Professional Documents
Culture Documents
Thoracic Surgery Outcomes For Patients With Coronavirus Disease 2019
Uploaded by
lutfor rahmanOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Thoracic Surgery Outcomes For Patients With Coronavirus Disease 2019
Uploaded by
lutfor rahmanCopyright:
Available Formats
Since January 2020 Elsevier has created a COVID-19 resource centre with
free information in English and Mandarin on the novel coronavirus COVID-
19. The COVID-19 resource centre is hosted on Elsevier Connect, the
company's public news and information website.
Elsevier hereby grants permission to make all its COVID-19-related
research that is available on the COVID-19 resource centre - including this
research content - immediately available in PubMed Central and other
publicly funded repositories, such as the WHO COVID database with rights
for unrestricted research re-use and analyses in any form or by any means
with acknowledgement of the original source. These permissions are
granted for free by Elsevier for as long as the COVID-19 resource centre
remains active.
Chang et al Thoracic
Thoracic surgery outcomes for patients with Coronavirus
Disease 2019
Stephanie H. Chang, MD,a David Chen, MD,a Darien Paone, MD,b Travis C. Geraci, MD,a
Joshua Scheinerman, MD,a Costas Bizekis, MD,a Michael Zervos, MD,a and Robert J. Cerfolio, MDa
ABSTRACT
Objective: As the Coronavirus Disease 2019 pandemic continues, appropriate man-
agement of thoracic complications from Coronavirus Disease 2019 needs to be
determined. Our objective is to evaluate which complications occurring in patients
with Coronavirus Disease 2019 require thoracic surgery and to report the early
outcomes.
Methods: This study is a single-institution retrospective case series at New York Pneumatocele requiring resection in a patient with
COVID-19.
University Langone Health Manhattan campus evaluating patients with confirmed
Coronavirus Disease 2019 infection who were hospitalized and required thoracic
CENTRAL MESSAGE
surgery from March 13 to July 18, 2020.
Patients with COVID-19 can
Results: From March 13 to August 8, 2020, 1954 patients were admitted to New
York University Langone Health for Coronavirus Disease 2019. Of these patients, develop complex unresolving
13 (0.7%) required thoracic surgery. Two patients (15%) required surgery for pneumothoraces, pneumato-
complicated pneumothoraces, 5 patients (38%) underwent pneumatocele resec- celes, empyemas, or hemo-
THOR
tion, 1 patient (8%) had an empyema requiring decortication, and 5 patients
(38%) developed a hemothorax that required surgery. Three patients (23%) thoraces that require thoracic
died after surgery, 9 patients (69%) were discharged, and 1 patient (8%) remains intervention, which can be safely
in the hospital. No healthcare providers were positive for Coronavirus Disease 2019 performed in selected patients.
after the surgeries.
Conclusions: Given the 77% survival, with a majority of patients already discharged PERSPECTIVE
from the hospital, thoracic surgery is feasible for the small percent of patients hos- We found that 0.7% of patients with COVID-19
pitalized with Coronavirus Disease 2019 who underwent surgery for complex pneu- admitted to the hospital developed complica-
tions requiring thoracic surgery. Of the 13 pa-
mothorax, pneumatocele, empyema, or hemothorax. Our experience also supports
tients, a majority (77%) had a minimally invasive
the safety of surgical intervention for healthcare providers who operate on patients
procedure, with 77% patient survival. Thoracic
with Coronavirus Disease 2019. (J Thorac Cardiovasc Surg 2021;-:1-11) surgery is feasible in select patients with COVID-
19. Earlier resection of pneumatoceles with air
leak also may improve patient outcomes.
See Commentary on page XXX.
The rapid spread of severe acute respiratory syndrome coro- early research shows that SARS-CoV-2 results in a number
navirus 2 (SARS-CoV-2) and the resultant Coronavirus Dis- of unique systemic and end-organ derangements,1-3 with a
ease 2019 (COVID-19) pandemic have brought incredible different phenotype than standard ARDS.4 The conse-
challenges in understanding how to best care for critically quences of this pathophysiology may lead to the increased
ill patients. Although other respiratory viruses can also pulmonary and thoracic complications requiring surgical
progress to acute respiratory distress syndrome (ARDS), intervention.
ARDS caused by COVID-19 often leads to a reduction in
lung compliance.4 Because of the high peak end-expiratory
From the aDivision of Thoracic Surgery, Department of Cardiothoracic Surgery, New pressure required to ventilate patients, as well as distinct
York University Langone Health, New York, NY; and bDepartment of General Sur-
pulmonary pathology,5 patients with COVID-19 have a
gery, New York University Langone Health, New York, NY.
Received for publication Sept 22, 2020; revisions received Jan 15, 2021; accepted for
publication Jan 17, 2021.
Address for reprints: Stephanie H. Chang, MD, Division of Thoracic Surgery, Depart- Scanning this QR code will take
ment of Cardiothoracic Surgery, New York University Langone Health, 530 First you to the table of contents to
Ave, Suite 9V, New York, NY 10016 (E-mail: stephanie.chang@nyulangone.org).
0022-5223/$36.00 access supplementary informa-
Copyright Ó 2021 by The American Association for Thoracic Surgery tion.
https://doi.org/10.1016/j.jtcvs.2021.01.069
The Journal of Thoracic and Cardiovascular Surgery c Volume -, Number - 1
Thoracic Chang et al
admission), and August 8, 2020. Data collection was performed on
September 8, 2020, to allow for 30-day follow-up. Patients were deemed
Abbreviations and Acronyms positive for COVID-19 by reverse transcriptase polymerase chain reaction
ARDS ¼ acute respiratory distress syndrome (rtPCR). Thoracic surgery was defined as any procedure performed in the
COVID-19 ¼ Coronavirus Disease 2019 operating room that involved the thoracic cavity, including pleural proced-
CT ¼ computed tomography ures and pulmonary resection. All patients with COVID-19 requiring
PPE ¼ personal protective equipment thoracic surgery were included. There were no exclusion criteria, although
each patient was assessed by a thoracic surgeon who determined the need
rtPCR ¼ reverse transcriptase polymerase for surgical intervention. The New York University Langone Health Insti-
chain reaction tutional Review Board approved this human subject study (Institutional Re-
SARS-CoV-2 ¼ severe acute respiratory syndrome view Board S20-00485), and data were collected from direct chart review.
coronavirus 2
VATS ¼ video-assisted thoracoscopic Indications for Surgery
surgery All patients with clinically significant pneumothoraces underwent tube
VV-ECMO ¼ veno-venous extracorporeal thoracostomy. Patients with a chest tube and nonresolving air leaks after
2 weeks who could not tolerate water seal underwent a chest computed to-
membrane oxygenation mography (CT) to further evaluate their pleural space and lung paren-
chyma, and ability to undergo thoracic surgery. Additionally, patients
with chest tubes and continued large pneumothorax were evaluated for sur-
gical management.
Patients who were febrile with a loculated empyema were evaluated for
empyema evacuation and decortication. All patients with a loculated hemo-
thorax that was still present after tube thoracostomy were evaluated for
higher incidence of barotrauma compared with patients possible hemothorax evacuation and decortication. Furthermore, all pa-
with ARDS due to other causes.6 Other patients with tients with worsening respiratory status or hypotension secondary to active
COVID-19 develop pneumatoceles,7 which are thin- bleeding or expanding pneumothorax despite chest tube placement were
THOR
walled, air-filled cysts in the lung parenchyma that are also taken to the operating room for management.
sequelae of pneumonia.8
Hypercoagulability is common in patients with COVID- Perioperative Care
19, with many patients expressing elevated D-dimer levels All operations were performed in negative pressure operating rooms. Per-
sonal protective equipment (PPE) in the operating room consisted of a hair
and sustaining a high incidence of arterial thrombosis, pul- cover, N95 mask, eye protection, nonsterile gown, and gloves throughout
monary embolism, and often mortality due to thromboem- the entirety of the procedure. During intubation, nonanesthesia personnel
bolic complications.1 Although guidelines regarding were asked to wait outside the operating room. Once the patient was intubated,
anticoagulation vary, the high rate of thrombosis has led bronchoscopy was performed, by the anesthesiologist or the surgical service if
to some critically ill patients with COVID-19 being placed needed, to position the double lumen tube. For hemodynamically unstable pa-
tients, the existing tracheostomy or single lumen tube was used for intraoper-
on therapeutic anticoagulation.9 Additionally, some pa- ative ventilation. Standard intraoperative sterile PPE with an N95 mask was
tients with COVID-19 may require further respiratory sup- used for the operation (Video 1). Thoracic surgery was performed by 1 of 4
port, such as veno-venous extracorporeal membrane thoracic surgeons, with the assistance of a cardiothoracic surgery resident. Pa-
oxygenation (VV-ECMO),10 which is another indication tients were readmitted to a dedicated COVID-19 intensive care unit
for anticoagulation. postoperatively.
The potential consequences of barotrauma, pneumato-
celes, and therapeutic anticoagulation are pulmonary or Outcomes
The primary outcome for this study is to report the incidence and
pleural complications that may require surgical intervention. describe the complications of COVID-19 that required thoracic surgery.
Little data are reported regarding the need for and efficacy of The secondary outcomes for this study are the early outcomes from the op-
thoracic surgery for sequelae of COVID-19. The primary erations and healthcare provider safety, defined as freedom from conver-
purpose of this study is to evaluate what complications sion from a negative to positive COVID-19 rtPCR test result. All
develop in patients with COVID-19 that require thoracic sur- healthcare providers were screened for COVID-19 symptoms (fever,
cough, shortness of breath, chills, myalgia, diarrhea, and headaches), and
gery at a tertiary hospital in New York City. We also will all underwent rtPCR testing on a monthly basis.
describe the operations performed and early outcomes for
these patients, and evaluate the safety of performing thoracic
surgery operations for healthcare providers. RESULTS
Patients Who Underwent Thoracic Surgery
From March 13, 2020, to July 18, 2020, 1899 patients with
MATERIALS AND METHODS a positive rtPCR test result for COVID-19 were admitted to
Study Design Manhattan Tisch Hospital. During this time period, 13 pa-
This study is a single-institution retrospective case series evaluating all
patients who were positive for COVID-19, who were admitted to the hos- tients (0.7%) who were hospitalized for COVID-19 under-
pital at New York University Langone Health Manhattan campus, and who went thoracic surgery. All 13 patients (100%) were male.
underwent thoracic surgery between March 13, 2020 (the time of first Patient characteristics are summarized in Table 1.
2 The Journal of Thoracic and Cardiovascular Surgery c - 2021
Chang et al Thoracic
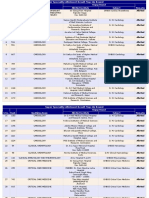
TABLE 1. Patient demographics
Patients with COVID-19
requiring thoracic surgery
Variable (n ¼ 13)
Gender, no. (%)
Male 13 (100)
Female 0 (0)
Age, median (IQR), y 46 (38-60)
2
BMI, median (IQR), kg/m 27 (25-29)
Comorbidities, no. (%)
Active malignancy 0 (0)
Asthma/COPD 0 (0)
Coronary artery disease 0 (0)
Diabetes 2 (15)
End-stage renal disease on dialysis 1 (8)
Hypertension 2 (15)
Known pulmonary embolism or deep 1 (8)
venous thrombosis
Right ventricular failure/pulmonary 1 (8)
hypertension
Stroke 2 (15)
Total with any comorbidity, no. (%) 4 (31)
THOR
Complication requiring surgery, no. (%)
Unresolving complex pneumothorax 2 (15)
Pneumatocele with ongoing air leak 5 (38)
Empyema 1 (8)
Hemothorax 5 (38)
COVID-19, Coronavirus Disease 2019; IQR, interquartile range; BMI, body mass in-
dex; COPD, chronic obstructive pulmonary disease.
pneumothoraces, which were evaluated with chest CT
(Figure 1). One patient underwent a robotic lysis of adhe-
sions and decortication, with a small wedge resection of
necrotic lung. The second patient underwent a video-
VIDEO 1. Demonstration of intraoperative PPE use. Operating room staff assisted thoracoscopic surgery (VATS) lysis of adhesions
wearing PPE during thoracic surgery in a patient with COVID-19. All non- with chest tube placements.
sterile personnel are wearing a gown, gloves, eye protection, N95, and hair Five patients (38%) underwent surgery for continued air
cover. All sterile personnel are wearing the standard sterile gown, sterile leak, with 1 or more pneumatoceles on chest CT (Figure 2).
gloves, eye protection, and hair cover, with the use of an N95 mask versus Of these 5 surgeries, 1 procedure (20%) was performed
a standard operating room mask. Video available at: https://www.jtcvs.org/ robotically, 3 procedures (60%) were performed via
article/S0022-5223(21)00168-9/fulltext. VATS, and 1 procedure (20%) was a thoracotomy. One pa-
tient had an unresolving recurrent pneumothorax who un-
Surgical Procedures derwent a robotic left lower lobe pneumatocele unroofing
Among 13 patients, 17 operations were performed. Two and decortication. The 3 VATS resections were also for un-
patients (15%) had multiple operations due to ongoing resolving recurrent pneumothoraces with active air leaks
bleeding. Of the 17 operations, 10 (61%) were performed and the presence of pneumatoceles on chest CT, with 1 pa-
in a minimally invasive fashion, which accounts for the op- tient undergoing a right VATS resection of blebs in all 3
erations in 10 (77%) of the 13 patients. Of the 3 patients lobes, 1 patient undergoing a right VATS upper lobe pneu-
who required thoracotomy, 2 underwent operation for motocele unroofing and decortication, and 2 patients under-
ongoing hemorrhage with hemodynamic instability and 1 going a left VATS pneumatocele resection and decortication.
had acute respiratory distress during induction (Table 2). The thoracotomy was performed for a patient with a large
Two patients (15%) required surgery for complicated loculated right pneumothorax with bilateral pneumatoceles
nonresolving pneumothoraces with ongoing air leak. Both and worsening hypoxia, hypercarbia, and hypotension
patients had multiple chest tube placements with continued despite right chest tubes who underwent decortication,
The Journal of Thoracic and Cardiovascular Surgery c Volume -, Number - 3
Thoracic Chang et al
TABLE 2. Patient-specific details regarding demographics, laboratory results, indications for surgery, surgical procedure, and outcomes
Age, Admit COVID-19 Respiratory status Date of
Patient y Gender Race BMI Comorbidities date treatments at surgery surgery Surgery Indication
1 60 M White 34 None 3/30/2020 Tocilizumab, On nasal cannula, 5/12/2020 Left robotic Multicystic lung disease,
sarilumab O2 sat 62% upon (HD 42) decortication, large pneumothorax
entering the OR lower lobe with worsening
wedge resection respiratory status
despite chest tube,
prior large effusion
2 52 M Asian 25 None 5/2/2020 Convalescent Intubated 5/21/2020 Right robotic Large loculated
plasma, (HD 19) decortication, hydropneumothorax,
tocilizumab lower lobe empyema
wedge resection
3 72 M White 27 Diabetes, 3/15/2020 Azithromycin/ Trached 6/3/2020 Right VATS Admission complicated
hypertension, plaquenil, (HD 78) hemothorax by pseudomonas pneumonia,
acute renal lopinavir/ evacuation, stroke, acute renal failure,
failure, stroke ritonavir, decortication, encephalopathy, hypoxic
steroids lower lobe arrest with post-CPR
wedge resection pneumothorax. He developed
an iatrogenic hemothorax
(10 3 12 cm) and was
taken to the OR.
4 35 M White 31 Pulmonary 4/4/2020 Tocilizumab, Trached, in extremis 6/1/2020 Left chest tube Recurrent right pneumothorax
hypertension, steroids (HD 57) for new left s/p 3 chest tubes, right upper
right ventricle pneumothorax, lobe endobronchial valve
failure right VATS placement, with acute
converted to decompensation on HD 57
thoracotomy with pCO2 170, tachycardia,
THOR
due to hypoxia, hypotension, and large
hemodynamic pneumothorax with transient
instability, improvement after needle
decortication, decompression, but still with
right upper lobe O2 sat 50%-70%
pneumatocele
resection,
pericardial
window
5 66 M Asian 29 Hypertension, 3/26/2020 Azithromycin/ room air 5/14/2020 Left VATS Chest x-ray done at rehabilitation
hyperlipidemia plaquenil, (HD 58) hemothorax showed left sided atelectasis,
hydroxychloroquine, evacuation, then CT with large hemothorax.
tocilizumab decortication Hemothorax incompletely drained
of left lower with pigtail catheter, taken to
lobe OR for washout.
6 65 M White 25 None 3/26/2020 Azithromycin/ Intubated 5/8/2020 Right VATS bleb Hypoxia with inability to
plaquenil, (HD 42) resections ventilate due to massive
tocilizumab from right alveolar pleural leak
upper, middle,
and lower lobes
7 60 M Asian 26 None 4/10/2020 Azithromycin/ On nasal cannula 5/18/2020 Left robotic Pneumothoraces unresolved
plaquenil O2 sat 62% upon (HD 37) decortication by prolonged
entering the OR of empyema, chest tube placement.
resection of
pneumatocele,
wedge resection
of consolidated/
diseased lung,
decortication
8 33 M Hispanic 30 None 3/26/2020 Azithromycin/ Trached, on VV-ECMO 4/29/2020 Right anterolateral Chest tube placement on
plaquenil, (HD 33) thoracotomy, anticoagulation for
nitrazoxanide hemothorax spontaneous pneumothorax,
evacuation, RLL followed by hemothorax
wedge resection with hemodynamic instability
3 2 for ruptured
hematoma,
chest packed
(Continued)
4 The Journal of Thoracic and Cardiovascular Surgery c - 2021
Chang et al Thoracic
TABLE 2. Continued
Age, Admit COVID-19 Respiratory status Date of
Patient y Gender Race BMI Comorbidities date treatments at surgery surgery Surgery Indication
9 31 M White 25 Diabetes 3/25/2020 Azithromycin/ Trached, on VV-ECMO 5/7/2020 Right VATS Persistent loculated pleural
plaquenil, (HD 42) with 5-cm effusion
nitazoxanide, anterolateral
tocilizumab thoracotomy,
evacuation
of loculated
right effusion,
partial
decortication
10 40 M Hispanic 29 Obesity, 4/5/2020 Azithromycin/ Trached, weaned 5/14/2020 Right VATS Incompletely drained
hyperlipidemia plaquenil, off VV-ECMO (HD 38) hemothorax right hemothorax
tocilizumab, evacuation, causing inadequate
remdesivir, decortication lung expansion
steroids of RUL,
RML, RLL
11 46 M Hispanic 25 Prior smoker 4/2/2020 Azithromycin/ Trached, on VV-ECMO 7/3/2020 Right VATS Bilateral blebs with
plaquenil, (HD 92) hemothorax pneumothoraces requiring
clazakizumab evacuation, chest tubes, development
RTC, steroids decortication, of right hemothorax
right upper
lobe blebectomy
12 43 M Hispanic 27 Active smoker 4/17/2020 Plaquenil, Trached, on VV-ECMO 7/7/2020 Left VATS Unable to wean VV-ECMO
tocilizumab, (HD 81) converted to support, large
remdesivir, axillary left pneumatocele/bleb
steroids thoracotomy,
THOR
decortication,
LUL and LLL
bleb resection
13 38 M White 24 None 3/30/2020 Azithromycin/ Trached, weaned 6/23/2020 Right VATS partial Persistent pneumomediastinum
plaquenil, off VV-ECMO (HD 86) lysis of after chest
possibly IL6RI/ adhesions and tube placement
sarilumab placement of 2
RCT, stem chest tubes,
cell infusion, trach exchange
IVIG, anakinra,
steroids
WBC: WBC: WBC: D-dimer: D-dimer: D-dimer: Necrotic Postoperative
Patient Admission Preoperative Postoperative Admission Preoperative Postoperative lung Pathology course Outcome
1 6.8 33 34.5 244 1256 831 Yes Extensive pulmonary Postoperative Discharged
arterial organizing air leak,
thrombi, pulmonary resolved
infarcts with necrosis within 1 wk
and abscess
formation and
reactive squamous
metaplasia. Scattered
fibrin thrombi in
parenchymal
arterioles/venules
2 13.1 27.6 29.1 187 2503 1122 Yes Pulmonary infarct and Cultures grew Discharged
abscess. Multiple Klebsiella
organizing pulmonary pneumonia
arterial thromboemboli.
Residual hyaline
membranes in the
infarct areas.
3 14.6 25.1 22.6 869 1033 1009 Yes Parenchymal abscess Progressive Dead
(HD 7) (6/1) with hematoma. pressor
Patchy end-stage requirement and
fibrosis with transition to
metaplasia. comfort care
on POD 2
(Continued)
The Journal of Thoracic and Cardiovascular Surgery c Volume -, Number - 5
Thoracic Chang et al
TABLE 2. Continued
WBC: WBC: WBC: D-dimer: D-dimer: D-dimer: Necrotic Postoperative
Patient Admission Preoperative Postoperative Admission Preoperative Postoperative lung Pathology course Outcome
4 9.6 9.2 Died 230 903 Died No None Continued Dead
postoperative
hypercarbia
and hypotension,
with comfort
care on POD 1
5 9.8 8.6 14.1 7824 1049 Not No None Admitted back to Discharged
(5/12) (5/12) checked rehabilitation
on POD 7
6 7.9 15.6 16.3 2226 437 549 Yes Organizing pneumonia. Ongoing leaks Dead
(cystic Organizing phase of from alveolar
lung diffuse alveolar pleural fistulas,
destruction) damage. Fibrous inability to
pleuritis. keep negative
suction on
chest tubes,
multisystem
organ failure,
distributive shock,
made hospice
7 9.4 6.1 10.3 693 Not Not No Organizing pneumonia Discharged with Discharged
checked checked with chronic chest tubes,
inflammation removed, then
THOR
reaccumulation
of pneumothorax.
Discharged again
with thopaz,
later removed.
8 9.6 7.9 18.7 645 6769 >10,000 Yes Hemorrhagic Taken back to OR Discharged
infarction with on POD1 for
cavities resulting ongoing
from ischemic hemorrhage,
necrosis of the underwent RLL
lung parenchyma lobectomy
and alveolar
hemorrhage
9 8.8 6.9 9.9 223 1680 2186 No None Taken back to OR Discharged
on POD 1 and
POD 2 for
retained
hemothorax
requiring chest
packing
10 10.6 7.5 12.9 450 1780 1427 None Chest tubes Discharged
removed by
POD 14
11 7.9 8.4 9.1 560 2041 663 Pulmonary bleb, Later developed a Discharged
thrombus, chronic large complex
pleuritis with left
granulation tissue multiloculated
pneumothorax,
multiple
pneumatoceles,
and alveolar
pleural fistula
requiring left
VATS
adhesiolysis.
Decannulated
from
VV-ECMO.
(Continued)
6 The Journal of Thoracic and Cardiovascular Surgery c - 2021
Chang et al Thoracic
TABLE 2. Continued
WBC: WBC: WBC: D-dimer: D-dimer: D-dimer: Necrotic Postoperative
Patient Admission Preoperative Postoperative Admission Preoperative Postoperative lung Pathology course Outcome
12 10.4 13.5 31.1 249 720 934 No Organizing diffuse Decannulated Alive, inpatient
alveolar damage from
with residual VV-ECMO,
hyaline membranes, left chest tube
pleuritis, and remains,
pneumatocele lined continues to
by inflammation require
including giant cells ventilation
support
13 8.4 16 15.8 508 938 852 No None Resolved Discharged
pneumothorax
with removal
of chest tube
and discharge
to rehabilitation.
BMI, Body mass index; COVID-19, Coronavirus Disease 2019; HD, hospital day; VATS, video-assisted thoracoscopic surgery; CPR, cardiopulmonary resuscitation; IVIG, intra-
venous immunoglobulin; OR, operating room; VV-ECMO, veno-venous extracorporeal membrane oxygenation; RUL, right upper lobe; RML, right middle lobe; RLL, right lower
lobe; LUL, left upper lobe; LLL, left lower lobe; RCT, randomized control trial; WBC, white blood cell count; POD, postoperative day.
unroofing of the pneumatocele, and pericardial window. Of the right lower lobe that was removed by a wedge resection.
note, 3 (60%) of the 5 patients were former smokers. One thoracotomy was a hemothorax evacuation for active
One patient (8%) had a multi-loculated right hydropneu- hemorrhage from the chest wall and diaphragm. The other
THOR
mothorax (Figure 3), concerning for empyema due to a was a hemothorax evacuation and right lower lobectomy
white blood cell count of 25,000 cells/mL, fever, and hypo- for an infarcted right lower lobe secondary to venous throm-
tension consistent with sepsis. A robotic right decortication bosis.11 All 5 patients were on therapeutic anticoagulation
was performed. The patient was also noted to have a before development of the hemothorax. Indications for ther-
partially necrotic right lower lobe adjacent to the inferior apeutic anticoagulation were presumed pulmonary embolus
pulmonary ligament, with resection of the necrotic area. in 1 patient, lacunar infarcts in 1 patient, elevated D-dimer
Operative cultures grew Klebsiella pneumonia. greater than 10,000k in 1 patient, and VV-ECMO in 2 pa-
Five patients (38%) developed a hemothorax that required tients. All patients on VV-ECMO were anticoagulated using
surgery (Figure 4). Three patients (60%) underwent VATS a heparin infusion, with a goal anti-factor Xa greater than
hemothorax evacuation, and 2 patients (40%) had a thora- 0.15 IU/mL and a partial thromboplastin time less than
cotomy secondary to ongoing hemorrhage. The VATS 70 seconds.12 Although 2 hemothoraces were spontaneous,
procedures were all hemothorax evacuations and decortica- 3 were postprocedural after tube thoracostomy in 2 patients
tions, with 1 of the patients having an area of necrosis in or after central line placement in 1 patient.
FIGURE 1. Chest CT of complex pneumothorax. Chest CT scan of a patient with COVID-19 with axial (left) and sagittal (right) views of a nonresolving
complex pneumothorax despite tube thoracostomy (not pictured in these images). This patient required surgical intervention.
The Journal of Thoracic and Cardiovascular Surgery c Volume -, Number - 7
Thoracic Chang et al
FIGURE 2. Chest CT of pneumatocele. Chest CT scan of a patient with COVID-19 with axial (left) and coronal (right) views of a pneumatocele in a patient
with a persistent active air leak. This patient required a surgical intervention for pneumatocele resection.
Evaluation of Patient Outcomes failure and new-onset liver failure leading to death
Among the 13 patients who underwent thoracic surgery, 9 postoperatively.
(69%) have been discharged from the hospital and are on
room air, 3 (23%) have died postoperatively, and 1 (8%) re- Healthcare Provider Safety
THOR
mains hospitalized (Figure 5). Patient characteristics and Four thoracic surgeons, 3 residents, and 2 thoracic anes-
outcomes for each COVID-19 complication requiring sur- thesiologists performed all thoracic surgeries in patients
gery are shown in Table 3. with COVID-19 during this time frame. One resident
The postoperative mortalities were due to respiratory tested positive for COVID-19 before the first thoracic sur-
failure in 2 patients and multisystem organ failure in 1 pa- gical case on a patient with COVID-19. The remaining 8
tient. Both patients with pneumatoceles who died postoper- healthcare providers have tested negative by COVID-19
atively had ongoing active air leaks after resection, with rtPCR testing on a monthly basis, and all remain antibody
worsening hypoxic and hypercarbic respiratory failure. negative. All healthcare providers were screened daily for
The patient who died after a hemothorax evacuation had symptoms, which would have required quarantine,
acute renal failure before surgery, with worsening renal although none developed any symptoms. No operating
FIGURE 3. Chest CT of loculated hydropneumothorax/empyema. Chest CT scan of a patient with COVID-19 with axial (left) and coronal (right) views of
the patient with a loculated hydro-pneumothorax, with a basilar chest tube (not pictured in these CT slices) in place. This patient had a leukocytosis with
concern for empyema, underwent a decortication, and grew Klebsiella pneumonia from the fluid collection.
8 The Journal of Thoracic and Cardiovascular Surgery c - 2021
Chang et al Thoracic
FIGURE 4. Chest CT of hemothorax. Chest CT scan of a patient with COVID-19 with axial (left) and coronal (right) views of a right hemothorax that
occurred after a right chest tube placement in a patient on therapeutic anticoagulation. Because of retained hemothorax, this patient was taken to the oper-
ating room for a hemothorax evacuation.
room staff contracted COVID-19 after a workplace empyema, and hemothorax. These patients were critically
exposure. ill with prolonged COVID-19 courses, with the median
date of surgery on hospital day 43 (interquartile range,
THOR
DISCUSSION 42-78). Despite a high mortality of intensive care unit pa-
This series demonstrates that only 0.7% of patients tients with COVID-19,13,14 a majority (69%) of the patients
admitted with COVID-19 required thoracic surgery. who were operated on have been discharged, with a current
Reasons for operative intervention included unresolving survival of 77%. Patients who died were high risk, with pro-
pneumothorax, pneumatocele with continued air leak, gressive respiratory distress leading to acute surgical
Thoracic Surgery Outcomes for Patients with
Coronavirus Disease 2019
1954 Patients Admitted for COVID-19
(March 13th-August 8th, 2020)
Methods
13 patients (0.7%) had thoracic surgery
2 complex 5 pneumatocele 1 empyema 5 hemothorax
pneumothorax
Results
77% patient survival
0% transmission of COVID-19 to providers
Implications Thoracic surgery for patients with COVID-19
is rare, but can be performed safely
FIGURE 5. Flowchart demonstrating the main findings of this study. Of the 1954 patients admitted during the study period for COVID-19, 13 (0.7%)
required thoracic surgery for the following indications: 2 pneumothoraces, 5 pneumatoceles, 1 empyema, and 5 hemothoraces; 77% of the patients survived,
with no transmission of COVID-19 to any providers. Although rare, thoracic surgery for complications associated with COVID-19 is feasible and safe for
patients and providers. COVID-19, Coronavirus Disease 2019.
The Journal of Thoracic and Cardiovascular Surgery c Volume -, Number - 9
Thoracic Chang et al
TABLE 3. Characteristics and outcomes of thoracic surgery for patients with Coronavirus Disease 2019
Variable Pneumothorax (n ¼ 2) Pneumatocele (n ¼ 5) Empyema (n ¼ 1) Hemothorax (n ¼ 5) All patients (n ¼ 13)
Hospital day of surgery, 63.5 (42-85) 57 (42-81) 19 43 (42-48) 43 (42-78)
median (IQR)
Postoperative length of stay, 33 (14-52) 5 (4-6) (n ¼ 3) 21 22 (8-34) 14 (5.5-28)
d, median (IQR)
Smoking history, no. (%) 0 (0) 3 (60) 0 (0) 1 (20) 4 (31)
Anticoagulation, no. (%) 1 (50) 1 (20) 1 (100) 5 (100) 8 (62)
Type of resection, no. (%)
Robotic 1 (50) 1 (20) 1 (100) 0 (0) 3 (23)
VATS 1 (50) 3 (60) 0 (0) 3 (60) 7 (54)
Thoracotomy 0 (0) 1 (60) 0 (0) 2 (40) 3 (23)
Necrotic lung present, no. (%) 1 (50) 0 (0) 1 (100) 2 (40) 4 (31)
Patient outcomes
Alive, discharged home 2 (100) 1 (40) 1 (100) 4 (80) 9 (69)
Alive, remains inpatient 0 (0) 1 (20) 0 (0) 0 (0) 1 (8)
Mortality 0 (0) 2 (40) 0 (0) 1 (20) 3 (23)
IQR, Interquartile range; VATS, video-assisted thoracoscopic surgery.
intervention or age more than 70 years with multiple comor- risk requiring intervention should be taken into consider-
bidities. Therefore, standard high-risk patients for thoracic ation when weighing the risks and benefits of therapeutic
THOR
procedures that may normally lead to a prolonged hospital anticoagulation.
course or other morbidity are more likely to result in death Regarding efficacy of surgery for bleeding, the only pa-
if they have concurrent COVID-19. tient in this group who died postoperatively was aged
Although individual case reports of pneumatoceles in more than 70 years, with acute renal failure, a stroke, and
COVID-19 have been described,15 this is the largest cohort cardiac arrest previously during his hospital stay. Because
with 5 patients requiring surgery. Most pneumatoceles are of the patient’s large hemothorax with inability to wean
described in children and frequently spontaneously resolve. from the ventilator, surgery was performed. However, given
For the patients described in this article, all 5 required sur- his age and comorbidities, the postoperative liver failure
gery for continued air leaks, with 4 patients in worsening and resultant mortality are likely due to patient-specific fac-
respiratory failure from difficulty ventilating. Because of tors. The remaining 4 patients (80%) have all been dis-
the existing poor ventilation, with fragile pulmonary paren- charged, indicating that surgery for bleeding in patients
chyma associated with pneumatoceles, 2 of the patients with COVID-19 is reasonable.
(40%) had progressive postoperative respiratory failure A secondary finding in this report is the rate of incidental
leading to death. Despite this high mortality rate, both of lobar and sub-lobar necrosis present in 31% of patients
those patients were in progressive respiratory distress that (n ¼ 4), although only 1 patient (7.7%) had complete lobar
would have resulted in death without surgical intervention. necrosis. Although hypercoagulability, with resultant
The other 2 patients with pneumatoceles and difficult venti- strokes16,17 and myocardial ischemia,18,19 has been
lation were on ECMO and have now been weaned off described in COVID-19, no such report exists for lung ne-
ECMO support. Notably, the patient with a pneumatocele crosis. Although 3 of the 4 patients were receiving therapeu-
with an air leak but no respiratory distress was discharged tic anticoagulation before surgery, pulmonary necrosis was
on postoperative day 5 and remains home on room air. present and necessitated resection, indicating a microvas-
Perhaps, for patients with COVID-19 complicated by pneu- cular disease process that may be refractory to anticoagula-
matoceles and an associated pneumothorax, more prompt tion. Pathology of autopsy specimens indicates that
surgical intervention, before worsening respiratory condi- microthrombus and large-vessel thrombus were present in
tion, is warranted. a cohort of patients with a median age of 73 years, and
Hemothoraces requiring surgical intervention occurred 60% of patients had more than 3 comorbidities,5 although
in 5 patients, all of whom were receiving therapeutic antico- the rate of anticoagulation in those patients was not re-
agulation. Although the rate of hemothorax requiring sur- ported. Additional pathologic evaluation of these resected
gery is unknown (the number of hospitalized patients on necrotic pulmonary specimens is necessary to further eluci-
therapeutic anticoagulation during this time is unavailable), date the mechanism of pulmonary injury in patients with
postprocedural hemothorax occurred in 3 patients and spon- COVID-19. Of note, no pulmonary necrosis was evident
taneous hemothorax occurred in 2 patients. This bleeding on preoperative imaging for any patient.
10 The Journal of Thoracic and Cardiovascular Surgery c - 2021
Chang et al Thoracic
Healthcare providers are also wary of performing References
thoracic surgery, particularly minimally invasive surgery 1. Al-Samkari H, Karp Leaf RS, Dzik WH, Carlson JCT, Fogerty AE, Waheed A,
et al. COVID-19 and coagulation: bleeding and thrombotic manifestations of
using insufflation, in patients with COVID-19 because of SARS-CoV-2 infection. Blood. 2020;136:489-500.
the risk of aerosolization and transmission of disease. 2. Bajwa H, Riaz Y, Ammar M, Farooq S, Yousaf A. The dilemma of renal involve-
Some surgeons have advocated the use of port-only access ment in COVID-19: a systematic review. Cureus. 2020;12:e8632.
3. Varga Z, Flammer AJ, Steiger P, Haberecker M, Angermatt R, Zinkernagel AS,
for minimally invasive procedures, as well as insufflation et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;
using continuous smoke/aerosol removal and filtration, 395:1417-8.
and minimizing instrumentation changes.20 For thoracot- 4. Marini JJ, Gattinoni L. Management of COVID-19 respiratory distress. JAMA.
2020;332:2329-30.
omy cases, a continuous-suction system with filtration is 5. Borczuk AC, Salvatore SP, Seshan SV, Patel SS, Bussel JB, Mostyka M, et al.
recommended.20 Additionally, transmission of virus from COVID-19 pulmonary pathology: a multi-institutional autopsy cohort from Italy
aerosolization from a chest drain with an air leak has been and New York City. Mod Pathol. 2020;33:2156-68.
6. McGuinness G, Zhan C, Rosenberg N, Azour L, Wickstrom M, Mason DM, et al.
anecdotally reported, with suggestions of placing a viral fil- High incidence of barotrauma in patients with COVID-19 infection on invasive me-
ter in the drainage system.21 However, for these 13 cases chanical ventilation [published online July 2, 2020]. Radiology. 2020;l297:E252-62.
that were performed at our institution, the only extra pre- 7. Shi H, Han X, Jiang N, Cao Y, Alwalid O, Gu J, et al. Radiologic findings from 81
patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lan-
cautions used were PPE with full gowns for all personnel cet Infect Dis. 2020;20:425-34.
in the room, N95 masks worn throughout the entire proced- 8. Tuddenham WJ. Glossary of terms for thoracic radiology: recommendations of
ure, and all operations performed in a negative pressure the Nomenclature Committee of the Fleischner Society. AJR Am J Roentgenol.
1984;143:509-17.
operating room. Standard postoperative chest tube manage- 9. Bikdeli B, Madhavan MV, Jimenez D, Chuich T, Dreyfus I, Driggin E, et al.
ment was performed without a viral filter, with no known COVID-19 and thrombotic of thromboembolic disease: implications for preven-
perioperative or postoperative transmission of the SARS- tion, antithrombotic therapy, and follow-up. J Am Coll Cardiol. 2020;75:2950-73.
10. Kon ZN, Smith DE, Chang SH, Goldenberg RM, Angel LF, Carillo JA, et al.
CoV-2 virus to any healthcare worker. Extracorporeal membrane oxygenation support in severe COVID-19. Ann
Thorac Surg. 2020;111:537-43.
THOR
Study Strengths and Limitations 11. Geraci TC, Narula N, Smith DE, Moreira AL, Kon ZN, Chang SH. Lobectomy
for hemorrhagic lobar infarction in a patient with COVID-19. Ann Thorac
The major strength of this series is that it is the largest Surg. 2020;111:e183-4.
case series to describe the complications of COVID-19 12. Arnouk S, Altshuler D, Lewis TC, Merchan C, Smith DE, Toy B, et al. Evaluation
that require thoracic surgical intervention and to report of anti-Xa and activated partial thromboplastin time monitoring of heparin in
adult patients receiving extracorporeal membrane oxygenation support. ASAIO
early outcomes. This report demonstrates the feasibility of J. 2020;66:300-6.
operating in patients with COVID-19 without transmission 13. Auld SC, Caridi-Scheible M, Blum JM, Robichaux C, Kraft C, Jacob JT, et al.
of the disease to healthcare workers. This study is limited ICU and ventilator mortality among critically ill adults with coronavirus disease
2019. Crit Care Med. 2020;48:e799-804.
because it is a single-institution retrospective analysis. 14. Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, Castelli A, et al.
Furthermore, data regarding the total number of patients Baseline characteristics and outcomes of 1591 patients infected with SARS-
who were evaluated for and declined for surgical interven- CoV-2 admitted to ICUS of the Lombardy region, Italy. JAMA. 2020;323:
1574-81.
tion are not available because of the retrospective nature of 15. Castiglioni M, Pelosi G, Meroni A, Tagliabue M, Uslenghi E, Salaris D, et al.
this study. Surgical resections of superinfected pneumatoceles in a COVID-19 patient.
Ann Thorac Surg. 2020;111:e23-5.
16. Merkler AE, Parikh NS, Mir S, Gupta A, Kamel H, Lin E, et al. Risk of ischemic
CONCLUSIONS stroke in patients with coronavirus disease 2019 (COVID-19) vs patients with
COVID-19 can lead to thoracic complications that influenza [published online July 2, 2020]. JAMA Neurol. 2020;77:1-7.
require surgical intervention. The indications for surgery 17. Qin C, Zhou L, Hu Z, Yang S, Zhang S, Chen M, et al. Clinical characteristics and
outcomes of COVI-19 patients with a history of stroke in Wuhan, China. Stroke.
at our institution were complex pneumothorax, pneumato- 2020;51:2219-23.
cele, empyema, or hemothorax. Given the good overall sur- 18. Shi S, Qin M, Shen B, Cai Y, Liu T, Yang F, et al. Association of cardiac injury
vival and lack of transmission of the SARS-CoV-2 virus to with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA
Cardiol. 2020;5:802-10.
health care providers, surgical intervention is feasible and 19. Guo T, Fan Y, Chen M, Wu X, Zhang L, He T, et al. Cardiovascular implications
safe for patients with COVID-19. of fatal outcomes of patients with Coronavirus Disease 2019 (COVID-19). JAMA
Cardiol. 2020;5:811-8.
20. Seco M, Wood J, Wilson MK. COVIDSafe thoracic surgery: minimizing intrao-
Conflict of Interest Statement perative exposure to the aerosols. JTCVS Tech. 2020;3:412-4.
The authors reported no conflicts of interest. 21. Internullo E, West D, Krishnadas R, Batchelor T, Saftic I. COVID-19: safe
The Journal policy requires editors and reviewers to thoracic surgery. Available at: https://www.ctsnet.org/article/COVID-19-safe-
thoracic-surgery. Accessed September 8, 2020.
disclose conflicts of interest and to decline handling or re-
viewing manuscripts for which they may have a conflict
Key Words: COVID-19, empyema, hemothorax, pneuma-
of interest. The editors and reviewers of this article have
tocele, pneumothorax
no conflicts of interest.
The Journal of Thoracic and Cardiovascular Surgery c Volume -, Number - 11
You might also like
- Jurnal 2Document8 pagesJurnal 2DelisQurrotaA'yunNo ratings yet
- Pneumothorax in COVID-19 Disease-Incidence and Clinical CharacteristicsDocument9 pagesPneumothorax in COVID-19 Disease-Incidence and Clinical CharacteristicsFolder PulmoNo ratings yet
- George - Acompanhamento pós-COVIDDocument8 pagesGeorge - Acompanhamento pós-COVIDMichelle TabletNo ratings yet
- Pneumothorax and Pneumomediastinum Among COVID-19 Patients With Mechanical Ventilation: A Case SeriesDocument8 pagesPneumothorax and Pneumomediastinum Among COVID-19 Patients With Mechanical Ventilation: A Case SeriesIJPHSNo ratings yet
- Aerosol-Generating Procedures inDocument5 pagesAerosol-Generating Procedures inHaris WidodoNo ratings yet
- J of Thrombosis Haemost - 2020 - Spyropoulos - Scientific and Standardization Committee Communication Clinical Guidance OnDocument7 pagesJ of Thrombosis Haemost - 2020 - Spyropoulos - Scientific and Standardization Committee Communication Clinical Guidance OnTaufiqurrokhman RofiiNo ratings yet
- High Incidence of Barotrauma in Patients With Severe Coronavirus Disease 2019Document9 pagesHigh Incidence of Barotrauma in Patients With Severe Coronavirus Disease 2019AMBUJ KUMAR SONINo ratings yet
- Surgery in Covid19 - 2Document4 pagesSurgery in Covid19 - 2Anonymous VV4iStxLNo ratings yet
- Clinical Microbiology and Infection: Research NoteDocument4 pagesClinical Microbiology and Infection: Research NoteNoorNo ratings yet
- RISK of Thromboembolism in Patient With Covid 19 MétaanalysisDocument14 pagesRISK of Thromboembolism in Patient With Covid 19 MétaanalysisDelgado OnthemixNo ratings yet
- Timing of Tracheostomy For Prolonged Respiratory Wean in Critically Ill Coronavirus Disease 2019 Patients A Machine Learning ApproachDocument9 pagesTiming of Tracheostomy For Prolonged Respiratory Wean in Critically Ill Coronavirus Disease 2019 Patients A Machine Learning ApproachDewa OkaNo ratings yet
- Point-of-Care Ultrasound For COVID-19 Pneumonia Patients in The ICUDocument9 pagesPoint-of-Care Ultrasound For COVID-19 Pneumonia Patients in The ICUEduardo RuizNo ratings yet
- Efficient GAN-based Chest Radiographs (CXR) Augmentation To Diagnose Coronavirus Disease PneumoniaDocument10 pagesEfficient GAN-based Chest Radiographs (CXR) Augmentation To Diagnose Coronavirus Disease PneumoniaRabah AlobaidyNo ratings yet
- Jurnal Deskriptif IngDocument6 pagesJurnal Deskriptif IngAulin putri damayantiNo ratings yet
- Systematic Review and Meta-Analysis of TracheostomyDocument12 pagesSystematic Review and Meta-Analysis of Tracheostomycelma44No ratings yet
- Pathophysiology Underlying Haigh Prevelanvce of DVTDocument8 pagesPathophysiology Underlying Haigh Prevelanvce of DVTZainab MotiwalaNo ratings yet
- Perfusie Afwijkingen in Covid 19 Patienten 1603707976Document10 pagesPerfusie Afwijkingen in Covid 19 Patienten 1603707976Muhammad Al-DulaimyNo ratings yet
- Utility of A Pulmonary Oedema Score For Predicting The Need For Mechanical Ventilation in COVID-19 Patients in A General HospitalDocument8 pagesUtility of A Pulmonary Oedema Score For Predicting The Need For Mechanical Ventilation in COVID-19 Patients in A General HospitalMax JaksicNo ratings yet
- Journal Reading Muhamad Fakhri PPDS JantungDocument24 pagesJournal Reading Muhamad Fakhri PPDS JantungLycka AkaishaNo ratings yet
- Management of Appendicitis During COVID-19: Short-Term OutcomesDocument5 pagesManagement of Appendicitis During COVID-19: Short-Term OutcomesJamila JuwitaNo ratings yet
- Management of Appendicitis During COVID-19 Pandemic Short-Term OutcomesDocument5 pagesManagement of Appendicitis During COVID-19 Pandemic Short-Term OutcomesLidiaNo ratings yet
- Covid and VTEDocument10 pagesCovid and VTExtineNo ratings yet
- Covid Long The LancetDocument2 pagesCovid Long The LancetAlexandra IonițăNo ratings yet
- Incidence of Deep Venous Thrombosis in Hospitalized COVID-19 Patients in Isolated de Martini Hospital Mogadishu SomaliaDocument8 pagesIncidence of Deep Venous Thrombosis in Hospitalized COVID-19 Patients in Isolated de Martini Hospital Mogadishu SomaliaInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Implementation of A Non-Invasive Oxygenation Support Strategy During The COVID-19 Pandemic in An Ephemeral Respiratory Intermediate Care UnitDocument3 pagesImplementation of A Non-Invasive Oxygenation Support Strategy During The COVID-19 Pandemic in An Ephemeral Respiratory Intermediate Care UnitJHNo ratings yet
- Treatment of Covid19 Patients at Intensive Care Unit of General Hospital of PrizrenDocument4 pagesTreatment of Covid19 Patients at Intensive Care Unit of General Hospital of PrizrenAnila CakeNo ratings yet
- Correlation Between Ground-Glass Opacity On Pulmonary CT and The Levels of Inflammatory CytokinesDocument7 pagesCorrelation Between Ground-Glass Opacity On Pulmonary CT and The Levels of Inflammatory CytokinesEarlya RifaniNo ratings yet
- Jurnal KLDocument4 pagesJurnal KLDiornald MogiNo ratings yet
- Time Course of Lung Changes at Chest CT During Recovery From Coronavirus Disease 2019 (COVID-19)Document7 pagesTime Course of Lung Changes at Chest CT During Recovery From Coronavirus Disease 2019 (COVID-19)Kykie KhongtokNo ratings yet
- Pathophysiological Patterns For TriagepdfDocument3 pagesPathophysiological Patterns For TriagepdfMayra VinuezaNo ratings yet
- Spontaneous Pneumomediastinum, Pneumothorax and Subcutaneous Emphysema in COVID-19 Patients-A Case SeriesDocument6 pagesSpontaneous Pneumomediastinum, Pneumothorax and Subcutaneous Emphysema in COVID-19 Patients-A Case SeriesPradnyaNo ratings yet
- Where Do We Stand With Antithrombotic Prophylaxis in Patients With COVID-19Document1 pageWhere Do We Stand With Antithrombotic Prophylaxis in Patients With COVID-19Shone DayNo ratings yet
- Management and Outcomes of Patients With STEMI During The COVID-19 Pandemic in ChinaDocument7 pagesManagement and Outcomes of Patients With STEMI During The COVID-19 Pandemic in ChinaMelinda AmelindaNo ratings yet
- Management and Outcomes of Patients With STEMI During The COVID-19 Pandemic in ChinaDocument7 pagesManagement and Outcomes of Patients With STEMI During The COVID-19 Pandemic in ChinaMelinda AmelindaNo ratings yet
- Journal ReadingDocument7 pagesJournal ReadingTheresa JulietNo ratings yet
- Computers in Biology and MedicineDocument11 pagesComputers in Biology and MedicineMuhammad Awais 1071-FET/BSME/F21No ratings yet
- PIIS0735675720303569Document3 pagesPIIS0735675720303569Dewianggreini DandaNo ratings yet
- Pneumothorax 2Document5 pagesPneumothorax 2maurelyaapwNo ratings yet
- Point of Care Chest Ultrasonography As A DiagnostiDocument5 pagesPoint of Care Chest Ultrasonography As A DiagnostiTari AudinaNo ratings yet
- Abdomen Quirurgico AgudoDocument7 pagesAbdomen Quirurgico AgudoJorge Luis Plasencia CubaNo ratings yet
- Resuscitation Plus: SciencedirectDocument7 pagesResuscitation Plus: SciencedirectSYARIFAH NURWAHDANINo ratings yet
- Asian Journal of AnesthesioloyDocument4 pagesAsian Journal of AnesthesioloyFitriani MadiNo ratings yet
- Venous Thromboembolism Complicated With COVID-19: What Do We Know So Far?Document8 pagesVenous Thromboembolism Complicated With COVID-19: What Do We Know So Far?anamad948No ratings yet
- Jurnal Hospital ManagementDocument10 pagesJurnal Hospital ManagementAzhari RachmanNo ratings yet
- Resuscitation: European Resuscitation Council COVID-19 Guidelines ExecutiveDocument11 pagesResuscitation: European Resuscitation Council COVID-19 Guidelines ExecutiveRicardo BarreraNo ratings yet
- Acute Pulmonary Embolism Associated With COVID-19 Pneumonia Detected With Pulmonary CT AngiographyDocument3 pagesAcute Pulmonary Embolism Associated With COVID-19 Pneumonia Detected With Pulmonary CT AngiographyAdriano OliveiraNo ratings yet
- المصريةDocument9 pagesالمصريةAbdelrahman ElrashidyNo ratings yet
- COVID Plasma ConvalescenteDocument11 pagesCOVID Plasma ConvalescenteBreno Bertozo SilvaNo ratings yet
- Engineering: Research Coronavirus Disease 2019-ArticleDocument8 pagesEngineering: Research Coronavirus Disease 2019-ArticleJackyNo ratings yet
- Rsna CovidDocument10 pagesRsna CovidcornealenutaNo ratings yet
- 7 Clinical Characteristics00196 FinalDocument9 pages7 Clinical Characteristics00196 FinalDarveen VijayanNo ratings yet
- Pulmonary Cavitation An Under-RecognizedDocument8 pagesPulmonary Cavitation An Under-RecognizedChavdarNo ratings yet
- Calon Jurnal Radio 1Document10 pagesCalon Jurnal Radio 1harryNo ratings yet
- Bronchoscopy in Critically Ill COVID-19 Patients - Findings, Microbiological Profile, and CoinfectionDocument5 pagesBronchoscopy in Critically Ill COVID-19 Patients - Findings, Microbiological Profile, and CoinfectionJeisson Osorio TrujilloNo ratings yet
- Coagulation Disorders in Coronavirus Infected PatientsDocument6 pagesCoagulation Disorders in Coronavirus Infected PatientsQuang TrầnNo ratings yet
- Clinical Characteristics of COVID-19 Complicated With Pleural EffusionDocument10 pagesClinical Characteristics of COVID-19 Complicated With Pleural EffusionInternal MedicineNo ratings yet
- ExperimentalDocument6 pagesExperimentalDiego TorresNo ratings yet
- The Egyptian Journal of Critical Care Medicine: Ahmed Abdelrazik Othman, Mohsen Salah AbdelazimDocument3 pagesThe Egyptian Journal of Critical Care Medicine: Ahmed Abdelrazik Othman, Mohsen Salah AbdelazimAquardoleo ValentinoNo ratings yet
- Surgery in Covid-19Document7 pagesSurgery in Covid-19Anonymous VV4iStxLNo ratings yet
- Cardiothoracic SurgeryDocument24 pagesCardiothoracic SurgeryMARTINNo ratings yet
- Shahrina Binti Shah Azam Khan Lab5 Q3Document1 pageShahrina Binti Shah Azam Khan Lab5 Q3Reena KhanNo ratings yet
- Hospitals and Diagnostic CentreDocument32 pagesHospitals and Diagnostic CentreMurmu BricksNo ratings yet
- Corey S. Scher Anna Clebone Sanford M. Miller J. David Roccaforte Levon M. Capan Eds. Youre Wrong Im Right - Dueling Authors Reexamine Classic Teachings in Anesthesia 2017 Springer InternationaDocument201 pagesCorey S. Scher Anna Clebone Sanford M. Miller J. David Roccaforte Levon M. Capan Eds. Youre Wrong Im Right - Dueling Authors Reexamine Classic Teachings in Anesthesia 2017 Springer InternationaThinh LeNo ratings yet
- HealthDocument21 pagesHealthLalita NaiduNo ratings yet
- SBRT Vs SurgeryDocument7 pagesSBRT Vs SurgerySandra SkaržinskaitėNo ratings yet
- The Tamil Nadu Dr. M.G.R. Medical University - MSC Nursing Second YrDocument10 pagesThe Tamil Nadu Dr. M.G.R. Medical University - MSC Nursing Second YrNoufal100% (1)
- Acute Stream Cardiorespiratory: Independent Learning PackageDocument50 pagesAcute Stream Cardiorespiratory: Independent Learning PackagePurvi PatelNo ratings yet
- Pictorial Consent in Cardiac SurgeryDocument4 pagesPictorial Consent in Cardiac SurgeryDebmalyaSahaNo ratings yet
- Nguyen (2021)Document11 pagesNguyen (2021)Stefanie MelisaNo ratings yet
- Hospital List District WiseDocument34 pagesHospital List District WiseArki100% (1)
- Abstract BookDocument170 pagesAbstract BookausterkoolNo ratings yet
- Aesculap Surgical Instruments: Cardiovascular and Thoracic Surgery Main CatalogDocument31 pagesAesculap Surgical Instruments: Cardiovascular and Thoracic Surgery Main Cataloginstrumed_globalNo ratings yet
- Regulations of The UEMS Board of Thoracic Surgery - January 2019Document5 pagesRegulations of The UEMS Board of Thoracic Surgery - January 2019Roxana Maria MunteanuNo ratings yet
- List of Empanelled (South)Document14 pagesList of Empanelled (South)Ilam BaruthiNo ratings yet
- Perioperative Care of Ectopia CordisDocument10 pagesPerioperative Care of Ectopia CordisAnne Reichel MinasNo ratings yet
- List of Empanelled Hospitals Updated 01032023Document24 pagesList of Empanelled Hospitals Updated 01032023ARIZ HAMIDNo ratings yet
- Mopup Round S.No. Rank Qualifying Exam Allotted Institute Subject RemarksDocument12 pagesMopup Round S.No. Rank Qualifying Exam Allotted Institute Subject RemarksDigvijay ChavanNo ratings yet
- 3 RD Year BSC NursingDocument67 pages3 RD Year BSC NursingSURAJ2792100% (1)
- Bala'sDocument20 pagesBala'sBalaMuruganNo ratings yet
- Sree Chitra Tirunal Institute Course CurriculumsDocument55 pagesSree Chitra Tirunal Institute Course Curriculumsfindingnemo667No ratings yet
- Untitled PDFDocument8 pagesUntitled PDFAndrei BriceagNo ratings yet
- New Latest List of Delhi Updated June 2020Document88 pagesNew Latest List of Delhi Updated June 2020Ashish Singh NegiNo ratings yet
- Sternotomi PDFDocument11 pagesSternotomi PDFHeri PrasetyoNo ratings yet
- FC Cardio(SA) Final Exam ReviewDocument4 pagesFC Cardio(SA) Final Exam ReviewmatentenNo ratings yet
- Physiotherapy For Cardio Respiratory Conditions: Q.P.CODE:1119-NSDocument22 pagesPhysiotherapy For Cardio Respiratory Conditions: Q.P.CODE:1119-NSSHAIK SHABEENANo ratings yet
- Cardiothoracic Surgeon Dr. Jennifer Hanna Now Seeing Patients at Cardiothoracic & Vascular Surgery Associates at HCA Healthcare/HealthONE's The Medical Center of AuroraDocument3 pagesCardiothoracic Surgeon Dr. Jennifer Hanna Now Seeing Patients at Cardiothoracic & Vascular Surgery Associates at HCA Healthcare/HealthONE's The Medical Center of AuroraPR.comNo ratings yet
- DNB 2017 Closing Ranks - UR - Round 3 - Col. CourseDocument79 pagesDNB 2017 Closing Ranks - UR - Round 3 - Col. Coursehakim shaikhNo ratings yet
- Thoracic SurgeryDocument33 pagesThoracic SurgeryChino Estoque FragataNo ratings yet
- Tissue Patch 3 Information For Distributors v1Document30 pagesTissue Patch 3 Information For Distributors v1malaramamurthyNo ratings yet