Professional Documents
Culture Documents
Endocrine
Uploaded by
Datu Hakeem Hadji Norodin0 ratings0% found this document useful (0 votes)
23 views17 pagesThe adrenal glands produce hormones that help regulate metabolism, the immune system, blood pressure, stress response and other functions. They are located above the kidneys and have two main parts - the adrenal cortex and medulla. The cortex produces cortisol, aldosterone and other hormones. The medulla produces epinephrine and norepinephrine to initiate the fight or flight response. Hypofunction can cause Addison's disease, while hyperfunction can cause Cushing's syndrome, both with various symptoms.
Original Description:
endocrine science biology
Original Title
endocrine
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThe adrenal glands produce hormones that help regulate metabolism, the immune system, blood pressure, stress response and other functions. They are located above the kidneys and have two main parts - the adrenal cortex and medulla. The cortex produces cortisol, aldosterone and other hormones. The medulla produces epinephrine and norepinephrine to initiate the fight or flight response. Hypofunction can cause Addison's disease, while hyperfunction can cause Cushing's syndrome, both with various symptoms.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
23 views17 pagesEndocrine
Uploaded by
Datu Hakeem Hadji NorodinThe adrenal glands produce hormones that help regulate metabolism, the immune system, blood pressure, stress response and other functions. They are located above the kidneys and have two main parts - the adrenal cortex and medulla. The cortex produces cortisol, aldosterone and other hormones. The medulla produces epinephrine and norepinephrine to initiate the fight or flight response. Hypofunction can cause Addison's disease, while hyperfunction can cause Cushing's syndrome, both with various symptoms.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 17
NCM114 - Endocrine System
Lesson 1.4. Adrenal Glands
Adrenal glands, also known as
suprarenal glands, are small,
triangular-shaped glands located
on top of both kidneys.
Adrenal glands produce hormones
that help regulate your
metabolism, immune system,
blood pressure, response to stress
and other essential functions.
An adrenal gland is made of two It is released norepinephrine
main parts: during times of (noradrenaline)
stress to help your these hormones are capable
o The adrenal cortex is the body get an of increasing the heart rate
outer region and also the energy boost and and force of heart
largest part of an adrenal better handle an contractions, increasing
gland. emergency blood flow to the muscles
o The adrenal medulla is situation. and brain, relaxing airway
located inside the adrenal Aldosterone - This smooth muscles, and
cortex in the center of an mineralocorticoid assisting in glucose (sugar)
adrenal gland hormone plays a central metabolism.
o The adrenal cortex and role in regulating blood They also control the
adrenal medulla are pressure and certain squeezing of the blood
enveloped in an adipose electrolytes (sodium and vessels (vasoconstriction),
capsule that forms a potassium). helping maintain blood
protective layer around an Androgenic Steroids - pressure and increasing it in
adrenal gland. are weak male response to stress.
Hormones of the Adrenal hormones. They are Epinephrine and
Glands precursor hormones that norepinephrine are often
o from the Adrenal Cortex are converted in the activated in physically and
Cortisol - is a ovaries into female emotionally stressful
glucocorticoid hormone hormones (estrogens) situations when your body
that helps control the and in the testes into needs additional resources
body’s use of fats, male hormones and energy to endure
proteins and (androgens). However, unusual strain.
carbohydrates; estrogens and
suppresses androgens are produced Hypofunction of the Adrenal
inflammation; regulates in much larger amounts Glands
blood pressure; by the ovaries and ADRENAL
increases blood sugar; testes. INSUFFICIENCY/ADDISON’
and can also decrease o From the Adrenal Medulla S DISEASE
bone formation. controls hormones that
This hormone initiate the flight or fight o Addison’s disease is
also controls the response, the epinephrine a disorder in which the
sleep/wake cycle. (adrenaline) and adrenal do not produce
enough of the hormones infections, and fungal Vomiting
cortisol and aldosterone. infections Worsening fatigue
Cancer cells from (extreme tiredness)
o Cortisol helps the body another part of the body o Addisonian Crisis
respond to stress, including that have invaded the In some cases – such
the stress of illness, injury, adrenal glands as an injury, illness, or
or surgery. It also helps Bleeding into the time of intense stress –
maintain blood pressure, adrenal glands symptoms can come on
heart function, the immune Surgical removal of the quickly and cause a
system and blood glucose adrenal glands serious event called an
(sugar) levels. Genetic defects Addisonian crisis, or
o Symptoms: acute adrenal
o Aldosterone affects the Abdominal pain insufficiency. An
balance of sodium and Abnormal menstrual Addisonian crisis is a
potassium in the blood. periods medical emergency. If it
This in turn controls the Craving for salty food is not treated, it can
amount of fluid the kidneys Dehydration lead to shock and
remove as urine, which Depression death.
affects blood volume and Diarrhea Symptoms:
blood pressure. Irritability Feeling
Lightheadedness restless, confused, or
o Affects 1 in 100,000 or dizziness when afraid, or other mental
people. It occurs in both standing up changes
men and women equally Loss of appetite Dehydration
and in all age groups, but is Low blood glucose Extreme weakness
most common in the 30-50 Low blood pressure Having trouble
year-old age range. Muscle weakness staying awake, or
o Causes: Nausea a total loss of
Autoimmune Disorder Patches of dark skin, consciousness
Injury to the adrenal especially High fever
glands around scars, skin Lightheadedness or
Infection, folds, and joints feeling faint
including tuberculosis, Sensitivity to cold
Paleness
HIV/AIDS-related Unexplained weight
Severe vomiting and
loss
diarrhea
Sudden, deep pain in o Children who are born with manifestations of cortisol
the lower back, belly this disorder are missing an excess, has two causes:
or legs essential enzyme Adrenal tumor that causes
o Diagnosis necessary to produce the adrenal gland to
History and physical: cortisol, aldosterone or produce excessive
Blood tests: These will both. At the same time, glucocorticoid (cortisol)
be done to measure the they often experience Prolonged administration
levels of sodium, excess of androgen, which of corticosteroid therapy
potassium, cortisol and may lead to male o Risk factors
ACTH in the blood. characteristics in girls Female
ACTH stimulation and precocious puberty in Altered pituitary function
test: This tests the boys. Prolonged corticosteroid
adrenal glands’ therapy
response after being o Congenital adrenal Tumor of the adrenal
given a shot of artificial hyperplasia can remain cortex
ACTH. If the adrenal undiagnosed for years o Signs and symptoms
glands produce low depending on the severity
levels of cortisol after of the enzyme deficiency.
the shot, they may not In more severe cases,
be functioning properly. infants may suffer from
X-rays ambiguous genitalia,
Computed dehydration, vomiting and
tomography (CT scan) failure to thrive.
o Treatment: Hormonal
Replacement Therapy Hyperfunction of the Adrenal
hydrocortisone pills for Glands
cortisol replacement CUSHING’S SYNDROME
fludrocortisone acetate o Cushing’s Disease results
pills for aldosterone when too much ACTH
replacement (adrenocorticotropic
hormone) is produced by a
CONGENITAL ADRENAL tumor of the pituitary gland. Weight gain specially in the
HYPERPLASIA o Cushing’s syndrome which trunk, face and neck
refers to the clinical (“buffalo hump”)
o A genetic disorder.
Muscle wasting of c. Signs of infection HYPERALDOSTERONISM
extremities d. Urinary and serum o Hyperaldosteronism results
Weakness glucose levels from overproduction of
Ruddy complexion 2. Nursing Activities aldosterone from one or
“moon face” a. Provide emotional both adrenal glands. This is
Abdominal striae support related to characterized by increase in
Hyperglycemia body image changes blood pressure that often
Electrolyte imbalances and mood swings requires many medications
Emotional b. Promote skin integrity to control. Some people can
changes/depression c. Prevent injury develop low potassium
Excessive hair growth in d. Encourage intake in levels in the blood, which
women high protein, low can cause muscle aches,
Thin, easily bruised skin calorie diet weakness and spasms.
Risk for infection, immune e. Assist with o When the cause is adrenal
suppression preparation for oversecretion, the disease is
Bone demineralization surgery if indicated called Conn syndrome.
Cataracts f. Prepare for radiation PHEOCHROMOCYTOMA
Glaucoma therapy if indicated is a tumor that results in
Hypertension g. Teach the client the excess production of
o Diagnostic and Laboratory importance of not adrenaline or
Tests discontinuing noradrenaline by the
History and physical corticosteroid adrenal medulla that often
examination medications abruptly happens in bursts.
Urine cortisol o Pharmacology o Pheochromocytoma may
Plasma cortisol Adrenal enzyme inhibitors cause persistent or sporadic
Dexamethasone for Cushing’s disease high blood pressure that
suppression test caused by tumor may be difficult to control
MRI o Complications with regular medications.
CT Scan Secondary diabetes Other symptoms include
Ultrasound mellitus headaches, sweating,
o Therapeutic Nursing Osteoporosis and tremors, anxiety and rapid
Management spontaneous fractures heartbeat. Some people are
1. Assess/Monitor Alteration in mental status genetically predisposed to
a. Intake and Output Shock developing this type of
b. Weight Death tumor.
Insulin are secreted by the beta of fats and conversion of fat
cells into ketone bodies
Glucagon are secreted by the o Stimulates protein synthesis
alpha cells within the tissues and inhibits
Somatostatin and gastrin are the breakdown of protein into
synthesized by the delta cells. amino acids
Gastrin is used in the metabolism Glucagon:
of foods o Promotes a rise in blood
Somatostatin decreases the glucose level when glucose
secretion of insulin, glucagon, levels drop too low by
growth hormone, gastrin promoting the conversion of
Insulin and Glucagon are the liver glycogen into glucose.
primary pancreatic hormones Factors needed for insulin and
secreted by these cells and plays glucagon release:
a vital role in the control of o A healthy pancreas with
carbohydrate metabolism functioning alpha and beta
Insulin: cells
o Stimulates the active o A diet adequate in protein.
transport of glucose into Both insulin and glucagon
muscle and adipose tissue are protein substances
cells o Normal potassium levels
o Regulates the rate at which Diabetes Mellitus
carbohydrates are used by DEFINITION
Lesson 1.5. Pancreas cells for energy o Diabetes Mellitus is a group
o Promotes the conversion of of metabolic diseases
Pancreas is a large fish-shaped glucose to glycogen for characterized by increased
organ that lies Sbehind the storage and inhibits the levels of glucose in the blood
stomach conversion of glycogen into resulting from defects in
It has both exocrine and glucose insulin secretion, insulin
endocrine functions o Promotes the conversion of action or both (American
The endocrine functions of the fatty acids into fat, to be Diabetes Association, 2004).
pancreas are carried out by the stored as adipose tissue, o Hyperglycemia refers to
islets of Langerhans which inhibits the breakdown of elevated in blood glucose
contains alpha, beta and delta adipose tissue, mobilization level, fasting level greater
cells than 110mg/dL (6.1 mmol/L)
o Hypoglycemia refers to low Diabetes environmental Non-ketotic
blood glucose level (less than Mellitus factors coma
60 mg/dL [less than 2.7 (IDDM) Little or no
mmol/L]) endogenous Gestati Gestational Onset during
RISK FACTORS insulin onal Diabetes pregnancy,
o Family History Need insulin Diabete usually in the
o Obesity to preserve s 2nd or 3rd
o Race/ethnicity (African- life trimester of
American, Hispanic- High risk to pregnancy
American, Native Americans, diabetic Due to
Asian Americans) ketoacidosis hormones
o Age >45 yo (DKA) secreted by
o Previously identified impaired the placenta,
Type 2 Adult-onset Onset at any which inhibit
fasting glucose or impaired
DM (90- diabetes age, usually the action of
glucose tolerance
95% of Non-Insulin over 30 yo insulin
o Hypertension
all Dependent Usually obese Occurs about
o Elevated HDL and/or
diabete Diabetes at diagnosis 2-3% of all
triglyceride level s) Mellitus Causes pregnancies
o History of gestational Obese (NIDDM) includes
diabetes or delivery of babies (80% of obesity,
over 9lb type 2) heredity and PHYSIOLOGY
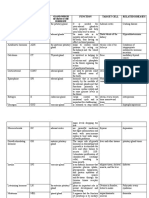
TYPES/CLASSIFICATIONS Non- environmental o Insulin is secreted by beta cells
obese factors of the Islets of Langerhans in
TYPE PREVIOUS CLINICAL
(20% of Decrease in the pancreas.
CLASSIFICA CHARACTERI
TIONS STICS AND
type 2) endogenous o When a person eats, insulin
IMPLICATION insulin, or secretion increases and moves
S increased glucose from the blood to the
Type 1 Juvenile Onset at early with insulin muscle, liver and fat cells. In
DM (5- Diabetes age resistance those cells, insulin
10% of Juvenile- Etiology Acute Transports and
all onset includes complication: metabolizes glucose for
diabete Diabetes genetic, Hyperglycemi energy
s) Insulin immunologic c Stimulates storage of
Dependent and Hyperosmolar glucose in the liver and
muscle (in the form of Refractoriness to insulin This can lead to
glycogen) in the cell membrane acidosis (diabetic
Signals the liver to stop receptor ketoacidosis) and
the release of glucose Seen in persons with increased osmotic
Enhances storage of long-term obesity diuresis
dietary fat in the adipose METABOLIC EFFECTS OF When fats are used for
tissue DIABETES a primary source of
Accelerates the transport o Decreased utilization of energy, the body fluid
of amino acids (derived glucose level increases and can
from dietary protein) into Glucose remains in the lead to atherosclerosis
cells blood causing blood o Increased protein utilization
o Insulin also inhibits the glucose level to rise – Without insulin to
breakdown of stored glucose, HYPERGLYCEMIA stimulate protein
protein and fat The kidney will excrete synthesis, protein
o Glucagon is another pancreatic excess glucose – wasting happens
hormone secreted by the alpha GLUCOSURIA Results to being thin
cells of the islets of Glucose excreted in the and emaciated of the
Langerhans which is released urine acts as osmotic affected individual, this
when blood glucose levels diuretic that causes leads to increase desire
decrease and stimulates the increase fluid excretion to eat (POLYPHAGIA)
liver to release stored glucose. (POLYURIA) and CARDINAL SIGNS OF
o Both insulin and glucagon results to fluid volume DIABETES
maintain a constant level of deficit, increased thirst Clinical Pathophysiologic
glucose in the blood by and increase fluid Manifestations Bases
stimulating the release of intake (POLYDIPSIA) Polyuria Water not
glucose from the liver. o Increased fat metabolism (frequent reabsorbed from
PATHOPHYSIOLOGY The body rely on fat urination) renal tubules
o IDDM stores as source of because of the
Associated with energy osmotic activity
inflammation of the islets The process of fat of glucose in the
of Largerhans (Insulitis) metabolism leads to the tubules
which appears to be an formation of breakdown Polydipsia Polyuria causes
autoimmune response products called (excessive severe
o NIDDM KETONES thirst) dehydration
which causes
thirst syndrome (HHS) is a resulting to
Polyphagia Tissue serious complication hyperglycemia
(excessive breakdown and of NIDDM. HHS and metabolic
hunger) wasting cause a occurs when a acidosis.
state of person’s blood Blood glucose
starvation that glucose (sugar) levels levels higher than
compels the are too high for a long 300mg/dL
client to eat period, leading to Kussmaul’s
excessive severe dehydration respirations
amounts of food (extreme thirst) and (deep, gasping,
Weight loss Glucose not confusion rapid breathing
(primarily available on the High blood sugar associated with
IDDM) cells, thus the level (over 600 severe diabetic or
body breaks mg/dL) renal acidosis or
down fat and If not treated, can coma)
protein stores for lead to Blood pH less
energy Seizures than 7.3
Coma. Presence of
Other manifestations Swelling of the serum ketones,
o Fatigue and weakness brain. urine ketones
o Vision disturbances Organ failure. (KETONURIA)
o Confusion and changes in Death. and glucose
mentation Abnormal levels
o Delayed wound healing o Diabetic Ketoacidosis of serum sodium,
o Behavioural changes, (DKA) is a life- potassium and
including irritability threatening chloride
Complications complication of IDDM, Fruity (acetone)
o Hyperglycemic resulting from severe odor to breath
Hyperosmolar Nonketotic insulin deficiency. Hypotension
Coma In response to CNS depression
(HHNK)/Hyperosmolar insulin deficiency, progressing to
Hyperglycemic Syndrome the body uses fats coma, cerebral
(HHS) and proteins to anoxia and death
Hyperosmolar meet cellular
hyperglycemic metabolic needs, CHRONIC COMPLICATIONS
o Macroangiopathy numbness and Therapeutic Nursing
(Atherosclerosis) pain, usually in Management
A disease of the large the hands and o Assess/monitor
blood vessels in feet. Dietary intake
which fat and blood o Autonomic For factors that may
clots build up and Neuropathy impede the client’s
stick to the vessel Occurs when ability to learn or
walls, blocking the there is damage perform self-care
flow of blood to the nerves For signs of
Coronary artery that control hypoglycaemia or
disease (CAD) automatic body insulin shock
Cerebrovascula functions. It can Skin for alterations
r disease affect blood For signs of infection
Peripheral pressure, For risk of injury/falls
vascular temperature related to
disease control, neuropathies
o Microangiopathy digestion, For signs of DKA
Is a disease of the bladder function Acid-base status
microvessels, small and sexual Electrolyte status
blood vessels in the function. o Nursing Activities
microcirculation o Infections Encourage self-care
Retinopathy Diagnostic and laboratory test Teach regarding self-
Nephropathy o History and physical administration of
o Neuropathy examination insulin or oral
o Peripheral o GTT (glucose tolerance hypoglycemic agents
Neuropathy test) Teach regarding
A result of o FBG/FBS (fasting blood specific dietary
damage to the glucose/fasting blood requirements
nerves located sugar) Teach client signs
outside of the o GHb (glycosylated and symptoms of
brain and spinal haemoglobin) hypoglycaemia and
cord (peripheral o Urine glucose and ketone insulin shock
nerves) that levels Encourage increased
often cause o Serum electrolytes intake of dietary fiber
weakness,
Encourage daily o Oral Hypoglycemic agents o Avoid tight socks and
exercise. Exercise (acarbone, metformin) shoes
promotes utilization o Insulin therapy o
of carbohydrates o Complications of Insulin
Teach regarding therapy
alterations in insulin Hypoglycemia
administration if sick, Tissue
NPO or physically hyperthrophy or
active. Infection is Atrophy
associated with Insulin allergy
insulin resistance Insulin resistance Foot and Skin
Encourage Care 1
avoidance of o Do not soak feet unless
smoking to reduce directed to do so
cardiovascular risks o Use mild soap and
Provide emotional
washcloth to clean
support for family
between toes
and client
o Check water temperature
Teach regarding
o Use lotion with lanolin
blood glucose
monitoring o Do not use harsh
Encourage regular chemicals (betadine,
blood glucose peroxide) on the feet 2
monitoring o Cut nails straight across
Encourage use of a and not an angle
medical alert bracelet o See a podiatrist if possible
or card o Do not go barefoot
Teach client and o Do not use hot water
family the signs of bottles, heating pads
hyperglycemia, o Wear good-fitting shoes,
hypoglycaemia or leather shoes are
DKA encouraged
Pharmacology and Treatment 3
You might also like
- Bodybuilding Chemical Muscle Enhancement SteroidsDocument226 pagesBodybuilding Chemical Muscle Enhancement SteroidsLak vir Singh100% (3)
- Practical MindfulnessDocument70 pagesPractical Mindfulnessnagaraja100% (4)
- Endocrine SystemDocument14 pagesEndocrine SystemNovie Jane HontiverosNo ratings yet
- Qigong For Strengthening The KidneysDocument15 pagesQigong For Strengthening The Kidneysdan20050505100% (1)
- Adrenal Fatigue Cure Guide (Beat Chronic fatigue): Restoring your Hormones and Controling Thyroidism: Restoring your Hormones and Controling ThyroidismFrom EverandAdrenal Fatigue Cure Guide (Beat Chronic fatigue): Restoring your Hormones and Controling Thyroidism: Restoring your Hormones and Controling ThyroidismRating: 1 out of 5 stars1/5 (1)
- Adrenal Fatigue: Understanding the Symptoms: How Malfunctioning Adrenal Glands Negatively Affect the BodyFrom EverandAdrenal Fatigue: Understanding the Symptoms: How Malfunctioning Adrenal Glands Negatively Affect the BodyNo ratings yet
- Theories of LabourDocument22 pagesTheories of LaboursubashikNo ratings yet
- The Endocrine Glands & Their HormonesDocument35 pagesThe Endocrine Glands & Their HormonesEtta Sagita Leonora100% (1)
- Adrenal Gland DisordersDocument7 pagesAdrenal Gland Disorderscn351073No ratings yet
- Addison' S Disease: Case PresentationDocument34 pagesAddison' S Disease: Case PresentationShane Olanosa PillonarNo ratings yet
- Adrenal InsufficiencyDocument33 pagesAdrenal InsufficiencypukitagabNo ratings yet
- NCM 116: Neurologic Dysfunctions: Joyce Bernadette P. Andot - Anna Delle Nicole P. Aranding, BSN-IIIDocument46 pagesNCM 116: Neurologic Dysfunctions: Joyce Bernadette P. Andot - Anna Delle Nicole P. Aranding, BSN-IIIMercy Anne EcatNo ratings yet
- Addison's DiseaseDocument1 pageAddison's DiseaseDurrotul SalmaNo ratings yet
- Adrenal Fatigue: Enhancing Quality of Life For Patients With A Functional DisorderDocument6 pagesAdrenal Fatigue: Enhancing Quality of Life For Patients With A Functional Disordercraig10140% (1)
- UWorld Endocrinology - Pathology PhysiologyDocument136 pagesUWorld Endocrinology - Pathology PhysiologyDaniel DiasNo ratings yet
- The Teenage Brain: New Knowledge From NeuroscienceDocument7 pagesThe Teenage Brain: New Knowledge From NeuroscienceLegal MomentumNo ratings yet
- Stress Management.Document404 pagesStress Management.James Adhikaram100% (1)
- Introduction To Adrenal Fatigue DR LamDocument21 pagesIntroduction To Adrenal Fatigue DR Lamiri_bal0% (1)
- Addison's DiseaseDocument17 pagesAddison's DiseaseMah Jezthy100% (1)
- 02 StressDocument44 pages02 StressnowayidontwantitNo ratings yet
- Autoimmune DiseasesDocument125 pagesAutoimmune DiseasesJustin Ahorro-DionisioNo ratings yet
- Biology: D.Harish Kannan Topic: Addison's DiseaseDocument7 pagesBiology: D.Harish Kannan Topic: Addison's DiseaseG. ShanjanaNo ratings yet
- Diseases of Circulatory SystemDocument7 pagesDiseases of Circulatory SystemMary Anne YadaoNo ratings yet
- Igcse Biology: Co-Odination and ResponseDocument9 pagesIgcse Biology: Co-Odination and ResponseThamiso GolwelwangNo ratings yet
- Endocrine System: One of Us, and I'm Not Certain Which, Has A Glandular DisorderDocument10 pagesEndocrine System: One of Us, and I'm Not Certain Which, Has A Glandular Disorderroserem2000No ratings yet
- Adrenal Glands MS2Document38 pagesAdrenal Glands MS2Tatiana Leashe WootenNo ratings yet
- Adrenal Gland Grp5Document17 pagesAdrenal Gland Grp5Kathrine GoNo ratings yet
- Stress and AdaptationDocument4 pagesStress and AdaptationAlec Xavier MirandaNo ratings yet
- The Endocrine SystemDocument38 pagesThe Endocrine Systemsaifulla dubaiNo ratings yet
- Adrenal GlandsDocument2 pagesAdrenal GlandsYary MayorNo ratings yet
- Module 3 - Non-Communicable DiseaseDocument2 pagesModule 3 - Non-Communicable DiseasejessafesalazarNo ratings yet
- Hormones, The Endocrine System and HomeostasisDocument5 pagesHormones, The Endocrine System and Homeostasischiusavi77No ratings yet
- Endocrine SystemDocument22 pagesEndocrine SystemUnknownKidNo ratings yet
- NCMB 316 Lecture & RleDocument34 pagesNCMB 316 Lecture & RleVenansius GanggusNo ratings yet
- Adrenal GlandDocument16 pagesAdrenal GlandTanya SinghNo ratings yet
- Chapter 15 - Hormones & Endocrine GlandsDocument17 pagesChapter 15 - Hormones & Endocrine Glandsapi-3728508100% (1)
- Insufisiensi Adrenal (Dr. Makbul)Document52 pagesInsufisiensi Adrenal (Dr. Makbul)Rahmat AzimiNo ratings yet
- Adrenalglandlecture 111115200310 Phpapp01Document25 pagesAdrenalglandlecture 111115200310 Phpapp01varshasharma05No ratings yet
- Adrenal GlandDocument28 pagesAdrenal GlandAthar Habib ShahaniNo ratings yet
- EndocrineDocument7 pagesEndocrineKharrel YballeNo ratings yet
- WK 4 Learning IssuesDocument7 pagesWK 4 Learning Issuesjacintacw7No ratings yet
- AdrenalDocument5 pagesAdrenalJC MolNo ratings yet
- Adrenal Glands: Crishkey Cuario Nathaniel Estipona Mario Revillosa Jopay ContrerasDocument8 pagesAdrenal Glands: Crishkey Cuario Nathaniel Estipona Mario Revillosa Jopay ContrerasKathlene BalicoNo ratings yet
- SCIENCE-REPORT-GROUP-2.pdf 20240211 212133 0000Document48 pagesSCIENCE-REPORT-GROUP-2.pdf 20240211 212133 0000taishishiroganeNo ratings yet
- Hormone Abbreviation Function Target Cell Related Diseases: Gland Which Secretes The HormoneDocument4 pagesHormone Abbreviation Function Target Cell Related Diseases: Gland Which Secretes The HormoneMarianne Jubille CataquisNo ratings yet
- Endo 3 Notes PDFDocument9 pagesEndo 3 Notes PDFDilNo ratings yet
- Lecture 15 - Adrenal Gland BNS KUMDocument17 pagesLecture 15 - Adrenal Gland BNS KUMabdulsaboor30No ratings yet
- BIOLOGY 10 REVIEWER - 3rd QuarterDocument10 pagesBIOLOGY 10 REVIEWER - 3rd QuarterGeromme TudNo ratings yet
- Hormonas de Estrés English FinalDocument46 pagesHormonas de Estrés English FinalGuillermo Alfonso Solórzano MoralesNo ratings yet
- Endocrine System ActivityDocument4 pagesEndocrine System ActivityPablo GarciaNo ratings yet
- Dynamic Balance: Steady BalanceDocument17 pagesDynamic Balance: Steady Balancesakura1717No ratings yet
- The Endocrine Glands & Their HormonesDocument35 pagesThe Endocrine Glands & Their HormonesRizky PratamaNo ratings yet
- CortisolDocument4 pagesCortisollevelupwithlaura21No ratings yet
- Bio - EndocrineDocument16 pagesBio - EndocrineYash PrajapatiNo ratings yet
- Control CoordinationDocument7 pagesControl CoordinationShaurya AgrawalNo ratings yet
- Endocrine Disorders and Their PharmacotherapyDocument4 pagesEndocrine Disorders and Their PharmacotherapyYemaya84No ratings yet
- Stress and AdaptationDocument4 pagesStress and AdaptationJonna EstabilloNo ratings yet
- Lecture 13Document23 pagesLecture 13Rezwan Noor NSUNo ratings yet
- Anatomy & Physiology Endocrine System: Ilah M, SKPDocument36 pagesAnatomy & Physiology Endocrine System: Ilah M, SKPOmbun FajarNo ratings yet
- Steroids AND TerpenesDocument88 pagesSteroids AND Terpenesbuttercuplady_18763No ratings yet
- Ana, Patho UroDocument5 pagesAna, Patho UroDan Ataniel EnsaladaNo ratings yet
- Adrenal GlandDocument9 pagesAdrenal GlandArzooGargNo ratings yet
- Chapter 5 - The Endocrine System - FinalDocument57 pagesChapter 5 - The Endocrine System - FinalKharrel YballeNo ratings yet
- Ca1 DLP Ms2 Nursing Care Management 103 CodyyoungbloodDocument3 pagesCa1 DLP Ms2 Nursing Care Management 103 CodyyoungbloodYoungbloodNo ratings yet
- Anatomy: Pineal GlandDocument5 pagesAnatomy: Pineal GlandJoshua LuminariasNo ratings yet
- Nursing Intervention For DKADocument3 pagesNursing Intervention For DKADarius CrisostomoNo ratings yet
- Anatomy ActivityDocument15 pagesAnatomy ActivityAllesa San JoseNo ratings yet
- Q3 1 EndocrineDocument42 pagesQ3 1 Endocrineerlamay.valeNo ratings yet
- Clinical MarasmusDocument27 pagesClinical MarasmusHANNo ratings yet
- NCMB 316 Lec Midterm 1Document14 pagesNCMB 316 Lec Midterm 1zh4hft6pnzNo ratings yet
- Jillian Michaels - HormonesDocument6 pagesJillian Michaels - HormonesalerynNo ratings yet
- A New Paradigm For Student LearnersDocument92 pagesA New Paradigm For Student LearnersTerry DoyleNo ratings yet
- 4.1 Reading VocabularyDocument4 pages4.1 Reading VocabularyMahmoud RammalNo ratings yet
- CUSHING'S SyndromeDocument9 pagesCUSHING'S SyndromeTheavuthyNo ratings yet
- AldosteronismDocument48 pagesAldosteronismMiguel Cuevas DolotNo ratings yet
- Cortisol II 2020-03 v6Document5 pagesCortisol II 2020-03 v6Parishan SaeedNo ratings yet
- Biochemistry JD 2Document6 pagesBiochemistry JD 2failinNo ratings yet
- Effects of Stress On Human Health: By: Liza Ormol 5 SemesterDocument14 pagesEffects of Stress On Human Health: By: Liza Ormol 5 SemesterANA LEE MENDOZANo ratings yet
- Midl Nursing NowDocument213 pagesMidl Nursing Nowbemina jaNo ratings yet
- Answers To Case StudiesDocument7 pagesAnswers To Case StudiesPhú NguyễnNo ratings yet
- Webinar 14 Juli 2020: Dr. Rachmi Primadiati, Darom, Dherbmed, Cidesco, CibtacDocument35 pagesWebinar 14 Juli 2020: Dr. Rachmi Primadiati, Darom, Dherbmed, Cidesco, CibtacDefi PazdilaNo ratings yet
- Laboratory and Diagnostic Tests Answer KeyDocument25 pagesLaboratory and Diagnostic Tests Answer KeyCourtney Dela FierraNo ratings yet
- Learning and The BrainDocument5 pagesLearning and The BrainBrendan MakidonNo ratings yet
- Uman Hysiology: Endocrine Control of Growth and MetabolismDocument24 pagesUman Hysiology: Endocrine Control of Growth and Metabolismpanairina03026273No ratings yet
- LaughterDocument4 pagesLaughterRizqon Sya'baniNo ratings yet
- AACE Abstracts 2019 Los AngelesDocument357 pagesAACE Abstracts 2019 Los Angelesmimran1974No ratings yet
- Internal Medicine TopicsDocument56 pagesInternal Medicine TopicsBogdan UrichianuNo ratings yet
- Effects of Yoga Practice On Neuroendocrinological ChangesDocument6 pagesEffects of Yoga Practice On Neuroendocrinological ChangesJelly JewelryNo ratings yet
- Adrenal PathophysiologyDocument5 pagesAdrenal PathophysiologyditabokNo ratings yet