Professional Documents
Culture Documents
107 Nicole
107 Nicole
Uploaded by
Ann Nicole BarreraOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
107 Nicole
107 Nicole
Uploaded by
Ann Nicole BarreraCopyright:
Available Formats
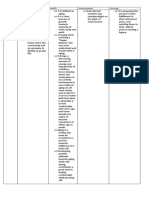
NCM 107 MATERNAL AND CHILD
HEALTH
Ovaries NURSING
old & male at 12-14 yrs old the hypothalamus serve as a
o Almond shaped gonad stat or regulation mechanism set to “turn on”
gonad functioning at this age
o Produce, mature and discharge ova
o Initiate and regulate menstrual cycle Reproductive Development
o 4 cm long, 2 cm in diameter, 1.5 cm thick ✓ Readiness for child bearing
o Produce estrogen and progesterone -begins during intrauterine life
Estrogen: -full functioning initiated at puberty
- promotes breast dev’t & pubic hair -the hypothalamus releases the GRF
which triggers the APG to form and
distribution prevents osteoporosis keeps release FSH and LH. (FSH & LH
cholesterol levels reduced & so limits initiates production of androgen and
effects of atherosclerosis estrogen --->2°
Fallopian tubes. Sexual characteristics
- Approximately 10 cm in length Conveys Role of Androgen
Androgenic hormones
ova from ovaries to the uterus Site of
- are produced by the testes, ovaries and
fertilization adrenal cortex which is responsible for:
Parts: interstitial muscular development physical growth inc.
isthmus – cut/sealed in BTL sebaceous gland secretions
ampulla – site of fertilization Testosterone
infundibulum – most distal segment; covered with - primary androgenic hormone
fimbria Related terms
a. Adrenarche – the development of pubic and axillary
Uterus hair (due to androgen stimulation)
- Hollow muscular pear shaped organ b. Thelarche – beginning of breast development
-uterine wall layers: endometrium; c. Menarche – first menstruation period in girls (early 9
myometrium; perimetrium y.o. or late 17 y.o.)
Organ of menstruation d. Tanner Staging
-It is a rating system for pubertal development
-receives the ova -It is the biologic marker of maturity
-Provide place for implantation & -It is based on the orderly progressive
nourishment during fetal growth development of: breasts and pubic hair in
-Protects growing fetus female’s genitalia and pubic hair in males
-Expels fetus at maturity Body Structures Involved
1 Hypothalamus
-Has 3 divisions: corpus – fundus , isthmus 2 Anterior Pituitary Gland
(most commonly cut during CS delivery) 3 Ovary
and cervix 4 Uterus
Uterine Wall
-Endometrial layer: formed by 2 layers of 4. Menstrual Cycle
cells which are as follows: -Female reproductive cycle wherein periodic uterine
bleeding occurs in response to cyclic hormonal changes
basal layer- -Allows for conception and implantation of a new life
- closest to the uterine wall -Its purpose it to bring an ovum to maturity; renew a
glandular layer uterine bed that will be responsive to the growth of a
- inner layer influenced by fertilized ovum
estrogen and progesterone; thickens and shed Menstrual Phases
• First: 4-5 days after the menstrual flow; the
off as menstrual flow endometrium is very thin, but begins to proliferate
-Myometrium rapidly; thickness increase by 8 folds under the influence
- composed of 3 interwoven layers of of increase in estrogenlevel also known as: proliferative;
smooth muscle; fibers are arranged in estrogenic; follicular and postmentrual phase
longitudinal; transverse and oblique • Secondary: after ovulation the corpus luteum produces
progesterone which causes the endometrium become
directions giving it extreme strength twisted in appearance and dilated; capillaries increase in
Vagina amount (becomes rich, velvety and spongy in
-Acts as organ of copulation appearance also known as: secretory;progestational;
-Conveys sperm to the cervix luteal and premenstrual
-Expands to serve as birth canal • Third: if no fertilization occurs; corpus luteum regresses
--Wall contains many folds or rugae making it after 8 – 10 days causing decrease in progesterone and
very elastic estrogen level leading to endometrial degeneration;
Fornices – capillaries rupture; endometrium sloughs off ; also
- uterine end of the vagina; serve as a place known as: ischemic
for pooling of semen following coitus • Final phase: end of the menstrual cycle; the first day
Bulbocavernosus – mark the beginning of a new cycle; discharges contains
- circular muscle act as a voluntary blood from ruptured capillaries, mucin from glands,
sphincter at the external opening to the vagina fragments of endometrial tissue and atrophied ovum.
(target of Kegel’s exercise)
II. PUBERTAL DEVELOPMENT
Puberty: the stage of life at which secondary sex
changes begins the development and maturation of
reproductive organs which occurs in female 10-13 years
Physiology of Menstruation folds
1. About day 14 an upsurge of LH occurs and the Artificial menopause / surgically induced menopause
Graafian follicle ruptures and the ovum a. oophorectomy or irradiation of ovaries
is released b. panhysterectomy
2. After release of ovum and fluid filled follicle cells
remain as an empty pit; FSH
decrease in Amount; LH increase continues to act on
follicle cells in ovary to produce III. PROMOTE RESPONSIBLE
lutein which is high in progesterone (yellow fluid) thus PARENTHOOD – FAMILY PLANNING
the name corpus luteum or A. Artificial Methods:
yellow body 1. physiologic method: oral contraceptives; natural
3. Corpus luteum persists for 16 – 20 weeks with methods
pregnancy but with no fertilization ovum 2. mechanical methods
atropies in 4 – 5 days, corpus luteum remains for 8 -10 3. chemical methods
days regresses and replaced by white 4. surgical methods
fibrous tissue, corpus albicans Oral contraceptive
Action:
Characteristics of Normal Menstruation Period inhibits release of FSH no ovulation
1. Menarche – average onset 12 -13 years Type:
2. Interval between cycles – average 28 days Combined ;
3. Cycles 23 – 35 days Sequential;
4. Duration – average 2 – 7 days; range 1 – 9 days Mini pill
5. Amount – average 30 – 80 ml ; heavy bleeding
saturates pad in <1hour Side Effects: due to estrogen and progesterone
6. Color – dark red; with blood; mucus; and endometrial > nausea and vomiting
cells > Headache and weight gain
> breast tenderness
Associated Terms > dizziness
1. Amenorrhea - temporary cessation of menstrual flow > breakthrough bleeding/spotting
2. Oligomenorrhea - markedly diminished menstrual flow > chloasma
3. Menorrhagia - excessive bleeding during regular Contraindications:
menstruation a. Breastfeeding
4. Metrorrhagia - bleeding at completely irregular b. Certain diseases:
Intervals o thromboembolism
5. Polymenorrhea - frequent menstruation occurring at o Diabetes Mellitus
intervals of less than 3 weeks o Liver disease
o migraine; epilepsy; varicosities
Ovulation o CA; renal disease;recent hepatitis
1. Occurs approximately the 14th day before the onset of c. Women who smoke more than 2 packs of cigarette
next cycle (2 weeks before) per day
2. If cycle is 20 days – 14 days before the next cycle is d. Strong family Hx of heart attack
the 6th day, so ovulation is day 6 Note: If taking pill is missed on schedule, take one as
3. If cycle is 44 days – 14 days, ovulation is day 30. soon as remembered and
4. Slight drop in BT (0.5 – 1.0 °F) just before day of take next pill on schedule; if not done withdrawal
ovulation due to low progesterone bleeding occurs.
level then rises 1°F on the day following ovulation
(spinnbarkheit; mittelschmerz) B. Natural Methods:
5. If fertilization occurs, ovum proceeds down the a. Rhythm/Calendar/Ogino Knause Formula
fallopian tube and implants on the o Couple abstains on days that the woman is fertile
endometrium o Menstrual cycles are observed and charted for 12
months
Menopause Standard Formula:
o Mechanism- a transitional phase (period of 1 – 2 first day of the beginning of one cycle to the first day of
years) called i macte ri c, heralds the next cycle
shortest cycle = minus 18
the onset of menopause.
longest cycle = minus 11
o Monthly menstrual period is less frequent, irregular
and with diminished amount. Example: shortest cycle = 28
o Period may be ovulatory or unovulatory - advised to longest cycle = 35
use Family planning method until Shortest cycle:
menses have 28 days – 18 = 10
Longest cycle:
been absent for 6 continuous months
o Menopause is has occurred if there had been no 35 days – 11 = 24
period for one year.
Fertile pd:
Classical signs: Vasomotor changes due to hormonal 10th to 24th day of cycle = No sexual intercourse
imbalance b. Billings Method / Cervical Mucus
o woman is fertile when cervical mucus is thin and
a. hot flushes
b. excessive sweating especially at night watery; may be extended
c. emotional changes o Sexual Intercourse may be resumed after 3 – 4 days
d. insomnia c. Symptothermal Method / BBT
e. headache
f. palpitations 1. Requires daily observation and recording of body
g. nervousness temperature before rising in
h. apprehension the
i. depression morning or doing any activity to detect time of ovulation
j. tendency to gain weight more rapidly 2. Ovulation is indicated by a slight drop of temperature
k. tendency to lose height because of osteoporosis and then rises
(dowager hump) 3. Resume Sexual intercourse after 3 – 4 days
l. arthralgias and muscle pains 4. Recommended observation of BBT is 6 menstrual
m. loss of skin elasticity and subcutaneous fat in labial cycle to establish pattern of
fluctuations
C. Mechanical Methods o Implantation is also called nidation, takes
1. Intrauterine Device - prevents implantation by place about a week after fertlization
non-specific cell C. Stages of human prenatal development
inflammatory reaction 1. Cytotrophoblast – inner layer
inserted during menstruation (cervix is dilated) 2. Syncytiotrophoblast – the outer layer
containing finger like projections called chorionic
SE: villi which differentiates into:
increased menstrual flow o angerhan’s layer – protective against
spotting or uterine cramps Treponema Pallidum, present only
increased risk of infection during the second trimester
Note: when pregnancy occurs, no need to remove IUD, o Syncytial Layer – gives rise to the fetal
will not harm membranes, amnion and chorion
fetus
2. Diaphragm D. Fetal Membranes
o disc that fits over the cervix of 1. Amnion – gives rise to umbilical cord/funis –
forms a barrier against the entrance of sperms with 2 arteries and 1 vein supported by
o initially inserted by the doctor 2. Wharton’s jelly
o maybe washed with soap and water is 3. Amniotic fluid: clear albuminous fluid, begins
reusable to form at 11 – 15th week of gestation, chiefly
o when used, must be kept in place because derived from maternal serum and fetal urine,
sperms remains viable for 6 hrs. in the urine is added by the 4th lunar month, near term
vagina but must be removed within 24 hours (to is clear, colorless, containing little white specks
decrease risk of of vernix caseosa, produced at rate of 500
toxic shock syndrome) ml/day. Known as BOW or Bag of Water
3. Condom
1. a rubber sheath where sperms are deposited E. Amniotic Fluid
2 .it lessens the chance of contracting STDs Purposes of Amniotic Fluid
3. most common complaint of users Protection – shield against pressure and
interrupts sexual act when to apply temperature changes. Can be used to diagnose
congenital abnormalities
D. Chemical Methods intrauterine– amniocentesis Aid in the descent of
These are spermicidals (kills sperms) like jellies, creams, fetus during active labor
foaming tablets, suppositories Implication:
E. Surgical Method F. Fetal Membranes
a. Tubal Ligation: •Chorion - together with the deciduas basalis
- Fallopian tubes are ligated to prevent gives rise to the placenta, start to form at 8th
passage of sperms Menstruation and week of gestation; develops 15 – 20 cotyledons
ovulation continue
b. Vasectomy: •Purpose of Placenta: respiratory; exchange of
- Vas deferens is tied and cut blocking the nutrients and oxygen
passage of sperms Sperm production •Renal system
continues Sperms in the cut vas •Gastrointestinal system
deferens remains viable for about 6 •Circulatory system
months hence couple needs to observe •Endocrine system: produces hormones (before
a form of contraception this time to 8th week-corpus luteum produces these
prevent pregnancy hormones) hCG keeps corpus luteum to
continue producing estrogen and progesterone
•HPL or human chorionic somatomammotropin
IV. BEGINNING OF PREGNANCY
which promotes growth of mammary glands for
A.Fertilization
lactation
1. Union of the ovum and spermatozoon
•Protective barrier: inhibits passage of some
2. Other terms: conception, impregnation or fecundation
bacteria and large molecules
3. Normal amount of semen/ejaculation= 3-5 cc = 1 tsp.
4. Number of sperms: 120-150 million/cc/ejaculation
5. Mature ovum may be fertilized for 12 –24 hrs after V. FETAL GROWTH AND DEVELOPMENT
Ovulation First lunar month
6. Sperms are capable of fertilizing even for 3 – 4 days •Germ layers differentiate by the 2nd week
after ejaculation (life 1. endoderm – gives rise to lining of GIT,
span of sperms 72 hrs) Respiratory Tract, tonsils, thyroid (for
basal metabolism), parathyroid (for
B.Implantation calcium metabolism), thymus gland (for
General Considerations: development of immunity), bladder and
o Once implantation has taken place, the uterine urethra
endometrium is now termed decidua 2. Mesoderm – forms into the supporting
o Occasionally, a small amount of vaginal structures of the body (connective
bleeding occurs with implantation due to tissues, cartilage, muscles and
breakage of capillaries tendons); heart, circulatory system,
o Immediately after fertilization, the fertilized blood cells, reproductive system,
ovum or zygote stays in the fallopian tube for 3 kidneys and ureters.
days, during which time rapid cell division 3. Ectoderm – responsible for the
(mitosis) is taking place. The developing cells formation of the nervous system, skin,
now called blastomere and when about to have hair and nails and the mucous
16 blastomere called morula. membrane of the anus and mouth
o Morula travels to uterus for another 3 – 4 days - 1 month: 2nd week – fetal membranes
o When there is already a cavity in the morula - 16th day – heart forms ; 4th week – heart beats
called blastocyt - 2nd month: All vital organs and sex organs formed;
o finger like projections called trophoblast form placental fully developed;
around the blastocyst, which implant on the -meconium formed (5th –8th wk)
uterus - 3rd month: Kidneys function - 12th wk- urine formed ;
Buds of milk teeth form ; begin bone ossification ; allows frequently due to hormonal changes
amniotic fluid ; establishment •Change in Sexual Desire – may increase or decrease
of feto-placental exchange needs correct interpretation… not
-4th month: Lanugo appears; buds of permanent teeth as a loss of interest in sexual partner
form; heart beat heard by fetoscope VIII. LOCAL CHANGES DURING
PREGNANCY
Focus of Fetal Development 1. Uterus – with increase to about 1000 grams at full
- First Trimester – period of term due to an increase in fibrous and elastic
organogenesis tissues
- Second Trimester – period of continued a. Becomes ovoid in shape
fetal growth and development; rapid b. Softening of lower uterine segment: Hegar’s
increase in length sign seen at 6th week
- Third Trimester – period of most rapid c. Operculum – mucus plug to seal out bacteria
growth and development because of the d. Goodell’s sign – cervix becomes vascular and
deposition of edematous giving it consistency of the earlobe
subcutaneous fat 2. Vagina – increased vascularity occurs
Assessing Fetal Well-being a. Chadwick’s sign – purplish discoloration of the
Fetal Movement: vagina
- Quickening at 18 – 20 weeks , peaks at b. Leukorrhea – increased amount of vaginal
29 -38 weeks Consistently felt until term discharges due to increased activity
a. Cardiff Method: a. Trichomonas – causes trichomonas vaginalis/vagnitis
“Count to ten” - records time interval it takes for 10 or trichomoniasis
- fetal movements to be felt usually occurs 4. Abdominal Wall
in 60minutes 1 Striae Gravidarum – due to rupture and
b. Contraction Stress Test: atrophy of connective tissue layers on the
Fetal Heart Rate (FHR) analyzed in conjunction with growing abdomen
contractions 2 Linea Nigra
Nipple stimulation done to induce gentle contractions 3 Umbilicus is pushed out
***3 contractions with 40 sec duration or more must 4 Melasma or Chloasma – increased
be present pigmentation due increased production of
in 10 minutes window melanocytes by the pitutitary
Normal Result no fetal decelerations with 5 Unduly activated sweat glands
contractions d. Ballotement – on 5th month
c. Non-stress Test: e. Pap Smear
Measures response of FHR to fetal movement (10- f. Pelvic measurements (done after 6th month or 2 wks
20mins.) before EDC)
with fetal movement FHR increase by 15 beats and
remain for 15 seconds then decrease to average rate a. Age of Gestation:
(no increase means poor oxygen perfusion to fetus) Nagele’s Rule: -3 calendar months and +7 days
d. Amniocentesis - done to determine fetal maturity:
Identify L/S ratio 2. FOUR P’S OF LABOR
16 wks – detect genetic disorder a. Power - the uterine contraction
30 wks – assess b. Passenger – the fetus
c. Passageway – the maternal pelvis
1. Prior to the procedure, bladder should be emptied; d. Psyche – the mental and emotional aspect of the
ultrasonography is used woman
to avoid
trauma from the needle to the placenta, fetus a. POWER -Uterine Contractions:
2. Complications include premature labor, infection, Rh a.1. Frequency – the beginning of one contraction to the
isoimmunization beginning of the next contraction
3. Monitor fetus electronically after procedure, monitor a.2. Interval – pattern which increases in frequency and
for uterine contractions duration
4. Teach client to report decreased fetal movement, a.3. Duration – the beginning of one contraction to the
contractions, or abdominal end of the same contraction
discomfort a.4. Intensity – strength of contraction, measured
after procedure. through a monitor or through touch of
a fingertip
a. Ultrasound – transducer on abdomen transmits sound on the fundus (mild, moderate or strong)
waves that show b. PASSENGER -Fe t us
fetal image on screen b.1. Fetal Skull:
b. Done as early as five weeks to confirm pregnancy,
gestational age Fetal Lie – relationship of the cephalocaudal axis of
c. Multiple purposes – to determine position, number, the fetus to the cephalocaudal axis of the mother.
measurement of fetus(es)
and other structures (placenta) PASSAGEWAY – maternal pelvis
d. Client must drink fluid prior to test to have full bladder
to assist in clarity of 3.PRELIMINARY/PRODROMAL SIGNS OF LABOR
image a. Lightening
e. No known harmful effects for fetus or mother b. Increased activity level- “nesting behavior”
f. Noninvasive procedure c. Loss of weight ( 2-3 lbs)
d. Braxton Hick’s Contractions
e. Cervical Changes – effacement
VII. COMMON EMOTIONAL RESPONSES - Goodell’s sign – ripening of the cervix
DURING PREGNANCY f. Increase in back discomfort
•Stress –decrease in responsibility taking is the reaction g. Bloody Show - pinkish vaginal discharge
to the stress of pregnancy not the h. Rupture of Membranes– labor expect in 24 hours
pregnancy itself affects decision making abilities i. Sudden burst of energy
•Couvade – syndrome – men experiencing j. Diarrhea
nausea/vomiting, backache due to stress, anxiety k. Regular Contractions - phases:
and empathy for partner increment,acme,decrement
•Emotional labile – mood changes/swings occur
- characteristics: intensity, frequency, interval,
Duration
.1. Analgesia – relieves pain and its perception
5.2. Anesthesia – produces local or general loss of
sensation ;
- usually regional anesthesia (e.g. spinal)
Demerol is most commonly used
Has sedative and antispasmodic effect
XIII. ASSOCIATED PROBLEMS
1. Engorgement
breast becomes full, tense and hot with throbbing
pain expected to occur on the 3rd post partum day
accompanied by fever (milk fever)last
for 240 due to increased lymphatic and venous
circulation
Nursing care:
o encourage breastfeeding
o advise use of firm-supportive brassiere
o (if not going to breastfeed – apply cold
compress; no massage; no breast pump; apply
breast binder)
2. Sore Nipples
Nursing care:
encourage to continue BF
expose nipples to air for 10 – 15 minutes after feeding
(alternative) exposure to 20 watt bulb placed 12 – 18
inches away promotes
vasodilation
and therefore promote healing
do not use plastic liners
use nipple shield
3. Mastitis -
inflammation of the breast
Signs & Symptoms: pain, swelling, redness, lumps in the
breasts, milk becomes
scanty
Nursing Care:
Ice compress
Supportive brassiere , empty breast with pump
Discontinue BF in affected breast
Apply warm dressing to increase drainage
Administer antibiotics as prescribed
*** Postpartum Check-up: 6th week postpartum to
assess involution
Method of delivery – preferably Vaginal but if not
possible CS
Prognosis: the danger of convulsions is present until 48
hrs postpartum
f. Cathartic – cause shift of fluid from the extra cellular
spaces into the
intestines from where the fluid can be excreted
Dosage:
DYSTOCIA - broad term for abnormal or difficult labor
and delivery
Uterine Inertia – sluggishness of contractions
Cause:
Inappropriate use of analgesics
Pelvic bone contraction
Poor fetal position
Overdistention – due to multiparity, multiple pregnancy,
polyhydrmanios or excessively large baby
Management: Stimulation of labor by oxytocin
administration or amniotomy
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5819)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (845)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Ethico-Legal Considerations in Nursing PracticeDocument3 pagesEthico-Legal Considerations in Nursing PracticeAnn Nicole BarreraNo ratings yet
- Leadership & ManagementDocument3 pagesLeadership & ManagementAnn Nicole BarreraNo ratings yet
- Ge 5 Module 3Document8 pagesGe 5 Module 3Ann Nicole BarreraNo ratings yet
- meTAPARADIGM OF LOCAL THEORIESDocument3 pagesmeTAPARADIGM OF LOCAL THEORIESAnn Nicole BarreraNo ratings yet
- Barrera Ann NicoleDocument7 pagesBarrera Ann NicoleAnn Nicole BarreraNo ratings yet
- Barrera, Ann Nicole S. BSN1-N InfographicDocument1 pageBarrera, Ann Nicole S. BSN1-N InfographicAnn Nicole BarreraNo ratings yet
- Exercise 3 - Gram StainingDocument3 pagesExercise 3 - Gram StainingAnn Nicole BarreraNo ratings yet
- Exercise 6 - Bacterial StructuresDocument4 pagesExercise 6 - Bacterial StructuresAnn Nicole BarreraNo ratings yet
- Exercise 5 - Sterilization and DisinfectionDocument6 pagesExercise 5 - Sterilization and DisinfectionAnn Nicole BarreraNo ratings yet
- For Activity Anthro Socio Pol SciDocument1 pageFor Activity Anthro Socio Pol SciAnn Nicole BarreraNo ratings yet
- MICRO1Document1 pageMICRO1Ann Nicole BarreraNo ratings yet
- NCM 103 Reviewer MidtermDocument7 pagesNCM 103 Reviewer MidtermAnn Nicole BarreraNo ratings yet
- Business: ProposalDocument19 pagesBusiness: ProposalAnn Nicole BarreraNo ratings yet