Professional Documents
Culture Documents
LDCU Neuro Rotation (Reading Assignments) Feb 1 - 15, 2022
Uploaded by
Jalanie AbubacarCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
LDCU Neuro Rotation (Reading Assignments) Feb 1 - 15, 2022
Uploaded by
Jalanie AbubacarCopyright:
Available Formats
LICEO DE CAGAYAN UNIVERSITY - COLLEGE OF MEDICINE
GROUP 4 ROTATORS
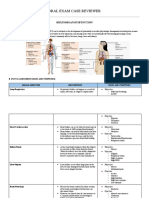
NEUROLOGY READING ASSIGNMENTS AND NOTES Subtypes of GBS:
FROM DR. SURDILLA
● GBS (Guillain-Barré Syndrome)
Definition:
○ Acute, frequently severe, and
fulminant polyradiculoneuropathy
that is autoimmune in nature
○ Occurs year-round at a rate of
between 1 and 4 cases per 100,000
annually
○ Males > Females
○ Adults > Children
Clinical Manifestation:
○ A rapidly evolving areflexic motor
paralysis
○ With or without sensory disturbance.
○ AscendingParalysis - Legs > Arms
○ Facial diparesis - 50%
○ Lower cranial nerves - bulbar Immunopathogenesis:
weakness ○ T cell activation - elevated levels of
○ 30% - ventilatory assistance cytokines and cytokine receptors are
○ Fever (-) at onset present in serum (interleukin [IL] 2,
○ DTR - attenuate or (-) soluble IL-2 receptor) and in
○ Cutaneous sensory deficit - usually
cerebrospinal fluid (CSF) (IL-6, tumor
relatively mild
○ Bladder Dysfunction - in severe cases necrosis factor a, interferon y)
but usually transient ○ complex glycosphingolipids that
○ Plateau - 4 weeks contain one or more sialic acid
○ Autonomic - BP, Cardiac Arrhythmia residues
○ Pain — deep aching, dysesthetic ■ cell-cell interactions
(including those between
Antecedent Events:
○ 1-3 weeks after infection axons and glia)
○ Vaccines ■ modulation of receptors
■ Respiratory or Gastrointestinal ■ regulation of growth
■ Campylobacter jejuni ○ AIDP - induction of tissue damage >
■ Human herpes virus early step: complement deposition
■ Mycoplasma pneumoniae along the outer surface of the
○ Lymphoma
Schwann cell.
○ HIV
○ SLE ○ AMAN/AMSAN - complement is
○ Zika virus deposited along with IgG at the nodes
of Ranvier along large motor axons
BY: BARODI, BUSCAINO, CHENG, JARIOL, NAMOCATCAT, SANGGACALA
LICEO DE CAGAYAN UNIVERSITY - COLLEGE OF MEDICINE
GROUP 4 ROTATORS
Laboratory Features: CIDP (Chronic Inflammatory Demyelinating
○ CSF FINDINGS Polyradiculoneuropathy)
■ Albuminocytologic
dissociation ○ CIDP is distinguished from GBS by its
■ Elevated protein (1-10 g/L chronic course.
[100 - 1000 mg/dL) ○ Onset is usually gradual over a few
months or longer, but in a few cases,
■ No pleocytosis
the initial attack is indistinguish- able
■ Normal if <48h from that of GBS.
○ ELECTRODIAGNOSTICS ○ An acute-onset form of CIDP may
■ Mild or absent in the early mimic GBS but should be considered if
stages it deteriorates >9 weeks after onset or
● Prolonged F wave relapses at least three times.
latencies ○ Most cases occur in adults, and males
● Prolonged distal are affected slightly more often than
latencies females. The incidence of CIDP is
● Reduced amplitude of lower than that of GBS, but due to the
compound muscle protracted course, the prevalence is
action potentials greater.
(CMAP) ○ Diagnosis
■ Later ■ The diagnosis rests on
● Slowing of conduction characteristic clinical, CSF, and
velocity electrophysiologic findings.
● Conduction Block The CSF is usually acellular
● Temporal dispersion with an elevated protein level,
Treatment: sometimes several times
○ Intravenous Immune Globulin (IVIg) normal.
■ Easy to administer; Safe; For ■ Biopsy typically reveals little
AMAN & MFS inflammation and onion-bulb
■ 5 daily infusions for a total changes these are the
dose of 2 g/kg body weight (imbricated layers of
○ Plasmapheresis attenuated Schwann cell
■ 40-50 mL/kg PE 4-5 times processes surrounding an
over 7 10 days axon) that result from recurrent
○ Critical Care demyelination and
■ Vital capacity remyelination
■ Heart rhythm ■ The response to therapy
■ Blood pressure suggests that CIDP is
■ Nutrition immune-mediated; this
■ DVT prophylaxis responds well to
■ Cardiovascular status glucocorticoids, whereas GBS
■ Early consideration of does not.
tracheotomy ○ Treatment
■ Chest physiotherapy ■ If mild, management can be
expectant, awaiting
spontaneous remission.
Prognosis: ■ Initial therapy is usually with
IVIg, administered as 2.0 g/kg
○ 85% - full functional recovery body weight given in divided
○ <5% - Mortality Rate doses over 2–5 days; three
■ Severe proximal and sensory monthly courses are generally
axonal damage recommended before
■ Advanced age concluding a patient is a
■ Fulminant or severe attack treatment failure
■ Delay in the onset of ■ PE, which appears to be as
treatment effective as IVIg, is initiated at
BY: BARODI, BUSCAINO, CHENG, JARIOL, NAMOCATCAT, SANGGACALA
LICEO DE CAGAYAN UNIVERSITY - COLLEGE OF MEDICINE
GROUP 4 ROTATORS
2-3 treatments per week for 6 ● Horner’s Syndrome
weeks; periodic re-treatment
may also be required.
■ Treatment with glucocorticoids
is another option (60–80 mg
prednisone PO daily for 1–2
months, followed by a gradual
dose reduction of 10 mg per
month as tolerated),
● Pupillary light reflex
Syndrome: Ptosis, miosis, anhidrosis
Affects 1 side of the face
Oculosympathetic lesion - caused by a lesion
anywhere along the sympathetic pathway that
supplies the head, neck and eyes
Affects 3 neuron arch:
○ 1st order Neuron- from hypothalamus
descends along the posterior lateral
The pupillary reflex pathway begins with brainstem then down into the spinal
retinal ganglion cells, which convey cord all the way to C8 to T2 level/
information from photoreceptors to the optic Ciliospinal center of budge
nerve (via the optic disc). ○ 2nd order Neuron - from the
sympathetic trunk thru brachial plexus
The optic nerve connects to the pretectal goes over the apex of the lungs then
nucleus of the upper midbrain, bypassing the ascend up the sympathetic chain then
lateral geniculate nucleus and the primary on to the superior cervical ganglion
visual cortex. roughly around the bifurcationof the
common carotid artery
From the pretectal nucleus, axons connect to ○ 3rd order Neuron -also called
neurons in the Edinger-Westphal nucleus, oculosympathetic fiber, ascends within
which supplies preganglionic parasympathetic the adventitia of the internal carotid
fibers to the eye, constricting the pupil, artery. Innervates iris dilator muscle
accommodating the lens, and convergence of and muller’s muscle.
the eyes. These fibers exit the midbrain with ■ Branches from the superior
CN III and synapse with postganglionic cervical ganglion - innervates
parasympathetic neurons of the ciliary sweat glands and vasodilation
ganglion, which innervates the sphincter Etiology:
muscle of the iris. Oculomotor nerve axons ○ 40% unknown
synapse on ciliary ganglion neurons. ○ Majority: 2nd order and 3rd order
neuron lesions
○ 1st order: hypothalamus (stroke,
tumor), brainstem (stroke (wallenberg
syndrome), tumor, demyelination),
BY: BARODI, BUSCAINO, CHENG, JARIOL, NAMOCATCAT, SANGGACALA
LICEO DE CAGAYAN UNIVERSITY - COLLEGE OF MEDICINE
GROUP 4 ROTATORS
spinal cord (tumor, myelitis, neuron to the effector
demyelination, spingomyalgia) muscle to perform a
○ 2nd order: Apical lung lesions movement.
(pancoast tumor, subclavian artery There are three broad types of lower motor
aneurysm, mediastinal masses) neurons:
○ 3rd order: Cavernous sinus (tumor, ○ somatic motor neurons- in the
thrombosis, carotid aneurysm, pituitary brainstem and further divide into three
tumor) categories: alpha, beta, and gamma
○ special visceral efferent (branchial)
● UMN vs LMN motor neurons- innervate extrafusal
muscle fibers and are the primary
Motor neurons (or motoneurons) comprise means of skeletal muscle contraction.
various tightly controlled, complex circuits ■ It innervates the muscles of
throughout the body that allows for both the head and neck that derive
voluntary and involuntary movements through from the branchial arches.
the innervation of effector muscles and glands. They are in the brainstem.
■ The branchial motor neurons
The upper and lower motor neurons form a and sensory neurons together
two-neuron circuit. form the nuclei of cranial
○ Upper motor neurons originate in the nerves V, VII, IX, X, and XI.
cerebral cortex and travel down to the ■ general visceral motor neurons
brainstem or spinal cord. It uses
glutamate. ● Hemorrhagic stroke vs Ischemic stroke
■ responsible for integrating all ○ A hemorrhagic stroke, or cerebral
of the excitatory and inhibitory hemorrhage, is a form of stroke that
signals from the cortex and occurs when a blood vessel in the
translating it into a signal that brain ruptures or bleeds.
will initiate or inhibit voluntary ■ Like ischemic strokes,
movement. hemorrhagic strokes interrupt
● The axons of the upper the brain's blood supply
motor neuron travel because the bleeding vessel
down through the can no longer carry the blood
posterior limb of the to its target tissue.
internal capsule. From ■ In addition, blood irritates brain
there, they continue tissue, disrupting the delicate
through the cerebral chemical balance, and, if the
peduncles in the bleeding continues, it can
midbrain, longitudinal cause increased intracranial
pontine fibers, and pressure which physically
eventually the impinges on brain tissue and
medullary pyramids. restricts blood flow into the
■ Lower motor neurons begin in brain.
the spinal cord and go on to ■ There are two types of
innervate muscles and glands hemorrhagic stroke:
throughout the body. It uses intracerebral hemorrhage, and
acetylcholine. subarachnoid hemorrhage.
● is responsible for
transmitting the signal
from the upper motor
BY: BARODI, BUSCAINO, CHENG, JARIOL, NAMOCATCAT, SANGGACALA
LICEO DE CAGAYAN UNIVERSITY - COLLEGE OF MEDICINE
GROUP 4 ROTATORS
Intracerebral Subarachnoid ● Cerebral amyloid
hemorrhage hemorrhage angiopathy
High blood pressure and Subarachnoid Intraventricular
aging blood vessels are hemorrhage is hemorrhage (IVH) can
the most common considered a stroke be:[6][7]
causes of intracerebral when it occurs
hemorrhage spontaneously (not Primary, confined to the
(intraparenchymal result from external ventricles
hemorrhage). forces and head trauma). Secondary, originating as
● Hypertensive A spontaneous an extension of an ICH
Intracerebral hemorrhage in the brain Most IVH is secondary
hemorrhage usually results from: and related to
(ICH) usually ● Sudden rupture hypertensive
results from of an aneurysm hemorrhages involving
spontaneous in an artery in the basal ganglia and
rupture of a the brain thalamus.
small artery ● Congenital
deep in the aneurysms
brain. ● Aneurysm Drugs that can cause ICH
● Circle of willis ● Methamphetamine
Anatomical locations (bifurcations) ● Phenylpropanolamine- sympathomimetic
● Secondary to ● Illicit drugs
The most common sites prolonged
include: hypertension
Trauma bleeding sites
● Basal ganglia (occurs when
(especially the an artery ● Superficial /base
putamen) branches in a AV malformation
● Thalamus weakened area ● parenchymal/superficial/around sylvian
● Cerebellum of artery's wall) fissure
● Pons ● Rupture of an Deep hematoma in elderly
The small arteries in abnormal ● Aneurysm
these areas seem more connection
● Amyloid angiopathy
sensitive to hypertension between
and as a result, it may arteries and
progress to vascular veins The symptoms of an ischemic stroke vary widely
injury. (arteriovenous depending on the site and blood supply of the area
malformation involved
If intracerebral AVM)
hemorrhage (ICH) occurs ● Inflamed artery
in other brain areas or in (Septic emboli)
non hypertensive travels to an
patients, the other artery that
causes of intracerebral supplies the
hemorrhage should be brain, and
considered such as: causes
inflammation
● Neoplasms and as a result
● Hemorrhagic the inflamed
disorders artery may
● Vascular weaken and
malformations rupture
● Arteriovenous
malformation
(AVM)
BY: BARODI, BUSCAINO, CHENG, JARIOL, NAMOCATCAT, SANGGACALA
LICEO DE CAGAYAN UNIVERSITY - COLLEGE OF MEDICINE
GROUP 4 ROTATORS
Bradykinesia or slowness of movement is one of the
three main signs of Parkinson’s, along with tremor
and rigidity (stiffness).
● Bradykinesia implies slowness in carrying out
(rather than initiating) movements, as well as
reduced amplitude of movement and
sequence effect. Up to 98% of all people with
Parkinson’s experience slowness of
movement.
Bradykinesia is one of the early signs of a movement
disorder such as Parkinson’s or parkinsonism and it is
caused by reduced levels of dopamine in the brain.
Medial Longitudinal Fasciculus - Six ocular motor
nuclei (pairs of cranial nerve III, IV, VI) are
interconnected via the MLF, which transmits vital
information for the purpose of coordinated and
synchronized movements of the eyes to a visual target
BY: BARODI, BUSCAINO, CHENG, JARIOL, NAMOCATCAT, SANGGACALA
LICEO DE CAGAYAN UNIVERSITY - COLLEGE OF MEDICINE
GROUP 4 ROTATORS
enhanced flow of Brisk osmotic this is not
H2O from tissues, diuresis → achievable by
including the hypovolemia other masses.
brain and CSF, and
into interstitial hypotension
fluid and plasma
As a result,
cerebral edema,
elevated ICP and
CSF volume and
pressure may be
reduced.
Primary
Increased
gradient across
BBB
Rapid reduction
of ICP
Duration of effect:
up to 6 hrs.
Secondary
Cerebral
vasoconstriction
Decreased blood
SAH management mnemonic: viscosity
Increased
cerebral blood
S - Sedation
flow
A - Analgesic
B - bed rest with head of bed at 30 degrees ASPIRIN
A - antiemetics
D - dexamethasone MECHANISMS EFFECT INDICATION
O - oxygenation
→ Blocks → Relieving → Secondary
prostaglandin pain. Reducing prevention of
● DRUGS USED IN NCCU synthesis pain thrombotic
○ Mannitol → Nonselective → Lowering cerebrovascul
○ Furosemide for COX-1 and inflammation ar disease
○ Acetazolamide COX-2 enzymes in higher doses
Inhibition of
platelet
MECHANISMS, EFFECT, INDICATION OF MANNITOL,
aggregation for
ASPIRIN AND DEXAMETHASONE about 7-10 days
→ Acetyl group
MANNITOL of aspirin binds
with a serine
MECHANISMS EFFECT INDICATION residue of COX-1
enzyme, leading
Osmotic diuretic Transient Reduction of to irreversible
elevates blood expansion of ICP and brain inhibition
plasma intravascular mass → Prevents
osmolality and volume Reduce IOP if production of
BY: BARODI, BUSCAINO, CHENG, JARIOL, NAMOCATCAT, SANGGACALA
LICEO DE CAGAYAN UNIVERSITY - COLLEGE OF MEDICINE
GROUP 4 ROTATORS
● Stroke
pain causing
prostaglandin.
→ Also, steps the Steps to diagnose Stroke
conversion of 1. CVD
arachidonic acid 2. Territory (MCA, PCA, ACA, ICA, Basillar,
to thromboxane Vertebral)
A2, which is a 3. Etiology/ Mechanism
potent inducer of
a. Hemorrhagic
platelet
aggregation b. Infarct
→ Result in clots i. Thrombose
and harmful 1. Athero
venous and 2. Embolic -
arterial thrombo- heart/cardioembolic,
embolism, lead to
carotid/artery to artery,
pulmonary
embolism/stroke pulmonary via fistula,
extremities/paradoxic
DEXAMETHASONE embolism
Risk factors:
MECHANISMS EFFECT INDICATION ○ Modifiable
■ Hypertension
→ Long acting →Persistent → Reduce
corticosteroid headache water content ● Primary Hypertension -
with minimal ➔ There and local no cause/etiology
sodium-retaining maybe tissue ● Secondary
potential. increasi pressure Hypertension - usually
→ Decreases ng in → subtly renal, cardiac,
inflammation by swelling increases endocrine, neurologic,
suppression of of the perfusion in
metabolic, or adrenal
neutrophil brain the
migration, edematous cause (e.g.
decreased brain. pheochromocytoma)
production of ■ Lifestyle
inflammatory ○ Non-modifiable - age, gender (<60
mediators; years old)
suppress normal
immune response
● FAST HUG BID - mnemonics for proper
Induce apoptosis
in multiple monitoring and management of stroke
myeloma cells. patients
F - feeding
A - analgesia
S - sedation
T - thromboembolism
H - head of bed 45 degrees angle
U - ulcer
G - glucose
B - bowel movement
I - indwelling catheter
D - descalation
BY: BARODI, BUSCAINO, CHENG, JARIOL, NAMOCATCAT, SANGGACALA
LICEO DE CAGAYAN UNIVERSITY - COLLEGE OF MEDICINE
GROUP 4 ROTATORS
● Indication for Extubation: ● Causes in comatose patients having
○ Spontaneous regular breathing decreased sensorium:
○ Sensorium/Consciousness ○ Hypoglycemia
○ Coughing reflex ○ Hypoxia
○ Hypercarbia > hypoventilation
● ESUS - Embolic stroke of undetermined ○ Brainstem location lesion
source
○ Embolic stroke of undetermined ● Metastatic bleeder to the brain:
source (ESUS) designates patients with ○ Lung cancer
non lacunar cryptogenic ischemic ○ Breast cancer
strokes in whom embolism is the likely ○ Choriocarcinoma
stroke mechanism. ○ Melanoma
○ It has been hypothesized that
anticoagulation is more efficacious ● Important Points:
than antiplatelet therapy for secondary ○ Strongest stimulus in GBS patients -
stroke prevention in ESUS patients. breathing exercise
○ ESUS comprises about 1 ischemic ○ R-L shunt of the heart - normally do
stroke in 6. Patients with ischemic not cross due to pressure gradient
stroke meeting criteria for ESUS were ○ To know if there’s opening of the heart
relatively young compared with other - inject air/saline and look for embolic
ischemic stroke subtypes and had, on phenomenon via transcranial doppler
average, minor strokes, consistent with ○ Pupils - note for size (3mm), reaction
small emboli. (brisk), shape (regular),
○ Retrospective methods of available accommodation (convergence)
studies limit confidence in stroke ○ Hypoglycemia - affects neurons
recurrence rates but support a ○ Glucose - substrate of energy in the
substantial (>4% per year) rate of stroke brain
recurrence during (mostly) antiplatelet ○ Hypoxia - neurons are mostly affected
therapy. in both brainstem and hemispheres
○ Hypoventilation
● Respiratory Distress in intubated patient: ■ Caused by CO2 retention,
○ Mucus plug in ETT vasodilation > increased blood
■ Bronchi location flow > edema
● Causes wheezing ■ Management: mannitol, head
● Chest X-Ray - elevation
atelectasis finding ■ Fastest mechanism is to
○ Furosemide overnight hyperventilate the patient
■ Pulmonary congestion > ● Signs: dyspnea,
causes left-sided heart failure carpopedal spasm,
■ Pulmonary hypertension tingling sensation.
○ Pulmonary edema - fruity, blood
tinged secretion ○ Cushing’s triad: late sign of increased
○ Asynchrony (awake but anxious intracranial pressure
patients) ■ Increased BP
■ Decreased HR
● Novel anticoagulants: ■ Change in respiration
○ Dabigatran - direct thrombin inhibitor
○ Rivaroxaban and Endoxaban - Factor
Xa inhibitors
BY: BARODI, BUSCAINO, CHENG, JARIOL, NAMOCATCAT, SANGGACALA
LICEO DE CAGAYAN UNIVERSITY - COLLEGE OF MEDICINE
GROUP 4 ROTATORS
○ Differential for patients having ○ CSF production - between 0.2 - 0.35
progressive weakness with no sensory ml/min, 288 ml/day
deficit ○ DVT prophylaxis
■ Myasthenia gravis ■ exercise/movement
■ Amyotrophic lateral sclerosis ■ Sequential compression
■ Chronic inflammatory stocking
demyelinating ○ Virchow’s triad:
polyradiculoneuropathy ■ Stasis
■ Myopathies ■ Hypercoagulability
■ Anterior horn cell disease ■ Endothelial damage
■ Lambert-Eaton myasthenic ○ Persistent hyperventilation - cerebral
syndrome vasoconstriction > ischemia
○ CN 3 palsy: ○ HICCUPS
■ Diaphragm innervated by CN
10 (intracranial, intrathoracic,
and intraabdominal in location)
○ CN 6 - longest nerve intracranially
○ Hyperdense on CT Brain:
■ Blood
■ Calcification - metastatic or
dystrophic
■ Bone
○ Central Nutrient of the nerves via
retrograde axonal transport
○ Cheyne-Stoke pattern:
○ Wound healing
■ Hyperpnea then apnea
■ Vitamin C
○ Brainstem lesion: Bilateral babinski,
■ Zinc
decreased sensorium
■ Proteins (0.2-1 g/kg)
■ Midbrain (pants/dorsal
○ Calories:
lithotomy position in CT scan) -
■ Fat - 9 g
CN 3, 4
■ Protein - 4 g
■ Pons (onion-bulb in CT scan) -
■ Carbohydrates - 4 g (60%) of
CN 6, 7, 8
the remaining --4g
■ Medulla - CN 9, 10, 12
○ AV malformation - “bag of worms”
○ Pupils in:
seen on MRI
■ Pontine lesion - pinpoint, small,
○ Cortical blindness - bioccipital infarct
2mm, brisk
○ Parietal Herniation - herniated to
■ Midbrain - 4-5 mm,
midbrain
sluggish/nonreactive
○ Cerebellar herniation - herniates to
○ Visual test in bedside - confrontation
medulla > causes respiratory arrest
test
○ Medial longitudinal fasciculus -
○ Weber Syndrome - CN 3 palsy and
connects 2 nuclei of midbrain and
hemiplegia
pons
○ Aqueduct of sylvius - connect 3rd and
○ Diabetes mellitus - risk for early
4th ventricle
atherosclerosis
○ Basilar artery - runs in the pons
■ Atherosclerosis - starts at
○ Vertebral artery - fused to become
young age, fibro-fatty streaks >
basilar artery, runs in the medulla
can ulcerate and trigger
clotting mechanism
BY: BARODI, BUSCAINO, CHENG, JARIOL, NAMOCATCAT, SANGGACALA
LICEO DE CAGAYAN UNIVERSITY - COLLEGE OF MEDICINE
GROUP 4 ROTATORS
○ Embolus > Hemorrhagic conversion by DENSE MCA sign -
1st week ● Early sign of stroke
■ Treat by anticoagulant
○ Strongest stimulus for ventilation -
PCO2
○ Tube ventriculostomy - drains CSF:
prevent hydrocephalus
○ Prolonged intubation > laryngeal
edema
■ Use steroids
○ Gaze center:
■ Brainstem
■ Cortex
○ External ventricular drainage
■ Infection: Staphylococcus > RTPA- can be given through
ventriculitis ● IV
■ Treatment: direct to ventricles ● Intraarterial
● Mechanical thrombectomy
○ Hemorrhagic cystitis Most common cause of parenchymal bleed
■ Hypotension after inserting ● Hypertension
catheter, with blood in urine ● Rupture of small penetrating arteries
○ Distal weakness - neuropathies Bleed in MRI brain in young patients:
○ Proximal weakness - myopathies ● Hypertensive bleed sites - basal ganglia
■ Exception: GBS (putamen), thalamus, pons, cerebellum
● Illicit drugs - methamphetamine,
Cuff - Deflate test: to watch out for phenyl-propanolamine
● Tidal volume - decreases after removing ET ● Trauma - superficial/base
due to air lek ● AV malformation - around sylvian fissure,
● Blood pressure parenchymal + superficial hemorrhage
● Respiration
Aneurysm:
Dominant hemisphere- LEFT ● Subarachnoid bleed
● Language area ● Bifurcation of major vessels (Circle of Willis)
● 95 % of right handed -Left hemisphere
dominant Deep hematomas in Elderly:
● 70% of left-handers also process language ● Aneurysm - subarachnoid
more in the left hemisphere. ● Amyloid angiopathy
BY: BARODI, BUSCAINO, CHENG, JARIOL, NAMOCATCAT, SANGGACALA
LICEO DE CAGAYAN UNIVERSITY - COLLEGE OF MEDICINE
GROUP 4 ROTATORS
CHARACTERISTICS OF THE PRINCIPAL TYPES OF Respiratory Center of the brain
CEREBRAL EDEMA
The respiratory center is composed of three distinct
FEATURE CYTO VASO INTERSTIT OSMOTIC
neuronal groups in the brain: the dorsal respiratory
TOXIC GENIC IAL EDEMA EDEMA group in the nucleus tractus solitarius, the ventral
EDEMA EDEMA
respiratory group in the medulla, and the pontine
Mechanism Failure of Breakdow Transepen The brain respiratory group in the pons. The latter is further
sodium n of dymal flow is classified into the pneumotaxic center and the
pump, blood-brai of water hyperosm
sodium n barrier and olar with
apneustic center.
and water with solutes respect to
enter cells increased into the plasma;
(neurons, vascular periventric water
glia) which permeabili ular moves
swell ty allowing extracellul along the
extracellul ar space osmotic
ar fluid gradient
accumulat
ion off an
ultrafiltrati
on of
plasma
Compositio Intracellul Ultrafiltrat Cerebrospi Water and
n of edema ar e of nal fluid sodium
fluid accumulat plasma
ion of
water and
sodium
Location of Predomina Predomina Periventric White
edema ntly gray ntly white ular white matter
matter matter matter
Etiology Ischemic Brain Hydroceph SIADH,
stroke, tumors alus hemodialy
anoxia, (primary sis,
exposure and excessive
to toxins, metastatic water
hepatic ), intake
encephalo meningitis,
pathy, brain
Reye’s abscess,
syndrome, encephalit
diabetic is,
coma ischemic
trauma stroke in
the late
stages,
trauma
Response Not Effective Effective Not
to Drug effective Effective
Therapy
BY: BARODI, BUSCAINO, CHENG, JARIOL, NAMOCATCAT, SANGGACALA
You might also like
- Nurse Practitioner Board ReviewFrom EverandNurse Practitioner Board ReviewRating: 5 out of 5 stars5/5 (1)
- Bells Palsy Nelsons TextBook of Pediatrics 20th EditionDocument3 pagesBells Palsy Nelsons TextBook of Pediatrics 20th EditionKRIZIA CORRINE CAINGCOY SAN PEDRONo ratings yet
- Neurology Summary FileDocument29 pagesNeurology Summary FileLaura A M MNo ratings yet
- Guillain - Barre Syndrome: Judi D. Segotier BSPT 3-BDocument8 pagesGuillain - Barre Syndrome: Judi D. Segotier BSPT 3-BsegotierjudiNo ratings yet
- Covid 19 NotesDocument4 pagesCovid 19 NotesJulius QuilapioNo ratings yet
- Rehabilitation Post StrokeDocument27 pagesRehabilitation Post StrokeNorNashiraMohdIbrahimNo ratings yet
- Spinal Cord Injury Lecture Notes Chapter 60Document7 pagesSpinal Cord Injury Lecture Notes Chapter 60Raina Ginella DsouzaNo ratings yet
- TBL - LeprosyDocument24 pagesTBL - Leprosychew weijianNo ratings yet
- Adrenal Gland OSCEDocument14 pagesAdrenal Gland OSCEOmar AttaNo ratings yet
- Medicine GBS: Guillain Barre SyndromeDocument4 pagesMedicine GBS: Guillain Barre SyndromedinakarNo ratings yet
- Guillain Barre SyndromeDocument16 pagesGuillain Barre SyndromeAgnes NesiaNo ratings yet
- MIS C Algorithim Version 2Document8 pagesMIS C Algorithim Version 2Saima UmairNo ratings yet
- Diara Jossiean M. Rogacion: Clinical Clerk 2020-2021 Group 5B Department of MedicineDocument19 pagesDiara Jossiean M. Rogacion: Clinical Clerk 2020-2021 Group 5B Department of MedicineJara RogacionNo ratings yet
- Guillane Barre SyndromeDocument8 pagesGuillane Barre SyndromeyasiraNo ratings yet
- GR4 HemoflagellatesDocument41 pagesGR4 HemoflagellatesEran Mark RojasNo ratings yet
- 9 1-SepsisDocument14 pages9 1-SepsisCHRISTIAN ASHLEY PASCUANo ratings yet
- GbsDocument28 pagesGbsYolanda YaoNo ratings yet
- Benign Febrile Seizure: PediatricsDocument2 pagesBenign Febrile Seizure: PediatricsKrista P. AguinaldoNo ratings yet
- Material, Vincent M. Drug Study - (Ceftriaxone and Salbutamol)Document6 pagesMaterial, Vincent M. Drug Study - (Ceftriaxone and Salbutamol)vincent materialNo ratings yet
- Icu AwDocument40 pagesIcu AwSiriporn PongpattarapakNo ratings yet
- PharmacologyDocument20 pagesPharmacologyJayla MarieNo ratings yet
- Overview and Treatment of Guillain-Barré Syndrome (GBS)Document9 pagesOverview and Treatment of Guillain-Barré Syndrome (GBS)anjelika100% (1)
- ComatoseDocument4 pagesComatoseBarii IkraamNo ratings yet
- Case Presentation Station 3B Drug Study ClinidineDocument6 pagesCase Presentation Station 3B Drug Study ClinidinehahahahaaaaaaaNo ratings yet
- Communicable Disease NursingDocument22 pagesCommunicable Disease NursingNur SanaaniNo ratings yet
- COVIDDocument16 pagesCOVIDanaNo ratings yet
- CANOMAD Responding To Weekly IV ImmunoglobulinDocument4 pagesCANOMAD Responding To Weekly IV ImmunoglobulindoctorebrahimNo ratings yet
- CCE1 AirwayDocument8 pagesCCE1 AirwayHoward ChangNo ratings yet
- Drugs For Angina Pectoris and Myocardial Infarction: OpioidDocument6 pagesDrugs For Angina Pectoris and Myocardial Infarction: OpioidApple MaeNo ratings yet
- Nursing Interventions Ii (N109/N124)Document12 pagesNursing Interventions Ii (N109/N124)Trisha Rimando ÜNo ratings yet
- Chapter 27 - Infectious DiseaseDocument8 pagesChapter 27 - Infectious DiseaseDrashtibahen PatelNo ratings yet
- Contoh Kasus MCTDDocument3 pagesContoh Kasus MCTDElva KadarhadiNo ratings yet
- Journal of The American Academy of Physician Assistants Volume 30 Issue 12 2017 (Doi 10.1097/01.JAA.0000526785.27024.Bb) Gelbart, David - TetanusDocument2 pagesJournal of The American Academy of Physician Assistants Volume 30 Issue 12 2017 (Doi 10.1097/01.JAA.0000526785.27024.Bb) Gelbart, David - TetanusPutri YunandaNo ratings yet
- CBD A Sick NeonateDocument36 pagesCBD A Sick NeonateAly MorsyNo ratings yet
- Ptosis Without Ophthalmoplegia: A Rare Manifestation of Guillain-Barré SyndromeDocument5 pagesPtosis Without Ophthalmoplegia: A Rare Manifestation of Guillain-Barré SyndromeMosNo ratings yet
- 00 Communicable DiseasesDocument8 pages00 Communicable DiseasesAngelica AlayonNo ratings yet
- Metronidazole Drug StudyDocument4 pagesMetronidazole Drug StudyJC LumayaNo ratings yet
- Agrawal2007 GBSDocument9 pagesAgrawal2007 GBSSimón Fuentes (STAHLGREIFER)No ratings yet
- Rapid Plasma Reagin SyphilisDocument24 pagesRapid Plasma Reagin SyphilisVia Gail CanlasNo ratings yet
- Granuloma Inguinale: Basic Information DiagnosisDocument2 pagesGranuloma Inguinale: Basic Information Diagnosiseibar camarenaNo ratings yet
- WEEK 2.2 - Mental DisordersDocument21 pagesWEEK 2.2 - Mental DisordersDump AccNo ratings yet
- Paraneoplastic Syndrome of CNSDocument71 pagesParaneoplastic Syndrome of CNSpreeti sharmaNo ratings yet
- Presentation On Guillain Barre Syndrome: Submitted To: Submitted byDocument12 pagesPresentation On Guillain Barre Syndrome: Submitted To: Submitted bypandem soniyaNo ratings yet
- Multiorgan DysfunctionDocument24 pagesMultiorgan DysfunctionJazzy Kathlene DumableNo ratings yet
- Guillain-Barre Syndrome: Presented by DR - Ruma Dey Dept. of KayachikitsaDocument33 pagesGuillain-Barre Syndrome: Presented by DR - Ruma Dey Dept. of KayachikitsaSushanta DasNo ratings yet
- ChancroidDocument2 pagesChancroidJoseLuisNo ratings yet
- Drug 1Document2 pagesDrug 1Butts McgeeNo ratings yet
- Male Breast Carcinoma: Yang Lu MS3 AUC School of MedicineDocument10 pagesMale Breast Carcinoma: Yang Lu MS3 AUC School of MedicineYang JunNo ratings yet
- Guillain-Barré Syndrome Med Student PresentationDocument16 pagesGuillain-Barré Syndrome Med Student PresentationRon ShenkarNo ratings yet
- GanciclovirDocument3 pagesGanciclovirRosher Deliman JanoyanNo ratings yet
- Filgastrim (GCSF)Document3 pagesFilgastrim (GCSF)Kyla Barrera TabungarNo ratings yet
- Neuro NotesDocument15 pagesNeuro NotesClyde CapapasNo ratings yet
- MS Lec IicpDocument4 pagesMS Lec IicpTrishia Camille GuillermoNo ratings yet
- Guillain-Barré Syndrome Pediatrico 2018Document4 pagesGuillain-Barré Syndrome Pediatrico 2018Mariam Plata100% (1)
- 3 PRIORITY NURSING CARE PLANS (Intrapartum and Postpartum Periods)Document11 pages3 PRIORITY NURSING CARE PLANS (Intrapartum and Postpartum Periods)Ryan Robert V. VentoleroNo ratings yet
- Drug StudyDocument30 pagesDrug StudyClaire MachicaNo ratings yet
- Cyto FinalsDocument36 pagesCyto FinalsjermieliamNo ratings yet
- CCU NCP Week 2Document4 pagesCCU NCP Week 2April Kate BanagodosNo ratings yet
- Guiilan Barre SyndromeDocument19 pagesGuiilan Barre SyndromeDhayaneeDruAinsleyIINo ratings yet
- 3939 - Update 2nd CNE 2017Document16 pages3939 - Update 2nd CNE 2017Virly EffendiNo ratings yet
- Handbook of Indexing Techniques A Guide For Beginn... - (Chapter 3 Writing The Index)Document16 pagesHandbook of Indexing Techniques A Guide For Beginn... - (Chapter 3 Writing The Index)joseph jaalaNo ratings yet
- R U-ChnDocument16 pagesR U-ChnRichelle RodrigoNo ratings yet
- 4 November 2004 DR - Supparearg DisayabutrDocument38 pages4 November 2004 DR - Supparearg DisayabutrDonnaya KrajangwittayaNo ratings yet
- American Stroke AssociationDocument1 pageAmerican Stroke AssociationritadoloksaribuNo ratings yet
- AC After StrokeDocument6 pagesAC After StrokeDileepa chathurangaNo ratings yet
- Natural Law Non-Voluntary Euthanasia and Public Policy - Am PDFDocument21 pagesNatural Law Non-Voluntary Euthanasia and Public Policy - Am PDFHubert SelormeyNo ratings yet
- MedicationReview PracticeGuide2011Document29 pagesMedicationReview PracticeGuide2011Yusnia Gulfa MaharaniNo ratings yet
- Vertebrobasilar Stroke - Overview of Vertebrobasilar Stroke, Anatomy of The Vertebral and Basilar Arteries, Pathophysiology of Vertebrobasilar StrokeDocument26 pagesVertebrobasilar Stroke - Overview of Vertebrobasilar Stroke, Anatomy of The Vertebral and Basilar Arteries, Pathophysiology of Vertebrobasilar StrokeLuis SilvaNo ratings yet
- Physical Therapy Leg Exercises For Stroke Patients - Flint RehabDocument16 pagesPhysical Therapy Leg Exercises For Stroke Patients - Flint RehabSabita SinghNo ratings yet
- Free Travel Guide PDFDocument7 pagesFree Travel Guide PDFFarhanjeeNo ratings yet
- Kunj Sakit MeiDocument178 pagesKunj Sakit MeiParnart ChristineNo ratings yet
- Stroke Patients - ReadingDocument24 pagesStroke Patients - ReadingSyed Suleman ShahNo ratings yet
- Aunali S Khaku, MD, Mba: Undergraduate: Lehigh University, (Aug 2003 - Apr 2005), BS Biology HighestDocument10 pagesAunali S Khaku, MD, Mba: Undergraduate: Lehigh University, (Aug 2003 - Apr 2005), BS Biology Highestask1288No ratings yet
- Qbase Medicine 1 MCQs For The MRCPDocument132 pagesQbase Medicine 1 MCQs For The MRCPsosoposo2100% (2)
- 13 JiggingDocument33 pages13 JiggingTapas DasNo ratings yet
- 50 Landmark Papers Every Vascular and Endovascular Surgeon Should KnowDocument283 pages50 Landmark Papers Every Vascular and Endovascular Surgeon Should KnowAhmed Elmallah100% (1)
- Siriraj Stroke ScoreDocument3 pagesSiriraj Stroke ScoreHendy SetiawanNo ratings yet
- Initial Assessment and Management of Acute Stroke - UpToDateDocument27 pagesInitial Assessment and Management of Acute Stroke - UpToDateDiego VillacisNo ratings yet
- Modified Rankin Scale How To PDFDocument15 pagesModified Rankin Scale How To PDFKNI Maret 2023No ratings yet
- AJH - Winter 2015Document52 pagesAJH - Winter 2015Sunand UnniNo ratings yet
- National Red Sock Day Declared For Peripheral Artery Disease AwarenessDocument4 pagesNational Red Sock Day Declared For Peripheral Artery Disease AwarenessPR.comNo ratings yet
- Pharmacology of Medical Cannabis - Ruhul AminDocument11 pagesPharmacology of Medical Cannabis - Ruhul AminjuciarampNo ratings yet
- (CLINPHAR) 2015 Clinical Practice Guidelines For The Management of Dyslipidemia in The Philippines - ExtractedDocument44 pages(CLINPHAR) 2015 Clinical Practice Guidelines For The Management of Dyslipidemia in The Philippines - ExtractedDenise Yanci DemiarNo ratings yet
- Dr. Andrew Moulden Interview - What You Were Never Told About VaccinesDocument16 pagesDr. Andrew Moulden Interview - What You Were Never Told About VaccinesTiffany Torres100% (1)
- Proiect Informatica Josanu RaduDocument5 pagesProiect Informatica Josanu RaduMihai VladNo ratings yet
- NASCETDocument9 pagesNASCETsirrfsNo ratings yet
- Hemorrhagic StrokeDocument31 pagesHemorrhagic StrokeKaren Mae Dacoco MamuyacNo ratings yet
- Medications Commonly Prescribed After A Stroke - GoodRxDocument11 pagesMedications Commonly Prescribed After A Stroke - GoodRxAnonymous EAPbx6No ratings yet
- Measuring The Difficulty Watching Video With HemianopiaDocument10 pagesMeasuring The Difficulty Watching Video With HemianopiaEvelin HarrizonNo ratings yet