Professional Documents
Culture Documents
Myasthenia Gravis: Murali Thavasothy DCH MRCP FRCA Nicholas Hirsch FRCA
Uploaded by
Mirela CiobanescuOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Myasthenia Gravis: Murali Thavasothy DCH MRCP FRCA Nicholas Hirsch FRCA
Uploaded by
Mirela CiobanescuCopyright:
Available Formats
Myasthenia gravis
Murali Thavasothy DCH MRCP FRCA
Nicholas Hirsch FRCA
Aetiology Table 1 Classification of myasthenia gravis
Key points
Myasthenia gravis (MG) is an autoimmune Type
Myasthenia gravis is an
condition in which IgG autoantibodies interact I Ocular signs and symptoms only
autoimmune disease in
with the postsynaptic acetylcholine receptors IIA Generalised mild muscle weakness responding
which IgG antibodies
well to therapy
decrease postsynaptic (AChR) at the nicotinic neuromuscular junction IIB Generalised moderate muscle weakness
receptor density at the (NMJ). The AChR antibodies reduce the num- responding less well to therapy
neuromuscular junction III Acute fulminating presentation and/or
ber of functional receptors by blocking attach-
The cardinal feature is respiratory dysfunction
ment of acetylcholine molecules, by increasing IV Myasthenic crisis requiring artificial ventilation
weakness and fatigability
of voluntary muscles the rate of degradation of the receptors and by
Pre-operative manage- complement-induced damage to the NMJ.
ment must include care- Thus, patients with MG have a reduced AChR exercise (fatigability) and is relieved with rest.
ful assessment of respira- density and, on average, have 30% of the nor- In 15% of patients, the disease is confined to the
tory and bulbar muscle eyes with diplopia and ptosis being the most
mal number of AChR. Therefore, the normal
function and optimisation
‘margin of safety’ found at the NMJ in health is common symptom and sign. However, in the
of medication
lost. remaining 85%, the disease is generalised with
Patients are extremely
sensitive to non-depolar- Although it is widely accepted that MG is an weakness of ocular, facial, bulbar and limb
ising neuromuscular antibody-mediated condition, the origin of the muscles. Although respiratory muscles are nor-
blocking drugs mally affected only mildly, respiratory failure
process remains uncertain. However, the thy-
There may be resistance mus gland has been implicated as a possible requiring artificial ventilation may occur, i.e.
to the effects of succinyl- myasthenic crisis. The distribution of weakness
choline generator of the immune process. The gland is
abnormal in 75% of patients with MG (85% and the response to drug therapy allows classi-
A period of postopera-
hyperplasia, 15% thymoma). One hypothesis fication of MG (Table 1).
tive ventilation may be
necessary following suggests that the B and T lymphocytes within
major surgery Diagnosis
the thymus become sensitised to AChR found
on ‘myoid’ cells within the gland. The reason The diagnosis of MG depends on a careful his-
for a breakdown in the normal immune toler- tory and examination, pharmacological tests,
ance between these components in the thymus electromyography (EMG) and detection of the
gland remains obscure. anti-AChR antibodies. Although historically an
exaggerated response to a small dose of curare
was taken as evidence supporting the diagnosis
Clinical features of MG, the Tensilon test, in which up to 10 mg
Murali Thavasothy
Myasthenia gravis affects 1 in 10,000 of the of edrophonium is administered i.v., is the stan-
DCH MRCP FRCA
Specialist Registrar, Department of population, predominantly young women dard pharmacological test. Patients with MG
Anaesthesia,The Royal Free (20–30 yr) and older men (60–70 yr). The often show a marked improvement in muscle
Hospital, Pond Street,
London NW3 2GQ, UK reduced AChR density seen in MG results in power after 30 s and this is sustained for
Nicholas Hirsch FRCA decreased amplitude of action potentials in the approximately 5 min. A negative result does not
Consultant Anaesthetist,The postsynaptic region causing a failure in initia- exclude MG. The most commonly used EMG
National Hospital for Neurology and tion of muscle fibre contraction. When this
Neurosurgery, Queen Square,
test in the diagnosis of MG is the recording of
London WC1N 3BG, UK occurs at many NMJs, it is manifest clinically compound muscle action potentials (CMAP)
(for correspondence)
Tel: 020 7829 8711
as weakness of voluntary muscle – the cardinal following repetitive stimulation of the motor
Fax: 020 7829 8734 feature of MG. The weakness is accentuated by nerve. In MG, repetitive stimulation results in a
British Journal of Anaesthesia | CEPD Reviews | Volume 2 Number 3 2002
88 © The Board of Management and Trustees of the British Journal of Anaesthesia 2002
Myasthenia gravis
Table 2 Autoimmune conditions associated with myasthenia gravis Thymectomy
Hyper/hypothyroidism Polymyositis/dermatomyositis Thymectomy is indicated for most patients with MG up to the
Rheumatoid disease Systemic lupus erythematosis age of 60 years and for those patients with a thymoma. The lat-
Scleroderma Pernicious anaemia ter may invade local mediastinal structures and ‘seed’ along the
Psoriasis/vitiligo
pleura. In patients with thymic hyperplasia, the aim is to induce
remission, or at least to produce sufficient improvement, to allow
the dose of immunosuppressive drugs to be reduced. The benefi-
progressive decrease (> 10%) in CMAP – a finding termed
cial effects may take several years to realise fully. Complete
decrement or fade. Single muscle fibre recordings are a more
removal of thymic tissue is necessary. Therefore, full exposure
sensitive indicator of neuromuscular junction blockade, but it
via a median sternotomy is the usual approach. However, some
must be stressed that all EMG abnormalities seen are not spe-
advocate removal via a cervical approach and mediastinoscopy.
cific for MG. Anti-AChR antibodies are detected in 80–85% of
patients with MG and are pathognomonic for the disease. Plasma exchange
Disorders associated with myasthenia gravis Plasma exchange is reserved for producing short-term remission
of myasthenic weakness in patients with a myasthenic crisis or
The immunological basis of MG is further re-inforced by the
those patients who need improvement before thymectomy. The
wide variety of other autoimmune diseases associated with the
reduction in the level of anti-AChR antibodies largely correlates
condition. These are listed in Table 2.
with the improvement in muscle power. Improvement is general-
ly seen within days of the exchange, but is usually short lived.
Treatment Complications include worsening of pre-existing infection, intra-
Standard treatment includes anticholinesterase and immunosup- venous catheter sepsis and haemodynamic instability.
pression therapy and thymectomy. In addition, short-term
improvement of myasthenic weakness may be effected by plas- Intravenous immunoglobulin
ma exchange and i.v. immunoglobulin. It must be remembered The indications for administering i.v. immunoglobulin are simi-
that some drugs may exacerbate myasthenic weakness. lar to those of plasma exchange. Improvement occurs within
days and may be sustained for months. Complications include
Anticholinesterase therapy
headaches and, rarely, renal failure.
The aim of anticholinesterase therapy is to enhance neuromuscu-
lar transmission by delaying degradation of ACh at the NMJ. Avoidance of drugs exacerbating myasthenia gravis
Pyridostigmine is the most commonly used drug in the UK. It Some drugs can worsen myasthenic weakness and should be
acts within 30 min, has a peak effect at 2 h and a clinical half-life avoided. The polymyxin group of antibacterial drugs cause
of approximately 4 h. Although often very effective initially, its blocking of AChR ion channels and the aminoglycoside antibi-
effects may diminish over months and most patients require otics decrease ACh release and postsynaptic AChR sensitivity.
immunosuppression. Procainamide, quinine and β-adrenergic receptor blocking drugs
may exacerbate weakness.
Immunosuppression therapy
Corticosteroids are the mainstay of treatment. Prednisolone is Anaesthetic management
given initially at 20 mg day–1 and gradually increased to 60 Anaesthetic management depends on the severity of disease and
mg day–1. Many patients show a worsening of their weakness in type of surgery being considered. Local and regional anaesthesia
the first 2 weeks of therapy. Once MG is controlled, the dose is should be employed when possible. General anaesthesia requires
gradually decreased to the lowest effective alternate day regimen. meticulous pre-operative and peri-operative care.
Azathioprine 1–2 mg kg–1 day–1 is often given in conjunction
with prednisolone in order to allow a reduction in the dose of cor- Pre-operative considerations
ticosteroid. Cyclosporine 5 mg kg–1 day–1 has been used as an Patients undergoing major elective surgical procedures should
alternative to prednisolone, but its high cost and nephrotoxicity be admitted 48 h prior to surgery. This allows detailed assess-
may limit its use. ment and monitoring of respiratory and bulbar function as
British Journal of Anaesthesia | CEPD Reviews | Volume 2 Number 3 2002 89
Myasthenia gravis
well as allowing adjustment of anticholinesterase and corti- ventilation. Many anaesthetists achieve tracheal intubation by
costeroid medication, if indicated. Chest physiotherapy is deepening anaesthesia using inhalational anaesthetic agents.
started at this time. Patients with severe MG may need a Patients with MG are more sensitive to the neuromuscular
course of plasma exchange or i.v. immunoglobulin before blocking effects of these agents and they often provide suffi-
surgery is considered. cient muscle relaxation without having to resort to the use of
The airway must be assessed carefully as associated neuromuscular blockers. Most avoid the latter because of the
rheumatoid disease may limit neck extension and flexion. In abnormal responses of MG patients. These responses are seen
addition, although unusual, a large thymoma may cause dis- even in patients with purely ocular myasthenia and those in
tortion and compression of the trachea. Respiratory muscle remission. Because of the reduced number of functional post-
function may be assessed in a number of ways, but serial mea- synaptic AChR, there is often a relative resistance to usual
surements of forced vital capacity (FVC) are the most repro- doses of succinylcholine and higher doses may be required.
ducible and easily performed test on the general ward. Pre- However, this may be followed by the development of a phase
operative factors that correlate with the need for prolonged II block.
ventilation following thymectomy include FVC < 2.9 litres, a In contrast, patients with MG are extremely sensitive to
history of chronic respiratory disease, grades III and IV MG non-depolarising neuromuscular blocking drugs. This sensi-
and a long history of the disease (> 6 yr). tivity varies according to agent. Thus, only one-tenth of the
Care must also be taken during the pre-operative assessment dose of tubocurare or pancuronium may be required for ade-
to exclude associated autoimmune disease (Table 2). Thyroid quate relaxation whereas 30–40% of the normal dose of
function testing is essential as approximately 15% of MG atracurium or vecuronium may be needed. The latter two
patients have some abnormality of the gland. Following pre- agents have gained popularity as they have a more predictable
operative evaluation, a full explanation of the procedure and duration of action than older agents. Furthermore, reversal of
anaesthetic course is given to the patient and this should their affects with anticholinesterases is often unnecessary and
include the possibility of needing postoperative mechanical this avoids the potential for a cholinergic crisis in the postop-
ventilation. erative period.
Many avoid the use of sedative premedication but, in the
absence of respiratory muscle compromise, it may be used
Postoperative management
safely. Antimuscarinic agents such as glycopyrronium are The majority of patients who have well-controlled MG pre-oper-
helpful in reducing secretions. Corticosteroid treatment is atively can have their tracheas safely extubated at the end of the
continued pre-operatively and additional hydrocortisone procedure. This especially applies to patients undergoing trans-
administered on the day of surgery. Traditionally, anti- cervical thymectomy who are less likely to require a period of
cholinesterase therapy is withheld on the morning of surgery postoperative ventilation than those undergoing trans-sternal
as myasthenic patients often do not require these drugs in the thymectomy. They should be nursed in a high-dependency area
immediate postoperative period. In theory, anticholinesterases and adequate analgesia provided. A combination of non-
may prolong the action of succinylcholine and possibly steroidal anti-inflammatory drugs and parenteral opioids usually
increase the requirements of non-depolarising neuromuscular provides good analgesia. Anticholinesterases are restarted at a
blocking drugs (but see below). reduced dose in the immediate postoperative period and are then
increased as necessary as the patient becomes ambulant.
Induction and maintenance of anaesthesia
Routine monitoring is supplemented with invasive blood pres- Key references
sure measurement in those patients undergoing median ster- Baraka A. Anaesthesia and myasthenia gravis. Can J Anaesth 1992; 39:
1992–6
notomy for thymectomy. Neuromuscular transmission should
Drachman DB. Myasthenia gravis. N Engl J Med 1994; 330: 1797–808
be monitored continuously during the procedure.
Krucylak PE, Naunheim KS. Preoperative preparation and anaesthetic
Following pre-oxygenation, anaesthesia is induced with management of patients with myasthenia gravis. Semin Thorac
thiopental or propofol. The trachea is then intubated using an Cardiovasc Surg 1999; 11: 47–53
oro- or nasotracheal tube. The latter may be preferred if there is
a possibility of requiring prolonged postoperative mechanical See multiple choice questions 62–66.
90 British Journal of Anaesthesia | CEPD Reviews | Volume 2 Number 3 2002
You might also like
- 2 Myasthenia Gravis and MS 2Document50 pages2 Myasthenia Gravis and MS 2Rawbeena RamtelNo ratings yet
- Miastenia GravisDocument28 pagesMiastenia Gravismariateresajijon7No ratings yet
- Myasthenia Gravis and Lambert-Eaton Myasthenic Syndrome - Continuum December 2016Document28 pagesMyasthenia Gravis and Lambert-Eaton Myasthenic Syndrome - Continuum December 2016Habib G. Moutran BarrosoNo ratings yet
- Motor Endplate Disorders Myasthenia Gravis Overview and DefinitionDocument4 pagesMotor Endplate Disorders Myasthenia Gravis Overview and DefinitionPJHGNo ratings yet
- 51.differential Diagnosis of Myasthenia Gravis - A ReviewDocument11 pages51.differential Diagnosis of Myasthenia Gravis - A ReviewSeptime TyasNo ratings yet
- Myasthenia Gravis Anesthetic Implications and ManagementDocument31 pagesMyasthenia Gravis Anesthetic Implications and Managementaashish45No ratings yet
- Review: Myasthenic CrisisDocument11 pagesReview: Myasthenic CrisisRaisha TriasariNo ratings yet
- RJN 2017 2 Art-04Document3 pagesRJN 2017 2 Art-04Ana GabrielaNo ratings yet
- Myasthenia Gravis and Other Neuromuscular Junction DisordersDocument8 pagesMyasthenia Gravis and Other Neuromuscular Junction Disordersidno1008No ratings yet
- Myasthenia Gravis: A Review: Hideyuki Matsumoto, MD, PHD and Yoshikazu Ugawa, MD, PHDDocument7 pagesMyasthenia Gravis: A Review: Hideyuki Matsumoto, MD, PHD and Yoshikazu Ugawa, MD, PHDZainal AbidinNo ratings yet
- Neuromuscular Junction DisordersDocument32 pagesNeuromuscular Junction Disordersepic sound everNo ratings yet
- L 7 ANESTHESIS Myasthenia GravisDocument20 pagesL 7 ANESTHESIS Myasthenia Graviskatherinerance331No ratings yet
- Myesthenia Gravis MedscapeDocument8 pagesMyesthenia Gravis MedscapeSarah OvinithaNo ratings yet
- Bja MGDocument6 pagesBja MGVignesh VenkatesanNo ratings yet
- Referat MG Desya BismillahDocument20 pagesReferat MG Desya BismillahDesya BillaNo ratings yet
- Myasthenia Gravis: Assoc. Prof. Dr. Rodica BălașaDocument31 pagesMyasthenia Gravis: Assoc. Prof. Dr. Rodica BălașaIstván MáthéNo ratings yet
- Neuromuscular DisordersDocument3 pagesNeuromuscular DisordersMaharaniDewiNo ratings yet
- Source 3Document3 pagesSource 3PJHGNo ratings yet
- Neuromuscular Junction DisorderDocument10 pagesNeuromuscular Junction DisorderZosmita Shane GalgaoNo ratings yet
- Myasthenia Gravis Lecture 12Document59 pagesMyasthenia Gravis Lecture 12Pop D. MadalinaNo ratings yet
- Myasthenia GravisDocument11 pagesMyasthenia GravisParvathy RNo ratings yet
- Presented By: VIVEK DEVDocument38 pagesPresented By: VIVEK DEVFranchesca LugoNo ratings yet
- Myasthenia GravisDocument17 pagesMyasthenia GravisYanski DarmantoNo ratings yet
- Jurnal Trigeminal Neuralgia 1Document12 pagesJurnal Trigeminal Neuralgia 1nabilla putriNo ratings yet
- MyasteniaDocument7 pagesMyastenialmcarmonaNo ratings yet
- Lambru2021 2Document12 pagesLambru2021 2Deyvid CapeloNo ratings yet
- MG Desya BismillahDocument20 pagesMG Desya BismillahDesya BillaNo ratings yet
- Myasthenia Gravis in Clinical Practice: Miastenia Gravis Na Prática ClínicaDocument9 pagesMyasthenia Gravis in Clinical Practice: Miastenia Gravis Na Prática ClínicaMasDhedotNo ratings yet
- Myasthenia Gravis ReferenceDocument19 pagesMyasthenia Gravis ReferenceIka Wulan PermataNo ratings yet
- Trigeminal Neuralgia - A Practical GuideDocument12 pagesTrigeminal Neuralgia - A Practical Guide전영우No ratings yet
- Myastenia Gravis PDFDocument7 pagesMyastenia Gravis PDFAdrian CiurciunNo ratings yet
- MG 2Document5 pagesMG 2vaishnaviNo ratings yet
- Anaesthesia For Children WithDocument5 pagesAnaesthesia For Children Withnanang hidayatullohNo ratings yet
- Debilidad Muscular en UciDocument16 pagesDebilidad Muscular en UcipakokorreaNo ratings yet
- Crisis MiastenicaDocument12 pagesCrisis MiastenicaOsvaldo CortésNo ratings yet
- Update On Ocular Myasthenia GravisDocument12 pagesUpdate On Ocular Myasthenia GravisAnonymous QLadTClydkNo ratings yet
- Autoimmune Myasthenia Gravis: Emerging Clinical and Biological HeterogeneityDocument16 pagesAutoimmune Myasthenia Gravis: Emerging Clinical and Biological HeterogeneityGiuseppeNo ratings yet
- Search Criteria: Table 1Document16 pagesSearch Criteria: Table 1Armansyah Nur DewantaraNo ratings yet
- Myasthenia GravisDocument18 pagesMyasthenia GravisvandanaNo ratings yet
- Step 7 1. Mengapa Pada Skenario Pasien Merasakan Lemah Pada Kelopak Mata Dan Mengapa Paling Berat Dirasakan?Document11 pagesStep 7 1. Mengapa Pada Skenario Pasien Merasakan Lemah Pada Kelopak Mata Dan Mengapa Paling Berat Dirasakan?novkar9No ratings yet
- MG-New and Emerging Treatments (Bmjmed-2023)Document6 pagesMG-New and Emerging Treatments (Bmjmed-2023)Apostolos T.No ratings yet
- Presentation On Myasthenia Gravis: Presented By: Sandhya Harbola M.Sc. Nursing 1 Year PcnmsDocument32 pagesPresentation On Myasthenia Gravis: Presented By: Sandhya Harbola M.Sc. Nursing 1 Year PcnmsShubham Singh Bisht100% (3)
- 114 Clinical Evaluation and Management of Myasthenia Gravis - DONEDocument22 pages114 Clinical Evaluation and Management of Myasthenia Gravis - DONEpyshcotNo ratings yet
- Myasthenia Gravis: Submitted ToDocument6 pagesMyasthenia Gravis: Submitted ToRomans 6:23No ratings yet
- 156 FullDocument7 pages156 FullDorotea ArlovNo ratings yet
- A Case ReportDocument8 pagesA Case ReportYosephine MulianaNo ratings yet
- CME Article 2010 JulyDocument10 pagesCME Article 2010 JulyIlda EscalanteNo ratings yet
- Myasthenia Gravis: Moderator: DR Anitha PG: DR VijethaDocument45 pagesMyasthenia Gravis: Moderator: DR Anitha PG: DR VijethaJerusha VijethaNo ratings yet
- Myastenia GrvaisDocument4 pagesMyastenia GrvaisteenaNo ratings yet
- Anaesthesia and Myasthenia GravisDocument12 pagesAnaesthesia and Myasthenia Gravis37435rlcNo ratings yet
- Myasthenia GravisDocument11 pagesMyasthenia GravisSandeepSethiNo ratings yet
- Myasthenia Gravis - A Review of Current TherapeutiDocument7 pagesMyasthenia Gravis - A Review of Current TherapeutiZainal AbidinNo ratings yet
- ShwetaDocument9 pagesShwetasagar KumarNo ratings yet
- NEJMra 1602678Document12 pagesNEJMra 1602678Olga Manco GuzmánNo ratings yet
- NMJ Disorders: For Clinical I StudentsDocument49 pagesNMJ Disorders: For Clinical I StudentsdenekeNo ratings yet
- Myasthenia GravisDocument32 pagesMyasthenia GravisSandhya HarbolaNo ratings yet
- Maddison 2006Document10 pagesMaddison 2006Mayara MoraisNo ratings yet
- Myasthenia Gravis: by Neha Mhapralkar MSCBT 12015Document20 pagesMyasthenia Gravis: by Neha Mhapralkar MSCBT 12015Neha MhapralkarNo ratings yet
- Locuri A 2-A Specialitate NOIEMBRIE 2023Document2 pagesLocuri A 2-A Specialitate NOIEMBRIE 2023Mirela CiobanescuNo ratings yet
- Quinlan 2006Document5 pagesQuinlan 2006Mirela CiobanescuNo ratings yet
- Mks 054Document7 pagesMks 054Mirela CiobanescuNo ratings yet
- Guidelines ProcessDocument3 pagesGuidelines ProcessMirela CiobanescuNo ratings yet
- MKN 051Document5 pagesMKN 051Mirela CiobanescuNo ratings yet
- Diagnostics: Acute Labyrinthitis Revealing COVID-19Document3 pagesDiagnostics: Acute Labyrinthitis Revealing COVID-19Mirela CiobanescuNo ratings yet
- Enter Patient Weight in KG: Anticonvulsant and CNS DrugsDocument1 pageEnter Patient Weight in KG: Anticonvulsant and CNS DrugsMirela CiobanescuNo ratings yet
- Pre Operative Fasting in Children A Guideline.2Document22 pagesPre Operative Fasting in Children A Guideline.2Yulieth VanessaNo ratings yet
- Euroanaesthesia 2022 Full Programme - DBD May22Document53 pagesEuroanaesthesia 2022 Full Programme - DBD May22Mirela CiobanescuNo ratings yet
- SodiumChloridesharedcare Guideline14Document2 pagesSodiumChloridesharedcare Guideline14Mirela CiobanescuNo ratings yet
- Diploma Guide - English 2019 ApprovedDocument11 pagesDiploma Guide - English 2019 ApprovedMinaz PatelNo ratings yet
- Noradrenaline Infusion Rate BSUH Critical CareDocument4 pagesNoradrenaline Infusion Rate BSUH Critical CareAndreiCostei100% (1)
- 2021 ESC Guidelines On Cardiac Pacing andDocument94 pages2021 ESC Guidelines On Cardiac Pacing andLeo Purba100% (1)
- Antibiotic Guidelines (2020) - 0Document55 pagesAntibiotic Guidelines (2020) - 0yudhit bessieNo ratings yet
- ESPEN Guideline On Clinical Nutrition in The Intensive Care UnitDocument32 pagesESPEN Guideline On Clinical Nutrition in The Intensive Care UnitDiana MonroyNo ratings yet
- Dannandd PhillllDocument1 pageDannandd PhillllMirela CiobanescuNo ratings yet
- MetamizoleDocument15 pagesMetamizoleFahri AnugrahNo ratings yet
- Reasons Why Phil Lester Is Phil BesterDocument1 pageReasons Why Phil Lester Is Phil BesterMirela CiobanescuNo ratings yet
- Nume: Varsta: Conditii de Viata Si Munca: Motivele InternariiDocument7 pagesNume: Varsta: Conditii de Viata Si Munca: Motivele InternariiMirela CiobanescuNo ratings yet
- BM Notes SeniorDocument393 pagesBM Notes SeniorShreya KishorNo ratings yet
- Chapter 27 Chest Injuries Final TermDocument4 pagesChapter 27 Chest Injuries Final Termluwi vitonNo ratings yet
- Health Talk On AnemiaDocument15 pagesHealth Talk On Anemiasimonjosan89% (63)
- Endoscopy For Upper and Lower Gastrointestinal Procedures Standard Operating Procedure UHL Gastroenterology LocSSIPDocument15 pagesEndoscopy For Upper and Lower Gastrointestinal Procedures Standard Operating Procedure UHL Gastroenterology LocSSIPIlu SinghNo ratings yet
- 10 Penyakit Terbanyak Di Rawat Jalan Di Puskesmas Provinsi Dki Jakarta TW I Tahun 2019Document9 pages10 Penyakit Terbanyak Di Rawat Jalan Di Puskesmas Provinsi Dki Jakarta TW I Tahun 2019Klinik pratama Iqra' medical centreNo ratings yet
- Osmosis 4Document1 pageOsmosis 4dysa ayu shalsabilaNo ratings yet
- Allopurinol (Drug Study)Document2 pagesAllopurinol (Drug Study)Daisy PalisocNo ratings yet
- Cholecystitis: By: Myla Rojas. BalandraDocument5 pagesCholecystitis: By: Myla Rojas. BalandraMyla Rojas BalandraNo ratings yet
- Sports Taping Techniques Expected OutcomesDocument5 pagesSports Taping Techniques Expected OutcomesMarc Angelo DareNo ratings yet
- PSW1365 Care of The Client With Dementia Assignment Revsion S2023Document11 pagesPSW1365 Care of The Client With Dementia Assignment Revsion S2023Odia OaikhenaNo ratings yet
- Sars-Cov-2 (Covid 19) Detection (Qualitative) by Real Time RT PCRDocument3 pagesSars-Cov-2 (Covid 19) Detection (Qualitative) by Real Time RT PCRShivam GarodiaNo ratings yet
- Majorsol CottonDocument5 pagesMajorsol CottonAries Agro LimitedNo ratings yet
- Anatomy and Physiology of The EyeDocument22 pagesAnatomy and Physiology of The EyeBalkos 61No ratings yet
- Contact Dermatitis BADDocument13 pagesContact Dermatitis BADDurgaMadhab TripathyNo ratings yet
- Chapter I 5Document51 pagesChapter I 5RamNo ratings yet
- Mathematical Modeling of COVID-19 Spreading With Asymptomatic Infected and Interacting PeoplesDocument23 pagesMathematical Modeling of COVID-19 Spreading With Asymptomatic Infected and Interacting PeoplesYjhvhgjvNo ratings yet
- Formative Test DMS 2021-2022Document37 pagesFormative Test DMS 2021-2022Lidwina ChandraNo ratings yet
- Myofascial and Endodontics. 2022Document15 pagesMyofascial and Endodontics. 2022David MonroyNo ratings yet
- Spinal Cord Injury: Barrios, Kevin George BDocument52 pagesSpinal Cord Injury: Barrios, Kevin George B乔治凯文No ratings yet
- AARC Clinical Practice Guideline - Management of Airway EmergenciesDocument7 pagesAARC Clinical Practice Guideline - Management of Airway EmergenciesdoterofthemosthighNo ratings yet
- COVID-19 Travel Recommendations by Destination - CDCDocument5 pagesCOVID-19 Travel Recommendations by Destination - CDCAli Ben HusseinNo ratings yet
- Implementation of New Safety Protocols of Calle Arco Restaurant in Pagsanjan, Laguna During Pandemic CrisisDocument42 pagesImplementation of New Safety Protocols of Calle Arco Restaurant in Pagsanjan, Laguna During Pandemic CrisisOliveros John Brian R.No ratings yet
- Pune CME 2011 BrochureDocument4 pagesPune CME 2011 BrochuredrpajaniNo ratings yet
- Endodontics Principles and Practice (139 279)Document141 pagesEndodontics Principles and Practice (139 279)Daniel Ricardo Moreno HernandezNo ratings yet
- Effect of Social Media Health Communication On Knowledge Attitude and Intention To Adopt Health-Enhancing BehavDocument170 pagesEffect of Social Media Health Communication On Knowledge Attitude and Intention To Adopt Health-Enhancing Behavchukwu solomonNo ratings yet
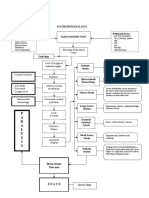
- Pathophysiology: P A R A L Y S I SDocument1 pagePathophysiology: P A R A L Y S I SJordan Garcia AguilarNo ratings yet
- Lower Limb BlocksDocument5 pagesLower Limb BlocksParvathy R NairNo ratings yet
- Bones and Joints Quiz Questions - Footprints-Science GCSE Science Animations and QuizzesDocument1 pageBones and Joints Quiz Questions - Footprints-Science GCSE Science Animations and Quizzescpcp6n7tc5No ratings yet
- Common River Medicinal Plant Handbook FINAL4Document40 pagesCommon River Medicinal Plant Handbook FINAL4Shime EthiopianNo ratings yet
- Cholinergic DrugsDocument22 pagesCholinergic Drugsmug ashNo ratings yet