A.
10, 1. Mebazaa, C. Mueller, Crit. Care. 2010, 14, R198.
[29] K. E. Greene, J. R. Wright, K. P. Steinberg, J. T. Ruzinski, E. Caldwell, [62] M. O. Al-Qadi, R. Kashyap, Am J. Respir. Crit. Care Med. 2015, 191, p.
W. B. Wong, W. Hull, J. A. Whitsett, T. Akino, Y. Kuroki, H. Nagae, L. A1602.
D. Hudson, T. R. Martin, Am J. Respir. Crit. Care Med. 1999, 160, 1843. [63] B. Rassler, Scientifica 2012, 2012, 1.
[30] J. Yu, L. Ni, X. Zhang, J. Zhang, O. Abdel-Razek, G. Wang, Shock 2019, [64] M. Gruszecki, R. Rółkowski, R. Pawlak, W. Buczko, Pol. J. Pharmacol.
51, 557. 2001, 53, 5.
BioEssays 2020, 42, 2000094 2000094 (8 of 9) © 2020 Wiley Periodicals LLC
www.advancedsciencenews.com www.bioessays-journal.com
[65] M. R. Hoppener, R. A. Kraaijenhagen, B. A. Hutten, H. R. Buller, R. J. [70] Y. Zhou, Y. Zhang, Y. Guo, Y. Zhang, M. Xu, B. He, PLoS One 2014, 9,
G. Peters, M. Levi, J. Thromb. Haemost. JTH 2004, 2, 1316. e97788.
[66] J. J. H. Bunge, S. Diaby, A. L. Valle, J. Bakker, D. Gommers, J. L. Vin- [71] C. Wu, Y. Liu, Y. Yang, P. Zhang, W.u Zhong, Y. Wang, Q. Wang, Y. Xu,
cent, J. Creteur, F. S. Taccone, D. Reis Miranda, J. Crit. Care 2019, 53, M. Li, X. Li, M. Zheng, L. Chen, H. Li, Acta Pharm. Sin. B 2014, 10,
248. 766.
[67] H. J. Khambatta, J. G. Stone, J. Askanazi, E. Khan, Br. J. Anaesth. 1987, [72] W. T. Wong, L. H. Li, Y. K. Rao, S. P. Yang, S. M. Cheng, W. Y.
59, 1171. Lin, C. C. Cheng, A. Chen, K. F. Hua, Front. Immunol. 2018, 9,
[68] J. L. Vincent, H. Lignian, J. B. Gillet, J. Berre, E. Contu, Chest 1985, 88, 1920.
558. [73] A. O. Nielsen, L. Pedersen, B. F. Sode, M. Dahl, EClinicalMedicine
[69] G. Wood, Crit. Care Med. 1997, 25, 1807. 2019, 7, 21.
BioEssays 2020, 42, 2000094 2000094 (9 of 9) © 2020 Wiley Periodicals LLC
You might also like
- Emergency Care Algorithms 2018 PDFDocument77 pagesEmergency Care Algorithms 2018 PDFFranklin Correa100% (2)
- HESI Study GuideDocument38 pagesHESI Study GuideJeffrey Viernes100% (3)
- Acute Respiratory Distress Syndrome (ARDS) : MR Sanjay. M. Peerapur, Principal, KLES Institute of Nursing Sciences, HubliDocument22 pagesAcute Respiratory Distress Syndrome (ARDS) : MR Sanjay. M. Peerapur, Principal, KLES Institute of Nursing Sciences, Hublimanish dafdaNo ratings yet
- Complications of FracturesDocument13 pagesComplications of FracturesmilananandNo ratings yet
- Ot - Role of Ot in Pulmonary RehabDocument32 pagesOt - Role of Ot in Pulmonary RehabAlyssa Bituin100% (1)
- ARDS With PathophysiologyDocument79 pagesARDS With Pathophysiologymabec pagaduan95% (19)
- Chapter 38 - Thoracic TraumaDocument24 pagesChapter 38 - Thoracic TraumaHamilton Delgado100% (1)
- Abdominal Compartment Syndrome PDFDocument326 pagesAbdominal Compartment Syndrome PDFviaereaNo ratings yet
- 2009 Grainger & Allison'sDocument409 pages2009 Grainger & Allison'sGabriel Callupe100% (4)
- A Study On Impact of Covid 19 OnDocument108 pagesA Study On Impact of Covid 19 OnFaisal ArifNo ratings yet
- Acute Respiratory Distress Syndrome 2022Document182 pagesAcute Respiratory Distress Syndrome 2022Dalí Fuentes GonzalezNo ratings yet
- SuctioningDocument17 pagesSuctioningKandi Issaya100% (1)
- Medical HypothesesDocument5 pagesMedical Hypothesesnow youloseNo ratings yet
- 2022 - Bishop StudyDocument10 pages2022 - Bishop StudyGustavo ResendeNo ratings yet
- Comprehensive Treatment COVID 19Document49 pagesComprehensive Treatment COVID 19ekoNo ratings yet
- The Role of Janus Kinases in The Pathogenesis and Treatment of Covid-19 OJPRMDocument31 pagesThe Role of Janus Kinases in The Pathogenesis and Treatment of Covid-19 OJPRMayron600No ratings yet
- 8 DBFDocument4 pages8 DBFFatimaNo ratings yet
- Editorial: COVID-19: An Unexpected Indication For Anti-Rheumatic Therapies?Document4 pagesEditorial: COVID-19: An Unexpected Indication For Anti-Rheumatic Therapies?dayuseed001No ratings yet
- Anticoagulant Treatment in COVID 19: A Narrative ReviewDocument7 pagesAnticoagulant Treatment in COVID 19: A Narrative ReviewossinNo ratings yet
- Title: Mass Cytometry and Artificial Intelligence Define CD169 As A Specific Marker of SARSDocument32 pagesTitle: Mass Cytometry and Artificial Intelligence Define CD169 As A Specific Marker of SARSいちらさみNo ratings yet
- Original Research ArticleDocument21 pagesOriginal Research ArticlePrabhuNo ratings yet
- Supplementation With Vitamin D in The COVID-19 Pandemic?: Nutrition in Clinical CareDocument9 pagesSupplementation With Vitamin D in The COVID-19 Pandemic?: Nutrition in Clinical Caresuci argithaNo ratings yet
- Is COVID-19 A New Hematologic Disease?Document5 pagesIs COVID-19 A New Hematologic Disease?Liya AnjelinaNo ratings yet
- Kinins and Cytokines in COVID-19: A Comprehensive Pathophysiological ApproachDocument18 pagesKinins and Cytokines in COVID-19: A Comprehensive Pathophysiological ApproachRara AuliaNo ratings yet
- E499 FullDocument6 pagesE499 FullAlizaPinkyNo ratings yet
- COVID-19 and Coagulopathy: Malay Sarkar - Irappa V. Madabhavi - Pham Nguyen Quy - Manjunath B. GovindagoudarDocument16 pagesCOVID-19 and Coagulopathy: Malay Sarkar - Irappa V. Madabhavi - Pham Nguyen Quy - Manjunath B. GovindagoudarsamuelNo ratings yet
- Covid - 19Document14 pagesCovid - 19saravana kumarNo ratings yet
- 2021-COVID-19-Related Arrhythmias and The Possible Effects of RanolazineDocument4 pages2021-COVID-19-Related Arrhythmias and The Possible Effects of RanolazineNurettin AbacıoğluNo ratings yet
- Jurnal C - 19Document10 pagesJurnal C - 19Echy SanndahNo ratings yet
- Journal Pre-Proof: Cytokine and Growth Factor ReviewsDocument27 pagesJournal Pre-Proof: Cytokine and Growth Factor ReviewsTufik NaderNo ratings yet
- Medical Hypotheses: Ziad A. Ali, Rif S. El-Mallakh TDocument3 pagesMedical Hypotheses: Ziad A. Ali, Rif S. El-Mallakh TRobert ChristevenNo ratings yet
- Life Sciences: Rishabh Hirawat, Mohd Aslam Saifi, Chandraiah GoduguDocument14 pagesLife Sciences: Rishabh Hirawat, Mohd Aslam Saifi, Chandraiah GoduguPaoloMafaldoNo ratings yet
- Perspectives: Endothelial Dysfunction and Immunothrombosis As Key Pathogenic Mechanisms in COVID-19Document11 pagesPerspectives: Endothelial Dysfunction and Immunothrombosis As Key Pathogenic Mechanisms in COVID-19Jackson ErasmoNo ratings yet
- Endothelial Dysfunction and ImmunothrombosisDocument11 pagesEndothelial Dysfunction and ImmunothrombosisJob GonzagaNo ratings yet
- Cholesterol Covid19Document9 pagesCholesterol Covid19Rheum RaponticumNo ratings yet
- Spice Prophylactic Use in COVID-19 in India & Lower DamageDocument8 pagesSpice Prophylactic Use in COVID-19 in India & Lower DamageUtkarsh GhateNo ratings yet
- Hypokalemia and Clinical Implications in Patients With Coronavirus Disease 2019 (COVID-19)Document22 pagesHypokalemia and Clinical Implications in Patients With Coronavirus Disease 2019 (COVID-19)M. Fakhrul AnamNo ratings yet
- Viral CoagulopathyDocument7 pagesViral CoagulopathyGheavita Chandra DewiNo ratings yet
- Nuaa 081Document9 pagesNuaa 081Andrea G.No ratings yet
- N Acetilcisteína COVID19Document9 pagesN Acetilcisteína COVID19Luis C Ribon VNo ratings yet
- N Acetilcisteína COVID19 PDFDocument9 pagesN Acetilcisteína COVID19 PDFLuis C Ribon VNo ratings yet
- Journal of Clinical MedicineDocument12 pagesJournal of Clinical MedicineGonzalo Gobbi100% (1)
- Kidney Diseases in The Time of COVID-19: Major Challenges To Patient CareDocument4 pagesKidney Diseases in The Time of COVID-19: Major Challenges To Patient CareJeff LapianNo ratings yet
- Acute Kidney Injury in Hospitalized Patients With Coronavirus Disease 2019 (Covid-19) and Literature ReviewDocument5 pagesAcute Kidney Injury in Hospitalized Patients With Coronavirus Disease 2019 (Covid-19) and Literature ReviewIJAR JOURNALNo ratings yet
- Predictors of Mortality of Covid-19 Infected Patients With Acute Kidney InjuryDocument7 pagesPredictors of Mortality of Covid-19 Infected Patients With Acute Kidney InjuryKevin TandartoNo ratings yet
- Pharmacotherapy in Covid 19 Potential Impact of Targeting The Complement SystemDocument12 pagesPharmacotherapy in Covid 19 Potential Impact of Targeting The Complement SystemDENiS ROSARIO CASABONA ACEVEDONo ratings yet
- Molecules: Can Natural Polyphenols Help in Reducing Cytokine Storm in COVID-19 Patients?Document14 pagesMolecules: Can Natural Polyphenols Help in Reducing Cytokine Storm in COVID-19 Patients?Sammy HolidayNo ratings yet
- Nutrition: Adam F. Feyaerts PH.D., Walter Luyten PH.D., M.DDocument4 pagesNutrition: Adam F. Feyaerts PH.D., Walter Luyten PH.D., M.DVania ZahraNo ratings yet
- Sri Ratu Septini Farmasi 4B PDFDocument8 pagesSri Ratu Septini Farmasi 4B PDFWinanda SitinjakNo ratings yet
- Convalescent PlasmaDocument42 pagesConvalescent PlasmaOlaniyi John OlajideNo ratings yet
- Main PDFDocument4 pagesMain PDFRSDC Tower 5No ratings yet
- The Neurological Manifestations of COVID-19 - NEUROL SCI 2020Document5 pagesThe Neurological Manifestations of COVID-19 - NEUROL SCI 2020Nicole Ferreira PiccoliNo ratings yet
- AKI Pada Covid19Document10 pagesAKI Pada Covid19ita maghfirah IlhamjayaNo ratings yet
- Covid 19 NsaidDocument5 pagesCovid 19 Nsaidsstefan888No ratings yet
- Jurnal LR 1Document9 pagesJurnal LR 1ENRICO 102011216No ratings yet
- HipocalemiaDocument22 pagesHipocalemiaitalofabregaNo ratings yet
- Reviews: COVID-19 and Cardiovascular Disease: From Basic Mechanisms To Clinical PerspectivesDocument16 pagesReviews: COVID-19 and Cardiovascular Disease: From Basic Mechanisms To Clinical PerspectivesLAURA ALEJANDRA PARRA GOMEZNo ratings yet
- Cytokine Storm Is The Cryptic Killer Behind.9Document9 pagesCytokine Storm Is The Cryptic Killer Behind.9Aanchal DeviNo ratings yet
- Clinical Features, Ventilatory Management, and Outcome of ARDS Caused by COVID-19 Are Similar To Other Causes of ARDS-5Document12 pagesClinical Features, Ventilatory Management, and Outcome of ARDS Caused by COVID-19 Are Similar To Other Causes of ARDS-5hemodiálise NIRNo ratings yet
- Abbas If Ard 2020Document10 pagesAbbas If Ard 2020amamggNo ratings yet
- Life Sciences: Review ArticleDocument10 pagesLife Sciences: Review ArticleTufik NaderNo ratings yet
- COVID-19 - Verma - 2020Document13 pagesCOVID-19 - Verma - 2020Bayu SomantaraNo ratings yet
- 2020 Emerging Blood Gas MonitorsDocument15 pages2020 Emerging Blood Gas MonitorsSHANU KUMARNo ratings yet
- The Association of Cardiovascular Diseases and Diabetes Mellitus With COVID-19 (SARS-CoV-2) and Their Possible MechanismsDocument6 pagesThe Association of Cardiovascular Diseases and Diabetes Mellitus With COVID-19 (SARS-CoV-2) and Their Possible MechanismsPatty MArivel ReinosoNo ratings yet
- Imaging in COVID 19 Related Myocardial InjuryDocument12 pagesImaging in COVID 19 Related Myocardial Injuryorkut verificationNo ratings yet
- Actualizar Definición SIRA en COVIDDocument3 pagesActualizar Definición SIRA en COVIDjoelNo ratings yet
- Ferrando2020 Article ClinicalFeaturesVentilatoryManDocument12 pagesFerrando2020 Article ClinicalFeaturesVentilatoryManMedicina InternaNo ratings yet
- Mesenchymal Stem Cell Immunomodulation and Regeneration TherapeuticsDocument13 pagesMesenchymal Stem Cell Immunomodulation and Regeneration TherapeuticswiwiNo ratings yet
- Covid Adulto Mayor Acer 2020Document10 pagesCovid Adulto Mayor Acer 2020Carlos BucaraNo ratings yet
- MAY 2020 SINTOMAS Gastrointestinal Symptoms Associated WithDocument14 pagesMAY 2020 SINTOMAS Gastrointestinal Symptoms Associated WithMayaraNo ratings yet
- Gopalaswamy y Subbian - 2021 - Corticosteroids For COVID-19 Therapy Potential ImDocument18 pagesGopalaswamy y Subbian - 2021 - Corticosteroids For COVID-19 Therapy Potential ImOsmar SulcaNo ratings yet
- COVID-19: Effects in Comorbidities and Special PopulationsFrom EverandCOVID-19: Effects in Comorbidities and Special PopulationsNo ratings yet
- Basics of Mechanical Ventilation (SIPHW)Document68 pagesBasics of Mechanical Ventilation (SIPHW)Sudip beraNo ratings yet
- Acute Respiratory Distress Syndrome: Jurnal RespirasiDocument11 pagesAcute Respiratory Distress Syndrome: Jurnal RespirasiArmia UsnihidayatiNo ratings yet
- Cureus 0014 00000032158Document8 pagesCureus 0014 00000032158Daniel Martinez HernándezNo ratings yet
- IV-B Total Parenteral Nutrition (TPN) and Central Venous Pressure Line (CVP) / Mechanical VentilatorDocument23 pagesIV-B Total Parenteral Nutrition (TPN) and Central Venous Pressure Line (CVP) / Mechanical VentilatorRio DanteNo ratings yet
- Airway Pressure Release VentilationDocument31 pagesAirway Pressure Release VentilationsakuraleeshaoranNo ratings yet
- I-Choose The Correct Answer of The Following Sentences:: Palestine College of NursingDocument9 pagesI-Choose The Correct Answer of The Following Sentences:: Palestine College of NursingHasan A AsFourNo ratings yet
- Fraktur FemurDocument11 pagesFraktur FemurYusuf BrilliantNo ratings yet
- WINFOCUS - ICM 2012 - Lung US GuidelinesDocument15 pagesWINFOCUS - ICM 2012 - Lung US GuidelinesDiego Andres VasquezNo ratings yet
- ARDS Berlin Definition JAMA 2012Document8 pagesARDS Berlin Definition JAMA 2012Irfan HardiNo ratings yet
- Acute Respiratory Distress SyndromeDocument7 pagesAcute Respiratory Distress SyndromeDashhh RamirezNo ratings yet
- 10 1001@jama 2020 12866Document11 pages10 1001@jama 2020 12866Jordi Piñeros AriasNo ratings yet
- Vti Carotideo RevisarDocument9 pagesVti Carotideo RevisarCurro MirallesNo ratings yet
- Zone 3 REBOA EvaluationDocument7 pagesZone 3 REBOA EvaluationJean CotteNo ratings yet
- Physiotherapy Management For COVID-19 in The Acute Hospital Setting and Beyond: An Update To Clinical Practice RecommendationsDocument18 pagesPhysiotherapy Management For COVID-19 in The Acute Hospital Setting and Beyond: An Update To Clinical Practice RecommendationsJimena Vásquez RodríguezNo ratings yet
- Paper 9, Aboelnazar 2018Document11 pagesPaper 9, Aboelnazar 2018NITIN SENTHILKUMARNo ratings yet
- Progressive Mobility in The Critically Ill PDFDocument15 pagesProgressive Mobility in The Critically Ill PDFydtrgnNo ratings yet
- EXPRESS Trial 2008Document10 pagesEXPRESS Trial 2008Dr. Sergio Oscar AlunniNo ratings yet
- CHPT 70 Respiratory Part 2Document56 pagesCHPT 70 Respiratory Part 2helen brockNo ratings yet