Professional Documents
Culture Documents
The Role of Dental Hygienists and Therapists in Paediatric Oral Healthcare in Scotland
Uploaded by
Harris SaeedCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
The Role of Dental Hygienists and Therapists in Paediatric Oral Healthcare in Scotland
Uploaded by
Harris SaeedCopyright:
Available Formats
RESEARCH
The role of dental hygienists and therapists in
paediatric oral healthcare in Scotland
Stephen Turner,*1 Praveena Symeonoglou2 and Margaret K. Ross3
Key points
Helps clarify the potential of Illustrates the commitment and Reflects respondents’ commonly held Identifies the barriers to the fuller
dental therapists and hygienists enthusiasm for greater involvement in view that a team approach is required, utilisation of hygienists’ and
for improving paediatric oral this challenging field. both with other dental professionals therapists’ skills, including financial
healthcare. and with parents and carers. and regulatory issues, and the
need for greater awareness on the
part of dentists and patients.
Abstract
Introduction The scope of practice of qualified dental hygienists and therapists allows them to undertake non-surgical
periodontal screening, treatment and preventive care, and to diagnose and treatment plan. Therapists are also
qualified to restore primary and secondary teeth, and to extract primary teeth. Both professions may see patients
directly without needing a dentist’s referral. In Scotland, they operate in a context of relatively poor but improving
child oral health.
Aim To investigate provision of dental care to children, including challenges encountered, by dental hygienists and
therapists in the Scottish General Dental Service (GDS).
Method An online survey of Scotland-based, GDC-registered dental hygienists and therapists in the GDS.
Results Of 426 potential respondents, 194 (46%) responded, including 113 hygienists. Thirty hygienists and six
therapists did not currently see child patients. Lack of referrals from dentists/specialisation by other team members,
financial/contract reasons and lack of demand were the reasons given. Of those who did see children, most were
therapists. Responsibility for preventive paediatric care was evenly split, with 71 (46%) citing the hygienist or therapist
and 69 (45%) the dentist. Sixty-five (43%) reported barriers, most commonly relating to parents and children
themselves. Time pressures, cost implications for practice and parents, and a number of practice and regulatory
barriers were also mentioned.
Discussion The response rate is considered to be very good. Limiting factors regarding provision of paediatric dental
care include lack of referrals from GDPs and financial or contractual issues.
Conclusion There appears to be considerable underuse of hygienists and therapists in respect to paediatric dental care.
Introduction a similar proportion to that recorded in Dental hygienists, as well as screening for oral
the eight NDIP surveys over the previous disease, are able to undertake all aspects of non-
Historically, paediatric dental health in 15 years.1 Children in the 2003 survey who surgical periodontal treatment and preventive
Scotland has been poor. According to the had experienced dental decay had an average care for patients of all ages, and to diagnose and
2003 National Dental Inspection Programme of five affected teeth. The Scottish Executive’s treatment plan. Dental hygienist-therapists are
(NDIP) report, 55% of Scottish primary response was to set up a programme to also qualified to provide all direct restorations
1 children had ‘obvious decay experience’, improve the oral health of children in Scotland, in the primary and secondary dentition and
and to reduce inequalities in dental health and to extract primary teeth within their scope of
1
Edinburgh Dental Institute, University of Edinburgh, access to services.2 The Childsmile programme practice. Since 2013, they have been able to
Lauriston Place, Edinburgh, EH3 9HA, UK; 2Department of began in 2006, although its geographical and see patients directly without a referral from a
Public Health, NHS Lanarkshire Headquarters, Kirklands,
Fallside Road, Bothwell, G71 8BB, UK; 3Retired Senior
functional roll-out was spread over a number dentist, following the conclusion of the 1993
Lecturer for Dental Care Professionals, Edinburgh Dental of years. By 2014, the proportion of five-year- Nuffield Report, Education and Training of
Institute, University of Edinburgh, Lauriston Place,
Edinburgh, EH3 9HA, UK.
old schoolchildren in Scotland with ‘obvious Personnel Auxiliary to Dentistry, that oral
*Correspondence to: Stephen Turner decay experience’ in their primary teeth had health needs of the population could be met by
Email address: s.turner@dundee.ac.uk
fallen to 32%. The mean number of affected a variety of professionals, including hygienists
Refereed Paper. teeth in these children was 4.0.3 The equivalent and therapists, each possessing specific skills.5,6
Accepted 9 June 2020 figures for England and Wales at that time were In 2015, the Scottish Dental Needs
https://doi.org/10.1038/s41415-020-1980-1
31% and 3.4 affected teeth.4 Assessment Programme (SDNAP) working
BRITISH DENTAL JOURNAL | ONLINE PUBLICATION | AUGUST 27 2020 1
© The Author(s), under exclusive licence to British Dental Association null
RESEARCH
group decided to review the current provision Dental Service, three in the Armed Forces No demand (6)
of dental care to children across Scotland and and one was undertaking full-time study. It is • ‘The children that attend the practice
identify gaps in the service, and to highlight likely that a number of non-respondents were generally are good with their [oral health]’
difficulties experienced by service providers similarly ineligible because they did not work in • ‘Fully private implant and periodontal care.
and patients. The aim of the current study was the GDS. The response of 194 from 426 eligible No child patients seen in the practice’
to investigate the experiences and perceptions clinicians represents 46%, and included 113 • ‘Hygienist appointments are private so very
of dental hygienists and therapists working (58%) hygienists, 78 (40%) hygienist-therapists rarely see children’.
within the Scottish General Dental Service and three (2%) singly qualified therapists.
(GDS) regarding the provision of dental care to Seventy-six (39%) also had other qualifications, When asked who undertook preventive
children and any challenges they encountered mostly in dental nursing. Eighty-two (43%) said care with children in their practice, 71 (46%)
in this work. A second SDNAP study, using they worked in all private or mostly private said the hygienist or therapist and 69 (45%)
the same methodology, was conducted in 2019 practices, 56 (28%) said their practices were said the dentist. With regards to restorative
and focused on the oral health of older people. 50/50 private and NHS, and 61 (31%) said their care, the figures were 56 (36%) and 96 (62%),
practices were mainly or all NHS. Thirteen (7%) respectively. The 158 (81%) who saw child
Method also worked in the community service, 11 (6%) patients were asked what types of treatment
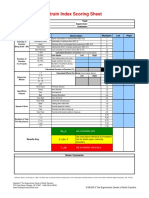
in hospital, four (2%) in the corporate sector they undertook with children. Figure 1
An online survey was conducted among and five (3%) in other settings. shows treatments within the clinical remit
Scotland-based, GDC-registered dental of both groups. Figure 2 shows treatments
hygienists and therapists employed in the GDS. Paediatric care within the clinical remit of dually qualified
The list of names, qualifications and e-mails of Thirty-six (19%) said they did not currently see hygienist-therapists only.
all GDC-registered dental care professionals was child patients – 30 hygienists and 6 therapists.
obtained from the GDC under strict conditions This difference was statistically significant Limitations on treatments undertaken
of confidentiality and use, detailed in a licensing (X2 = 13.95, p = 0.001). Of the 36, 32 explained Forty-seven (30%) said some procedures were
agreement signed 9 November 2015. The West why they did not see children. Their comments not referred to them even though they were
of Scotland Research Ethics Committee assessed fall into three categories; examples of each within their scope of practice. Treatments
the need for ethical approval for the overall are given. specified were: fissure sealant application
SDNAP review of children’s services, of which (15), fluoride varnish application (7),
the survey formed part. Their response was that Lack of referrals from dentists/specialisation radiographs (5), restorations (4), pulpotomies
NHS Research Ethics Committee approval was by other team members (19) (4), preformed metal crowns (3), extractions
not required as the project was considered to be • ‘I do not get referred them. One practice has (3), impressions (2), oral health instruction
service evaluation and not research. Would-be a dedicated children’s dentist’ (OHI) (2), and scaling and polishing (1). In
respondents were informed that any information • ‘Not referred any by employers. Very few addition, 10 (5%) said they themselves chose
they gave would remain confidential to the referred to me. Most patients I treat have not to undertake certain child treatments:
research team and that no individual or practice periodontal issues’ pulpotomies (4), restorations (2), whitening
would be identifiable in any report. • ‘I see patients privately and the principal (2), fissure sealants (1), and scale and polish
An initial screening e-mail asked if the treats children under 18 on the NHS. (1). Reasons why specific treatments were not
individual did not work in the GDS. The So, any perio/OHI/TBI [tooth brushing referred to them fall into six groups (Fig. 3).
survey then took place between 6 January and instruction]/diet advice is done by my
1 March 2016 using online survey software principal’ Financial reasons (11)
accessed through the University of Edinburgh. • ‘Rarely referred them we have a Childsmile • ‘Dentist diaries have sufficient space to not
Reminders were sent on 2 and 15 February nurse and the dentist do [sic] any work require these treatments to be carried out
2016. The results file was transferred to an needed to be carried out’. by myself routinely. As the dentists work as
SPSS v24 file for analysis, enabling comments associates they would prefer to claim the fee
to be sub-coded thematically and related Financial/contract reasons (7) for themselves’
to the qualification, background etc of the • ‘Mainly private practice. Dentist treat [sic] • ‘Probably because it takes time out my book
respondent. Responses by qualification as NHS patients and refer private patients to & dentist doesn’t get fee for it’
hygienist or therapist were tested using the hygienist’ • ‘Don’t think the dentists get a fee for
two-tailed chi-square test of significance, • ‘Dentist does not pass patients to me. She referring children to me so hardly see any
with p <0.05. Please see online supplementary doesn’t think therapists are properly trained now’
information for the full list of survey comments and passes a lot to VT dentist as doesn’t • ‘The dentists would rather I was doing
by question and response. have to pay me’ scalings to make the practice more money’.
• ‘I presume it’s due to costs. Seeing children
Results and paying a dental hygienist is not cost- Dentists’ preference (10)
effective for dentist. I am so disappointed • ‘Extractions are preferred by dentist [sic]
Twenty-five respondents indicated at the onset as trained on prevention of caries and perio in the practice’
that they did not work in the GDS: 15 worked disease but now only treat perio problems. • ‘Dentist tend to complete these treatments
in the community service; six in the Hospital Have not seen any children for [ages]’. themselves [sic]’
2 BRITISH DENTAL JOURNAL | ONLINE PUBLICATION | AUGUST 27 2020
© The Author(s), under exclusive licence to British Dental Association null
RESEARCH
• ‘Dentist doesn’t see the point of restoring
Fig. 1 Percentage of dental hygienists and therapists reporting routinely providing certain
treatments for child patients (n = 152) primary teeth’
• ‘The dentists aren’t good at referrals for
%
them so I generally only ask if I suspect
0 10 20 30 40 50 60 70 80 90 100
carious permanent teeth or missing
OHI permanent teeth which is rare’.
Fissure sealant application***
No nurse support/adequate equipment (3)
• ‘Dentists prefer [as initially didn’t have a
Scale and polish**
nurse]’
• ‘I don’t have a light for curing and my surgery
Dietary advice**
is not laid out in a way that I can do this
treatment myself as I work without a nurse’.
Fluoride varnish application***
Acclimatisation***
Other reasons (8)
• ‘Dentist’s referral is more targeted at
Infiltration analgesia*** restoring a cavity instead of alternative
treatments such as PMC [preformed metal
Caries risk assessment*** crowns]’
KEY: • ‘Possibly due to...relatively new to practice
Therapists (n=73)
Prescribe radiographs*** where I currently work 2 days (started
Hygienists (n=79)
3 weeks ago)’
** p<0.01 *** p<0.001
• ‘I see patients privately – do not see many
NHS patients’
Fig. 2 Percentage of therapists reporting routinely providing certain treatments for child • ‘Most parents opt for private composites.
patients (n = 73) All private cons [composites] carried out
% by dentists’
0 10 20 30 40 50 60 70 80 90 • ‘I am very busy and see very few children
the dentists have quieter books so undertake
Preventive resin restorations (secondary teeth)
preventative treatment themselves’.
Multi-surface restorations (primary teeth)
Single surface restorations (primary teeth) Barriers
Extractions (primary teeth) Sixty-five (43%) felt there were barriers to
Single surface restorations (secondary teeth) providing paediatric dental care. The most
commonly cited issues related to parents and
Multi-surface restorations (secondary teeth)
the child patients themselves. Time pressures
Amalgam restorations (secondary teeth)
and cost implications for practice and parents,
Pre-formed metal crowns (Hall technique)
and a number of practice and regulatory
Composite restorations (secondary teeth) barriers, were also mentioned (Fig. 4). Some
Composite restorations (primary teeth) gave more than one response.
Pre-formed metal crowns
Preventive resin restorations (primary teeth)
Patient/parent issues
Thirty-five cited patient/parent issues; these
Amalgam restorations (primary teeth)
comments have been broken down into the
Pulpotomies
following subheadings: parental attitudes,
lack of understanding/language skills, child
• ‘Dentist prefers to do themselves [sic]’ • ‘Dentist takes req radiographs’ reluctance, poor attendance and diet.
• ‘Sometimes they say it is to do with control • ‘The dentist claims acclimatisation in the
and knowing what the condition of the dentist’s surgery’ Parental attitudes (14)
cavity was before filling. Both terrible • ‘Childsmile dentist and nurse do this’. • ‘Parents trying to help but end up giving the
excuses’. wrong advice or info. Or frighten the child
Dentist unfamiliar with dental therapist’s with negative language and words like “jag”’
Convenience – eg done together with exam/ role (4) • ‘I work with a lot of foreign pts (Asian,
other treatment/by other clinicians (9) • ‘Dentists unaware of the scope of practice Polish) and their beliefs often make it
• ‘Dentist chooses to perform this procedure of a therapist’ difficult for me to treat them. Particularly
as majority are carried out at check-up appt • ‘I work with foreign dentists who haven’t those from Asian culture where males
with dentist’ used them’ “overrule” females thus treating young
BRITISH DENTAL JOURNAL | ONLINE PUBLICATION | AUGUST 27 2020 3
© The Author(s), under exclusive licence to British Dental Association null
RESEARCH
males with this outlook is difficult because
Fig. 3 Reasons given as to why treatments are not referred (n = 45)
they don’t listen and they don’t behave and
their mothers just stand and watch’
• ‘Little time for acclimatisation as I need to
meet daily financial targets. Parents often 8 Financial reasons
11
want all treatment carried out in 1–2 visits
which can be difficult when pt. is afraid/ Dentist preference
uncooperative/needs a lot of treatment’ 3
Convenience
• ‘Parents do not seem to realise/care that other
patients are waiting, when trying to coax their Dentist unfamiliar with DT's role
4
child into having treatment. Rather than allow
acclimatisation and make an appointment Lack of support, equipment
10
to come back they think it’s acceptable to
Other reasons
insist their child stays in the surgery until 9
they accept treatment. Parents often refuse
stainless steel crowns/LA [local anaesthetic]/
XLA [extraction under local anaesthetic]’.
Fig. 4 Barriers to paediatric dental care (n = 65)
Lack of understanding/language skills (5)
• ‘Parents’ involvement, education, 8
cooperation’
Parent and patient issues
• ‘Another issue this brings is that a lot of the
parents can’t speak English and rely on their
kids to translate. Trying to persuade a kid to 14 Time issues
tell his parents not to give him/her sweets 35
isn’t easy!’
Costs
Child reluctance (9)
• ‘Children are often very reluctant to have Practice/regulatory issues
treatment done based on fear and lack of 15
previous treatment experience. Therefore
often require extra acclimatisation’
• ‘Dentists often refer children to me for
treatment, and admit that due to lack of their children’s teeth have not been getting Costs to practice or parents (14)
cooperation they would not attempt to treat cleaned properly and parents can be slightly • ‘Sadly in practise [sic] the financial
the patient, and before I joined the practice defensive. I believe that social situations in implications of using the hygienist time
would refer the patient to community which children find themselves in such as is more weighted to paying adults. It is
and are therefore aware I’m unlikely to play time at school, birthday parties, peer more cost-effective to treat adults rather
successfully treat the patient’. pressure, sleepovers etc are also used as an than OHI, dietary advice for children. I
excuse to consume sugary products’. think the children are missing out. Cost
Poor attendance (6) and time are the 2 main barriers. Also the
• ‘High FTA [failure to attend] rates in NHS Time pressures (15) claiming system in no way recognises any
practices’ • ‘Within a 15min appointment it’s difficult of our work, no codes for OHI unless 3
• ‘Parents’ willingness to...bring them to to disclose/scale and polish and OHI in visits are undertaken, no code for S/P [scale
appointments’ that time’ and polish] for kids this would make a big
• ‘Parents fail to take them for appointment’ • ‘Time in practice for acclimatisation. Too difference if the work we do can be claimed
• ‘I deal with a lot of parents that only care much time spent on treating probs rather for kids’
about getting their kids out of pain. Thus than prevention’ • ‘Sometimes not having enough time/visits
FTA [failure to attend] future appts for • ‘Books are full for approx. 3–4 months for acclimatisation can bring on a barrier as
prevention/fills on asymptomatic teeth’. ahead. Dentists will not refer patients it’s not cost-effective to bring children in for
for Childsmile as they would not get any visits when no treatment can be claimed’
Diet (3) payments if I carried it out’ • ‘Prescriptions for Duraphat both t paste
• ‘Management of the parent, lack of • ‘In most of my practices time is so booked and varnish as per SDCEP. NHS no fee for
knowledge of what child eats outwith the up with hygiene that it is quicker for the prevention’
home or with other parents/grandparents’ child to be booked in with the dentist. In • ‘Commercial viability. No fee given for this
• ‘In my personal experience, it can be quite 1 of my practices it’s not so much of an issue which means OHI has to be given during tx
difficult for some parents to hear that as there is another hygienist’. [treatment] appt, and not given separately.
4 BRITISH DENTAL JOURNAL | ONLINE PUBLICATION | AUGUST 27 2020
© The Author(s), under exclusive licence to British Dental Association null
RESEARCH
If I could have separate appt I could focus in a different order to what I would like • ‘To be able to treat patients needs that is,
more directly on this subject only’. (for example, long appt for asymptomatic missing filling without having to reappoint
fills before fissure sealants etc). It would for a treatment plan’
Practice and regulatory barriers (8) also allow me to maintain my knowledge • ‘Would allow clinicians to diagnose and
• ‘The final barrier may be that dentists are of diagnosing/tx [treatment] planning plan their own treatment as they see best
concerned about job security since the as I graduated 2 years ago and fear my for the patient’
advent of direct access...certainly it has confidence will deteriorate and it will • ‘Able to see patients directly within the NHS
made the scope of work further reduced’ prevent me finding work in a private clinic and diagnose and treatment plan for myself
• ‘Not being able to prescribe treatment on one day (if I chose this path)’ without having to rely on dentist referrals.
the NHS for example, needing an LA [local • ‘Pt’s would have a choice of who they see Be able to work on a rapport with child
anaesthetic] prescription or having to go for treatments and dentists’ books wouldn’t before treatment is complete’.
back to the dentist if they have missed be so busy’
something which can mean having to send • ‘A layer of time has been removed; a child Patient choice (9)
the patient away if the dentist is not in’ requiring preventative treatments could be • ‘Parents could choose to send their kids
• ‘Sometimes the dentist carries out the screened and treated in a single appointment rather than waiting to be referred. Also
treatment without referring on the child rather than a check then a subsequent I don’t think a lot of people are aware
and the child is already happy to attend appointment to provide this care’. children can be seen by other members
the hygienist surgery as they have been of the dental team. I think pt’s appreciate
many times with parents when they were Promote prevention/more appropriate care being referred to the hygienist/therapist
attending for treatment’. (12) more than dentists realise’
• ‘The ability to work under direct access with • ‘More discussion with parents as to what
Views on the future of paediatric dental children I feel would improve prevention treatment they wanted for their children
care in paediatric patients as dentists appear to and what the child would benefit from’
All respondents – whether they treated have little to no time to do this’ • ‘Because parents sometimes ask if their
children or not – were asked whether having an • ‘Unfortunately I am witness to many child can be seen by myself to reinforce all
NHS list number would have an effect on the children offered GA [general anaesthetic] OHI and the dentist won’t refer’
service they were able to provide for children. rather than a little more acclimatisation • ‘Would give more choice for parents
Responses were divided: 55 (30%) said they time or with those with the skills to manage wanting a more proactive approach’.
thought there would be a positive effect, 15 such cases. Paediatric dental care could be
(8%) said it would have a mixed effect, 2 (1%) very well placed with the therapist’ Promote rapport (7)
said there would be a negative effect and 98 • ‘More freedom to change tx [treatment] • ‘I feel that it would ensure that an ongoing
(54%) said there would be no effect (unsure/ plan if you feel it is appropriate, ie pt is relationship would be formed between both
other answers: 13 [7%]). in pain contradicting present plan. Also the hygienist therapist and the patient as
Respondents were asked the same question being able to use F [fluoride] varnish and well as the parent. It would lead to paediatric
with regards to working on a direct patient radiographs without referral would help patients becoming more acclimatised to a
access basis. Here, the response was more improve preventative care’ situation and more comfortable. I also feel
positive, with 82 (45%) saying it would have • ‘Yes, dental decay can progress rapidly in that I am qualified to make a treatment plan
a positive effect, 20 (11%) saying mixed effect, primary teeth and sometimes the time for a paediatric patient – one that often
5 (3%) saying a negative effect and 66 (36%) period between the initial examination differs from another clinician’s treatment
saying no effect (unsure/other answers: 9 with the dentist and the time the patient plan – and that there are some treatments
[5%]). attends for treatment will mean that the that dental clinicians have not heard of or
Comments regarding the benefits of treatment required has changed, having have minimal information on (preformed
direct access cover five themes. Again, some the opportunity to alter treatment to suit metal crowns being at the top of the list)
respondents referred to more than one. the patient’s needs...allows for much more that I feel are excellent, viable treatment
efficient treatment and a better outcome... options’
Efficiency (24) Sometimes children who have high rates of • ‘Sometimes children are scared of “the
• ‘Yes this would help (meet) the demand decay may not attend with the frequency dentist” – hygienist can spend more time
for increasing provision of dental care to which would help benefit their decay building confidence’
children’ progression. Therefore, working on a direct • ‘Also the child seeing one clinician from
• ‘Being able to treatment plan would remove patient access allows all necessary treatment start to end of treatment would be better
the barriers that can slow treatment down. to be carried out without unnecessary delay’. for building a rapport/trust foundation’
It prevents going back and forth from • ‘I try and actively encourage children to
dentist to therapist which can be unsettling Clinical autonomy (10) come to (hygienist) for oral health care
for children. It would allow me to assess • ‘You have the authority to treat a child advice and direct access really helps parents
pts cooperation from day 1 and arrange patient without having to directly follow who frequently ask if their children can
my appts accordingly. Often the dentist a prescription and therefore manage see the hygienist. It’s very rewarding to see
makes appts with me too short/long and treatment as you feel is appropriate’ these children growing up caries free!’
BRITISH DENTAL JOURNAL | ONLINE PUBLICATION | AUGUST 27 2020 5
© The Author(s), under exclusive licence to British Dental Association null
RESEARCH
Other (2) been delegated to dental therapists reports that provision of oral healthcare to older patients
• ‘Direct Access system in general needs interviews using narrative and ethnographic by these same groups of clinicians.
more support from the NHS, it will save techniques revealed overwhelmingly positive The full SDNAP report on children’s oral
them a lot of money if it fully utilised [sic], experiences.10 The need for trust in clinicians health needs was published in 2017.18
and will help dental therapists to carry out and the health system emerged as a key factor in
their full scope of practice’ its acceptability. These findings are supported References
• ‘With a PGD [patient group direction] by a similar UK study which evaluated the 1. Scottish Dental Epidemiological Co-ordinating Committee.
Scotland’s National Dental Inspection Programme. 2003.
there would be no worries about fluoride, acceptability of preformed metal crowns being
Available at http://ndip.minervation.net/wp-content/
LA [local anaesthetic] etc’. placed by dental therapists and hygienists in uploads/2014/07/ndip_scotland2003-P1.pdf (accessed
February 2020).
Scotland.11 High patient and parent satisfaction
2. Scottish Government. An Action Plan for Improving Oral
Comments regarding mixed or negative was reported. Health and Modernising NHS Dental Services in Scotland.
effect (15) A number of earlier studies12,13,14 identified 2005. Available online at http://www.gov.scot/Resource/
Doc/37428/0012526.pdf (accessed October 2016).
• ‘I would have more responsibility in treating reservations on the part of dentists and dental 3. NDIP, ISD Scotland and NHS Scotland. National Dental
patients and make my own decisions as to students regarding developing the teamwork Inspection Programme (NDIP) 2014: Report of the 2014
Detailed National Dental Inspection Programme of
the best way forward for individual patients. model, including knowledge of dental therapists’ Primary 1 children and the Basic Inspection of Primary
I would need to have further training as to remit, concern about patient acceptance, 1 and Primary 7 children. 2014. Available at https://ndip.
scottishdental.org/wp-content/uploads/2014/10/2014-
treatment planning for individuals’ accommodation, availability and supervision. 10-28-NDIP-Report.pdf (accessed February 2020).
• ‘I feel as a hyg/ther I wasn’t trained to deal However, a recent review of the impact of 4. Health and Social Care Information Centre. Children’s
Dental Health Survey: Executive Summary – England,
with children in an emergency setting and dental therapists worldwide concluded: ‘The Wales and Northern Ireland. 2013. Available at https://
feel this would be the way my day would evidence indicates that dental therapists provide files.digital.nhs.uk/publicationimport/pub17xxx/
pub17137/cdhs2013-executive-summary.pdf (accessed
go – seeing kids in pain as some dentists effective, quality, and safe care for children in an February 2020).
are very reluctant to see kids patients [sic] economical manner and are generally accepted 5. General Dental Council. Direct access. 2019. Available
at https://www.gdc-uk.org/information-standards-
especially when they are in pain as they find both by the public and where their use is guidance/standards-and-guidance/direct-access (accessed
it difficult to manage’ established, by the dental profession’.15 February 2020).
6. Nuffield Foundation. Education and Training of Personnel
• ‘Positive: in continuity care (ie not referred A second recent review echoed these Auxiliary to Dentistry. London: Nuffield Foundation, 1993.
between diff people), possibly allow more conclusions, and argued that reform of the 7. Koh R, Pukallus M, Kularatna S et al. Relative cost-
effectiveness of home visits and telephone contacts in
time for prevention and advice. Negative: funding mechanisms and regulations limiting preventing early childhood caries. Community Dent Oral
could still mean ref back to GDP for things patient access to therapists is essential to the Epidemiol 2015; 43: 560–568.
8. Arrow P; Klobas E. Minimum intervention dentistry
outwith scope practice [sic] (depending on removal of barriers to their full use within approach to managing early childhood caries: a
additional training able to be undertaken)’ the NHS.16 Until this last issue is resolved randomized control trial. Community Dent Oral Epidemiol
2015; 43: 511–520.
• ‘I am not able to prescribe local anaesthetic through the matter of NHS provider numbers 9. Teusner D N, Amarasena N, Satur J, Chrisopoulos S,
therefore the patient would have to attend for dental therapists, it has been argued, the Brennan D S. Dental service provision by oral health
therapists, dental hygienists and dental therapists in
the practice for a second visit for an exam recommendations of the 1993 Nuffield Report 6 Australia: implications for workforce modelling. Community
with the dentist to then have to come back will remain unfulfilled.17 Dent Health 2016; 33: 15–22.
10. Dyer T A, Owens J, Robinson P G. The acceptability of care
for another visit for their treatment’.
delegation in skill-mix: the salience of trust. Health Policy
Conclusion 2014; 117: 170–178.
11. Jackson G. Placement of Preformed Metal Crowns on
Discussion Carious Primary Molars by Dental Hygiene/Therapy
The main factors preventing respondents Vocational Trainees in Scotland: A Service Evaluation
A number of studies both in the UK and abroad seeing any children or limiting their role Assessing Patient and Parent Satisfaction. Prim Dent J
2015; 4: 46–51.
have confirmed the value of involving dental with them appear to be: lack of referrals from 12. Ward P. The changing skill mix – experiences on the
therapists and hygienists in providing oral care GDPs; financial implications; or contractual introduction of the dental therapist into general dental
practice. Br Dent J 2006; 200: 193–197.
to children within general dental services. For problems. These restrictions were reported 13. Ross M K, Ibbetson R, Turner S. The acceptability of dually-
example, in the U.S., Koh et al. found that home more frequently by hygienists than therapists qualified dental hygienist-therapists by General Dental
Practitioners in South East Scotland. Br Dent J 2007; DOI:
visits and telephone-based interventions by and it is possible that, as dual qualification and 10.1038/bdj.2007.45.
dental therapists were effective in preventing direct access become more the norm in general 14. Ross M K, Turner S, Ibbetson R J. The impact of
teamworking on the knowledge and attitudes of final year
early childhood caries.7 A study conducted in practice, these restrictions will become less dental students. Br Dent J 2009; 206: 163–167.
Western Australia found that therapists were pervasive. Many saw working with children on 15. Nash D A, Friedman J W, Mathu-Muju K R et al. A review of
the global literature on dental therapists. Community Dent
more effective in providing minimally invasive a direct access basis as being a more efficient Oral Epidemiol 2014; 42: 1–10.
dentistry without recourse to specialist referral arrangement which would enable a more 16. Barnes E, Bullock A, Chestnutt I G, Cowpe J, Moons K,
Warren W. Dental therapists in general dental practice.
than dentists were.8 A second Australian study appropriate and preventive approach. A literature review and case-study analysis to determine
reported that the rate of preventive services While this view chimes with the conclusions what works, why, how and in what circumstances. Eur
J Dent Educ 2020; 24: 109–120.
per patient provided by oral health therapists, of the studies reviewed above, the present 17. Ross M K. Muddy water or a clear horizon? FDJ 2015; 6:
dental hygienists and dental therapists varied study also suggests that there is considerable 74–77.
18. Scottish Dental Needs Assessment Programme. Oral
significantly by the proportion of child patients underuse of hygienists and therapists with Health and Dental Services for Children: Needs Assessment
treated.9 respect to paediatric dental care. In the Report. 2017. Available at http://www.scottishdental.
org/wp-content/uploads/2017/03/SDNAP_Oral-Health-
A UK study based on a purposive sample of 15 companion article to this, similar barriers Dental-Services-for-Children-2017.pdf (accessed July
adults whose care, or that of their children, had and problems were reported regarding the 2020).
6 BRITISH DENTAL JOURNAL | ONLINE PUBLICATION | AUGUST 27 2020
© The Author(s), under exclusive licence to British Dental Association null
You might also like
- Pediatric Restorative DentistryFrom EverandPediatric Restorative DentistrySoraya Coelho LealNo ratings yet
- Dental workforce attitudes on hygienist employment and scopeDocument7 pagesDental workforce attitudes on hygienist employment and scopetea metaNo ratings yet
- Attitudes To and Knowledge About Oral Health Care Among Nursing Home Personnel - An Area in Need of ImprovementDocument6 pagesAttitudes To and Knowledge About Oral Health Care Among Nursing Home Personnel - An Area in Need of ImprovementSaravanan ThangarajanNo ratings yet
- Working Practices and Job Satisfaction of Victorian Dental HygienistsDocument6 pagesWorking Practices and Job Satisfaction of Victorian Dental Hygieniststea metaNo ratings yet
- Specialist and Transitional Care Provision For Amelogenesis Imperfecta - A UK-wide SurveyDocument5 pagesSpecialist and Transitional Care Provision For Amelogenesis Imperfecta - A UK-wide SurveyMohammad Abdulmon’emNo ratings yet
- 1.1 Original ResearchDocument8 pages1.1 Original ResearchNovita RNo ratings yet
- 10 33631-Sabd 1055376-2182384Document10 pages10 33631-Sabd 1055376-2182384rose1999.rjNo ratings yet
- s41415 021 3130 9 PDFDocument12 pagess41415 021 3130 9 PDFrasiNo ratings yet
- Complete Article Apc Jisppd-1Document17 pagesComplete Article Apc Jisppd-1Nishant MehtaNo ratings yet
- Safeguarding Children in Dentistry: 2. Do Paediatric Dentists Neglect Child Dental Neglect?Document6 pagesSafeguarding Children in Dentistry: 2. Do Paediatric Dentists Neglect Child Dental Neglect?bkprosthoNo ratings yet
- Promoting Oral Health in Older PeopleDocument2 pagesPromoting Oral Health in Older PeopleatikramadhaniNo ratings yet
- Attitude ArticleDocument9 pagesAttitude Articlemeena syedNo ratings yet
- Title: Children's Oral Health Strategy in The UKDocument8 pagesTitle: Children's Oral Health Strategy in The UKshahryar eskandarzadeNo ratings yet
- Oral Health PromotionDocument29 pagesOral Health PromotionRob21aNo ratings yet
- Effective Interventions To Prevent Dental Caries in Preschool ChildrenDocument56 pagesEffective Interventions To Prevent Dental Caries in Preschool ChildrenDiego AzaedoNo ratings yet
- Trends in Paediatric First Dental Visit A RetrospeDocument6 pagesTrends in Paediatric First Dental Visit A RetrospeData VaksinNo ratings yet
- Version of Record Doi: 10.1111/IPD.12599Document10 pagesVersion of Record Doi: 10.1111/IPD.12599AndreBarrancoNo ratings yet
- 03 Knowledge Attitudes and Behavior Towards Oral Health Among A Group of Staff Caring For Elderly People in Long Term Care Facilities in Bangkok ThailandDocument16 pages03 Knowledge Attitudes and Behavior Towards Oral Health Among A Group of Staff Caring For Elderly People in Long Term Care Facilities in Bangkok ThailandFadli AlwiNo ratings yet
- 98c458e29834139d9bd40f4a84411bc2Document9 pages98c458e29834139d9bd40f4a84411bc2andres.ft12345No ratings yet
- Foreign LiteratureDocument13 pagesForeign LiteratureJm. n BelNo ratings yet
- 2 Master Article 2Document5 pages2 Master Article 2neetika guptaNo ratings yet
- AAPD Policy on Workforce Issues and Delivery of Oral Health Care Services in a Dental HomeDocument5 pagesAAPD Policy on Workforce Issues and Delivery of Oral Health Care Services in a Dental HomefaizahNo ratings yet
- Ejpd 2018 19 3 3Document6 pagesEjpd 2018 19 3 3Javier Cabanillas ArteagaNo ratings yet
- Review On Infant Oral HealthDocument11 pagesReview On Infant Oral HealthIJAR JOURNALNo ratings yet
- Direct Pulp Capping in Priamry Teeth A Systematic ReviewDocument11 pagesDirect Pulp Capping in Priamry Teeth A Systematic ReviewDaniel Pierre DyotteNo ratings yet
- Public Health Dentistry Thesis TopicsDocument5 pagesPublic Health Dentistry Thesis Topicss0kuzej0byn2100% (2)
- Oral Health in Institutionalised Elderly People in Oslo, Norway and Its Relationship With Dependence and Cognitive ImpairmentDocument8 pagesOral Health in Institutionalised Elderly People in Oslo, Norway and Its Relationship With Dependence and Cognitive ImpairmentTria Sesar AprianiNo ratings yet
- Erosion Guidelines - 2021 - V4 - MJDocument32 pagesErosion Guidelines - 2021 - V4 - MJAARON DIAZ RONQUILLONo ratings yet
- CBOHMaindocument JUNE2014Document66 pagesCBOHMaindocument JUNE2014fashuanmi ibukunNo ratings yet
- Impact of Regular Professional Toothbrushing On Oral Health, Related Quality of Life, and Nutritional and Cognitive Status in Nursing Home ResidentsDocument13 pagesImpact of Regular Professional Toothbrushing On Oral Health, Related Quality of Life, and Nutritional and Cognitive Status in Nursing Home ResidentsMarco Antonio García LunaNo ratings yet
- Using Oral Hygiene Education in Schools To Tackle Child Tooth Decay A Mixed Methods Study With Children and Teachers in EnglandDocument16 pagesUsing Oral Hygiene Education in Schools To Tackle Child Tooth Decay A Mixed Methods Study With Children and Teachers in EnglandDiandra Sariarum DjajakusumahNo ratings yet
- Development of A Model of Care For Dental and Mouth Health in Toddlers With The Game "Ma'Boy" As An Alternative Change in Mother's Behavior and Formation of Children's Teeth-Brushing SkillsDocument9 pagesDevelopment of A Model of Care For Dental and Mouth Health in Toddlers With The Game "Ma'Boy" As An Alternative Change in Mother's Behavior and Formation of Children's Teeth-Brushing SkillsInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Hill Adult Dental Health SurveyDocument8 pagesHill Adult Dental Health Surveydesy purnama sariNo ratings yet
- Oral Health Promotion and Intervention Activities Carried Out in Rural Areas of Davangere DistrictDocument49 pagesOral Health Promotion and Intervention Activities Carried Out in Rural Areas of Davangere DistrictShabby PoetNo ratings yet
- NHS England Paediatric DentistryDocument15 pagesNHS England Paediatric DentistryDina ElkharadlyNo ratings yet
- Oral Health ProgramDocument8 pagesOral Health Programapi-292263050No ratings yet
- The Shortened Dental Arch Concept Awareness and Opinion of Dentists in Australia PDFDocument8 pagesThe Shortened Dental Arch Concept Awareness and Opinion of Dentists in Australia PDFKarina OjedaNo ratings yet
- Community Project 1Document10 pagesCommunity Project 1Scott Michael SonnierNo ratings yet
- Assessment of Knowledge Attitude and Perception of Dental Students Towards Obesity in Kanpur CityDocument6 pagesAssessment of Knowledge Attitude and Perception of Dental Students Towards Obesity in Kanpur CityAdvanced Research PublicationsNo ratings yet
- Keywords:-Data Collection and Evaluation, UKGSDocument11 pagesKeywords:-Data Collection and Evaluation, UKGSInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Oral Health Education Improved Oral Health KnowledgeDocument11 pagesOral Health Education Improved Oral Health KnowledgeGita PratamaNo ratings yet
- Adj 12749Document10 pagesAdj 12749Irfan HussainNo ratings yet
- Application of Machine Learning For Diagnostic Prediction of Root CariesDocument10 pagesApplication of Machine Learning For Diagnostic Prediction of Root CariesHarisankar BNo ratings yet
- International Association of Dental Traumatology Guidelines For The Management of Traumatic Dental Injuries: 3. Injuries in The Primary DentitionDocument44 pagesInternational Association of Dental Traumatology Guidelines For The Management of Traumatic Dental Injuries: 3. Injuries in The Primary DentitionaNo ratings yet
- Index for Interceptive ReferralDocument22 pagesIndex for Interceptive Referral강북다인치과No ratings yet
- Longetivity of DentureDocument9 pagesLongetivity of DentureShyam DangarNo ratings yet
- Thesis Topics Public Health DentistryDocument5 pagesThesis Topics Public Health DentistryKristen Flores100% (2)
- Oral Health Coalition: Knowledge, Attitude, Practice Behaviours Among Gynaecologists and Dental PractitionersDocument8 pagesOral Health Coalition: Knowledge, Attitude, Practice Behaviours Among Gynaecologists and Dental PractitionersIndah AmaliaNo ratings yet
- 40368_2022_Article_721Document8 pages40368_2022_Article_721cosadedubsNo ratings yet
- Attitudes and Lifestyle Factors in Relation To Oral Health and Dental Care in Sweden A Cross Sectional StudyDocument9 pagesAttitudes and Lifestyle Factors in Relation To Oral Health and Dental Care in Sweden A Cross Sectional Studyasem sardyNo ratings yet
- Healthcare 10 00406Document12 pagesHealthcare 10 00406AamirNo ratings yet
- Desai 2001Document11 pagesDesai 2001Layal J. AlQahtaniNo ratings yet
- Analysis of Oral Hygiene Education in Obese Children in Local Population of PakistanDocument5 pagesAnalysis of Oral Hygiene Education in Obese Children in Local Population of PakistaniajpsNo ratings yet
- Jurnal Kedokteran Gigi TerindeksDocument5 pagesJurnal Kedokteran Gigi TerindeksALFEARA YUNIARNo ratings yet
- HSDC QuintesenceDocument6 pagesHSDC QuintesenceDavid CasaverdeNo ratings yet
- P DentalhomeDocument5 pagesP Dentalhomemehta15drishaNo ratings yet
- 6 - Original Article PDFDocument7 pages6 - Original Article PDFIna BogdanNo ratings yet
- Policy On Model Dental Benefits For InfantsDocument4 pagesPolicy On Model Dental Benefits For InfantsمعتزباللهNo ratings yet
- Examining The Oral Health of Filipinos: Policy Analysis: Original ArticleDocument7 pagesExamining The Oral Health of Filipinos: Policy Analysis: Original ArticleTimothy LimaNo ratings yet
- Booklet - e 1 - 2013Document101 pagesBooklet - e 1 - 2013Dani AedoNo ratings yet
- Measurement and Correlates of Family Caregiver Self-Efficacy For Managing DementiaDocument9 pagesMeasurement and Correlates of Family Caregiver Self-Efficacy For Managing DementiariskhawatiNo ratings yet
- Borderline Personality DisorderDocument7 pagesBorderline Personality DisorderleaNo ratings yet
- Chapter 1 2 3Document77 pagesChapter 1 2 3Ferissa MohammadNo ratings yet
- Should Homework Be Banned From School?Document7 pagesShould Homework Be Banned From School?Chuyên ĐỗNo ratings yet
- Intrathecal MTX & Cytarabine & Hydrocortisone V4 2.15Document2 pagesIntrathecal MTX & Cytarabine & Hydrocortisone V4 2.15GabrielNo ratings yet
- Question and AnswerDocument4 pagesQuestion and AnswerShaf AbubakarNo ratings yet
- TC Elastomeric Tapes SDS Rev 3, 2-19 - 1 PDFDocument6 pagesTC Elastomeric Tapes SDS Rev 3, 2-19 - 1 PDFEbondNo ratings yet
- Nelson Textbook of Pediatrics (2-Volume Set) by Robert M. Kliegman, Bonita F. Stanton, Joseph W. ST Geme III, Nina F. SchorDocument312 pagesNelson Textbook of Pediatrics (2-Volume Set) by Robert M. Kliegman, Bonita F. Stanton, Joseph W. ST Geme III, Nina F. SchorFaisal MomenNo ratings yet
- Tung DocumentreviewDocument8 pagesTung DocumentreviewRodrigo Bittencourt100% (3)
- Perioperative Concepts and Nursing ManagementDocument107 pagesPerioperative Concepts and Nursing ManagementHarley Justiniani Dela CruzNo ratings yet
- SIP Physical SCiDocument8 pagesSIP Physical SCiShane Catherine BesaresNo ratings yet
- Introduction of Online Basic First Aid Course - For Circulation April 2021Document39 pagesIntroduction of Online Basic First Aid Course - For Circulation April 2021Yuwaraj NaiduNo ratings yet
- Pathology of the EndocardiumDocument31 pagesPathology of the EndocardiumAlexe VladNo ratings yet
- Acute Respiratory Distress Syndrome: Jason D. Sciarretta, M.D. Critical Care Conference October 13, 2010Document24 pagesAcute Respiratory Distress Syndrome: Jason D. Sciarretta, M.D. Critical Care Conference October 13, 2010JelenaNo ratings yet
- Small-Sided Games and Integrating Physical PreparationDocument196 pagesSmall-Sided Games and Integrating Physical Preparationbolebs1475% (4)
- BCS Class of DrugsDocument45 pagesBCS Class of DrugsLionO50% (2)
- Amway ProductDocument9 pagesAmway ProductAbu Sayed Md. RashedNo ratings yet
- Mercury in The MistDocument2 pagesMercury in The MistAnand BhagwaniNo ratings yet
- AOTA Statement On Role of OT in NICUDocument9 pagesAOTA Statement On Role of OT in NICUMapi RuizNo ratings yet
- Grain Legumes/Pulses Introduction and ImportanceDocument5 pagesGrain Legumes/Pulses Introduction and ImportancesumandhakalNo ratings yet
- Health Information Technology-HISMLSDocument1 pageHealth Information Technology-HISMLSJanela Escalante TaboraNo ratings yet
- Strain Index Scoring Sheet: Date: Task: Company: Supervisor: Dept: EvaluatorDocument1 pageStrain Index Scoring Sheet: Date: Task: Company: Supervisor: Dept: EvaluatorUdaydeep SinghNo ratings yet
- Effects of Energy Gel Ingestion On Blood Glucose, Lactate, and Performance Measures During Prolonged CyclingDocument9 pagesEffects of Energy Gel Ingestion On Blood Glucose, Lactate, and Performance Measures During Prolonged Cyclingjose david HerreraNo ratings yet
- Project ProposalDocument16 pagesProject ProposalMashaal FasihNo ratings yet
- ICICI Bank Mortgage - HS360 Product FinalDocument29 pagesICICI Bank Mortgage - HS360 Product FinalRishu GiriNo ratings yet
- Veteran Resource Guide For Congressional District 9Document27 pagesVeteran Resource Guide For Congressional District 9RepSinemaNo ratings yet
- Babu Jagjivan RamDocument24 pagesBabu Jagjivan RamAnonymous qFWInco8cNo ratings yet
- Change Your Life in 7 Days With NLP - Paul Mckenna BrochureDocument2 pagesChange Your Life in 7 Days With NLP - Paul Mckenna Brochureapi-385316675% (4)
- HRM Case StudyDocument21 pagesHRM Case StudyNabil Eyg Iakini100% (1)