0% found this document useful (0 votes)
2K views54 pagesSPINAL Anaesthesia
This document provides information on spinal anaesthesia including:
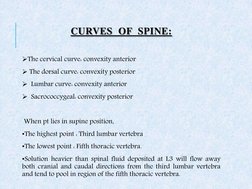
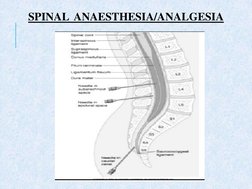
1. Spinal anaesthesia involves injecting local anaesthetic into the subarachnoid space to produce reversible sympathetic block. It is commonly performed at the L3-L4 vertebral level.
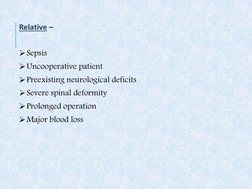
2. Indications include lower body and lower abdominal surgeries. Contraindications include infection, coagulopathy, and increased intracranial pressure.
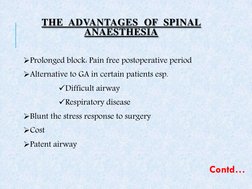
3. Advantages include prolonged postoperative pain relief, maintaining a patent airway, and reducing surgical stress response. Proper patient positioning, identification of anatomical landmarks, and choice of needle and local anaesthetic are important considerations for safe and effective spinal anaesthesia.
Uploaded by
darsh bhattiCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PDF, TXT or read online on Scribd
0% found this document useful (0 votes)
2K views54 pagesSPINAL Anaesthesia
This document provides information on spinal anaesthesia including:
1. Spinal anaesthesia involves injecting local anaesthetic into the subarachnoid space to produce reversible sympathetic block. It is commonly performed at the L3-L4 vertebral level.
2. Indications include lower body and lower abdominal surgeries. Contraindications include infection, coagulopathy, and increased intracranial pressure.
3. Advantages include prolonged postoperative pain relief, maintaining a patent airway, and reducing surgical stress response. Proper patient positioning, identification of anatomical landmarks, and choice of needle and local anaesthetic are important considerations for safe and effective spinal anaesthesia.
Uploaded by
darsh bhattiCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PDF, TXT or read online on Scribd
- Introduction to Spinal Anesthesia
- Indications and Contraindications
- Advantages of Spinal Anesthesia
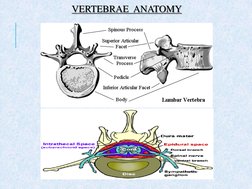
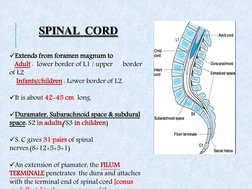
- Anatomy Relevant to Spinal Anesthesia
- Positioning for Spinal Anesthesia
- Spinal Anesthesia Approaches
- Technique and Tools for Lumbar Puncture
- Dermatomes and Effects
- Management and Complications
- Conclusion