Professional Documents
Culture Documents
Archfaci 1 1 27
Uploaded by
Sam CastilloOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Archfaci 1 1 27
Uploaded by
Sam CastilloCopyright:
Available Formats
ORIGINAL ARTICLE
Comparison of Topical Anti-ischemic Agents
in the Salvage of Failing Random-Pattern
Skin Flaps in Rats
Richard E. Davis, MD; Jeffrey H. Wachholz, MD; David Jassir, MD; Chad A. Perlyn, BS; Mark H. Agrama, MD
Objective: To determine the efficacy of topical anti- Results: Topical anti-ischemic drug therapy resulted in
ischemic drug therapy in the salvage of failing, random- a statistically significant reduction in ischemic flap ne-
pattern skin flaps. crosis for each drug (or combination) tested relative to
the 44.2% mean necrosis observed in control animals.
Design: Prospective, randomized, placebo-controlled, Treatment with the combination of topical nitroglyc-
therapeutic trial. erin and topical trolamine salicylate resulted in the best
salvage response (25.2% mean necrosis) with a statisti-
Setting: Academic medical center. cally significant improvement in flap survival relative to
both controls and nitroglycerin alone.
Subjects: Sixty-one adult male Sprague-Dawley rats.
Conclusions: Topical anti-ischemic agents are effec-
Intervention: Each experimental rat underwent a cau- tive in reducing ischemic necrosis of failing, random-
dally based random-pattern skin flap using the modified pattern skin flaps in the rat model. Although nitroglyc-
McFarlane technique. Rats were randomized to 1 of 6 treat- erin, trolamine salicylate, and nifedipine possess unique
ment groups: topical nifedipine, topical trolamine salicy- pharmacologic mechanisms of action, each drug pro-
late, topical nitroglycerin, topical trolamine salicylate- duced a statistically significant improvement in flap sur-
nitroglycerin combination, topical nifedipine-trolamine vival. The results of this study suggest that topical drug
salicylate-nitroglycerin combination, or inert carrier oint- therapy may play an important role in clinical salvage of
ment (control). Treatment was initiated immediately fol- the failing skin flap. Further studies are needed to ex-
lowing flap closure and continued every 6 hours for 7 days. plore the potential of combination drug therapy.
At the end of the treatment period, animals were eutha-
nized and flap survival was determined for each one. Arch Facial Plast Surg. 1999;1:27-32
B
ECAUSE OF thegrowingpreva- ment of flap ischemia has become an area
lence of skin malignancy, re- of increasing interest.2,3 To date, numerous
constructive surgeons are pharmacologicalagentshavebeenexamined
confronted by an increasing for their ability to prevent or reverse skin flap
number of complex skin de- ischemia. These drugs include sympatho-
fects. Most of these defects arise on the face lytics, vasodilators, calcium channel block-
where cosmetic concerns are of prime im- ers, hemorheologics, prostaglandin in-
portance.Becauserandom-patternskinflaps hibitors, anticoagulants, glucocorticoids,
typically enjoy excellent color, texture, and and free radical scavengers.1-6 Unfortu-
thickness match, they remain a valuable as- nately, few of these drugs have proven
set in facial reconstruction. Unfortunately, unequivocally effective. Of those agents
the susceptibility of these flaps to ischemic with proven experimental efficacy, most
necrosis is difficult to predict owing to varia- have been limited by undesirable adverse
tions in flap design and intrinsic tissue vas- effects, high cost, or restricted availabil-
cularity.1 As a consequence, unforeseen skin ity. Moreover, to use many of these drugs,
flap necrosis remains a rare but serious com- extensive preoperative treatment or direct
From the Division of Facial
plication of facial reconstruction. A safe, vascular infusion is required, making their
Plastic and Reconstructive convenient, and cost-effective treatment for use in postoperative ischemic flap sal-
Surgery, Department of failing skin flaps is currently needed. vage either impractical or impossible. As
Otolaryngology, University of As the pathophysiologic characteristics a consequence, the ideal agent for salvage
Miami School of Medicine, of random-patternskinflap necrosis become of the failing, random-pattern skin flap does
Miami, Fla. more clearly defined, pharmacologic treat- not currently exist.
ARCH FACIAL PLAST SURG/ VOL 1, JAN-MAR 1999
27
©1999 American Medical Association. All rights reserved.
a major role in the reduction of nutrient capillary blood
flow.2,7-9 Various pharmacologic agents that diminish sym-
MATERIALS AND METHODS pathetic tone or promote arteriolar smooth muscle re-
laxation have been shown to improve skin flap perfu-
Sixty-one adult male Sprague-Dawley rats (weigh- sion and survival, lending support to this proposed
ing 250-275 mg) were used as experimental sub- pathophysiologic mechanism.10 One such group of va-
jects in full accordance with the protocols estab- soactive drugs is the calcium channel blockers. Nifed-
lished by the Institutional Animal Care and Use ipine is a clinically available calcium channel blocker be-
Committee (IACUC) at the University of Miami, in lieved to block adrenergically mediated vasoconstriction
Florida. Isoflurane inhalational anesthesia was se- by inhibiting calcium ion flux into vascular smooth muscle
lected to approximate routine surgical conditions. An- cells.10 Other potential benefits of calcium channel block-
esthetic induction was achieved with 5% isoflurane ers, such as inhibition of platelet activation and cell mem-
and subjects were maintained intraoperatively on a brane stabilization, may also contribute to improved skin
1.5% isoflurane regimen administered through a snout
flap survival.10-12
cone by spontaneous ventilation.
Following induction, animals were shaved, pre- To date, 3 animal studies using oral nifedipine have
pared, and uniformly immobilized in the prone posi- demonstrated improvement in random-pattern skin flap
tion. Restrictive collars were then placed to prevent survival with postoperative drug administration.10,13,14 Pal
unwanted ingestion of ointment during self-groom- and coworkers13 noted a reduction in random-pattern skin
ing. After adequate depth of anesthesia was con- flap necrosis from 37% to 12% in rats given 0.3 to 0.5
firmed using the pinch flexion/withdrawal test, cau- mg/kg per day of postoperative oral nifedipine. Only a
dally based, random-pattern skin flaps, each measuring slight additional benefit was observed when treatment
3 x 10 cm, were raised along the dorsal midline by sharp was initiated preoperatively. Similarly, Bailet and co-
dissection. Flaps were designed according to the Khouri workers10 showed a 25% reduction in ischemic flap ne-
modification of the original McFarlane tech-
nique,33,34 and care was taken to elevate the pannicu-
crosis in the rodent model when nifedipine administra-
lus carnosus with the overlying skin flap. After hemo- tion was begun intraoperatively by intraperitoneal
stasis was secured with electrocautery, the flaps were injection (0.75 mg/kg) and continued orally for 7 days
sutured in the native position using 4-0 interrupted postoperatively with rat chow containing 3000-ppm nifed-
silk sutures (Ethicon Inc, Somerville, NJ). To pre- ipine.10 Pretreatment with oral nifedipine reduced ne-
vent postoperative flap cannibalization, all animals were crosis further to 50% of controls. Hypotension was not
returned to solitary housing following emergence from reported in either experiment. Finally, Hira et al14 ob-
anesthesia. Subjects were allowed water and rat chow served improved flap survival from 56% in the control
ad libitum throughout the study period, and acetami- group to 77% in animals treated with 1 mg/kg per day of
nophen with codeine was added to the drinking wa- postoperative oral nifedipine. Interestingly, in the same
ter for 5 days postoperatively.
Immediately following flap closure, each flap
study, animals given much higher doses of oral nifed-
pedicle was uniformly coated with topical carrier oint- ipine (10 mg/kg per day) also demonstrated an im-
ment containing active drugs according to 1 of 6 ran- proved mean flap survival of 72%. The failure of this much
domized treatment groups. The control group re- higher dose to produce systemic hypotension and flap
ceived only inert (placebo) carrier ointment, while hypoperfusion is difficult to explain. Bailet and cowork-
the remaining groups received either nifedipine ers10 have theorized that other pharmacological proper-
(5 mg), trolamine salicylate (30 mg), nitroglycerin ties of nifedipine, such as platelet deactivation and cell
(30 mg), trolamine salicylate-nitroglycerin combi- membrane stabilization, may have been responsible for
nation (30 mg each), or trolamine salicylate-nitro- the beneficial effects of nifedipine at higher doses.
glycerin-nifedipine combination (30 mg, 30 mg, 5 mg, In contrast to these reports, 2 additional studies have
respectively). Care was taken to distribute ointment
evenly along the entire flap and dosing was repeated
shown no beneficial effects of nifedipine on flap sur-
every 6 hours for 7 days postoperatively. vival. Miller et al15 reported no improvement in random-
At the conclusion of the study period, all of the pattern skin flap survival using pigs treated postopera-
animals were euthanized by rapid carbon dioxide as- tively with 1.5 mg/kg of oral nifedipine. However, the
phyxia in accordance with approved IACUC proto- authors reported significant hypotension following nifed-
cols. Comparisons of flap survival were then deter- ipine administration and concluded that drug-related hy-
mined for each cohort by calculating ratios of ischemic potension may have negated any beneficial effects on flap
to healthy flap tissue using the acetate weight tech- survival. Similarly, Emery et al16 observed no improve-
nique previously described.35 Data were statistically ment in flap survival in rats treated with 2.5 mg/kg of oral
evaluated using 1-way analysis of variance (ANOVA) nifedipine. In their study, blood pressure monitoring was
to detect differences between treatment groups. Pair-
wise comparisons were performed at the 95% confi-
conducted in only a single test animal, and although hy-
dence level using the least significant difference potension was not observed at the 2.5-mg/kg dose, this dose
criterion. has been previously shown to produce hypotension in nor-
motensive rats.17 Thus, unrecognized hypotension may
have also been a factor in this experiment. Moreover, Fu-
mas18 has suggested that vasoconstricting agents con-
Although the mechanisms for random-pattern skin tained within the drug vehicle (caffeine, theobromine, and
flap ischemia have yet to be fully elucidated, surgically theophylline) may have further negated any beneficial ef-
induced adrenergic vasoconstriction is believed to play fects of nifedipine on flap survival.
ARCH FACIAL PLAST SURG/ VOL 1, JAN-MAR 1999
28
©1999 American Medical Association. All rights reserved.
From these data, it seems likely that nifedipine im- temic drug distribution. Hypotension or other adverse ef-
proves ischemic random-pattern skin flap survival if thera- fects produced by systemic drug distribution are thus
peutic tissue levels can be achieved without significant reduced or avoided. Previous studies of salicylate levels fol-
reductions in systemic blood pressure. Moreover, since lowing topical application of trolamine salicylate have con-
nifedipine is safe, widely available, and inexpensive, it firmed intra-articular drug levels comparable to those
is potentially well suited to clinical use in ischemic flap achieved with oral aspirin administration, while serum lev-
salvage. els remained hundreds of times lower.31 Studies using the
Another commonly recognized vasoactive drug that re- adrenergic blocking agents phentolamine and phenoxy-
laxes smooth muscle tone in peripheral arteries and veins benzamine applied in a high-dose topical paste to random-
is nitroglycerin.19 Nitroglycerin acts predominantly through pattern skin flaps in rats have shown increased postopera-
venous dilation and is commonly prescribed in the treatment tive flap survival relative to treatment with intramuscular
of angina pectoris due to coronary artery disease.19 The va- injection.32 Despite the topical application of doses con-
sodilatory effect of nitroglycerin is believed to stem from the siderably higher than that recommended for parenteral
releaseofprostacyclin,apotentendogenousvasodilatorfound use, animal mortality was not observed, suggesting that
in vascular endothelium.20 In addition, nitroglycerin also ap- the normally potent adverse effects of phentolamine or
pears to preferentially dilate spastic vessels within ischemic phenoxybenzamine were significantly reduced by topi-
tissue.21 Recent animal studies have shown a reduction in cal application. Animal experiments with topical nitro-
random-pattern skin flap necrosis following treatment with glycerin ointment have also demonstrated augmented
nitroglycerin, suggesting a beneficial effect on nutrient blood random-pattern skin flap survival.22,23 Rohrich and co-
flow.22-24 Like nifedipine, nitroglycerin is widely available, workers22 observed statistically significant improve-
inexpensive, and generally well tolerated, making it poten- ments in flap survival using 2% nitroglycerin ointment
tially suitable for clinical use in flap salvage. applied to skin flaps raised in both the rat and pig. Again,
no lethal adverse effects were reported despite compar-
atively large topical doses. Similarly, Blomain et al23 stud-
I
N ADDITION to adrenergic vasoconstriction, an- ied random-pattern skin flap necrosis in pigs treated post-
other proposed mechanism for ischemic skin flap operatively for 4 days with 2% nitroglycerin ointment.
necrosis is microvascular compromise result- Survival improved to 125% of controls in dorsally based
ing from platelet aggregation.2,3 Surgically in- flaps and 176% of controls in ventrally based flaps, and
duced platelet aggregation is believed to stem no lethal adverse effects of drug therapy were reported.
from release of thromboxane A2 (TXA2), a platelet- Based on these studies, it appears that direct tissue tar-
derived prostaglandin that behaves as a potent vasocon- geting through topical drug application may improve is-
strictor and promoter of platelet aggregation.2,25 Under chemic flap survival while simultaneously minimizing
normal circumstances, TXA2 is held in check by its more dose-limiting adverse effects. Topical drug delivery also
abundant antagonist, prostacyclin (PGI2), which is se- appears to be particularly well suited to skin flap ische-
lectively synthesized and released by vascular endothe- mia where flap hypoperfusion often prevents effective in-
lium. However, following surgical trauma there seems travascular drug distribution, particularly in the pres-
to be an accelerated synthesis of TXA2 and a correspond- ence of co-existing hypotension.
ing reduction in PGI2 synthesis, both of which lead to In addition to improving the therapeutic ratio,
increased platelet aggregation.2,26 topical drug administration is also convenient, cost-
Trolamine salicylate (Aspercreme) is a topical anti- effective, and noninvasive. Because of its simplicity,
inflammatory analgesic hydrolyzed to salicylic acid, a topical administration is well suited to outpatient use,
potent inhibitor of prostaglandin synthesis. 27,28 Like and drug administration may continue without inter-
other aspirin-containing compounds, trolamine salicy- ruption despite impaired or restricted oral intake. Fi-
late is an irreversible inhibitor of platelet aggregation. nally, because nitroglycerin and trolamine salicylate are
Because experimental results using either nonspecific commercially available as topical ointments, and be-
TXA2 inhibitors or selective TXA2 antagonists have cause nifedipine is largely lipophilic, all 3 drugs are
shown improvements in random-pattern skin flap sur- likely to achieve therapeutic tissue levels via topical ap-
vival,1,2,26,29,30 trolamine salicylate may also prove effica- plication.
cious in the salvage of failing random-pattern skin flaps. The purpose of this study is to establish the effi-
Like both nifedipine and nitroglycerin, trolamine salicy- cacy of anti-ischemic agents when administered through
late is readily available, inexpensive, and generally well the transdermal route. The 3 drugs selected for this study,
tolerated. nitroglycerin, trolamine salicylate, and nifedipine, have
In an effort to enhance the target tissue response, re- widely differing mechanisms of action, and each drug has
duce systemic adverse effects (such as hypotension), and either a theoretical or proven potential for the salvage of
avoid cumbersome intravascular drug delivery systems, we ischemic random-pattern skin flaps. We have chosen to
chose to evaluate the efficacy of anti-ischemic agents ad- evaluate the efficacy of topical anti-ischemic therapy in
ministered through topical application. Topical drug therapy the setting of postoperative flap salvage using an animal
enjoys several potential advantages over oral or intravas- model. The model selected in this study has been previ-
cular methods of drug delivery. Foremost among these ad- ously standardized to produce consistent levels of ische-
vantages is the direct targeting of ischemic tissue. Direct mic flap necrosis in untreated (control) animals and serves
application of anti-ischemic drugs to the target tissue op- as a statistically valid method for assessing the preven-
timizes local drug concentrations while minimizing sys- tion of surgically induced ischemic flap changes.33
ARCH FACIAL PLAST SURG/ VOL 1, JAN-MAR 1999
29
©1999 American Medical Association. All rights reserved.
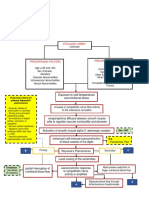
NTG NTG+TS+Nifed Nifed TS NTG+TS Control
31.63 26.22 26.21 26.16 25.16 44.15
Schematic representation of mean percentage of random-pattern skin flap necrosis (percentage) for each experimental group. NTG indicates nitroglycerin; TS,
trolamine salicylate; and Nifed, nifedipine. For each group, P = .05.
RESULTS failure remains comparatively low, the morbidity asso-
ciated with flap necrosis has fueled the search for an ef-
Sixty-one animals were enrolled in the study and 59 fective drug therapy. To date, there is no ideal drug therapy
animals were available for data collection at the conclu- for random-pattern skin flap necrosis.
sion of the study period. Two animals died intraopera- Although some drugs have demonstrated experi-
tively from anesthetic overdose. Postmortem examina- mental reductions in ischemic flap necrosis, these ben-
tion of all animals revealed no evidence of hematoma or efits have usually been offset by systemic adverse ef-
seroma formation. fects, high cost, or poor availability. In addition,
The mean percentage of flap necrosis was com- administration of many of these agents requires lengthy
pared for each treatment group. Control animals treated pretreatment dosing schemes or invasive drug delivery
with inert petrolatum ointment exhibited the highest per- systems for therapeutic success, limiting their effective-
centage of flap necrosis (mean = 44.1% ± 1.6% SE). By ness in the treatment of unexpected flap ischemia or acute
comparison, all animals treated with topical anti- skin trauma.
ischemic agents exhibited a statistically significant re- Moreover, since most random-pattern skin flap pro-
duction in ischemic flap necrosis at the 95% confidence cedures are not associated with flap ischemia, it is diffi-
level (Figure). Treatment with topical nitroglycerin pro- cult to justify the routine use of anti-ischemic prophy-
duced the weakest salvage response with 31.6% ± 3.1% laxis for low-risk patients, particularly if drug therapy is
flap necrosis. However, relative to control animals, this associated with increased cost or significant adverse ef-
reduction in flap necrosis was statistically significant fects. Consequently, a safe, inexpensive salvage drug is
(P,.05). Similarly, in comparison to control subjects, both currently needed.
topical nifedipine and topical trolamine salicylate dem- To be most effective, the ideal salvage drug would
onstrated an improved salvage response with 26.2% ± need to prevent tissue necrosis even when drug admin-
1.5% and 26.2% ± 2.5% flap necrosis, respectively istration was withheld pending the development of early
(P,.05). However, the trend toward reduction in flap ne- ischemic signs or symptoms. Ideally, such a drug would
crosis relative to nitroglycerin was not statistically sig- also be well tolerated, cost-effective, readily available, and
nificant. Combining all 3 agents failed to improve the suitable for outpatient administration. Because such a sal-
salvage response relative to any single agent alone, al- vage agent would obviate the need for global prophy-
though the salvage response of 26.2% ± 1.5% flap necro- laxis or expensive flap delay procedures, it would also
sis was statistically significant relative to the control group be well suited for use in acute skin trauma. Currently,
(P,.05). Overall, the best salvage response was pro- the ideal salvage drug does not exist.
duced from the combination of topical nitroglycerin and To date, drug therapy for the salvage of failing skin
topical trolamine salicylate with 25.2% ± 1.9% flap ne- flaps has focused largely on systemic and sometimes in-
crosis. This reduction in flap necrosis was statistically sig- vasive routes of drug delivery. Although these ap-
nificant relative to both the control group (P,.05) and proaches have occasionally met with experimental suc-
the nitroglycerin treatment group (P,.05). In contrast, cess, dose-limiting adverse effects from systemic drug
this combination failed to produce a statistically signifi- distribution have often been an obstacle to satisfactory
cant improvement over either the nifedipine or the tro- flap salvage. Ironically, the adverse effect most fre-
lamine salicylate treatment groups. quently encountered, systemic hypotension, likely serves
to increase ischemic tissue loss by further reducing per-
COMMENT fusion pressure in the already compromised skin flap.
Consequently, many potentially efficacious drugs, in-
Because ischemic necrosis is difficult to predict, unfore- cluding sympatholytics, vasodilators, and calcium chan-
seen flap loss remains a serious complication of random- nel blockers, have likely been rendered ineffective in flap
pattern skin flap surgery. Although the incidence of flap salvage as a consequence of systemic drug distribution.
ARCH FACIAL PLAST SURG/ VOL 1, JAN-MAR 1999
30
©1999 American Medical Association. All rights reserved.
In an effort to circumvent the problem of systemic Because nifedipine, trolamine salicylate, and nitro-
drug distribution, we chose to evaluate the efficacy of glycerin presumably work by distinct pharmacological
flap salvage using topical drug administration. Topical mechanisms of action (ie, inhibition of calcium ion flux
anti-ischemic therapy offers numerous advantages over into vascular smooth muscle, inhibition of TXA2 synthe-
conventional oral or parenteral therapy, the foremost of sis, and stimulation of endothelial PGI2 release, respec-
which is the ability to achieve therapeutic target tissue tively), the results of this study support the notion that
levels without significant systemic drug distribution. In the origin of random-pattern skin flap necrosis is com-
spite of drug levels far in excess of recommended par- plex and multifactorial. Hence, combining drugs with dif-
enteral or oral doses, results of initial investigations us- fering mechanisms of action should theoretically result
ing topical salvage agents have shown reductions in tis- in an additive or even synergistic salvage response. The
sue necrosis without dose-limiting systemic adverse failure of combination drug therapy to produce such a
effects.22,23,32 In contrast to oral or parenteral adminis- response in this study is difficult to explain. Perhaps the
tration, topical drug therapy may also continue uninter- absence of additive or synergistic drug interactions re-
rupted despite postoperative nausea, oral intake restric- flects a single common mechanism of action for the 3
tions, or patient discharge, making them ideal for drugs tested. Another possible explanation is that the com-
postoperative ambulatory use. bination of 2 potent vasodilators may have negated any
In this study we chose to evaluate 3 different topi- beneficial effects of topical drug therapy through suble-
cal drugs, each with the potential to prevent or reverse thal reductions in systemic blood pressure. Although the
ischemic injury in the failing, random-pattern skin flap. combination of trolamine salicylate and nitroglycerin did
The results of this study suggest that all 3 drugs are ef- produce a statistically significant reduction in flap ne-
fective in reducing impending ischemic tissue loss when crosis relative to nitroglycerin alone, the response was
applied topically to the target tissue. Using a carefully stan- not statistically significant relative to trolamine salicy-
dardized animal model, topical nifedipine and topical tro- late alone, suggesting that the observed improvement may
lamine salicylate therapy improved survival from 56% in have been from the isolated effect of trolamine salicy-
control animals to 74% in treated animals. This reduc- late. Because these 3 drugs are believed to work through
tion in ischemic necrosis was observed without the separate and complementary mechanisms, further study
need for pretreatment or systemic drug delivery. More- using variations in drug dosages and drug combinations
over, the magnitude of tissue salvage observed follow- will be necessary to assess the potential for improved flap
ing topical nifedipine administration compares favor- salvage through combined (synergistic) drug therapy.
ably with studies using oral drug administration. To our
knowledge, this is also the first published report of sta- CONCLUSIONS
tistically significant flap salvage using a topically ap-
plied platelet inhibitor (trolamine salicylate). Although The results of this animal investigation indicate that topi-
topical nitroglycerin demonstrated the weakest salvage caldrugsalvageof ischemicrandom-patternskinflapsissafe,
response (68% flap survival), these results are similar in efficacious, and potentially well suited to clinical applica-
magnitude to those previously reported by Rohrich and tion. Further studies of this potential treatment modality are
coworkers22 or Blomain et al23 and serve to confirm the needed to better define optimal drug doses, application in-
efficacy of topical nitroglycerin in ischemic flap salvage. tervals, and drug combinations. Ultimately, topical anti-
As with previous experimental studies of topical anti- ischemic drug therapy may provide a needed pharmacologic
ischemic agents, we also observed no visible evidence of rescue in the clinical management of failing skin flaps.
adverse effects, suggesting that systemic effects of topi-
cal drug therapy were negligible. Unlike many drugs Accepted for publication September 22, 1998.
previously evaluated in flap salvage, the drugs used in We wish to express our gratitude to Robert Duncan,
this study are widely available, inexpensive, and well PhD, professor of epidemiology and biostatistics, for his as-
tolerated. Based on the results of this preliminary ani- sistance with statistical data analysis.
mal study, topical drug therapy may eventually provide Corresponding author: Richard E. Davis, MD, Uni-
an effective clinical means for the salvage of failing ran- versity of Miami Hospitals and Clinics, Suite 4027 (D-1),
dom-pattern skin flaps. 1475 NW 12th Ave, Miami, FL 33136.
It is worth emphasizing that this study did not con-
firm a true salvage drug response because drug therapy
was initiated prior to clinical signs of tissue ischemia. REFERENCES
Rather, these data suggest only that trolamine salicy-
late, nifedipine, and nitroglycerin are effective for in- 1. Sloan GM, Reinsch JF. Flap physiology and the prediction of flap viability. Hand
creasing tissue tolerance to surgical ischemia. Whether Clin. 1985;1:609-619.
2. Pang CY, Forrest CR, Morris SF. Pharmacological augmentation of skin flap vi-
topical drug therapy would augment flap survival if treat- ability: a hypothesis to mimic the surgical delay phenomenon or a wishful thought.
ment were withheld pending the onset of visible signs Ann Plast Surg. 1989;22:293-306.
of flap ischemia was not assessed in this study. How- 3. Nichter LS, Sobieski MW, Edgerton MT. Augmentation of critical skin flap sur-
ever, because both nitroglycerin and nifedipine presum- vival following ibuprofen therapy. Ann Plast Surg. 1986;16:305-312.
ably improve impaired nutrient blood flow through va- 4. Kerrigan CL, Daniel RK. Pharmacologic treatment of the failing skin flap. Plast
Reconstr Surg. 1982;70:541-548.
sodilation, these drugs may also have efficacy as legitimate 5. Pratt MF. Evaluation of random skin flap survival in a porcine model. Laryngo-
salvage drugs. Further studies will be necessary to de- scope. 1996;106:700-712.
fine their precise efficacy as salvage agents. 6. Davis RE, Cohen JI, Robinson JE, Urben SL, Cook TA. Ketorolac (Toradol) and
ARCH FACIAL PLAST SURG/ VOL 1, JAN-MAR 1999
31
©1999 American Medical Association. All rights reserved.
acute random-pattern skin flap survival in rat. Arch Otolaryngol Head Neck Surg. 22. Rohrich RJ, Cherry GW, Phil D, Spira M. Enhancement of skin flap survival uti-
1995;121:673-677. lizing nitroglycerin ointment. Plast Reconstr Surg. 1984;73:943-948.
7. Kerrigan CL. Skin flap failure: pathophysiology. Plast Reconstr Surg. 1983;72: 23. Blomain EW, Manders EK, Saggers G, et al. Topical nitroglycerin ointment en-
766-774. hances the survival of skin flaps. Surg Forum. 1982;33:594-595.
8. Cutting CB, Robson MC, Koss N. Dennervation supersensitivity and the delay 24. Gatti JE, Brousseau DA, Silverman DG, LaRossa D. Intravenous nitroglycerin as
phenomenon. Plast Reconstr Surg. 1978;61:881-887. a means of improving ischemic tissue hemodynamics and survival. Ann Plast
9. Moore GK, Trachy RE, Cummings CW. The effect of alpha-adrenergic stimula- Surg. 1986;16:521-526.
tion and blockage of perfusion of myocutaneous flaps. Otolaryngol Head Neck 25. Moncada S, Vane JR. Arachidonic acid metabolites and the interactions be-
Surg. 1986;94:489-496. tween platelets and blood vessel walls. N Engl J Med. 1979;300:1142-1147.
10. Bailet JW, Hoffman LF, Trachy RE, Weymuller EA. The effect of nifedipine on skin 26. Sasaki GH, Pang CY. Experimental evidence for involvement of prostaglandins
flap survival in rats. Laryngoscope. 1994;104:253-258. in viability of acute skin flaps: effects on viability and mode of action. Plast Re-
11. Stein HJ, Fayman MS, Oosthuizen MMJ, Hinder RA. Verapamil improves sur- constr Surg. 1981;67:335-340.
vival of rat hyperemic island flaps. Surgery. 1989;106:617-623. 27. Myoflex Creme [product information pamphlet]. Fort Washington, Pa: Rorer Phar-
12. Malamet R, Wise RA, Ettinger WH, Wigely FM. Nifedipine in the treatment of maceuticals; 1990.
Raynaud’s phenomenon: evidence for inhibition of platelet activation. Am J Med. 28. Gilman AG, Rall TW, Nies AS, et al, eds. Goodman and Gilman’s The Pharma-
1985;78:602-608. cologic Basis of Therapeutics, 8th ed. Elmsford, NY: Pergamon Press Inc; 1990.
13. Pal S, Khazanchi RK, Moudgil K. An experimental study on the effect of nife- 29. Banic A, Kouris K, Rajacic N, Nazzal M, Al-Ghussain NM, Thulesius O. Effect of
dipine on ischaemic skin flap survival in rats. Br J Plast Surg. 1991;44:299-301. ridogrel, a thromboxane receptor blocker and synthesis inhibitor on plasma and
14. Hira M, Tajima S, Sano S. Increased survival length of experimental flap by cal- red blood cell flow in an arterial skin flap in sheep. Scand J Plast Reconstr Hand
cium antagonist nifedipine. Ann Plast Surg. 1990;24:45-48. Surg. 1991;25:9-14.
15. Miller AP, Falcone RE, Nappi J, Redmon HA. The lack of effect of nifedipine on 30. Zachary LS, Heggers JP, Robson MC, Murphy RC. Combined prostacyclin and
failing skin flaps. J Dermatol Surg Oncol. 1985;11:612-614. thromboxane synthetase inhibitor UK 38485 in flap survival. Ann Plast Surg. 1986;
16. Emery FM, Kodey TR, Bomberger RA, McGregor DB. The effect of nifedipine on 17:112-115.
skin flap survival. Plast Reconstr Surg. 1990;85:61-63. 31. Shamszad M, Perkal M, Golden EL, et al. Two double-blind comparisons of a
17. Ishii H, Itoh K, Nose T. Different antihypertensive effects of nifedipine in conscious topically applied salicylate cream and orally ingested aspirin in the relief of chronic
experimental hypertensive and normotensive rats. Eur J Pharmacol. 1980;64:21. musculoskeletal pain. Curr Ther Res. 1986;39:470-479.
18. Fumas H. The effect of nifedipine on skin flap survival. Plast Reconstr Surg. 1990; 32. Goshen J, Wexler MR, Peled IJ. The use of two alpha blocking agents, phenoxy-
86:1239. benzamine and phentolamine, in ointment and injection form to improve skin
19. Arky R, medical consultant. Physician’s Desk Reference. Montvale, NJ: Medical flap survival in rats. Ann Plast Surg. 985;15:431-435.
Economics Data Production Co; 1998:1226. 33. Khouri RK, Angel MF, Edstrom LE. Standardizing the dorsal rat flap. Plast Surg.
20. Miller RR, Fennel WH, Young JB, et al. Differential systemic arterial and venous 1986;37:590-591.
actions and consequent cardiac effects of vasodilator drugs. Prog Cardiovasc 34. McFarlane RM, DeYoung G, Henry RA. The design of a pedicle flap in the rat to
Dis. 1982;24:353. study necrosis and its prevention. Plast Reconstr Surg. 1965;35:177-182.
21. Goldstein RE, Stinson EB, Scherer JL, et al. Intraoperative coronary occlusive 35. Barton RM, Gilliand MD, Miller TA, Melissinos EG. The effect of 16,16-dimethyl
disease: nitroglycerin responsiveness and angiographic correlations. Circula- prostaglandin E2 on autogenous flap survival in rats. J Surg Res. 1981;30:
tion. 1974;49:298-308. 530-533.
Acknowledgment
Thanks to a generous grant from LifeCell Corporation, all fellows and
residents who are members of the American Academy of Facial Plastic and
Reconstructive Surgery will receive a 1-year subscription to the Archives of
Facial Plastic Surgery. LifeCell Corporation is dedicated to making valuable
educational resources available to physicians. We thank them for their
commitment and encouragement in our inaugural year.
Wayne F. Larrabee, Jr, MD
Editor
ARCH FACIAL PLAST SURG/ VOL 1, JAN-MAR 1999
32
©1999 American Medical Association. All rights reserved.
You might also like
- Hyaluronic Acid Embolism Treated With Subcutaneous High and Low Hyaluronidase Doses: Efficacy and Surrounding Tissue EffectDocument8 pagesHyaluronic Acid Embolism Treated With Subcutaneous High and Low Hyaluronidase Doses: Efficacy and Surrounding Tissue Effectkalinca marizyNo ratings yet
- 2020 - Treatment of Melasma A Review of Less Commonly Used AntioxidantsDocument8 pages2020 - Treatment of Melasma A Review of Less Commonly Used Antioxidantsnancyerlen100% (1)
- Pharmacology of Uterotonics & TocolyticsDocument60 pagesPharmacology of Uterotonics & TocolyticsSiddiq Blackhell Cakep100% (2)
- Term 3 Rationale Pharmacology and MCNDocument35 pagesTerm 3 Rationale Pharmacology and MCNKing KongNo ratings yet
- BrasilDocument4 pagesBrasilsofimm9804No ratings yet
- Tadalafil PDFDocument6 pagesTadalafil PDFWara Samsarga GedeNo ratings yet
- Effects of Sildenafil On The Viability of Random S PDFDocument6 pagesEffects of Sildenafil On The Viability of Random S PDFWara Samsarga GedeNo ratings yet
- Sarifakioglu2004 PDFDocument4 pagesSarifakioglu2004 PDFWara Samsarga GedeNo ratings yet
- OlsonDocument4 pagesOlsonIgor VainerNo ratings yet
- Lee 2014Document11 pagesLee 2014lisnallNo ratings yet
- Topical Histamine Stimulates Repigmentation of Nonsegmental Vitiligo by A Receptor-Dependent MechanismDocument7 pagesTopical Histamine Stimulates Repigmentation of Nonsegmental Vitiligo by A Receptor-Dependent MechanismManu PalaoNo ratings yet
- Crouch1997 PDFDocument7 pagesCrouch1997 PDFTrisya PutriNo ratings yet
- HyaluronidaseDocument2 pagesHyaluronidaseirwan junNo ratings yet
- Aac00042 0048Document5 pagesAac00042 0048Mohamed Abo El FadlNo ratings yet
- RETINOL (Improvement of Naturally Age Skin)Document7 pagesRETINOL (Improvement of Naturally Age Skin)produksi roiNo ratings yet
- Articol 2018Document13 pagesArticol 2018Ioana-Alexandra TrofinNo ratings yet
- Pi Is 0190962205002550Document15 pagesPi Is 0190962205002550Evy Afrianti DariseNo ratings yet
- Chemotherapy of Squamous Cell Carcinoma in SkinDocument5 pagesChemotherapy of Squamous Cell Carcinoma in SkinBagus MahendraNo ratings yet
- Artigo Cientifico 007Document10 pagesArtigo Cientifico 007BetoPereiraNo ratings yet
- Melasma Treatment: An Evidence Based Review: Jacqueline Mckesey Andrea Tovar Garza Amit G. PandyaDocument53 pagesMelasma Treatment: An Evidence Based Review: Jacqueline Mckesey Andrea Tovar Garza Amit G. PandyaStella SunurNo ratings yet
- Exilis - Elite - CB - Apoptosis Porcine 12-14 MCDANIELS - HQDocument5 pagesExilis - Elite - CB - Apoptosis Porcine 12-14 MCDANIELS - HQMarcia HernandezNo ratings yet
- Clinical Pearls in NephrologyDocument5 pagesClinical Pearls in NephrologyEdmilson R. LimaNo ratings yet
- (S) Controlled Delivery of Rivastigmine Using Transdermal Patch For EffectiveDocument7 pages(S) Controlled Delivery of Rivastigmine Using Transdermal Patch For EffectiveJoana SpiessNo ratings yet
- Ref Granuloma 4Document4 pagesRef Granuloma 4gabbynengNo ratings yet
- Paper 1Document8 pagesPaper 1Santhoshi Sadhanaa SankarNo ratings yet
- Hyaluronic Acid - Vascular ComplicationDocument9 pagesHyaluronic Acid - Vascular ComplicationAnkita GuravNo ratings yet
- Wound Care The Role of Advanced Wound-Healing TechnologiesDocument9 pagesWound Care The Role of Advanced Wound-Healing TechnologiesJose Antonio Chavez MNo ratings yet
- Histological Assessment of On-Ablative Laser Stimulation of Tissue Repair in Acellular Dermal GraftsDocument8 pagesHistological Assessment of On-Ablative Laser Stimulation of Tissue Repair in Acellular Dermal GraftsLívia ZerbinatiNo ratings yet
- Integrated Treatment During The Intravitreal Melphalan Era: Concurrent Intravitreal Melphalan and Systemic ChemoreductionDocument7 pagesIntegrated Treatment During The Intravitreal Melphalan Era: Concurrent Intravitreal Melphalan and Systemic ChemoreductionVlady BordaNo ratings yet
- Danh Gia NAG Ket Hop B3Document7 pagesDanh Gia NAG Ket Hop B3anh.tranNo ratings yet
- SADICK VenusLegacy CoolsculptStudyDocument5 pagesSADICK VenusLegacy CoolsculptStudyDomenico NarcisoNo ratings yet
- Epilepsia - 2018 - Maglalang - Rescue Therapies For Seizure Emergencies New Modes of AdministrationDocument9 pagesEpilepsia - 2018 - Maglalang - Rescue Therapies For Seizure Emergencies New Modes of AdministrationKikie Rizky HeningNo ratings yet
- Ofl Oxacin-Induced Toxic Epidermal Necrolysis: Vikas Saini, Dinesh Sardana, Tanvir SamraDocument2 pagesOfl Oxacin-Induced Toxic Epidermal Necrolysis: Vikas Saini, Dinesh Sardana, Tanvir SamraDarwyn Paul DagumanNo ratings yet
- Crisaborole RCTDocument6 pagesCrisaborole RCTNotfor TaoNo ratings yet
- Journal ReadingDocument6 pagesJournal ReadingKulit SukapuraNo ratings yet
- Effects of Parentereal Hydration in Terminally Ill Cancer Patients A Preleminary StudyDocument6 pagesEffects of Parentereal Hydration in Terminally Ill Cancer Patients A Preleminary StudyCristian Meza ValladaresNo ratings yet
- TX, HQ, NdYagDocument12 pagesTX, HQ, NdYagade fitriyani lubisNo ratings yet
- Comparison of Hemorrhoid Sclerotherapy Using Glucose 50% vs. Phenol in Olive OilDocument4 pagesComparison of Hemorrhoid Sclerotherapy Using Glucose 50% vs. Phenol in Olive OilGabrielEnricoPangarianNo ratings yet
- J of Cosmetic Dermatology - 2023 - Konisky - Tranexamic Acid in Melasma A Focused Review On Drug Administration RoutesDocument10 pagesJ of Cosmetic Dermatology - 2023 - Konisky - Tranexamic Acid in Melasma A Focused Review On Drug Administration RoutesSamir TannuriNo ratings yet
- Melo Toxicity and Penetration Retina 2010Document7 pagesMelo Toxicity and Penetration Retina 2010Igor VainerNo ratings yet
- Microsurgery ArticleDocument6 pagesMicrosurgery Articlecusom34No ratings yet
- TherapeuticsDocument13 pagesTherapeuticsChecko LatteNo ratings yet
- Efficacy and Safety of Neem Seed Extract Compared With Clotrimazole in Tinea Corporis/ Cruris: A Randomized Controlled TrialDocument6 pagesEfficacy and Safety of Neem Seed Extract Compared With Clotrimazole in Tinea Corporis/ Cruris: A Randomized Controlled TrialnaveenNo ratings yet
- Jurnal 2Document11 pagesJurnal 2Putri AprilianiNo ratings yet
- Fixing The Skin Barrier: Past, Present and Future - Man and Dog ComparedDocument6 pagesFixing The Skin Barrier: Past, Present and Future - Man and Dog ComparedasesortecnicoNo ratings yet
- Ingenol Mebutate Gel For Actinic Keratosis: BackgroundDocument24 pagesIngenol Mebutate Gel For Actinic Keratosis: BackgroundMuhammad FarisNo ratings yet
- Li2008 PDFDocument9 pagesLi2008 PDFPatrick KimNo ratings yet
- 1 s2.0 S0305417918306983 MainDocument7 pages1 s2.0 S0305417918306983 MainFloriPuspaHumaniNo ratings yet
- J of Cosmetic Dermatology - 2019 - Zhang - A Cream of Herbal Mixture To Improve MelasmaDocument8 pagesJ of Cosmetic Dermatology - 2019 - Zhang - A Cream of Herbal Mixture To Improve Melasmaemily emiNo ratings yet
- Topical Propranolol Cream in Treatment of Superficial Infantile Hemangiomas: A Literature Review and 4 Years of Clinical ExperienceDocument4 pagesTopical Propranolol Cream in Treatment of Superficial Infantile Hemangiomas: A Literature Review and 4 Years of Clinical ExperienceJovana S. PelemišNo ratings yet
- A Randomized, Open-Label, Comparative Study of Oral Tranexamic Acid and Tranexamic Acid Microinjections in Patients With MelasmaDocument5 pagesA Randomized, Open-Label, Comparative Study of Oral Tranexamic Acid and Tranexamic Acid Microinjections in Patients With MelasmaPande Agung MahariskiNo ratings yet
- Role of Sialendoscopy in Juvenile Recurrent Parotitis (JRP)Document3 pagesRole of Sialendoscopy in Juvenile Recurrent Parotitis (JRP)mvrodriguez1No ratings yet
- J Clindermatol 2020 04 003Document7 pagesJ Clindermatol 2020 04 003R RahmadaniNo ratings yet
- Palliative Care PilocarpinaDocument7 pagesPalliative Care PilocarpinaIsteicy CortezNo ratings yet
- Jurnal UlkusDocument6 pagesJurnal UlkusIndri AnggraeniNo ratings yet
- Guo Qian2011Document6 pagesGuo Qian2011Sam CastilloNo ratings yet
- Delivery of ALA For PDT Using DendrimersDocument11 pagesDelivery of ALA For PDT Using Dendrimersenglish-exactlyNo ratings yet
- 4 TCM Scleroderma - PAEONIA, Keishi-Bukuryo-GanDocument6 pages4 TCM Scleroderma - PAEONIA, Keishi-Bukuryo-GanAndreas AdiwinataNo ratings yet
- Review JurnalDocument4 pagesReview Jurnalwalit1101 mukrininNo ratings yet
- Treatment of Chancroid With Enoxacin: ReferencesDocument3 pagesTreatment of Chancroid With Enoxacin: References7dsp7xvs8dNo ratings yet
- Anti-Aging Therapeutics Volume XIVFrom EverandAnti-Aging Therapeutics Volume XIVRating: 3 out of 5 stars3/5 (1)
- Wang 2020Document7 pagesWang 2020Sam CastilloNo ratings yet
- Gdalevitch 2015Document10 pagesGdalevitch 2015Sam CastilloNo ratings yet
- Ricci 2018Document6 pagesRicci 2018Sam CastilloNo ratings yet
- Guo Qian2011Document6 pagesGuo Qian2011Sam CastilloNo ratings yet
- Jurell 1981Document4 pagesJurell 1981Sam CastilloNo ratings yet
- Aps 2017 00934Document7 pagesAps 2017 00934Sam CastilloNo ratings yet
- Incompetent Cervix Case Analysis Subgroup 2Document44 pagesIncompetent Cervix Case Analysis Subgroup 2bunso padillaNo ratings yet
- Grade C: 296 Henley Beach RD, Underdale, 5032Document1 pageGrade C: 296 Henley Beach RD, Underdale, 5032Heba ZaherNo ratings yet
- Price List September 14 2020 Generic PrincipalDocument11 pagesPrice List September 14 2020 Generic PrincipalSotero AlgerNo ratings yet
- DrugsDocument3 pagesDrugsxsuilujxNo ratings yet
- Garlic Creatine Bittermelon FinalpptDocument43 pagesGarlic Creatine Bittermelon Finalpptapi-202881815No ratings yet
- Tocolytic AgentDocument13 pagesTocolytic AgentHania Asmarani RahmanitaNo ratings yet
- Management of Hypertensive Crisis: British and Irish Hypertension Society Position DocumentDocument17 pagesManagement of Hypertensive Crisis: British and Irish Hypertension Society Position DocumentPaula SantosNo ratings yet
- Reviewer For CV and Respiratory DrugsDocument9 pagesReviewer For CV and Respiratory Drugsprinz1mendezNo ratings yet
- HPCSA Clinical Practice Guidelines 2016 - Request For CommentDocument218 pagesHPCSA Clinical Practice Guidelines 2016 - Request For CommentDarryl Betts50% (2)
- Tutorial Report 1 Pharmacology and Therapy: Lecturer: Nurmawati Fatimah DR., M.SiDocument34 pagesTutorial Report 1 Pharmacology and Therapy: Lecturer: Nurmawati Fatimah DR., M.SiGitaaNo ratings yet
- 04.03-02 Endocrine IV - Uterine Pharmacology PDFDocument4 pages04.03-02 Endocrine IV - Uterine Pharmacology PDFMaikka IlaganNo ratings yet
- Case Study of Pregnancy Induced HypertensionDocument12 pagesCase Study of Pregnancy Induced HypertensionJamaica Leslie Noveno100% (1)
- Cor Pulmonale EmedicineDocument16 pagesCor Pulmonale EmedicineHengki Permana PutraNo ratings yet
- Drugs in ObgDocument41 pagesDrugs in ObgkishorNo ratings yet
- Case Presentation On Ischemic Stroke: G.Hari Prakash Pharm.D InternDocument22 pagesCase Presentation On Ischemic Stroke: G.Hari Prakash Pharm.D InterngeethaNo ratings yet
- DiarryDocument10 pagesDiarryVan Ryan CondenoNo ratings yet
- Nifedipine Drug ProfileDocument8 pagesNifedipine Drug ProfileM NoumanNo ratings yet
- URAPIDILDocument41 pagesURAPIDILFrancesco LucianiNo ratings yet
- Hypnotics SedDocument13 pagesHypnotics SedSamantha ReyesNo ratings yet
- Cardiovascular Drugs and Medications Pharmacology QuizDocument7 pagesCardiovascular Drugs and Medications Pharmacology QuizIsabel Bibat DavidNo ratings yet
- Pathophysiology Raynauds Phenomenon Schematic DiagramDocument6 pagesPathophysiology Raynauds Phenomenon Schematic DiagramEerie Era0% (1)
- Combination of Lisinopril and Nifedipine GITS.10Document7 pagesCombination of Lisinopril and Nifedipine GITS.10Andi PermanaNo ratings yet
- Nifedipine-Drug Study 2BSN3Document3 pagesNifedipine-Drug Study 2BSN3Nichole DancelNo ratings yet
- Casos Clínicos InglésDocument15 pagesCasos Clínicos InglésClaudio R. MonteroNo ratings yet
- NifedipineDocument2 pagesNifedipineapi-3797941100% (3)
- CPM 1st Ed HypertensionDocument26 pagesCPM 1st Ed HypertensionSuresh ShresthaNo ratings yet
- Drug Index Updated2Document113 pagesDrug Index Updated2tam meiNo ratings yet
- Arya 18 4 2379Document8 pagesArya 18 4 2379Kiki KokolNo ratings yet